Abstract
Introduction
Attracting graduates was recommended as a means of diversifying the UK medical student population. Graduates now make up nearly a quarter of the total medical student population. Research to date has focused on comparing the sociodemographic characteristics of applicants to and/or students on traditional and graduate entry programmes (GEMs), yet GEMs account for only 40% of the graduate medical student population. Thus, we aimed to compare the sociodemographic characteristic and outcomes of graduates and non-graduate applicants across a range of programmes.
Methods
This was an observational study of 117 214 applicants to medicine who took the UK Clinical Aptitude Test (UKCAT) from 2006 to 2014 and who applied to medical school through Universities and Colleges Admissions Service (UCAS). We included applicant demographics, UKCAT total score and offers in our analysis. Applicants were assigned as graduates or non-graduates on the basis of their highest qualification. Multiple logistic regression was used to predict the odds of receiving an offer, after adjusting for confounders.
Results
Irrespective of graduate or non-graduate status, most applicants were from the highest socioeconomic groups and were from a white ethnic background. Receiving an offer was related to gender and ethnicity in both graduates and non-graduates. After adjusting for UKCAT score, the OR of an offer for graduates versus non-graduates was approximately 0.5 (OR=0.48, 95% CI 0.46 to 0.49).
Discussion
Our findings indicate that the aim of diversifying the medical student population on socioeconomic grounds by attracting graduates has been only marginally successful. Graduate applicants from widening access backgrounds are less likely than others to be offered a place at medical school. Different approaches must be considered if medicine is to attract and select more socially diverse applicants.
Keywords: medical school admissions, graduates, ukcat, widening access, statistical analysis
Strengths and limitations of this study.
A large multicohort study to look at the population of graduate applicants to UK medical schools, including those on graduate entry programme and traditional programmes.
The study uses a contemporary dataset to examine the socioeconomic differences of those who apply to medical school; and it is important to know more about who applies, as medical schools can only select from the pool of applicants.
The study examines what sociodemographic factors are associated with receiving an offer to study medicine and whether these differ in graduates and non-graduates.
Measures of socioeconomic status are self-declared and there was a large proportion of missing socioeconomic data for the graduate subgroup.
Allocating students to an occupational group that depends on their family circumstances (area, parental occupation) can be problematic, especially for mature applicants.
Introduction
Despite much activity, investment and policy directives, people from backgrounds perceived as disadvantaged and minority, ethnic and cultural groups, remain under-represented or excluded from medicine worldwide on the basis of, for example, their social class or ethnic origin.1–5 In UK, the vast majority of medical students come from the highest socioeconomic groups,6–9 and more than 20% of medical students have attended independent (usually fee paying) schools, compared with an average of 7% of all school pupils.10 The professions have traditionally been dominated by those in high socioeconomic groups and this issue was summarised concisely in a report by the Independent Reviewer on Social Mobility and Child Poverty: ‘Medicine… has a long way to go when it comes to making access fairer, diversifying its workforce and raising social mobility’.10
In UK, most students enter medicine as school-leavers aged 17–20 years. In 1997, the UK Medical Workforce Standing Advisory Committee recommended that one way of diversifying the medical student population was to attract graduates into medical schools.11 The assumption behind this was that, by accepting students with more life experience, the diversity of students and hence doctors would be increased12–15 and this would result in more doctors willing to work in deprived and underserved areas.16–18 This recommendation led to the introduction (in 2000) of the first 4-year graduate entry medical courses (GEM) as well as a more general drive to encourage graduates into medicine.
Graduates now make up nearly a quarter of the contemporary UK medical student population.13 19 However, to date, there is relatively little information relating to whether, or not, attracting graduates has increased the diversity of medicine in the UK. Earlier studies tend to be single-site and/or focused on the relative performance of graduates versus school-leaver entrants.20–26 In an exception to this, Mathers and colleagues carried out a large-scale study of applicants to 31 UK medical schools between 2002 and 2006 in order to determine whether the newly introduced GEM programmes had widened access to medicine.6 They concluded that graduate entry programmes do attract more students from less affluent backgrounds than traditional 5-year programmes but overall GEMs had not led to significant changes to the socioeconomic profile of UK medical student population. It is possible, however, that this study was undertaken too soon after the establishment of the first GEM programmes to assess their true impact, given the typical time lag between policy implementation and impact on practice in education.27
Moreover, GEM programmes only account for about 10% of all medical programmes: there are more graduates in traditional 5-year programmes than in GEM programmes. Yet, to the best of our knowledge, no previous studies have looked directly at the whole population of graduate medical students—that is, those on both GEM and traditional programmes.
Finally, most studies have only looked at those graduates who were successful in obtaining a place at medical school.6 28 It is also important to know more about who applies, as medical schools can only select from the pool of applicants.8 In one of the few studies looking at both applicants and admissions, Garrud found some differences between both applicants and admissions to graduate-entry and traditional programmes, mostly in terms of ethnicity, but did not examine differences in terms of socioeconomic markers.29 This is, however, a complex area to investigate. There are issues surrounding these markers in graduate students, particularly given parental occupation is taken into account for school leavers, but occupation for graduates and older applicants may be that of the applicant themselves, particularly if they have been employed after leaving school or after a first degree. This ambiguity also holds for area of domicile (Index of Multiple Deprivation (IMD): measured by postcode) as again that may be of the parental home or the home of the applicant for mature students and graduates. However, to attempt to address these gaps in the literature, we used a contemporary dataset to compare the sociodemographic characteristics of graduates and non-graduate applicants to medicine. The main objective was to determine whether graduate and non-graduate applicants to medicine differ on a range of sociodemographic variables. Our second aim was to examine what sociodemographic factors are associated with receiving an offer to study medicine and whether these differ in graduates and non-graduates.
