Abstract
PURPOSE
In literature, many studies compare survival rates of different types of FPDs. Most of them compared restorations, which originated from one university, but from different clinicians. Data about restoration survival rates by only one experienced dentist are very rare. The aim of this study was to evaluate the survival rate of allceramic FPDs without the blurring effects of different clinicians.
MATERIALS AND METHODS
153 veneeredzirconia FPDs were observed for follow-up. 22 patients received 131 single crowns and 22 bridges. Because of the different bridge lengths, one unit was defined as a restored or replaced tooth. In total, 201 units were included. Only the restorations performed by the same clinician and produced in the same dental laboratory from 2011 to 2016 were included. Considered factors were defined as “type of unit”, “type of abutment”, “intraoral region”, and “vitality”. Modified UHPHS criteria were used for evaluation. Statistical analysis was performed using cox-regression.
RESULTS
189 units (94.0%) showed no kind of failure. 5 chippings (2.4%) could be corrected by intraoral polishing. 4 units (1.9%) exhibited spontaneous decementation. These polishable and recementable restorations are still in clinical use. Chippings or decementations, which lead to total failure, did not occur. One unit was completely fractured (0.5 %). Biological failures (caries, periodontitis or periimplantitis) did not occur. The statistical analysis of the factors did not reveal any significant differences.
CONCLUSION
Modern all-ceramic FPDs seem to be an appropriate therapy not only for single restorations but for complex occlusal rehabilitations.
Keywords: All-ceramic, Survival, Single crowns, Zirconia
INTRODUCTION
The development of new ceramic materials and new manufacturing techniques is still an important theme in prosthetic dentistry, especially for tooth- or implant-retained single crowns or fixed partial dentures (FPDs). Nevertheless, failures such as chipping or fractures are still a problem with all-ceramic FPDs.1 Beside advances in material science, different strategies have been developed in recent years to reduce the risk of chipping in these restorations (e.g. by avoiding thin veneering ceramic layers or by using anatoform frameworks to support the veneering ceramic in the cusp).2,3 In 2015, Naenni et al.4 observed more chipping in the pressing technique, but this was not statistically significant. Full anatomical monolithic restorations, e.g. zirconia restorations, seem to be a good alternative to veneered restorations,5 especially in posterior regions. Unfortunately, zirconia has some disadvantages, such as poorer aesthetic quality than monolithic crowns of silicate ceramics or manually veneered restorations.6 Furthermore, there is a spontaneous t-m phase transformation in the superficial layer of zirconia in contact with water. This phenomenon is called long term low temperature degradation and leads to a roughened surface and reduction in mechanical stability.7 Beside zirconia, there are many different types of monolithic ceramic materials, such as lithium disilicate, or hybrid zirconia-stabilized glass-ceramics, e.g. Celtra Duo (Degudent, Germany) or Suprinity (VITA Zahnfabrik, Germany). The indications for these materials are often restricted to anterior crowns or small bridges including the second premolar. In this context, Marquardt and Strub found a 5 year survival rate of approximately 70% for IPS empress 2 all-ceramic FPDs.8 However, further prospective research on veneered zirconia restorations is needed, especially for large restorations.3
Because of the continuing development of materials for all-ceramic restorations in recent years, it is essential to document the success or failure of these restorations, in order to learn more about treatment strategies for all ceramic restorations. Some of the studies include patients who were treated at a single university hospital, but by many different clinicians9 or by clinicians in different practices. Only a few studies include patients who were treated by only one experienced clinician10 or in one dental practice.11 Most of the studies that address the long term success of all-ceramic restorations emphasize that more publications on this theme are needed.
The aim of the current study was to evaluate the survival rate of modern all-ceramic crowns, with special focus on the influence of the type of crown, the type of abutment, and the intraoral region, and on the vitality of the tooth. To avoid the effect of different clinicians or different dental laboratories, only the restorations were included, which were performed by the same experienced clinician and produced in the same dental laboratory.
