Abstract
PURPOSE
To investigate the effect of accelerated aging on surface properties of glazed CAD/CAM resin blocks using a 2D surface profilometer and a 3D non-contact optical profilometer.
MATERIALS AND METHODS
Three types of CAD/CAM resin restorative materials, LAVA Ultimate (3M ESPE, St Paul, MN, USA), VITA Enamic (Vita Zahnfabrik H. Rauter, Bad Säckingen, Germany), and Cerasmart (GC Corparation, Tokyo, Japan) were used for this study. CAD/CAM blocks were cut in 3-mm thickness slabs and divided into three groups; Group 1: control group (specimens polished with 600 grit SCI paper); Group 2: specimens sandblasted, silanized, and glazed with Optiglaze Color (GC); Group 3: glazed specimens subjected to 5000 thermocycles (n=15). The surface roughness (Ra and Rz) was evaluated using a profilometer and a 3D scanning instrument. Data were analyzed using two-way ANOVA and Tukey's post-hoc test (P<.05).
RESULTS
LAVA, VITA, and Cerasmart exhibited statistically similar Ra and Rz values for each group (P>.05). For VITA and Cerasmart, the specimens in Group 1 exhibited significantly higher Ra values than Group 2 (P<.05). Group 1 (0.502 Ra), Group 2 (0.384 Ra), and Group 3 (0.431 Ra) exhibited statistically similar Ra values for LAVA (P=.062). After 5000 thermocycles, surface roughness values did not change significantly for glazed LAVA, VITA, and Cerasmart (P>.05).
CONCLUSION
Glaze material Optiglaze Color makes CAD/CAM resin surfaces smooth and glazed CAD/CAM surfaces seem resistant to deterioration under 5000 thermocycles.
Keywords: CAD/CAM restoratives, Sandblasting, Optiglaze color, Surface roughness
INTRODUCTION
Computer-aided design/computer-aided manufacturing (CAD/CAM) advancements were introduced during the 1970s and have only been available for routine dental practice since 1990.1 However, interest in CAD/CAM technology has increased sharply over the last few years2,3 and nowadays, a large-scale class of indirect materials are represented.4 CAD/CAM materials have several advantages such as biocompatibility, durability, and esthetics, reduced clinical steps, shorter production runtime, and lower cost.5,6 These systems can be used to construct inlays, onlays, crowns, and veneers. There are currently two main groups for CAD/CAM materials; ceramics and composites. Composite restorative materials have some advantages compared with ceramics, and ceramics have some advantages over composites. Composite-incorporating materials are more compliant and soft, have easy finishing and polishing properties, and are less abrasive for opposite teeth, although they experience high wear.5 On the other hand, ceramic restorations with esthetic properties are superior to composite materials. Additionally, ceramics are more wear resistant, biocompatible, and discoloration resistant.6,7
Surface roughness in restorations may cause plaque accumulation and discoloration on restorative materials.8,9,10 It is reported that surface irregularities that form on the restoration as a result of a successful finishing and polishing process are smaller than the average bacterial diameter so that bacterial adhesion should be prevented.10 A rough surface may cause adhesion of bacteria to restorative material8,11,12 and secondary caries. A rough restoration may also cause dental abrasions for antagonist teeth. Furthermore, surface roughness can affect the fracture resistance of materials causing micro-crack creation and propagation on restorative materials.13,14 In general, 0.3 Ra surface roughness values on restoration surfaces are clinically acceptable.11 Polishing processes can create smooth surfaces with maximum bend strength and minimal risk of cracking and fracture in CAD/CAM restorations.13,14,15,16 Therefore, accomplishing a smooth surface for restorations is critical for patient satisfaction, as well as for esthetic and natural reasons.8,9,17,18
Therefore, during milling and finishing procedures, a rough surface may be produced and this roughness may cause surface flaws and reduce strength of restorative materials. Various techniques such as glazing have been proposed to strengthen restoratives after surface flaws have been introduced.13 Laboratory and clinical data are highly needed because composite CAD/CAM blocks are new materials. Therefore, the surface structure of three different CAD/CAM resin blocks were investigated in this study, in particular to assess the effect of glaze material on surface topography of CAD/CAM system and the effect of thermocycles on their surface roughness. Our hypotheses were 1) Glazing does not affect surface properties of CAD/CAM resin restoratives; 2) Thermocycles deteriorate glazed CAD/CAM surfaces.
MATERIALS AND METHODS
Three CAD/CAM resin blocks; LAVA Ultimate CAD/CAM restorative (3M ESPE, St. Paul, MN, USA), VITA Enamic (Vita Zahnfabrik H. Rauter, Bad Säckingen, Germany), and Cerasmart (GC Corporation, Tokyo, Japan) were used in this study. The manufacturers and compositions are shown in Table 1.
