Abstract
Objectives
To establish healthcare professionals’ (HCPs) views about clinical roles, and the barriers and enablers to delivery of diabetes care for people with severe mental illness (SMI).
Design
Cross-sectional, postal and online survey.
Setting
Trusts within the National Health Service, mental health and diabetes charities, and professional bodies.
Participants
HCPs who care for people with type 2 diabetes mellitus (T2DM) and/or SMI in the UK.
Primary and secondary outcome measures
The barriers, enablers and experiences of delivering T2DM care for people with SMI, informed by the Theoretical Domains Framework.
Results
Respondents were 273 HCPs, primarily mental health nurses (33.7%) and psychiatrists (32.2%). Only 25% of respondents had received training in managing T2DM in people with SMI. Univariate analysis found that mental health professionals felt responsible for significantly fewer recommended diabetes care standards than physical health professionals (P<0.001). For those seeing diabetes care as part of their role, the significant barriers to its delivery in the multiple regression analyses were a lack of knowledge (P=0.003); a need for training in communication and negotiation skills (P=0.04); a lack of optimism about the health of their clients (P=0.04) and their ability to manage T2DM in people with SMI (P=0.003); the threat of being disciplined (P=0.02); fear of working with people with a mental health condition (P=0.01); a lack of service user engagement (P=0.006); and a need for incentives (P=0.04). The significant enablers were an understanding of the need to tailor treatments (P=0.04) and goals (P=0.02) for people with SMI.
Conclusions
This survey indicates that despite current guidelines, diabetes care in mental health settings remains peripheral. Even when diabetes care is perceived as part of an HCP’s role, various individual and organisational barriers to delivering recommended T2DM care standards to people with SMI are experienced.
Keywords: General Diabetes, Quality In Health Care, Mental Health
Strengths and limitations of this study.
The survey is informed by the Theoretical Domains Framework, a robust theoretical approach to exploring the barriers and enablers to behaviour change, guided by the Medical Research Council Framework for developing complex interventions.
We attempted to recruit participants from a range of sources, including National Health Service Trusts, charities and professional bodies in the UK.
The cross-sectional study design means cause and effect relationships cannot be established.
The survey failed to capture the barriers and enablers to delivering recommended diabetes care to people with severe mental illness by healthcare professionals who did not see this as being part of their clinical role.
Despite the recruitment strategy aiming to target a range of healthcare professionals, general practitioners, diabetologists and physical health nurses are under-represented.
Introduction
Diabetes affects an estimated 415 million people worldwide and accounts for 12% of international health expenditure.1 In the UK, 6.2% of adults are estimated to have diabetes and as in other high-income countries approximately 90% of these have type 2 diabetes mellitus (T2DM).1 There are a range of important risk factors for the development of T2DM, one of which is diagnosis of a severe mental illness (SMI), which is associated with a twofold to threefold increase in the likelihood of developing the condition.2 This increased risk has been attributed to poor diet, obesity and physical inactivity,2 3 the effects of antipsychotic medications,4 and high rates of smoking.5 As a consequence, those with T2DM and SMI die significantly younger than people with T2DM without SMI6 and experience a greater risk of T2DM complications that require specialist treatment.7
These significant health inequalities may in part be explained by variations in diabetes care.8 9 Evidence suggests that people with SMI can be less likely to receive more novel cost-intensive medications,10 retinopathy screening,8 11 foot examinations,8 testing of haemoglobin A1c (HbA1c),8 9 renal checks8 and diabetes education.12 They are also less likely to be hospitalised for diabetes than those with diabetes alone.9 12 The reasons for these disparities in care are wide-ranging. At an individual level the knowledge and skills of mental health nurses to deliver and support diabetes care have been questioned,13–15 and previous theory-driven qualitative research that underpins this study16 found that not knowing how to manage and monitor T2DM and engage and communicate with service users was a significant barrier to delivering recommended care. There is also poor awareness, particularly among mental health professionals, about national and local guidelines for managing T2DM.16 Despite hope and optimism being central to facilitating recovery in people with SMI,17 healthcare professionals have also been found to be despondent about the health of their clients,16 which could impact on how service users are engaged and how care is delivered.
At an organisational level the lack of integrated mental and physical healthcare services has been identified as a barrier to delivering care. Care pathways for people with SMI and diabetes are often complex and fragmented, and healthcare professionals value integrated care and easy access to a multidisciplinary team.16 Despite this, colocation of mental and physical services seems to have had variable impact on the delivery of diabetes care.18 There also appears to be issues in relation to perceived roles and responsibilities. While some research shows confusion and role ambiguity about the responsibility for monitoring and supporting people with T2DM and SMI,13 our previous qualitative research indicates a clear demarcation between the perceived responsibilities of mental health versus primary care and specialist diabetes services.16 While all professional groups felt it was their role to ensure the population was able to access relevant diabetes services, support service users to lead healthier lifestyles, and either monitor or help service users to monitor their blood glucose levels, it was those from primary care and specialist diabetes services that felt that starting new or titrating diabetes treatments in people with SMI was their responsibility. Mental health professionals felt that monitoring medication adherence, blood pressure (BP) and weight and assisting service users to attend their diabetes appointments were their responsibility. This is in opposition to current recommendations that promote shared responsibility between mental and physical healthcare services, for at least the first 12 months or until the person’s condition has stabilised.19–21
Guided by the Medical Research Council recommendations for developing complex interventions22 to create a theoretically and evidence-based intervention, this study aimed to explore a full range of potential barriers and enablers to delivering diabetes care to people with SMI and model these relationships. This will allow for selection of key behaviour change techniques and subsequent incorporation of them in an intervention to improve the care delivered to this population. The purpose of this study was therefore to identify the primary barriers and enablers that affect the practice of primary care, specialist mental health and diabetes specialist clinicians in their management of T2DM in people with SMI. Using these data the intervention components that could overcome these barriers and enhance the enablers can then be identified.
Methods
Participants
A cross-sectional, online survey was conducted between September 2015 and September 2016. The target population was any healthcare professional involved in the care of people with either T2DM and/or SMI. Targeted staff emails, containing a link to the survey, were sent to relevant staff groups by nine National Health Service (NHS) Trusts providing mental health services in the UK. General Practitioners (GP) across the UK were approached via five clinical commissioning groups. Flyers were distributed at eight professional healthcare conferences in the UK and Europe. The Royal Colleges of GPs, Psychiatrists and Nursing, along with the Association of British Clinical Diabetologists, shared the survey via social media and/or via their postal and online newsletters, as did the charity Diabetes UK. Staff were informed that a donation of £2 would be made to a diabetes or mental health charity for each completed survey questionnaire.
The size of the target population is in excess of 100 000, which comprises UK GPs, specialists in general psychiatry and in endocrinology and diabetes mellitus,23 as well as qualified mental health nurses (MHN)24 and diabetes specialist nurses.25
Measures
Demographic factors
Age and gender were collected from participants.
Occupational factors
Data were collected on profession, length of time in current role, length of time qualified, country of practice and site of practice (inpatient or outpatient). Participants were asked the proportion of their patient group who had T2DM, SMI, and comorbid T2DM and SMI, and if they had received training in how to care for people with T2DM and comorbid T2DM and SMI, and if so when and where this was, along with the access they had to any clinical guidelines for the management of T2DM.
