Abstract
Aimed at covering the large fraction of workers in the informal sector without access to a social security program, the Mexican public health insurance program Seguro Popular began in 2002 and now reaches more than 50 million individuals. We estimate impacts of Seguro Popular for the population aged 50 and older on a set of indicators related to health care including utilization, diagnostic/preventive tests, and treatment conditional on being ill. Using the longitudinal Mexican Health and Aging Study over the period 2001–2012, we conduct before and after difference-in-difference matching impact estimators. Our results suggest large and important effects of the Program on utilization and diagnostic tests. We find overall smaller effects on the probability of being in treatment for individuals with chronic diseases, but these effects are concentrated in rural areas with relatively more health services versus rural areas with lower levels of health services. These results suggest that, to the extent that health services become more available in rural areas lacking services, effects of health insurance may increase.
Keywords: Aging, Health insurance, Mexico, Evaluation, MHAS
Introduction
Providing universal health insurance coverage is a major challenge in most developing countries because typically, the majority of workers belong to the informal sector (Bitran 2014). Social security in Mexico is no exception and has historically provided health benefits to only a fraction of the population. Those without social security or other coverage generally have relied on the Secretary of Health institutions and out-of-pocket expenditures to cover health events. To address this lack of basic health coverage, the Mexican government piloted the health insurance program Seguro Popular in 2002, transitioning to a formal program in 2003. Since then, Seguro Popular has expanded at an impressive rate: as of this writing, the program covers approximately 51 million individuals (more than one-third of the Mexican population) and is nearing its goal of covering all of the population without formal sector health insurance. Services covered include a package of mainly primary and secondary interventions managed and delivered at the state level, although the services and interventions covered have increased over time.
In this study, we analyze the effect of Seguro Popular on a series of indicators related to health care usage for the aging population1 in Mexico. We study the effects of Seguro Popular on (1) health services utilization specifically, doctor visits, dentist visits, and hospitalizations; (2) diagnostic tests for hypertension and diabetes, and gynecological exams for women and prostate cancer tests for men; and (3) the probability of receiving treatment for those diagnosed with hypertension or diabetes. We conduct impact estimates separately by area of residence, urban and rural.
Several previous studies have analyzed the short-term (one to two years) effects of the Seguro Popular program, but our study is one of the first to estimate medium- to longer-term effects. Our study also innovates by analyzing the effects of the program on the population of older adults, whereas most previous studies have focused on working-age adults and children. For the empirical analysis, we use the Mexican Health and Aging Study (MHAS), a longitudinal survey of the population aged 50 and older with three rounds carried out over the period 2001–2012. The first round of the MHAS was completed in 2001, just prior to the beginning of the Seguro Popular program, providing a convenient baseline with preprogram information just before the Program began. Unlike most previous studies, which used cross-sectional after-program estimators, we conduct before and after difference-in-difference estimators, which are less likely to be contaminated by selection bias (Heckman et al. 1997).
Our study is also relevant to the emerging literature on the effects of health insurance in developing countries. Several other developing countries—including Thailand, Ghana, and Indonesia—have recently created universal health care plans (Lagomarsino et al. 2012; Somkotra and Lagrada 2008), largely targeting uncovered populations related to the informal sector.
Background and Seguro Popular
Aging and the Demographic Transition in Mexico
Mexico has followed a familiar pattern in demographic transitions, with a long period of high mortality and high fertility, followed by declining mortality and a subsequent decline in fertility. Falls in mortality rates over the past century have been particularly impressive, with life expectancy increasing from 33 years in 1920 to 74 years in 2000 (Partida-Bush 2006). According to population projections from the Mexican National Population Council (CONAPO 2005), the percentage of the population aged 60 and older is expected to grow from 6 % in the year 2000 to 15 % by 2027.
The rapid epidemiologic transition in Mexico is evident also in changes in the main causes of death. Using data from the Mexican Ministry of Health based on death certificates, Ham Chande (2003) presented the causes of death by importance over the period 1970–2000. For men aged 65 and older, despite heart disease remaining the largest cause of death throughout the period, pneumonia/influenza lost importance, moving from the second cause of death in 1970 to the seventh in 2000. Similarly, intestinal infections moved from third in 1970 to thirteenth in 2000. Diabetes mellitus gained importance, moving from eighth in importance in 1970 to third by the year 2000. Relatedly, obesity substantially increased, making Mexico a country with one of the highest obesity rates. By 2012, 73 % of women and 70 % of men aged 20 and older were classified as overweight or obese (Instituto Nacional de Salud Pública 2012).
Health Insurance and Seguro Popular in Mexico
Health insurance is recognized as one of the enabling means to improve health in populations (Babitsch et al. 2012) because having insurance can affect whether individuals will seek needed medical attention, both preventive and curative. Older adults without health insurance are likely to postpone or avoid regular checkups and screenings, thus increasing the risk that conditions such as high blood pressure, diabetes, or cancer will go undetected or will be detected at later stages of disease. Furthermore, high out-of-pocket costs of medical treatment among the uninsured are likely to produce poor treatment compliance even if diagnosed. Ultimately, catastrophic health expenditures, poorer health, and higher mortality have been found to be associated with a lack of health insurance. Conversely, having health insurance coverage has been associated with a higher likelihood of getting medical care and needed follow-up care as well as certain favorable health outcomes: see, for example, Tejeda et al. 2013; Hadley (2007). However, having health insurance coverage does not guarantee that the population will access and use health care services. The supply of services may act as a constraint to meeting the demand for lower-cost medical attention afforded by insurance.
In Mexico, the Seguro Popular program is part of the 2003 Social Health Protection System reform (SPSS), designed to provide health coverage to individuals not affiliated with any social security institution. Social security includes the Mexican Social Security Institute (IMSS), which provides benefits for private sector workers, Social Security for Government Workers (ISSSTE), and several smaller systems. [The Seguro Popular program is voluntary and covers (as of this writing) 284 interventions as well as more than 1,500 illnesses. The list of covered illnesses/procedures is published by the Secretary of Health (Catálogo Universal de Servicios de Salud; CAUSES) and has grown since inception.
As mentioned earlier, the Seguro Popular program began as a pilot in 2002 and was formally created in 2003. In 2002, approximately 58 % of households lacked health insurance of any type; that percentage declined to 13 % by 2012, having affiliated more than 50 million individuals with Seguro Popular (Gonzalez-Pier et al. 2013; Knaul et al. 2016). To meet the demand for health care, the reform included a program to increase and strengthen the provision of services. Health infrastructure also grew during this period, with new construction of 15 centers of high specialties, 200 hospitals, and almost 2,000 mobile clinics. In addition, 4,000 health centers were renovated and equipped. Seguro Popular hired corresponding new personnel as well, but by 2012, the challenge continued to be a shortage of specialized medical personnel as well as difficulties in reaching the population in remote rural communities (Gonzalez-Pier et al. 2013).
The population eligible for Seguro Popular includes those who are not beneficiaries of any social security program. To apply, an individual visits the nearest registration center (Módulo de Afiliación y Orientación), where a socioeconomic evaluation is conducted. Families classified in the lower 40 % of the income distribution do not pay an enrollment fee. For those families in the upper 60 % of the income distribution, the cost ranges from approximately $150 US annually to $1,000 US (increasing with income decile). Coverage is also available on an individual-level basis. In practice, a very low proportion of beneficiaries pay the enrollment fee (Knaul et al. 2012), a finding that may reflect applicants’ underreporting of income, which is not verified. Apart from the enrollment fee, there are no copayments.[Table 1 shows how affiliation to Seguro Popular has increased since its inception.
Table 1.
Growth in the Seguro Popular program
| Year | Affiliated Families |
Affiliated Individuals |
|---|---|---|
| 2002 | 295,513 | 1,094,236 |
| 2003 | 613,938 | 2,224,411 |
| 2004 | 1,563,572 | 5,318,289 |
| 2005 | 3,555,977 | 11,404,861 |
| 2006 | 5,100,000 | 15,672,374 |
| 2007 | 7,307,173 | 21,176,914 |
| 2008 | 9,146,013 | 27,176,914 |
| 2009 | 10,514,325 | 31,132,949 |
| 2010 | 15,760,805 | 43,518,719 |
| 2011 | 19,811,349 | 51,823,314 |
| 2012 | 52,908,011 |
Source: Secretaria de Salud (2013).
A number of other developing countries have implemented health insurance programs over a similar period as the Seguro Popular. The Thailand Universal Coverage Scheme (UCS), which began in 2001, is financed primarily through general taxes and small copayments per medical visit or admission. Approximately 30 % of the population in Thailand was uninsured in 2001, but more than 98 % of the population was covered by some form of health insurance by 2011 (Limwattananon et al. 2015). Indonesia launched Askeskin—health insurance for the poor—which evolved into Jaminan Kesehatan Nasional (JKN) in 2014; this program provides comprehensive health care through public and private funding (Mboi 2015). Subsidies are provided for the poor, and the formally employed pay a premium for health coverage (Hidayat 2015). A universal health care scheme was implemented in Ghana in 2004, National Health Insurance Scheme (NHIS), and is funded both by insurance premiums and taxes, with the poor, pregnant women, children under age 18, and the aged (70+ years) are free from insurance premiums (Alatinga and Williams 2015).
Previous Literature
A number of previous studies have covered the effects of the Seguro Popular program on indicators related to health. Nearly all of these studies, with the exception of Knox (2008), used cross-sectional data to analyze program impacts.
