Abstract
Purpose
Centenarians, a segment of the population which some 50 years ago comprised only a few individuals, now count thousands in many countries, and demographic projections forecast that this growth will continue. The study of this new population will give us new information on extreme longevity and help prepare for their health and social needs. The aim of the Centenari a Trieste study is to describe the health and health service use by centenarians, with specific focus on cognitive status.
Participants
This is a population-based study of centenarians living in the province of Trieste (Italy), a small area with a high prevalence of centenarians and a close network of health and social services, which makes it possible to conduct a study. Consenting individuals were visited by a clinician, tested by neuropsychologists and also gave a sample of their blood. Administrative data were retrieved as well.
Findings to date
Of the 163 centenarians, 70 could be contacted and participated in the study. The main reasons for non-participation were impossibility to contact the subject (70) and death (20). Centenarians were mostly women (90%), tended to live in a nursing home (60%) and were generally severely functionally impaired (Barthel Index <50: 61%). Data from the administrative database showed that about one out of five needed hospitalisation in the preceding year and more than three out of four had at least one drug prescription.
Future plans
In 2017, we started a new wave of the study enrolling people who had just become centenarian and reassessing subjects already seen; we hope to extend this recruitment in the next years. Subjects are now examined also by cardiologists and dental specialists. We are collecting further different biological specimens to investigate new hypotheses on the cognitive function of the centenarians.
Keywords: centenarians, oldest old, dementia, longevity, risk factors, protective factors, activities of daily living, health service use
Strengths and limitations of this study.
The major strength of the study lies in it being a population-based study, where all centenarians are invited to participate, and no exclusion criterion is used.
In order to build a comprehensive picture of the centenarians, we included in the first wave neuropsychological testing, clinical examinations, blood drawing and administrative data access and enhanced the procedure in the second wave adding different medical disciplines and procedures such as ECG, echocardiography, and saliva and faeces collection.
The study benefits from the close network of collaboration with the centenarians’ families, nursing homes, social services, general practitioners, and biological and clinical researchers.
The complex procedure of the enrolment in the first wave of the study caused a low response rate among the centenarians, which we are trying to overcome in the second wave.
We could not verify the age of the individuals, which is an important piece of information in studies on centenarians; however, we found an almost perfect concordance between the data from the city demographic offices and those from the Italian National Institute of Statistics.
Introduction
The numbers and percentages of older people are dramatically growing in most parts of the world and people aged 90 years old and older, termed ‘oldest old’, are the fastest growing group. Compared with younger people, the oldest old have more functional variability and these differences contribute to the complexity of understanding their clinical and cognitive status. Furthermore, because of the small number of centenarians in the past decades and the difficulties of studying them, despite the large number of studies on older people younger than 85 years old very few population-based studies have focused on centenarians until now,1 and even fewer population-based studies included a neuropathological examination.2 Most studies on centenarians present understandable limitations. The first is the difficulty in recruiting centenarians, so most studies have enrolled only small numbers, often scattered over large, widely differing areas. The second is related to testing cognitive abilities, because many centenarians are almost deaf and have visual and movement impairment3 4; then too, in the oldest old, the criteria for a diagnosis of dementia pose intrinsic difficulties and there is a lack of consensus on ‘how’ and ‘when’ making a dementia diagnosis.5 Centenarians often lack brain imaging and neuropathological examinations are rare. For all these reasons our knowledge of centenarians, and specifically of their cognitive status, is still limited and hazy.
Centenarians have been studied using two approaches. The main studies, such as the Georgia Centenarian Study,6 New England Centenarian Study,7 90+ Study8 and others, have very wide catchment areas in order to recruit a large number of centenarians, but at the cost of having a population who do not share genetic traits, food, religion and lifestyle habits. Other studies are limited to small regions where the populations present specific characteristics. These areas, called ‘Blue Zones’ (BZs), are limited areas with a high prevalence of centenarians, with rather homogeneous characteristics, lifestyles and environments.9 The BZs identified so far are in Okinawa (Japan),10 on the Nicoya peninsula11 (Costa Rica), on the island of Ikaria12 (Greece) and in Ogliastra (Sardinia, Italy).9
The numbers of centenarians are rapidly increasing worldwide and so are the studies on this segment of the population, advancing the knowledge acquired so far. In Italy, where the number of centenarians rose from 150 in the mid-1950s to approximately 20 000 in 2014, there are several population studies on the oldest old.13 14 The Centenari a Trieste (CaT) or Centenarians in Trieste study started in 2014 and is currently ongoing. It is a population-based study on centenarians living in the province of Trieste, an Italian city where the prevalence of centenarians is very high: 7 per 10 000 inhabitants against 3 per 10 000 in Italy as a whole.15 Trieste, with just over 200 000 inhabitants, is located in the north-east of Italy, on the border with Slovenia, overlooking the Adriatic Sea. The demographic structure of Trieste is unusual, because the city has always been influenced by its location at the crossroads of Latin, Slavic and Germanic cultures. Until the end of the First World War, when Trieste was part of the Austro-Hungarian Empire, the city was one of the most important Mediterranean seaports and many people with different habits and religions moved there from different parts of Europe for their business. For this reason, although small like a BZ, Trieste is a sort of ethnic melting pot and a centenarian study is interesting and special. Furthermore, the small area and the close network between health and social services make the study easier to manage.
Aims of the CaT study
The objective of the study is to describe the health status of a population of centenarians, measuring disease and disability prevalence, use of social and health services, and present and past lifestyles. It is particularly interesting to quantify cognitive impairment, because of its high prevalence and its consequences at the personal and societal levels. Investigations will also concentrate on correlations between these variables and genetic and biological characteristics.