Barriers and enablers
A 33-item questionnaire (online supplementary file A) was developed to measure the barriers and enablers to delivering diabetes care to people with SMI, based on qualitative work undertaken by the team.16 Items were generated based on the beliefs reported by healthcare professionals (HCPs) in these interviews, with the most relevant selected through a consensus approach.16 The Theoretical Domains Framework (TDF)26 was used to guide this process to ensure that the survey was able to capture a comprehensive range of factors that could act as barriers or enablers to delivering diabetes care. Items covered each of the 14 domains within the TDF: (1) knowledge, (2) skills, (3) intention, (4) social professional role and identity, (5) social influence, (6) goals, (7) beliefs about consequences, (8) beliefs about capabilities, (9) memory, attention and decision processes, (10) environmental context and resources, (11) behavioural regulation, (12) emotion, (13) reinforcement, and (14) optimism. Responses were on a 5-point Likert scale from 1 (strongly agree) to 5 (strongly disagree). All items were reverse-scored.
bmjopen-2017-019400supp001.pdf (103.1KB, pdf)
Delivery of diabetes care
As part of the 33-item TDF questionnaire, participants were asked if each of the nine key components of diabetes care27 were part of their role. A sum score was calculated in order to measure the degree to which diabetes care was part of a person’s professional role. If participants responded yes to this question, they were then asked: ‘Over the past 12 months, given 10 service users with diabetes and SMI, for how many did you deliver that aspect of care?’
Sample size estimation
To conduct multiple regression analyses with 38 predictor variables, which included the 33 items of the barrier and enablers questionnaire, gender, age, profession, years in role and years in practice, a total of 208 participants were required. Calculation was based on an anticipated medium effect size of f2=0.15, with 80% power and alpha of 0.05.
Analysis
Data were analysed using IBM SPSS Statistics V.23. Differences between the professional groups were explored using analysis of variance. Negative binomial and Poisson regressions were used to assess the predictors of the number of people with SMI for which diabetes guidelines were implemented. Entry of variables into the multiple regression analysis was based on significant univariate associations between the predictor and outcome (P=0.05).
In order to identify the intervention components, otherwise known as behaviour change techniques, which could overcome the identified barriers and enhance the enablers to delivering T2DM to people with SMI, we were informed by matrices that map theoretical domains of the TDF to the appropriate behaviour change techniques.28–30 The experience of the research team, which included clinicians, psychologists and clinician educators, was then used to select the appropriate behaviour change techniques.
Results
Participants
A total of 386 HCPs consented into the study. Across the entire data set there was 27.86% missing data, with complete data for 151 participants (39.11%) and 113 participants (29.27%) with more than 50% missing data. Of the 88 individual variables, all had some degree of missing data. After excluding participants with more than 50% missing data, there was a final sample of 273 (71%). Little’s Missing Completely at Random (MCAR) test was non-significant (χ2=439.564, df=484, P=0.93), and hence data were assumed to be MCAR. Missing data were therefore managed using multiple imputation methods.
A majority of the 273 participants were British (n=179, 66%) and female (n=96, 35%) (table 1). Participants were primarily mental health nurses (n=92, 33.7%) or psychiatrists (n=88, 32.2%). Most were practising in England, in a community setting and had been in their current role for on average 9 years (SD=8.39 years).
Table 1.
Participant descriptors
| Variable | n | % |
| Ethnicity | ||
| British | 179 | 66 |
| Any other white | 29 | 11 |
| Irish | 10 | 3.7 |
| Indian | 10 | 3.7 |
| African | 9 | 3.3 |
| Asian | 5 | 1.8 |
| Pakistani | 5 | 1.8 |
| Any other ethnic group | 5 | 1.8 |
| White and black African | 4 | 1.5 |
| Any other mixed | 4 | 1.5 |
| White and Asian | 3 | 1.1 |
| Caribbean | 3 | 1.1 |
| Bangladeshi | 2 | 0.7 |
| Chinese | 2 | 0.7 |
| White and black Caribbean | 1 | 0.4 |
| Any other black | 1 | 0.4 |
| Profession | ||
| Mental health nurse psychiatrist | 92 | 34 |
| General practitioner | 88 | 32 |
| Diabetes specialist nurse | 24 | 8.8 |
| Practice nurse | 17 | 6.2 |
| Diabetologist | 12 | 4.4 |
| Physical health nurse | 8 | 2.2 |
| Other | 8 | 2.9 |
| District or community nurse | 6 | 2.9 |
| Occupational therapist | 5 | 1.8 |
| Assistant practitioner | 2 | 0.7 |
| Social worker or social | 2 | 0.7 |
| Therapist | 2 | 0.7 |
| Endocrinologist | 1 | 0.4 |
| Dietitian | 1 | 0.4 |
| Student | 1 | 0.4 |
| Audiologist and speech | 1 | 0.4 |
| Therapist | 1 | 0.4 |
| Healthcare assistant | 1 | 0.4 |
| Mental health support worker podiatrist | 1 | 0.4 |
| Country of practice | ||
| England | 236 | 86 |
| Scotland | 4 | 1.5 |
| Wales | 2 | 0.7 |
| Other | 5 | 1.8 |
| Site | ||
| Community | 142 | 52 |
| Inpatient | 72 | 26 |
| Both | 59 | 22 |
Care of T2DM
The proportion of respondents’ case load with T2DM was primarily either less than 5% or greater than 20% (table 2). Approximately 60% of the sample specifically managed diabetes in people with SMI; however, only 25% had received any training in how to do so. Of those who had, this had been within their service or via continuing professional development (CPD), in the past year. There was no significant association between profession and receipt of training (χ2 (1, n=273)=4.72, P=0.32).
Table 2.