Several studies have documented an increase in the use of health services (Barros 2008; Harris and Sosa-Rubí 2009; Sosa-Rubí et al. 2009a) and a reduction in the probability of catastrophic health expenditures (Barros 2008; Galárraga et al. 2012; Grogger et al. 2014). Barros (2008), using the 2000 and 2006 rounds of the Mexican National Health Surveys (ENSANUT), found no effect of Seguro Popular on health outcomes, including self-reported health and having hypertension (both measured and self-reported). Bleich et al. (2007) also studied effects on treatment of hypertension (using propensity score matching) and in contrast to Barros (2008), found that individuals with hypertension are 50 % more likely to be receiving treatment with Seguro Popular coverage than those without coverage; in results not shown, Barros suggested that effects were even larger in areas with a higher supply of health professionals.
In the only previous study we are aware of using longitudinal data, Knox (2008) used the evaluation surveys from the urban Oportunidades conditional cash transfer program to study the health effects of Seguro Popular two years post-program. Although her evidence suggested that the Seguro Popular program increases health care usage, Knox did not find any effects on reported health outcomes, perhaps reflecting the short time post-program studied. Sosa-Rubí et al. (2009b) analyzed the impact of Seguro Popular on access to health resources, treatment, and blood glucose control among poor adults with diabetes using the cross-sectional 2006 ENSANUT. They found that those enrolled in Seguro Popular were more likely to report having had regular blood glucose control tests, but no significant difference in the probability of reporting that diabetes was controlled.
In the study most similar to ours in scope, Rivera-Hernandez et al. (2016) analyzed the impact of Seguro Popular on treatment indicators for diabetes and hypertension for older adults, pooling the ENSANUT surveys from 2000, 2006, and 2012. They instrumented Seguro Popular participation using the interaction of the round of the ENSANUT and the population of the municipality of residence in each survey round, arguing these instruments predicted the order of incorporation and did not have an independent effect on the health indicators studied. Their estimates suggested few effects of Seguro Popular on treatment indicators, with significant and positive effects observed only for the use of insulin among diabetes patients.
We close this section by mentioning that one finding supported by several studies is that Seguro Popular effects appear to be larger in areas with a greater supply of health professionals/services (Bleich et al. 2007). We will also test this hypothesis using information on available health services in the community of residence at the beginning of the MHAS panel.
Data
Our main data source is the Mexican Health and Aging Study (MHAS), a prospective study of aging that includes a sample of Mexicans aged 50 and older in 2001, with national and urban/rural representation. The study uses protocols and survey instruments that are highly comparable with the U.S. Health and Retirement Study (HRS) and is funded in part by the National Institute on Aging (NIA) of the National Institutes of Health (NIH).
The baseline survey was conducted in 2001, and follow-up interviews were conducted in 2003 and 2012. The sample for the MHAS baseline was selected from residents from the National Employment Survey (Encuesta Nacional de Empleo; ENE), carried out by the Instituto Nacional de Estadística y Geografía (INEGI) in Mexico; 11,000 households with at least one age-eligible (aged 50 and older) resident were selected to be part of the MHAS baseline sample. The selected person and the spouse (regardless of age) were recruited to be part of the longitudinal study. The baseline survey in 2001 was completed with a sample size of 15,186 respondents. A follow-up survey conducted in 2003 targeted all age-eligible subjects from the 2001 wave even if they had moved. If the subject had died, an interview was conducted with an informed respondent. A third wave survey was completed in 2012. Response/follow-up rates for 2001, 2003, and 2012 were 91.8 %, 93.3 %, and 88.1 %, respectively (Wong et al. 2017).
The MHAS provides detailed information on health expenditures, health facility utilization and health status, including mortality. In particular, the MHAS includes variables measuring self-reported health and symptoms of illness, health care utilization in the different subsystems of health in Mexico, lifestyle behaviors, depressive symptoms, and cognitive function. The MHAS also provides economic variables, including labor force participation history, all income sources, and assets. The first round of the survey was conducted shortly before the Seguro Popular program began and thus provides a convenient baseline for our analysis.
To the MHAS, we merge information on health facilities. We link preprogram information from the 2000 Mexican Census of Population and Dwellings with the Directory of Public Health Sector Facilities 2002, provided by the Mexican Ministry of Health. The census information includes community-level statistics on total population, education levels, disabilities, and dwelling characteristics, among others. The Mexican health sector information includes number of facilities and number of physical and human resources available in those facilities, including beds, operating rooms, physicians, and nurses. The variables included in the file represent the services available in the community of residence or in a neighboring community (within 10km) if services were unavailable in the community of residence. The community information used here dates from just prior to the implementation of the Seguro Popular program. We use preprogram data on health services because the Seguro Popular program might affect the construction of new health facilities, in which case health facilities postprogram would not be exogenous to Seguro Popular effects.2
Table 2 presents data from the MHAS on health insurance coverage among the different providers in Mexico in 2001 and 2012, by gender. In 2001, almost one-half of the population aged 50 and older (49.3 % of men and 45.1 % of women) reported having no health insurance. Approximately 40 % of women and 35 % of men were affiliated with the Mexican Social Security Institute (IMSS), and approximately 10 % of men and women were affiliated with the social security institution for government workers (ISSSTE). By 2012, drastic positive changes occurred in the health insurance status for this same population, with only 17 % of men and 14 % of women reporting having no health insurance. Seguro Popular is clearly the main factor increasing the coverage of this population, with approximately 30 % of both men and women reporting affiliation to the Seguro Popular program in 2012. Proportions affiliated with IMSS and ISSSTE remained similar over this period. Thus, a substantial proportion of the population aged 50 and older without health insurance in 2001 obtained health insurance by 2012, largely because of the Seguro Popular program.
Table 2.
Population aged 50 and older by type of health insurance, 2001 and 2012: Percentages
| 2001 | 2012 | |||
|---|---|---|---|---|
|
|
||||
| Type of Health Insurance | Men | Women | Men | Women |
| IMSS (Mexican Social Security Institute) | 35.8 | 39.2 | 33.5 | 34.1 |
| ISSSTE (Government) | 9.7 | 11.4 | 10.6 | 11.7 |
| Seguro Popular | NA | NA | 31.3 | 32.5 |
| Private, Pemex, Defense, and Other | 5.2 | 4.2 | 7.8 | 8.0 |
| None | 49.3 | 45.1 | 16.9 | 13.7 |
Source: Authors' calculations using the Mexican Health and Aging Study (MHAS).
Table 3 divides the population into four groups by rural/urban residence: (1) those with any form of health insurance in both 2001 and 2012; (2) those with health insurance only in 2001; (3) those with health insurance only in 2012; and (4) those without health insurance in both years. Table 3 makes clear that the largest increases in health insurance coverage between 2001 and 2012 occurred for the rural population. The population without coverage in 2001 and with coverage in 2012 is 20 % for urban areas and 46 % for rural areas. Given the larger increases in insurance coverage over time for the rural population, we may expect overall impacts of the Seguro Popular program to be greater in rural areas than in urban areas. However, rural areas have fewer and more limited health facilities, and previous studies have suggested stronger effects of the Seguro Popular program in areas with greater access to health facilities (Bleich et al. 2007).
Table 3.
Health insurance for MHAS individuals interviewed in 2001 and 2012: Percentages
| Insurance Status in 2001 and 2012 | Urban (>100,000 inhabitants) |
Rural (<100,000 inhabitants) |
|---|---|---|
| With Insurance in 2001 and 2012 | 71.5 | 39.1 |
| With Insurance 2001, Without in 2012 | 2.6 | 1.9 |
| With Insurance 2012, Without in 2001 | 19.9 | 46.4 |
| Without Insurance in 2001 and 2012 | 6.0 | 12.6 |
| 100 | 100 |
Source: Author's calculations using data from the Mexican Health and Aging Study (MHAS).
We aim to provide a broad vision of impacts on variables related to the use of health services that may potentially affect health outcomes by analyzing three sets of indicators. First, we study the impact of Seguro Popular on utilization, including doctor visits, hospitalization, and dentist visits in the year prior to the survey. Second, we study the impact of Seguro Popular on diagnostic tests. In particular, we evaluate the probability of having hypertension, diabetes, prostate cancer, and cervical cancer tests conducted during the two years prior to the survey. Finally, we study the effects on chronic disease treatment, conditional on reporting having an illness, for hypertension and diabetes. For those who report having been told by a doctor or other medical personnel that they have high blood pressure or hypertension, we analyze whether they report taking medication for hypertension. For the case of diabetes, we evaluate whether those who report having been told by a doctor or medical personnel that they have diabetes report taking insulin or following a special diet to control their diabetes.
Note that being in treatment is asked only of those individuals reporting having an illness; thus, our impact estimations on the probability of ill individuals being in treatment do not include individuals who are ill but are unaware.3 We use the 2012 MHAS biomarker subsample to examine how potentially different the unaware population is from the aware population conditional on having hypertension. We conduct a logistic regression of knowledge of hypertension as a function of socioeconomic conditions and access to medical services, finding that the only significant predictor of lack of awareness is gender, with men being 13 % less likely to be aware of their hypertension condition. (This finding has been shown in other countries as well; for instance; see Cutler et al. (2008).) Rural/urban residence or the supply of medical services as well as socioeconomic indicators (including age and education) were surprisingly not significant determinants of awareness. Thus, although our results only reflect impacts of the Seguro Popular on treatment for those who are aware of their condition, there appear to be surprisingly few observable predictors of lack of awareness in the Mexican context.4,5
Methodology
To identify the impact of the Seguro Popular program, we carry out difference-in-difference propensity score matching estimators using before and after program information on health indicators (2001 and 2012) and self-reported information on participation in the Seguro Popular program in 2012. Our individual-level difference-in-difference matching estimators (Heckman et al. 1997) are analogous to the standard difference-in-difference regression estimator but do not impose functional form restrictions in estimating the conditional expectation of the outcome variable and reweight the observations according to the weighting functions implied by the matching estimators.