Cohort description
Study population
On 1 January 2014, the Province of Trieste was inhabited by approximately 236 000 individuals, of whom 87% lived in Trieste city. In Italy, all inhabitants are cared for by the National Health System, organised, on a regional basis, in autonomous local health authorities (LHAs), which usually correspond to the provinces, as in our case. The study population comprised all subjects born before 1914 and registered on 1 January 2014, with the Trieste LHA (ASS1 or Azienda Servizi Sanitari 1 Triestina, now ASUITS or Azienda Sanitaria Universitaria Integrata di Trieste).
Study design
After obtaining the list of the centenarians cared for by the Trieste LHA, we sent a request to the LHA professionals already in contact with the centenarians and their families (general practitioner (GP), nursing home or community service personnel) asking them to allow us to explain the study to the centenarians and their families for their enrolment. After receiving consent to the study presentation (first informed consent), one of us (GM) went to the centenarian’s residence (home or institute) to describe the study procedures. If the person was willing to participate in the study, we obtained a second signed informed consent for enrolment and possibly a third signed informed consent for a blood sample.
The examination involved two visits: (1) a clinical visit to collect data on present and past pathologies and on daily living activities; (2) a neuropsychological assessment during which the patients were tested using an ad hoc battery on cognitive and mood domains. At a subsequent visit, a blood sample was obtained from the subset of consenting centenarians by one of us (GM) together with a registered nurse. The samples were immediately processed in the laboratory for lymphocyte cell isolation and DNA extraction. Subsequently all parts of the sample were stocked at −80°C.
In some cases, data from the centenarians were obtained interviewing an informant: a relative, a close friend or personnel of the institute where the subject lived. Further information on present and past health of the centenarians enrolled was extracted from the LHA administrative databases.
Interviews were conducted between January 2014 and July 2015.
Clinical evaluation: personal history and neurological examination
The clinical evaluation was done by one of us (GM, neurologist) and involved obtaining information using a standardised questionnaire on family history and sociodemographic data, present and past lifestyles, lifetime eating habits, currently taken drugs, surgical interventions, hospitalisations or access to the emergency room (ER), hearing and vision impairment and need for assistance or supervision. Information on present and past pathologies (cardiovascular, central nervous system and diabetes) with related therapies was recorded. A second part of the clinical evaluation was the physical examination.
Diagnosis of dementia
The neurologist and the neuropsychologists independently made a tentative diagnosis of dementia applying the criteria of Diagnostic and Statistical Manual of Mental Disorders—fourth edition.16 In some cases, we had difficulty in assessing the presence of dementia due to sensory impairment or fatigue which prevented us from having a complete picture of the cognitive status of the centenarian.
Scales and tests
An important part of the visits was devoted to administering neuropsychological tests or assessing the person’s daily living activities and quality of life or anxiety/depression using validated structured questionnaires, administered in a specific sequence. Subjects were interviewed at their place of residence.
Neuropsychological testing
Subjects were tested using the Italian version17 of the Mini-Mental State Examination18 (MMSE), a brief screening instrument commonly used in epidemiological studies to assess cognitive status. In cases with severe dementia, a similar but much less demanding test, the Severe MMSE,19 was used.
A series of seven tests taken from the Consortium to Establish a Registry on Alzheimer’s Dementia (CERAD)20 battery was then tried: Verbal Fluency (animal categories), Boston Naming Test (15 items), Word List Memory, Word List Recall and Word List Recognition, Constructional Praxis and Recall of Constructional Praxis. This battery was translated into Italian by the laboratory to which one (MT) of us is affiliated, and was validated in elderly native Italian speakers.21
Three other specific tests were used: the Visual Search on Matrices of Digits,22 the forward and backward Digit Span test23 and the Prose Memory test.22
After the tests, the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE)24 25 was administered to an informant. The IQCODE assesses change in the cognitive function of the subject. Change was assessed relative to 10 years ago and, whenever possible, also 40 years ago.
Mood and quality of life
Depression symptoms were assessed using the 15-item version26 of the Geriatric Depression Scale,27 a rating scale specifically developed to test elderly people. Anxiety was tested with the Beck Anxiety Inventory.28
Quality of life was assessed using the Short Form-12,29 a brief questionnaire composed of 12 items, derived from a larger 36-item questionnaire.30
The scales were usually administered by or compiled under the supervision of the neuropsychologist, rather than being self-administered, on account of visual or motor impairments. Answers given by subjects with severe cognitive impairment were not considered reliable, and therefore not used.
Activities of daily living
Independence in daily living tasks was assessed in three hierarchically related domains.
The lowest domain, pertaining to the simplest tasks, that is, the basic activities of daily living (BADL), was assessed using the Barthel Index.31
The Instrumental Activities of Daily Living32 (IADL) was used to characterise subjects at a higher level than the BADL. This instrument assesses competence in common tasks requiring interaction with instruments or media. Scores were normalised so that both men and women had a possible range between 0 (completely dependent) and 100 (completely independent).
At the highest level, we gathered data on Advanced Activities of Daily Living (AADL) using a modification of the questionnaire developed by Verghese et al33 investigating participation in leisure activities. In addition to frequency of present activities, whenever possible we also recorded (from an informant) the frequency of the activities approximately 40 years ago (ie, around retirement age).
Administrative data
Italy has universal health insurance, and all contacts between citizens and health service providers are recorded for administrative purposes (mainly for direct payment and cost governance). For the centenarians in our study, we had access to the following datasets: hospitalisations (dates of hospital admission and discharge, ICD-9-CM34 diagnostic codes at discharge and procedures during hospitalisation, life status at discharge), ER admissions (date, text summary relative to the event), drug prescriptions (name of drug, date of dispensation, number of boxes, Anatomical Therapeutic Chemical (ATC) classification35), specialty visits (general type of visit, date of visit). We also had access to the same data, anonymised, for subjects we could not trace in person. Data were available from 2000 to 2014.