Table 1. Materials used in this study.
| Material | Type | Component | Filler | Filler Content (wt %) |
|---|---|---|---|---|
| Optiglaze Color (GC Corparation, Tokyo, Japan) | Nano-filled glaze system | PMMA, MMA, photo inhibitor | Silica filler | NA |
| LAVA Ultimate (3M ESPE, St. Paul, MN, USA) | Resin Nano-ceramic | Bis-GMA, UDMA, Bis-EMA, TEGDMA | SiO2, ZrO2 | 80 |
| Si/ZrO2 cluster | ||||
| VITA Enamic (Vita Zahnfabrik H. Rauter, Bad Säckingen, Germany) | Hybrid-ceramic (polymer-infiltrated ceramic) | UDMA, TEGDMA | Feldspar ceramic enriched with aluminum oxide | 86 |
| Cerasmart (GC Corparation, Tokyo, Japan) | Nano-ceramic | Bis-MEPP, UDMA, DMA | SiO2 Barium glass | 71 |
PMMA; Poly methyl methacrylate; MMA: Methyl methacrylate; Bis-GMA: Bisphenol A glycidyl methacrylate; UDMA: Urethane dimethacrylate; Bis-EMA: Bisphenol A polyethethylene glycol diether dimethacrylate; TEGDMA: Triethylene glycol dimethacrylate; Bis-MEPP: 2,2-Bis (4-methacryloxypolyethoxyphenyl) propane; DMA: Dimethacrylate.
A total of 45 CAD/CAM block sections (3-mm thickness) were prepared for surface roughness measurements, (n = 15 specimens for each CAD/CAM block) and 9 block sections were prepared for 3D images using a slow-speed diamond saw (Isomet 1000, Buehler, Lake Bluff, IL, USA). The top surface of the sectioned slices was polished with 600 grit SiC papers for 60 seconds under running water. The specimens were then divided into three groups for surface roughness measurements (n = 15);
Group 1: Control group (600 SiC grinding).
Group 2: The specimens were sandblasted with Al2O3 (mean particle size 50 µm) (Renfert GmbH, 78247, Hilzingen, Germany) using a sandblaster machine (Basic Eco, Renfert GmbH, 78247, Hilzingen, Germany) at 2.5 bars pressure approximately 10 mm from the composite surface for 10 seconds. After this procedure, all samples were washed using air-water spray, cleaned in distilled water in an ultrasonic bath for 5 minutes, and finally air dried. After sandblasting, all specimens were silanized with G-Multi PRIMER (GC) for 30 seconds and air dried. Following silanization, Optiglaze Color (GC Corporation, Tokyo, Japan) was applied on all specimens according to the manufacturer's instructions. Specimens were then placed in a Labolight Duo (GC) indirect composite light oven and specimens were polymerized for 10 minutes Surface roughness measurements and 3D images were obtained again following polymerization.
Group 3: After 24 hours, three different CAD/CAM specimens were subjected to 5000 thermocycles between 5° – 55℃ with 30 seconds dwell time. Surface roughness values of specimens and 3D images were obtained again following thermocycling.
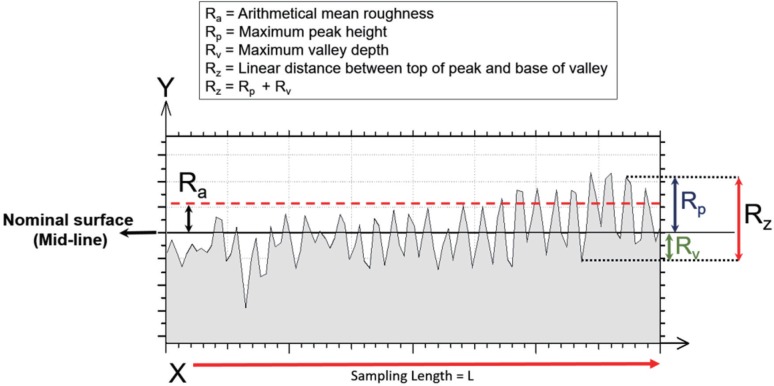
The surface roughness of specimens was measured using a 2-dimensional profilometer (Surtronic S128, Taylor Habson Ltd., Leicester, England) with a 5-µm diamond stylus angled at 90°. Starting from the midpoint of each specimen, 5 measurements were taken in different directions, with a cut-off length of 0.8 mm and measuring length of 4 mm, and the average roughness value for each specimen was then calculated and recorded (Ra and Rz values, in µm, Fig. 1).19
Fig. 1. Illustration of surface roughness parameters.