The main obstacle to overcome in our empirical analysis is the potential endogeneity of participation in Seguro Popular. The before and after difference-in-difference estimators that we use have the substantial advantage over cross-sectional after-program difference estimators of allowing for selectivity into the program to be based on unobserved fixed attributes (analogous to fixed effects). The conditional independence assumption in this case requires trends, but not levels, to be similar in the treatment and comparison groups conditional on the propensity score. Our upcoming descriptive analysis furthermore shows that preprogram, the treated and comparison groups have relatively similar indicators of baseline health, although this is not a requirement of our difference-in-difference identification.
The propensity score matching estimators have two stages. In the first stage, the propensity score is estimated using a logistic model and a set X consisting of preprogram (2001) individual-level, household-level, and locality-level characteristics. The second stage uses local-linear regressions to construct matched nontreatment outcomes for each treated individual. We use local linear matching and bootstrapping to calculate standard errors for the main estimates presented here.6 In all cases, the matching is based on the propensity score with exact matching done on age and gender. Results are presented by rural and urban areas.
We now turn to the definition of the treatment and comparison groups and discussion of the relevant counterfactual. Our sample of individuals comprises those who preprogram do not have health insurance. The treatment group consists of individuals who in 2012 (i.e., postprogram) report participating in Seguro Popular: that is, they become Seguro Popular beneficiaries during the panel. We use two comparison groups for the estimation. The first comparison group comprises those individuals who do not have Seguro Popular postprogram: that is, the counterfactual is not having Seguro Popular. This is not equivalent to not having health insurance postprogram because some of those in the comparison group obtain health insurance over the panel (usually, social security).7 However, this comparison and counterfactual may best approximate the impacts of the program given the policy context into which the Seguro Popular program was introduced. In particular, Seguro Popular was introduced to increase health coverage for workers in the informal sector but was initiated in a context of several existing health insurance alternatives, including social security, and where workers move between formal and informal sectors.8
However, using all individuals without Seguro Popular as the comparison group to measure impacts may underestimate the impacts of Seguro Popular relative to the potential counterfactual of no other available health insurance (for instance, in a context with few formal sector jobs available). For this reason, we conduct a second set of estimations, using as the comparison group the set of individuals without health insurance both in the baseline and in 2012. These estimates provide a closer approximation to the effects of Seguro Popular when the counterfactual is no alternative health insurance. We expect this second set of estimates to provide larger impact estimates than the first set of estimations.
Individual-level information on participation in Seguro Popular was collected only in 2012. The Seguro Popular program began in 2002, but individual- or household-level information on participation in Seguro Popular is not available in the MHAS prior to 2012. Thus, we do not know how long current beneficiaries have been receiving Seguro Popular or whether current nonbeneficiaries were Seguro Popular beneficiaries at some point prior to 2012. In addition, for those leaving the sample by 2012 (either because of mortality or being lost to follow up for other reasons), we have no individual level information on whether they received Seguro Popular.
To validate the self-reported information on Seguro Popular participation, we compared the number of Seguro Popular beneficiaries in the weighted MHAS data with the actual numbers of beneficiaries in 2012 according to administrative data. Table 4 shows that by age group and gender, Seguro Popular receipt is quite comparable in the MHAS and in the administrative data for the population aged 51 to 65. For the population older than age 65, the number of beneficiaries is somewhat lower in the MHAS (by approximately 16 %) than according to administrative information. This finding is perhaps suggestive of a greater reporting bias for the older population.
Table 4.
Comparison of Seguro Popular enrollment reported in the Mexican Health and Aging Study (2012) with administrative data from Seguro Popular among older Mexican adults (aged 51+)
| Enrolled Population (Seguro Popular Estimatesa) |
Enrolled Population (MHAS Estimatesb) |
|||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Age Group | Male | Female | Total | Male | Female | Total |
| 51–60 | 1,704,585 | 2,014,639 | 3,719,224 | 1,587,190 | 2,029,923 | 3,617,113 |
| 61–65 | 578,045 | 665,665 | 1,243,710 | 701,120 | 686,474 | 1,387,594 |
| 66+ | 1,363,062 | 1,592,508 | 2,955,570 | 1,168,372 | 1,299,388 | 2,467,760 |
| All (51+) | 3,645,692 | 4,272,812 | 7,918,504 | 3,456,682 | 4,015,785 | 7,472,467 |
Estimates of the enrolled population from Seguro Popular are obtained from http://www.seguro-popular.salud.gob.mxand from 2012.
Estimates of the enrolled population from the MHAS are 2012 and weighted using individual-level population weights.
We restrict the impact analysis to those in the sample who were alive and interviewed in 2012—63.4 % of the original sample—which brings up the issue of attrition. Those reinterviewed are likely to be a selected sample of those in the original 2001 baseline; and in particular, those who survive and are followed up may be more likely to be younger and healthier in 2001 than those who left the sample. There may also be differential selection by Seguro Popular participation; in fact, if the Seguro Popular program reduces mortality, one would expect to observe differential selection by program participation.
The main source of attrition in the MHAS is mortality. Of the 15,186 individuals in the baseline 2001 MHAS, 3,242 (21.4 % of the original sample) had died by 2012. Another 2,308 (15.2 % of the original sample) are lost to follow-up. The main reasons for being lost to follow-up include empty household/subject was unable to be located and refusal to answer. If the Seguro Popular program does reduce mortality, then the remaining MHAS sample interviewed in 2012 is likely to contain, on average, less-healthy Seguro Popular beneficiaries than this sample would have contained in the absence of the program. There is additional potential selection from leaving the sample not from mortality but from refusal to participate or inability to be located.
We thus now test for the possibility that the program affects who leaves the MHAS sample by 2012. Unfortunately, we do not have information on Seguro Popular participation for the population who had left the sample by 2012. To identify the effect of the Seguro Popular program on attrition, we use state-level administrative information on the proportion of individuals in a state who are covered by the program to estimate regression models of the following form:
where Yis is the probability of leaving the sample of interest for individual i in state s by 2012 for all individuals in the sample in 2001, Sst represents the proportion of individuals in state s in time t covered by the Seguro Popular program, Xist are control variables and eist is the error term. The model then relates the proportion covered in a state to the probability of leaving the sample by the 2012 round. The information on individuals affiliated is derived from administrative records on the Seguro Popular program provided by the Mexican National Commission on Social Protection in Health. The population numbers used to construct proportions come from state-level census data provided by the Mexican Statistical Institute (INEGI).9
Table 5 shows the impact of the Seguro Popular program on the probability of attriting from the MHAS sample by 2012. We also separate the probability of attriting into two sources: (1) mortality and (2) loss to follow up for other reasons (e.g., migration or refusal to answer). We provide two alternative specifications. The first includes, in addition to the proportion of beneficiaries in the state of residence, individual controls for age, gender, education level, indigenous status, preprogram health status, and durable goods at the household level. For the second specification, we additionally include locality-level indicators of the supply of health services. The results do not vary by the set of included controls.
Table 5.