General practitioners
GPs caring for the centenarians were contacted to complete a questionnaire on disease presence, the Cumulative Illness Rating Scale,36 and a form on drug prescriptions.
Participants
On 1 January 2014, there were 163 centenarians in the Trieste LHA, 21 (13%) men and 142 (87%) women. Most of the centenarians were born in the Province of Trieste (42%), in the other provinces of the Friuli-Venezia Giulia Region (15%) or in the nearby territories now part of Slovenia or Croatia (23%). The rest were born in other parts of Italy (17%) or abroad (3%).
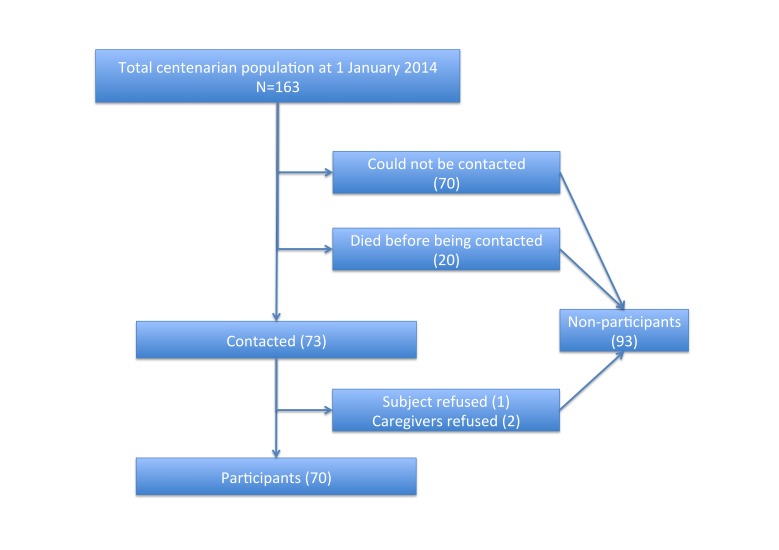
Seventy subjects were visited by one of us (GM) and for most of them another visit was done by a neuropsychologist (see figure 1 for the flow chart of the study). Ninety-three subjects did not participate in the study: for most of them (70 subjects, 75%) we could not find an LHA professional who was willing or had time to introduce us to the centenarian, while 20 (22%) died between prevalence day and the day in which we tried to contact them, one refused and two did not participate because the relatives thought the visit could bother the centenarian. Sex ratio and age were only slightly different between participating and non-participating subjects (χ2 and Mann-Whitney U test, P>0.17) (data for non-participating subjects retrieved anonymously from administrative database).
Figure 1.
Flow chart of the study.
The main characteristics of the participating and non-participating subjects are reported in tables 1 and 2.
Table 1.
Main sociodemographic characteristics of the participating subjects (n=70)
| n (%) | Available data | |
| Age (mean±SD) | 102.1±1.9 | 70 |
| Sex | 70 | |
| Males | 7 (10%) | |
| Females | 63 (90%) | |
| Native Italian speakers | 49 (78%) | 63 |
| Living condition | 66 | |
| Institutionalised | 40 (60%) | |
| Living alone | 5 (8%) | |
| Living with others | 21 (32%) | |
| Years of education: mean (SD) | 6.3 (2.6) | 65 |
Table 2.
Age and sex distributions of the non-participating subjects (n=93)
| n (%) | Available data | |
| Age (mean±SD) | 101.8±1.7 | 93 |
| Sex | 93 | |
| Males | 14 (15%) | |
| Females | 79 (85%) |
Statistical analysis
Numeric variables were summarised using means and SDs when the distribution of the variable was approximately symmetrical or medians when it was skewed or in presence of outliers. Numeric variables were dichotomised when the resulting clinical meaning was clearer (eg, IADL). Ordinal variables were dichotomised to avoid having classes with very few or no individuals (eg, AADL). Differences between participants and non-participants were tested using χ2 (nominal variables) or Mann-Whitney U test (numeric variables).
Findings to date
Participating subjects
In many cases (74%), the information received from the centenarian was supplemented by data from an informant. Mean age of the informant was 69.6 years, with a majority of females (81%). In almost half of the cases (24 subjects), the informant was a daughter. When the subject was institutionalised and no relatives could be traced or when the centenarian was living alone (26%), we did not have an informant.
The mean (SD) number of chronic drugs was 2.9 (2.2), with a moderately high prevalence (24%) of polytherapy (five or more drugs). Subjects not using any drug were 23% of the population. The most prevalent drug classes were antithrombotic agents, ATC B01 (40%), and drugs for acid-related disorders, mainly proton pump inhibitors (PPIs), ATC A02 (37%), followed by cardiovascular system drugs (diuretics, ATC C03 (31%), cardiac therapy, ATC C01 (30%), agents acting on the renin–angiotensin system, ATC C09 (26%)) and psycholeptics (mainly benzodiazepines) ATC N05 (21%). All other drug categories were used by less than 10% of the centenarians.
The majority of centenarians had significant hearing problems (60 subjects, 86%) or seeing (54 subjects, 76%) or both (47 subjects, 67%). A sizeable minority (16%) was completely deaf, but only one was totally blind.
