Abstract
Objectives
Obesity management is an important issue for the international primary care community. This scoping review examines the literature describing the role of the family doctor in managing adults with obesity. The methods were prospectively published and followed Joanna Briggs Institute methodology.
Setting
Primary care. Adult patients.
Included papers
Peer-reviewed and grey literature with the keywords obesity, primary care and family doctors. All literature published up to September 2015. 3294 non-duplicate papers were identified and 225 articles included after full-text review.
Primary and secondary outcome measures
Data were extracted on the family doctors’ involvement in different aspects of management, and whether whole person and person-centred care were explicitly mentioned.
Results
110 papers described interventions in primary care and family doctors were always involved in diagnosing obesity and often in recruitment of participants. A clear description of the provider involved in an intervention was often lacking. It was difficult to determine if interventions took account of whole person and person-centredness. Most opinion papers and clinical overviews described an extensive role for the family doctor in management; in contrast, research on current practices depicted obesity as undermanaged by family doctors. International guidelines varied in their description of the role of the family doctor with a more extensive role suggested by guidelines from family medicine organisations.
Conclusions
There is a disconnect between how family doctors are involved in primary care interventions, the message in clinical overviews and opinion papers, and observed current practice of family doctors. The role of family doctors in international guidelines for obesity may reflect the strength of primary care in the originating health system. Reporting of primary care interventions could be improved by enhanced descriptions of the providers involved and explanation of how the pillars of primary care are used in intervention development.
Keywords: preventive medicine, primary care
Strengths and limitations of this study.
The protocol for this scoping review was prospectively published and was based onthe Joanna Briggs Institute (JBI) scoping review methodology.
All types of articles have been included in this scoping review including international guidelines from relevant family medicine colleges.
Feedback was obtained from three groups of interested clinical and academic colleagues in Australia and internationally as per the JBI methodology for a scoping review.
Articles in languages other than English were excluded from the review and therefore the results are not representative of non-English-speaking countries.
Introduction
Obesity is recognised as a risk factor for the development of chronic disease and is often comorbid with diseases such as diabetes, osteoarthritis, cardiovascular disease and depression.1 As such, obesity is a condition that is commonly associated with a larger set of health issues encountered by an individual. As in all cases of multimorbidity, a person’s care will benefit from the coordinated and continuous care offered by an interdisciplinary team in primary care.2 3 By exploring the role of the family doctor, we are not questioning the importance of team-based care. Instead, we aim to explore how family doctors are represented in the broad literature to further understand the profession’s role. This understanding is important when interdisciplinary teams are not accessible (eg, rural location), affordable (eg, health insurance differentials) or part of the patient’s preference for care.4–6 Thus, the literature that focuses on the management of adults with obesity by the family doctor is important to understand.
With the rising numbers of adults living with obesity and related chronic diseases, there is an increasing demand from health systems for primary care, and family doctors in particular, to identify and manage this as a chronic condition.6 With this changing landscape, it was anticipated that the academic literature would explore the effectiveness of primary care, as well as the involvement of different practitioners in obesity management. However, our initial explorations into this literature found a lack of clarity in this area. A scoping review was chosen to explore emerging patterns, and gaps, in the literature based on the role of the family doctor in managing adults with obesity.
The term used to describe a family doctor varies internationally, and includes general practitioner and family physician. The term ‘primary care physician’, which stems from the USA, includes paediatricians, obstetricians and internists. In this review, we define ‘family doctor’ as a physician with specialist training in primary care who practises in the community, as an expert generalist.
Different practitioners will bring varying strengths and limitations to any intervention and it is important for family doctors to understand what skills they offer in the setting of obesity management. The importance of understanding provider role is demonstrated in the methodology of critical realism where realist evaluation acknowledges the importance of context of any intervention.7 Translating rigorous scientific trials into policy and practice is challenging and realist evaluation is an increasingly used tool to inform effective translation of evidence.8 Part of understanding context in the realist evaluation is knowing the type of provider, and their experience level, in delivering an intervention. This scoping review provides an overview of the role of the family doctor in interventions, clinical overviews and opinions, observed practice and clinical guidelines.
The pillars of primary care—being the first point of health system entry, delivering continuous, whole person (ie, concerned with every body system and the mind) and person-centred care (ie, elucidates comorbidities, social circumstances, and maintains the beliefs and values of the person at the heart of management for all health problems in all patients in all stages)—are well established.9 Other tiers of the health system may provide some, but not all, of the four pillars. Each of these concepts needs to be present in the management of a patient to gain the full benefits of primary care.10 Patient management that is not based around these four pillars is unlikely to reap the benefits of coordinated, comprehensive, expert generalist care.11–13
This scoping review aims to examine and map the current research base, and broader literature, for the role of the family doctor in managing adults with obesity.
The objectives, inclusion criteria and methods of analysis for this review were specified in advance and documented in a protocol.14 The scoping review questions we aimed to answer were:
What supporting evidence (both primary and secondary) do we have for the role family doctors play in obesity management for adults in primary care?
What is the role of the family doctor in managing obesity as a primary risk as supported by the evidence base?
What do primary care guidelines say about the role of the family doctor? What do peak bodies (ie, advocacy group) say about the role of the family doctor? Are these both in line with what is conveyed by current research?
Methods
The complete methods were prospectively published in a protocol.14 Our search strategy included all literature published until September 2015. A preliminary search for existing scoping reviews did not find any with the same concept and topic (databases searched JBISRIR, Cochrane Database of Systematic Reviews, CINAHL, PubMed, EPPI). Manuscripts were included when they involved adults (18+ years) with a body mass index (BMI) of greater than 25 (overweight or obesity), any involvement of a primary care doctor/physician, a primary care setting and inclusion of obesity management (online supplementary file 1). Contrary to our outlined protocol, we excluded papers in languages other than English, including those with an English abstract, as we could not perform data extraction adequately on these papers. In addition to this search strategy, we specifically sought relevant clinical guidelines from countries with strong involvement in the World Organization of National Colleges, Academies and Academic Associations of General Practitioners/Family Physicians (Australia, UK, USA, New Zealand, the Netherlands, Denmark, Finland, Estonia, Slovenia, Belgium, Spain and Portugal). We explored the family medicine college web sites from these countries and contacted the colleges via email when guidelines were not accessible.
bmjopen-2017-019367supp001.pdf (235.1KB, pdf)
This scoping review was purposefully restricted to obesity management of adults in primary care. As suggested in the Joanna Briggs Institute methodology, the scope has to take account of feasibility while maintaining a broad and comprehensive approach. By restricting the scoping review to obesity, we were able to extract more detail about the family doctor’s role than if we had included articles with a main focus on a specific non-communicable disease (eg, diabetes, heart disease). For this same reason, we did not include articles that were only describing nutrition care or physical activity advice unless they were specifically in relation to care of a patient with obesity. Due to the differences in the management of obesity in children and adolescents these population groups were not included in this review.
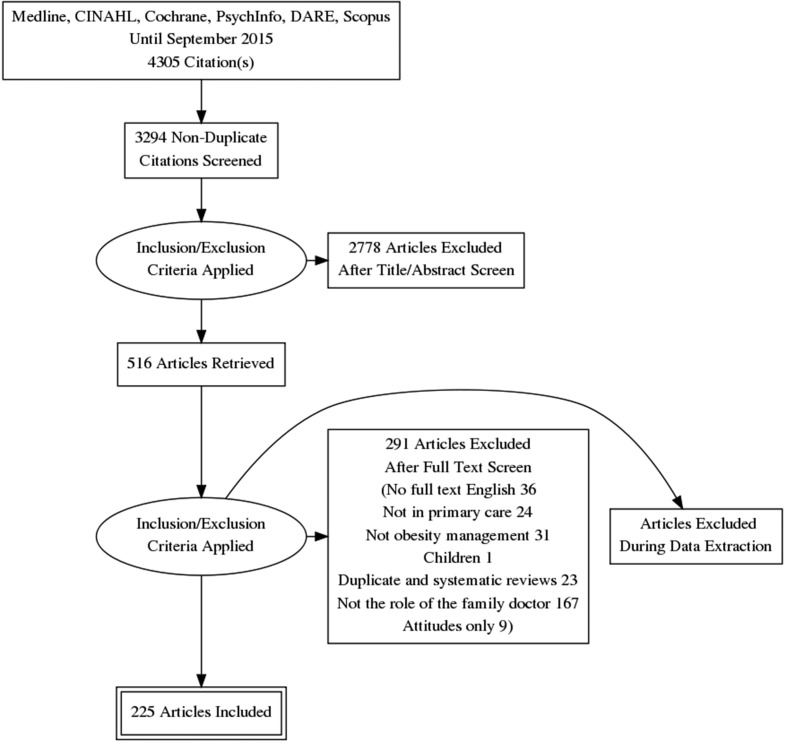
Two reviewers (EAS, NE) independently reviewed the abstracts, followed by the full papers, as described in the flow chart (figure 1). Our data extraction tool captured the author, country of intervention, year of publication, aim, term used to describe the primary care practitioner, methodology, type of involvement of the primary care doctor, skills needed by the doctor and whether the pillars of primary care were identified. Whole person care was judged as included if the paper described obesity management provided in the context of other health needs. Person-centredness was considered as incorporated when the patient’s values, beliefs, cultural needs or context of their community were discussed. First point of contact with the health system was part of all the interventions as ‘primary care’ was part of the search term. Elements of continuity of care were captured with data extracted about communication between any other types of providers and the family doctor. We did not complete a thematic analysis of the included papers.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for scoping review of the role of family doctors in obesity management.
We iteratively developed the data extraction tool based on the information we found in a first pass of all of the intervention papers. The role of the family doctor was extracted in line with clinical management processes in a primary care setting starting with anthropometric measurements, diagnosis, referrals, nutrition care, physical activity advice, as well as more intensive treatments such as medications and bariatric surgery. For the intervention articles, data specific to clinical trials were extracted such as recruitment and control or intervention involvement. A third reviewer (EH) reviewed the extraction data sheets and recommended additional details to be added and reviewed the guideline extraction in full.
Our scoping review of interventions involving family doctors in the management of obesity drew on the Template for Intervention Description and Replication (TIDieR) guidelines for the description of interventions.15 These guidelines outline the parts of interventions that need to be described in order for other practitioners to replicate the intervention, either for research or clinical practice. TIDieR was developed to standardise intervention description and support their implementation, which has been an undervalued aspect of health research.15
Results were presented to stakeholders including patients, clinicians, primary health network representatives, chronic disease organisations and academics at three sessions (April 2015 preliminary results presented during a seminar in Canberra; March 2016 results presented to international academic audience in the Netherlands; June 2017 results presented at an academic meeting of clinicians and academics). The input from these meetings was used to debate the justification for the review, the interpretation of the data extraction and the synthesis of the findings.
Results
This scoping review uncovered 3294 non-duplicate citations, and after title and abstract screening 516 articles were reviewed in full. Up to 291 articles were excluded on full review for the reasons shown in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram (figure 1). A total of 225 articles were included in the final review. The inter-rater agreement for the data extraction points exceeded 95% (62 points of disagreement out of 4992 data extraction points).
Using the focus of the three scoping questions, the following is a description of the literature that was reviewed.
What supporting evidence (both primary and secondary) do we have for role family doctors play in obesity management for adults in primary care?
Of the 225 articles that were included in the review, 110 were about interventions in primary care. There were 77 different interventions described in these papers as some intervention were portrayed in multiple papers (tables 1 and 2). Fifty-seven per cent (44/77) of the interventions were carried out in the USA, with the remainder taking place in a variety of countries (table 1). Forty-eight per cent (37/77) of the interventions described were randomised controlled trials (RCT) (table 1). A majority of interventions on the management of adults with obesity stem from the USA, and RCTs are a common study design.
Table 1.
Number of different interventions identified in scoping review that describe a role for the family doctor in primary care obesity management—by country where the intervention was undertaken, and study design
| Country of intervention | Study design | ||
| Australia | 2 | RCT | 40 |
| Canada | 5 | Single-arm trial | 21 |
| Denmark | 1 | Cohort | 7 |
| Germany | 3 | Non-randomised two-arm trial | 2 |
| Israel | 2 | Cost-effectiveness | 2 |
| Italy | 1 | Action research (protocol) | 1 |
| Japan | 1 | Case–control | 1 |
| Netherlands | 3 | Clinical audit | 1 |
| New Zealand | 2 | Cross sectional | 1 |
| Scotland | 1 | Educational intervention | 1 |
| Spain | 1 | ||
| Switzerland | 4 | ||
| UK | 5 | ||
| UK/Australia/Germany | 1 | ||
| UK/Scotland | 1 | ||
| USA | 44 | ||
| Total | 77 | Total | 77 |
RCT, randomised controlled trial.