MATERIALS AND METHODS
In total, 153 veneered-zirconia restorations were observed retrospectively during the periodic follow-up examinations. Twenty-two patients received 131 single crowns and 22 bridges. In contrast to many other studies, only patients were included who had been treated by the same experienced clinician (PCP) in the Department of Prosthetic Dentistry and Biomedical Materials Research at Hannover Medical School in the period from 2011 to 2016. Patients with veneered zirconia restorations were included in this study. These patients received single crowns, FPDs of different size or full arch restorations with occlusal reconstructions on natural teeth or implants. All of the 153 restorations were produced at the same dental laboratory (Reese & Deppe GmbH, Minden, Germany). All of the zirconia frameworks had a reduced anatoform design and were milled from Zenotec Zr Bridge (Wieland Dental, Pforzheim, Germany) and veneered manually using IPS e.max Ceram (Ivoclar Vivadent AG, Schaan Liechtenstein). Before cementation, the abutment-teeth were degreased with alcohol and dried with oil-free pressured air. The restorations were cemented using permanent glass ionomer luting cement (Ketac Cem, 3M, Neuss, Germany). The patients made frequent follow-up visits to the same clinician during the first year after 3, 6, and 12 months. The subsequent follow-up period was extended to 12 months.
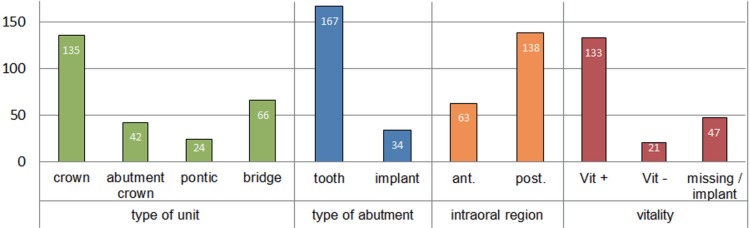
The patients' data are given in Table 1. Because of the different lengths of the bridges, one unit was defined as a restored tooth (single crowns, abutment crowns) or replaced tooth (implant retained crown, pontics). For example, a bridge with two abutment crowns and two replaced teeth is considered four units. Factors of the restorations that might influence the survival rates were defined as “type of unit”, “type of abutment”, “intraoral region”, and “vitality”. The “type of unit” could be a crown, abutment-crown, or pontic. The “type of abutment” was tooth or implant and the “intraoral region” was anterior or posterior. The distribution of the units to these factors is shown in Fig. 1. Modified UHPHS criteria12 were used to evaluate the restorations during the regular follow-up care (Table 2).
Table 1. Data and distribution of the units (n = 201).
| 22 Patients, n = 201 units = 153 restorations | |
|---|---|
| Male | n = 11 |
| Female | n = 11 |
| Patients with < 6 units | n = 8 = 23 units = 15 restorations |
| Patients with ≥ 6 units | n = 14 = 178 units = 138 restorations |
Fig. 1. Distribution of the units to “type of units”, “type of abutment”, “intraoral region”, and to “vitality”.
Table 2. Definition of modified UHPHS criteria for chipping, decementation, and fracture.
| Alpha (A) | Bravo (B) | Charlie (C) | Delta (D) | |
|---|---|---|---|---|
| Chipping | Small chipping - polishing possible | Chipping - reparation possible | ||
| Fracture | no failure | - | - | New restoration is necessary |
| Decementation | Recementation possible | Recementation - reparation possible |
For all types of failure, Alpha (A) describes a situation without failures. Bravo (B) signifies chipping and describes small fractures within the superficial veneering layer. In this case, only some reshaping and polishing was necessary. (B) was also given with decementation, if recementation without repair was possible. The classification Charlie (C) specified chipping and decementation, for which repair was possible with intra-oral or extra-oral composite prior to recementation. Chipping, fracture, or decementation, which lead to replacement of the damaged restoration, were defined as Delta (D) (Table 2). If there was more than one type of failure in one unit, the first failure was taken as the failure of the restoration.
Statistical analysis was performed using SPSS 23.0 (IBM Corporation, Armonk, NY, USA). Initially descriptive analysis was performed. Survival rates were described by Kaplan-Meier analysis and log-rank tests. The comparison between the Kaplan-Meier curves was performed with the Cox regression. The level of significance was set at P = .05.
RESULTS
In total, 153 restorations with 201 units were evaluated in follow-up care from 2011 to 2016. All of the units were allocated to 133 single crowns (66.2%) and 20 bridges, with 44 abutment-crowns (21.9%) and 24 pontics (11.9%). Sixty-three (63) units (31.1%) were located in the anterior region, with 138 units (68.7%) in the posterior region. 83.1% units were cemented onto natural teeth, and 16.9% onto implant-abutments. The mean follow-up period for all restorations was 31.8 ± 15.0 months. The shortest observation time was 7.4 months and the longest 58.6 months.
