INTRODUCTION
Trauma continues to be the leading cause of death and acquired disability in children and adolescents.[1–8] In the United States, 12,000 children die from injury each year.[6] The temporal nature of death in adult trauma patients has been extensively studied, beginning with Trunkey’s adult cohort study which described a trimodal distribution of death after traumatic injury.[9] In this study, most patients died immediately after injury, with a second peak of mortality in the first few hours, and a third peak due to late complications related to trauma (typically occurring more than one week after injury). Recent studies have challenged this trimodal concept, suggesting a shift in the temporality of trauma deaths largely from a decline in late mortality.[10–17] It is not known if these patterns are observed after pediatric injury. Although the overall principles of pediatric trauma care are similar to those for adult trauma care, important differences in mechanism of injury, anatomy, and physiology are observed between adults and children that lead to many differences in initial care.[18] Children have fewer or no comorbid conditions compared to adults, and are not as likely to succumb to long-term complications occurring after injury. Furthermore, adult trauma centers are more mature and numerous than pediatric trauma centers in the United States, and the incorporation of pediatric trauma centers into trauma systems may lead to differences in outcomes.[19,20]
The purpose of this study was to investigate the temporal distribution of death after injury in children compared to adults. We hypothesized that the temporal distribution of mortality is different in pediatric and adult trauma patients, with a greater proportion of pediatric mortality in the “early” timeframe. We also performed secondary analyses to determine predictors of late mortality and prevalence of complications associated with late mortality.
METHODS
Study Design and Patient Selection
We performed a retrospective cohort study of patients treated at trauma centers in the United States from 2007–2014 using the American College of Surgeons National Trauma Data Bank® (NTDB®) Research Dataset (RDS). Patients were included in this study if they were less than 65 years old and had either an ED or inpatient discharge disposition code of died or expired. Patients were excluded if they sustained burn, drowning, hanging, or military injuries; or if they were transferred from a referral center. Patients were categorized as children (0–14 years) or adult (15–64 years) for the primary analysis and were further stratified for secondary analyses based on the Centers for Disease Control defined ranges (<1 year, 1–4 years, 5–9 years, 10–14 years, 15–24 years). [6]
Categorization of Death and Calculation of Time to Death
The primary outcome for this study was death by phase of care (dead on arrival [DOA], emergency department [ED], early inpatient [≤24 h], and late inpatient [>24 h]) for children compared to adults. Patients were categorized as dead on arrival, died in ED, or inpatient death based on the emergency department disposition and hospital discharge disposition variables (all years) as well as time of ED phase of care combined with death in ED (2007–2010 datasets) or absent signs of life on arrival variables (2011–2014 datasets). Specific combinations of disposition codes and categorization schema are tabulated in Appendix A. Total number of EMS minutes (EMSMINS), minutes in the ED (EDMIN), and length-of-stay minutes (LOSMIN) were used to calculate the total time to death for patients who survived ED resuscitation. Time was modeled in two ways: 1) dichotomized into early inpatient mortality (≤24 h) or late inpatient mortality (>24 h) for the primary outcome, and 2) treated as a continuous interval variable for survival analysis for the secondary outcome of inpatient time to death. Inpatient time was not calculated for patients who died on arrival or died in ED.
Predictors of Early versus Late Mortality
To better understand risk factors for mortality, demographic and clinical variables potentially related to mortality were modeled, including: age, gender, race, ethnicity, insurance status, physiologic variables, mechanism of injury, severity of injury (using Abbreviated Injury Scales) and procedures within the first day of admission. Race was determined using the “RACE1” and “RACE2” variables, and a “multiracial” category was created to account for the reporting of more than 1 race per person. Primary payment method was classified into three groups: “no insurance” (self-pay, not billed, and other), “Medical/Medicaid” (Medicaid and Medicare), and “private insurance” (Blue Cross/Blue Shield, no fault automobile, worker’s compensation, private/commercial insurance, and other government). Systolic blood pressure and heart rate were adjusted for age using normative values used in Pediatric Advanced Life Support (PALS) and transformed to dichotomous age-adjusted variables for hypotension, tachycardia, and bradycardia.[21] External cause of injury codes (ECODES) were used to classify whether a patient suffered a blunt or penetrating injury. The maximum Abbreviated Injury Score (AIS) was calculated for head and neck, face, thorax, abdomen, extremity, and external using predot codes and severity variables.[22] Specific procedures (endotracheal intubation, chest tube placement, transfusion, craniotomy, thoracotomy, and laparotomy) were identified by ICD-9 codes and included if they occurred within the first 24 hours after injury.
Complications in Late Mortality Patients
To assess for prevalence of complications in the late mortality subgroup, complication codes were used to identify specific complications including: acute respiratory distress syndrome, pneumonia, acute kidney failure/injury, deep venous thrombosis or pulmonary embolism (DVT/PE), decubitus ulcer, urinary tract infection, sepsis, catheter associated bloodstream infection, pulmonary thrombosis, and deep space surgical site infection (SSI). Due to known variability in reporting of complications between centers and to decrease the impact of reporting bias, the analysis of complications was conducted on a subset of patients treated at trauma centers that have a history of reporting these complications to the database using previously described methodology.[23]
Statistical Analysis
Descriptive analyses were performed to report the frequency counts and percentages for categorical variables. Because all continuous variables were not normally distributed, the median and interquartile ranges were reported. A chi-square test or Fisher’s exact test were used to determine if categorical variables differed between pediatric and adult groups, as well as between early and late mortality groups in pediatric trauma patients. The Wilcoxon-Mann-Whitney test was used to analyze the difference between early and late pediatric mortality groups for continuous variables. Inpatient mortality over time for patients surviving ED resuscitation was assessed with Kaplan-Meier survival plots and testing the equality over strata using the Kruskal-Wallis test, because no censored observations occurred. Odds ratios and 95% confidence intervals were reported for the logistic regression model looking at the outcome of early versus late mortality for pediatric trauma patients. Model covariates included age, gender, race, ethnicity, mechanism, AIS head and neck, AIS face, AIS chest, AIS abdomen, AIS extremity, AIS external, endotracheal intubation, chest tube placement, transfusion, craniotomy, thoracotomy, laparotomy, bradycardia, tachycardia, hypotension, and insurance payment. For variables that had 10% or more of the data missing (race, ethnicity, hypotension, and insurance payment), a “not specified” or “not reported” category was created to account for this group. Otherwise, patients with missing data on single variables were excluded from the multivariable analysis. Significance tests were two-tailed, with α=0.05. All analyses were performed using SAS software v. 9.4 (SAS Institute Inc).