Case load and experiences of training
| Variable | n | % |
| Proportion of patients with T2DM | ||
| 5% or less | 76 | 27.8 |
| 10% | 47 | 17.2 |
| 15% | 33 | 12.1 |
| 20% or more | 71 | 26.0 |
| Have you had specific training in assessing and managing T2DM? | ||
| Yes | 147 | 53.8 |
| No | 126 | 46.2 |
| When was the most recent training in T2DM you received? | ||
| In the last year | 65 | 44.23 |
| 1–2 years ago | 26 | 17.69 |
| 2–4 years ago | 20 | 13.61 |
| More than 4 years ago | 36 | 24.49 |
| If you have received training for assessing and/or managing T2DM, where was this? | ||
| Degree | 49 | 33.33 |
| Diploma | 21 | 14.29 |
| Inservice training | 94 | 63.95 |
| CPD | 69 | 46.94 |
| Postgraduate | 2 | 1.36 |
| Other | 15 | 10.20 |
| Do you have access to clinical guidelines for the management of T2DM? | ||
| Yes | 238 | 87.2 |
| No | 35 | 12.8 |
| If yes, which guidelines are these? | ||
| National Institute for Health and Care Excellence | 12 | 5.04 |
| Local trust | 146 | 61.34 |
| WHO | 3 | 1.26 |
| Scottish Intercollegiate Guidelines Network | 5 | 2.10 |
| Trend UK | 1 | 0.42 |
| American Diabetes Association | 5 | 2.10 |
| Research Society for the Study of Diabetes in India | 1 | 0.42 |
| International Diabetes Federation | 1 | 0.42 |
| American Association of Clinical Endocrinologists | 2 | 0.84 |
| European Medicines Agency | 1 | 0.42 |
| Joint British Diabetes Societies | 2 | 0.84 |
| Charity | 2 | 0.84 |
| European Foundation for the Study of Diabetes | 1 | 0.42 |
| Other | 8 | 3.36 |
| Do any of the patients that you provide care for have SMI? | ||
| Yes | 258 | 94.5 |
| No | 15 | 5.5 |
| If yes, what proportion of your patients has SMI? | ||
| 5% or less | 42 | 16.28 |
| 10% | 11 | 4.26 |
| 15% | 11 | 4.26 |
| 20% or more | 162 | 62.79 |
| Have you had specific training in assessing and managing SMI? | ||
| Yes | 209 | 76.6 |
| No | 64 | 23.4 |
| When was the most training in SMI you received? | ||
| In the last year | 137 | 65.55 |
| 1–2 years ago | 19 | 9.09 |
| 2–4 years ago | 19 | 9.09 |
| More than 4 years ago | 34 | 16.27 |
| If you have received training for assessing and/or managing SMI, was this: | ||
| Preregistration | 17 | 8.13 |
| Postregistration | 49 | 23.44 |
| Both | 143 | 68.42 |
| If you have received training for assessing and/or managing SMI, where was this? | ||
| Degree | 110 | 52.63 |
| Diploma | 63 | 30.14 |
| Inservice training | 158 | 75.60 |
| CPD | 128 | 61.24 |
| MRCPsych | 7 | 3.35 |
| Other | 10 | 4.78 |
| Do you provide diabetes care for people who have SMI? | ||
| Yes | 163 | 59.7 |
| No | 110 | 40.3 |
| Have you had specific training in assessing and managing diabetes in people with SMI? | ||
| Yes | 71 | 26 |
| No | 202 | 74 |
| When was the most training in assessing and managing diabetes in people with SMI you received? | ||
| In the last year | 29 | 40.85 |
| 1–2 years ago | 18 | 25.35 |
| 2–4 years ago | 12 | 16.90 |
| More than 4 years ago | 12 | 16.90 |
| If you have received training for assessing and/or managing diabetes in people with SMI, was this: | ||
| Preregistration | 6 | 8.45 |
| Postregistration | 45 | 63.38 |
| Both | 20 | 28.17 |
| If you have received training for assessing and/or managing T2DM in people with SMI, where was this? | ||
| Degree | 10 | 14.08 |
| Diploma | 9 | 12.68 |
| Inservice training | 44 | 61.97 |
| CPD | 36 | 50.70 |
| Other | 5 | 7.04 |
CPD, Continuing Professional Development; SMI, severe mental illness; T2DM, type 2 diabetes mellitus.
Barriers and enablers to delivering diabetes care
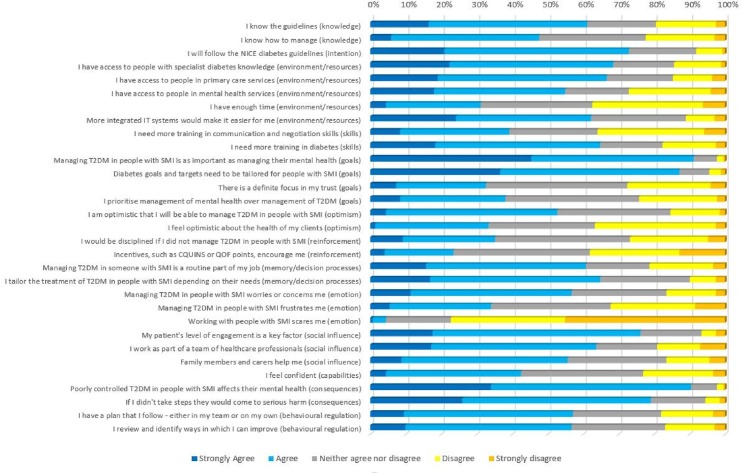
In order to have sufficient numbers to make univariate comparisons between professions, participants were grouped as either (1) mental health nurses (MHN) and support workers, (2) psychiatrists, (3) GPs, (3) other nurses (including practice nurses, diabetes specialist nurses, district or community nurses, healthcare assistants, assistant practitioners), (4) allied and other health professions (AHP), and (5) diabetologists and endocrinologists. Figure 1 displays the responses in relation to each of the 33 items of the TDF questionnaire. Only statistically significant differences between the professions are reported below (online supplementary file B for all analyses).
Figure 1.
Barriers and enablers to delivery of T2DM care in people with SMI (n=273). CQUINS, Commissioning for Quality and Innovation; NICE, National Institute for Health and Care Excellence; QOF, Quality Outcomes Framework; SMI, severe mental illness; T2DM, type 2 diabetes mellitus.
bmjopen-2017-019400supp002.pdf (46.7KB, pdf)
Barriers
Individual factors
Only a third of the sample felt confident in their abilities to manage T2DM in people with SMI and only 42% were optimistic about the health of their clients with T2DM. Although 57% felt that managing T2DM in people with SMI was at times worrying or concerning, only a third felt frustrated and only 4% fearful of working with people with SMI. Physical health nurses were, however, significantly more scared to work with someone with SMI compared with psychiatrists (P=0.002).
Organisational factors
A third of respondents felt they would be disciplined if they did not manage T2DM in someone with SMI. Mental health nurses and support workers were significantly more likely to believe this than both psychiatrists (P=0.002) and GPs (P=0.03).
While 65% reported that they needed more training in diabetes in order to manage T2DM in people with SMI, a third requested more training to improve their communication and negotiation skills. AHP along with MHN and support workers, were more likely to agree that they needed more training in diabetes than GPs (MHN, P=0.12; AHP, P=0.02) and diabetologists or endocrinologists (AHP, P=0.04). Physical health nurses were more likely to request training in communication and negotiation skills compared with psychiatrists (P<0.001).
Only a third of the sample felt that there was a definite focus within their organisation on the management of T2DM in people with SMI. GPs were significantly less likely to agree that this was the case than mental health professionals (MHN, P<0.001; psychiatrists, P=0.01), physical health nurses (P=0.02), and diabetologists or endocrinologists (P=0.03).
Perceived roles and responsibilities varied significantly between professions and the elements of care. Only a quarter of the sample felt that examining sensation and circulation in the feet, agreeing a personalised HbA1c target and offering regular reviews, and referring for retinopathy screening were part of their role (table 3). Approximately half felt that providing general education, monitoring cholesterol and kidney function, and providing personalised advice about diet and exercise were part of their clinical role, while 67% and 83% of participants, respectively, felt that monitoring BP and giving advice about weight management were within their remit. Diabetologists or endocrinologists, GPs and physical health nurses all reported being responsible for significantly more of the nine diabetes care standards than MHN and support workers (P<0.001), psychiatrists (P<0.001), and AHP (P<0.001).
Table 3.
Healthcare professionals’ perceived role in the management of T2DM in people with SMI
| This is part of my clinical role. n (%) |
Average number of service users out of 10, with both type 2 diabetes and SMI that had been…? M (SD) |
|
| Given advice about weight management | 226 (82.78) | 5.84 (3.28) |
| Had their blood pressure monitored | 184 (67.40) | 6.75 (2.92) |
| Given general education about T2DM | 162 (59.34) | 5.58 (3.12) |
| Given personalised advice about diet and nutrition | 159 (58.24) | 5.88 (3.11) |
| Had their cholesterol monitored | 128 (46.87) | 6.77 (2.80) |
| Had their kidney function monitored | 121 (44.32) | 7.39 (2.44) |
| Had their feet examined | 77 (28.21) | 5.45 (3.29) |
| Agreed personalised haemoglobin A1c target | 77 (28.21) | 6.55 (2.85) |
| Referred for retinopathy screening | 68 (24.91) | 4.92 (3.81) |
SMI, severe mental illness; T2DM, type 2 diabetes mellitus.