Methods
Study context
Data were obtained from the UKCAT database which comprises data from two sources: UCAS and UKCAT (http://www.ukcat.ac.uk/). UKCAT is the UK Clinical Aptitude Test for applicants to medical and dental schools. UCAS is the Universities and Colleges Admissions Service, a UK-based organisation whose primary role is to operate the application process for British universities. Through the UCAS system (https://www.ucas.com/), candidates can apply to up to four medical courses out of five options in any one cycle, but there is no preference order of course choice. We compiled data for all candidates who sat the UKCAT between 2006 and 2014 and who applied to medical school through UCAS.
The UKCAT database only holds UCAS data relating to UKCAT candidates who have applied to a UKCAT University. Therefore, the data is a subset of graduate applicants to UK Universities. A number of graduate entry programmes use other admission tests (both BioMedical Admissions Test (BMAT) and Graduate Australian Medical School Admissions Test (GAMSAT)). Of the 16 graduate entry programmes in the UK, seven require the UKCAT, four require GAMSAT and 1 programme requires a BMAT.30 The other four graduate entry programmes do not use any of these admission tests. Where UKCAT candidates have applied to non-UKCAT Universities, these choices and the outcome of these choices are not known.
Although individuals can have multiple applications, within and between years, the sociodemographic variables presented in this study are per unique applicant. These variables include gender, ethnicity, secondary school attended, domicile (UK, International, EU). The socioeconomic status (SES) of the candidates was determined by parental National Statistics Socio-Economic Classification (NS-SEC) and IMD, an area-based measurement of material deprivation.
Design and procedures
Access to the data was via a safe haven31 (to ensure adherence to the highest standards of security, governance and confidentiality when storing, handling and analysing identifiable data). Ethical approval was not required because the focus of this study was a secondary analysis of anonymised data. Applicants who took the UKCAT were notified that their data would be used for research purposes. Data files were merged into a single SPSS file for cleaning and analysis. The online supplementary file 1 illustrates a flow diagram showing how the data files were merged from different source documents.
bmjopen-2017-018946supp001.pdf (831.5KB, pdf)
The applications were assigned into two categories, graduate or non-graduate, at the time of application. This was primarily based on applicants’ highest qualification but some amendments were necessary. For example, where this information was missing, we imputed the outcome variable based on applicants’ age and programme applied. For instance, all applicants aged less than 20 on their final UKCAT attempt were assumed to have applied shortly after leaving school; these were classified as school-leavers or non-graduate applicants. Similarly, applicants with missing information on academic qualification, aged over 21 and had applied for a graduate entry programme were classified as ‘graduates’. The outcome measures were the UKCAT score and whether the applicant received an offer or not. We also considered all conditional and unconditional offers as an ‘offer’.
Statistical analysis
All the data were analysed using SPSS (IBM SPSS Statistics for Windows V.22.0, Armonk, New York, USA). The results are reported in terms of numbers, percentages and mean (SD) or median (IQR) as appropriate. The UKCAT scores were normally distributed. Therefore we used independent-samples t-test to compare the means between two groups. One-way analysis of variance was used to compare means between more than two independent groups. A binary logistic regression analysis was employed to predict the odds of getting an offer from an application based on an applicant’s graduate status. The specific factors we adjusted for in the regression models were: socioeconomic status (NS-SEC and IMD), gender, graduate status, ethnicity and the total UKCAT score. The purpose was to assess the odds of receiving an offer for a graduate relative to a non-graduate after accounting for any differences in total UKCAT score. The analysis considered only the final application of each applicant to ensure independence (ie, to control for those who made repeated applications).
Results
From 2006 to 2014, the UKCAT database comprises 117 214 applicants to medicine, applying through UCAS on a total of 146 146 occasions (ie, some applied in more than one cycle and hence sat the UKCAT more than once). The time-trend analysis shows that the proportion of graduate applicants to UK medical schools has risen from 8.5% in 2006 to 26.9% in 2013 (see online supplementary file 2, time-trend analysis). While dramatic, this increase is at least in part due to the increase in the number of institutions joining the UKCAT consortium and thus more data supply. 23.6% of the applicants were graduates and 76.4% non-graduates. In general, there were more female graduate applicants than male applicants. The median age for the non-graduate applicants was 18 years and it was 23 years for the graduate applicants.
bmjopen-2017-018946supp002.pdf (335.7KB, pdf)
Table 1 summarises a comparison of graduate and non-graduate applicants by different sociodemographic factors. The main pattern across the two groups was that most applicants were from the highest socioeconomic group, with nearly 80% of all applicants having a parent/guardian in the managerial and professional occupations. The groups were also similar in that one-fifth of the graduate and non-graduate applicants had attended a fee-paying (independent) school. (However, note that type of school was only available for one-third of graduates and so this was not included in the later multivariable regression analysis with other covariates due to concern about bias and a lack of representativeness among graduates.) The sample was predominantly of candidates from white ethnic backgrounds, for both graduates (64.3%; n=14 014) and non-graduates (61.9%; n=47 103). Around 7.7% of the graduates were classified as international applicants, as compared with 12.1% of the non-graduate applicants. The number of EU applicants was similar for both graduates (6.0%) and non-graduates (7.6%).
Table 1.