Table 2.
Interventions in primary care in the management of adult obesity involving the general practitioner (over seven pages)
| Author | Multiple21 22 | Multiple23–29 | Bolognesi et al30 |
Bodenlos31 | Kerr et al32 |
Multiple33–35 | Multiple36–39 | Multiple16 40–46 | Tsai et al47 |
Banerjee et al48 |
Blonstein et al49 |
Barnes et al50 |
| Name of intervention | Meal replacements in weight | Counterweight | PACE | NA | NA | Be Fit Be Well | POWER | POWER-UP | NA | NA | NA | NA |
| Number of papers | 2 | 7 | 1 | 1 | 1 | 3 | 4 | 8 | 1 | 1 | 1 | 1 |
| Country | USA | UK/Scotland | Italy | USA | USA | USA | USA | USA | USA | USA | USA | USA |
| Year | 2001 | 2004–2012 | 2006 | 2007 | 2008 | 2009–2013 | 2009–2015 | 2009–2015 | 2010 | 2013 | 2013 | 2015 |
| Design | RCT | Cohort/single arm | RCT | RCT | RCT | RCT | RCT/cohort | RCT | RCT | RCT | Single-arm trial | Single-arm trial |
| Diagnosis | X | X | X | X | X | X | X | |||||
| Recruitment into the trial | X | X | X | X | X | X | ||||||
| Coordination | X | X | X | X | ||||||||
| Weight and height | X | X | X | |||||||||
| Waist circumference | X | |||||||||||
| System level/implementation | ||||||||||||
| Doctor–patient relationship | X | X | X | |||||||||
| Public health role | ||||||||||||
| Prevention | ||||||||||||
| Nutrition education | X | X | X | X | ||||||||
| Physical activity education | X | X | X | X | X | |||||||
| Behaviour modification | X | X | X | |||||||||
| Counselling/psychology | X | |||||||||||
| Role modelling | ||||||||||||
| Group-based interventions | 90 | |||||||||||
| Medications | X | |||||||||||
| Bariatric surgery referral | ||||||||||||
| Bariatric surgery work-up | ||||||||||||
| Bariatric surgery after care | ||||||||||||
| Commercial weight loss programme referral | ||||||||||||
| Bariatric equipment in consultation room | ||||||||||||
| Standard care undefined | ||||||||||||
| Standard care was used | X | X | X | X | X | X | ||||||
| Exact role uncertain | X | |||||||||||
| Person-centredness | X | X | ||||||||||
| Whole person care | X | X | X | X |
| Author | Booth et al51 |
Bordowitz et al52 |
Bowerman et al53 |
Clark et al54 55 |
Coupar et al56 |
Cutler et al57 |
Doering et al58 |
Dutton et al59 |
Eichler et al60 |
| Name of intervention | NA | NA | NA | Primary care weight management program | NA | NA | NA | NA | NA |
| Number of papers | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 |
| Country | Australia | USA | USA | USA | Scotland | New Zealand | USA | USA | Switzerland |
| Year | 2006 | 2007 | 2001 | 2008–2010 | 1980 | 2010 | 2013 | 2015 | 2007 |
| Design | Single-arm trial | Cross sectional | Single-arm trial | Single-arm trial | Single-arm trial | Single-arm trial | Single-arm trial | Single-arm trial | Single-arm trial |
| Diagnosis | X | X | X | X | X | X | X | ||
| Recruitment into the trial | X | X | X | X | X | X | X | ||
| Coordination | X | X | X | ||||||
| Weight and height | X | X | X | X | |||||
| Waist circumference | X | ||||||||
| System level/implementation | |||||||||
| Doctor–patient relationship | X | ||||||||
| Public health role | |||||||||
| Prevention | X | ||||||||
| Nutrition education | X | X | X | X | |||||
| Physical activity education | X | X | |||||||
| Behaviour modification | X | X | X | ||||||
| Counselling/psychology | X | X | |||||||
| Role modelling | X | ||||||||
| Group-based interventions | X | X | |||||||
| Medications | X | ||||||||
| Bariatric surgery referral | |||||||||
| Bariatric surgery work-up | |||||||||
| Bariatric surgery after care | |||||||||
| Commercial weight loss programme referral | |||||||||
| Bariatric equipment in consultation room | |||||||||
| Standard care undefined | |||||||||
| Standard care was used | |||||||||
| Exact role uncertain | |||||||||
| Person-centredness | X | ||||||||
| Whole person care | X | X |
| Author | Ely et al61 |
Feigenbaum et al62 |
Kanke et al63 |
Multiple64–66 | Huerta et al67 |
Garies et al68 |
Gusi et al69 |
Haas et al70 |
Multiple71–73 | Hauner et al74 |
Hoke and Franks 75 |
| Name of intervention | NA | NA | NA | Commercial weight loss referral | NA | NA | NA | NA | Lighten-Up | NA | NA |
| Number of papers | 1 | 1 | 1 | 3 | 1 | 1 | 1 | 1 | 3 | 1 | 1 |
| Country | USA | Israel | Japan | UK/Australia/ Germany |
USA | Canada | Spain | USA | UK | Germany | USA |
| Year | 2008 | 2005 | 2015 | 2011–2014 | 2004 | 2015 | 2008 | 2012 | 2010–2012 | 2004 | 2002 |
| Design | RCT | Two-arm trial, non-randomised | RCT | RCT | Cohort | Cohort | RCT | Cohort | RCT | RCT | Single-arm trial |
| Diagnosis | X | X | X | X | X | X | X | X | X | ||
| Recruitment into the trial | X | X | X | X | X | X | X | X | X | X | |
| Coordination | X | X | X | ||||||||
| Weight and height | X | X | X | X | X | X | X | X | |||
| Waist circumference | X | X | |||||||||
| System level/implementation | |||||||||||
| Doctor–patient relationship | X | X | X | ||||||||
| Public health role | |||||||||||
| Prevention | |||||||||||
| Nutrition education | X | X | X | X | X | ||||||
| Physical activity education | X | X | X | X | |||||||
| Behaviour modification | X | X | |||||||||
| Counselling/psychology | X | ||||||||||
| Role modelling | |||||||||||
| Group-based interventions | |||||||||||
| Medications | X | X | |||||||||
| Bariatric surgery referral | |||||||||||
| Bariatric surgery work-up | |||||||||||
| Bariatric surgery after care | |||||||||||
| Commercial weight loss programme referral | X | ||||||||||
| Bariatric equipment in consultation room | |||||||||||
| Standard care undefined | |||||||||||
| Standard care was used | X | X | X | X | |||||||
| Exact role uncertain | |||||||||||
| Person-centredness | |||||||||||
| Whole person care | X |
| Author | Kumanyika et al76 77 |
Kuppersmith and Miles78 | Laing et al79 |
Lewis et al80 |
Logue et al81 82 |
Logue et al83 |
Lowe et al84 |
Madigan et al85 |
Martin et al86 87 |
McDoniel et al88 89 |
Mehring et al90 |
| Name of intervention | Think Health | NA | NA | NA | Transtheoretical Model-Chronic Disease Care for Obesity in Primary Care | NA | NA | NA | A Primary Care Weight Management Intervention for Low-Income African-American Women | The SMART motivational trial | NA |
| Number of papers | 2 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 2 | 2 | 1 |
| Country | USA | USA | USA | UK | USA | USA | USA | UK | USA | USA | Germany |
| Year | 2011–2012 | 2006 | 2014 | 2013 | 2000–2005 | 2012 | 2014 | 2014 | 2006–2008 | 2009–2010 | 2013 |
| Design | RCT | Single-arm trial | RCT | RCT | RCT | RCT | RCT | RCT | RCT | Single-arm trial | RCT |
| Diagnosis | X | X | X | X | X | X | |||||
| Recruitment into the trial | X | X | X | X | X | X | X | X | |||
| Coordination | X | X | X | X | |||||||
| Weight and height | X | X | X | ||||||||
| Waist circumference | X | ||||||||||
| System level/implementation | |||||||||||
| Doctor–patient relationship | X | X | X | ||||||||
| Public health role | |||||||||||
| Prevention | |||||||||||
| Nutrition education | X | X | X | ||||||||
| Physical activity education | X | X | |||||||||
| Behaviour modification | X | X | X | ||||||||
| Counselling/psychology | X | X | X | ||||||||
| Role modelling | |||||||||||
| Group-based interventions | |||||||||||
| Medications | X | ||||||||||
| Bariatric surgery referral | X | ||||||||||
| Bariatric surgery work-up | |||||||||||
| Bariatric surgery after care | |||||||||||
| Commercial weight loss programme referral | X | ||||||||||
| Bariatric equipment in consultation room | |||||||||||
| Standard care undefined | X | X | X | X | |||||||
| Standard care was used | X | X | X | X | X | ||||||
| Exact role uncertain | |||||||||||
| Person-centredness | X | X | X | ||||||||
| Whole person care | X | X | X | X |
| Author | Munsch et al91 |
O’Grady et al92 |
Olsen et al93 |
Pellegrini et al94 |
Richman et al95 |
Ross et al96 97 |
Rutten et al98 |
Saris et al99 |
Stephens et al100 |
Multiple101–105 | Thomas et al106 |
Toth-Capelli et al107 |
| Name of intervention | NA | NA | NA | NA | NA | PROACTIVE | NA | NA | NA | Groningen Overweight | NA | NA |
| Number of papers | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 5 | 1 | 1 |
| Country | Switzerland | USA | Denmark | USA | Australia | Canada | Netherlands | Netherlands | USA | Netherlands | USA | USA |
| Year | 2003 | 2013 | 2005 | 2014 | 1996 | 2009–2012 | 2014 | 1992 | 2008 | 2009–2012 | 2015 | 2013 |
| Design | RCT | Clinical audit | Cost-effectiveness | RCT | Case–control | RCT | Cohort | Single-arm trial | Cohort | Single-arm trial, RCT | RCT | Single-arm trial |
| Diagnosis | X | X | X | X | X | X | X | |||||
| Recruitment into the trial | X | X | X | X | X | X | X | |||||
| Coordination | X | X | X | X | ||||||||
| Weight and height | X | X | X | X | X | X | ||||||
| Waist circumference | X | X | ||||||||||
| System level/implementation | ||||||||||||
| Doctor–patient relationship | X | X | ||||||||||
| Public health role | ||||||||||||
| Prevention | ||||||||||||
| Nutrition education | X | X | X | |||||||||
| Physical activity education | X | X | ||||||||||
| Behaviour modification | X | X | ||||||||||
| Counselling/psychology | X | |||||||||||
| Role modelling | ||||||||||||
| Group-based interventions | X | |||||||||||
| Medications | ||||||||||||
| Bariatric surgery referral | ||||||||||||
| Bariatric surgery work-up | ||||||||||||
| Bariatric surgery after care | ||||||||||||
| Commercial weight loss programme referral | ||||||||||||
| Bariatric equipment in consultation room | ||||||||||||
| Standard care undefined | X | X | X | X | X | |||||||
| Standard care used | X | X | X | X | X | |||||||
| Exact role uncertain | X | |||||||||||
| Person-centredness | X | |||||||||||
| Whole person care | X | X | X |
| Author | Tsai et al108 |
Wadden et al109 |
Wilson et al110 |
Wirth111 | Yardley et al112 |
Tsai et al113 |
Ryan et al114 |
Baillargeon et al115 |
Baillargeon et al116 |
Katz et al117 |
Buclin-Thiébaud et al118 |
Feuerstein et al119 |
| Name of intervention | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Number of papers | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Country | USA | USA | USA | Germany | UK | USA | USA | Canada | Canada | Israel | Switzerland | USA |
| Year | 2012 | 2005 | 2010 | 2005 | 2014 | 2015 | 2010 | 2007 | 2014 | 2005 | 2010 | 2015 |
| Design | Cost-effectiveness | RCT | Non-randomised two-arm trial | Single-arm trial | RCT | RCT | RCT | Action research (protocol) | RCT (protocol) | Educational intervention | Single-arm trial | Single-arm trial |
| Diagnosis | X | X | X | X | X | |||||||
| Recruitment into the trial | X | X | X | X | ||||||||
| Coordination | X | X | X | X | X | |||||||
| Weight and height | X | X | X | X | X | |||||||
| Waist circumference | X | X | ||||||||||
| System level/implementation | ||||||||||||
| Doctor–patient relationship | ||||||||||||
| Public health role | ||||||||||||
| Prevention | ||||||||||||
| Nutrition education | X | X | X | X | X | |||||||
| Physical activity education | X | X | X | |||||||||
| Behaviour modification | X | X | X | |||||||||
| Counselling/psychology | ||||||||||||
| Role modelling | ||||||||||||
| Group-based interventions | X | |||||||||||
| Medications | X | X | X | |||||||||
| Bariatric surgery referral | X | |||||||||||
| Bariatric surgery work-up | ||||||||||||
| Bariatric surgery after care | ||||||||||||
| Commercial weight loss programme referral | ||||||||||||
| Bariatric equipment in consultation room | ||||||||||||
| Standard care undefined | X | X | ||||||||||
| Standard care was used | X | X | X | |||||||||
| Exact role uncertain | X | X | ||||||||||
| Person-centredness | ||||||||||||
| Whole person care | X | X | X |
| Author | Hartman et al120 |
Lin et al121 |
Moore et al122 |
Rodondi et al123 |
Rueda-Clausen et al124 |
Schuster et al125 |
Yank et al126 |
Goodyear-Smith et al127 |
Jay et al128 |
Wadden et al129 |
| Name of intervention | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Number of papers | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Country | USA | USA | UK | Switzerland | Canada | USA | USA | New Zealand | USA | USA |
| Year | 2014 | 2015 | 2003 | 2006 | 2014 | 2008 | 2013 | 2014 | 2013 | 1997 |
| Design | RCT (protocol) | RCT | RCT | Cohort study | Single-arm trial | Single-arm trial | RCT | RCT | RCT | RCT |
| Diagnosis | X | X | X | X | X | X | X | |||
| Recruitment into the trial | X | X | X | |||||||
| Coordination | X | X | X | X | ||||||
| Weight and height | X | X | X | X | X | |||||
| Waist circumference | X | |||||||||
| System level/implementation | X | |||||||||
| Doctor–patient relationship | X | X | ||||||||
| Public health role | X | |||||||||
| Prevention | ||||||||||
| Nutrition education | X | X | X | X | ||||||
| Physical activity education | X | X | X | X | ||||||
| Behaviour modification | X | X | X | X | ||||||
| Counselling/psychology | ||||||||||
| Role modelling | ||||||||||
| Group-based interventions | ||||||||||
| Medications | ||||||||||
| Bariatric surgery referral | ||||||||||
| Bariatric surgery work-up | ||||||||||
| Bariatric surgery after care | ||||||||||
| Commercial weight loss programme referral | ||||||||||
| Bariatric equipment in consultation room | ||||||||||
| Standard care undefined | X | X | X | X | ||||||
| Standard care was used | X | X | X | X | ||||||
| Exact role uncertain | X | X | ||||||||
| Person-centredness | ||||||||||
| Whole person care |
NA, not applicable; RCT, randomised controlled trial.