Mortality and attrition in the MHAS 2001–2012: Effects of the Seguro Popular program
| Not Found in 2012 | Died Before 2012 | All Attritors in 2012 | ||||
|---|---|---|---|---|---|---|
| 2002 % Enrolled in Seguro Popular | 0.051 (0.146) | 0.137 (0.147) | −0.005 (0.161) | 0.015 (0.162) | 0.047 (0.198) | 0.152 (0.199) |
| 2004 % Enrolled in Seguro Popular | −0.191 (0.166) | −0.278† (0.169) | 0 (0.182) | 0.012 (0.186) | −0.191 (0.225) | −0.266 (0.229) |
| 2006 % Enrolled in Seguro Popular | 0.042 (0.114) | −0.052 (0.119) | 0.098 (0.125) | 0.134 (0.131) | 0.140 (0.154) | 0.083 (0.161) |
| 2008 % Enrolled in Seguro Popular | −0.241 (0.174) | 0.077 (0.184) | 0.071 (0.191) | −0.004 (0.203) | −0.170 (0.235) | 0.072 (0.249) |
| 2010 % Enrolled in Seguro Popular | 0.263* (0.113) | 0.133 (0.117) | −0.114 (0.124) | −0.074 (0.130) | 0.150 (0.152) | 0.059 (0.159) |
| Age | −0.002** (0.000) | −0.002** (0.000) | 0.014** (0.000) | 0.014** (0.000) | 0.012** (0.001) | 0.011** (0.001) |
| Gender (female = 1) | −0.007 (0.009) | −0.002 (0.009) | 0.027* (0.010) | 0.027** (0.010) | 0.02 (0.013) | 0.025* (0.013) |
| Years of Schooling | 0.013** (0.001) | 0.011** (0.001) | 0 (0.002) | 0 (0.002) | 0.013** (0.002) | 0.011** (0.002) |
| Speaks Indigenous Language | −0.009 (0.016) | −0.015 (0.019) | 0.008 (0.017) | 0.024 (0.021) | −0.001 (0.021) | 0.009 (0.026) |
| Water in Household | 0.039** (0.011) | 0.024* (0.011) | 0.012 (0.012) | 0.006 (0.013) | 0.051** (0.015) | 0.03* (0.015) |
| Radio | −0.017 (0.013) | −0.019 (0.013) | −0.037* (0.014) | −0.037** (0.015) | −0.054** (0.018) | −0.057** (0.018) |
| Television | −0.020 (0.015) | −0.023 (0.015) | 0.008 (0.016) | −0.001 (0.016) | −0.012 (0.020) | −0.024 (0.020) |
| Refrigerator | 0.015 (0.013) | 0.007 (0.013) | −0.016 (0.014) | −0.019 (0.014) | −0.001 (0.017) | −0.012 (0.017) |
| Washing Machine | 0.004 (0.012) | 0.003 (0.012) | 0.004 (0.013) | 0.003 (0.013) | 0.008 (0.016) | 0.006 (0.016) |
| Telephone | 0.002 (0.012) | −0.020 (0.012) | −0.028* (0.013) | −0.029* (0.014) | −0.026 (0.016) | −0.049** (0.017) |
| Water Heater | 0.009 (0.013) | 0.007 (0.013) | −0.026† (0.014) | −0.027† (0.014) | −0.017 (0.017) | −0.020 (0.017) |
| Reports Hypertension | −0.003 (0.010) | 0 (0.010) | 0.024* (0.011) | 0.025* (0.011) | 0.021 (0.013) | 0.025† (0.013) |
| Reports Diabetes | 0.002 (0.014) | −0.001 (0.014) | 0.197** (0.016) | 0.197** (0.016) | 0.199** (0.019) | 0.196** (0.019) |
| Reports Heart Attack | −0.030 (0.031) | −0.035 (0.030) | 0.131** (0.034) | 0.129** (0.034) | 0.101* (0.041) | 0.093* (0.041) |
| Serious Health Problem Before Age 10 | 0.004 (0.015) | 0.001 (0.015) | −0.033* (0.016) | −0.034* (0.016) | −0.029 (0.020) | −0.032 (0.020) |
| Height | 0.001** (0.000) | 0.001** (0.000) | 0* (0.000) | 0* (0.000) | 0 (0.000) | 0 (0.000) |
| Constant | 0.090† (0.050)* | 0.010 (0.078) | −0.538** (0.054) | −0.689** (0.086) | −0.448** (0.067) | −0.680** (0.105]) |
| Number of Observations | 5,827 | 5,827 | 5,827 | 5,827 | 5,827 | 5,827 |
| R2 | .05 | .07 | .21 | .21 | .11 | .12 |
| Includes Locality Indicators | No | Yes | No | Yes | No | Yes |
| Number of Observations | 14,782 | 14,782 | 14,782 | 14,782 | 14,782 | 14,782 |
| R2 | .03 | .04 | .18 | .21 | .09 | .11 |
Notes: Standard errors are shown in parentheses. All control variables are from 2001 (preprogram), MHAS round. Locality indicators include total population, population aged 5 and older who speaks an indigenous language, population aged 5 and older who is Catholic, population aged 15 and older without education, population aged 12 and older who is employed, total number of dwellings with good floor materials, total dwellings with gas stove, total dwellings with sewage and running water, total number of clinics, and total number of doctors.
p < .10;
p < .05;
p < .01
We also consider a number of specifications to best capture the effect of the Seguro Popular program and present specifications based on using administrative information on Seguro Popular state-level beneficiaries from the following years of the program (2002, 2004, 2006, 2008, and 2010) to capture the effect of the program on attrition. Modifying the years or alternative specifications (e.g., overall yearly growth rate in beneficiaries) does not significantly alter the results.
Table 5 demonstrates little support for the hypothesis that the Seguro Popular program affected the probability of attriting from the sample or the separate components of attrition—for example, of mortality and of other factors affecting loss to follow-up, including refusal to answer and migration. Of the 30 variables measuring Seguro Popular affiliates in one’s state in the six specifications, only one is significantly related to the probability that an individual attrits over the course of the panel. With respect to other variables affecting attrition or its components, Table 5 shows that older individuals and male individuals are more likely to attrit, through the effect of age and gender on mortality. As might be expected, baseline indicators of health and chronic illness are strong predictors of attrition again through their effects on mortality.10 The results suggest that the subsequent analyses conducted in this study, which restrict attention to those individuals in the sample in both 2001 and 2012, are not likely to be biased by differential attrition by program participation.
Finally, Table 6 compares preprogram health and socioeconomic characteristics of Seguro Popular beneficiaries, both in rural and urban areas, and tests for significant differences between beneficiaries and nonbeneficiaries. Note that we might expect adverse selection in program participation, with less-healthy individuals choosing to participate compared with healthier individuals; we might also expect, given the means testing of the Seguro Popular described earlier, that participants would be somewhat poorer than nonparticipants. Table 6 shows that in general, we find few significant preprogram differences in the levels of the outcome indicators studied in both the rural and urban populations. We do find a few preprogram differences in usage, with Seguro Popular beneficiaries being more likely than nonbeneficiaries to have seen a doctor in the previous year in both rural and urban areas, to have had a gynecological test in rural areas, and to have been hospitalized and to have had a test for diabetes in urban areas. For the remainder of the health indicators studied, we find no statistically significant differences. Also strikingly, the proportion reporting hypertension or diabetes does not differ by treatment status. As discussed previously, however, these figures exclude those who may not be aware of their illness. For being in treatment conditional on having hypertension or diabetes, Table 6 also suggests no significant differences by treatment status.
Table 6.
Preprogram (2001) outcome variables and socioeconomic and health characteristics, by Seguro Popular beneficiaries versus nonbeneficiaries: All uninsured individuals in 2001
| Untreated | Treated | Significant Difference |
|||
|---|---|---|---|---|---|
|
|
|||||
| Mean | SD | Mean | SD | p Value | |
| Rural | |||||
| Outcome variables | |||||
| Seen a doctor in previous year | 0.48 | 0.50 | 0.55 | 0.50 | 0.00 |
| Seen a dentist in previous year | 0.14 | 0.35 | 0.14 | 0.34 | 0.64 |
| Hospitalized in previous year | 0.05 | 0.22 | 0.06 | 0.22 | 0.81 |
| Diabetes test in past two years | 0.42 | 0.49 | 0.44 | 0.50 | 0.69 |
| Prostate exam in past two years | 0.08 | 0.27 | 0.07 | 0.26 | 0.56 |
| Gynecological exam past two years | 0.44 | 0.50 | 0.55 | 0.50 | 0.00 |
| Hypertension test in past two years | 0.55 | 0.50 | 0.57 | 0.50 | 0.47 |
| For those with hypertension, taking medication | 0.53 | 0.50 | 0.59 | 0.49 | 0.16 |
| For those with diabetes, on diet as treatment | 0.53 | 0.50 | 0.64 | 0.48 | 0.19 |
| For those with diabetes, taking insulin as treatment | 0.06 | 0.24 | 0.05 | 0.22 | 0.76 |
| Baseline socioeconomic, other health, and consumer durables used as control variables | |||||
| Age | 58.92 | 9.70 | 58.04 | 9.50 | 0.05 |
| Gender (male = 1) | 0.46 | 0.50 | 0.44 | 0.50 | 0.39 |
| Years of education | 2.59 | 2.90 | 2.04 | 2.45 | 0.00 |
| Speaks indigenous language | 0.12 | 0.33 | 0.19 | 0.40 | 0.00 |
| Self-reported hypertension | 0.35 | 0.47 | 0.32 | 0.46 | 0.06 |
| Self-reported diabetes | 0.13 | 0.34 | 0.13 | 0.34 | 0.94 |
| Self-reported heart attack | 0.02 | 0.14 | 0.02 | 0.13 | 0.42 |
| Serious health problem before age 10 | 0.10 | 0.30 | 0.10 | 0.31 | 0.51 |
| Height (cm) | 160.80 | 8.28 | 159.60 | 8.25 | 0.76 |
| Piped water in house | 0.53 | 0.50 | 0.43 | 0.50 | 0.00 |
| Radio | 0.82 | 0.38 | 0.78 | 0.41 | 0.04 |
| Television | 0.82 | 0.39 | 0.74 | 0.44 | 0.00 |
| Refrigerator | 0.65 | 0.48 | 0.51 | 0.50 | 0.00 |
| Washing machine | 0.43 | 0.49 | 0.35 | 0.48 | 0.00 |
| Phone | 0.28 | 0.45 | 0.15 | 0.35 | 0.00 |
| Gas heater | 0.27 | 0.44 | 0.15 | 0.36 | 0.00 |
| Number of observations | 646 | 1,457 | |||
| Urban | |||||
| Outcome variables | |||||
| Seen a doctor in previous year | 0.44 | 0.50 | 0.51 | 0.50 | 0.03 |
| Seen a dentist in previous year | 0.22 | 0.42 | 0.23 | 0.42 | 0.73 |
| Hospitalized in previous year | 0.03 | 0.17 | 0.07 | 0.25 | 0.01 |
| Diabetes test in past two years | 0.42 | 0.49 | 0.50 | 0.50 | 0.01 |
| Prostate exam in past two years | 0.10 | 0.29 | 0.09 | 0.28 | 0.76 |
| Gynecological exam past two years | 0.51 | 0.50 | 0.58 | 0.49 | 0.11 |
| Hypertension test in past two years | 0.57 | 0.50 | 0.62 | 0.49 | 0.13 |
| For those with hypertension, taking medication | 0.54 | 0.50 | 0.52 | 0.50 | 0.77 |
| For those with diabetes, on diet as treatment | 0.58 | 0.51 | 0.62 | 0.49 | 0.76 |
| For those with diabetes, taking insulin as treatment | 0.05 | 0.23 | 0.06 | 0.24 | 0.93 |
| Baseline socioeconomic, other health, and consumer durables used as control variables | |||||
| Age | 59.22 | 9.96 | 57.26 | 9.88 | 0.00 |
| Gender (male = 1) | 0.42 | 0.49 | 0.39 | 0.49 | 0.51 |
| Years of education | 4.15 | 4.44 | 3.49 | 3.42 | 0.00 |
| Speaks indigenous language | 0.07 | 0.26 | 0.08 | 0.27 | 0.83 |
| Self-reported hypertension | 0.36 | 0.48 | 0.34 | 0.47 | 0.46 |
| Self-reported diabetes | 0.12 | 0.33 | 0.15 | 0.35 | 0.30 |
| Self-reported heart attack | 0.03 | 0.27 | 0.03 | 0.26 | 0.67 |
| Serious health problem before age 10 | 0.10 | 0.31 | 0.02 | 0.12 | 0.76 |
| Height (cm) | 160.91 | 20.71 | 159.67 | 8.26 | 0.42 |
| Piped water in house | 0.72 | 0.45 | 0.69 | 0.46 | 0.24 |
| Radio | 0.89 | 0.31 | 0.89 | 0.31 | 0.85 |
| Television | 0.91 | 0.29 | 0.94 | 0.23 | 0.02 |
| Refrigerator | 0.78 | 0.42 | 0.80 | 0.40 | 0.37 |
| Washing machine | 0.60 | 0.49 | 0.52 | 0.50 | 0.00 |
| Phone | 0.55 | 0.50 | 0.41 | 0.49 | 0.00 |
| Gas heater | 0.56 | 0.50 | 0.35 | 0.48 | 0.00 |
| Number of observations | 679 | 1,015 | |||
Source: MHAS 2001, authors’ calculations.
