Abstract
Patient: Female, 74
Final Diagnosis: Acute coronary syndrome
Symptoms: Throat pain
Medication: —
Clinical Procedure: Percutaneous coronary intervention
Specialty: Cardiology
Objective:
Challenging differential diagnosis
Background:
Acute coronary syndrome (ACS) is a common and potentially life-threatening condition encountered in emergency departments. Despite its dreaded nature, nearly one-third of ACS present without chest pain and may mislead clinicians. Additionally, Wellens’ syndrome is a pre-infarction stage of significant proximal left anterior descending (LAD) artery stenosis, which can lead to extensive anterior wall myocardial infarction without timely intervention.
Case Report:
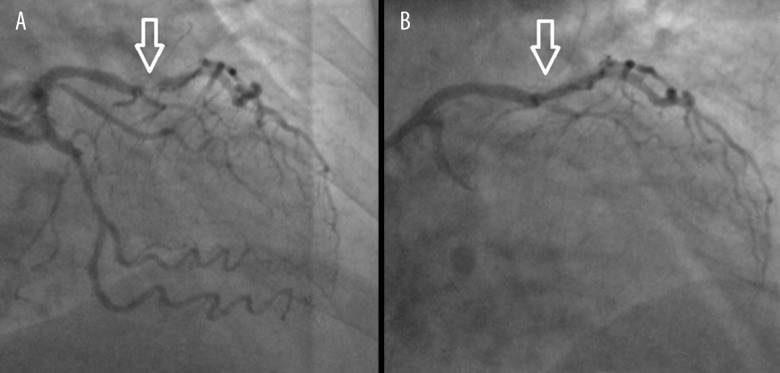
We report the case of a 74-year-old woman presenting with isolated throat pain and Wellens’ pattern in the initial EKG, which prompted the proper workup and management. Subsequently, coronary angiogram revealed more than 90% occlusion of the proximal LAD artery, and a drug-eluting stent was deployed. The patient did well after the procedure and the follow-up at 2 weeks after discharge was uneventful.
Conclusions:
This case highlights the importance of awareness of atypical presentation of ACS and importance of Wellens’ syndrome. We also discuss the incidence of craniofacial symptoms of ACS, and the epidemiology, pathophysiology, management, and prognosis of Wellens’ syndrome.
MeSH Keywords: Acute Coronary Syndrome; Neck Pain; Asymptomatic Diseases; Percutaneous Coronary Intervention; Diagnostic Techniques, Cardiovascular
Background
Typical chest pain in acute coronary syndrome (ACS) is pressure-like left-sided chest pain, possibly with radiation to the left shoulder/arm and associated dyspnea, nausea/vomiting, diaphoresis, or lightheadedness. However, ACS can present with no or atypical symptoms, which can lead to delayed diagnosis and suboptimal treatment, and subsequent detrimental outcome, especially in elderly patients [1–3]. Additionally, Wellens’ syndrome is abnormal T wave changes in patients with suspected ACS, indicating significant occlusion of the proximal left anterior descending (LAD) artery [4]. Herein, we report the case of a 74-year-old woman who presented with isolated throat pain and was found to have Wellens’ syndrome and ACS.