There were a total of 74 articles that were clinical overviews and opinion papers on the primary care management of obesity that included discussion of the role of the family doctor (table 3), and 25 papers that described current practice of family doctors in obesity management, usually through surveys or clinical audits (table 4). There were 16 international guidelines relevant to family doctors focused on the management of obesity (table 5).
Table 3.
Clinical overviews and opinion articles on the role of the family doctor in the management of adult obesity in primary care (over seven pages)
| Author | Anderson and Wadden130 | Rao131 | Simkin-Silverman et al132 |
Logue and Smucker133 | Lyznicki et al134 |
Sherman et al135 |
Vallis et al136 |
Benotti137 | Brown et al138 |
Choban et al139 |
| Title | Treating the obese patient: suggestions for primary care practice | Office-based strategies for the management of obesity | Treatment of overweight and obesity in primary care practice: current evidence and future directions | Obesity management in primary care: changing the status quo | Obesity: assessment and management in primary care | Health coaching integration into primary care for the treatment of obesity | Modified 5 As: minimal intervention for obesity counseling in primary care | Patient preparation for bariatric surgery | Laparoscopic adjustable gastric banding | Bariatric surgery for morbid obesity: why, who, when, how, where, and then what? |
| Country | USA | USA | USA | USA | USA | USA | Canada | USA | Australia | USA |
| Year | 1999 | 2010 | 2008 | 2001 | 2001 | 2013 | 2013 | 2014 | 2009 | 2002 |
| Overview/opinion | Overview | Overview | Overview | Editorial | Overview | Opinion | Overview | Overview (bariatric) | Overview (bariatric) | Overview (bariatric) |
| Diagnosis | X | X | X | X | X | X | X | X | X | X |
| Coordination | X | X | X | X | X | X | X | X | ||
| Weight and height | X | X | X | X | X | X | ||||
| Waist circumference | X | X | X | X | ||||||
| System level/implementation | ||||||||||
| Doctor–patient relationship | ||||||||||
| Public health role | ||||||||||
| Prevention | ||||||||||
| Nutrition education | X | X | X | X | X | X | ||||
| Physical activity education | X | X | X | X | ||||||
| Behaviour modification | X | X | X | X | ||||||
| Counselling/psychology | X | |||||||||
| Role modelling | X | |||||||||
| Group-based interventions | ||||||||||
| Medications | X | X | X | X | ||||||
| Bariatric surgery referral | X | X | X | X | X | X | ||||
| Bariatric surgery work-up | X | |||||||||
| Bariatric surgery after care | X | |||||||||
| Commercial weight loss programme referral | X | X | ||||||||
| Bariatric equipment in consultation room | ||||||||||
| Standard care undefined | ||||||||||
| Exact role uncertain | X | X | ||||||||
| Person-centredness | X | X | ||||||||
| Whole person care | X | X | X | X |
| Author | DeMaria140 | Dixon141 | Heber et al142 |
Karmali et al143 |
Pietras et al144 |
Richardson145 | Shafipour et al146 |
Snow et al147 |
Van Sickle148 | Virji and Murr149 | Wilbert et al150 |
| Title | Bariatric surgery for morbid obesity | Referral for a bariatric surgical consultation: it is time to set a standard of care | Endocrine and nutritional management of the post-bariatric surgery patient: an endocrine society clinical practice guideline | Bariatric surgery: a primer | Preoperative and postoperative management of the bariatric surgical patient | Bariatric society is here to help | What do I do with my morbidly obese patient? A detailed case study of bariatric surgery in Kaiser Permanente Southern California | Pharmacologic and surgical management of obesity in primary care: a clinical practice guideline from the American College of Physicians | Management of the challenging bariatric surgical patient | Caring for patients after bariatric surgery | Appetite suppressants as adjuncts for weight loss |
| Country | USA | Australia | USA | Canada | USA | USA | USA | USA | USA | USA | USA |
| Year | 2007 | 2009 | 2010 | 2010 | 2007 | 2010 | 2009 | 2005 | 2007 | 2006 | 2011 |
| Overview/opinion | Overview | Opinion | Expert opinion | Overview | Overview | Single opinion | Overview | Expert opinion | Overview | Overview | Overview |
| Diagnosis | X | X | X | X | X | X | X | X | |||
| Coordination | X | X | X | X | X | X | X | ||||
| Weight and height | X | X | X | X | X | ||||||
| Waist circumference | |||||||||||
| System level/implementation | |||||||||||
| Doctor–patient relationship | |||||||||||
| Public health role | |||||||||||
| Prevention | |||||||||||
| Nutrition education | X | X | X | ||||||||
| Physical activity education | X | X | |||||||||
| Behaviour modification | X | ||||||||||
| Counselling/psychology | X | ||||||||||
| Role modelling | |||||||||||
| Group-based interventions | |||||||||||
| Medications | X | X | |||||||||
| Bariatric surgery referral | X | X | X | X | X | X | X | X | X | ||
| Bariatric surgery work-up | X | X | |||||||||
| Bariatric surgery after care | X | X | X | X | X | X | X | ||||
| Commercial weight loss programme referral | |||||||||||
| Bariatric equipment in consultation room | |||||||||||
| Standard care undefined | |||||||||||
| Exact role uncertain | X | X | |||||||||
| Person-centredness | X | ||||||||||
| Whole person care | X | X |
| Author | Kolasa et al151 |
Mercer152 | UK Health Development Agency153 | Agrawal et al154 |
Brunton et al155 |
Bartlett156 | Benjamin et al157 |
Birmingham et al158 |
Caulfield159 | Cerveny160 | Fitzpatrick et al161 |
| Title | Weight loss strategies that really work | How useful are clinical guidelines for the management of obesity in general practice? | Care pathways for the prevention and management of obesity | Managing obesity like any other chronic condition. Long-term therapy may reduce comorbidity as well | Management of obesity in adults | Motivating patients toward weight loss: practical strategies for addressing overweight and obesity | Can primary care physician-driven community programs address the obesity epidemic among high-risk populations? | The management of adult obesity | Obesity, legal duties, and the family physician | Approaching the obese patients in primary health care in the Czech Republic | An evidence-based guide for obesity treatment in primary care |
| Country | USA | UK | UK | USA | USA | USA | USA | Canada | Canada | Czech Republic | USA |
| Year | 2010 | 2009 | 2004 | 2000 | 2014 | 2003 | 2013 | 2003 | 2007 | 2007 | 2015 |
| Overview/opinion | Overview | Guideline summary | Draft clinical pathway | Overview | Overview | Overview | Editorial overview | Overview | Legal overview | Overview | Overview |
| Diagnosis | X | X | X | X | X | X | X | X | X | ||
| Coordination | X | X | X | X | X | X | X | X | X | X | |
| Weight and height | X | X | X | X | X | X | X | ||||
| Waist circumference | X | X | X | X | X | X | X | ||||
| System level/implementation | X | X | |||||||||
| Doctor–patient relationship | X | X | X | X | X | X | X | ||||
| Public health role | X | X | |||||||||
| Prevention | X | X | X | X | |||||||
| Nutrition education | X | X | X | X | X | X | X | ||||
| Physical activity education | X | X | X | X | X | X | |||||
| Behaviour modification | X | X | X | X | X | X | X | ||||
| Counselling/psychology | X | X | X | X | |||||||
| Role modelling | |||||||||||
| Group-based interventions | |||||||||||
| Medications | X | X | X | X | X | X | X | ||||
| Bariatric surgery referral | X | X | X | X | X | ||||||
| Bariatric surgery work-up | |||||||||||
| Bariatric surgery after care | |||||||||||
| Commercial weight loss programme referral | |||||||||||
| Bariatric equipment in consultation room | |||||||||||
| Standard care undefined | |||||||||||
| Exact role uncertain | |||||||||||
| Person-centredness | X | X | X | X | X | X | X | ||||
| Whole person care | X | X | X | X | X | X |
| Author | Frank162 | Gandjour et al163 |
Grief164 | Grima and Dixon165 | Hagaman166 | Hill167 | Hill and Wyatt168 | Iacobucci169 | Kausman and Bruere170 | Kolasa171 |
| Title | A multidisciplinary approach to obesity management: the physician’s role and team care alternatives | Development process of an evidence-based guideline for the treatment of obesity | Strategies to facilitate weight loss in patients who are obese | Obesity—recommendations for management in general practice and beyond | FP’s patients are successful ‘losers’ | Dealing with obesity as a chronic disease | Outpatient management of obesity: a primary care perspective | Pay GPs to tackle obesity, doctors urge UK government | If not dieting, now what? | Summary of clinical guidelines on the identification, evaluation, and treatment of overweight and obesity |
| Country | USA | Germany | USA | Australia | USA | USA | USA | UK | Australia | USA |
| Year | 1998 | 2001 | 2010 | 2013 | 2010 | 1998 | 2002 | 2014 | 2006 | 1999 |
| Overview/opinion | Overview | Overview | Single opinion | Overview | Single opinion | Overview | Overview | Single opinion | Overview | Overview |
| Diagnosis | X | X | X | X | X | X | X | X | X | X |
| Coordination | X | X | X | X | X | X | X | X | X | |
| Weight and height | X | X | X | X | X | X | X | |||
| Waist circumference | X | X | X | X | X | X | ||||
| System level/implementation | X | |||||||||
| Doctor–patient relationship | X | X | X | X | X | |||||
| Public health role | X | |||||||||
| Prevention | ||||||||||
| Nutrition education | X | X | X | |||||||
| Physical activity education | X | X | ||||||||
| Behaviour modification | X | X | X | X | ||||||
| Counselling/psychology | X | X | X | |||||||
| Role modelling | X | |||||||||
| Group-based interventions | X | |||||||||
| Medications | X | X | X | X | ||||||
| Bariatric surgery referral | X | X | X | X | X | |||||
| Bariatric surgery work-up | ||||||||||
| Bariatric surgery after care | ||||||||||
| Commercial weight loss programme referral | ||||||||||
| Bariatric equipment in consultation room | X | |||||||||
| Standard care undefined | X | |||||||||
| Exact role uncertain | X | X | ||||||||
| Person-centredness | X | X | X | X | X | |||||
| Whole person care | X | X | X |
| Author | Kushner172 | Landau and Moulton173 | Lenfant174 | Maryon-Davis175 | Mogul et al176 |
Newton et al177 |
Nichols and Bazemore178 | Nonas179 | Orzano and Scott180 | Ossolinski et al181 |
| Title | Tackling obesity: is primary care up to the challenge? | General principles in the primary care of obesity | Physicians need practical tools to treat the complex problems of overweight and obesity | Weight management in primary care: how can it be made more effective? | New perspectives on diagnosis and treatment of obesity Winnable Battles: family physicians play an essential role in addressing tobacco use and obesity |
Supporting behavior change in overweight patients: a guide for the primary care physician Winnable Battles: family physicians play an essential role in addressing tobacco use and obesity for the primary care physician |
Winnable Battles: family physicians play an essential role in addressing tobacco use and obesity | A model for chronic care of obesity through dietary treatment | Diagnosis and treatment of obesity in adults: an applied evidence-based review | Weight management practices and evidence for weight loss through primary care: a brief review |
| Country | USA | USA | USA | UK | USA | USA | USA | USA | USA | Australia |
| Year | 2010 | 1992 | 2001 | 2005 | 1999 | 2008 | 2014 | 1998 | 2004 | 2015 |
| Overview/opinion | Editorial | Overview | Editorial | Overview | Overview | Overview | Editorial | Overview | Overview | Overview |
| Diagnosis | X | X | X | X | X | X | X | X | X | X |
| Coordination | X | X | X | X | X | X | X | |||
| Weight and height | X | X | X | X | X | |||||
| Waist circumference | X | X | X | |||||||
| System level/implementation | X | X | ||||||||
| Doctor–patient relationship | X | X | X | X | ||||||
| Public health role | X | X | ||||||||
| Prevention | X | |||||||||
| Nutrition education | X | X | X | X | X | X | X | X | ||
| Physical activity education | X | X | X | X | X | X | X | X | ||
| Behaviour modification | X | X | X | X | X | X | X | |||
| Counselling/psychology | X | X | X | |||||||
| Role modelling | ||||||||||
| Group-based interventions | X | |||||||||
| Medications | X | X | X | X | X | X | X | X | X | |
| Bariatric surgery referral | X | X | X | X | X | X | X | |||
| Bariatric surgery work-up | ||||||||||
| Bariatric surgery after care | ||||||||||
| Commercial weight loss programme referral | X | X | ||||||||