Most centenarians were severely or completely functionally impaired even at the basic stage of the BADLs (Barthel Index <50: 61%), while three (5%) were completely independent. At a hierarchically higher level, 80% of the centenarians have IADL residual ability lower than 50% and only one was completely independent (missing data: BADL 6 subjects, IADL 11 subjects). Due to physical and cognitive limitations leisure activities involved only a small percentage of subjects. Watching television was still a very popular, although highly passive, activity (60% watched television at least two times per week), followed by listening to music (44%), reading newspapers/magazine (37%) and walking (31%). Among those still taking a walk, the median time was relatively limited (15 min/day). A couple of subjects still walked 2 hours/day. No other activity was performed at least two times per week by 20% or more of the centenarians (missing data: 35 subjects—information unavailable for subjects without neuropsychological examination or missing informant).
A neuropsychological test session was possible only in 51 subjects (73%) (five died before the neuropsychologist could contact the centenarian, three had a relative who felt the neuropsychological examination could bother the centenarian, one was very sick, six could not be tested because of administrative reasons and four were not tested since the subject was in a severe/terminal dementia condition: for these four persons a score of zero was given in the MMSE—these imputed scores may have reduced the mean MMSE score). In the CERAD tests, the ones completed by the largest number of subjects were the Verbal Fluency test and the Boston Naming Test (table 3).
Table 3.
Neuropsychological test results and depression and quality of life scores
| Test | n | Attainable range | Mean (SD) |
| MMSE* | 45 | 0–30 | 11.9 (8.4) |
| CERAD Verbal Fluency | 39 | 0– | 6.3 (3.3) |
| CERAD Boston Naming Test | 35 | 0–15 | 7.3 (2.9) |
| CERAD Word List Memory | 28 | 0–10 | 6.7 (3.5) |
| CERAD Word List Recall | 26 | 0–10 | 1.0 (1.2) |
| CERAD Word List Recognition | 25 | 0–10 | 4.5 (3.3) |
| CERAD Constructional Praxis | 30 | 0–11 | 4.8 (2.2) |
| CERAD Recall Constructional Praxis | 21 | 0–11 | 1.1 (2.0) |
| IQCODE | 20 | 5–0 | 4.1 (0.6) |
| Geriatric Depression Scale† | 15 | 0–15 | 5.8 (4.2) |
| SF-12—physical status† | 13 | 0–100 | 38.5 (12.3) |
| SF-12—mental status† | 13 | 0–100 | 47.4 (9.8) |
Tests were reported if they were completed by at least 20 centenarians.
*Contains data from MMSE, data derived from SMMSE and zeros for subjects with severe or terminal dementia.
†Only for subjects judged by the neurologist as not having dementia.
CERAD, Consortium to Establish a Registry on Alzheimer’s Dementia; IQCODE, Informant Questionnaire on Cognitive Decline in the Elderly; MMSE, Mini-Mental State Examination; SF-12, 12-item Short-Form questionnaire; SMMSE, Severe Mini-Mental State Examination.
Administrative database information
The availability of the administrative databases in the year preceding the cohort selection enabled us to achieve two goals: retrieve health service usage for the total centenarian population and compare usages by the participating and non-participating subjects, in order to assess differences between the two groups.
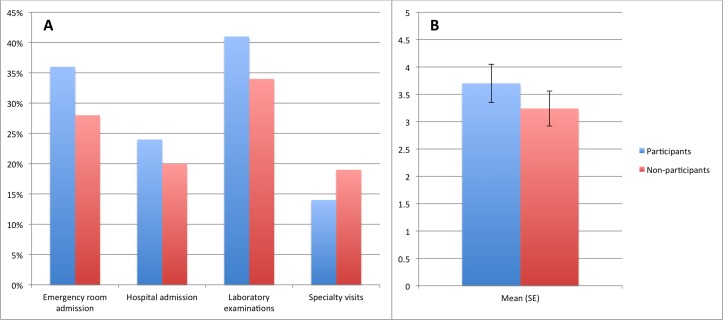
Almost one out of three (31%) centenarians had at least one ER admission, with a higher incidence, not statistically significant, in the participating subjects (χ2, P=0.29) (figure 2A). During these admissions, the mean number of services activated (eg, ECG, specialty visit, catheterisation, etc) was 3.6 (SD 2.9), with no difference between the two groups (Mann-Whitney U test, P=0.72).
Figure 2.
Health service use by participating and non-participating centenarians. (A) Service use prevalence (%). (B) Number of prescribed drugs.
Similarly, 36 centenarians (22%) had been hospitalised in the year preceding the prevalence day, 17 (24%) in the participant group and 19 (20%) in the non-participant group. Among those hospitalised, the median number of days in hospital was 8.5, similar for participants (8 days) and non-participants (9 days). Diseases of the vascular, respiratory and digestive systems were the main primary reasons for hospitalisation (33 cases, 62% in the whole population, 68% of participants, 57% of non-participants).
A high proportion of centenarians (61 subjects, 37%) had laboratory tests in 2013, with similar numbers for participants (29 subjects, 41%) and non-participants (32 subjects, 34%), while a substantial minority needed a specialty visit (total: 28 subjects, 17%, 10 participants, 14%, 18 non-participants, 19%). Of these 60% (33 subjects) had a cardiologic visit or an eye examination.
Finally, the numbers of drugs (different therapeutic subgroups) taken in 2013 were very similar for participants and non-participants (respective means and SDs 3.7±2.9 and 3.2±3.1, figure 2B). Since the time window encompasses an entire year, unlike data collected directly from the centenarian, antibacterials for systemic use, ATC J01, were highly prevalent (39%), while ATC A02 (46%), B01 (36%) and C03 (21%) drug use remained high. Two other cardiovascular classes (cardiac therapy, ATC C01 (25%) and agents acting on the renin–angiotensin system, ATC C09 (26%)), and analgesics, ATC N02 (21%) were the only other therapeutical subclasses with a prevalence of use over 20%. None of the reported differences between participants and non-participants related to administrative data reached 0.05 for significance, suggesting that participants’ characteristics were similar to those of the whole population.