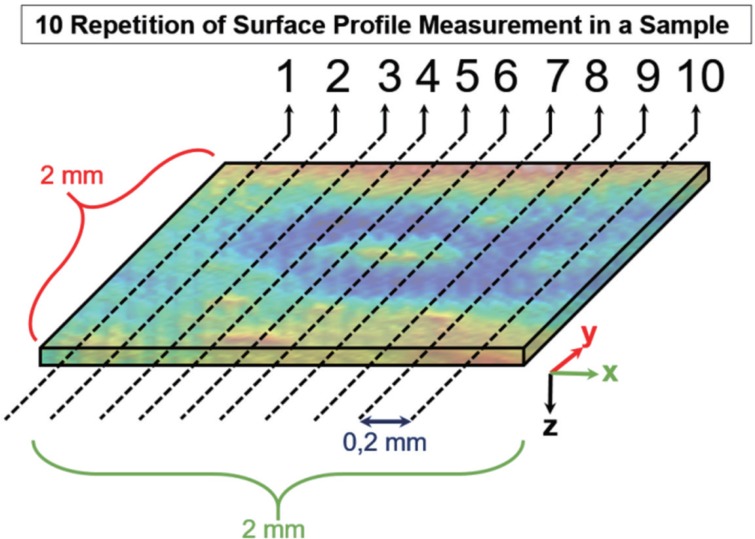
To determine the surface morphology and roughness parameters of samples, a Nanovea 3D Non-Contact Profilometer PS50 (Nanovea, 6 Morgan Ste 156, Irvine, CA, USA) was used. The non-contact laser profilometer has a leading edge optical pen that uses superior white light axial chromatism. A 2 × 2 mm square area was used for roughness analyses. The scanning process was accomplished in steps of 20 µm in both X and Y directions with 0.1 mm/s velocity. 3D surface topographies and profile roughness evaluations were realized using Mountain Software Version 6.2.7487 (Digital Surf). Profile roughness lines were taken from 3D scanned surfaces. In order to calculate the profile lines, 10 repetitions for each measurement were performed and the median values were used (Fig. 2). Surface profile lines 0.2 mm apart were taken and percentage error calculations were made for every sample.
Fig. 2. Illustration of obtaining profile roughness lines from 3D scanned surfaces. Ten repetitions were performed for each measurement and the median value was accepted as the profile image.
All statistical analyses were performed using IBM SPSS for Windows version 20.0 (SPSS, Chicago, IL, USA). Kolmogorov-Smirnov tests were used to test the normality of data distribution. Normally distributed continuous variables were expressed as mean ± standard . Differences between the groups and materials were analyzed using two-way ANOVA and Tukey's post-hdeviationoc test. P < .05 was considered statistically significant.
RESULTS
Surface roughness values (Ra and Rz values, in µm) are presented in Table 2 and Table 3. After SiC paper grinding, surface roughness Ra values for LAVA, VITA, and Cerasmart were found as 0.502, 0.584, and 0.490, respectively; all were found statistically similar (P = .141). In groups 2 and 3, LAVA, VITA, and Cerasmart exhibited statistically similar Ra values (P = .540 for VITA and P = .617 for Cerasmart).
Table 2. Surface roughness values (Ra, µm) (mean ± SD of the groups (n = 15)).
| Group | LAVA | VITA | CERASMART | P |
|---|---|---|---|---|
| 1 | 0.502 ± 0.135Aa | 0.584 ± 0.132Aa | 0.490 ± 0.144Aa | .141 |
| 2 | 0.384 ± 0.097Aa | 0.402 ± 0.114Ba | 0.358 ± 0.112Ba | .540 |
| 3 | 0.431 ± 0.144Aa | 0.396 ± 0.131Ba | 0.386 ± 0.126ABa | .617 |
| P | .062 | .001 | .026 |
Means followed by different lowercase letter in the row and different uppercase letter in the column are statistically significant different (P < .05).
Table 3. Surface roughness values (Rz, µm) (mean ± SD of the groups (n = 15)).
| Group | LAVA | VITA | CERASMART | P |
|---|---|---|---|---|
| 1 | 3.201 ± 0.444Aa | 3.566 ± 0.937Aa | 3.646 ± 1.042Aa | .317 |
| 2 | 2.280 ± 0.776Ba | 2.301 ± 0.671Ba | 2.153 ± 0.664Ba | .827 |
| 3 | 2.733 ± 0.632ABa | 2.453 ± 0.748Ba | 2.353 ± 0.939Ba | .396 |
| P | < .05 | < .05 | < .05 |
Means followed by different lowercase letter in the row and different uppercase letter in the column are statistically significant different (P < .05).
A comparison between groups showed that group 1 (0.502 Ra), group 2 (0.384 Ra), and group 3 (0.431 Ra) exhibited statistically similar Ra values for LAVA CAD/CAM restorative (P = .62). For VITA, group 2 (0.402 Ra) and group 3 (0.396 Ra) had statistically lower Ra values than group 1 (0.584 Ra) (P = .001). For Cerasmart, group 2 (0.358 Ra) had statistically lower Ra values than group 1 (0.490 Ra) (P = .026).
After glazing, the mean Ra values decreased for each CAD/CAM restorative, but only significantly for VITA and Cerasmart. After 5000 thermocycles (group 3), surface roughness values did not significantly change compared with group 2 (glazed LAVA, VITA, and Cerasmart) (P > .05).
According to Rz results, LAVA, VITA, and Cerasmart exhibited statistically similar results for group 1 (P = .317), group 2 (P = .827), and for group 3 (P = .396). For LAVA, the specimens in group 1 exhibited significantly higher Rz values than group 2 (P < .05). For VITA and Cerasmart, the specimens in group 1 exhibited significantly higher Rz values than group 2 and group 3 (P < .05). The specimens in group 2 and group 3 exhibited statistically similar Rz values for the three CAD/CAM restoratives (P < .05).