Enablers
Individual factors
Half of the sample reported that they knew how to manage T2DM in people with SMI, although AHP felt significantly less able to manage T2DM in people with SMI than MHN and support workers (P=0.03), GPs (P=0.04), and diabetologists and endocrinologists (P=0.003). Diabetologists and endocrinologists also felt more able than psychiatrists (P=0.03). While 61% knew the local or national guidelines for managing T2DM, 75% reported that the likelihood of following these guidelines was high. Those working primarily within the physical health domain felt significantly more knowledgeable about these guidelines than MHS and support workers (P≤0.001), psychiatrists (P<0.001), and AHP (P=0.001).
For 61% of the sample, care of T2DM had become a routine part of their role, more so for GPs than psychiatrists (P=0.009) and AHP (P=0.009), and 53% felt optimistic that they would be able to do it in the future. Although 91% believed that managing T2DM in people with SMI is as important as managing their mental health, in practice 38% prioritised the management of mental health over the management of T2DM.
For three-quarters of respondents, being able to engage with service users was a key factor in being able to manage T2DM in this population. For 65% this included being able to tailor treatments, along with the service user’s goals and targets (87%), depending on the client’s needs and abilities. Physical health nurses were more likely to report doing this than psychiatrists (P<0.01). For half of the sample this was aided by having a plan and reviewing their practice to improve the delivery of future care.
Between 80% and 90% reported that poorly controlled T2DM in people with SMI further affected the service user’s mental health, and that if they did not take steps to manage T2DM service users would come to serious harm.
Organisational factors
Less than a quarter of participants felt they were encouraged to manage T2DM in people with SMI by incentives. Both MHN and support workers and GPs were however more likely to agree that incentives encouraged them compared with psychiatrists (MHN, P=0.007; GP, P=0.01). Overall 60% of the sample had sufficient time to manage this population; MHN and support workers were however more likely to agree that this was the case than GPs (P=0.04). Between half and three quarters of respondents felt they had access to other professionals or worked within multidisciplinary teams who could assist them in caring for someone with T2DM and SMI, and this included working with family members or carers. This could be better aided by integrated IT systems for 62% of participants.
Implementation of diabetes care
For those participants who indicated that a diabetes care standard was part of their role (table 3), on average 5 out of every 10 service users with diabetes and SMI were referred for retinopathy screening; 5–6 were offered diabetes education, advice about weight management, diet and nutrition, or had their feet examined; 6–7 had their BP monitored, personalised HbA1c targets agreed or their cholesterol monitored; and 7 out of 10 had their kidney function monitored.
Predictors of implementing diabetes care
Table 4 displays the results of Poisson and negative binomial regression analyses to predict implementation of the nine diabetes care standards. The predictors shown in the table are those that were entered into the multiple regression analyses as they were significantly related to the outcomes in the univariate analysis.
Table 4.
Poisson and negative binomial regressions displaying predictors of diabetes care
| Outcome | Predictors | Hypothesis test | Exp(β) | 95% Wald CI for exp(β) | |||
| Wald χ2 | df | P | Lower | Upper | |||
| Education | (Intercept) | 6.07 | 1.00 | 0.02 | 2.39 | 1.19 | 4.80 |
| I know the guidelines. | 0.38 | 1.00 | 0.90 | 0.99 | 0.90 | 1.10 | |
| I know how to manage. | 5.51 | 1.00 | 0.04 | 1.15 | 1.02 | 1.30 | |
| I will follow the NICE diabetes guidelines. | 1.75 | 1.00 | 0.33 | 1.07 | 0.96 | 1.18 | |
| I have access to people with specialist diabetes knowledge. | 0.48 | 1.00 | 0.76 | 1.02 | 0.94 | 1.10 | |
| I need more training in diabetes. | 1.79 | 1.00 | 0.25 | 0.96 | 0.89 | 1.02 | |
| I am optimistic that I will be able to manage T2DM in people with SMI. | 0.07 | 1.00 | 0.88 | 0.99 | 0.88 | 1.11 | |
| Managing T2DM in someone with SMI is a routine part of my job. | 0.74 | 1.00 | 0.52 | 1.04 | 0.94 | 1.16 | |
| I tailor the treatment of T2DM in people with SMI depending on their needs. | 0.14 | 1.00 | 0.95 | 1.00 | 0.90 | 1.11 | |
| Managing T2DM in people with SMI worries or concerns me. | 1.55 | 1.00 | 0.26 | 0.95 | 0.88 | 1.03 | |
| I feel confident. | 0.62 | 1.00 | 0.64 | 0.96 | 0.84 | 1.10 | |
| I review how I manage T2DM in people with SMI, and identify ways in which I can improve. | 0.24 | 1.00 | 0.86 | 1.01 | 0.92 | 1.11 | |
| How many of the nine diabetes care standard are you responsible for? | 10.52 | 1.00 | 0.00 | 1.06 | 1.02 | 1.10 | |
| Weight | (Intercept) | 16.34 | 1.00 | 0.00 | 2.97 | 1.75 | 5.03 |
| Profession | 24.18 | 4.00 | 0.00 | – | – | – | |
| MHN and support workers | 0.55 | 1.00 | 0.50 | 0.91 | 0.71 | 1.18 | |
| Psychiatrists | 2.86 | 1.00 | 0.09 | 1.24 | 0.97 | 1.59 | |
| GP | 1.15 | 1.00 | 0.33 | 0.86 | 0.65 | 1.14 | |
| Other nurses | 0.35 | 1.00 | 0.56 | 1.08 | 0.84 | 1.38 | |
| I know the guidelines. | 3.21 | 1.00 | 0.10 | 1.08 | 0.99 | 1.17 | |
| I know how to manage. | 1.55 | 1.00 | 0.24 | 1.06 | 0.96 | 1.17 | |
| I have access to people with specialist diabetes knowledge. | 1.99 | 1.00 | 0.26 | 0.96 | 0.90 | 1.02 | |
| I need more training in diabetes. | 1.10 | 1.00 | 0.34 | 0.97 | 0.92 | 1.03 | |
| I feel confident. | 0.21 | 1.00 | 0.80 | 1.01 | 0.92 | 1.11 | |
| I review how I manage T2DM in people with SMI, and identify ways in which I can improve. | 1.84 | 1.00 | 0.32 | 1.05 | 0.97 | 1.13 | |
| How many of the nine diabetes care standard are you responsible for? | 7.00 | 1.00 | 0.02 | 1.04 | 1.01 | 1.07 | |
| Diet | (Intercept) | 11.62 | 1.00 | 0.01 | 2.07 | 1.36 | 3.16 |
| I know the guidelines. | 0.51 | 1.00 | 0.65 | 1.02 | 0.94 | 1.12 | |
| I know how to manage. | 1.26 | 1.00 | 0.41 | 1.05 | 0.95 | 1.16 | |
| I feel optimistic about the health of my clients. | 4.69 | 1.00 | 0.04 | 1.08 | 1.01 | 1.17 | |