RESULTS
From 2007 to 2014, 5,836,507 patients were entered into the National Trauma Database. After excluding transfer patients, we identified 109,688 pediatric and adult patients that died (either on arrival, in the ED, or as inpatients). Pediatric patients had a lower proportion of male patients, higher rate of blunt trauma, greater frequency of head and neck injuries, lower rates of procedures, and a higher frequency of bradycardia (Table 1).
Table 1.
Patient Characteristics for Pediatric and Adult Patients (N=109,688).
| Characteristics | N | Pediatric (0–14 y) |
N | Adult (15+ y) |
|---|---|---|---|---|
| Median (IQR) | Median (IQR) | |||
| Age | 5463 | 5 (2, 11) | 104225 | 35 (24, 50) |
| N (%) | N (%) | |||
| Gender | 5455 | 103971 | ||
| Male | 3402 (62.36) | 83047 (79.88) | ||
| Female | 2053 (37.64) | 20924 (20.12) | ||
| Race | 5463 | 104225 | ||
| White | 2530 (46.31) | 55067 (52.83) | ||
| Asian | 94 (1.72) | 1706 (1.64) | ||
| Native Hawaiian or Other Pacific Islander | 18 (0.33) | 220 (0.21) | ||
| Other Race | 915 (16.75) | 11963 (11.48) | ||
| American Indian | 31 (0.57) | 509 (0.49) | ||
| Black or African American | 1412 (28.85) | 27837 (26.71) | ||
| Multiracial | 5 (0.09) | 36 (0.03) | ||
| Race not Specified | 458 (8.38) | 6887 (6.61) | ||
| Ethnicity | 5463 | 104225 | ||
| Hispanic or Latino | 1097 (20.08) | 13805 (13.25) | ||
| Not Hispanic or Latino | 2889 (52.88) | 61197 (58.72) | ||
| Ethnicity not Specified | 1477 (27.04) | 29223 (28.04) | ||
| Mechanism | 5463 | 104225 | ||
| Blunt | 4549 (83.27) | 65566 (62.91) | ||
| Penetrating | 884 (16.18) | 37730 (36.20) | ||
| Combined | 30 (0.55) | 929 (0.89) | ||
| Median (IQR) | Median (IQR) | |||
| AIS Head and Neck | 5384 | 4 (0, 5) | 102870 | 3 (0, 5) |
| AIS Face | 5384 | 0 (0, 1) | 102870 | 0 (0, 1) |
| AIS Chest | 5384 | 0 (0, 3) | 102870 | 2 (0, 4) |
| AIS Abdomen | 5384 | 0 (0, 1) | 102870 | 0 (0, 2) |
| AIS Extremity | 5384 | 0 (0, 2) | 102870 | 0 (0, 2) |
| AIS External | 5384 | 0 (0, 0) | 102870 | 0 (0, 0) |
| N (%) | N (%) | |||
| Hospital Procedures* in First 24h | ||||
| Endotracheal Intubation | 5326 | 62 (1.16) | 101979 | 4150 (4.07) |
| Chest Tube Placement | 5326 | 823 (15.45) | 101979 | 24633 (24.15) |
| ICP Monitor Placement | 5326 | 619 (11.62) | 101979 | 8914 (8.74) |
| Transfusion | 5326 | 1223 (22.96) | 101979 | 23004 (22.56) |
| Craniotomy | 5326 | 605 (11.36) | 101979 | 10156 (9.96) |
| Thoracotomy | 5326 | 633 (11.89) | 101979 | 19735 (19.35) |
| Laparotomy | 5326 | 939 (17.63) | 101979 | 29643 (29.07) |
| Procedure for Extremity Hemorrhage Control | 5326 | 12 (0.23) | 101979 | 737 (0.72) |
| Angiography | 5326 | 1607 (30.17) | 101979 | 36392 (35.69) |
| Bradycardia | 5086 | 2570 (50.53) | 97837 | 40405 (41.30) |
| Tachycardia | 5086 | 1263 (24.83) | 97837 | 31604 (32.30) |
| Hypotension | 5463 | 104225 | ||
| Yes | 2658 (48.65) | 47566 (45.64) | ||
| No | 2243 (41.06) | 49376 (47.37) | ||
| Not reported | 562 (10.29) | 7283 (6.99) | ||
| Payment | 5463 | 104225 | ||
| Private Insurance | 1786 (32.69) | 33532 (32.17) | ||
| No Insurance | 1134 (20.76) | 42618 (40.89) | ||
| Medical/Medicaid | 1856 (33.97) | 14729 (14.13) | ||
| Payment not Specified | 687 (12.58) | 13346 (12.80) |
AIS = Abbreviated Injury Scale; IQR = interquartile range; ICP = intracranial pressure
Hospital procedures were not mutually exclusive from one another.