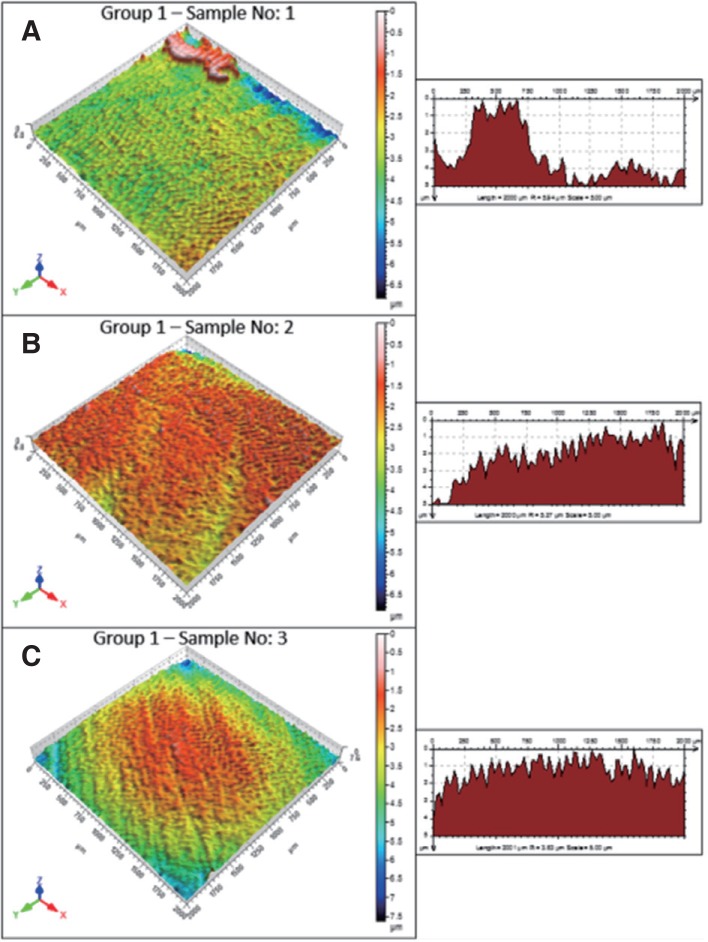
After SiC paper grinding, CAD/CAM restorative surfaces had the largest surface irregularities with concentrated sharp peaks and valleys. Surface roughness or irregularities of LAVA (Fig. 3A) were found higher than VITA (Fig. 3B) and Cerasmart (Fig. 3C). LAVA displayed a rough surface in a small area (Fig. 3A). The surface topography of VITA exhibited smooth in general and surface roughness increased in very small fields (Fig. 3B). For Cerasmart, surface irregularities showed variability with deep scratches, concentrated sharp peaks and valleys (Fig. 3C).
Fig. 3. 3D images of the specimens in group 1 (SiC paper grinding specimens). (A) LAVA, (B), VITA, (C) Cerasmart.
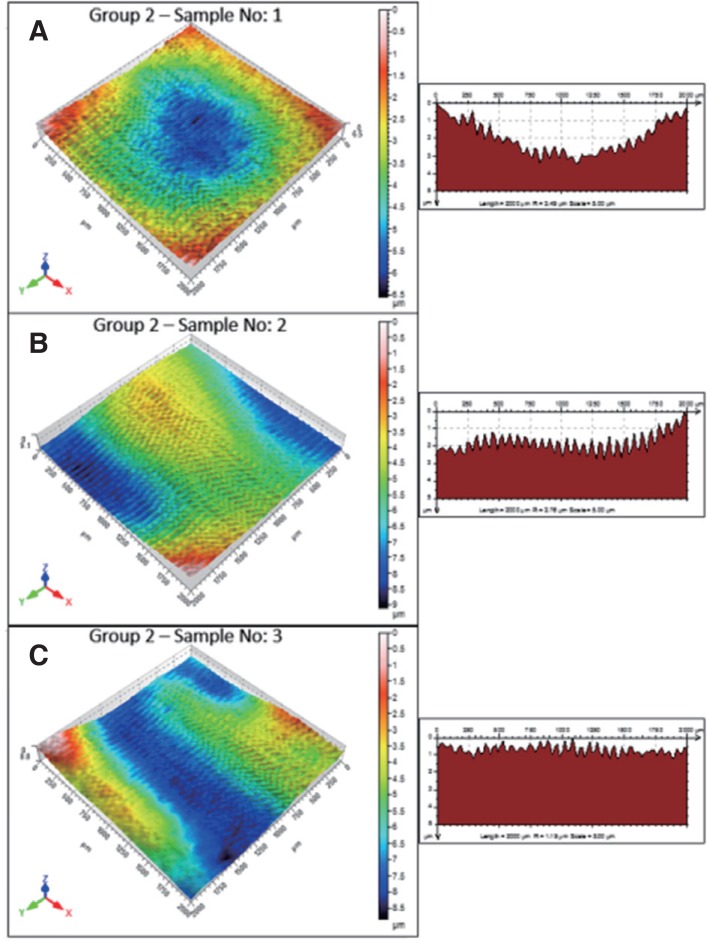
After Optiglaze color application (group 2), some irregularities and waving were observed on the surface with some concentrated peaks and valleys on the specimens of LAVA, VITA, and Cerasmart (Fig. 4). Surface roughness was moderate in some regions but decreased in others (Fig. 4). LAVA exhibited slightly less irregularity (Fig. 4A), followed by VITA and Cerasmart, respectively (Fig. 4B, 4C).