Discussion
The CaT study was designed in 2013 to investigate the clinical, biological and social characteristics of centenarians living in Trieste.
Our centenarians tended to live in nursing home/sheltered houses (60%) similarly to centenarians in North European and American countries, such as Denmark37 (59%) and Georgia (USA38) (56%), although there are also opposite findings, as in Portugal39 (29%), South Korea40 (7%) and Japan (Tokyo41) (32%). The Italian Multicenter Study on Centenarians (IMUSCE) results42 found that only 34% of centenarians lived in a nursing home. The difference is probably due to at least two factors: the first is a difference between the south of Italy (where most of the IMUSCE centenarians lived) where it is more likely that, for cultural and economical reasons, old people continue to live at home with their close relatives than in north of Italy (CaT Study); the second reason is a cohort effect, for attitudes towards keeping old relatives at home have rapidly shifted (IMUSCE was carried out in the mid-1990s). Similarly, at the level of education, 33% of IMUSCE participants were illiterate, against a 2% in CaT. Worldwide situations also differed widely, from South Korea40 (illiterate: 91%) to USA,38 where subjects with less than 5 years of schooling were a small minority (5%, while 30% had more than 13 years of schooling).
Chronic drug therapy was highly prevalent (77%) and similar to that one reported from a UK GP database43 (73%), but lower than in two Italian44 45 (90% and 95%) and one Danish46 (95%) population studies, and substantially higher than in an administrative database study conducted in France47 (44%). Since specific guidelines are widely shared for all the diseases highly prevalent in the elderly, we expected the pharmacological subclasses used in our study to be similar to those reported by others; in fact, the studies that reported drug use by therapeutical subclasses did give similar results, though with some interesting differences: Australian Veterans48 had generally slightly higher drug use, the Danish population46 had lower antithrombotic and PPI use, Ontario49 had higher diuretic and antidepressant and lower PPI use and Swedish population50 had higher analgesic and benzodiazepine and lower PPI use.
Since we looked at pharmacological therapies from two different points of view (day prevalence, at place of residence and year prevalence from administrative databases), we found two interesting differences: benzodiazepines were absent from administrative databases, since they are not reimbursed in Italy, but were present at place of residence, while antibacterials had been widely prescribed in the previous year, but were not being used at the time of the visit. Except for Australian veterans, PPI use was lower in the other studies. High PPI use, with a large proportion of inappropriate use,51 has been already reported in elderly Italian patients,52 in both primary and secondary care.
When looking at health services, we need to consider that both the state of health of the population and the national legislative/financial regulations for treatment possibilities contribute to their use. However, our data on use of services (ER 31% and hospital admissions (H) 22%) are similar to the ones reported elsewhere: Ontario49 (ER 26.6%, H 18.2%), UK53 (H 41.5%, in the year following the prevalence day), Denmark37 (H 56.5% in 5 years) and Veterans in Australia48 (H 19.1%), while the number of ER admissions was much lower than in the USA54 (73.6%). Such great use of expensive services may have a profound impact on the sustainability of the health services, in view of the fast rise in the absolute numbers of centenarians. However, this gloomy future is tempered by the fact that the high costs are for a substantial part related to the proximity of death,55 so they are inescapable and are currently high among centenarians because of their very high mortality. It will be interesting to compare present and future service use rates to see if they shift with changes in mortality.
We also found that centenarians in Trieste had a very high degree of disability, as others have found.37 40 56 57 This requires a lot of assistance but, like for service use, Arai et al58 and Christensen et al56 demonstrated that even in extreme age disability is more prevalent in subjects who have the shortest life expectancy, so these results must be interpreted more from a dynamic than a static point of view, comparing results from different cohorts examined longitudinally.
Forthcoming wave of visits
In April 2017, we began a second wave of visits on the subjects who became centenarians after 2014 and to the centenarians included in the first wave. We also revised the tests and scales in the neuropsychological battery after a preliminary analysis of their completion rates, excluding tests that proved too hard to administer for cognitive or sensory impairment or for logistic difficulties. A digital recorder is being used to assess spoken language. Since two clinics of the department of medical sciences (dental medicine and cardiology) are now collaborating with us, the study was expanded to look closely at those specific characteristics in the centenarians and identify any link with dementia. A cardiologist makes a complete cardiologic visit, including echocardiogram, ECG and heart rate variability. A dentist does an objective examination of the oral cavity with oral mucosa brushing for biological studies. At the same time the diagnoses of dementia tentatively made in the first wave are being reappraised with the help of a third independent examiner to reach a consensus on the presence of the disease. The severity of the disease will be scored using the Clinical Dementia Rating59 staging rules. Results on the data from this forthcoming wave of visits are presently not available. The revised ongoing version of the protocol was presented and approved by the Regional Ethics Committee.
Strengths and limitations
The CaT Study was designed in 2013 to investigate the clinical, biological and social characteristics of centenarians living in Trieste. Since this is a study on centenarians, a limitation of the study is the absence of a confirmation of the age of the individuals, while in other studies on centenarians this checking is present. However, we are confident that the date of birth reported in the administrative database is the real date of birth since this database is frequently updated using the official data stored in the city demographic offices, and the data are in an almost perfect concordance with the numbers reported by the Italian National Institute of Statistics.