| Bariatric equipment in consultation room | ||||||||||
| Standard care undefined | X | X | ||||||||
| Exact role uncertain | X | X | ||||||||
| Person-centredness | X | X | X | X | X | X | ||||
| Whole person care | X | X | X | X | X |
| Author | Plourde and Prud’homme 182 | Rao et al183 |
Robinson et al184 |
Ruser et al185 |
Scherger186 | Schlair et al187 |
Spira188 | Thompson et al189 |
Tsai et al190 |
| Title | Managing obesity in adults in primary care | New and emerging weight management strategies for busy ambulatory settings: a scientific statement from the American Heart Association: endorsed by the society of behavioral medicine | Obesity: a move from traditional to more patient-oriented management | Whittling away at obesity and overweight: small lifestyle changes can have the biggest impact | Primary care physicians: on the front line in the fight against obesity | How to deliver high-quality obesity counseling in primary care using the 5As framework | Managing obesity in general practice | Treatment of obesity | Obesity |
| Country | Canada | USA | USA | USA | USA | USA | UK | USA | USA |
| Year | 2012 | 2011 | 1995 | 2005 | 1999 | 2012 | 1983 | 2007 | 2010 |
| Overview/opinion | Overview | Overview | Overview | Overview | Overview | Overview | Single opinion | Overview | Overview |
| Diagnosis | X | X | X | X | X | X | X | X | X |
| Coordination | X | X | X | X | X | ||||
| Weight and height | X | X | X | X | X | X | |||
| Waist circumference | X | X | X | X | X | X | |||
| System level/implementation | |||||||||
| Doctor–patient relationship | X | X | X | ||||||
| Public health role | X | ||||||||
| Prevention | X | ||||||||
| Nutrition education | X | X | X | X | X | X | X | X | |
| Physical activity education | X | X | X | X | X | X | X | X | |
| Behaviour modification | X | X | X | X | X | X | X | ||
| Counselling/psychology | X | X | X | X | |||||
| Role modelling | |||||||||
| Group-based interventions | X | ||||||||
| Medications | X | X | X | X | X | X | X | X | |
| Bariatric surgery referral | X | X | X | X | X | X | |||
| Bariatric surgery work-up | |||||||||
| Bariatric surgery after care | |||||||||
| Commercial weight loss programme referral | X | ||||||||
| Bariatric equipment in consultation room | |||||||||
| Standard care undefined | |||||||||
| Exact role uncertain | X | ||||||||
| Person-centredness | X | X | |||||||
| Whole person care | X | X | X |
| Author | Yanovski191 | Australian Medical Association192 | Zwar and Harris193 | Hainer194 | Seidell et al195 |
Anderson196 | Jarvis197 | Lowery198 | van Avendonk et al199 |
Al-Quaiz200 | Carvajal et al201 |
Kushner and Ryan202 | Obesity Australia203 |
| Title | A practical approach to treatment of the obese patient | Your family doctor—keeping you healthy AMA family doctor week, 20–26 July 2014 |
Are GPs doing enough to help patients lose weight? | How should the obese patient be managed? Possible approaches to a national obesity management network | An integrated health care standard for the management and prevention of obesity in The Netherlands | Reducing overweight and obesity: closing the gap between primary care and public health | Obesity and the overworked GP | Medical home concept: policy implications for an integrated approach in obesity management | Primary care and public health a natural alliance? The introduction of the guidelines for obesity and undernutrition of the Dutch College of General Practitioners | Current concepts in the management of obesity: an evidence based review | Managing obesity in primary care practice: a narrative review | Assessment and lifestyle management of patients with obesity: clinical recommendations from systematic reviews | The mission of Obesity Australia is to drive change in the public perceptions of obesity, its prevalence and its treatment. |
| Country | USA | Australia | Australia | Czech Republic | Netherlands | Spain | UK | USA | Netherlands | Saudi Arabia | USA | USA | Australia |
| Year | 1993 | 2014 | 2013 | 1999 | 2012 | 2008 | 2006 | 2010 | 2012 | 2001 | 2013 | 2014 | 2013 |
| Overview/opinion | Overview | Media release | Blog | Overview | Overview | Overview | Overview | Overview | Overview | Overview | Overview | Overview | Statement |
| Diagnosis | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Coordination | X | X | X | X | X | X | X | X | X | X | X | X | |
| Weight and height | X | X | X | X | X | X | X | X | X | X | |||
| Waist circumference | X | X | X | X | X | X | |||||||
| System level/implementation | X | X | X | X | |||||||||
| Doctor–patient relationship | X | X | X | X | X | X | |||||||
| Public health role | X | X | X | ||||||||||
| Prevention | X | X | X | ||||||||||
| Nutrition education | X | X | X | X | X | X | X | X | X | ||||
| Physical activity education | X | X | X | X | X | X | X | X | X | ||||
| Behaviour modification | X | X | X | X | X | X | X | ||||||
| Counselling/psychology | X | ||||||||||||
| Role modelling | |||||||||||||
| Group-based interventions | X | ||||||||||||
| Medications | X | X | X | X | |||||||||
| Bariatric surgery referral | X | X | X | X | X | X | X | X | |||||
| Bariatric surgery work-up | |||||||||||||
| Bariatric surgery after care | |||||||||||||
| Commercial weight loss programme referral | X | X | X | X | |||||||||
| Bariatric equipment in consultation room | |||||||||||||
| Standard care undefined | |||||||||||||
| Exact role uncertain | X | X | X | X | X | X | X | X | X | X | |||
| Person-centredness | X | X | |||||||||||
| Whole person care | X | X | X | X |
FP, family physician; GP, general practitioner.
Table 4.
Current practice articles on the role of the family doctor in the management of adult obesity in primary care (over three pages)
| Author | Bourn204 | Alexander et al205 |
Alexander et al206 |
Klumbiene et al207 |
Linné et al208 |
Patterson et al209 |
Hoyt210 | Fransen et al211 |
Cohen et al212 |
Fobi et al213 |
| Title | Tackling obesity in England | Do the five A’s work when physicians counsel about weight loss? | Weight-loss talks: what works (and what doesn’t) | Advising overweight persons about diet and physical activity in primary health care: Lithuanian health behaviour monitoring study | Success rate of Orlistat in primary-care practice is limited by failure to follow prescribing recommendations: the referral letter content vs clinical reality | Prescribing for weight loss in primary care: evidence from a population based study | Person, place, and prevention in primary care: a multilevel analysis of variation in the delivery of mental health, substance-use disorder, and obesity services | The development of a minimal intervention strategy to address overweight and obesity in adult primary care patients in The Netherlands | Laparoscopic Roux-en-Y gastric bypass for BMI<35 kg/m2: a tailored approach | Gastric bypass in patients with BMI<40 but >32 without life-threatening comorbidities: preliminary report |
| Country | England | USA | USA | Lithuania | Sweden | Northern Ireland | USA | Netherlands | USA | Brazil |
| Year | 2001 | 2011 | 2011 | 2006 | 2003 | 2013 | 2013 | 2008 | 2006 | 2002 |
| Methodology | Government report | Qualitative | Qualitative | Survey | Survey | Audit | Survey | Qualitative | Audit | Audit |
| Diagnosis | X | X | X | X | X | X | X | X | ||
| Coordination | X | X | X | X | X | X | X | |||
| Weight and height | X | X | X | X | ||||||
| Waist circumference | X | |||||||||
| System level/implementation | X | X | X | |||||||
| Doctor–patient relationship | X | |||||||||
| Public health role | X | |||||||||
| Prevention | X | |||||||||
| Nutrition education | X | X | X | X | X | X | ||||
| Physical activity education | X | X | X | X | X | |||||
| Behaviour modification | X | X | X | |||||||
| Counselling/psychology | X | |||||||||
| Role modelling | ||||||||||
| Group-based interventions | ||||||||||
| Medications | X | X | X | |||||||
| Bariatric surgery referral | X | X | ||||||||
| Bariatric surgery work-up | ||||||||||
| Bariatric surgery after care | ||||||||||
| Commercial weight loss programme referral | ||||||||||
| Bariatric equipment in consultation room | ||||||||||
| Standard care undefined | X | |||||||||
| Exact role uncertain | X | X | ||||||||
| Person-centredness | X | |||||||||
| Whole person care | X | X | ||||||||
| Under-recognition/undertreatment mentioned | X | X | X | X |
| Author | Kloek et al214 | Antognoli et al215 |
Nursing Standard216 | Binnie217 | Bramlage et al218 |
Kraschnewski et al219 |
Morris et al220 |
Sammut et al221 |
Smith et al222 |
Sonntag et al223 |
Timmerman et al224 |
| Title | Dutch general practitioners' weight management policy for overweight and obese patients | Direct observation of weight counselling in primary care: alignment with clinical guidelines | GPs failing to offer weight-loss advice to people who need it | Ten-year follow-up of obesity | Recognition and management of overweight and obesity in primary care in Germany | A silent response to the obesity epidemic: decline in US physician weight counseling | Who gets what treatment for obesity? A survey of GPs in Scotland | Audit of the diagnosis and management of adult obesity in a Maltese general practice | U.S. primary care physicians' diet-, physical activity-, and weight-related care of adult patients | Counseling overweight patients: analysis of preventive encounters in primary care | Weight management practices among primary care providers |
| Country | Netherlands | USA | UK | UK | Germany | USA | Scotland | Malta | USA | Germany | USA |
| Year | 2014 | 2014 | 2015 | 1977 | 2004 | 2013 | 1999 | 2012 | 2011 | 2010 | 2000 |
| Methodology | Cross-sectional survey | Direct observation | Editorial | Clinical audit | Cross-sectional survey | Clinical audit | Cross-sectional survey | Clinical audit | Clinical audit | Cross-sectional survey | Cross-sectional survey |
| Diagnosis | X | X | X | X | X | X | X | X | X | X | X |
| Coordination | X | X | X | X | X | X | X | ||||
| Weight and height | X | X | X | X | X | X | X | X | |||
| Waist circumference | X | X | X | X | |||||||
| System level/implementation | |||||||||||
| Doctor–patient relationship | X | X | X | ||||||||
| Public health role | |||||||||||
| Prevention | X | ||||||||||
| Nutrition education | X | X | X | X | X | X | X | X | X | X | X |
| Physical activity education | X | X | X | X | X | X | X | X | X | X | |
| Behaviour modification | X | X | X | X | X | X | X | ||||
| Counselling/psychology | X | ||||||||||
| Role modelling | |||||||||||
| Group-based interventions | X | X | X | ||||||||
| Medications | X | X | X | X | X | X | X | X | |||
| Bariatric surgery referral | X | X | X | X | |||||||
| Bariatric surgery work-up | |||||||||||
| Bariatric surgery after care | |||||||||||
| Commercial weight loss programme referral | X | X | X | ||||||||
| Bariatric equipment in consultation room | |||||||||||
| Standard care undefined | |||||||||||
| Exact role uncertain | X | ||||||||||
| Person-centredness | |||||||||||
| Whole person care | X | X | |||||||||
| Under-recognition/undertreatment mentioned | X | X | X | X | X | X | X |
| Author | Gaglioti et al225 | Morris and Gravelle226 | Huber et al227 |
Asselin et al228 |
| Title | Primary care’s ecologic impact on obesity | GP supply and obesity | Obesity management and continuing medical education in primary care: results of a Swiss survey | Missing an opportunity: the embedded nature of weight management in primary care |
| Country | USA | UK | Switzerland | Canada |
| Year | 2009 | 2008 | 2011 | 2015 |
| Methodology | Epidemiology | Cross-sectional survey | Cross-sectional survey | Qualitative |
| Diagnosis | X | X | X | X |
| Coordination | X | X | ||
| Weight and height | X | X | ||
| Waist circumference | X | |||
| System level/implementation | X | X | ||
| Doctor–patient relationship | ||||
| Public health role | X | |||
| Prevention | X | |||
| Nutrition education | X | X | ||
| Physical activity education | X | X | ||
| Behaviour modification | X | X | ||
| Counselling/psychology | ||||
| Role modelling | ||||
| Group-based interventions | ||||
| Medications | ||||
| Bariatric surgery referral | ||||
| Bariatric surgery work-up | ||||
| Bariatric surgery after care | ||||
| Commercial weight loss programme referral | ||||
| Bariatric equipment in consultation room | ||||
| Standard care undefined | ||||
| Exact role uncertain | X | X | X | |
| Person-centredness | X | |||
| Whole person care | X | |||
| Under-recognition/undertreatment mentioned | X |
GP, general practitioner.