Frequency distribution of applicants (and offers) to UKCAT consortium medical schools between 2006 and 2014
| Non-graduate | Graduate | |||||||
| Application | Offer | Application | Offer | |||||
| n | % | n | % | n | % | n | % | |
| Gender | ||||||||
| Female | 49 082 | 55.9 | 22 716 | 56.2 | 13 999 | 57.7 | 3812 | 56.7 |
| Male | 38 656 | 44.1 | 17 702 | 43.8 | 10 256 | 42.3 | 2910 | 43.3 |
| Total | 87 738 | 40 418 | 24 255 | 6722 | ||||
| Ethnicity II | ||||||||
| Caucasian | 47 103 | 61.9 | 25 421 | 69.8 | 14 014 | 64.3 | 4831 | 78.3 |
| Non-caucasian | 28 941 | 38.1 | 10 995 | 30.2 | 7765 | 35.6 | 1335 | 21.7 |
| Total | 76 044 | 36 416 | 21 779 | 6166 | ||||
| Missing | (11694) | (13.3) | (2476) | (10.2) | ||||
| School attended* | ||||||||
| Fee paying | 17 388 | 25.5 | 10 184 | 29.2 | 1672 | 21.1 | 664 | 24.5 |
| Non-fee paying | 50 796 | 74.5 | 24 705 | 70.8 | 6249 | 78.9 | 2043 | 75.5 |
| Total | 68 184 | 34 889 | 7921 | 2707 | ||||
| Missing | (2263) | (3.2) | (12988) | (62.1) | ||||
| IMD quintile* | ||||||||
| 1 | 28 518 | 34.6 | 14 043 | 40 | 5972 | 26.2 | 1894 | 32 |
| 2 | 19 202 | 23.3 | 8767 | 25 | 4693 | 20.6 | 1375 | 23.2 |
| 3 | 14 986 | 18.2 | 6196 | 17.6 | 4450 | 19.6 | 1134 | 19.2 |
| 4 | 10 883 | 13.2 | 3734 | 10.6 | 4261 | 18.7 | 959 | 16.2 |
| 5 | 8815 | 10.7 | 2394 | 6.8 | 3378 | 14.8 | 552 | 9.3 |
| Total | 82 404 | 35 134 | 22 754 | 5914 | ||||
| Missing | (1260) | (1.5) | (592) | (2.5) | ||||
| NS-SEC* | ||||||||
| Managerial and professional occupations | 61 624 | 84.1 | 28 025 | 87.9 | 15 622 | 78.7 | 4406 | 83.3 |
| Intermediate occupations | 3399 | 4.6 | 1337 | 4.2 | 1167 | 5.9 | 295 | 5.6 |
| Small employers and own account occupations | 4676 | 6.4 | 1501 | 4.7 | 1572 | 7.9 | 313 | 5.9 |
| Lower supervisory and technical occupations | 1410 | 1.9 | 423 | 1.3 | 639 | 3.2 | 129 | 2.4 |
| Routine and semiroutine occupations | 2198 | 3 | 580 | 1.8 | 848 | 4.3 | 149 | 2.8 |
| Total | 73 307 | 31 866 | 19 848 | 5292 | ||||
| Missing | (10357) | (12.4) | (3498) | (15) | ||||
| Domicile | ||||||||
| UK | 70 447 | 80.3 | 35 333 | 88 | 20 909 | 86.2 | 6051 | 90 |
| EU | 6694 | 7.6 | 1078 | 2.7 | 1467 | 6 | 280 | 4.2 |
| International | 10 597 | 12.1 | 3785 | 9.4 | 1879 | 7.7 | 391 | 5.8 |
| Total | 87 738 | 40 418 | 24 255 | 6722 | ||||
| UKCAT attempt number | ||||||||
| 1 | 75 049 | 85.5 | 34 770 | 86 | 15 562 | 64.2 | 4718 | 70.2 |
| 2 | 11 803 | 13.5 | 5390 | 13.3 | 5722 | 23.6 | 1425 | 21.2 |
| 3+ | 886 | 1 | 258 | 0.6 | 2971 | 12.2 | 579 | 8.6 |
| Total | 87 738 | 40 418 | 24 255 | 6722 | ||||
| Final outcome | ||||||||
| No offer | 43 964 | 52.1 | 14 736 | 68.7 | ||||
| Offer | 40 418 | 47.9 | 40 418 | 6722 | 27.7 | 6722 | ||
| Total | 84 382 | 21 458 | ||||||
| Missing | (3356) | (3.8) | (2797) | (11.5) | ||||
*Sample drawn from UK domiciled applicants only.
IMD, Index of Multiple Deprivation; NS-SEC, National Statistics Socio-Economic Classification; UKCAT, UK Clinical Aptitude Test.
Non-graduate applicants performed significantly better on the UKCAT (2535.4 points, SD=268.2) than graduate applicants (2498.5 points, SD=285.7), P<0.001. Graduates and non-graduate applicants from the top 20% affluent neighbourhoods (IMD ‘I’) obtained better UKCAT scores than applicants from the 20% most deprived areas (IMD ‘V’). The difference was approximately 200 points for graduate applicants and the same margin was observed in the non-graduate group. A similar pattern was also observed with parental occupation classification (NS-SEC) categories with the difference of over 100 UKCAT points between managerial and professional occupations and routine/semiroutine occupations.
The proportion of applicants who received offers was substantially lower for graduates (27.7%) than it was for non-graduates (47.9%). Graduate applicants who received offers had significantly better mean UKCAT scores (2697.7 points, SD=244.39) compared with their non-graduate colleagues who received offers (2657.7 points, SD=235.3), P<0.001. The preadmission attainment information (UKCAT scores) is summarised in table 2.
Table 2.