Case Report
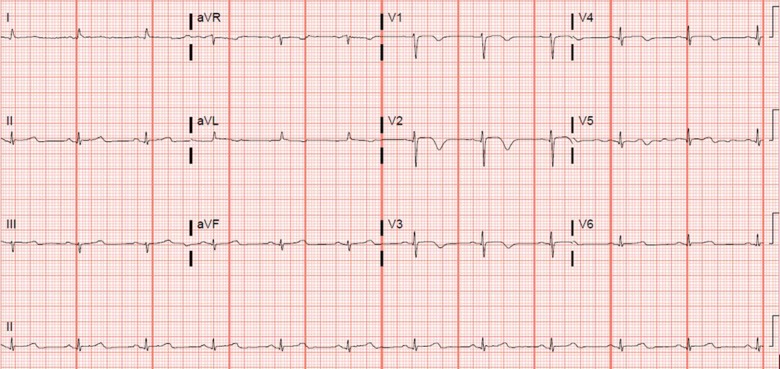
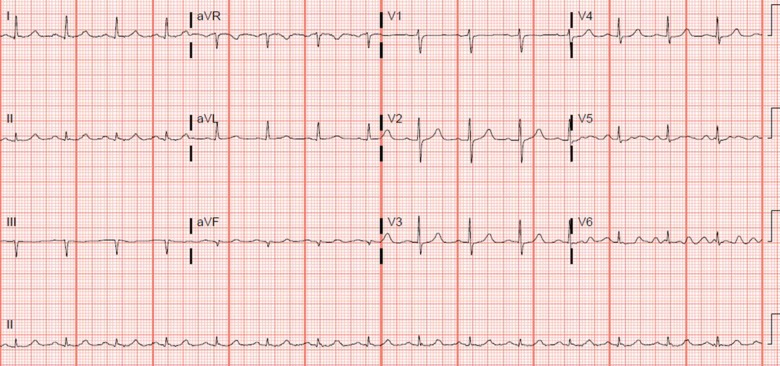
A 74-year-old woman with diabetes, hypertension, dyslipidemia, and hypothyroidism presented with a 3-week history of intermittent throat pain. She denied any chest pain, dyspnea, lightheadedness, nausea/vomiting, or stomach/back pain. She also denied any known coronary artery disease. Her home medications are metformin, vitamin B12, enalapril, atorvastatin, and levothyroxine. Her vital signs were stable and physical exam results were negative, including cardiac and pulmonary exam. Of note, the patient was completely asymptomatic at the time of evaluation. The initial electrocardiogram (EKG) showed T wave inversions over right precordial leads (Figure 1), which were new compared to prior EKG 2 years ago (Figure 2). Initial troponin was 0.9 ng/ml, which went up to 1.7 ng/ml 6 h later. The patient was treated with aspirin, clopidogrel, atorvastatin, carvedilol, and protocol-based heparin infusion for non-ST elevation myocardial infarction (NSTEMI). The patient was admitted to the coronary care unit for close monitoring. Subsequently, a coronary angiogram showed more than 90% stenosis in the proximal left anterior descending artery (LAD), for which a 2.5×12 mm Xience drug-eluting stent was deployed, with good flow (Figure 3). The patient tolerated the procedure and was discharged with standard medical therapy. Follow-up 2 weeks later showed favorable outcome without recurrent events.
Figure 1.
EKG showing deep symmetric T wave inversions in right precordial leads.
Figure 2.
Prior EKG 2 years ago, showing normal sinus rhythm without significant T/ST changes.
Figure 3.
Coronary angiogram showing more than 90% proximal LAD stenosis (A) and status-post stent with restoration of good flow in the LAD (B).
Discussion
ACS is a common and potentially life-threatening condition encountered at emergency departments (ED). Despite its dreaded nature, 33% of ACS may mislead clinicians with atypical presentations [1], which could be dyspnea (49.3%), diaphoresis (26.2%), nausea/vomiting (24.3%), or presyncope/syncope (19.1%), in the order of dominant presenting symptoms [2]. The atypical symptoms tend to occur more commonly among those who are older, female, diabetic (possibly due to autonomic neuropathy), hypertensive, and with prior heart failure. They were reported in 5.7% and 12.3% of patients with unstable angina and NSTEMI, respectively [2]. Consequently, they delay the correct diagnosis and optimal therapy, with an increased risk of in-hospital mortality. As would be expected, because of the frailty and comorbidities, elderly populations are more likely to have complications of ACS, especially when they present without chest pain [3].