Table 5.
International guidelines on the management of adult obesity in primary care, the role of the family doctor (FD) (over two pages)
| Guideline | Country | Year | Intended for an FD audience? | FD mentioned | Primary healthcare mentioned | FD—measure the patient | FD— nutrition/physical activity advice | FD— behavioural supports | FD—frequency of visits mentioned | FD—advice on use of intensive treatments | FD— referral to allied health | FD— referral to specialist obesity services | Does not mention specific role for FD |
| RACGP SNAP— Overweight and obesity, 2nd edition229 | Australia | 2015 | X | X | X | X | X | X | X | X | |||
| National Institute for Health and Care Excellence ‘Managing adults who are overweight or obese’230 | UK | 2015 | X | X | |||||||||
| Recommendations for prevention of weight gain and use of behavioural and pharmacological interventions to manage overweight and obesity in adults in primary care Canadian Task Force on Preventive Health Care231 | Canada | 2015 | X | X | X | ||||||||
| Clinical practice guidelines for the management of overweight and obesity in adults, adolescents and children in Australia1 | Australia | 2013 | X | X | X | X | X | X | X | X | X | ||
| Institute for Clinical Systems Improvement Health Care Guideline Prevention and Management of Obesity for Adults232 | USA | 2013 | X | X | X | ||||||||
| Guideline for the Management of Overweight and Obesity in Adults A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society233 |
USA | 2013 | Primary care practitioner (PCP) | PCP | X | X | |||||||
| New Zealand Primary Care Handbook 2012—Weight Management234 | New Zealand | 2012 | X | X | X | X | X | X | X | X | X | ||
| US Preventive Services Task Force Screening for and Management of Obesity in Adults: Recommendation Statement235 | USA | 2012 | X | X | X | X | X | X | X | X | X | ||
| Screening for and management of obesity in adults: US Preventive Services Task Force recommendation statement236 | USA | 2012 | X | X | X | X | X | ||||||
| RACGP guidelines for preventive activities in general practice, 8th edition; 7.2 Overweight237 | Australia | 2012 | X | X | X | X | X | X | X | X | |||
| National guide to a preventive health assessment for Aboriginal and Torres Strait Islander people, 2nd edition, Overweight/Obesity238 |
Australia | 2012 | X | X | X | X | |||||||
| British Columbia Ministry of Health Services primary care providers have an important role in preventing and managing obesity through services offered to patients239 | Canada | 2011 | X | X | X | ||||||||
| World Gastroenterological Organisation: Obesity Guideline240 | International | 2011 | X | X | X | ||||||||
| Scottish Intercollegiate Guidelines Network—Management of Obesity241 | Scotland | 2010 | X | X | X | ||||||||
| Dutch College of General Practitioners: Obesity Guideline242 | Netherlands | 2010 | X | X | X | X | X | X | X | X | |||
| WHO—Interventions on Diet and Physical Activity: What works243 | WHO | 2009 | X | X | X |
RACGP SNAP, Royal Australian College of General Practitioners "Smoking, Nutrition, Alcohol, Physical Activity".
What is the role of the family doctor in managing obesity as a primary risk as supported by the evidence base?
The family doctor was involved in varying ways in obesity management depending on the type of article. The most common role for the family doctor across all types of articles was the diagnosis of obesity. The diagnosis was based on the BMI of the patient and waist circumference measurements were rarely taken. Family doctors were not often involved in intervention studies beyond diagnosis and referral into the trial. Papers about current practice, including audits and surveys, mentioned a lack of recognition and treatment of obesity by family doctors. Current overview and opinion papers often suggested a wide role including diagnosis, nutrition and physical activity counselling, and options for appropriate referrals. And there was great variation in the international guidelines with the family doctor not mentioned by some, to a broad role in others. Unsurprisingly, this varied depending on whether a primary care organisation had developed the guideline.
In all types of articles, the family doctor was frequently involved in the diagnosis of obesity (73/110 intervention papers, 69/74 overview papers, 22/24 current practice papers). They were involved in height and weight measurements in 111 out of 225 total papers, and overall waist circumference was infrequently mentioned in all articles (50/209 papers, not including guidelines).
We included all interventions relevant to the review, whether they were reported the family doctor’s role as part of an experimental intervention or in a control arm (table 2). In 45 of the 77 interventions, the family doctor was involved in recruiting patients to the trial. The family doctor only had a role in care delivery in 27 interventions (35%) in either the intervention or the control arm of a trial. Across all interventions, ‘standard care’ was used in 27 trials; however, it was only well described in 12 of these. In one case, the ‘primary care provider’ was used in the standard care arm but was ‘instructed not to provide specific behavioral strategies for changing eating and activity habits’.16
We attempted to describe whether the pillars of primary care could be identified in the interventions as they were described. In 17 of the 77 interventions, the comprehensive, holistic care of the patient was described. In only seven of the interventions could person-centredness be seen in the description of the intervention.
Overview and opinion articles generally reported that the family doctor should be involved in all stages of management from diagnosis, nutrition and physical activity counselling, and ongoing follow-up. Not surprisingly, papers that were mainly about pharmacological interventions or bariatric surgery were only about that area of management. Bariatric surgery papers described the family doctor as required for referral, but not work-up, and some described the family doctor’s role in ongoing management after surgery.
Overall, the family doctor was commonly involved in the diagnosis of obesity, and as a referral source into intervention trials. Frequently, the under-recognition and management of obesity was noted in observational studies of current practice. It was difficult to identify the pillars of primary care practice in the description on interventions for adult obesity management.
What do primary care guidelines say about the role of the family doctor? What do peak bodies (ie, advocacy groups) say about the role of the family doctor? Are these both in line with what is conveyed by current research?
In terms of the specific role of the family doctor, guidelines were variable and ranged from no mention of the family doctor, to the family doctor being involved in every stage of management from diagnosis and advice on nutrition and physical activity, to intensive treatments and long-term follow-up. Not surprisingly, guidelines written by family medicine organisations described a greater role for the family doctor. For guidelines that were written with a national healthcare focus, there was less detail on the type of professional that should be involved in each of the management areas.
Seven of the 16 guidelines specifically mentioned family doctors (or synonym), with one referring to ‘primary care providers’ (table 5). Seven (44%) suggested the family doctor should be involved in anthropometric measures of the patient, five (31%) recommended the family doctor should provide nutrition and physical activity advice, and seven discussed the referral to allied health providers by the family doctor.
Discussion
This scoping review synthesises the current literature on the role of the family doctor in the management of obesity in primary care. This comprehensive set of articles provides the research community with a resource for further study, for example, systematic reviews and meta-analyses based on different aspects of primary care management of adult obesity.
The family doctor is mostly used as a recruitment source in primary care interventions, the majority of which have been carried out in the USA. This is in contrast to guidelines, clinical overviews and opinions that suggest a role for family doctors from diagnosis, offering lifestyle advice and behavioural support, and ongoing follow-up. Half of the articles that described current practice, mostly through clinical audits or surveys, reported that obesity was under-recognised by family doctors. There appears to be a misalignment between what commentators suggest as a role for the family doctor, and the current role they play in many primary care interventions.
The great majority of primary care interventions for adult obesity are being developed and tested in the USA healthcare setting. This has implications for the interpretation of the findings for translation into other contexts.17 For example, the USA does not have a ‘gatekeeper’ function for family doctors and patients are able to self-refer to tertiary services.18 Patients with health insurance also have different access to care compared with those who do not have.18 This may have ramification when translating an intervention to a context with universal healthcare access, such as the UK and Australia, and warrants further investigation.
We were also able to identify areas of concern for the publication of primary care research in obesity management. Twenty-seven of the interventions used standard care in the control arm, but standard care was poorly defined in 15 of these interventions. It is difficult to determine the relative effectiveness of new interventions in the management of obesity in primary care when they are compared with poorly defined standard care. More worryingly was the use of substandard care where family doctors were advised not to give lifestyle advice to patients.16 This suggests that usual care was artificially reduced in order to improve the apparent effectiveness of an intervention. This is a dubious practice from an ethical and scientific perspective and undermines the role of family doctors in obesity management.
Implications for practice
Guidelines are documents that are developed to assist practitioners in deciding on a course of action in a specific clinical circumstance19 and they often determine a standard of care. The obesity guidelines that were identified in this review had varying recommendations for the role of the family doctor. In some jurisdictions, including Australia, national guidelines do not often recommend that a specific profession must be responsible for a task, unless the task is limited to the scope of one profession alone. In contrast, in the Netherlands where the central role of family doctors is prescribed within the health system, family doctors are likely to have a foundational role in all guidelines that are produced. The role of guidelines and their development varies between nations and health systems and the centrality of the role of the family doctor in a guideline may reflect the strength of primary care in the specific healthcare system. Therefore, guidelines may not always be the definitive source for determining the clinical scope and responsibilities of specific professional groups such as family doctors in obesity care.
Implications for research
Poor descriptions of interventions could have been aided by adherence to the TIDieR guidelines.15 Specifically, the TIDieR guidelines suggest the health professionals involved in an intervention should be described in terms of their professional background, their expertise and any specific training given. The terms used to describe a family doctor were diverse in the intervention papers and ranged from primary care physician, primary care provider, family physician or general practitioner. The range of terms that are used in the primary care literature makes it impossible to understand the qualifications of professionals involved in the interventions. Trials from the USA often use ‘primary care providers’ or ‘primary care practitioners’, nebulous terms that could include a variety of professionals with vastly different training. This is particularly problematic when international primary care teams attempt to translate interventions to their local context. An international taxonomy for describing family doctors could assist in solving this issue.
The primary care literature has thoroughly described the fundamental factors that make primary care effective.9 However, it was challenging for reviewers to determine if interventions were inclusive of the principles of person-centredness and whole person care. Knowing that first point of contact, whole person, coordinated, person-centred, continuous care, is important in primary care; it would be helpful for primary care interventions to explicitly consider these factors in their design. Additionally, the specific reporting of these factors in primary care trials would be helpful in publications to improve the understanding of how and why primary care interventions work. It is perhaps important that primary care determines a specific set of reporting requirements for primary care research that could be added to the TIDieR checklist.