| Managing T2DM in someone with SMI is a routine part of my job. | 0.17 | 1.00 | 0.85 | 1.01 | 0.92 | 1.10 | |
| I review how I manage T2DM in people with SMI, and identify ways in which I can improve. | 3.60 | 1.00 | 0.15 | 1.08 | 0.99 | 1.18 | |
| How many of the nine diabetes care standard are you responsible for? | 4.48 | 1.00 | 0.06 | 1.04 | 1.00 | 1.07 | |
| Blood pressure | (Intercept) | 7.47 | 1.00 | 0.01 | 2.43 | 1.28 | 4.58 |
| I will follow the NICE diabetes guidelines. | 0.14 | 1.00 | 0.79 | 1.01 | 0.94 | 1.09 | |
| I have access to people with specialist diabetes knowledge. | 0.33 | 1.00 | 0.79 | 1.01 | 0.94 | 1.09 | |
| I need more training in diabetes. | 4.24 | 1.00 | 0.05 | 0.94 | 0.88 | 1.00 | |
| I am optimistic that I will be able to manage T2DM in people with SMI. | 2.97 | 1.00 | 0.11 | 1.09 | 0.99 | 1.20 | |
| Managing T2DM in someone with SMI is a routine part of my job. | 5.33 | 1.00 | 0.04 | 1.11 | 1.01 | 1.22 | |
| I tailor the treatment of T2DM in people with SMI depending on their needs. | 0.51 | 1.00 | 0.53 | 0.97 | 0.89 | 1.06 | |
| My patient’s level of engagement is a key factor. | 3.14 | 1.00 | 0.09 | 1.07 | 0.99 | 1.16 | |
| I feel confident. | 3.58 | 1.00 | 0.08 | 0.91 | 0.83 | 1.01 | |
| If I didn’t take steps to manage T2DM in people with SMI, they would come to serious harm. | 3.76 | 1.00 | 0.11 | 1.09 | 1.00 | 1.18 | |
| I review how I manage T2DM in people with SMI, and identify ways in which I can improve. | 0.54 | 1.00 | 0.60 | 1.02 | 0.95 | 1.11 | |
| How many of the nine diabetes care standard are you responsible for? | 4.36 | 1.00 | 0.06 | 1.03 | 1.00 | 1.06 | |
| Feet | (Intercept) | 0.30 | 1.00 | 0.79 | 0.87 | 0.29 | 2.59 |
| I need more training in communication and negotiation skills. | 4.98 | 1.00 | 0.05 | 1.11 | 1.01 | 1.22 | |
| Diabetes goals and targets need to be tailored for people with SMI. | 0.92 | 1.00 | 0.42 | 1.08 | 0.91 | 1.29 | |
| My patient’s level of engagement is a key factor. | 8.45 | 1.00 | 0.01 | 1.21 | 1.06 | 1.38 | |
| How many of the nine diabetes care standard are you responsible for? | 7.44 | 1.00 | 0.02 | 1.09 | 1.02 | 1.16 | |
| Profession | 9.36 | 4.00 | 0.08 | – | – | – | |
| Mental health nurses and support workers | 4.69 | 1.00 | 0.07 | 0.70 | 0.50 | 0.98 | |
| Psychiatrists | 4.73 | 1.00 | 0.04 | 0.68 | 0.47 | 0.97 | |
| GP | 5.36 | 1.00 | 0.03 | 0.62 | 0.42 | 0.93 | |
| Other nurses | 1.30 | 1.00 | 0.27 | 0.85 | 0.64 | 1.13 | |
| Cholesterol | (Intercept) | 62.95 | 1.00 | 0.00 | 4.83 | 3.27 | 7.12 |
| Working with people with SMI scares me. | 6.97 | 1.00 | 0.01 | 0.90 | 0.83 | 0.97 | |
| My patient’s level of engagement is a key factor. | 8.68 | 1.00 | 0.00 | 1.14 | 1.05 | 1.25 | |
| HbA1c | (Intercept) | 6.57 | 1.00 | 0.01 | 2.42 | 1.23 | 4.77 |
| Diabetes goals and targets need to be tailored for people with SMI. | 1.57 | 1.00 | 0.23 | 1.08 | 0.96 | 1.22 | |
| I am optimistic that I will be able to manage T2DM in people with SMI. | 9.16 | 1.00 | 0.00 | 1.20 | 1.06 | 1.34 | |
| Retinopathy | (Intercept) | 0.34 | 1.00 | 0.59 | 1.79 | 0.24 | 13.35 |
| Diabetes goals and targets need to be tailored for people with SMI. | 5.55 | 1.00 | 0.03 | 1.62 | 1.08 | 2.42 | |
| I would be disciplined if I did not manage T2DM in people with SMI. | 6.14 | 1.00 | 0.02 | 0.71 | 0.53 | 0.93 | |
| Incentives, such as CQUINS or QOF points, encourage me. | 4.43 | 1.00 | 0.04 | 0.77 | 0.60 | 0.98 | |
| Family members and carers help me. | 2.05 | 1.00 | 0.16 | 1.22 | 0.93 | 1.60 | |
CQUINS, Commissioning for Quality and Innovation; GP, general practitioner; HbA1c, haemoglobin A1c; MHN, Mental Health Nurses; NICE, National Institute for Health and Care Excellence; QOF, Quality Outcomes Framework; SMI, severe mental illness; T2DM, type 2 diabetes mellitus.
Figures in bold indicate statistically significant predictors.
Education
The significant independent predictors of the number of people who were given general education about T2DM were knowledge about how to manage T2DM in people with SMI (P=0.04) and the degree to which diabetes care was part of their role (P<0.001). For every additional element of diabetes care that was part of a person’s role, there was a 6% (95% CI 1.02 to 1.10) increase in the number of people referred for diabetes education (P=0.003). For every point increase in knowledge about managing diabetes, there was a 15% (95% CI 1.02 to 1.30) increase in the number of people referred for diabetes education (P=0.04).
Weight
The significant independent predictors of the number of people who had advice about weight management were the degree to which diabetes care was part of their role (P=0.02) and profession (P<0.001). For every additional element of diabetes care that was part of their role, there was a 4% (95% CI 1.01 to 1.07) increase in the number of people advised about weight management. Psychiatrists reported advising more people about weight management than both MHN and support workers (Mean difference (MD)=1.78, SE=0.44) and GPs (MD=2.06, SE=0.64).
Diet and nutrition
Optimism about the health of their clients (P=0.04) was the only independent predictor of the number of people who were advised about diet and nutrition. For every point increase in optimism about the health of their clients, there was an 8% (95% CI 1.01 to 1.17) increase in the number of people given personalised advice about diet and nutrition.
Monitoring BP
The degree to which diabetes care was a routine part of their role (P=0.04) was the only independent predictor of the number of people who had their BP monitored. For every point increase in the routine nature of diabetes care in a respondent’s role, there was an 11% (95% CI 1.02 to 1.22) increase in the number of people given personalised advice about diet and nutrition.
Examining feet
The degree to which diabetes care was part of their role (P=0.02) and the level of engagement from the service user (P=0.01) and profession (psychiatrists, P=0.04; GPs, P=0.03, compared with AHP) were significant independent predictors of the number of people who had their feet examined. For every additional element of diabetes care that was part of their role, there was a 9% (95% CI 1.02 to 1.16) increase in the number of people who had their feet checked. For every point increase in engagement from the service user, there was a 21% (95% CI 1.06 to 1.38) increase in the number of foot checks.