Mortality by categorical phase of care (on arrival, in ED, inpatient <24h, and inpatient >24h) differed between pediatric and adult patients, with a higher proportion of death on arrival and ED death for children compared to adults and a higher proportion of adults with inpatient deaths (p<0.01; Figure 1). A Kaplan-Meir survival plot of inpatient hours after ED resuscitation for pediatric (0–14 years), adolescent (15–24 years), and adult (25–64 years) strata showed significant differences, with the shortest median time to death in the adolescent group and the longest in adults (0.78 days versus 1.55 days, p<0.001, Figure 2a). Survival analysis for pediatric-aged patients who survived ED resuscitation showed statistically different (p<0.001) survival among the four age strata, with longer median time to death for children under one year of age compared to children ages 1–14 years old (1.83 days versus 0.99–1.15 days, p<0.001, Figure 2b).
Figure 1. Percent Mortality by Phase of Care for Pediatric (0–14 y) and Adult (15–64 y) Patients.
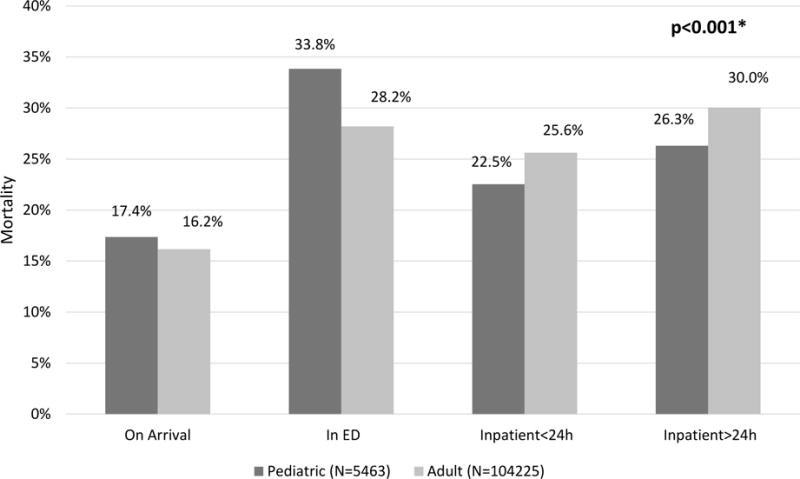
*P-value from chi-square test comparing death categories between pediatric and adults.
Figure 2. Inpatient Mortality Over Days for Patients Who Survived ED Resuscitation Stratified by: A) Children, Adolescent, and Adult groups and B) Pediatric Age Strata.
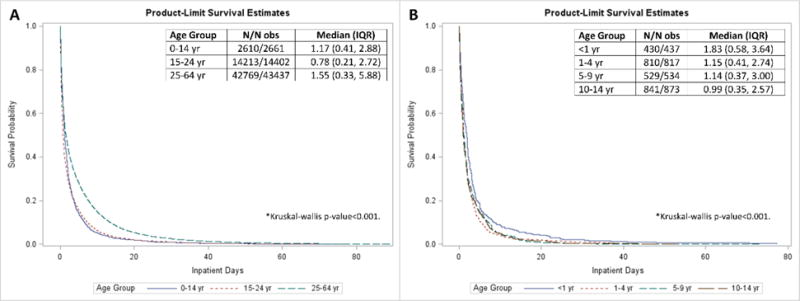
*N/N obs = Observations used/Total observations; IQR=Interquartile range.
Of the pediatric patients (age 1–14 years) who died, 4,027 (74%) were early deaths (DOA, ED, and inpatient ≤ 24h) and 1,436 (26%) were late (inpatient >24h) patients. Groups were similar with respect to gender, race, and ethnicity (Table 2). The early mortality group was older, had higher frequency of penetrating injuries, higher frequency of bradycardia, lower frequency of tachycardia, and a higher frequency of hypotension compared to the late mortality group (all p-values<0.01). In the first 24 hours, early mortality patients had a higher percentage of chest tube placement and thoracotomy, while late mortality patients had a higher rate of endotracheal intubation, ICP monitor placement, transfusion, craniotomy, laparotomy, and angiography (all p-values<0.01).
Table 2.
Unadjusted Univariate Comparison and Multivariate Logistic Regression of Predictors of Early (≤24h) versus Late (>24h) Mortality for Pediatric Trauma Patients (0–14 y).
| Early Mortality (≤24h) |
Late Mortality (>24h) | Unadjusted | Multivariate Logistic Regression | ||||
|---|---|---|---|---|---|---|---|
| N | Median (IQR) |
N | Median (IQR) | p-value | Odds Ratio (95% CI) |
p-value | |
| Age, y | 4027 | 5 (2, 11) | 1436 | 4 (1, 11) | <0.01 | 1.05 (1.03, 1.07) | <0.01 |
| N | N (%) | N | N (%) | ||||
| Gender | 4021 | 1434 | 0.12 | ||||
| Male | 2532 (63.0 | 870 (60.7) | Reference | ||||
| Female | 1489 (37.0) | 564 (39.3) | 0.97 (0.82, 1.15) | 0.76 | |||
| Race | 4027 | 1436 | 0.08 | ||||
| White | 1819 (45.2) | 711 (49.51) | Reference | ||||
| Asian | 68 (1.7) | 26 (1.81) | 1.00 (0.56, 1.78) | 0.99 | |||
| Native Hawaiian or Other Pacific Islander | 15 (0.4) | 3 (0.21) | 1.88 (0.42, 8.43) | 0.41 | |||
| Other Race | 674 (16.7) | 241 (16.8) | 0.93 (0.71, 1.22) | 0.6 | |||
| American Indian | 25 (0.6) | 6 (0.4) | 1.76 (0.56, 5.49) | 0.33 | |||
| Black or African American | 1068 (26.5) | 344 (24.0) | 1.05 (0.86, 1.29) | 0.65 | |||
| Multiracial | 3 (0.1) | 2 (0.1) | 0.19 (0.02, 1.96) | 0.16 | |||
| Race not Specified | 355 (8.8) | 103 (7.2) | 1.10 (0.79, 1.54) | 0.58 | |||
| Ethnicity | 4027 | 1436 | 0.68 | ||||
| Hispanic or Latino | 820 (20.4) | 277 (19.3) | Reference | ||||
| Not Hispanic or Latino | 2120 (52.6) | 769 (53.6) | 1.05 (0.80, 1.38) | 0.73 | |||
| Ethnicity not Specified | 1087 (27.0) | 390 (27.2) | 0.82 (0.62, 1.09) | 0.18 | |||