Limitations
This scoping review is limited to the context of obesity management in primary care. Articles that reported on other important and related topics like nutrition, lifestyle change or cardiovascular health were not included. We chose to limit the review to obesity as we were interested in this specific literature and wanted to maintain the depth of our data extraction while maintaining feasibility. The review was also limited to publications in the English language and this may have missed work that included family doctors in non-English speaking healthcare settings. We may have missed international guidelines that were not picked up in our search strategy. As expected in a scoping review, articles were not assessed for quality or the specific outcomes of reported trials. Further work would have to be done from the identified literature and this could include a thematic analysis. The aim of the scoping review is to widely and broadly search the literature to identify gaps and inconsistencies, and provide a platform for further systematic work.20
Conclusion
There appears to be a disconnect between how family doctors are involved in primary care interventions, the message that is found in academic literature and the apparent role of the family doctor in current practice. Guidelines that are developed by national bodies are not necessarily the definitive source of information for the discrete role of specific health professionals. Improvement is required in the reporting of primary care interventions, particularly in the professional background of those involved in the trial and the acknowledgement of the pillars of primary care in intervention development. This foundation work provides a platform for further interpretation of existing literature on the role of the family doctor in obesity management.
Supplementary Material
Acknowledgments
Dr Ginny Sargent is thanked for her assistance in developing the protocol, feedback on the final analysis and review of the manuscript.
Footnotes
Twitter: @LizSturgiss
Contributors: EAS, NE, EH, CvW and KAD were part of the development and publication of the protocol. EAS and NE were involved in the search and data extraction. EH was the third author to check the data extraction tool. EAS and NE did the initial analysis and synthesis. EAS and NE presented the findings of the scoping review at the stakeholder sessions. EAS wrote the first draft of the manuscript. EAS, NE, EH, CvW and KAD then contributed to the writing of the manuscript and approved the final version.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Further data about the studies that were excluded from the scoping review are available by request from the authors. All data regarding included studies are included in this paper and no additional data on these studies are available.
References
- 1.National Health and Medical Research Council. National Health and Medical Research Council Clinical practice guidelines for the management of overweight and obesity in adults, adolescents and children in Australia. : Melbourne: National Health and Medical Research Council, 2013. [Google Scholar]
- 2.Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37–43. 10.1016/S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 3.Bayliss EA. Simplifying care for complex patients. Ann Fam Med 2012;10:3–5. 10.1370/afm.1352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tan D, Zwar NA, Dennis SM, et al. Weight management in general practice: what do patients want? Med J Aust 2006;185:73–5. [DOI] [PubMed] [Google Scholar]
- 5.Sturgiss EA, van Weel C, Ball L, et al. Obesity management in Australian primary care: where has the general practitioner gone? Aust J Prim Health 2016;22:473 10.1071/PY16074 [DOI] [PubMed] [Google Scholar]
- 6.Jansen S, Desbrow B, Ball L. Obesity management by general practitioners: the unavoidable necessity. Aust J Prim Health 2015;21:366–8. 10.1071/PY15018 [DOI] [PubMed] [Google Scholar]
- 7.Clark AM, Briffa TG, Thirsk L, et al. What football teaches us about researching complex health interventions. BMJ 2012;345:e8316 10.1136/bmj.e8316 [DOI] [PubMed] [Google Scholar]
- 8.Wong G, Westhorp G, Manzano A, et al. RAMESES II reporting standards for realist evaluations. BMC Med 2016;14:96 10.1186/s12916-016-0643-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stange KC. Barbara Starfield: passage of the pathfinder of primary care. Ann Fam Med 2011;9:292–6. 10.1370/afm.1293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Radcliffe Publishing. Chapter 1: Meeting people’s health needs : Kidd M, The contribution of family medicine to improving health systems: a guidebook from the World Organization of Family Doctors. 2nd Edn London: Radcliffe Publishing, 2013:1–13. [Google Scholar]
- 11.Stange KC. A science of connectedness. Ann Fam Med 2009;7:387–95. 10.1370/afm.990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stange KC. The paradox of the parts and the whole in understanding and improving general practice. Int J Qual Health Care 2002;14:267–8. 10.1093/intqhc/14.4.267 [DOI] [PubMed] [Google Scholar]
- 13.Gray DP, Evans P, Sweeney K, et al. Towards a theory of continuity of care. J R Soc Med 2003;96:160–6. 10.1177/014107680309600402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sturgiss EA, Elmitt N, van Weel C, et al. The role of the family doctor in the management of adults who are obese: a scoping review protocol. Springerplus 2015;4:820 10.1186/s40064-015-1647-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- 16.Wadden TA, Volger S, Sarwer DB, et al. A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med 2011;365:1969–79. 10.1056/NEJMoa1109220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pfadenhauer LM, Gerhardus A, Mozygemba K, et al. Making sense of complexity in context and implementation: the Context and Implementation of Complex Interventions (CICI) framework. Implement Sci 2017;12:21 10.1186/s13012-017-0552-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shi L. The Impact of Primary Care: A Focused Review. Scientifica 2012;2012:22–22. 10.6064/2012/432892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Woolf S, Schünemann HJ, Eccles MP, et al. Developing clinical practice guidelines: types of evidence and outcomes; values and economics, synthesis, grading, and presentation and deriving recommendations. Implement Sci 2012;7:61 10.1186/1748-5908-7-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The Joanna Briggs Institute. The Joanna Briggs Institute Reviewers’ Manual 2015 Methodology for JBI Scoping Reviews. Adelaide, Australia: Joanna Briggs Institute, 2015. [Google Scholar]
- 21.Ashley JM, St Jeor ST, Perumean-Chaney S, et al. Meal replacements in weight intervention. Obes Res 2001;9 Suppl 4(Suppl 4):312S–20. 10.1038/oby.2001.136 [DOI] [PubMed] [Google Scholar]
- 22.Ashley JM, St Jeor ST, Schrage JP, et al. Weight control in the physician’s office. Arch Intern Med 2001;161:1599–604. 10.1001/archinte.161.13.1599 [DOI] [PubMed] [Google Scholar]
- 23. A new evidence-based model for weight management in primary care: The Counterweight Programme. Journal of Human Nutrition and Dietetics 2004;17:191–208. [DOI] [PubMed] [Google Scholar]
- 24.Counterweight Project Team. The implementation of the Counterweight Programme in Scotland, UK. Fam Pract 2012;29 Suppl 1(Suppl 1):I139–I44. 10.1093/fampra/cmr074 [DOI] [PubMed] [Google Scholar]
- 25.Laws R; Counterweight Project Team. Current approaches to obesity management in UK Primary Care: the Counterweight Programme. J Hum Nutr Diet 2004;17:183-90 10.1111/j.1365-277X.2004.00528.x [DOI] [PubMed] [Google Scholar]
- 26.Laws R; Counterweight Project Team. A new evidence-based model for weight management in primary care: the Counterweight Programme. J Hum Nutr Diet 2004;17:191-208 10.1111/j.1365-277X.2004.00517.x [DOI] [PubMed] [Google Scholar]
- 27.McQuigg M, Brown J, Broom J, et al. Empowering primary care to tackle the obesity epidemic: the Counterweight Programme. Eur J Clin Nutr 2005;59 Suppl 1(SUPPL. 1):S93–S101. 10.1038/sj.ejcn.1602180 [DOI] [PubMed] [Google Scholar]
- 28.McQuigg M, Brown JE, Broom J, et al. The Counterweight programme: Prevalence of CVD risk factors by body mass index and the impact of 10% weight change. Obes Res Clin Pract 2008;2:15–27. 10.1016/j.orcp.2008.01.002 [DOI] [PubMed] [Google Scholar]
- 29.McQuigg M, Brown JE, Broom JI, et al. Engaging patients, clinicians and health funders in weight management: the Counterweight Programme. Fam Pract 2008;25 Suppl 1(Suppl 1):i79–86. 10.1093/fampra/cmn081 [DOI] [PubMed] [Google Scholar]
- 30.Bolognesi M, Nigg CR, Massarini M, et al. Reducing obesity indicators through brief physical activity counseling (PACE) in Italian primary care settings. Ann Behav Med 2006;31:179–85. 10.1207/s15324796abm3102_10 [DOI] [PubMed] [Google Scholar]
- 31.Bodenlos JS. Impact of a stage-matched weight loss intervention on stage of change progression in predominantly African-American female primary care patients. Dissertation Abstracts International: Section B: The Sciences and Engineering 2007;67:7364. [Google Scholar]
- 32.Kerr J, Patrick K, Norman G, et al. Randomized control trial of a behavioral intervention for overweight women: impact on depressive symptoms. Depress Anxiety 2008;25:555–8. 10.1002/da.20320 [DOI] [PubMed] [Google Scholar]
- 33.Bennett GG, Warner ET, Glasgow RE, et al. Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Arch Intern Med 2012;172:565–74. 10.1001/archinternmed.2012.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ritzwoller DP, Glasgow RE, Sukhanova AY, et al. Economic analyses of the Be Fit Be Well program: a weight loss program for community health centers. J Gen Intern Med 2013;28:1581–8. 10.1007/s11606-013-2492-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Greaney ML, Quintiliani LM, Warner ET, et al. Weight Management Among Patients at Community Health Centers: The “Be Fit, Be Well” Study. Obes Weight Manag 2009;5:222–8. 10.1089/obe.2009.0507 [DOI] [Google Scholar]
- 36.Appel LJ, Clark JM, Yeh HC, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med 2011;365:1959–68. 10.1056/NEJMoa1108660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bennett WL, Gudzune KA, Appel LJ, et al. Insights from the POWER practice-based weight loss trial: a focus group study on the PCP’s role in weight management. J Gen Intern Med 2014;29:50–8. 10.1007/s11606-013-2562-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bennett WL, Wang NY, Gudzune KA, et al. Satisfaction with primary care provider involvement is associated with greater weight loss: Results from the practice-based POWER trial. Patient Educ Couns 2015;98:1099–105. 10.1016/j.pec.2015.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jerome GJ, Yeh H-C, Dalcin A, et al. Treatment of Obesity in Primary Care Practice: The Practice Based Opportunities for Weight Reduction (POWER) Trial at Johns Hopkins. Obes Weight Manag 2009;5:216–21. 10.1089/obe.2009.0506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alfaris N, Wadden TA, Sarwer DB, et al. Effects of a 2-year behavioral weight loss intervention on sleep and mood in obese individuals treated in primary care practice. Obesity 2015;23:558–64. 10.1002/oby.20996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tsai AG, Wadden TA, Volger S, et al. Cost-effectiveness of a primary care intervention to treat obesity. Int J Obes 2013;37:S31–S37. 10.1038/ijo.2013.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sarwer DB, Moore RH, Diewald LK, et al. The impact of a primary care-based weight loss intervention on the quality of life. Int J Obes 2013;37 Suppl 1(Supp 1):S25–S30. 10.1038/ijo.2013.93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Derbas J, Vetter M, Volger S, et al. Improving Weight Management in Primary Care Practice: A Possible Role for Auxiliary Health Professionals Collaborating with Primary Care Physicians. Obes Weight Manag 2009;5:210–5. 10.1089/obe.2009.0505 [DOI] [Google Scholar]