Table 3 shows an overview of all failures during the observation period from 2011 to 2016. The data were differentiated between damaged restorations and damaged units. In total, 189 units (94.0%) showed no failure (UHPHS-A). Five chippings (2.4%, UHPHS-B) could be easily corrected by intraoral polishing. Furthermore, 4 units (1.9%, UHPHS-B) exhibited spontaneous decementation. It was unnecessary to replace polishable or recementable restorations, and the restorations are still in clinical use. UHPHS-C failures did not occur. Finally one unit fractured completely (0.5%, UHPHS-D) and had to be replaced. This fracture occurred on a second upper molar due to accidental mechanical overload during chewing. Biological failures, such as caries, inflammation of periodontal tissues, or peri-implantitis, did not occur.
Table 3. Distribution of the observed failure types: chipping, fracture, and decementation, categorized by modified UHPHS criteria.
| 100% = 153 restorations in total (131 crowns, 22 bridges) = 201 units | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chipping | Fracture | Decementation | ||||||||||
| UHPHS criteria | A | B | C | D | A | B | C | D | A | B | C | D |
| Number of damaged units | - | 5 | - | 1 | - | 1 | - | 4 | - | - | ||
| Number of damaged restorations | - | 5 | - | 1 | - | 1 | - | 3 | - | - | ||
The cumulative survival rates of the restorations were analyzed by the Kaplan-Meier procedure, both overall and with respect to the initially defined factors. Cox regression was used for this analysis.
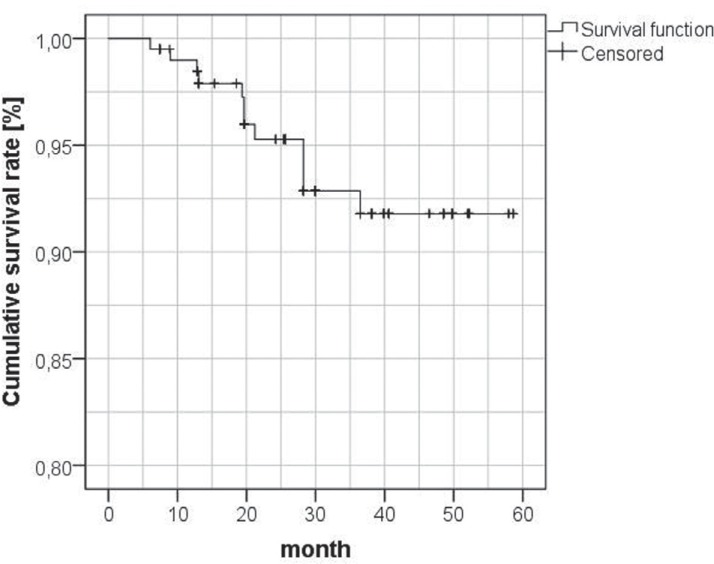
The graph in Fig. 2 shows the cumulative survival rate (CSR) of all units. The first chipping occurred after 6 months (CSR6 = 99.5%). Within the next 6 months, two more failures were observed, resulting in CSR12 = 98.5%. The 95% survival rate was reached at 21.2 months. In all, 11 failures were observed after 36 months (CSR36 = 91.8%). There were no more failures during the rest of the observation period.
Fig. 2. Cumulative survival rate of all restorations: Kaplan-Meier graph of cumulative survival rates in percent.