The major strength of the study lies in it being a population-based study, where all centenarians are invited to participate, and no exclusion criterion is used. The study was designed with an open mind towards collaboration: in the first wave neurologists, neuropsychologists, biologists, GPs, data administrators and social workers were invited to collaborate. In the second wave, we were joined by two new medical disciplines, which will implement procedures as ECG, echocardiography, and saliva and faeces collection.
The major limitation in the first wave of this study was the low response rate among the centenarians, which could cast doubt on the generalisability of the results. The impossibility of directly asking subjects about their willingness to participate in the study, and the consequent need to ask persons not directly involved, left us with a high percentage of centenarians we could not contact. This contrasts with the willing acceptance shown by almost all the centenarians we could approach. However, the access to the administrative data allowed us to test if the enrolled sample was different from the subjects we could not contact: importantly, these supplementary data suggest that the sample we could contact is not biased since it has very similar features to those of the whole population. Moreover, to increase the response rate, we are now experimenting new ways to contact the centenarians, seeking the cooperation from other health and social service professionals.
An important added strength of the new wave of this study is the presence of dental medicine and cardiology specialists, which will give the study the opportunity to assess aspects of the centenarian population with little or no publication record.
Acknowledgments
We thank Nicola Delli Quadri, Adriano Marcolongo, Emanuela Fragiacomo, Fabio Samani and Adele Maggiore for help in starting and keeping the study going; Giacomo Benedetti and Marco Spanò for assistance in data retrieval; Filomena Vella, Miriam Vignando, Fabio Campanella, Marijana Music and Cristiano Stea for testing the centenarians; Ilaria Speranza for assistance in data analysis; Enrico Nicolis for database hosting and help; J. D. Baggot for language editing; Ugo Lucca for advice and direction; Roberto Di Lenarda, Gianfranco Sinagra, Mauro Giacca, Raffaella Rumiati, Maria Rita Piras and Fabio Casati for expanding the original protocol to include new sections; Marcello Fracanzani for encouragement and Silvio Garattini for suggestions and warm support. We are also grateful to Fondazione Foreman Casali for a grant and to the Trieste centenarians, their families, the general practitioners and the nursing home and community service personnel for taking time to participate in the study.
Footnotes
Contributors: MT and GM ideated and designed the study. GM visited the centenarians and coordinated data acquisition. MT organised data input, cleaning and analysis. Both authors drafted the manuscript and approved its final version.
Funding: Two grants were received from Fondazione Benefica Kathleen Foreman Casali of Trieste: (1) to buy a freezer to store biomedical specimens and (2) to economically support the processing of blood samples.
Disclaimer: The design of the study, the collection, analysis and interpretation of data, and writing the manuscript rests solely on the authors.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: The following ethic committees approved this study: Trieste LHA Ethics Committee (first wave) and Friuli-Venezia Giulia Regional Ethics Committee (present wave).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The datasets used during the current study are available from the corresponding author on reasonable request.
Author note: We are willing to share our data and protocols with other researchers: please send an email to the corresponding author detailing your aims and methods and we will soon get in touch with you. Provided ethics and privacy laws are respected, we are in principle willing to share information on every different aspect of our study. Presently we are already collaborating with other groups that are part of the International Centenarian Consortium. Since a revised baseline can be implemented every new wave of the study, we are also eager to expand our focus to study new aspects of centenarians’ health.
References
- 1.Brodaty H, Woolf C, Andersen S, et al. ICC-dementia (International Centenarian Consortium - dementia): an international consortium to determine the prevalence and incidence of dementia in centenarians across diverse ethnoracial and sociocultural groups. BMC Neurol 2016;16:52 10.1186/s12883-016-0569-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang Z, Slavin MJ, Sachdev PS. Dementia in the oldest old. Nat Rev Neurol 2013;9:382–93. 10.1038/nrneurol.2013.105 [DOI] [PubMed] [Google Scholar]
- 3.Gussekloo J, de Craen AJ, Oduber C, et al. Sensory impairment and cognitive functioning in oldest-old subjects: the Leiden 85+ Study. Am J Geriatr Psychiatry 2005;13:781–6. 10.1097/00019442-200509000-00006 [DOI] [PubMed] [Google Scholar]
- 4.Kahle-Wrobleski K, Corrada MM, Kawas C, et al. Dementia and cognition in the oldest-old : Miller BL, Boeve BF, The behavioral neurology of dementia. Cambridge: UK University Press, 2009:254–63. [Google Scholar]
- 5.Slavin MJ, Brodaty H, Sachdev PS. Challenges of diagnosing dementia in the oldest old population. J Gerontol A Biol Sci Med Sci 2013;68:1103–11. 10.1093/gerona/glt051 [DOI] [PubMed] [Google Scholar]
- 6.Poon LW, Jazwinski M, Green RC, et al. Methodological Considerations in Studying Centenarians: Lessons Learned From the Georgia Centenarian Studies. Annu Rev Gerontol Geriatr 2007;27:231–64. [PMC free article] [PubMed] [Google Scholar]
- 7.Perls TT, Bochen K, Freeman M, et al. Validity of reported age and centenarian prevalence in New England. Age Ageing 1999;28:193–7. 10.1093/ageing/28.2.193 [DOI] [PubMed] [Google Scholar]
- 8.Corrada MM, Brookmeyer R, Berlau D, et al. Prevalence of dementia after age 90: results from the 90+ study. Neurology 2008;71:337–43. 10.1212/01.wnl.0000310773.65918.cd [DOI] [PubMed] [Google Scholar]
- 9.Poulain M, Pes GM, Grasland C, et al. Identification of a geographic area characterized by extreme longevity in the Sardinia island: the AKEA study. Exp Gerontol 2004;39:1423–9. 10.1016/j.exger.2004.06.016 [DOI] [PubMed] [Google Scholar]
- 10.Willcox DC, Willcox BJ, Hsueh WC, et al. Genetic determinants of exceptional human longevity: insights from the Okinawa Centenarian Study. Age 2006;28:313–32. 10.1007/s11357-006-9020-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosero-Bixby L, Dow WH, Rehkopf DH. The Nicoya region of Costa Rica: a high longevity island for elderly males. Vienna Yearb Popul Res 2013;11:109–36. 10.1553/populationyearbook2013s109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stefanadis CI. Unveiling the secrets of longevity: the Ikaria study. Hellenic J Cardiol 2011;52:479–80. [PubMed] [Google Scholar]
- 13.Lucca U, Garrì M, Recchia A, et al. A Population-based study of dementia in the oldest old: the Monzino 80-plus study. BMC Neurol 2011;11:54 10.1186/1471-2377-11-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Franceschi C, Motta L, Valensin S, et al. Do men and women follow different trajectories to reach extreme longevity? Italian Multicenter Study on Centenarians (IMUSCE). Aging 2000;12:77–84. [DOI] [PubMed] [Google Scholar]
- 15.Demographic statistics. http://demo.istat.it (accessed 16 Oct 2017).