Mean UKCAT scores*
| Non-graduate | Graduate | |||||||
| N | Mean | SD | P value | N | Mean | SD | P value | |
| Gender | ||||||||
| Female | 49 047 | 2532.2 | 269.8 | <0.001 | 13 974 | 2501.7 | 285.71 | <0.001 |
| Male | 38 633 | 2581.8 | 267.7 | 10 241 | 2550.9 | 291.22 | ||
| Ethnicity | ||||||||
| Caucasian | 47 102 | 2597.9 | 243.6 | <0.001 | 14 000 | 2591.2 | 261.15 | |
| Non-Caucasian | 26 298 | 2512.1 | 282.0 | 7128 | 2402.3 | 294.32 | ||
| School attended† | ||||||||
| Fee paying | 17 388 | 2632.5 | 239.2 | <0.001 | 1670 | 2611.6 | 233.21 | <0.001 |
| Non-fee paying | 50 787 | 2562.8 | 260.0 | 6233 | 2527.2 | 265.93 | ||
| IMD quintile† | ||||||||
| I | 24 427 | 2627.9 | 237.8 | <0.001 | 5395 | 2600.4 | 263.94 | <0.001 |
| II | 16 291 | 2604.6 | 244.6 | 4206 | 2578.1 | 269.33 | ||
| III | 12 505 | 2576.7 | 253.6 | 3937 | 2531.5 | 273.30 | ||
| IV | 8936 | 2516.6 | 269.3 | 3801 | 2479.3 | 298.79 | ||
| V | 7194 | 2425.9 | 282.8 | 2990 | 2397.5 | 312.92 | ||
| NS-SEC† | ||||||||
| Managerial and professional occupations | 52 555 | 2604.1 | 249.0 | <0.001 | 14 084 | 2560.6 | 281.44 | <0.001 |
| Intermediate occupations | 2784 | 2568.7 | 246.3 | 1059 | 2541.3 | 272.21 | ||
| Small employers and own account occupations | 3635 | 2518.8 | 256.5 | 1367 | 2466.0 | 279.27 | ||
| Lower supervisory and technical occupations | 1181 | 2486.6 | 259.5 | 551 | 2448.9 | 296.20 | ||
| Routine and semiroutine occupations | 1775 | 2465.0 | 270.2 | 740 | 2441.2 | 276.38 | ||
| Number of attempts | ||||||||
| 1 | 75 000 | 2541.7 | 272.9 | <0.001 | 15 554 | 2507.5 | 299.42 | <0.001 |
| 2 | 11 798 | 2628.4 | 237.9 | 5711 | 2552.7 | 273.84 | ||
| 3 or more | 882 | 2604.4 | 256.0 | 2950 | 2543.5 | 254.43 | ||
| Final outcome | ||||||||
| No offer | 43 925 | 2455.6 | 265.2 | <0.001 | 14 713 | 2443.9 | 278.01 | <0.001 |
| Offer | 40 405 | 2657.7 | 235.3 | 6711 | 2697.7 | 244.39 | ||
*The numbers presented here are the mean scores based on the applicants’ last UKCAT sitting. However, the counts of applicants are not the same as in table 1 because some applicants had missing UKCAT scores.
†Sample drawn from UK domiciled applicants only.
IMD, Index of Multiple Deprivation; NS-SEC, National Statistics Socio-Economic Classification; UKCAT, UK Clinical Aptitude Test.
A binary logistic regression analysis was employed to predict the odds of getting an offer based on the applicant’s highest qualification (graduate or not) and total UKCAT score. After adjusting for UKCAT score alone, the OR of an offer for graduates versus non-graduates was approximately 0.5 (OR=0.48, 95% CI 0.46 to 0.49).
Several variables that were considered to be representative of widening participation backgrounds were included in univariate analyses. The multiple logistic regression analysis was repeated including, in addition to UKCAT and graduate status, only those variables that were statistically significant (P≤0.05) when associated with offer status. The specific factors were gender, ethnicity and socioeconomic class (IMD and NS-SEC). We also tested for interaction of these factors which enabled us to ask whether graduates from different socioeconomic backgrounds were more or less likely to receive offers. The overall model performance, using Nagelkerke’s R2 ranged from 0.20 to 0.23 across the models developed. Results of the two-way interaction terms (table 3) showed that after adjusting for other factors, the additional effect of socioeconomic disadvantage for graduates (compared with non-graduates) was small and did not reach statistical significance (P=0.69 for the interaction of graduate status and IMD; P=0.22 for the interaction of graduate status and parental occupation (NS-SEC)). The result suggests that the association between socioeconomic disadvantage and the likelihood of getting an offer for medical school affected graduates and non-graduates in a similar way.
Table 3.