| Mechanism | 4027 | 1436 | <0.01 | ||||
| Blunt | 3238 (80.4) | 1311 (91.3) | Reference | ||||
| Penetrating | 761 (18.9) | 123 (8.6) | 1.83 (1.40, 2.39) | <0.01 | |||
| Combined | 28 (0.7) | 2 (0.1) | 3.51 (0.74, 16.53) | 0.11 | |||
| N | Median (IQR) | N | Median (IQR) | ||||
| AIS Head and Neck | 3959 | 4 (0, 5) | 1425 | 5 (4, 5) | <0.01 | 0.81 (0.78, 0.84) | <0.01 |
| AIS Face | 3959 | 0 (0, 1) | 1425 | 0 (0, 1) | <0.01 | 0.98 (0.88, 1.09) | 0.68 |
| AIS Chest | 3959 | 0 (0, 3) | 1425 | 0 (0, 3) | 0.41 | 0.94 (0.90, 0.99) | 0.02 |
| AIS Abdomen | 3959 | 0 (0, 1) | 1425 | 0 (0, 2) | 0.67 | 1.12 (1.05, 1.19) | <0.01 |
| AIS Extremity | 3959 | 0 (0, 2) | 1425 | 0 (0, 2) | 0.16 | 0.99 (0.92, 1.07) | 0.87 |
| AIS External | 3959 | 0 (0, 0) | 1425 | 0 (0, 0) | 0.05 | 1.04 (0.85, 1.27) | 0.71 |
| N | N (%) | N | N (%) | ||||
| Hospital Procedures in First 24h* | |||||||
| Endotracheal Intubation | 3912 | 30 (0.8) | 1414 | 32 (2.3) | <0.01 | 0.32 (0.16, 0.65) | <0.01 |
| Chest Tube Placement | 3912 | 653 (16.7) | 1414 | 170 (12.0) | <0.01 | 1.57 (1.22, 2.02) | <0.01 |
| ICP Monitor | 3912 | 258 (4.0) | 1414 | 461 (32.6) | <0.01 | 0.28 (0.22, 0.35) | <0.01 |
| Placement | |||||||
| Transfusion | 3912 | 714 (18.3) | 1414 | 509 (36.0) | <0.01 | 0.89 (0.74, 1.08) | 0.24 |
| Craniotomy | 3912 | 163 (4.2) | 1414 | 442 (31.3) | <0.01 | 0.33 (0.26, 0.42) | <0.01 |
| Thoracotomy | 3912 | 540 (13.8) | 1414 | 93 (6.6) | <0.01 | 1.36 (1.01, 1.84) | 0.04 |
| Laparotomy | 3912 | 541 (13.8) | 1414 | 398 (28.2) | <0.01 | 0.69 (0.56, 0.86) | <0.01 |
| Procedure for Extremity Hemorrhage Control | 3912 | 7 (0.2) | 1414 | 5 (0.4) | 0.32 | 0.65 (0.15, 2.86) | 0.57 |
| Angiography | 3912 | 860 (22.0) | 1414 | 747 (52.8) | <0.01 | 0.42 (0.35, 0.50) | <0.01 |
| Bradycardia | 3691 | 2249 (60.9) | 1395 | 321 (23.0) | <0.01 | 2.19 (1.77, 2.71) | <0.01 |
| Tachycardia | 3691 | 720 (19.5) | 1395 | 543 (38.9) | <0.01 | 0.85 (0.70, 1.04) | 0.12 |
| Hypotension | 4027 | 1436 | <0.01 | ||||
| Yes | 2327 (57.8) | 331 (23.1) | Reference | ||||
| No | 1218 (30.3) | 1025 (71.4) | 0.42 (0.35, 0.51) | <0.01 | |||
| Not reported | 482 (12.0) | 80 (5.6) | 0.96 (0.66, 1.39) | 0.82 | |||
| Payment | 4027 | 1436 | <0.01 | ||||
| Private Insurance | 1330 (33.0) | 456 (31.8) | Reference | ||||
| No Insurance | 923 (22.9) | 211 (14.7) | 0.94 (0.74, 1.20) | 0.61 | |||
| Medical/Medicaid | 1270 (31.5) | 586 (40.8) | 0.58 (0.48, 0.70) | <0.01 | |||
| Payment not Specified | 504 (12.5) | 183 (12.7) | 0.60 (0.46, 0.79) | <0.01 | |||
AIS = Abbreviated Injury Scale; IQR = interquartile range; ICP = intracranial pressure
Hospital procedures were not mutually exclusive from one another.
In a multivariate logistic regression model (Table 2), the odds of early mortality increased with age, penetrating mechanism, bradycardia, hypotension, and higher AIS score for abdominal injuries (all p<0.05). Conversely head, neck, and chest injuries were associated with a lower odds of early mortality. There appears to be a statistically lower risk of early mortality for patients who received certain procedures in the first 24 hours after injury (endotracheal intubation, ICP monitor placement, craniotomy, laparotomy, or angiography), but this lower odds ratio likely represents survival bias as emergent procedures often performed in the ED including chest tube placement (OR 1.57, CI 1.22–2.02) and thoracotomy (OR 1.36, CI 1.01–1.84) were predictors for early mortality.
Subgroup analysis of complications in late inpatient mortality patients that were treated at centers that report complications (N=889) showed that acute respiratory distress syndrome was the most common complication followed by pneumonia. The overall rate of reported complications in patients with late mortality was low (Table 3).