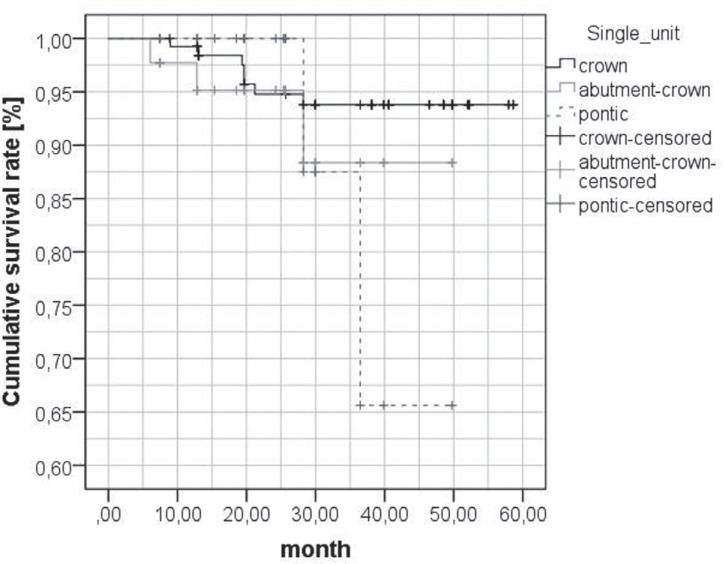
Fig. 3 shows the Kaplan-Meier analysis for the different types of the units, divided into tooth- and implant-retained single crowns, abutment crowns and pontics. The first failure of a single crown (n = 133), a decementation, occurred after 8.9 months. Further 5 failures of single crowns (4 chippings and 1 decementation) were observed by 28.2 months after cementation (CSR36 = 93.8%). During the rest of the observation time, no more failures occurred on the single crowns. For the abutment-crowns (n = 44), the first chipping occurred after 6.1 months (CSR6 = 97.7%). Further 2 failures were observed by 12.8 months (CSR12 = 95.2%) and by 28.2 month (CSR36 = 88.4%). Two failures occurred on pontics (n = 24) within the first 36 months (CSR36 = 65.6%). Cox regression detected no significant influence of the type of the units (P = .250).
Fig. 3. Cumulative survival rate for the types of the units: Kaplan-Meier graph of cumulative survival rates in percent.
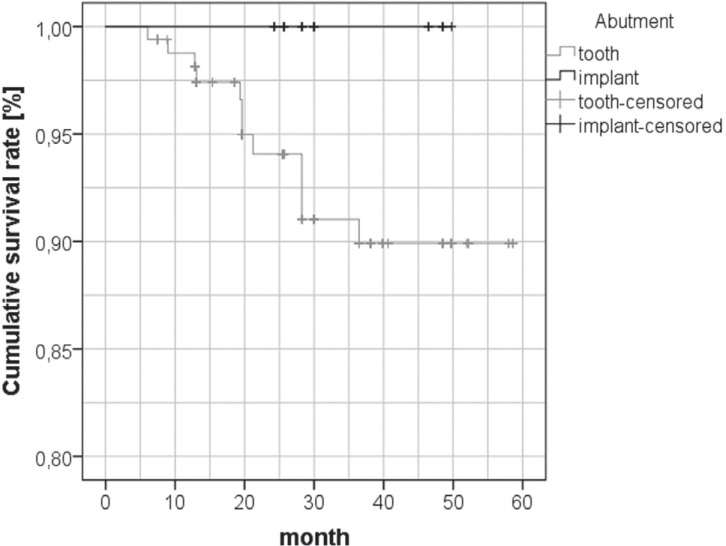
In Fig. 4, the CSR is given for crowns (single crowns and abutment-crowns) cemented either on natural teeth or on implants. No failure occurred on implant-retained restorations during the complete observation period (CSR = 100%). Tooth-retained restorations showed 1 failure during the first 6 months (CSR6 = 99.4%). Further two failures occurred during the first year (CSR12 = 98.8%). During the second year, further five failures occurred on tooth-retained restorations (CSR24 = 94.1 %). Two more failures occurred in the third year (CSR36 = 89.9 %). After that, no further failures were recorded. Cox regression detected no significant influence of the type of abutment (P = .978).
Fig. 4. Cumulative survival rate depending on the type of abutment: Kaplan-Meier graph of cumulative survival rates in percent.