Multiple logistic regression for offers to medical school 2007–2014
| Model 1, R2=0.22 | Model 2, R2=0.21 | Model 3, R2=0.22 | Model 4, R2=0.22 | |||||||||
| OR | Lower | Upper | OR | Lower | Upper | OR | Lower | Upper | OR | Lower | Upper | |
| UKCAT | 1.032 | 1.032 | 1.033 | 1.032 | 1.032 | 1.033 | 1.032 | 1.032 | 1.033 | 1.032 | 1.032 | 1.033 |
| Graduate status | ||||||||||||
| Non-graduate (default) | 1 | 1 | 1 | 1 | ||||||||
| Graduate | 0.429 | 0.399 | 0.461 | 0.438 | 0.419 | 0.458 | 0.441 | 0.421 | 0.463 | 0.450 | 0.432 | 0.468 |
| Gender | ||||||||||||
| Female (default) | 1 | 1 | 1 | |||||||||
| Male | 0.830 | 0.803 | 0.857 | 0.830 | 0.803 | 0.857 | 0.830 | 0.804 | 0.857 | 0.830 | 0.804 | 0.857 |
| Ethnicity | ||||||||||||
| White (default) | 1 | 1 | 1 | 1 | ||||||||
| Asian | 0.781 | 0.750 | 0.813 | 0.780 | 0.748 | 0.812 | 0.774 | 0.741 | 0.809 | 0.780 | 0.748 | 0.812 |
| Black | 0.574 | 0.527 | 0.625 | 0.572 | 0.525 | 0.623 | 0.544 | 0.495 | 0.598 | 0.572 | 0.525 | 0.623 |
| Mixed | 0.823 | 0.756 | 0.896 | 0.823 | 0.756 | 0.896 | 0.808 | 0.736 | 0.888 | 0.823 | 0.756 | 0.896 |
| Other | 0.804 | 0.718 | 0.900 | 0.803 | 0.717 | 0.899 | 0.818 | 0.722 | 0.927 | 0.803 | 0.717 | 0.900 |
| IMD | ||||||||||||
| I—Most affluent (default) | 1 | 1 | 1 | 1 | ||||||||
| II | 0.917 | 0.876 | 0.960 | 0.921 | 0.884 | 0.960 | 0.921 | 0.884 | 0.960 | 0.921 | 0.884 | 0.960 |
| III | 0.866 | 0.823 | 0.911 | 0.869 | 0.830 | 0.909 | 0.869 | 0.830 | 0.909 | 0.868 | 0.830 | 0.909 |
| IV | 0.775 | 0.731 | 0.823 | 0.808 | 0.766 | 0.852 | 0.806 | 0.765 | 0.850 | 0.806 | 0.764 | 0.850 |
| V—Least affluent | 0.707 | 0.657 | 0.760 | 0.724 | 0.679 | 0.773 | 0.723 | 0.678 | 0.771 | 0.723 | 0.677 | 0.771 |
| Parental occupation NS-SEC | ||||||||||||
| I—Managerial and professional occupations (default) | 1 | 1 | 1 | |||||||||
| II—Intermediate occupations | 0.891 | 0.828 | 0.960 | 0.879 | 0.808 | 0.956 | 0.891 | 0.828 | 0.960 | 0.891 | 0.827 | 0.960 |
| III—Small employers and own account occupations | 0.854 | 0.797 | 0.914 | 0.829 | 0.768 | 0.894 | 0.852 | 0.796 | 0.912 | 0.853 | 0.796 | 0.913 |
| IV—Lower supervisory and technical occupations | 0.768 | 0.684 | 0.862 | 0.709 | 0.621 | 0.809 | 0.766 | 0.683 | 0.860 | 0.767 | 0.683 | 0.860 |
| V—Routine and semiroutine occupations | 0.766 | 0.693 | 0.847 | 0.732 | 0.654 | 0.820 | 0.765 | 0.692 | 0.845 | 0.764 | 0.691 | 0.844 |
| Graduate status by IMD, P = 0.69 | ||||||||||||
| Graduate by IMD I—most affluent neighbourhood (default) | 1 | |||||||||||
| Graduate vs IMD_II | 1.030 | 0.922 | 1.150 | |||||||||
| Graduate vs IMD_III | 1.021 | 0.909 | 1.147 | |||||||||
| Graduate vs IMD_IV | 1.189 | 1.049 | 1.348 | |||||||||
| Graduate vs IMD_V—least affluent neighbourhood | 1.112 | .957 | 1.293 | |||||||||
| Graduate status by parental occupation (NS-SEC), P = 0.22 | ||||||||||||
| Graduate by NS-SEC-I (default) | 1 | |||||||||||
| Graduate by NS-SEC-II | 1.068 | 0.893 | 1.276 | |||||||||
| Graduate by NS-SEC-III | 1.149 | 0.974 | 1.355 | |||||||||
| Graduate by NS-SEC-IV | 1.383 | 1.064 | 1.797 | |||||||||
| Graduate by NS-SEC-V | 1.211 | 0.959 | 1.530 | |||||||||
| Graduate status by ethnicity, P = 0.10 | ||||||||||||
| Graduate by white (default) | 1 | |||||||||||
| Graduate by Asian | 1.039 | 0.931 | 1.160 | |||||||||
| Graduate by black | 1.300 | 1.060 | 1.593 | |||||||||
| Graduate by mixed | 1.101 | 0.885 | 1.371 | |||||||||
| Graduate by other ethnic group | 0.900 | 0.668 | 1.211 | |||||||||
Model 1: shows the interaction of graduate status by area deprivation (IMD), note non-significant value of P=0.69.
Model 2: shows the interaction of graduate status by parental occupation (NS-SEC), note non-significant value of P=0.22.
Model 3: shows the interaction of graduate status by ethnicity, note the non-significant value of P=0.10.
Model 4: is the final model of all covariates, note all values are statistically significant, P<0.001.
IMD, Index of Multiple Deprivation; NS-SEC, National Statistics Socio-Economic Classification; UKCAT, UK Clinical Aptitude Test.