Overall then, this preprogram health analysis suggests relatively similar health utilization and conditions preprogram between the Seguro Popular population and nonbeneficiaries in the absence of the program. With respect to socioeconomic conditions preprogram, as expected, the overall characteristics of Seguro Popular beneficiaries are suggestive of a population more likely to be in poverty than nonbeneficiaries, particularly for rural areas. Rural Seguro Popular beneficiaries have lower education levels, are more likely to be indigenous, and have lower levels of durable goods than nonbeneficiaries. In urban areas, the differences are less prevalent, although beneficiaries have lower education levels, on average. The difference-in-difference matching estimators eliminate preprogram differences and provide unbiased estimates of program impact conditional on similar trends in both groups (beneficiaries and nonbeneficiaries) in the absence of the program. Although we are fortunate that the first round of the MHAS provides a baseline for our analysis, we do not have information on our sample for an earlier preprogram period, which would allow for an additional testing of the parallel trends assumption.
As a final note, the population that we study generally has very low pension receipt, with less than 1 % of the uninsured population preprogram (2001) receiving a pension (for retirement, widowhood, disability, or other federal/state program). However, this proportion increased to approximately 7 % by 2012, partly reflecting the introduction in 2007 of the program 70 y Mas through the Ministry of Social Development, which provides a monthly pension of 500 pesos for individuals 70 and older who have no alternative pension. If beginning to receive a pension over the period were correlated with Seguro Popular receipt, this might contaminate our impacts. Thus, we test whether this increase in pension receipt is similar for Seguro Popular beneficiaries as for nonbeneficiaries. For rural areas only, we find a slightly higher increase in the probability of Seguro Popular beneficiaries acquiring a pension over time. These differences are small (at approximately 3 percentage points), so we believe it is unlikely that this differential increase in pension receipt over time captures much of the impact of the Seguro Popular. Nevertheless, we rerun our main results for rural areas excluding those individuals who received a pension in 2012 and find that the results are nearly identical to those reported.
Results
We now turn to the principal results of the program impact on our selected outcomes. We begin by presenting estimations of the propensity scores and then present impact estimation results for both rural and urban areas.
Table S1 in Online Resource 1 reports the complete results of the propensity score estimation and shows that overall, Seguro Popular beneficiaries look somewhat poorer in terms of education levels, housing characteristics, and durable goods. With regard to preprogram health status, however, we find few significant differences in preprogram health indicators between beneficiaries and nonbeneficiaries, as suggested by the descriptive analysis presented in Table 6.
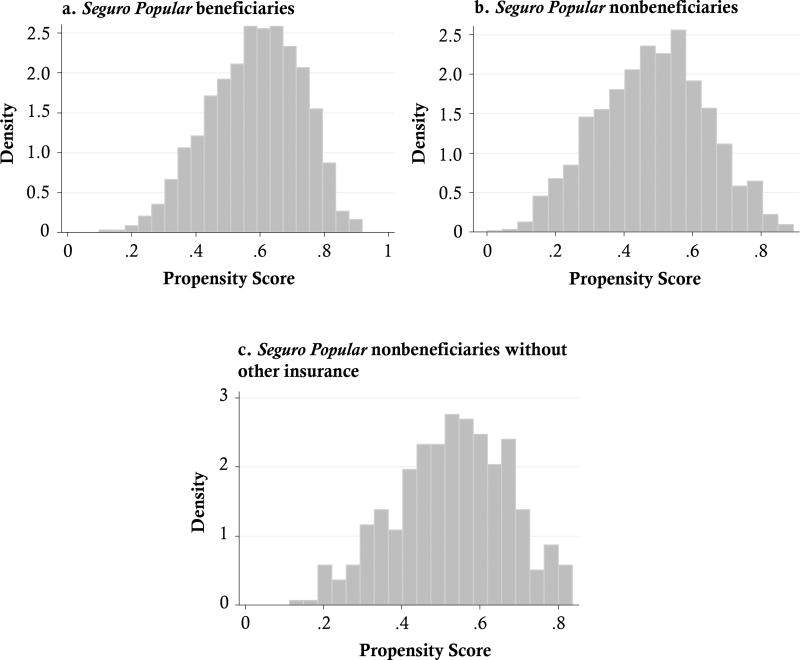
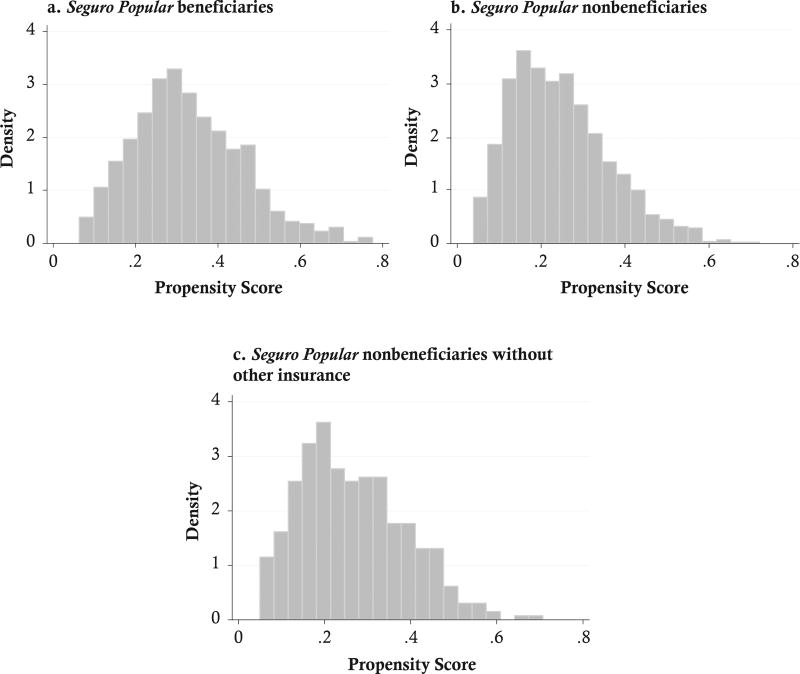
Figures 1 and 2 provide graphs showing the distribution of estimated propensity scores for Seguro Popular beneficiaries, the distribution of nonbeneficiaries, and the distribution of nonbeneficiaries who also have no alternative health insurance postprogram for rural and urban areas, respectively. The distribution of estimated propensity scores is remarkably similar between Seguro Popular beneficiaries and both groups of nonbeneficiaries, particularly in rural areas.11 For urban areas, the distribution of propensity scores is also very similar between beneficiaries and the two groups of nonbeneficiaries. The only exception is the group of urban beneficiaries with propensity scores greater than 0.5, among whom there are fewer comparable nonbeneficiaries. We thus also conducted an alternative estimation in urban areas, restricting the effect analysis to include beneficiaries with propensity scores less than 0.5. These results were extremely similar to the results for all urban beneficiaries. In the main body of the text, then, we report only those results based on the entire sample of beneficiaries in both rural and urban areas.
Fig. 1.
Propensity scores for Seguro Popular beneficiaries and nonbeneficiaries for men and women aged 50 and older without a health insurance preprogram in 2001: Rural areas
Fig. 2.