Agreeing a personalised HbA1c target and providing ongoing review
How optimistic a person was in their ability to manage T2DM in people with SMI (P<0.001) was the only independent predictor of the number of service users with whom HbA1c targets were set and ongoing reviews provided. For every point increase in how optimistic a person was in their ability to manage T2DM in people with SMI, there was a 20% (95% CI 1.07 to 1.34) increase in the number of service users with whom HbA1c targets were set and ongoing reviews provided.
Monitoring cholesterol
The level of engagement from the service user (P<0.001) and fear of working with someone with SMI (P=0.01) were the independent predictors of the number of people who had their cholesterol monitored. For every point increase in enagagement from the service user, there was a 14% (95% CI 1.05 to 1.25) increase in the number of people whose cholesterol was monitored, and for every point increase in fear there was a 10% (95% CI 0.83 to 0.97) decrease in the number of cholesterol checks performed.
Monitoring kidney function
There were no significant univariate associations between the number of people in whom kidney function was monitored and any of the demographic, occupational or TDF factors.
Referring for retinopathy screening
The belief that goals and targets need to be tailored for people with SMI (P=0.03), that they would be disciplined for not managing T2DM in people with SMI (P=0.02) and the need for incentives to encourage them to manage T2DM in this population (P=0.04) were the significant independent predictors of the number of people referred for retinopathy screening. For every point increase in the belief that goals and targets need to be tailored for people with SMI, there was a 62% (95% CI 1.08 to 2.42) increase in the number of people who were referred for retinopathy screening. For every point increase in the belief they would be disciplined for not managing T2DM in people with SMI or that incentives would encourage them to manage T2DM in this population, there was a 29% (95% CI 0.54 to 0.93) and a 23% (95% CI, 0.60 to 0.98) decrease, respectively, in the number of people referred for retinopathy screening.
Intervention components
Table 5 highlights the TDF domains which were found to be either barriers or enablers to delivering T2DM care to people with SMI, along with the associated behaviour change techniques.28–30 The techniques highlighted in column 2 are those intervention components selected as most appropriate for addressing the barrier or enabler identified in the study.
Table 5.
Mapping of relevant Theoretical Domains Framework (TDF) domains on intervention components
| Relevant TDF domains | Behaviour change techniques |
| Knowledge | Information regarding behaviour, outcome |
| Health consequences | |
| Biofeedback | |
| Antecedents | |
| Feedback on the behaviour | |
| Social professional role and identity | Social process of encouragement, pressure and support |
| Optimism | Verbal persuasion to boost self-efficacy |
| Focus on past success | |
| Social influence | Social process of encouragement, pressure and support |
| Modelling/demonstration of the behaviour by others | |
| Social comparison | |
| Vicarious reinforcement | |
| Restructuring the social environment | |
| Identification of self as a role model | |
| Social reward | |
| Emotion | Stress management |
| Coping skills | |
| Reduce negative emotions | |
| Emotional consequences | |
| Self-assessment of affective consequences | |
| Social support (emotional) | |
| Goals | Goal/target specified: behaviour or outcome |
| Contract | |
| Rewards, incentives (including self-evaluation) | |
| Graded task, starting with easy tasks | |
| Increasing skills: problem-solving, decision-making, goal-setting | |
| Social process of encouragement, pressure and support | |
| Persuasive communication | |
| Information regarding behaviour, outcome | |
| Motivational interviewing | |
| Review of outcome goal(s) | |
| Review of behaviour goal(s) | |
| Action planning (including implementation intentions) | |
| Reinforcement | Threat |
| Self-reward | |
| Differential reinforcement | |
| Incentive | |
| Thinning | |
| Negative reinforcement | |
| Shaping | |
| Counterconditioning | |
| Discrimination training | |
| Material reward | |
| Social reward | |
| Non-specific reward | |
| Response cost | |
| Anticipation of future rewards or removal of punishment | |
| Punishment | |
| Extinction | |
| Classical conditioning | |
| Counterconditioning |
Discussion
We found that delivery of diabetes care for people with SMI is influenced by a range of individual and organisational factors. Although there were clear differences in the extent of involvement, mental health professionals noted active engagement in many of the aspects of diabetes care, as identified elsewhere in the literature.13–15 Confirming our qualitative findings,16 however, specialist mental health clinicians reported being responsible for fewer diabetes care standards than primary care and specialist diabetes clinicians. This contests the idea that there is confusion and role ambiguity about the responsibility for monitoring and supporting T2DM in SMI.13 In fact this survey indicates clear boundaries, but when diabetes management is perceived to be a greater part of a person’s role, more service users are treated according to recommended standards. This clearly reflects conflict between the shared care approach,20 21 which promotes mental health professionals broadening their delivery to address physical and mental health.19 This indicates a need for NHS Trusts to define roles and responsibilities more clearly. This is particularly relevant given that only a third of the sample felt that there was a definite focus in their trust on the management of T2DM in people with SMI.
Although 54% of respondents had received training in diabetes, only a quarter had been trained in how to manage the condition in people with SMI, and this figure did not differ between the professions. Despite receiving training, those working in mental health settings felt less knowledgeable about the guidelines for T2DM and had a desire for more training in how to manage the condition. This supports the findings of studies conducted in other UK mental health trusts13–15 31 32 and theory-driven qualitative work that formed the basis of this study.16 Importantly, this lack of knowledge and skills meant that HCPs treated fewer service users according to recommended diabetes care standards. Evaluations of diabetes training and educational packages for mental health clinicians are limited. Improvements in understanding and knowledge of diabetes have been reported; however, these findings are based on a small-scale, single group study consisting of primarily mental health students and hence fail to explore its impact on practice.33 Any such programme will need to consider the barriers to attending training of this nature, including a lack of management support, staff shortages, the discretionary nature of attending and lack of funding,34 along with the challenges of using psychosocial interventions to change practice.35–37
Being able to communicate and engage with service users was identified as an important facilitator in delivering effective diabetes care. As opposed to those working in mental health settings, primary care and diabetes specialists felt they needed more training in communication and negotiation skills in order for them to be able to motivate their clients and deliver recommended care. Difficulties motivating service users with diabetes to self-manage have been identified elsewhere in the literature13 32 38 and present an ongoing challenge for interventions aimed at changing the behaviour of service users with T2DM.39 Respondents stressed the importance of tailoring diabetes treatment, along with any goals and targets, to the needs and abilities of the service user. Mental health staff report experiencing difficulties engaging service users in their diabetes care, due to limitations in cognitive and executive functioning.32 38 Together this highlights the importance of training healthcare professionals to also be able to identify suitable times within the service users’ journey when they may need more support in order for them to self-manage effectively. The challenges of communicating and engaging service users in their care may also be precipitated or be a consequence of the fear some healthcare professionals experience about working with someone with SMI. This further supports research that shows some clinicians experience discomfort in dealing with people with mental illness, leading to physical diagnoses often being missed.40
Only a third of the sample were optimistic about the health of their clients with T2DM, and a majority of respondents lacked optimism about their ability to manage T2DM in people with SMI. This led to fewer service users receiving the recommended diabetes care standards. Given the importance of hope and optimism in the process of personal recovery in mental health,17 this could be an important focus for interventions aimed at improving diabetes care and outcomes for service users, with the potential for wider benefits. The powerful position that healthcare professionals hold as hope-inspiring role models17 can either enhance or diminish the hope of service users.41 42 This is particularly important considering that practitioner hope has been found to influence the outcomes of therapy over and above client hope43 and that cultivating hope in the context of T2DM is also associated with increased adherence.44