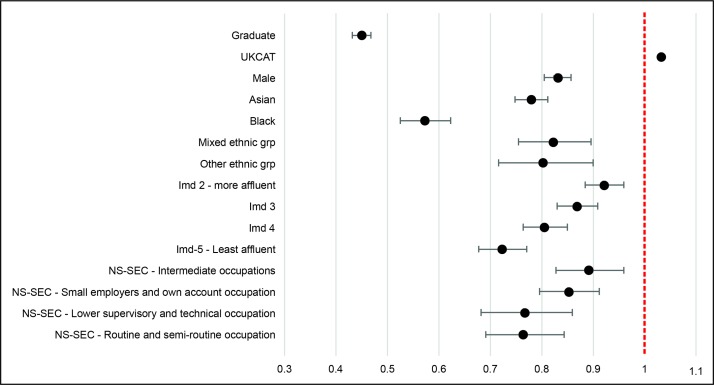
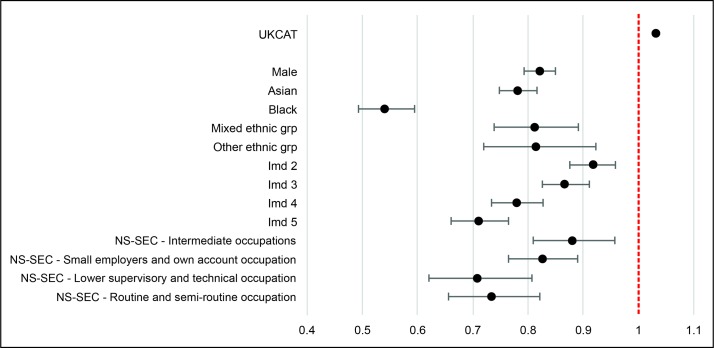
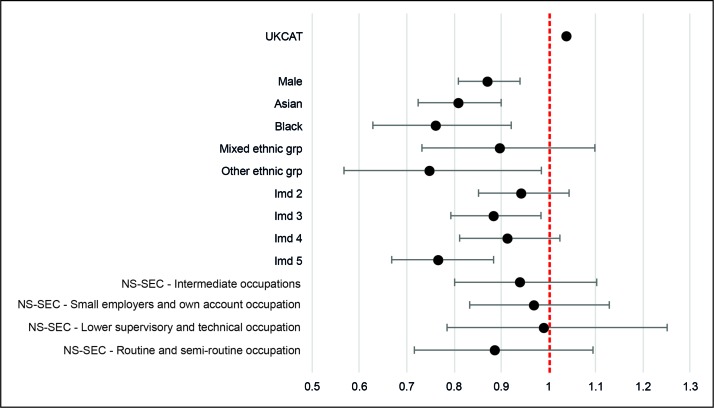
Figure 1 gives a graphical summary of the results from final model. In general, the odds of getting an offer to study medicine were lower if the applicant was male, graduate, from black and minority ethnic background and from lower socioeconomic groups (NS-SEC II-V and IMD ‘V’ – least affluent neighbourhood). Figures 2 and 3 give a graphical summary of the OR after separating graduates and non-graduates, to help further illustrate the difference between the two groups. For the non-graduates, the pattern is almost the same as the combined model in that the odds of getting an offer were higher if the applicant was female, from white ethnic background and from high socioeconomic groups (NS-SEC1 and IMD I—most affluent neighbourhood). Some explanation for this pattern is because the non-graduates were in such a high proportion of the whole group. In comparison, for graduates, the predictor values that stand out are gender and ethnicity. However, notably, nearly a quarter of graduate applicants had a missing combination of socioeconomic profile data (NS-SEC and IMD) which may explain why SES measures were less important predictors for graduates.
Figure 1.
Odds of an application resulting in offer of a place according to selected sociodemographic characteristics: OR, final model (all applicants).
Figure 2.
Odds of an application resulting in offer of a place according to selected sociodemographic characteristics: OR, non-graduate applicants.
Figure 3.
Odds of an application resulting in offer of a place according to selected sociodemographic characteristics: OR, graduate applicants.
Discussion
In this analysis of a large, multicohort contemporary dataset, we examined differences between graduates and non-graduate applicants to UK medical schools. Unlike previous studies in this area, we compared a larger sample of graduate applicants with non-graduates, rather than comparing by course (traditional vs GEM). This allowed us to capture the characteristics of a broader group of graduate applicants compared with earlier studies. Our results show that graduate and non-graduate applicants to UK medical schools are very similar on a range of sociodemographic markers, including multiple markers of SES. This indicates that, even with time and much investment in GEM courses, the aim of diversifying the medical student population on socioeconomic grounds by attracting graduates has not been successful.6
Interestingly, unlike previous studies,29 we did not identify any differences across graduates and non-graduates in terms of ethnicity. This may represent a change in the medical student population overall or may be an artefact of study design given that we looked at graduates in all medical programmes, not just GEM programmes.
We also looked at who received an offer. Put simple, non-graduates were twice as likely to receive an offer as graduates. The patterns across non-graduates and graduates were similar in terms of gender and ethnicity but, in non-graduates, offers to study medicine were higher if the applicant was from a higher socioeconomic group. However, measures of SES are self-declared and there was a large proportion of missing socioeconomic data for the graduate subgroup. This reflects patterns seen in other similar studies.32–36 Given the high proportion of missing data, it would be misleading to conclude that IMD and NS-SEC are weaker predictors for assessing the likelihood of getting an offer among graduate applicants because many graduate applicants were excluded from the logistic regression analysis and the missing data could also have led to insufficient power to detect smaller effects. Moreover, allocating students to an occupational group that depends on their family circumstances (area, parental occupation) can be problematic, especially for mature students.37 38 However, we had no other measures available to us: no matter how limited,32 34 those used are the ‘basic units’ that indicate educational disadvantage in UK. We urge organisations such as UCAS and UKCAT to explore ways of improving self-declared data reporting and government bodies such as the UK’s Office for National Statistics to explore more effective measures of SES.