Propensity scores for Seguro Popular beneficiaries and nonbeneficiaries for men and women aged 50 and older without a health insurance preprogram in 2001: Urban areas
Tables 7 and 8 present the main difference-in-difference matching results. As we discuss earlier, we present two sets of estimations: (1) those in which the comparison group are individuals without Seguro Popular postprogram; and (2) those in which the comparison group are individuals without Seguro Popular and with no other alternative health insurance postprogram. This first impact estimation better approximates the current policy context, where the Seguro Popular program was introduced in an environment with various available alternative health insurance options. The second set of impact estimations closer approximates the potential impact of Seguro Popular versus the counterfactual of no other health insurance. We expect that the impact estimates will be greater for this second comparison group.
Table 7.
Estimated effects of Seguro Popular on health care use in the MHAS in rural areas for all men and women aged 50 without health insurance preprogram (2001): Difference-in-difference local linear matching 2001–2012a
|
Seguro Popular vs. No Seguro Popular in 2012 |
Seguro Popular vs. No Other Health Insurance in 2012 |
|||
|---|---|---|---|---|
|
|
|
|||
| Nonbeneficiary Level 2012 |
Local Linear |
Nonbeneficiary Level 2012 |
Local Linear |
|
| Usage and Preventive Care | ||||
| Saw a doctor in past year | 0.62 | 0.048 (0.033) | 0.52 | 0.145** (0.044) |
| Saw a dentist in past year | 0.17 | 0.039† (0.024) | 0.14 | 0.056* (0.027) |
| Hospitalized in past year | 0.11 | 0.002 (0.187) | 0.08 | 0.024 (0.018) |
| Diabetes test in past two years | 0.67 | 0.083* (0.036) | 0.56 | 0.124*** (0.038) |
| Hypertension test in past two years | 0.27 | 0.069* (0.033) | 0.23 | 0.125** (0.045) |
| Gynecological exam in past two years | 0.50 | −0.014 (0.044) | 0.40 | 0.028 (0.052) |
| Prostate test in past two years | 0.72 | −0.004 (0.038) | 0.62 | 0.039 (0.039) |
| Receiving Treatmentb | ||||
| (Conditional) probability of being in treatment for hypertension | 0.83 | 0.011 (0.088) | 0.77 | 0.023 (0.081) |
| (Conditional) probability of following diet for diabetes | 0.57 | −0.064 (0.142) | 050 | −0.008 (0.275) |
| (Conditional) probability of taking insulin for diabetes | 0.12 | 0.023 (0.087) | 0.07 | 0.204** (0.070) |
Note: Standard errors are shown in parentheses.
All estimates are difference-in-difference estimators using information from 2001 and 2012.
Conditional probability of treatment, conditional on reporting having disease.
p < .10;
p < .05;
p < .01;
p < .001
Table 8.
Estimated impacts of Seguro Popular on health care use in the MHAS in urban areas for all men and women aged 50 without health insurance preprogram (2001): Difference-in-difference local linear matching 2001–2012 a
|
Seguro Popular vs. No Seguro Popular in 2012 |
Seguro Popular vs. No Other Health Insurance in 2012 |
|||
|---|---|---|---|---|
|
|
|
|||
| Nonbeneficiary Level 2012 |
Local Linear |
Nonbeneficiary Level 2012 |
Local Linear |
|
| Usage and Preventive Care | ||||
| Saw a doctor in past year | 0.70 | −0.007 (0.034) | 0.56 | 0.101* (0.042) |
| Saw a dentist in past year | 0.28 | −0.045† (0.027) | 0.24 | −0.033 (0.032) |
| Hospitalized in past year | 0.10 | −0.030 (0.020) | 0.07 | 0.009 (0.022) |
| Diabetes test in past two years | 0.74 | −0.012 (0.033) | 0.57 | 0.087† (0.044) |
| Hypertension test in past two years | 0.33 | −0.005 (0.040) | 0.22 | 0.101* (0.045) |
| Gynecological exam in past two years | 0.58 | 0.028 (0.048) | 0.40 | 0.157* (0.068) |
| Prostate test in past two years | 0.74 | 0.016 (0.047) | 0.60 | 0.131* (0.054) |
| Receiving Treatmentb | ||||
| (Conditional) probability of being in treatment for hypertension | 0.85 | −0.031 (0.065) | 0.78 | −0.020 (0.096) |
| (Conditional) probability of following diet for diabetes | 0.61 | −0.063 (0.124) | 0.53 | −0.014 (0.269) |
| (Conditional) probability of taking insulin for diabetes | 0.15 | −0.009 (0.071) | 0.05 | 0.190* (0.077) |
Note: Standard errors are shown in parentheses.
All estimates are difference-in-difference estimators using information from 2001 and 2012.
Conditional probability of treatment, conditional on reporting having disease.
p < .10;
p < .05;
p < .01;
p < .001
Beginning with Table 7, in rural areas, the results are suggestive of significant positive impacts of Seguro Popular on utilization and the use of diagnostic tests. In particular, participating in Seguro Popular in rural areas relative to not participating increases the probability of seeing a dentist during the previous year by 4 percentage points, the probability of having a test for hypertension by 7 percentage points, and the probability of having a test for diabetes by 8 percentage points. In the second set of estimates, in which the comparison group is the population with no health insurance, results are qualitatively similar and somewhat larger, as expected for this counterfactual. Effects on the probability of having a test for hypertension or diabetes both increase by 12 percentage points, and the point estimate for having seen a doctor during the previous year is significant at 14 percentage points. In this second set of estimates restricting the comparison population to be those with no health insurance, we also find a significant and very large effect of 20 percentage points on the probability of taking insulin among diabetics.
With respect to urban areas (see Table 8), the estimates comparing the Seguro Popular population with nonbeneficiaries overall show very few significant effects. Of the 10 impact indicators studied, only the probability of seeing a dentist over the previous year is significant at the 10 % level. This is not particularly surprising because the majority of uninsured individuals preprogram (approximately two-thirds) in urban areas who do not acquire Seguro Popular during the panel acquire an alternative form of health insurance. Thus, the comparison of beneficiaries to nonbeneficiaries is largely a comparison of those with Seguro Popular with a population in which the majority of individuals have alternative insurance.
The urban results, where the counterfactual is represented by the population without any health insurance, however, show a number of significant effects. In particular, of the 10 impact indicators studied, 6 show statistically significant and large effects. The effects are most apparent on diagnostic tests; of the four variables studied, hypertension test, diabetes test, prostate exam, and gynecological exam all are significant and positive, with marginal effects ranging from 9 to 15 percentage points.
The differences between the two sets of results for urban areas are striking and important to contextualize. We interpret the first set of results as better approximating the true effects of the introduction of the Seguro Popular program in urban areas because of the existence of other forms of health insurance when the program was introduced. This situation naturally reduces the estimated effects by taking into account potential health insurance substitutes for those not in the program. The second set of analyses, in which we effectively assume that nonbeneficiaries are unable to access other forms of health insurance, produces impact estimates that may be more applicable to areas of the country with few formal sector jobs available and thus fewer options for health insurance preprogram. In rural areas, we find fewer differences between the two sets of estimates, reflecting fewer health insurance alternatives for the population without Seguro Popular in rural areas versus urban areas. When the counterfactual is restricted to be the population with no alternative health insurance in 2012, the estimated impacts of Seguro Popular are large, significant, and of similar magnitudes in both rural and urban areas.
Finally, we take advantage of community-level information on health services in the geographical area of the respondent to test how impacts may vary by access to services. We carry out a simple test in which we divide the sample in two according to the median number of doctors per capita in the locality of residence. We carry out this analysis for rural areas only, for which we hypothesize greater limitations in the availability of services.
Table 9 presents these results. We compare Seguro Popular effects for the population with less than the median access to doctors and those with more than the median access to doctors. For the indicators of utilization and preventive/diagnostic tests, the effects of Seguro Popular are generally similar by the level of available medical services. As in the overall results from Tables 7 and 8, the impact estimates in the specification comparing beneficiaries to the population with no health insurance are larger than those comparing beneficiaries to nonbeneficiaries. These results suggest that the level of available medical services in one’s geographical residence does not seem to affect the magnitude of the impact estimates on the variables of health care usage and the use of diagnostic tests.
Table 9.
Estimated effects of Seguro Popular on health care use in the MHAS in rural areas for all men and women aged 50 without health insurance preprogram (2001), by above or below median access to health services: Difference-in-difference local linear matching 2001–2012a
| Rural Population With Less Than Median Access to Health Services |
Rural Population With More Than Median Access to Health Services |
|||
|---|---|---|---|---|
|
|
|
|||
| Indicator |
Seguro Popular vs. No Seguro Popular |
Seguro Popular vs. No Insurance |
Seguro Popular vs. No Seguro Popular |
Seguro Popular vs. No Insurance |
| Usage and Preventive Care | ||||
| Saw a doctor in past year | 0.025 (0.047) | 0.126* (0.059) | 0.063 (0.048) | 0.172* (0.069) |
| Saw a dentist in past year | 0.021 (0.036) | 0.068 (0.042) | 0.052 (0.032) | 0.056 (0.039) |
| Hospitalized in past year | 0.009 (0.025) | 0.028 (0.028) | 0.000 (0.023) | 0.030 (0.022) |
| Diabetes test in past two years | 0.136** (0.048) | 0.143* (0.058) | 0.016 (0.049) | 0.089 (0.057) |
| Hypertension test in past two years | 0.111† (0.062) | 0.113† (0.058) | 0.001 (0.054) | 0.115* (0.068) |
| Gynecological exam in past two years | 0.071 (0.068) | 0.077 (0.066) | −0.064 (0.064) | 0.014 (0.089) |
| Prostate test in past two years | 0.024 (0.026) | 0.027 (0.051) | 0.015 (0.051) | 0.069 (0.058) |
| Receiving Treatmentb | ||||
| (Conditional) probability of being in treatment for hypertension | −0.121 (0.101) | −0.050 (0.112) | 0.136 (0.091) | 0.165† (0.103) |
| (Conditional) probability of following diet for diabetes | −0.446 (0.421) | −0.363 (0.465) | −0.001 (0.072) | −0.014 (0.418) |
| (Conditional) probability of taking insulin for diabetes | −0.050 (0.177) | 0.117 (0.160) | 0.158* (0.076) | 0.308** (0.117) |
Note: Standard errors are shown in parentheses.