In line with the findings of our qualitative work,16 a third of respondents felt that they would be disciplined if they did not manage diabetes in people with SMI and approximately a quarter felt that incentives would encourage them. Despite this, the threat of being disciplined and need for incentives appeared to have a counterintuitive effect in the multiple regression analyses. The greater the perceived threat of being disciplined and a stronger belief that incentives would encourage them to manage diabetes, the fewer service users received recommended diabetes care. This suggests that the perceived threat of being disciplined and possibly the discordance between desire and receipt of incentives was having a paralysing effect on practice. Blame and punishment are felt by healthcare professionals to be part of health service culture, particularly when someone is involved in an error, near miss or incident.45 This however can lead to disempowerment, disunity and a lack of compassion in the workforce.46 Rather than allowing people to experiment without fear of reprisal and view errors as learning opportunities,46 the workforce are fearful of personal accountability, litigation and complaints.47 Although participants felt that incentives would improve their practice, this study and the evidence for pay-for-performance systems, such as the Quality Outcomes Framework (QOF), in changing HCP behaviour are limited, and there is insufficient evidence for their impact on patient health outcomes.48
Taken together, our findings suggest that a number of strategies could be implemented to improve the care offered to people with diabetes and SMI, and as a consequence address the inequalities experienced by this population. These techniques include increasing healthcare professionals’ knowledge about the guidelines for managing T2DM in people with SMI, increasing awareness of their role and responsibilities towards this patient group, boosting self-efficacy for addressing the needs of these clients, modelling or demonstrating how healthcare professionals can work with clients who are less engaged in their diabetes care, reducing fear of working with people with SMI, increasing skills in being able to tailor goals and targets to the needs of the individual service user, and eradicating fear of being disciplined. Identification of these barriers and enablers and subsequent behaviour change techniques now allows us to move towards development, feasibility testing and piloting of a new approach to delivering care.22
The study had a number of limitations. The need to adjust P values in studies using multiple outcome measures has been debated widely in the literature.49 The number of outcomes measures considered as a family-wise hypothesis has however not been defined, and although by not adjusting this may increase the likelihood of a type I error, adjusting would increase the chance of type II errors, which are no less important. We therefore acknowledge that some of the findings of this study may have been due to chance. As with any online survey, there are concerns about the representativeness of the sample.50 There was a bias in responses towards those who were likely to be more interested in the topic, with significantly more responses from those working within mental health settings. This raises a broader question about whether SMI is a priority or issue for diabetes specialists. Due to the online recruitment methods, it was not possible to estimate the response rate. In comparison with the target population, this sample represents only 0.3% of the population, therefore raising concerns about the generalisability of the findings to the broader population. Despite the recruitment strategy aiming to target a range of healthcare professionals, GPs, diabetologists and physical health nurses are under-represented. The data from this study focused on predicting delivery of diabetes care to people with SMI by healthcare professionals who stated this was part of their role. It may have however been the case that elements of diabetes care could have been undertaken by a professional even when it was not explicitly part of their job. Our results are also only a snapshot of the experiences and beliefs of HCPs; as the care of diabetes in people with SMI becomes of greater priority and services begin to develop, these views may change.
Supplementary Material
Footnotes
Contributors: HM: made a substantial contribution to the conception and design of the study, data analysis and interpretation of the data, created the first draft of the manuscript, approved the final version, and agreed to be accountable for all aspects of the work. FL-G: made a substantial contribution to the conception and design of the study, collection and interpretation of the data, commented on drafts of the manuscript, approved the final version, and agreed to be accountable for all aspects of the work. MH, AS, JC, JJ, CF and KM all made a substantial contribution to the conception and design of the study, interpretation of the data, commented on drafts of the manuscript, approved the final version, and agreed to be accountable for all aspects of the work.
Funding: This work was supported by Barts Charity, grant number 477/2314.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: The study was approved by the Wales Research Ethics Committee 7 (ref 15/WA/0310).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: There are no other additional unpublished data to be shared.
Correction notice: This article has been corrected since it first published. The affiliation ‘Community Health Newham, East London NHS Foundation Trust, London, UK’ is now associated with author Kathleen Mulligan instead of Chris Flood.
References
- 1.International Diabetes Federation. International Diabetes Federation Diabetes Atlas. 7th edn, 2015. [Google Scholar]
- 2.Osborn DP, Wright CA, Levy G, et al. Relative risk of diabetes, dyslipidaemia, hypertension and the metabolic syndrome in people with severe mental illnesses: systematic review and metaanalysis. BMC Psychiatry 2008;8:84 10.1186/1471-244X-8-84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Hert M, Dekker JM, Wood D, et al. Cardiovascular disease and diabetes in people with severe mental illness position statement from the European Psychiatric Association (EPA), supported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC). Eur Psychiatry 2009;24:412–24. 10.1016/j.eurpsy.2009.01.005 [DOI] [PubMed] [Google Scholar]
- 4.Alvarez-Jiménez M, Hetrick SE, González-Blanch C, et al. Non-pharmacological management of antipsychotic-induced weight gain: systematic review and meta-analysis of randomised controlled trials. Br J Psychiatry 2008;193:101–7. 10.1192/bjp.bp.107.042853 [DOI] [PubMed] [Google Scholar]
- 5.Lawrence D, Mitrou F, Zubrick SR. Smoking and mental illness: results from population surveys in Australia and the United States. BMC Public Health 2009;9:285 10.1186/1471-2458-9-285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vinogradova Y, Coupland C, Hippisley-Cox J, et al. Effects of severe mental illness on survival of people with diabetes. Br J Psychiatry 2010;197:272–7. 10.1192/bjp.bp.109.074674 [DOI] [PubMed] [Google Scholar]
- 7.Becker T, Hux J. Risk of acute complications of diabetes among people with schizophrenia in Ontario, Canada. Diabetes Care 2011;34:398–402. 10.2337/dc10-1139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McGinty EE, Baller J, Azrin ST, et al. Quality of medical care for persons with serious mental illness: a comprehensive review. Schizophr Res 2015;165:227–35. 10.1016/j.schres.2015.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scott D, Platania-Phung C, Happell B. Quality of care for cardiovascular disease and diabetes amongst individuals with serious mental illness and those using antipsychotic medications. J Healthc Qual 2012;34:15–21. 10.1111/j.1945-1474.2011.00155.x [DOI] [PubMed] [Google Scholar]
- 10.Rathmann W, Pscherer S, Konrad M, et al. Diabetes treatment in people with type 2 diabetes and schizophrenia: Retrospective primary care database analyses. Prim Care Diabetes 2016;10:36–40. 10.1016/j.pcd.2015.04.001 [DOI] [PubMed] [Google Scholar]
- 11.Mathur R, Hull SA, Boomla K, et al. Ethnic differences in primary care management of diabetes and cardiovascular disease in people with serious mental illness. Br J Gen Pract 2012;62:e582–8. 10.3399/bjgp12X653642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mitchell AJ, Malone D, Doebbeling CC. Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. Br J Psychiatry 2009;194:491–9. 10.1192/bjp.bp.107.045732 [DOI] [PubMed] [Google Scholar]
- 13.Robson D, Haddad M. Mental health nurses' attitudes towards the physical health care of people with severe and enduring mental illness: the development of a measurement tool. Int J Nurs Stud 2012;49:72–83. 10.1016/j.ijnurstu.2011.07.011 [DOI] [PubMed] [Google Scholar]
- 14.Nash M. Mental health nurses' diabetes care skills - a training needs analysis. Br J Nurs 2009;18:626–30. 10.12968/bjon.2009.18.10.42472 [DOI] [PubMed] [Google Scholar]
- 15.Howard L, Gamble C. Supporting mental health nurses to address the physical health needs of people with serious mental illness in acute inpatient care settings. J Psychiatr Ment Health Nurs 2011;18:105–12. 10.1111/j.1365-2850.2010.01642.x [DOI] [PubMed] [Google Scholar]
- 16.McBain H, Mulligan K, Lamontagne-Godwin F, et al. Implementation of recommended type 2 diabetes care for people with severe mental illness – a qualitative exploration with healthcare professionals. BMC Psychiatry 2016;16:222 10.1186/s12888-016-0942-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leamy M, Bird V, Le Boutillier C, et al. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry 2011;199:445–52. 10.1192/bjp.bp.110.083733 [DOI] [PubMed] [Google Scholar]
- 18.Kilbourne AM, Pirraglia PA, Lai Z, et al. Quality of general medical care among patients with serious mental illness: does colocation of services matter? Psychiatr Serv 2011;62:922–8. 10.1176/ps.62.8.pss6208_0922 [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization. Mental Health Action Plan 2013–2020. 2013.