Overall, we found that graduates were proportionally less likely to receive an offer than non-graduate applicants and those graduates who were offered places had significantly higher UKCAT scores than their non-graduate equivalents. We know from earlier studies29 and contemporary routine data that the average competition, or selection, ratios for GEM programmes are significantly higher than for traditional 5-year programmes. Moreover, GEM selection processes also tend to place more weight on UKCAT performance than do traditional programmes typically (this is associated with school leaving examinations being potentially less discriminatory for graduates—who would have taken these exams in earlier years, when it was less common to achieve top grades39). These factors may explain this outcome. However, future research which compares selection ratios for non-graduates and graduates by programme would provide a more nuanced understanding of differences across groups. Additionally, future studies could also look more closely at graduate and non-graduate patterns of performance in the various stages of medical school selection for the high number of graduates applying to traditional programmes. For example, we do not know whether graduates and non-graduates with equivalent grades and UKCAT scores are invited to interview, then graduates ‘fall down’ at that stage. These studies would address concerns in the wider education literature that graduates and non-graduates are judged differently.40
The present study has various limitations that must be taken into consideration when interpreting findings. It was not possible to compare prior attainment across graduate and non-graduate groups with any confidence in this study because of the different weightings given to school and degree qualifications. However, this is a tricky comparison at the best of times (see above—graduates by their very nature have taken the school leaving examinations which are typically used in medical selection to indicate prior attainment some years previous to their non-graduate counterparts). The issue of comparing ‘apples and oranges’ arises as over recent years the average A level score has progressively risen (‘grade inflation’).39 41 42
In conclusion, the aim of diversifying the medical student population on socioeconomic grounds by attracting graduates has been only marginally successful, with very minor positive trends in all areas. It may be that to draw a more diverse group of graduates into medicine requires different selection criteria for this group, one that places appreciable weight on the degree qualification and other graduate attributes, such as experience and passion for medicine. However, to change the selection process of graduates or indeed any group requires a shift towards affirmative action and/or a commitment to increase diversity. There appears to be little appetite for the former in the UK even though there is some evidence from other contexts that students from minority populations enrich the teaching environment of a medical school and may be more likely to practice in underserved areas.43–45
Supplementary Material
Acknowledgments
We thank UKCAT for releasing the data for this project via a competitive bid process. We are also grateful to Dr Sally Curtis (University of Southampton) for the general advice throughout the project.
Footnotes
Contributors: RKMcK led the funding bid which was cowritten by JC and GP and reviewed by RG. RG advised on the nature of the data. BK managed the data and planned and carried out the data analysis under the supervision of GP. JC guided the first draft of the introduction and discussion sections of this paper. BK and GP wrote the first drafts of the methods and results sections. JC edited the drafts. All authors reviewed and agreed the final draft of the paper.
Funding: This study is part of Ben Kumwenda’s doctoral programme of research funded by the UKCAT Research Panel, of which JC is a member and RG the Administrator.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available as the datasets are held in safe haven.
References
- 1.Castillo-Page L. Diversity in medical education: facts & figures. Washington DC: Association of American Medical Colleges, 2012. [Google Scholar]
- 2.Milburn A. University challenge: how higher education can advance social mobility. London: Cabinet Office, 2012. [Google Scholar]
- 3.Cleland J, Dowell J, McLachlan J, et al. Identifying best practice in the selection of medical students. Aberdeen: University of Aberdeen, 2012. A project commissioned by the General Medical Council. [Google Scholar]
- 4.Larkins S, Michielsen K, Iputo J, et al. Impact of selection strategies on representation of underserved populations and intention to practise: international findings. Med Educ 2015;49:60–72. 10.1111/medu.12518 [DOI] [PubMed] [Google Scholar]
- 5.Behrendt L, Larkin S, Griew R, et al. Review of higher education access and outcomes for aboriginal and Torres Strait Islander people final report. Canberra, Australia: Australian Government Department of Education and Training, 2012. [Google Scholar]
- 6.Mathers J, Sitch A, Marsh JL, et al. Widening access to medical education for under-represented socioeconomic groups: population based cross sectional analysis of UK data, 2002-6. BMJ 2011;342:d918 10.1136/bmj.d918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Griffin B, Hu W. The interaction of socio-economic status and gender in widening participation in medicine. Med Educ 2015;49:103–13. 10.1111/medu.12480 [DOI] [PubMed] [Google Scholar]
- 8.Steven K, Dowell J, Jackson C, et al. Fair access to medicine? Retrospective analysis of UK medical schools application data 2009-2012 using three measures of socioeconomic status. BMC Med Educ 2016;16:10 10.1186/s12909-016-0536-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nicholson S, Cleland JA. “It’s making contacts”: notions of social capital and implications for widening access to medical education. Adv Health Sci Educ Theory Pract 2017;22:477–90. 10.1007/s10459-016-9735-0 [DOI] [PubMed] [Google Scholar]
- 10.Independent Reviewer on Social Mobility and Child Poverty. Fair access to professional careers. London: Cabinet Office, 2012. [Google Scholar]
- 11.Medical Workforce Standing Advisory committee. 1997. Planning tHe medical workforce. Third report. London: Department of Health. [Google Scholar]
- 12.Wilkinson TJ, Wells JE, Bushnell JA. Are differences between graduates and undergraduates in a medical course due to age or prior degree? Med Educ 2004;38:1141–6. 10.1111/j.1365-2929.2004.01981.x [DOI] [PubMed] [Google Scholar]
- 13.Peile E. Should all medical students be graduates first? Yes. BMJ 2007;335:1072–3. 10.1136/bmj.39283.476725.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carter YH, Peile E. Graduate entry medicine: high aspirations at birth. Clin Med 2007;7:143–7. 10.7861/clinmedicine.7-2-143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.British Medical Association. Equality and diversification in UK medical schools. London: British Medical Association, 2009. [Google Scholar]
- 16.Dowell J, Norbury M, Steven K, et al. Widening access to medicine may improve general practitioner recruitment in deprived and rural communities: survey of GP origins and current place of work. BMC Med Educ 2015;15:165 10.1186/s12909-015-0445-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Puddey IB, Playford DE, Mercer A. Impact of medical student origins on the likelihood of ultimately practicing in areas of low vs high socio-economic status. BMC Med Educ 2017;17:13 10.1186/s12909-016-0842-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taskforce GP. Securing the future of GP workforce. Delivering the mandate on GP expansion. GP taskforce final report. 2014.