- 44.Volger S, Wadden TA, Sarwer DB, et al. Changes in eating, physical activity and related behaviors in a primary care-based weight loss intervention. Int J Obes 2013;37 Suppl 1:S12–S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vetter ML, Wadden TA, Chittams J, et al. Effect of lifestyle intervention on cardiometabolic risk factors: results of the POWER-UP trial. Int J Obes 2013;37 Suppl 1(Suppl 1):S19–S24. 10.1038/ijo.2013.92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wadden TA, Volger S, Tsai AG, et al. Managing obesity in primary care practice: an overview with perspective from the POWER-UP study. Int J Obes 2013;37 Suppl 1(Suppl 1):S3–S11. 10.1038/ijo.2013.90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tsai AG, Wadden TA, Rogers MA, et al. A primary care intervention for weight loss: results of a randomized controlled pilot study. Obesity 2010;18:1614–8. 10.1038/oby.2009.457 [DOI] [PubMed] [Google Scholar]
- 48.Banerjee ES, Gambler A, Fogleman C. Adding obesity to the problem list increases the rate of providers addressing obesity. Fam Med 2013;45:629–33. [PubMed] [Google Scholar]
- 49.Blonstein AC, Yank V, Stafford RS, et al. Translating an evidence-based lifestyle intervention program into primary care: lessons learned. Health Promot Pract 2013;14:491–7. 10.1177/1524839913481604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barnes ER, Theeke LA, Mallow J. Impact of the Provider and Healthcare team Adherence to Treatment Guidelines (PHAT-G) intervention on adherence to national obesity clinical practice guidelines in a primary care centre. J Eval Clin Pract 2015;21:300–6. 10.1111/jep.12308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Booth AO, Nowson CA, Huang N, et al. Evaluation of a brief pilot nutrition and exercise intervention for the prevention of weight gain in general practice patients. Public Health Nutr 2006;9:1055–61. 10.1017/PHN2006980 [DOI] [PubMed] [Google Scholar]
- 52.Bordowitz R, Morland K, Reich D. The use of an electronic medical record to improve documentation and treatment of obesity. Fam Med 2007;39:274–9. [PubMed] [Google Scholar]
- 53.Bowerman S, Bellman M, Saltsman P, et al. Implementation of a primary care physician network obesity management program. Obes Res 2001;9 Suppl 4:321S–5. 10.1038/oby.2001.137 [DOI] [PubMed] [Google Scholar]
- 54.Clark D, Chrysler L, Perkins A, et al. Screening, referral, and participation in a weight management program implemented in five CHCs. J Health Care Poor Underserved 2010;21:617–28. 10.1353/hpu.0.0319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Clark DO, Keith N, Chrysler L, et al. Design and reach of a primary care weight management program. J Health Care Poor Underserved 2008;19:171–9. 10.1353/hpu.2008.0014 [DOI] [PubMed] [Google Scholar]
- 56.Coupar AM, Kennedy T. Running a weight control group: experiences of a psychologist and a general practitioner. J R Coll Gen Pract 1980;30:41–8. [PMC free article] [PubMed] [Google Scholar]
- 57.Cutler L, King B, McCarthy N, et al. Appetite for life: an evaluation of a primary care lifestyle programme. J Prim Health Care 2010;2:281–7. [PubMed] [Google Scholar]
- 58.Doering T, Harwell S, Fassler C, et al. An interventional pilot study on obesity among low-income patients using a computer-based weight management module. J Community Hosp Intern Med Perspect 2013;3:20072 10.3402/jchimp.v3i1.20072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dutton GR, Phillips JM, Kukkamalla M, et al. Pilot study evaluating the feasibility and initial outcomes of a primary care weight loss intervention with peer coaches. Diabetes Educ 2015;41:361–8. 10.1177/0145721715575356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Eichler K, Zoller M, Steurer J, et al. Cognitive-behavioural treatment for weight loss in primary care: a prospective study. Swiss Med Wkly 2007;137(35-36):489–95. doi:2007/35/smw-11873 [DOI] [PubMed] [Google Scholar]
- 61.Ely AC, Banitt A, Befort C, et al. Kansas primary care weighs in: a pilot randomized trial of a chronic care model program for obesity in 3 rural Kansas primary care practices. J Rural Health 2008;24:125–32. 10.1111/j.1748-0361.2008.00148.x [DOI] [PubMed] [Google Scholar]
- 62.Feigenbaum A, Pasternak S, Zusk E, et al. Influence of intense multidisciplinary follow-up and orlistat on weight reduction in a primary care setting. BMC Fam Pract 2005;6:5 10.1186/1471-2296-6-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kanke S, Kawai T, Takasawa N, et al. Interventions for body weight reduction in obese patients during short consultations: an open-label randomized controlled trial in the Japanese primary care setting. Asia Pac Fam Med 2015;14:5 10.1186/s12930-015-0022-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fuller NR, Colagiuri S, Schofield D, et al. A within-trial cost-effectiveness analysis of primary care referral to a commercial provider for weight loss treatment, relative to standard care--an international randomised controlled trial. Int J Obes 2013;37:828–34. 10.1038/ijo.2012.139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Holzapfel C, Cresswell L, Ahern AL, et al. The challenge of a 2-year follow-up after intervention for weight loss in primary care. Int J Obes 2014;38:806–11. 10.1038/ijo.2013.180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jebb SA, Ahern AL, Olson AD, et al. Primary care referral to a commercial provider for weight loss treatment versus standard care: a randomised controlled trial. Lancet 2011;378:1485–92. 10.1016/S0140-6736(11)61344-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Huerta S, Li Z, Li HC, Hc L, et al. Feasibility of a partial meal replacement plan for weight loss in low-income patients. Int J Obes Relat Metab Disord 2004;28:1575–9. 10.1038/sj.ijo.0802792 [DOI] [PubMed] [Google Scholar]
- 68.Garies S, Irving A, Williamson T, et al. Using EMR data to evaluate a physician-developed lifestyle plan for obese patients in primary care. Can Fam Physician 2015;61:e225–e31. [PMC free article] [PubMed] [Google Scholar]
- 69.Gusi N, Reyes MC, Gonzalez-Guerrero JL, et al. Cost-utility of a walking programme for moderately depressed, obese, or overweight elderly women in primary care: a randomised controlled trial. BMC Public Health 2008;8:231 10.1186/1471-2458-8-231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Haas WC, Moore JB, Kaplan M, et al. Outcomes from a medical weight loss program: primary care clinics versus weight loss clinics. Am J Med 2012;125:603.e7–603.e11. 10.1016/j.amjmed.2011.07.039 [DOI] [PubMed] [Google Scholar]
- 71.Crawford-Faucher A. Which weight-loss programs are most effective? American Family Physician 2012;86:280–2. [Google Scholar]
- 72.Jolly K, Daley A, Adab P, et al. A randomised controlled trial to compare a range of commercial or primary care led weight reduction programmes with a minimal intervention control for weight loss in obesity: the Lighten Up trial. BMC Public Health 2010;10:439 10.1186/1471-2458-10-439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jolly K, Lewis A, Beach J, et al. Comparison of range of commercial or primary care led weight reduction programmes with minimal intervention control for weight loss in obesity: lighten Up randomised controlled trial. BMJ 2011;343:d6500 10.1136/bmj.d6500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hauner H, Meier M, Wendland G, et al. Weight reduction by sibutramine in obese subjects in primary care medicine: the SAT Study. Exp Clin Endocrinol Diabetes 2004;112:201–7. 10.1055/s-2004-817934 [DOI] [PubMed] [Google Scholar]
- 75.Hoke CN, Franks S. Work site, physician’s office, or medical university clinic: the effect of setting on success in a multidisciplinary weight-loss program. Eat Behav 2002;3:93–100. [DOI] [PubMed] [Google Scholar]
- 76.Kumanyika S, Fassbender J, Phipps E, et al. Design, recruitment and start up of a primary care weight loss trial targeting African American and Hispanic adults. Contemp Clin Trials 2011;32:215–24. 10.1016/j.cct.2010.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kumanyika SK, Fassbender JE, Sarwer DB, et al. One-year results of the Think Health! study of weight management in primary care practices. Obesity 2012;20:1249–57. 10.1038/oby.2011.329 [DOI] [PubMed] [Google Scholar]
- 78.Kuppersmith NC, Miles TP. Effect of a BMI chart on weight management discussions in a primary care setting. J Ky Med Assoc 2006;104:519–22. [PubMed] [Google Scholar]
- 79.Laing BY, Mangione CM, Tseng CH, et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients: a randomized, controlled trial. Ann Intern Med 2014;161(10 Suppl):S5–12. 10.7326/M13-3005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lewis A, Jolly K, Adab P, et al. A brief intervention for weight management in primary care: study protocol for a randomized controlled trial. Trials 2013;14:393 10.1186/1745-6215-14-393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Logue E, Sutton K, Jarjoura D, et al. Obesity management in primary care: assessment of readiness to change among 284 family practice patients. J Am Board Fam Pract 2000;13:164–71. 10.3122/15572625-13-3-164 [DOI] [PubMed] [Google Scholar]
- 82.Logue E, Sutton K, Jarjoura D, et al. Transtheoretical model-chronic disease care for obesity in primary care: a randomized trial. Obes Res 2005;13:917–27. 10.1038/oby.2005.106 [DOI] [PubMed] [Google Scholar]
- 83.Logue EE, Bourguet CC, Palmieri PA, et al. The better weight-better sleep study: a pilot intervention in primary care. Am J Health Behav 2012;36:319–34. 10.5993/AJHB.36.3.4 [DOI] [PubMed] [Google Scholar]
- 84.Lowe MR, Butryn ML, Thomas JG, et al. Meal replacements, reduced energy density eating, and weight loss maintenance in primary care patients: a randomized controlled trial. Obesity 2014;22:94–100. 10.1002/oby.20582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Madigan CD, Jolly K, Lewis AL, et al. A randomised controlled trial of the effectiveness of self-weighing as a weight loss intervention. Int J Behav Nutr Phys Act 2014;11:11 10.1186/s12966-014-0125-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Martin PD, Rhode PC, Dutton GR, et al. A primary care weight management intervention for low-income African-American women. Obesity 2006;14:1412–20. 10.1038/oby.2006.160 [DOI] [PubMed] [Google Scholar]
- 87.Martin PD, Dutton GR, Rhode PC, et al. Weight loss maintenance following a primary care intervention for low-income minority women. Obesity 2008;16:2462–7. 10.1038/oby.2008.399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.McDoniel SO, Wolskee P, Shen J. Treating obesity with a novel hand-held device, computer software program, and Internet technology in primary care: the SMART motivational trial. Patient Educ Couns 2010;79:185–91. 10.1016/j.pec.2009.07.034 [DOI] [PubMed] [Google Scholar]
- 89.McDoniel S. The short-term effect of a technology based comprehensive weight reduction program for obese adults in a primary care medical clinic: A three month psychobehavioral study. 2008.