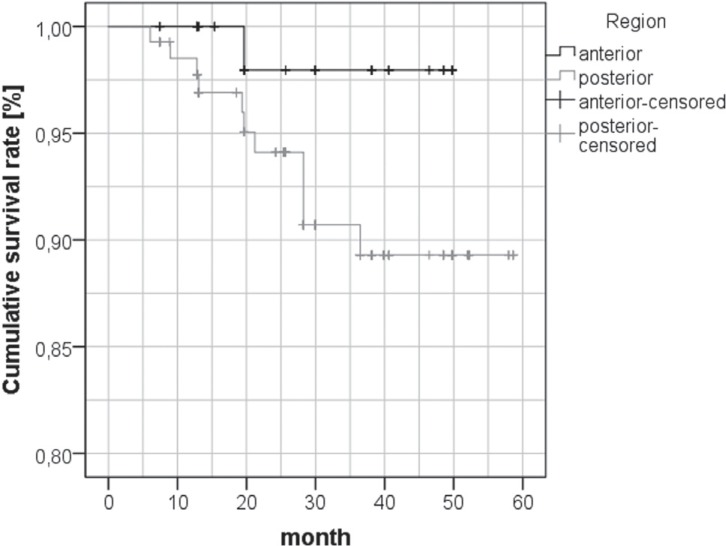
The influence of the region on CSR is shown in Fig. 5; in the anterior region, only one failure occurred during the first 2 years (CSR24 = 98.0%). In the posterior region, a total of 11 failures occurred. The first failure was observed after 6.1 months (CSR6 = 99.3%). During the first year after cementation, two more failures occurred (CSR12 = 97.7%). Further one fracture, three decementations, and five chippings could be seen during the first three years (CSR36 = 89.3%). After that, no more failures were found during the observation period. Cox regression showed no significant influence of the type of the region (P = .160).
Fig. 5. Cumulative survival rate for crowns in the anterior or posterior region: Kaplan-Meier graph of cumulative survival rates in percent.
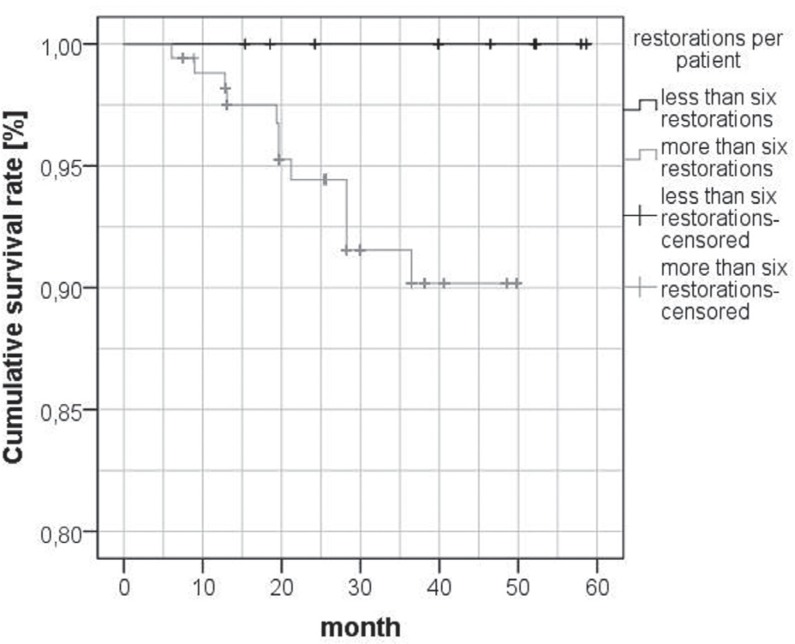
Fig. 6 shows the Kaplan-Meier graph of the CSR of all restorations depending on the number of units per patient. If there were less than six restorations per patient, no failures were observed (CSR = 100%). All failures occurred in patients with more than six restorations within the first 36 months (CSR24 = 91.5%). After that, no more failures were observed. Cox regression showed no significant influence of the number of restorations for each patient (P = .331).
Fig. 6. Cumulative survival rate for restorations consisting of up to 6 or more than 6 units: Kaplan-Meier graph of cumulative survival rates in percent.
DISCUSSION
In this study, 22 patients received 153 veneered zirconia restorations consisting of 201 units. This is a large number of restorations compared to most of the published literature. The data of the current study include a group of patients who were treated by only one experienced dentist. All of the restorations were produced in the same dental laboratory. The current study benefits from high standardization of the dental and technical quality. Existing literature often only includes patients with isolated restorations. In contrast, the current study included patients with one or more single crowns, with FPD and full arch reconstructions. This allows a more realistic view of failures, even in complex clinical situations. During the observation period of the current study, many new ceramics were developed. In particular, monolithic hybrid ceramic materials, e.g. Surprinity (VITA Zahnfabrik, Germany) and CeltraDuo (Degudent, Germany), were introduced. In 2006, Marquardt and Strub found a 5 year survival rate of 100% for all-ceramic single crowns and 70% for all-ceramic FPDs, both made of monolithic IPS-Empress 2 with adhesive luting.8 They showed that monolithic restorations can be an interesting alternative for veneered all-ceramic single crowns. Monolithic restorations have no need of any veneering process, and therefore no risk of chipping. However, these materials have a limited indication. For this reason, veneered restorations, which were observed in this study, still play an important role, especially in aesthetically important areas.