Craniofacial pain is the sole presenting symptom in 6% of patients with an ischemic cardiac event, and it is 4 times more frequent than stomach and back pain [5]. Craniofacial pain is a referred pain from the afferent vagal nerve of the heart to efferent somatic nerves to the head and neck [5,6]. It is also more prevalent in women than in men. The throat is the most common site of craniofacial pain. Other sites of referred pain are the mandible, temporomandibular joint, ears, neck, and teeth [5]. Hiccups, a rare presenting symptom, was reported in a patient with PCI (percutaneous coronary intervention)-related STEMI [7].
First reported by Zwaan et al. in 1982, Wellens’ syndrome is a pre-infarction stage of significant proximal LAD artery stenosis and may lead to extensive anterior wall myocardial infarction without timely intervention [4,8]. It was reported in 26% (35/137) of patients with suspected coronary artery disease (CAD) undergoing coronary angiogram [9]. T wave changes in Wellens’ syndrome are associated with widely scattered electrical and mechanical activities (QTc dispersion) in myocardium and severe myocardial dysfunction [9]. Wellens’ syndrome can be identified as 2 patterns on EKG [8]:
Pattern A has biphasic T waves in V2–V3 (25%) and
Pattern B has symmetric and deeply inverted T waves in chest leads (75%).
The diagnostic criteria for Wellens’ syndrome includes the presence of pattern A or pattern B in EKG plus a history of angina, pain-free period, little or no elevation of ST segment, no Q waves in chest leads, and normal or minimal elevation of cardiac enzymes [4,10]. The T wave inversion has 69% sensitivity, 89% specificity, and 86% positive predictive value for significant LAD occlusion [11]. Even in the challenging situations with pre-existing left bundle branch block (LBBB), Wellens’ EKG patterns can be used to detect acute coronary syndrome [12,13].
The differential diagnoses of T wave inversions are acute coronary syndrome (ACS), pulmonary embolism, myocarditis, left ventricular hypertrophy, juvenile T wave, Wolf-Parkinson-White syndrome, and digoxin toxicity [14]. Unlike the regular practice in patients with possible ischemic chest pains, cardiac stress testing is contraindicated in Wellens’ syndrome patients because it can precipitate acute myocardial infarction [9]. When Wellens’ sign is discovered in patients with suspected ACS, a low threshold should be maintained for prompt coronary angiography to determine treatment options [4,8,9]. If there is significant proximal LAD occlusion, percutaneous coronary intervention (PCI) or coronary bypass surgery should be performed to prevent extensive anterior myocardial infarction. When solely managed with medical therapy, 75% of Wellens’ syndrome patients developed extensive anterior wall infarction within 1 week [8].
Our patient initially presented with isolated throat pain without any other associated symptoms. Her vital signs and physical exam results were normal. Given the risk factors (age, sex, diabetes, dyslipidemia, and hypertension) and concern for ACS, routine EKG was done, which showed Wellens’ pattern B. Notably, she was asymptomatic when the EKG was performed. The patient was subsequently diagnosed with NSTEMI and underwent PCI. After discerning the Wellens’ sign, we were able to provide correct diagnosis and optimal management.
Conclusions
In conclusion, craniofacial pain can be the sole presentation of ACS, of which throat pain is the most common symptom. It can be a diagnostic challenge for clinicians, mandating a low threshold of clinical suspicion for ACS. The presence of Wellens’ sign in the EKG can be a crucial clue in patients with atypical presentation of ACS. Therefore, it is imperative for clinicians to identify the EKG characteristics of Wellens’ syndrome and provide necessary tests and appropriate intervention. Medically treated LAD stenosis with Wellens’ syndrome eventually requires coronary intervention to prevent re-occlusion and extensive myocardial injury [8,15–17].
Footnotes
Conflict of interests
None.