Fig. 4. 3D images of the specimens in group 2 (glazed specimens with Optiglaze Color). (A) LAVA, (B), VITA, (C) Cerasmart.
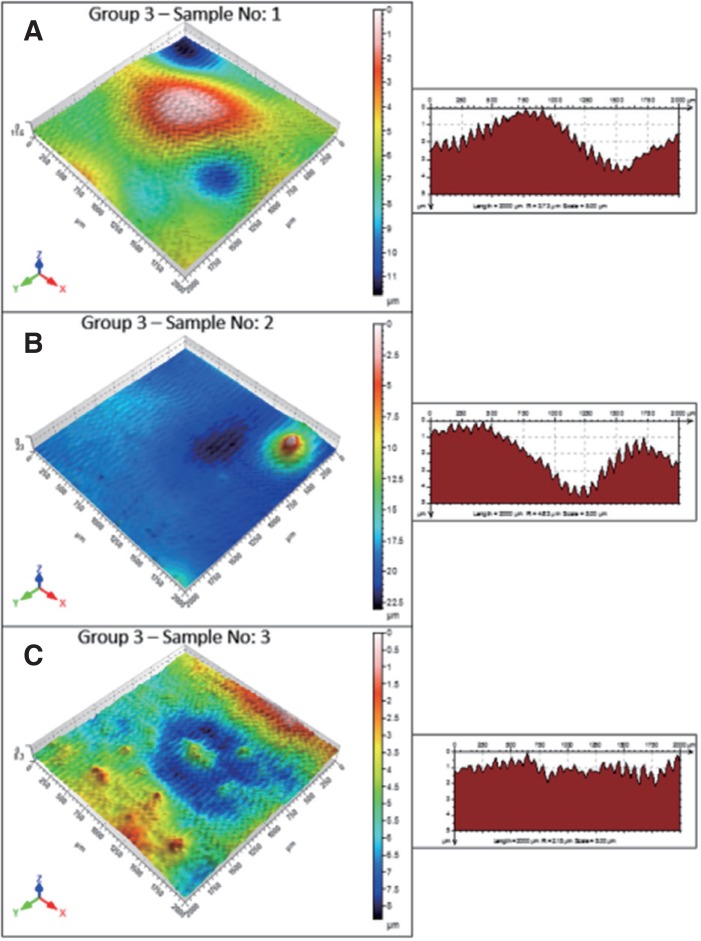
In thermocycled specimens (group 3), surface irregularities of CAD/CAM blocks showed concentrated peaks and valleys (Fig. 5). LAVA and VITA also exhibited slightly less irregularity than Cerasmart (Fig. 5). Surface irregularities of LAVA specimens showed variability. Surface roughness increased from slight to moderate and included excessive roughness in small areas in the form of islets (Fig. 5A). Only in a small area, VITA showed roughness from slight to moderate in a small islet shape (Fig. 5B). Cerasmart showed very variable surface irregularities (Fig. 5C). Surface roughness changed from slight to excessive. In some areas, moderate and slight roughness in the form of islets or peaks were also seen.
Fig. 5. 3D images of the specimens in group 3 (thermocycled specimens). (A) LAVA, (B), VITA, (C) Cerasmart.
DISCUSSION
Our first hypothesis; “Glazing does not affect surface properties of CAD/CAM resin restoratives” is rejected. After the glaze procedure, surface roughness values of each CAD/CAM restorative decreased and 3D surface topography was improved. Our second hypothesis “Thermocycles deteriorate glazed CAD/CAM surfaces” is also rejected. After 5000 thermocycles, surface roughness values of glazed CAD/CAM restoratives did not change significantly. Slight changes of surface properties of glazed CAD/CAM restoratives after 5000 thermal cycles were found on 3D images; however, they were negligible. Surface roughness is an important parameter for the clinical success of restoratives. A smooth surface provides comfort for patients and is important for the longevity of tooth-restoration integrity. The glaze procedure is the last step in the construction of CAD/CAM restoratives. Optiglaze Color is used as characterization material for direct and indirect composite materials, and it provides a smooth surface and wear resistance for restorations made of composite resin. Flury et al.20 reported that physicians should carefully finish and polish CAD/CAM restoratives to decrease surface roughness and to improve mechanical properties (surface hardness, elastic modulus, and flexural strength) of CAD/CAM materials.