Table 3.
Complication Prevalence in Late Mortality Pediatric Patients (N=889).
| Complication type* | N (%) |
|---|---|
| Acute Respiratory Distress Syndrome | 127 (14.29) |
| Pneumonia | 69 (7.76) |
| Acute Kidney Failure/Injury | 29 (3.26) |
| DVT/PE | 10 (1.12) |
| Decubitus Ulcer | 9 (1.01) |
| Urinary Tract Infection | 6 (0.67) |
| Sepsis | 4 (0.45) |
| Catheter Associated Bloodstream Infection | 1 (0.11) |
| Pulmonary Thrombosis | 1 (0.11) |
| Deep Space SSI | 0 (0) |
Complication types were not mutually exclusive from one another.
DISCUSSION
This study used the NTDB to determine the temporal distribution of death in pediatric trauma patients and compare this to adults. We have demonstrated that the temporal pattern of mortality in children is similar to that of adults, with pediatric patients having a small but significantly higher incidence of early deaths than adults. Penetrating mechanism, physiological factors (bradycardia and hypotension) and severe torso injuries were associated with early mortality, and craniotomy and ICP monitor placement were associated with late deaths. Infants under one year of age had the longest time to death, which we speculate may be related to the greater incidence of abusive head trauma in this population and the inherent time delay of brain death determination leading to longer survival times. Adolescents that survived the initial resuscitation had a temporal distribution of mortality more similar to young children than that of adults – likely related to fewer comorbidities and chronic health conditions that may predispose to late mortality.
This study provides important insight into the epidemiology of timing of mortality in injured children and an initial exploratory analysis of factors associated with mortality. While we attempted to associate hospital procedures with early mortality, the time scale available in the NTDB RDS (24 hour intervals) is not precise enough to infer any association of timing of intervention with outcomes in this severely injured sample. As with other retrospective cohorts, many of the associations with procedures and physiologic variables are difficult to interpret due to survival bias. Despite these limitations, the demonstrated pattern of mortality in children suggests that continued research and development of interventions to prevent or provide early treatment to injury is likely to have the greatest impact on decreasing death and disability in children.
Children who survived past 24 hours were most likely to undergo the procedures that we studied. This finding is likely explained by survival bias, as children who died early did not have time to undergo most procedures. Conversely, chest tube placement and thoracotomy were more likely in patients who suffered early mortality, an expected finding given that these procedures are often performed in the ED for patients who are either pulseless or in extremis.[24,25] Reported complication rates in children suffering late death are relatively low, which suggests that mortality in this group is not commonly related to complications – but these low complication rates must be interpreted cautiously due to known problems with reporting bias related to complications in the NTDB.[23]
Our study provides an important comparison to the growing body of literature in adults, which suggests that a higher proportion of early trauma deaths (≤24 hrs) than reported in Trunkey’s landmark study.[11,12] Our study must be interpreted within the context of the data source, however, as studies using NTDB or similar hospital data do not account for patients who are declared dead on scene and therefore never arrive at the hospital. Within Los Angeles County, 20% of patients are pronounced dead on scene and not transported to hospitals as described by Demetriades.[12] Similarly, studies often use different definitions of “early” versus “late” death, which can greatly affect the pattern of distribution of death. It is also very possible that advances in trauma care overall have led to a decline in late deaths, causing an increase in the proportion of reported early deaths.[11] Our rate of 74% early mortality (≤24h) in pediatric patients is within range of more recent adult literature,[11,12,14,15,17]. We have shown a lower proportion of late mortality in children compared to adults, which is likely related to significant comorbidities in the adult cohort. These comorbidities have been shown by Valdez et al to be associated with late death.[14]
Understanding the nuances of data associated with a high early death rate shown in this study is needed. While penetrating mechanism was associated with early death among children, the adult cohort had a much higher proportion of penetrating trauma, which has consistently been associated with early death among adults.[11,12,14,15] This higher proportion of penetrating injury implies that the adult cohort should have higher early death rates, the opposite of which was found. We suspect this difference in early mortality is more likely due to a significant proportion of children with blunt trauma who were declared DOA or in the ED after failed resuscitation. These children may not have had vital signs or a pulse in the field, and we did not adjust for how long CPR was performed prior to arrival; as it has been shown that out-of-hospital cardiac arrest is associated with extremely high mortality rates, particularly in children.[26,27] Children with no signs of life are more likely to be transported to a hospital than adults, which introduces selection bias into a dataset that only includes patients treated at hospitals. This form of selection bias due to differential EMS transport practices for children compared to adults is similar to the argument made by Gunst et al,[11] that the high early death rate could be attributed to a disproportionately low number of pediatric patients being declared dead at the scene, leading to many being declared DOA or in the ER after a failed resuscitation. Termination of resuscitation protocols for EMS have been implemented for adults,[28–30] children have generally been excluded, and are currently recommended to undergo resuscitative efforts by EMS providers in all but the most obvious cases of futility, such as decapitation or hemicorporectomy.[31]
Alternatively, it has been debated whether children receive suboptimal prehospital care when compared to adults, although the literature is inconclusive.[32–37] Many have suggested that specific training, including pediatric advanced life support (PALS), may improve outcomes.[38–41] Simulation-based training is being increasingly used in a variety of clinical scenarios, and has shown promise in early resuscitation training for pediatric trauma, though further studies are needed to measure the impact on clinical outcomes. [42–44]
This study has several limitations. First, the NTDB accounts only for in-hospital deaths, and does not account for patients who are declared dead on scene. We suspect this introduces selection bias that disproportionately affects children over adults, thereby increasing the DOA category for children as EMS teams may be uncomfortable declaring death in a pediatric patient.[28] The NTDB also only includes patients treated at a trauma center, not capturing those patients cared for at non-trauma centers. This population may be sizable, and could bias our study by affecting adults versus children differently. Our study also demonstrated that the frequency of reported complications in pediatric trauma patients is low, which is inherently subject to reporting bias and limits interpretation of these findings to hypothesis generation alone. We have tried to minimize this bias by only analyzing complications in centers that have demonstrated prior reporting of complications as described by Kardooni.[23] Procedure coding could similarly have been incomplete, biasing our results. Glasgow Coma Score (GCS) was not included in our study due to known frequent lack of documentation and consistency among providers.[45] Insurance status was included in our models, but the true impact of this is likely overstated as the incidence of insurance status misclassification is as high as 30% in trauma patients dying in the emergency department.[46] Finally, survival bias limits the ability to infer any causal association for any of the procedural factors associated with mortality. Despite these limitations, our study exhibits strength in its very large sample size, which provides important generalizability for the temporal relationship of mortality in children.