References:
- 1.Canto JG, Shlipak MG, Rogers WJ, et al. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000;283(24):3223–29. doi: 10.1001/jama.283.24.3223. [DOI] [PubMed] [Google Scholar]
- 2.Brieger D, Eagle KA, Goodman SG, et al. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: Insights from the Global Registry of Acute Coronary Events. Chest. 2004;126(2):461–69. doi: 10.1378/chest.126.2.461. [DOI] [PubMed] [Google Scholar]
- 3.Engberding N, Wenger NK. Acute coronary syndromes in the elderly. F1000Res. 2017;6:1791. doi: 10.12688/f1000research.11064.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rhinehardt J, Brady WJ, Perron AD, Mattu A. Electrocardiographic manifestations of Wellens’ syndrome. Am J Emerg Med. 2002;20(7):638–43. doi: 10.1053/ajem.2002.34800. [DOI] [PubMed] [Google Scholar]
- 5.Kreiner M, Okeson JP, Michelis V, et al. Craniofacial pain as the sole symptom of cardiac ischemia: a prospective multicenter study. J Am Dental Assoc. 2007;138(1):74–79. doi: 10.14219/jada.archive.2007.0024. [DOI] [PubMed] [Google Scholar]
- 6.Ahmed EK, Alkodaymi MS, Soliman MM, Shujaa AS. ST-elevation myocardial infarction due to left anterior descending artery occlusion presenting primarily with otalgia. Am J Case Rep. 2018;19:1044–47. doi: 10.12659/AJCR.905511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang F, Tongo ND, Hastings V, et al. ST-segment elevation myocardial infarction with acute stent thrombosis presenting as intractable hic-cups: An unusual case. Am J Case Rep. 2018;19:467–71. doi: 10.12659/AJCR.903345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103(4):730–36. doi: 10.1016/0002-8703(82)90480-x. [DOI] [PubMed] [Google Scholar]
- 9.Stankovic I, Kafedzic S, Janicijevic A, et al. T-wave changes in patients with Wellens syndrome are associated with increased myocardial mechanical and electrical dispersion. Int J Cardiovasc Imaging. 2017;33(10):1541–49. doi: 10.1007/s10554-017-1181-4. [DOI] [PubMed] [Google Scholar]
- 10.Mead NE, O’Keefe KP. Wellen’s syndrome: An ominous EKG pattern. J Emerg Trauma Shock. 2009;2(3):206–8. doi: 10.4103/0974-2700.55347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haines DE, Raabe DS, Gundel WD. Anatomic and prognostic significance of new T-wave inversion in unstable angina. Am J Cardiol. 1983;52(1):14–18. doi: 10.1016/0002-9149(83)90061-9. [DOI] [PubMed] [Google Scholar]
- 12.Meyers HP, Smith SW. Dynamic T-wave inversions in the setting of left bundle branch block. Am J Emerg Med. 2016;35(6):938.e5–e7. doi: 10.1016/j.ajem.2016.12.059. [DOI] [PubMed] [Google Scholar]
- 13.Grautoff S. Wellens’ syndrome can indicate high-grade LAD stenosis in case of left bundle branch block. Herzschrittmacherther Elektrophysiol. 2017;28(1):57–59. doi: 10.1007/s00399-017-0489-z. [DOI] [PubMed] [Google Scholar]
- 14.Ozdemir S, Ozturk TC, Eyinc Y, et al. Wellens’ syndrome – report of two cases. Turk J Emerg Med. 2015;15(4):179–81. doi: 10.1016/j.tjem.2014.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cruz MC, Luiz I, Ferreira L, Ferreira RC. Wellens’ syndrome: A bad omen. Cardiology. 2017;137(2):100–3. doi: 10.1159/000455911. [DOI] [PubMed] [Google Scholar]
- 16.Morris N, Howard L. BET 1: in patients with suspected acute coronary syndrome, does Wellens’sign on the electrocardiograph identify critical left anterior descending artery stenosis? Emerg Med J. 2017;34(4):264–66. doi: 10.1136/emermed-2017-206665.1. [DOI] [PubMed] [Google Scholar]
- 17.Aydin AA, Ulutas KT, Aydin C, et al. Successful evaluation of biphasic T-wave of Wellens syndrome in the Emergency Department. Acta Informatica Medica. 2016;24(1):72–73. doi: 10.5455/aim.2016.24.72-73. [DOI] [PMC free article] [PubMed] [Google Scholar]