Roughness is a key factor in evaluating surface-oriented scientific research such as polishing, wear, and degradation. In order to achieve a reliable analysis of surface quality and topography, using high-resolution surface roughness measurement techniques such as a non-contact laser profilometer is preferable. The development of laser technologies and computer analysis programs has made it possible to measure the surface roughness of materials using a non-contact method; white light induced by a laser source emitted by the optical pen to the sample surface and reflected from the surface. Surface analysis is performed using both sent and reflected light using program algorithms. Surface evaluation was achieved using a special program called Mountains 3D in this study. Thus, in this study, sample surfaces were scanned in 3D with a non-contact profilometer. From the surface scanning, besides gaining 3D surface topography maps, other important parameters such as Ra (arithmetic mean roughness) and Rz (mean roughness). Rz can be defined as the distance between maximum peak heights (Rp) and maximum valley depth (Rv). These roughness measurement parameters are schematically shown in Fig. 1. 3D roughness analysis was accomplished according to ISO 25178. Extracted profile line roughness parameters such as Ra were performed according to ISO 4287.
Bottino et al.21 reported that ceramics should always be polished to produce a smoother clinical surface. They glazed ceramic surfaces with Akzent 24 (VITA Zahnfabrik) and found 0.94 Ra surface roughness values. They showed that the smoothest ceramic surfaces were obtained after glazing. Perez et al.22 examined the effect of a glaze/composite sealant on the 3D surface roughness of esthetic restorative materials and showed that glaze material BisCover was capable of reducing surface roughness and provided polished surfaces for all materials (Filtek Supreme, Grandio and Vitremer). The authors attributed the dissimilarity in surface roughness of the materials to differences in their size and content of the filler particles. Al-Wahadni23 reported that regardless of the type of ceramic tested (IPS Empress or In-Ceram Alumina/Vita-dur Alpha) or pretreatment, any adjusted ceramic restoration should be glazed or subjected to finishing and polishing procedures. In agreement with Al-Wahadni,23 we found unglazed CAD/CAM surfaces were rougher than glazed surfaces.
Generally, dental technicians perform glaze procedures for many types of indirect restorations. However, together with the development of the CAD/CAM system, clinical application stages have started to decrease. Accordingly, after completion of the construction of a CAD/CAM restoration, physicians also wanted to eliminate the glaze stage. At this stage, clinically easy-to-use glaze materials entered clinical routine. Practitioners can easily apply sandblasting, silanization, and glaze by themselves. However, there is a lack of in vivo and in vitro studies related to the effectiveness of these glaze materials, especially on current CAD/CAM restoratives. Cilli et al.24 examined the role of surface sealant materials (glaze material for composites) on surface roughness of traditional composites after a simulated tooth brushing test. They revealed that glazed composites presented superior performance when compared with unglazed or unsealed composites. Dede et al.25 examined a conventional polishing system and three different glazed materials (Palaseal, Optiglaze, BisCover) on composite discs. The authors subjected specimens to 3000 thermocycles and measured surface roughness values using a profilometer and found that glaze techniques significantly improved the surface roughness of the tested composite resins. Sahin et al.26 examined the surface roughness values of Optiglaze-applied specimens (denture teeth) before and after 3000 thermocycles and reported that Optiglaze provided smooth and color-stable surfaces.
One of the aims of this study was to examine the changes in surface properties of glazed CAD/CAM resin restoratives after 5000 thermocycles. According to the profilometer results, no significant changes were observed after 5000 thermocycles, although slight deteriorations were observed in the 3D surface examination. In our previous studies, we examined the effect of glaze material (Fortify Plus) and accelerated aging on posterior composite surfaces. We found that rather than decreasing surface roughness values with the application of a glaze material, these values actually increased with an additional slight increase following thermocycling (10,000 thermocycles).19 Flury et al.27 examined the effect of water storage on the surface roughness of CAD/CAM restoratives. They found that surface roughness and micromechanical properties were significantly influenced by CAD/CAM material, polishing system, and water storage. Flury et al.27 reported that Lava Ultimate showed the lowest surface roughness values in 4 different CAD CAM blocks; Vitablocs Mark II, Paradigm MZ100, Vita Enamic, and Ambarino High-Class. Different from Flury et al.'s study, we found that LAVA, VITA, and Cerasmart exhibited statistically similar Ra results after SiC paper grinding, after glaze application, and after 5000 thermocycles. Tuncer et al.28 examined the effect of thermocycles on seven different composite materials. They reported that 10 000 thermocycles did not significantly affect the surface roughness values of the composites. Hahnel et al.29 examined the aging behavior of dental composites with regard to surface roughness after 7, 90, and 365 days or 2 × 3000 thermocycles. They reported that the composite material itself, the aging duration and, in part, the aging medium, all had a decisive influence on the mechanical properties of dental composites. They correlated the decreasing mechanical properties of composites with repeated temperature changes and degradation of matrix-filler bonds due to the different thermal expansion coefficients of fillers and the resin matrix. Different from light-curing composites, polymerization processes of CAD/CAM resin blocks become high-performance industrial polymerization involving high temperature and high pressure. Thus, a higher degree of conversion is obtained and more homogeneous polymerization is provided and the amount of internal defects decrease in CAD/CAM resin restoratives.30 Also, CAD/CAM resin materials generally incorporate urethane dimethacrylate (UDMA) instead of bisphenol A glycidyl methacrylate (Bis-GMA). UDMA shows higher degree of conversion and displays lower water sorption than Bis GMA.31,32 Therefore, mechanical properties of CAD/CAM resin materials enhanced according to light-curing composite materials.