CONCLUSIONS
Our study used a large nationwide database to demonstrate that pediatric trauma patients are more prone to early death than adult patients. Although retrospective, our large sample size increases the generalizability of the findings. Given the propensity for early death, more efforts in trauma prevention, pre-hospital systems development, and investigation targeted at developing new strategies to improve early resuscitation may play an important role in the reduction of pediatric trauma deaths.
Acknowledgments
This work was supported by grants KL2TR001854, UL1TR001855, and UL1TR000130 from the National Center for Advancing Translational Science (NCATS) of the U.S. National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix A Categorization of Death Based on Hospital Coding, 2007–2010
| Emergency Department Disposition | Death in ED | Hospital Discharge Disposition | Category |
|---|---|---|---|
| Eddisp = “Died” | Eddeath = “DOA” | Hospdisp ≠ “Discharge” | DOA |
| Eddisp = “Died” | Eddeath = “DOA” | Hospdisp = “Expired” | DOA |
| Eddisp = “Died” | Eddeath = “Death after failed resuscitation attempt”, “Died in ED” | Hospdisp = “Expired”, “Not Applicable”, “Not known”, “Not Recorded” | ED |
| Eddisp = “Died” | Eddeath = “Not Applicable”, “Not known”, “Not Recorded” | Hospdisp = “Expired”, “Not Applicable”, “Not known”, “Not Recorded” | ED |
| Eddisp = “Not Applicable” | Eddeath = “Death after failed resuscitation attempt”, “Died in ED” | Hospdisp = “Expired” | ED |
| Eddisp = “Not Applicable” | Eddeath = “Died in ED” | Hospdisp = “Not Applicable” | ED |
| Eddisp = “Floor bed”, “Operating Room”, “Observation unit”, “Intensive Care Unit”, “Observation unit”, “Telemetry/step-down unit” | Eddeath = “Not Applicable”, “Not known”, “Not Recorded” | Hospdisp = “Expired” | Inpatient |
Appendix B Categorization of Death Based on Hospital Coding, 2011–2014
| Emergency Department Disposition | Signs of Life | Hospital Discharge Disposition | Category |
|---|---|---|---|
| Eddisp = “Died”, “Died/Expired” | Signsoflife=“Arrived with NO signs of life” | Hospdisp = “Not Applicable” | DOA |
| Eddisp = “Not Applicable”, “Not known”, “Not Recorded” | Signsoflife=“Arrived with NO signs of life” | Hospdisp = “Expired”, “Deceased/Expired” | DOA |
| Eddisp = “Died”, “Died/Expired” | Signsoflife=“Arrived with signs of life”, Missing | Hospdisp = “Not Applicable” | ED |
| Eddisp = “Not Applicable”, “Not known”, “Not Recorded” | Signsoflife=“Arrived with signs of life” | Hospdisp = “Expired”, “Deceased/Expired” | ED |
| Eddisp = “Floor bed”, “Operating Room”, “Observation unit”, “Intensive Care Unit”, “Observation unit”, “Telemetry/step-down unit” | Signsoflife= Missing | Hospdisp = “Expired”, “Deceased/Expired” | Inpatient |
| Eddisp = “Floor bed”, “Operating Room”, “Observation unit”, “Intensive Care Unit”, “Observation unit”, “Telemetry/step-down unit” | Signsoflife=“Arrived with NO signs of life” | Hospdisp = “Expired”, “Deceased/Expired” | Inpatient |
| Eddisp = “Floor bed”, “Operating Room”, “Observation unit”, “Intensive Care Unit”, “Observation unit”, “Telemetry/step-down unit” | Signsoflife=“Arrived with signs of life” | Hospdisp = “Expired”, “Deceased/Expired” | Inpatient |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented at the 2017 Western Pediatric Trauma Conference, Santa Barbara, CA
None of the authors have any conflicts of interest to disclose.