All estimates are difference-in-difference estimators using information from 2001 and 2012.
Conditional probability of treatment, conditional on reporting having disease.
p < .10;
p < .05;
p < .01;
p < .001
However, turning to the indicators measuring treatment conditional on having a chronic illness, the results support the hypothesis of substantially greater effects on health indicators in areas where rural residents have access to more services. In particular, Table 9 shows no significant effects of the Program on the probability of being in treatment for the ill population in rural areas with lower than median access to doctors. However, for the population with greater than median access to health services, we find statistically significant and large positive program impacts on the probability of being in treatment for hypertension (14 to 17 percentage points) and the probability of taking insulin, conditional on having diabetes (16 to 30 percentage points).
The size of these effects is particularly noteworthy given the low proportion of ill individuals who are in treatment. Preprogram in rural areas, 53 % of those with hypertension reported taking medication, and only 6 % of diabetics reported taking insulin. The estimates are suggestive of large increases in treatment for those living in areas with greater than the median level of services.
Why would greater impacts for the Seguro Popular program in areas with more medical services be apparent only on treatment variables? We hypothesize that basic health services—such as seeing a doctor or having a test for hypertension—are broadly available even in isolated rural areas, and therefore that the effects of insurance on these variables are similar and independent of the supply of services. However, the supply of medications, such as insulin or hypertension medication, may be greater in areas with more medical services, thus permitting higher potential effects of a health insurance program (Rivera-Hernandez et al. 2016).
Conclusions
Using the longitudinal Mexican Health and Aging Study over the period 2001 to 2012, this article studied the effects of the Mexican health insurance program Seguro Popular on indicators related to health inputs for the population aged 50 and older, including utilization of health care services, diagnostic/preventive tests, and treatment, conditional on being ill. We have carried out longitudinal difference-in-difference matching estimators using information on Seguro Popular receipt. Our findings suggest significant positive effects on the usage of health care services and on receiving diagnostic tests, with more limited effects on treatment, conditional on being ill.
We also analyzed program impacts according to the availability of preprogram health services. Our evidence suggests important differences in the impacts of Seguro Popular on the probability of being in treatment in rural areas, depending on the availability of services. In particular, for the population with greater access to health services, we found larger and much more general effects on treatment conditional on illness. This is consistent with Bleich et al.’s (2007) finding of greater effects on treatment for hypertension in areas with a larger supply of medical services and with Grogger et al.’s (2014) finding of larger effects of Seguro Popular on catastrophic spending in areas with more medical services. Although public health insurance schemes might naturally aim to introduce health insurance to populations who have very low coverage preprogram, populations without health insurance in developing countries may also be located in geographic areas with few health services. Introducing health insurance to geographical areas lacking adequate health infrastructure is likely to be ineffective unless complemented by investment in the supply side of health services infrastructure (Travis et al. 2004). To our knowledge, few studies in other contexts have studied how health insurance impacts vary by the supply of health services, although a number of studies have related health outcomes to the supply of health services (e.g., see Shi and Starfield 2001). We consider this to be an important area for future research.
At an aggregate level, however, impacts were lower on variables measuring treatment conditional on illness compared with the impacts on utilization and diagnostic health tests. These results are consistent with those of Rivera-Hernandez et al. (2016), who found very limited effects of the Seguro Popular program on diverse treatment indicators for both hypertensive and diabetic patients. Although the Seguro Popular program covers medication for hypertension as well as insulin for diabetics, limited effects on treatment might result from insufficient supplies of these medicines or lack of adherence to treatment in spite of having access to medication. Mortality rates from diabetes in Mexico are exceedingly high—much higher than in the United States, despite similar levels of obesity. Data from the World Health Organization showed that the age-standardized death rate from diabetes was about 8 times higher in Mexico than in the United States (World Health Organization 2014). This likely reflects a complicated combination in Mexico of less detection/knowledge, later detection of ill individuals, lack of access to services for treatment, prohibitive costs of treatment, and lack of adherence/compliance to treatment for detected patients. Much future work is needed to understand and address these distinct obstacles to effective control of chronic illness (Rivera-Hernandez et al. 2016).
Finally, our study raised the issue of the appropriate counterfactual for impact estimation when introducing health insurance for uncovered workers when a covered or formal sector exists and mobility exists between sectors, as in Mexico. Unlike pilot programs introduced in areas with few substitute programs, the large-scale introduction of insurance for informal sector workers in Mexico occurred in a context of existing substitutes for a majority of workers, particularly those located in urban areas. When the existence of these alternatives to health insurance is taken into account, the overall effects of Seguro Popular are significantly smaller, as would be expected. Thus, we believe that the interactions between Seguro Popular coverage and coverage in social security and other institutions providing health insurance are an important dimension to continue studying in the future.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the very helpful assistance of Ana Cristina Perez-Gea. They also acknowledge support from the Sealy Center on Aging at the University of Texas Medical Branch in Galveston, from Grant R01AG018016, and the Health of Older Minorities T32AG00270 training grant from the National Institutes of Health/National Institute on Aging. The authors acknowledge also support from the Davis School of Gerontology at the University of Southern California and from the Multidisciplinary Research Training in Gerontology training grant (T32AG000037) and award P30AG043073—all from the National Institutes of Health/National Institute on Aging. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
For the purposes of this article, the aging population is defined as the population aged 50 and older.
An interesting research question is how Seguro Popular might affect the supply and quality of services. The Seguro Popular program does not have or build health facilities of its own but might affect construction of health facilities by the Secretary of Health through increased demand for health services associated with participation in the program. If this occurs, any impacts of Seguro Popular would reflect not only program characteristics but also these new facilities.
Lloyd-Sherlock et al. (2014) studied hypertension in six low- and middle-income countries, including Mexico, and found that for the case of hypertension, only about 44 % of Mexicans with hypertension were aware of their condition. They also found that only about 12 % of the ill population has effective control of their hypertension.
We do not use the MHAS 2012 subsample biomarker data to study impacts of the Seguro Popular for two reasons. First, our empirical strategy requires pre- and postprogram data, and the MHAS 2001 baseline does not include biomarkers. Second, the sample size of those with biomarkers in 2012 in our sample who report having a chronic disease is small.
Individuals in the subsample with biomarkers in 2012 are informed about the results of these tests. However, the biomarker tests were conducted after the self-report of treatment-seeking behaviors (in a subsequent health visit); thus, responses on treatment for ill individuals should not be biased by the results of the tests.
We also carry out impact estimates using nearest neighbor matching (two and five neighbors). Given their similarity to the estimates reported here, we report only estimates based on local linear matching.
Heckman and Smith (1995) coined the term “substitution bias” to refer to the situation in which individuals in a comparison group obtain a close substitute of the treatment. In our context, approximately 40 % of nonbeneficiaries in 2012 had an alternative form of health insurance in rural areas versus more than 60 % in urban areas.
Some studies (e.g., Maloney 1999) have shown substantial worker mobility in Mexico between formal (i.e., with social security benefits) and informal jobs (i.e., without social security benefits). Bosch and Campos-Vazquez (2014) demonstrated that the Seguro Popular program has reduced the number of employees affiliated with IMSS from small firms by approximately 4 %.
Censuses were conducted in 2000, 2005, and 2010. INEGI constructs population figures between census years by using a geometric model to extrapolate. The National Population Council (CONAPO) provides its own population series, adjusting for possible underreporting of census numbers. Results using either the INEGI series or the CONAPO series are extremely similar.
We analyze the effect of the Seguro Popular program on mortality in more detail in a separate study using survival analysis techniques (Parker et al. 2015).
We carry out balancing tests based on Dehejia and Wahba (2002), which examine whether the distribution of the covariates included in the propensity score model is independent of program participation conditional on the estimated propensity score—as it should be if the propensity score model is correctly specified, and the estimator is consistent. The test stratifies treatment and control observations into strata, based on the estimated propensity score (in quintiles), and then tests for significant differences between the covariates within each stratum. Nearly all of our covariates did not show significant differences.