In the current study, the influences of different factors on the cumulative survival rates were analyzed. For the different factors, Kaplan-Meier analysis showed CSRs between 100% and 65.6% because of case censoring. Although a large number of restorations were included, the distribution of the restorations to the different factors was not balanced; on the other hand, exclusion of restorations to equalize the number of restorations would have reduced the clinical relevance of the study.
Further, the length of the observation periods of the restorations differed in this study. Therefore, many restorations had to be censored in Kaplan-Meier analysis and Cox regression during the first years of their observation. The result was that the number of incidents during the later observation time decreased. Accordingly, this caused a very large decrease in the Kaplan-Meier curves, e.g. the pontic graph in Fig. 2. Further, the smaller number of restorations with an observation period of more than 36 month might be a reason for the decreasing number of incidents after 36 month. Eisenburger and Tschernitschek defined two phases after receiving new removable dentures: The first phase, the adaption phase, ends after 24 months, followed by the use phase. They found that the highest number of failures or need for corrections occurred during the adaption phase.13 The findings of the current study might suggest that the adaption phase of FDPs ends within the first 36 month, which also might result in a decreasing number of incidents.
The findings of the current study are in line with current literature on the overall survival of veneered zirconia restorations. In 2015, Beuer et al.14 published 3 year clinical results for veneered zirconia FPDs on teeth or implants. Kaplan-Meier analysis showed survival rate probabilities of 93.9% for all restorations. In their 2012 literature review titled “Survival and Complications of zirconia based FDPs”, Raigrodski et al.15 found comparable survival rates. They reported that, during the entire observation time of this study, 93.4% of 153 cases showed no failure. Ten restorations (6.6%) failed, but only two of these ten restorations (1.3%) had to be replaced.
In contrast to the current study, many studies only observed a small number of restorations. Isolated restorations were often included in these studies. Raigrodski et al.16 observed 20 zirconia-based posterior FPDs in 16 patients and found a 5-year survival rate of approximately 95%. Molin and Karlsson3 examined 19 FPDs in 18 patients for approximately 5 years and found no complete failure but one decementation and roughened surfaces in occlusal contact areas. In contrast to the current study, these two studies only focused on FPDs, not on single crowns, and might have less clinical relevance because of their relatively smaller number of restorations. In the published literature, studies with a large numbers of restorations are rare. In 2012, Ortorp et al.11 observed 206 zirconia single crowns in 169 patients. Of these veneered zirconia crowns, 143 could be observed for more than 5 years and showed a CSR of 88%. In their study, not only technical failures were observed but also biological failures, such as loss of the abutment tooth, periodontal problems or caries. However, the most common types of failure were loss of retention and chipping. The results of Ortorp et al. on the mechanical failures are comparable to the findings of the current study because of the similar number of restorations and a comparable study design. In contrast to the present study, Ortorp et al. only analyzed isolated restorations, excluding full-arch rehabilitations.
Modern metal-ceramic FPDs are still generally accepted alternatives for all-ceramic restorations. With modern CAD/CAM-fabricated veneered titanium crowns, Hey et al. reported a 6 year survival rate of 91.3%. They found 12 mechanical complications and 1 biological complication on 41 restorations in total.17 Prabhu et al.18 observed veneered FPDs built by “direct metal laser sintering technique”. They observed 45 patients with posterior restorations and found a CSR of 95.5%. In their June 2015 review, Sailer et al.19 compared the 5 year survival rates of metal-ceramic crowns to all-ceramic restorations. They found similar survival rates for metal-ceramic crowns (94.7%) and zirconia all-ceramic crowns (96.0%). The CSR of 93.4% of veneered zirconia restorations in the current study is in line with the study by Sailer et al. and indicates that these restorations may be a good alternative for modern metal-ceramic FPDs. In the current study, complete failures (UHPHS D) were observed in only 2 restorations. Biological failures - such as loss of restorations because of caries, periodontal inflammation, or peri-implantitis - did not occur in any of the observed restorations.