Optiglaze is a low-viscosity resin with filler. Filler is added into the material to improve the mechanical properties of the glaze. It was observed in this study that although the surface of materials is smooth, the general view of the material exhibits slight waving on CAD/CAM surfaces. Optiglaze propagates and spreads simultaneously on CAD/CAM surfaces. The slight waving on CAD/CAM surfaces may be related to two causes. One may be related to the sandblasting procedure. Sandblasting can damage CAD/CAM surfaces33 and may create micro or macro pits and deep cavities on CAD/CAM surfaces. Even though the glaze fills these gaps and spreads onto the material surface, there may be a general topographic deterioration. Another reason for glaze waving may be related to the filler content of Optiglaze. The filler content of Optiglaze may make it viscous and this might be an obstacle to a homogeneous spread on CAD/CAM surfaces.
CONCLUSION
To conclude, LAVA, VITA, and Cerasmart exhibited similar surface roughness values for each group. Glazed CAD/CAM surfaces are more advanced and smooth compared with non-glazed surfaces. All materials used in this study seem to be durable against 5000 thermocycles. The 3D optical profilometer gives more detailed information related to CAD/CAM surfaces and properly reflected all specifications.
References
- 1.Duret F, Preston JD. CAD/CAM imaging in dentistry. Curr Opin Dent. 1991;1:150–154. [PubMed] [Google Scholar]
- 2.van Noort R. The future of dental devices is digital. Dent Mater. 2012;28:3–12. doi: 10.1016/j.dental.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 3.Conrad HJ, Seong WJ, Pesun IJ. Current ceramic materials and systems with clinical recommendations: a systematic review. J Prosthet Dent. 2007;98:389–404. doi: 10.1016/S0022-3913(07)60124-3. [DOI] [PubMed] [Google Scholar]
- 4.Mainjot AK, Dupont NM, Oudkerk JC, Dewael TY, Sadoun MJ. From artisanal to CAD-CAM blocks: State of the art of indirect composites. J Dent Res. 2016;95:487–495. doi: 10.1177/0022034516634286. [DOI] [PubMed] [Google Scholar]
- 5.Ruse ND, Sadoun MJ. Resin-composite blocks for dental CAD/CAM applications. J Dent Res. 2014;93:1232–1234. doi: 10.1177/0022034514553976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coldea A, Swain MV, Thiel N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent Mater. 2013;29:419–426. doi: 10.1016/j.dental.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Blatz MB. Long-term clinical success of all-ceramic posterior restorations. Quintessence Int. 2002;33:415–426. [PubMed] [Google Scholar]
- 8.Kawai K, Urano M, Ebisu S. Effect of surface roughness of porcelain on adhesion of bacteria and their synthesizing glucans. J Prosthet Dent. 2000;83:664–667. [PubMed] [Google Scholar]
- 9.Yilmaz C, Korkmaz T, Demirköprülü H, Ergün G, Ozkan Y. Color stability of glazed and polished dental porcelains. J Prosthodont. 2008;17:20–24. doi: 10.1111/j.1532-849X.2007.00237.x. [DOI] [PubMed] [Google Scholar]
- 10.Weitman RT, Eames WB. Plaque accumulation on composite surfaces after various finising procedures. J Am Dent Assoc. 1975;91:101–106. doi: 10.14219/jada.archive.1975.0294. [DOI] [PubMed] [Google Scholar]
- 11.Jones CS, Billington RW, Pearson GJ. The in vivo perception of roughness of restorations. Br Dent J. 2004;196:42–45. doi: 10.1038/sj.bdj.4810881. [DOI] [PubMed] [Google Scholar]
- 12.Ikeda M, Matin K, Nikaido T, Foxton RM, Tagami J. Effect of surface characteristics on adherence of S. mutans biofilms to indirect resin composites. Dent Mater J. 2007;26:915–923. doi: 10.4012/dmj.26.915. [DOI] [PubMed] [Google Scholar]
- 13.de Jager N, Feilzer AJ, Davidson CL. The influence of surface roughness on porcelain strength. Dent Mater. 2000;16:381–388. doi: 10.1016/s0109-5641(00)00030-0. [DOI] [PubMed] [Google Scholar]
- 14.Fischer H, Schäfer M, Marx R. Effect of surface roughness on flexural strength of veneer ceramics. J Dent Res. 2003;82:972–975. doi: 10.1177/154405910308201207. [DOI] [PubMed] [Google Scholar]
- 15.Anusavice KJ, Shen C, Vermost B, Chow B. Strengthening of porcelain by ion exchange subsequent to thermal tempering. Dent Mater. 1992;8:149–152. doi: 10.1016/0109-5641(92)90072-k. [DOI] [PubMed] [Google Scholar]