References
- Alatinga KA, Williams JJ. Towards universal health coverage: Exploring the determinants of household enrolment into national health insurance in the Kassena Nankana District, Ghana. Ghana Journal of Development Studies. 2015;12(1–2):88–105. [Google Scholar]
- Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen’s behavioral model of health services use: A systematic review of studies from 1998–2011. GMS Psycho-Social-Medicine. 2012;9(Doc11) doi: 10.3205/psm000089. https://dx.doi.org/10.3205/psm000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barros R. Wealthier but not much healthier: Effects of a health insurance program for the poor in Mexico (Stanford Institute for Economic Policy Research Working Paper No. 09-002) Stanford, CA: Stanford University; 2008. [Google Scholar]
- Bitran R. Universal health coverage and the challenge of informal employment: Lessons from developing countries (Health, Nutrition, and Population Discussion Paper No. 87077) Washington, DC: World Bank Group; 2014. [Google Scholar]
- Bleich SN, Cutler DM, Adams AS, Lozano R, Murray CJ. Impact of insurance and supply of health professionals on coverage of treatment for hypertension in Mexico: Population based study. BMJ. 2007;335:875. doi: 10.1136/bmj.39350.617616.BE. https://doi.org/10.1136/bmj.39350.617616.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosch M, Campos-Vazquez RM. The trade-offs of welfare policies in labor markets with informal jobs: The case of the Seguro Popular program in Mexico. American Economic Journal. 2014;6(4):71–99. [Google Scholar]
- CONAPO. Envejecimiento de la población de Mexico: Reto del siglo XXI [Aging of the population of Mexico: Challenges for the 21st century] Mexico City, Mexico: Consejo Nacional de Poblacion; 2005. [Google Scholar]
- Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- Dehejia RH, Wahba S. Propensity score matching methods for nonexperimental causal studies. Review of Economics and Statistics. 2002;84:151–161. [Google Scholar]
- Galárraga O, Sosa-Rubí SG, Salinas A, Sesma S. Health insurance for the poor: Impact on catastrophic and out-of-pocket health expenditures in Mexico. European Journal of Health Economics. 2012;11:437–447. doi: 10.1007/s10198-009-0180-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Pier E, Juan M, Sepulveda J, Garcia-Junco D, Frenk J, Chertorivksi S, Soberon G. Hacia la cobertura universal en salud: Protección social para todos en Mexico [Toward universal health coverage: Social protection for all in Mexico]. Salud Pública de México. 2013;55:207–235. doi: 10.1590/s0036-36342013000200013. [DOI] [PubMed] [Google Scholar]
- Grogger J, Arnold T, Leon AS, Ome A. Heterogeneity in the effect of public health insurance on catastrophic out-of-pocket health expenditures: The case of Mexico. Health Policy and Planning. 2014;30:593–599. doi: 10.1093/heapol/czu037. [DOI] [PubMed] [Google Scholar]
- Hadley J. Insurance coverage, medical care use, and short-term health changes following an unintentional injury or the onset of a chronic condition. JAMA. 2007;297:1073–1084. doi: 10.1001/jama.297.10.1073. [DOI] [PubMed] [Google Scholar]
- Ham Chande R. El envejecimiento en Mexico: El siguiente reto de la transición demográfica [Aging in Mexico: The next challenge of the demographic transition] Tijuana, Baja California, Mexico: El Colegio de la Frontera Norte; 2003. [Google Scholar]
- Harris J, Sosa-Rubí S. Impact of “Seguro Popular” on prenatal visits in Mexico, 2002–2005: Latent class model of count data with a discrete endogenous variable (NBER Working Paper No. 14995) Cambridge, MA: National Bureau of Economic Research; 2009. [Google Scholar]
- Heckman J, Ichimura H, Todd P. Matching as an econometric evaluation estimator: Evidence from evaluating a job training program. Review of Economic Studies. 1997;64:605–654. [Google Scholar]
- Heckman JJ, Smith AS. Assessing the case for social experiments. Journal of Economic Perspectives. 1995;9(2):85–110. [Google Scholar]
- Hidayat B. Financial sustainability of the national health insurance in Indonesia: A first year review (Policy Brief of the Indonesian-German Social Protection Programme) 2015 Retrieved from http://health.bmz.de/what_we_do/Universal-Health-Coverage/Indonesia_on_the_way_to_universal_health_coverage/Policy_Brief_GIZ_SPP_Financial_Sustainability_of_Indonesian_Health_Insurance.pdf.
- Instituto Nacional de Salud Pública. Encuesta Nacional de Salud y Nutricion: Resultados nacionales [National Survey of Health and Nutrition: National results] Cuernavaca, Mexico: Instituto Nacional de Salud Pública; 2012. [Google Scholar]
- Knaul F, Méndez-Carniado O, Arreola-Ornelas H. Protección financiera en salud: Actualizaciones para México a 2014 [Financial protection in health: Updates for Mexico in 2014]. Salud Pública de México. 2016;58:341–350. doi: 10.21149/spm.v58i3.7886. [DOI] [PubMed] [Google Scholar]
- Knaul FM, González-Pier E, Gómez-Dantés O, García-Junco D, Arreola-Ornelas H, Barraza-Lloréns M, Frenk J. The quest for universal health coverage: Achieving social protection for all in Mexico. Lancet. 2012;380:1259–1279. doi: 10.1016/S0140-6736(12)61068-X. [DOI] [PubMed] [Google Scholar]
- Knox M. Health insurance for all: An evaluation of Mexico’s Seguro Popular program (Unpublished manuscript) Berkeley: Department of Economics, University of California; 2008. [Google Scholar]
- Lagomarsino G, Garabrant A, Adyas A, Muga R, Otoo N. Moving towards universal health coverage: Health insurance reforms in nine developing countries in Africa and Asia. Lancet. 2012;380:933–943. doi: 10.1016/S0140-6736(12)61147-7. [DOI] [PubMed] [Google Scholar]
- Limwattananon S, Neelsen S, O’Donnell O, Prakongsai P, Tangcharoensathien V, Van Doorslaer E, Vongmongkol V. Universal coverage with supply-side reform: The impact on medical expenditure risk and utilization in Thailand. Journal of Public Economics. 2015;121:79–94. [Google Scholar]
- Lloyd-Sherlock P, Beard J, Minicuci N, Ebrahim S, Chatterji S. Hypertension among older adults in low- and middle-income countries: prevalence, awareness and control. International Journal of Epidemiology. 2014;43:116–128. doi: 10.1093/ije/dyt215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maloney WF. Does informality imply segmentation in urban labor markets? Evidence from sectoral transitions in Mexico. World Bank Economic Review. 1999;13:275–302. [Google Scholar]
- Mboi N. Indonesia: On the way to universal health care. Health Systems & Reform. 2015;1:91–97. doi: 10.1080/23288604.2015.1020642. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) Global status report on noncommunicable diseases. Geneva, Switzerland: WHO; 2014. Retrieved from http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf?ua=1. [Google Scholar]
- Parker S, Saenz J, Wong R. Can health insurance improve health and reduce mortality? Evidence from the Seguro Popular program in Mexico; Paper presented at the annual meeting of the Population Association of America; San Diego, California. 2015. Apr, [Google Scholar]
- Partida-Bush V. Proceedings of the United Nations Expert Group Meeting on Social and Economic Implications of Changing Population Age Structures. Mexico City, Mexico: 2006. Aug, Demographic transition, demographic bonus and ageing in Mexico. Retrieved from http://www.un.org/esa/population/meetings/Proceedings_EGM_Mex_2005/partida.pdf. [Google Scholar]
- Rivera-Hernandez M, Rahman M, Mor V, Galarraga O. The impact of social health insurance on diabetes and hypertension process indicators among older adults in Mexico. Health Services Research. 2016;51:1323–1346. doi: 10.1111/1475-6773.12404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Secretaría de Salud. Carta de derechos y obligaciones [Letter of rights and obligations] Mexico City, Mexico: Secretaría de Salud; 2013. [Google Scholar]
- Shi L, Starfield B. The effect of primary care physician supply and income inequality on mortality among blacks and whites in US metropolitan areas. American Journal of Public Health. 2001;91:1246–1250. doi: 10.2105/ajph.91.8.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somkotra T, Lagrada LP. Payments for health care and its effect on catastrophe and impoverishment: Experience from the transition to Universal Coverage in Thailand. Social Science & Medicine. 2008;67:2027–2035. doi: 10.1016/j.socscimed.2008.09.047. [DOI] [PubMed] [Google Scholar]
- Sosa-Rubí SG, Galárraga O, Harris JE. Heterogeneous impact of the “Seguro Popular” program on the utilization of obstetrical services in Mexico, 2001–2006: A multinomial probit model with a discrete endogenous variable. Journal of Health Economics. 2009a;28:20–34. doi: 10.1016/j.jhealeco.2008.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sosa-Rubí SG, Galárraga O, López-Ridaura R. Diabetes treatment and control: The effect of public health insurance for the poor in Mexico. Bulletin of the World Health Organization. 2009b;87:512–519. doi: 10.2471/BLT.08.053256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tejeda S, Darnell JS, Cho YI, Stolley MR, Markossian TW, Calhoun EA. Patient barriers to follow-up care for breast and cervical cancer abnormalities. Journal of Women’s Health. 2013;22:507–517. doi: 10.1089/jwh.2012.3590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travis P, Bennett S, Haines A, Pang T, Bhutta Z, Hyder AA, Evans T. Overcoming health-systems constraints to achieve the Millennium Development Goals. Lancet. 2004;364:900–906. doi: 10.1016/S0140-6736(04)16987-0. [DOI] [PubMed] [Google Scholar]
- Wong R, Michaels-Obregon A, Palloni A. Cohort profile: The Mexican Health and Aging Study (MHAS) International Journal of Epidemiology. 2017;46:e2. doi: 10.1093/ije/dyu263. https://doi.org/10.1093/ije/dyu263. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.