- 16.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4 edition Washington, DC: American Psychiatric Association, 1994. [Google Scholar]
- 17.Measso G, Cavarzeran F, Zappalà G, et al. The mini‐mental state examination: Normative study of an Italian random sample. Dev Neuropsychol 1993;9:77–85. 10.1080/87565649109540545 [DOI] [Google Scholar]
- 18.Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- 19.Harrell LE, Marson D, Chatterjee A, et al. The Severe Mini-Mental State Examination: a new neuropsychologic instrument for the bedside assessment of severely impaired patients with Alzheimer disease. Alzheimer Dis Assoc Disord 2000;14:168–75. 10.1097/00002093-200007000-00008 [DOI] [PubMed] [Google Scholar]
- 20.Morris JC, Heyman A, Mohs RC, et al. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology 1989;39:1159–65. [DOI] [PubMed] [Google Scholar]
- 21.Lugli A. Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Studio normativo della batteria di valutazione neuropsicologica su una popolazione di lingua italiana [CERAD. Normative study of the neuropsychological assessment battery in an Italian speaking population. Postgraduate dissertation, in Italian].. 2002.
- 22.Spinnler H, Tognoni G. Standardizzazione e Taratura Italiana di Test Neuropsicologici [Standardization and Italian norms of neuropsychological tests].. Ital J Neurol Sci 1987;8(Suppl. 6):1–120. [PubMed] [Google Scholar]
- 23.Monaco M, Costa A, Caltagirone C, et al. Forward and backward span for verbal and visuo-spatial data: standardization and normative data from an Italian adult population. Neurol Sci 2013;34:749–54. 10.1007/s10072-012-1130-x [DOI] [PubMed] [Google Scholar]
- 24.Jorm AF, Jacomb PA. The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): socio-demographic correlates, reliability, validity and some norms. Psychol Med 1989;19:1015–22. 10.1017/S0033291700005742 [DOI] [PubMed] [Google Scholar]
- 25.Isella V, Villa ML, Frattola L, et al. Screening cognitive decline in dementia: preliminary data on the Italian version of the IQCODE. Neurol Sci 2002;23 Suppl 2(Suppl 2):s79–s80. 10.1007/s100720200079 [DOI] [PubMed] [Google Scholar]
- 26.D’Ath P, Katona P, Mullan E, et al. Screening, detection and management of depression in elderly primary care attenders. I: The acceptability and performance of the 15 item Geriatric Depression Scale (GDS15) and the development of short versions. Fam Pract 1994;11:260–6. 10.1093/fampra/11.3.260 [DOI] [PubMed] [Google Scholar]
- 27.Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1982;17:37–49. 10.1016/0022-3956(82)90033-4 [DOI] [PubMed] [Google Scholar]
- 28.Beck AT, Epstein N, Brown G, et al. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988;56:893–7. 10.1037/0022-006X.56.6.893 [DOI] [PubMed] [Google Scholar]
- 29.Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol 1998;51:1171–8. [DOI] [PubMed] [Google Scholar]
- 30.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 31.Mahoney FI, Barthel DW. Functional evaluation: the barthel index. Md State Med J 1965;14:61–5. [PubMed] [Google Scholar]
- 32.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179–86. 10.1093/geront/9.3_Part_1.179 [DOI] [PubMed] [Google Scholar]
- 33.Verghese J, Lipton RB, Katz MJ, et al. Leisure activities and the risk of dementia in the elderly. N Engl J Med 2003;348:2508–16. 10.1056/NEJMoa022252 [DOI] [PubMed] [Google Scholar]
- 34. International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM).. 2001.
- 35.The Anatomical Therapeutic Chemical (ATC) classification. About the ATC/DDD system. WHO Collaborating Centre for Drug Statistics Methodology. http://www.whocc.no/atcddd/ (accessed 16 Oct 2017).