Children’s Hospital Los Angeles Institutional Review Board Exemption #CHLA-16-00207
References
- 1.GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Center for Injury Prevention and Control, CDC using WISQARS. Ten Leading Causes of Death by Age Group, United States. 2015 https://www.cdc.gov/injury/wisqars/LeadingCauses.html; 2015 [accessed 17.05.17]
- 3.Albert M, McCaig LF. Emergency department visits for motor vehicle traffic injuries: United States, 2010–2011. NCHS Data Brief. 2015:1–8. [PubMed] [Google Scholar]
- 4.Albert M, McCaig LF. Injury-related emergency department visits by children and adolescents: United States, 2009–2010. NCHS Data Brief. 2014:1–8. [PubMed] [Google Scholar]
- 5.Borse N, Sleet DA. Cdc childhood injury report: Patterns of unintentional injuries among 0-to 19-year olds in the united states, 2000–2006. Fam Community Health. 2009;32:189. doi: 10.1097/01.FCH.0000347986.44810.59. [DOI] [PubMed] [Google Scholar]
- 6.Borse NN, Gilchrist J, Dellinger AM, Rudd RA, Ballesteros MF, Sleet DA. Unintentional childhood injuries in the United States: key findings from the CDC childhood injury report. J Saf Res. 2009;40:71–74. doi: 10.1016/j.jsr.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Borse NN, Rudd RA, Dellinger AM, Sleet DA. Years of potential life lost from unintentional child and adolescent injuries—United States, 2000–2009. J Saf Res. 2013;45:127–131. doi: 10.1016/j.jsr.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Vallipakorn SA-O, Plitapolkarnpim A, Suriyawongpaisal P, Techakamolsuk P, Smith GA, Thakkinstian A. Risk prediction score for death of traumatised and injured children. BMC Pediatr. 2014;14:60. doi: 10.1186/1471-2431-14-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trunkey DD. Trauma. Accidental and intentional injuries account for more years of life lost in the U.S. than cancer and heart disease. Among the prescribed remedies are improved preventive efforts, speedier surgery and further research. Sci Am. 1983;249:28–35. [PubMed] [Google Scholar]
- 10.Sobrino J, Shafi S. Timing and causes of death after injuries. Proc. 2013;26:120–123. doi: 10.1080/08998280.2013.11928934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gunst M, Ghaemmaghami V, Gruszecki A, Urban J, Frankel H, Shafi S. Changing epidemiology of trauma deaths leads to a bimodal distribution. Proc. 2010;23:349–354. doi: 10.1080/08998280.2010.11928649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Demetriades D, Kimbrell B, Salim A, Velmahos G, Rhee P, Preston C, et al. Trauma Deaths in a Mature Urban Trauma System: Is “Trimodal” Distribution a Valid Concept? J Am Coll Surg. 2005;201:343–348. doi: 10.1016/j.jamcollsurg.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Demetriades D, Murray J, Charalambides K, Alo K, Velmahos G, Rhee P, et al. Trauma fatalities: time and location of hospital deaths. J Am Coll Surg. 2004;198:20–26. doi: 10.1016/j.jamcollsurg.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Valdez C, Sarani B, Young H, Amdur R, Dunne J, Chawla LS. Timing of death after traumatic injury—a contemporary assessment of the temporal distribution of death. J Surg Res. 2016;200:604–609. doi: 10.1016/j.jss.2015.08.031. [DOI] [PubMed] [Google Scholar]
- 15.Lefering R, Paffrath T, Bouamra O, Coats TJ, Woodford M, Jenks T, et al. Epidemiology of in-hospital trauma deaths. Eur J Trauma Emerg Surg. 2012;38:3–9. doi: 10.1007/s00068-011-0168-4. [DOI] [PubMed] [Google Scholar]
- 16.Meislin H, Criss EA, Judkins D, Berger R, Conroy C, Parks B, et al. Fatal trauma: the modal distribution of time to death is a function of patient demographics and regional resources. J Trauma. 1997;43:433–440. doi: 10.1097/00005373-199709000-00008. [DOI] [PubMed] [Google Scholar]
- 17.de Knegt C, Meylaerts SAG, Leenen LPH. Applicability of the trimodal distribution of trauma deaths in a Level I trauma centre in the Netherlands with a population of mainly blunt trauma. Injury. 2008;39:993–1000. doi: 10.1016/j.injury.2008.03.033. [DOI] [PubMed] [Google Scholar]
- 18.Allen CJ, Wagenaar AE, Horkan DB, Baldor DJ, Hannay WM, Tashiro J, et al. Predictors of mortality in pediatric trauma: experiences of a level 1 trauma center and an assessment of the International Classification Injury Severity Score (ICISS) Pediatr Surg Int. 2016;32:657–663. doi: 10.1007/s00383-016-3900-7. [DOI] [PubMed] [Google Scholar]
- 19.Miyata S, Cho J, Park H, Matsushima K, Bliss DW. Comparison of outcomes in severe pediatric trauma at adult trauma centers with different trauma case volumes. J Pediatr Surg. 2017 doi: 10.1016/j.jpedsurg.2017.01.066. [DOI] [PubMed] [Google Scholar]
- 20.Amini R, Lavoie A, Moore L, Sirois M-J, Emond M. Pediatric trauma mortality by type of designated hospital in a mature inclusive trauma system. J Emerg Trauma Shock. 2011;4:12–9. doi: 10.4103/0974-2700.76824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Caen AR, Berg MD, Chameides L, Gooden CK, Hickey RW, Scott HF, et al. Part 12: Pediatric Advanced Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132:S526–542. doi: 10.1161/CIR.0000000000000266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gennarelli TA, Wodzin E. AIS 2005: a contemporary injury scale. Injury. 2006;37:1083–91. doi: 10.1016/j.injury.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 23.Kardooni S, Haut ER, Chang DC, Pierce CA, Efron DT, Haider AH, et al. Hazards of benchmarking complications with the National Trauma Data Bank: numerators in search of denominators. J Trauma. 2008;64:273–277. doi: 10.1097/TA.0b013e31816335ae. discussion 277-279. [DOI] [PubMed] [Google Scholar]