Beside the large number of restorations and patients treated by only one clinician, the clinical relevance of the current study is enhanced by the number of factors studied. Cox regression analysis of the type of restoration (or unit) failed to detect any statistically significant influence of this factor. There is apparently no published study which explicitly compares the survival rates for more than 5 years of single crowns and abutment-crowns depending on the support either on natural teeth or on implants. In 2007, Pjetursson et al.20 published a review of tooth- or implant-supported FPDs. They found comparable CSRs for tooth- or implant support if “end-abutment” restorations or single crowns were used. Beuer et al.14 also analyzed this factor and found no significant influence of the type of the abutment support after 3 years. The current study also showed no significant influence of the type of the abutment support.
Regarding the region, Sailer et al.19 found significantly more mechanical failures on veneered zirconia crowns in posterior regions than in anterior regions. The data of the current study also showed more failures in the posterior region than in the anterior region, but the statistical analysis showed no significance. This might be caused by the greater number of posterior restorations than anterior restorations in this study.
There are apparently no publications on the influence of the number of fixed all-ceramic restorations in one patient on the long term success. The data of the current study showed more failures in patients with more than 6 all-ceramic units, but cox-regression showed no statistically significant influence of this factor (P = .331). Therefore, modern veneered all-ceramic restorations seem to be a suitable option for full-arch restorations, although the theoretical risk of restoration damage will increase with the number of the restorations within one patient.
There is little published literature on the 10 year survival rates of all-ceramic FPDs. In 2011, Sax et al.21 reported the clinical outcomes of FPDs with zirconia frameworks. They concluded that zirconia frameworks showed good longterm stability (91.5%), but problems such as chipping were frequently reported. They found a mechanical complication rate of 32%, but traced this back to the “prototype status of the system”. In 2016, Ioannidis and Bindl22 published 10 year results of a clinical evaluation of 57 veneered zirconia-based three-unit FPDs. They found technical failure rates of 28%. The CSR after ten years was 85%. In total, only three (5.2%) of the 57 restorations failed because of biological complications.22 The data of the current study showed overall 5 year survival rates of porcelain veneered all-ceramic restorations of about 93.4%. However, further research is needed to expand our knowledge of the long-term survival of modern all-ceramic FPDs, especially for FPDs older than 10 years.
CONCLUSION
Within the limitations of the current study, the data showed that the survival of modern all-ceramic restorations does not depend on the factors observed in this study (Table 2). Further it can be concluded that modern all-ceramic restorations are an appropriate therapy for complex occlusal rehabilitations in addition to its use for isolated restorations.
References
- 1.Schmitter M, Mueller D, Rues S. Chipping behaviour of allceramic crowns with zirconia framework and CAD/CAM manufactured veneer. J Dent. 2012;40:154–162. doi: 10.1016/j.jdent.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 2.Alhasanyah A, Vaidyanathan TK, Flinton RJ. Effect of core thickness differences on post-fatigue indentation fracture resistance of veneered zirconia crowns. J Prosthodont. 2013;22:383–390. doi: 10.1111/jopr.12016. [DOI] [PubMed] [Google Scholar]
- 3.Molin MK, Karlsson SL. Five-year clinical prospective evaluation of zirconia-based Denzir 3-unit FPDs. Int J Prosthodont. 2008;21:223–227. [PubMed] [Google Scholar]