- 16.Anusavice KJ, Kakar K, Ferree N. Which mechanical and physical testing methods are relevant for predicting the clinical performance of ceramic-based dental prostheses? Clin Oral Implants Res. 2007;18:218–231. doi: 10.1111/j.1600-0501.2007.01460.x. [DOI] [PubMed] [Google Scholar]
- 17.Jefferies SR. Abrasive finishing and polishing in restorative dentistry: a state-of-the-art review. Dent Clin North Am. 2007;51:379–397. doi: 10.1016/j.cden.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 18.Antonson SA, Yazici AR, Kilinc E, Antonson DE, Hardigan PC. Comparison of different finishing/polishing systems on surface roughness and gloss of resin composites. J Dent. 2011;39:e9–17. doi: 10.1016/j.jdent.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 19.Tekçe N, Pala K, Tuncer S, Demirci M. The effect of surface sealant application and accelerated aging on posterior restorative surfaces: An SEM and AFM study. Dent Mater J. 2017;36:182–189. doi: 10.4012/dmj.2016-173. [DOI] [PubMed] [Google Scholar]
- 20.Flury S, Peutzfeldt A, Lussi A. Influence of surface roughness on mechanical properties of two computer-aided design/ computer-aided manufacturing (CAD/CAM) ceramic materials. Oper Dent. 2012;37:617–624. doi: 10.2341/11-391-L. [DOI] [PubMed] [Google Scholar]
- 21.Bottino MC, Valandro LF, Kantorski KZ, Bressiani JC, Bottino MA. Polishing methods of an alumina-reinforced feldspar ceramic. Braz Dent J. 2006;17:285–289. doi: 10.1590/s0103-64402006000400004. [DOI] [PubMed] [Google Scholar]
- 22.Perez Cdos R, Hirata RJ, da Silva AH, Sampaio EM, de Miranda MS. Effect of a glaze/composite sealant on the 3-D surface roughness of esthetic restorative materials. Oper Dent. 2009;34:674–680. doi: 10.2341/08-014-L. [DOI] [PubMed] [Google Scholar]
- 23.Al-Wahadni A. An in vitro investigation into the surface roughness of 2 glazed, unglazed, and refinished ceramic materials. Quintessence Int. 2006;37:311–317. [PubMed] [Google Scholar]
- 24.Cilli R, de Mattos MC, Honorio HM, Rios D, de Araujo PA, Prakki A. The role of surface sealants in the roughness of composites after a simulated toothbrushing test. J Dent. 2009;37:970–977. doi: 10.1016/j.jdent.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 25.Dede DÖ, Şahin O, Koroglu A, Yilmaz B. Effect of sealant agents on the color stability and surface roughness of nanohybrid composite resins. J Prosthet Dent. 2016;116:119–128. doi: 10.1016/j.prosdent.2015.11.024. [DOI] [PubMed] [Google Scholar]
- 26.Şahin O, Dede DÖ, Köroğlu A, Yılmaz B. Influence of surface sealant agents on the surface roughness and color stability of artificial teeth. J Prosthet Dent. 2015;114:130–137. doi: 10.1016/j.prosdent.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 27.Flury S, Diebold E, Peutzfeldt A, Lussi A. Effect of artificial toothbrushing and water storage on the surface roughness and micromechanical properties of tooth-colored CAD-CAM materials. J Prosthet Dent. 2017;117:767–774. doi: 10.1016/j.prosdent.2016.08.034. [DOI] [PubMed] [Google Scholar]
- 28.Tuncer S, Demirci M, Tiryaki M, Unlü N, Uysal Ö. The effect of a modeling resin and thermocycling on the surface hardness, roughness, and color of different resin composites. J Esthet Restor Dent. 2013;25:404–419. doi: 10.1111/jerd.12063. [DOI] [PubMed] [Google Scholar]
- 29.Hahnel S, Henrich A, Bürgers R, Handel G, Rosentritt M. Investigation of mechanical properties of modern dental composites after artificial aging for one year. Oper Dent. 2010;35:412–419. doi: 10.2341/09-337-L. [DOI] [PubMed] [Google Scholar]
- 30.Nguyen JF, Migonney V, Ruse ND, Sadoun M. Resin composite blocks via high-pressure high-temperature polymerization. Dent Mater. 2012;28:529–534. doi: 10.1016/j.dental.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 31.Sideridou I, Tserki V, Papanastasiou G. Effect of chemical structure on degree of conversion in light-cured dimethacrylate-based dental resins. Biomaterials. 2002;23:1819–1829. doi: 10.1016/s0142-9612(01)00308-8. [DOI] [PubMed] [Google Scholar]
- 32.Sideridou ID, Karabela MM. Sorption of water, ethanol or ethanol/water solutions by light-cured dental dimethacrylate resins. Dent Mater. 2011;27:1003–1010. doi: 10.1016/j.dental.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 33.Yoshihara K, Nagaoka N, Maruo Y, Nishigawa G, Irie M, Yoshida Y, Van Meerbeek B. Sandblasting may damage the surface of composite CAD-CAM blocks. Dent Mater. 2017;33:e124–e135. doi: 10.1016/j.dental.2016.12.003. [DOI] [PubMed] [Google Scholar]