- 24.Nicolson NG, Schwulst S, Esposito TA, Crandall ML. Resuscitative thoracotomy for pediatric trauma in Illinois, 1999 to 2009. Am J Surg. 2015;210:720–3. doi: 10.1016/j.amjsurg.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 25.Moore HB, Moore EE, Bensard DD. Pediatric emergency department thoracotomy: A 40-year review. J Pediatr Surg. 2016;51:315–8. doi: 10.1016/j.jpedsurg.2015.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.De Maio VJ, Osmond MH, Stiell IG, Nadkarni V, Berg R, Cabanas JG, et al. Epidemiology of out-of hospital pediatric cardiac arrest due to trauma. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2012;16:230–6. doi: 10.3109/10903127.2011.640419. [DOI] [PubMed] [Google Scholar]
- 27.Evans CCD, Petersen A, Meier EN, Buick JE, Schreiber M, Kannas D, et al. Prehospital traumatic cardiac arrest: Management and outcomes from the resuscitation outcomes consortium epistry-trauma and PROPHET registries. J Trauma Acute Care Surg. 2016;81:285–93. doi: 10.1097/TA.0000000000001070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Brien E, Hendricks D, Cone DC. Field termination of resuscitation: analysis of a newly implemented protocol. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2008;12:57–61. doi: 10.1080/10903120701707989. [DOI] [PubMed] [Google Scholar]
- 29.Cone DC, Bailey ED, Spackman AB. The safety of a field termination-of-resuscitation protocol. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2005;9:276–81. doi: 10.1080/10903120590961996. [DOI] [PubMed] [Google Scholar]
- 30.Richman PB, Vadeboncoeur TF, Chikani V, Clark L, Bobrow BJ. Independent evaluation of an out-of-hospital termination of resuscitation (TOR) clinical decision rule. Acad Emerg Med Off J Soc Acad Emerg Med. 2008;15:517–21. doi: 10.1111/j.1553-2712.2008.00110.x. [DOI] [PubMed] [Google Scholar]
- 31.American College of Surgeons Committee on Trauma, American College of Emergency Physicians Pediatric Emergency Medicine Committee, National Association of Ems Physicians, American Academy of Pediatrics Committee on Pediatric Emergency Medicine. Fallat ME. Withholding or termination of resuscitation in pediatric out-of-hospital traumatic cardiopulmonary arrest. Pediatrics. 2014;133:e1104–1116. doi: 10.1542/peds.2014-0176. [DOI] [PubMed] [Google Scholar]
- 32.Pointer JE. Clinical characteristics of paramedics’ performance of pediatric endotracheal intubation. Am J Emerg Med. 1989;7:364–6. doi: 10.1016/0735-6757(89)90039-9. [DOI] [PubMed] [Google Scholar]
- 33.Paul TR, Marias M, Pons PT, Pons KA, Moore EE. Adult versus pediatric prehospital trauma care: is there a difference? J Trauma. 1999;47:455–9. doi: 10.1097/00005373-199909000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Seid T, Ramaiah R, Grabinsky A. Pre-hospital care of pediatric patients with trauma. Int J Crit Illn Inj Sci. 2012;2:114–20. doi: 10.4103/2229-5151.100887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Seidel JS. Emergency medical services and the pediatric patient: are the needs being met? II. Training and equipping emergency medical services providers for pediatric emergencies. Pediatrics. 1986;78:808–12. [PubMed] [Google Scholar]
- 36.Hansen M, Meckler G, Dickinson C, Dickenson K, Jui J, Lambert W, et al. Children’s safety initiative: a national assessment of pediatric educational needs among emergency medical services providers. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2015;19:287–91. doi: 10.3109/10903127.2014.959223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bankole S, Asuncion A, Ross S, Aghai Z, Nollah L, Echols H, et al. First responder performance in pediatric trauma: a comparison with an adult cohort. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2011;12:e166–170. doi: 10.1097/PCC.0b013e3181f36f6e. [DOI] [PubMed] [Google Scholar]
- 38.Baker TW, King W, Soto W, Asher C, Stolfi A, Rowin ME. The efficacy of pediatric advanced life support training in emergency medical service providers. Pediatr Emerg Care. 2009;25:508–12. doi: 10.1097/PEC.0b013e3181b0a0da. [DOI] [PubMed] [Google Scholar]
- 39.Losek JD, Szewczuga D, Glaeser PW. Improved prehospital pediatric ALS care after an EMT-paramedic clinical training course. Am J Emerg Med. 1994;12:429–32. doi: 10.1016/0735-6757(94)90054-x. [DOI] [PubMed] [Google Scholar]
- 40.Andreatta P, Saxton E, Thompson M, Annich G. Simulation-based mock codes significantly correlate with improved pediatric patient cardiopulmonary arrest survival rates. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2011;12:33–8. doi: 10.1097/PCC.0b013e3181e89270. [DOI] [PubMed] [Google Scholar]
- 41.Mills DM, Wu CL, Williams DC, King L, Dobson JV. High-fidelity simulation enhances pediatric residents’ retention, knowledge, procedural proficiency, group resuscitation performance, and experience in pediatric resuscitation. Hosp Pediatr. 2013;3:266–75. doi: 10.1542/hpeds.2012-0073. [DOI] [PubMed] [Google Scholar]
- 42.Falcone RA, Daugherty M, Schweer L, Patterson M, Brown RL, Garcia VF. Multidisciplinary pediatric trauma team training using high-fidelity trauma simulation. J Pediatr Surg. 2008;43:1065–71. doi: 10.1016/j.jpedsurg.2008.02.033. [DOI] [PubMed] [Google Scholar]
- 43.Popp J, Yochum L, Spinella PC, Donahue S, Finck C. Simulation training for surgical residents in pediatric trauma scenarios. Conn Med. 2012;76:159–62. [PubMed] [Google Scholar]
- 44.Eppich WJ, Adler MD, McGaghie WC. Emergency and critical care pediatrics: use of medical simulation for training in acute pediatric emergencies. Curr Opin Pediatr. 2006;18:266–71. doi: 10.1097/01.mop.0000193309.22462.c9. [DOI] [PubMed] [Google Scholar]
- 45.Gabbe BJ, Cameron PA, Finch CF. The status of the Glasgow Coma Scale. Emerg Med Fremantle WA. 2003;15:353–60. doi: 10.1046/j.1442-2026.2003.00474.x. [DOI] [PubMed] [Google Scholar]
- 46.Carter EA, Waterhouse LJ, Xiao R, Burd RS. Use of Payer as a Proxy for Health Insurance Status on Admission Results in Misclassification of Insurance Status among Pediatric Trauma Patients. Am Surg. 2016;82:146–51. [PubMed] [Google Scholar]