- 4.Naenni N, Bindl A, Sax C, Hämmerle C, Sailer I. A randomized controlled clinical trial of 3-unit posterior zirconia-ceramic fixed dental prostheses (FDP) with layered or pressed veneering ceramics: 3-year results. J Dent. 2015;43:1365–1370. doi: 10.1016/j.jdent.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 5.Ramos GF, Monteiro EB, Bottino MA, Zhang Y, Marques de Melo R. Failure probability of three designs of zirconia crowns. Int J Periodontics Restorative Dent. 2015;35:843–849. doi: 10.11607/prd.2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harianawala HH, Kheur MG, Apte SK, Kale BB, Sethi TS, Kheur SM. Comparative analysis of transmittance for different types of commercially available zirconia and lithium disilicate materials. J Adv Prosthodont. 2014;6:456–461. doi: 10.4047/jap.2014.6.6.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kohorst P, Borchers L, Strempel J, Stiesch M, Hassel T, Bach FW, Hübsch C. Low-temperature degradation of different zirconia ceramics for dental applications. Acta Biomater. 2012;8:1213–1220. doi: 10.1016/j.actbio.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 8.Marquardt P, Strub JR. Survival rates of IPS empress 2 all-ceramic crowns and fixed partial dentures: results of a 5-year prospective clinical study. Quintessence Int. 2006;37:253–259. [PubMed] [Google Scholar]
- 9.Moráguez OD, Wiskott HW, Scherrer SS. Three- to nine-year survival estimates and fracture mechanisms of zirconia- and alumina-based restorations using standardized criteria to distinguish the severity of ceramic fractures. Clin Oral Investig. 2015;19:2295–2307. doi: 10.1007/s00784-015-1455-y. [DOI] [PubMed] [Google Scholar]
- 10.Rinke S, Kramer K, Bürgers R, Roediger M. A practice-based clinical evaluation of the survival and success of metal-ceramic and zirconia molar crowns: 5-year results. J Oral Rehabil. 2016;43:136–144. doi: 10.1111/joor.12348. [DOI] [PubMed] [Google Scholar]
- 11.Ortorp A, Kihl ML, Carlsson GE. A 5-year retrospective study of survival of zirconia single crowns fitted in a private clinical setting. J Dent. 2012;40:527–530. doi: 10.1016/j.jdent.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 12.Ryge G, Snyder M. Evaluating the clinical quality of restorations. J Am Dent Assoc. 1973;87:369–377. doi: 10.14219/jada.archive.1973.0421. [DOI] [PubMed] [Google Scholar]
- 13.Eisenburger M, Tschernitschek H. Clinical and technical comparison of the long term success of clasp retained dentures and of telescopic crown retained dentures. Dtsch Zahnärzl Z. 1998;53:257–259. [Google Scholar]
- 14.Beuer F, Sachs C, Groesser J, Gueth JF, Stimmelmayr M. Tooth-implant-supported posterior fixed dental prostheses with zirconia frameworks: 3-year clinical result. Clin Oral Investig. 2016;20:1079–1086. doi: 10.1007/s00784-015-1594-1. [DOI] [PubMed] [Google Scholar]
- 15.Raigrodski AJ, Hillstead MB, Meng GK, Chung KH. Survival and complications of zirconia-based fixed dental prostheses: a systematic review. J Prosthet Dent. 2012;107:170–177. doi: 10.1016/S0022-3913(12)60051-1. [DOI] [PubMed] [Google Scholar]
- 16.Raigrodski AJ, Yu A, Chiche GJ, Hochstedler JL, Mancl LA, Mohamed SE. Clinical efficacy of veneered zirconium dioxide-based posterior partial fixed dental prostheses: five-year results. J Prosthet Dent. 2012;108:214–222. doi: 10.1016/S0022-3913(12)60165-6. [DOI] [PubMed] [Google Scholar]
- 17.Hey J, Beuer F, Bensel T, Boeckler AF. Single crowns with CAD/CAM-fabricated copings from titanium: 6-year clinical results. J Prosthet Dent. 2014;112:150–154. doi: 10.1016/j.prosdent.2013.09.031. [DOI] [PubMed] [Google Scholar]
- 18.Prabhu R, Prabhu G, Baskaran E, Arumugam EM. Clinical acceptability of metal-ceramic fixed partial dental prosthesis fabricated with direct metal laser sintering technique-5 year follow-up. J Indian Prosthodont Soc. 2016;16:193–197. doi: 10.4103/0972-4052.176526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs) Dent Mater. 2015;31:603–623. doi: 10.1016/j.dental.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 20.Pjetursson BE, Brägger U, Lang NP, Zwahlen M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs) Clin Oral Implants Res. 2007;18:97–113. doi: 10.1111/j.1600-0501.2007.01439.x. [DOI] [PubMed] [Google Scholar]
- 21.Sax C, Hämmerle CH, Sailer I. 10-year clinical outcomes of fixed dental prostheses with zirconia frameworks. Int J Comput Dent. 2011;14:183–202. [PubMed] [Google Scholar]
- 22.Ioannidis A, Bindl A. Clinical prospective evaluation of zirconia-based three-unit posterior fixed dental prostheses: Up-to ten-year results. J Dent. 2016;47:80–85. doi: 10.1016/j.jdent.2016.01.014. [DOI] [PubMed] [Google Scholar]