- 20.NHS Diabetes. Commissioning mental health and diabetes services. 2011.
- 21.National Institute for Health and Care Excellence. Psychosis and schizophrenia in adults: prevention and management. 2014. [PubMed]
- 22.Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.General Medical Council. List of Registered Medical Practitioners - statistics. 2017.
- 24.NHS Digital. Provisional NHS Hospital & Community Health Service (HCHS) monthly workforce statistics. 2017.
- 25.Gosden C, James J, Anderson U, et al. UK workforce survey of DSNs and nurse consultants. J Diabetes Nurs 2010;14:250–7. [Google Scholar]
- 26.Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7:37 10.1186/1748-5908-7-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Institute for Health and Care Excellence. Diabetes in adults (QS6). 2011.
- 28.Michie S, Atkins L, West R. The behaviour change wheel: a guide to designing interventions. Great Britain: Silverback Publishing, 2014. [Google Scholar]
- 29.Michie S, Johnston M, Francis J, et al. From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol 2008;57:660–80. 10.1111/j.1464-0597.2008.00341.x [DOI] [Google Scholar]
- 30.Cane J, Richardson M, Johnston M, et al. From lists of behaviour change techniques (BCTs) to structured hierarchies: comparison of two methods of developing a hierarchy of BCTs. Br J Health Psychol 2015;20:130–50. 10.1111/bjhp.12102 [DOI] [PubMed] [Google Scholar]
- 31.Ward D. Improving physical health care in a mental health trust. Nurs Times 2005;101:32–3. [PubMed] [Google Scholar]
- 32.Hultsjö S. Mental healthcare staff’s knowledge and experiences of diabetes care for persons with psychosis–a qualitative interview study. Prim Health Care Res Dev 2013;14:281–92. 10.1017/S1463423612000321 [DOI] [PubMed] [Google Scholar]
- 33.Hemingway S, Trotter F, Stephenson J, et al. Diabetes: increasing the knowledge base of mental health nurses. Br J Nurs 2013;22:991–6. 10.12968/bjon.2013.22.17.991 [DOI] [PubMed] [Google Scholar]
- 34.Nash M. Physical care skills: a training needs analysis of inpatient and community mental health nurses. Mental Health Practice 2005;9:20–3. 10.7748/mhp2005.12.9.4.20.c1896 [DOI] [Google Scholar]
- 35.Brooker C, Brabban A. Effective training in psychosocial interventions for work with people with serious mental health problems. Mental Health Rev 2006;11:7–14. 10.1108/13619322200600014 [DOI] [Google Scholar]
- 36.Stanbridge R, Burbach F. Enhancing working partnerships with carers and families: a strategy and associated training programme. Mental Health Rev 2004;9:32–7. 10.1108/13619322200400041 [DOI] [Google Scholar]
- 37.Slade M, Bird V, Clarke E, et al. Supporting recovery in patients with psychosis through care by community-based adult mental health teams (REFOCUS): a multisite, cluster, randomised, controlled trial. Lancet Psychiatry 2015;2:503–14. 10.1016/S2215-0366(15)00086-3 [DOI] [PubMed] [Google Scholar]
- 38.Hultsjö S, Hjelm K. Community health-care staff’s experiences of support to prevent type 2 diabetes among people with psychosis: an interview study with health staff. Int J Ment Health Nurs 2012;21:480–9. 10.1111/j.1447-0349.2012.00820.x [DOI] [PubMed] [Google Scholar]
- 39.McBain H, Mulligan K, Haddad M, et al. Self management interventions for type 2 diabetes in adult people with severe mental illness. Cochrane Database Syst Rev 2016;4:CD011361 10.1002/14651858.CD011361.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jones S, Howard L, Thornicroft G. ‘Diagnostic overshadowing’: worse physical health care for people with mental illness. Acta Psychiatr Scand 2008;118:169–71. 10.1111/j.1600-0447.2008.01211.x [DOI] [PubMed] [Google Scholar]
- 41.Hobbs M, Baker M. Hope for recovery - how clinicians may facilitate this in their work. J Ment Health 2012;21:144–53. 10.3109/09638237.2011.648345 [DOI] [PubMed] [Google Scholar]
- 42.Niebieszczanski RJ, Dent H, McGowan A. ‘Your personality is the intervention’: a grounded theory of mental health nurses’ beliefs about hope and experiences of fostering hope within a secure setting. J Forens Psychiatry Psychol 2016;27:419–42. 10.1080/14789949.2015.1134626 [DOI] [Google Scholar]
- 43.Coppock TE, Owen JJ, Zagarskas E, et al. The relationship between therapist and client hope with therapy outcomes. Psychother Res 2010;20:619–26. 10.1080/10503307.2010.497508 [DOI] [PubMed] [Google Scholar]
- 44.Makarem SC, Smith MF, Mudambi SM, et al. Why people do not always follow the doctor’s orders: the role of hope and perceived control. J Consum Aff 2014;48:457–85. 10.1111/joca.12044 [DOI] [Google Scholar]
- 45.Dixon-Woods M, Baker R, Charles K, et al. Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;23:106–15. 10.1136/bmjqs-2013-001947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.de Zulueta PC. Developing compassionate leadership in health care: an integrative review. J Healthc Leadersh 2016;8:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goodman B. Risk, rationality and learning for compassionate care; the link between management practices and the ‘lifeworld’ of nursing. Nurse Educ Today 2014;34:1265–8. 10.1016/j.nedt.2014.04.009 [DOI] [PubMed] [Google Scholar]
- 48.Mendelson A, Kondo K, Damberg C, et al. The effects of pay-for-performance programs on health, health care use, and processes of care: a Systematic Review. Ann Intern Med 2017;166:341–53. 10.7326/M16-1881 [DOI] [PubMed] [Google Scholar]
- 49.Feise RJ. Do multiple outcome measures require p-value adjustment? BMC Med Res Methodol 2002;2:8 10.1186/1471-2288-2-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Whitehead LC. Methodological and ethical issues in Internet-mediated research in the field of health: an integrated review of the literature. Soc Sci Med 2007;65:782–91. 10.1016/j.socscimed.2007.03.005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-019400supp001.pdf (103.1KB, pdf)
bmjopen-2017-019400supp002.pdf (46.7KB, pdf)