- 19.Cleland J, Johnston PW, French FH, et al. Associations between medical school and career preferences in Year 1 medical students in Scotland. Med Educ 2012;46:473–84. 10.1111/j.1365-2923.2012.04218.x [DOI] [PubMed] [Google Scholar]
- 20.Niven V, Cabot LB, Gallagher JE. Widening participation - a comparison of the characteristics of successful UK applicants to the five-year and four-year dental programmes in 2007 and 2008. Br Dent J 2013;214:117–22. 10.1038/sj.bdj.2013.107 [DOI] [PubMed] [Google Scholar]
- 21.James D, Ferguson E, Powis D, et al. Graduate entry to medicine: widening psychological diversity. BMC Med Educ 2009;9:8 10.1186/1472-6920-9-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elliott SL, Epstein J. Selecting the future doctors: the role of graduate medical programmes. Intern Med J 2005;35:174–7. 10.1111/j.1445-5994.2004.00796.x [DOI] [PubMed] [Google Scholar]
- 23.Dodds AE, Reid KJ, Conn JJ, et al. Comparing the academic performance of graduate- and undergraduate-entry medical students. Med Educ 2010;44:197–204. 10.1111/j.1365-2923.2009.03559.x [DOI] [PubMed] [Google Scholar]
- 24.Byrne AT, Arnett R, Farrell T, et al. Comparison of performance in a four year graduate entry medical programme and a traditional five/six year programme. BMC Med Educ 2014;14:14 10.1186/s12909-014-0248-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Casey D, Thomas S, Hocking DR, et al. Graduate-entry medical students: older and wiser but not less distressed. Australas Psychiatry 2016;24:88–92. 10.1177/1039856215612991 [DOI] [PubMed] [Google Scholar]
- 26.Calvert MJ, Ross NM, Freemantle N, et al. Examination performance of graduate entry medical students compared with mainstream students. J R Soc Med 2009;102:425–30. 10.1258/jrsm.2009.090121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Les B, Howard S. Education policy: process, themes and impact. New York: Routledge, 2006. [Google Scholar]
- 28.Rolfe IE, Ringland C, Pearson SA. Graduate entry to medical school? Testing some assumptions. Med Educ 2004;38:778–86. 10.1111/j.1365-2929.2004.01891.x [DOI] [PubMed] [Google Scholar]
- 29.Garrud P. Who applies and who gets admitted to UK graduate entry medicine? - an analysis of UK admission statistics. BMC Med Educ 2011;11:4 10.1186/1472-6920-11-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Medschoolsonline. http://www.medschoolsonline.co.uk/graduate-entry-programme/ (accessed May 2017).
- 31.HIC Safe Haven. Health Informatics Centre. 2016. http://medicine.dundee.ac.uk/hic-safe-haven-0.
- 32.Do PC, Parry J, Mathers J, et al. Monitoring the widening participation initiative for access to medical school: are present measures sufficient? Med Educ 2006;40:750–8. 10.1111/j.1365-2929.2006.02535.x [DOI] [PubMed] [Google Scholar]
- 33.Hoare A, Johnston R. Widening participation through admissions policy – a British case study of school and university performance. Studies in Higher Education 2011;36:21–41. 10.1080/03075070903414297 [DOI] [Google Scholar]
- 34.Boliver V, Gorard S, Siddiqui N. Will the use of contextual indicators make UK higher education admissions fairer? Educ Sci 2015;5:306–22. 10.3390/educsci5040306 [DOI] [Google Scholar]
- 35.MacKenzie RK, Dowell J, Ayansina D, et al. Do personality traits assessed on medical school admission predict exit performance? A UK-wide longitudinal cohort study. Adv Health Sci Educ Theory Pract 2017;22:1–21. 10.1007/s10459-016-9715-4 [DOI] [PubMed] [Google Scholar]
- 36.James D, Ferguson E, Powis D, et al. Graduate entry to medicine: widening academic and socio-demographic access. Med Educ 2008;42:294–300. 10.1111/j.1365-2923.2008.03006.x [DOI] [PubMed] [Google Scholar]
- 37.Gorard S, Adnett N, May H, et al. Overcoming the barriers to higher education. Stoke-on-Trent: Trentham Books, 2007. [Google Scholar]
- 38.Harrison N, Hatt S. Knowing the ‘unknowns’: investigating the students whose social class is not known at entry to higher education. JFHE 2009;33:347–57. 10.1080/03098770903266042 [DOI] [Google Scholar]
- 39.McManus IC, et al. Intellectual aptitude tests and A levels for selecting UK school leaver entrants for medical school. BMJ 2005;331:555–9. 10.1136/bmj.331.7516.555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Blackstone T. Does maturity make a difference? Policy studies institute, 1997:38–45. [Google Scholar]
- 41.James D, Yates J, Nicholson S. Comparison of A level and UKCAT performance in students applying to UK medical and dental schools in 2006: cohort study. BMJ 2010;340:c478 10.1136/bmj.c478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Johnes G. Standards and grade inflation International handbook on the economics of education. Cheltenham: Edward Elgar Publishing Ltd, 2004. [Google Scholar]
- 43.Xu G, Fields SK, Laine C, et al. The relationship between the race/ethnicity of generalist physicians and their care for underserved populations. Am J Public Health 1997;87:817–22. 10.2105/AJPH.87.5.817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Whitla DK, Orfield G, Silen W, et al. Educational benefits of diversity in medical school: a survey of students. Acad Med 2003;78:460–6. [DOI] [PubMed] [Google Scholar]
- 45.Saha S, Guiton G, Wimmers PF, et al. Student body racial and ethnic composition and diversity-related outcomes in US medical schools. JAMA 2008;300:1135–45. 10.1001/jama.300.10.1135 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-018946supp001.pdf (831.5KB, pdf)
bmjopen-2017-018946supp002.pdf (335.7KB, pdf)