- 36.Parmelee PA, Thuras PD, Katz IR, et al. Validation of the Cumulative Illness Rating Scale in a geriatric residential population. J Am Geriatr Soc 1995;43:130–7. 10.1111/j.1532-5415.1995.tb06377.x [DOI] [PubMed] [Google Scholar]
- 37.Engberg H, Oksuzyan A, Jeune B, et al. Centenarians--a useful model for healthy aging? A 29-year follow-up of hospitalizations among 40,000 Danes born in 1905. Aging Cell 2009;8:270–6. 10.1111/j.1474-9726.2009.00474.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Martin P, MacDonald M, Margrett J, et al. Correlates of functional capacity among centenarians. J Appl Gerontol 2013;32:324–46. 10.1177/0733464811420563 [DOI] [PubMed] [Google Scholar]
- 39.Ribeiro O, Teixeira L, Araújo L, et al. Health profile of centenarians in Portugal: a census-based approach. Popul Health Metr 2016;14:13 10.1186/s12963-016-0083-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim H, Lee T, Lee S, et al. Factors associated with ADL and IADL dependency among Korean centenarians: reaching the 100-year-old life transition. Int J Aging Hum Dev 2012;74:243–64. 10.2190/AG.74.3.e [DOI] [PubMed] [Google Scholar]
- 41.Gondo Y, Hirose N, Arai Y, et al. Functional status of centenarians in Tokyo, Japan: developing better phenotypes of exceptional longevity. J Gerontol A Biol Sci Med Sci 2006;61:305–10. 10.1093/gerona/61.3.305 [DOI] [PubMed] [Google Scholar]
- 42.Centenarians I. Epidemiological and socioeconomic aspects of Italian centenarians. Arch Gerontol Geriatr 1997;25:149–57. [Google Scholar]
- 43.Hazra NC, Dregan A, Jackson S, et al. Drug Utilization and Inappropriate Prescribing in Centenarians. J Am Geriatr Soc 2016;64:1079–84. 10.1111/jgs.14106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lucca U, Tettamanti M, Logroscino G, et al. Prevalence of dementia in the oldest old: the Monzino 80-plus population based study. Alzheimers Dement 2015;11:258–70. 10.1016/j.jalz.2014.05.1750 [DOI] [PubMed] [Google Scholar]
- 45.Fradà G, Bennati E, Cardillo E, et al. Pharmacotherapy in the extreme longevity. Arch Gerontol Geriatr 2009;49:60–3. 10.1016/j.archger.2008.04.013 [DOI] [PubMed] [Google Scholar]
- 46.Andersen-Ranberg K, Schroll M, Jeune B. Healthy centenarians do not exist, but autonomous centenarians do: a population-based study of morbidity among Danish centenarians. J Am Geriatr Soc 2001;49:900–8. 10.1046/j.1532-5415.2001.49180.x [DOI] [PubMed] [Google Scholar]
- 47.Simiand-Erdociain E, Lapeyre-Mestre M, Bagheri-Charabiani H, et al. Drug consumption in a very elderly community-dwelling population. Eur J Clin Pharmacol 2001;57:691–2. 10.1007/s002280100344 [DOI] [PubMed] [Google Scholar]
- 48.Roughead EE, Kalisch LM, Ramsay EN, et al. Use of health services and medicines amongst Australian war veterans: a comparison of young elderly, near centenarians and centenarians. BMC Geriatr 2010;10:83 10.1186/1471-2318-10-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rochon PA, Gruneir A, Wu W, et al. Demographic characteristics and healthcare use of centenarians: a population-based cohort study. J Am Geriatr Soc 2014;62:86–93. 10.1111/jgs.12613 [DOI] [PubMed] [Google Scholar]
- 50.Wastesson JW, Parker MG, Fastbom J, et al. Drug use in centenarians compared with nonagenarians and octogenarians in Sweden: a nationwide register-based study. Age Ageing 2012;41:218–24. 10.1093/ageing/afr144 [DOI] [PubMed] [Google Scholar]
- 51.Forgacs I, Loganayagam A. Overprescribing proton pump inhibitors. BMJ 2008;336:2–3. 10.1136/bmj.39406.449456.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pasina L, Nobili A, Tettamanti M, et al. Prevalence and appropriateness of drug prescriptions for peptic ulcer and gastro-esophageal reflux disease in a cohort of hospitalized elderly. Eur J Intern Med 2011;22:205–10. 10.1016/j.ejim.2010.11.009 [DOI] [PubMed] [Google Scholar]
- 53.Dotchin CL, Gray WK, Gaskin E, et al. Frequency, nature and outcomes of hospital admissions in centenarians in an area of North-East England. Geriatr Gerontol Int 2016;16:969–75. 10.1111/ggi.12586 [DOI] [PubMed] [Google Scholar]
- 54.Carey MR, Howell EM, McHugh MC. Emergency department use by centenarians: the 2008 Nationwide Emergency Department Sample. Prev Chronic Dis 2013;10:E198 10.5888/pcd10.120006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang Z, Norton EC, Stearns SC. Longevity and health care expenditures: the real reasons older people spend more. J Gerontol B Psychol Sci Soc Sci 2003;58:S2–10. 10.1093/geronb/58.1.S2 [DOI] [PubMed] [Google Scholar]
- 56.Christensen K, McGue M, Petersen I, et al. Exceptional longevity does not result in excessive levels of disability. Proc Natl Acad Sci U S A 2008;105:13274–9. 10.1073/pnas.0804931105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mossakowska M, Broczek K, Wieczorowska-Tobis K, et al. Cognitive performance and functional status are the major factors predicting survival of centenarians in Poland. J Gerontol A Biol Sci Med Sci 2014;69:1269–75. 10.1093/gerona/glu003 [DOI] [PubMed] [Google Scholar]
- 58.Arai Y, Inagaki H, Takayama M, et al. Physical independence and mortality at the extreme limit of life span: supercentenarians study in Japan. J Gerontol A Biol Sci Med Sci 2014;69:486–94. 10.1093/gerona/glt146 [DOI] [PubMed] [Google Scholar]
- 59.Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology 1993;43:2412–2. 10.1212/WNL.43.11.2412-a [DOI] [PubMed] [Google Scholar]