- 90.Mehring M, Haag M, Linde K, et al. Effects of a general practice guided web-based weight reduction program--results of a cluster-randomized controlled trial. BMC Fam Pract 2013;14:76 10.1186/1471-2296-14-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Munsch S, Biedert E, Keller U. Evaluation of a lifestyle change programme for the treatment of obesity in general practice. Swiss Med Wkly 2003;133:133148–54. doi:2003/09/smw-10109 [DOI] [PubMed] [Google Scholar]
- 92.O’Grady JS, Thacher TD, Chaudhry R. The effect of an automated clinical reminder on weight loss in primary care. J Am Board Fam Med 2013;26:745–50. 10.3122/jabfm.2013.06.120340 [DOI] [PubMed] [Google Scholar]
- 93.Olsen J, Willaing I, Ladelund S, et al. Cost-effectiveness of nutritional counseling for obese patients and patients at risk of ischemic heart disease. Int J Technol Assess Health Care 2005;21:194–202. [PubMed] [Google Scholar]
- 94.Pellegrini CA, Hoffman SA, Collins LM, et al. Optimization of remotely delivered intensive lifestyle treatment for obesity using the Multiphase Optimization Strategy: Opt-IN study protocol. Contemp Clin Trials 2014;38:251–9. 10.1016/j.cct.2014.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Richman RM, Webster P, Salgo AR, et al. A shared care approach in obesity management: the general practitioner and a hospital based service. Int J Obes Relat Metab Disord 1996;20:413–9. [PubMed] [Google Scholar]
- 96.Ross R, Lam M, Blair SN, et al. Trial of prevention and reduction of obesity through active living in clinical settings: a randomized controlled trial. Arch Intern Med 2012;172:414–24. 10.1001/archinternmed.2011.1972 [DOI] [PubMed] [Google Scholar]
- 97.Ross R, Blair SN, Godwin M, et al. Prevention and Reduction of Obesity through Active Living (PROACTIVE): rationale, design and methods. Br J Sports Med 2009;43:57–63. 10.1136/bjsm.2008.053504 [DOI] [PubMed] [Google Scholar]
- 98.Rutten GM, Meis JJ, Hendriks MR, et al. The contribution of lifestyle coaching of overweight patients in primary care to more autonomous motivation for physical activity and healthy dietary behaviour: results of a longitudinal study. Int J Behav Nutr Phys Act 2014;11:11 10.1186/s12966-014-0086-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Saris WH, Koenders MC, Pannemans DL, et al. Outcome of a multicenter outpatient weight-management program including very-low-calorie diet and exercise. Am J Clin Nutr 1992;56:294S–6. 10.1093/ajcn/56.1.294S [DOI] [PubMed] [Google Scholar]
- 100.Stephens GS, Blanken SE, Greiner KA, et al. Visual prompt poster for promoting patient-physician conversations on weight loss. Ann Fam Med 2008;6 Suppl 1(SUPPL. 1):S33–S36. 10.1370/afm.780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Driehuis F, Barte JC, Ter Bogt NC, et al. Maintenance of lifestyle changes: 3-year results of the Groningen Overweight and Lifestyle study. Patient Educ Couns 2012;88:249–55. 10.1016/j.pec.2012.03.017 [DOI] [PubMed] [Google Scholar]
- 102.Barte JC, ter Bogt NC, Beltman FW, et al. Process evaluation of a lifestyle intervention in primary care: implementation issues and the participants' satisfaction of the GOAL study. Health Educ Behav 2012;39:564–73. 10.1177/1090198111422936 [DOI] [PubMed] [Google Scholar]
- 103.ter Bogt NC, Bemelmans WJ, Beltman FW, et al. Preventing weight gain: one-year results of a randomized lifestyle intervention. Am J Prev Med 2009;37:270–7. 10.1016/j.amepre.2009.06.011 [DOI] [PubMed] [Google Scholar]
- 104.ter Bogt NC, Bemelmans WJ, Beltman FW, et al. Preventing weight gain by lifestyle intervention in a general practice setting: three-year results of a randomized controlled trial. Arch Intern Med 2011;171:306–13. 10.1001/archinternmed.2011.22 [DOI] [PubMed] [Google Scholar]
- 105.ter Bogt NC, Milder IE, Bemelmans WJ, et al. Changes in lifestyle habits after counselling by nurse practitioners: 1-year results of the Groningen Overweight and Lifestyle study. Public Health Nutr 2011;14:995–1000. 10.1017/S1368980010003708 [DOI] [PubMed] [Google Scholar]
- 106.Thomas JG, Leahey TM, Wing RR. An automated internet behavioral weight-loss program by physician referral: a randomized controlled trial. Diabetes Care 2015;38:9–15. 10.2337/dc14-1474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Toth-Capelli KM, Brawer R, Plumb J, et al. Stage of change and other predictors of participant retention in a behavioral weight management program in primary care. Health Promot Pract 2013;14:441–50. 10.1177/1524839912460871 [DOI] [PubMed] [Google Scholar]
- 108.Tsai AG, Felton S, Hill JO, et al. A randomized pilot trial of a full subsidy vs. a partial subsidy for obesity treatment. Obesity 2012;20:1838–43. 10.1038/oby.2011.193 [DOI] [PubMed] [Google Scholar]
- 109.Wadden TA, Berkowitz RI, Womble LG, et al. Randomized trial of lifestyle modification and pharmacotherapy for obesity. N Engl J Med 2005;353:2111–20. 10.1056/NEJMoa050156 [DOI] [PubMed] [Google Scholar]
- 110.Wilson DB, Johnson RE, Jones RM, et al. Patient weight counseling choices and outcomes following a primary care and community collaborative intervention. Patient Educ Couns 2010;79:338–43. 10.1016/j.pec.2010.01.025 [DOI] [PubMed] [Google Scholar]
- 111.Wirth A. Reduction of body weight and co-morbidities by orlistat: The XXL - Primary Health Care Trial. Diabetes, Obesity and Metabolism 2005;7:21–7. 10.1111/j.1463-1326.2004.00428.x [DOI] [PubMed] [Google Scholar]
- 112.Yardley L, Ware LJ, Smith ER, et al. Randomised controlled feasibility trial of a web-based weight management intervention with nurse support for obese patients in primary care. Int J Behav Nutr Phys Act 2014;11:67 10.1186/1479-5868-11-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Tsai AG, Felton S, Wadden TA, et al. A randomized clinical trial of a weight loss maintenance intervention in a primary care population. Obesity 2015;23:2015–21. 10.1002/oby.21224 [DOI] [PubMed] [Google Scholar]
- 114.Ryan DH, Johnson WD, Myers VH, et al. Nonsurgical weight loss for extreme obesity in primary care settings: results of the Louisiana Obese Subjects Study. Arch Intern Med 2010;170:146–54. 10.1001/archinternmed.2009.508 [DOI] [PubMed] [Google Scholar]
- 115.Baillargeon JP, Carpentier A, Donovan D, et al. Integrated obesity care management system -implementation and research protocol. BMC Health Serv Res 2007;7:163 10.1186/1472-6963-7-163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Baillargeon JP, St-Cyr-Tribble D, Xhignesse M, et al. Impact of an integrated obesity management system on patient’s care - research protocol. BMC Obes 2014;1:19 10.1186/s40608-014-0019-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Katz S, Feigenbaum A, Pasternak S, et al. An interactive course to enhance self-efficacy of family practitioners to treat obesity. BMC Med Educ 2005;5:4 10.1186/1472-6920-5-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Buclin-Thiébaud S, Pataky Z, Bruchez V, et al. New psycho-pedagogic approach to obesity treatment: a 5-year follow-up. Patient Educ Couns 2010;79:333–7. 10.1016/j.pec.2009.11.001 [DOI] [PubMed] [Google Scholar]
- 119.Feuerstein J, Takayasu K, Maltz A, et al. Teaching a lifestyle intervention for reversing impaired fasting glucose, hyperlipidemia and obesity/overweight to a cohort of local physicians. Current Nutrition and Food Science 2015;11:65–9. 10.2174/1573401311666150113001304 [DOI] [Google Scholar]
- 120.Hartman SJ, Risica PM, Gans KM, et al. Tailored weight loss intervention in obese adults within primary care practice: rationale, design, and methods of Choose to Lose. Contemp Clin Trials 2014;38:409–19. 10.1016/j.cct.2014.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lin M, Mahmooth Z, Dedhia N, et al. Tailored, interactive text messages for enhancing weight loss among African American adults: the TRIMM randomized controlled trial. Am J Med 2015;128:896–904. 10.1016/j.amjmed.2015.03.013 [DOI] [PubMed] [Google Scholar]
- 122.Moore H, Summerbell CD, Greenwood DC, et al. Improving management of obesity in primary care: cluster randomised trial. BMJ 2003;327:1085 10.1136/bmj.327.7423.1085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Rodondi N, Humair JP, Ghali WA, et al. Counselling overweight and obese patients in primary care: a prospective cohort study. Eur J Cardiovasc Prev Rehabil 2006;13:222–8. 10.1097/01.hjr.0000209819.13196.a4 [DOI] [PubMed] [Google Scholar]
- 124.Rueda-Clausen CF, Benterud E, Bond T, et al. Effect of implementing the 5As of obesity management framework on provider-patient interactions in primary care. Clin Obes 2014;4:39–44. 10.1111/cob.12038 [DOI] [PubMed] [Google Scholar]
- 125.Schuster RJ, Tasosa J, Terwoord NA. Translational research--implementation of NHLBI Obesity Guidelines in a primary care community setting: the Physician Obesity Awareness Project. J Nutr Health Aging 2008;12:764s–9. [DOI] [PubMed] [Google Scholar]
- 126.Yank V, Stafford RS, Rosas LG, et al. Baseline reach and adoption characteristics in a randomized controlled trial of two weight loss interventions translated into primary care: a structured report of real-world applicability. Contemp Clin Trials 2013;34:126–35. 10.1016/j.cct.2012.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Goodyear-Smith F, McPhee J, Duncan S, et al. Evaluation of a primary care-based programme designed to increase exercise and improve nutrition in patients at risk. J Prim Health Care 2014;6:312–8. [PubMed] [Google Scholar]
- 128.Jay MR, Gillespie CC, Schlair SL, et al. The impact of primary care resident physician training on patient weight loss at 12 months. Obesity 2013;21:45–50. 10.1002/oby.20237 [DOI] [PubMed] [Google Scholar]
- 129.Wadden TA, Berkowitz RI, Vogt RA, et al. Lifestyle modification in the pharmacologic treatment of obesity: a pilot investigation of a potential primary care approach. Obes Res 1997;5:218–26. 10.1002/j.1550-8528.1997.tb00296.x [DOI] [PubMed] [Google Scholar]
- 130.Anderson DA, Wadden TA. Treating the obese patient. Suggestions for primary care practice. Arch Fam Med 1999;8:156–67. 10.1001/archfami.8.2.156 [DOI] [PubMed] [Google Scholar]
- 131.Rao G. Office-based strategies for the management of obesity. Am Fam Physician 2010;81:1449–56. quiz 29. [PubMed] [Google Scholar]
- 132.Simkin-Silverman LR, Conroy MB, King WC. Treatment of Overweight and Obesity in Primary Care Practice: Current Evidence and Future Directions. Am J Lifestyle Med 2008;2:296–304. 10.1177/1559827608317287 [DOI] [Google Scholar]
- 133.Logue EE, Smucker WD. Obesity management in primary care: changing the status quo. J Fam Pract 2001;50:520. [PubMed] [Google Scholar]
- 134.Lyznicki JM, Young DC, Riggs JA, et al. Obesity: assessment and management in primary care. Am Fam Physician 2001;63:2185–96. [PubMed] [Google Scholar]
- 135.Sherman R, Crocker B, Dill D, et al. Health coaching integration into primary care for the treatment of obesity. Glob Adv Health Med 2013;2:58–60. 10.7453/gahmj.2013.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Vallis M, Piccinini-Vallis H, Sharma AM, et al. Clinical review: modified 5 As: minimal intervention for obesity counseling in primary care. Can Fam Physician 2013;59:e1-e5 27–31. [PMC free article] [PubMed] [Google Scholar]
- 137.Benotti P. Patient Preparation for Bariatric Surgery. USA: Springer, 2014. [Google Scholar]
- 138.Brown W, Korin A, Burton P, et al. Laparoscopic adjustable gastric banding. Aust Fam Physician 2009;38:972–6. [PubMed] [Google Scholar]
- 139.Choban PS, Jackson B, Poplawski S, et al. Bariatric surgery for morbid obesity: why, who, when, how, where, and then what? Cleve Clin J Med 2002;69:897–903. 10.3949/ccjm.69.11.897 [DOI] [PubMed] [Google Scholar]
- 140.DeMaria EJ. Bariatric surgery for morbid obesity. N Engl J Med 2007;356:2176–83. 10.1056/NEJMct067019 [DOI] [PubMed] [Google Scholar]
- 141.Dixon JB. Referral for a bariatric surgical consultation: it is time to set a standard of care. Obes Surg 2009;19:641–4. 10.1007/s11695-008-9765-7 [DOI] [PubMed] [Google Scholar]
- 142.Heber D, Greenway FL, Kaplan LM, et al. Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2010;95:4823–43. 10.1210/jc.2009-2128 [DOI] [PubMed] [Google Scholar]
- 143.Karmali S, Johnson Stoklossa C, Sharma A, et al. Bariatric surgery: a primer. Can Fam Physician 2010;56:873–9. [PMC free article] [PubMed] [Google Scholar]
- 144.Pietras SM, Usdan LS, Apovian CM. Preoperative and Postoperative Management of the Bariatric Surgical Patient. JCOM 2007;14:262–74. [Google Scholar]
- 145.Richardson LA. Bariatric society is here to help. J Fam Pract 2010;59:488. [PubMed] [Google Scholar]
- 146.Shafipour P, Der-Sarkissian JK, Hendee FN, et al. What do I do with my morbidly obese patient? A detailed case study of bariatric surgery in kaiser permanente southern california. Perm J 2009;13:56–63. 10.7812/TPP/08-067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Snow V, Barry P, Fitterman N, et al. Pharmacologic and surgical management of obesity in primary care: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2005;142:525–31. 10.7326/0003-4819-142-7-200504050-00011 [DOI] [PubMed] [Google Scholar]
- 148.Van Sickle KR. Management of the challenging bariatric surgical patient. Med Clin North Am 2007;91:383–92. 10.1016/j.mcna.2007.02.003 [DOI] [PubMed] [Google Scholar]
- 149.Virji A, Murr MM. Caring for patients after bariatric surgery. Am Fam Physician 2006;73:1403–8. [PubMed] [Google Scholar]
- 150.Wilbert B, Mohundro BL, Shaw V, Andres A, et al. Appetite suppressants as adjuncts for weight loss. Am Fam Physician 2011;83:1–2. [PubMed] [Google Scholar]
- 151.Kolasa KM, Collier DN, Cable K. Weight loss strategies that really work. J Fam Pract 2010;59:378–85. [PubMed] [Google Scholar]
- 152.Mercer S. How useful are clinical guidelines for the management of obesity in general practice? Br J Gen Pract 2009;59:863–8. 10.3399/bjgp09X472917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Agency NHD. Care pathways for the prevention and management of obesity. London, UK: Health Development Agency, 2004. [Google Scholar]
- 154.Agrawal M, Worzniak M, Diamond L. Managing obesity like any other chronic condition. Long-term therapy may reduce comorbidity as well. Postgrad Med 2000;108:75–82. 10.3810/pgm.2000.07.1158 [DOI] [PubMed] [Google Scholar]
- 155.Brunton SA, Skolnik NS, Ryan DH, et al. Management of obesity in adults. The Journal of Family Practice 2014;63:S1–S33. [PubMed] [Google Scholar]
- 156.Bartlett SJ. Motivating patients toward weight loss: practical strategies for addressing overweight and obesity. Phys Sportsmed 2003;31:29–36. 10.3810/psm.2003.11.556 [DOI] [PubMed] [Google Scholar]
- 157.Benjamin RM, Yanovski SZ, Simons-Morton DG. Can primary care physician-driven community programs address the obesity epidemic among high-risk populations? JAMA Intern Med 2013;173:1778–9. 10.1001/jamainternmed.2013.7776 [DOI] [PubMed] [Google Scholar]
- 158.Birmingham CL, Jones P, Hoffer LJ. The management of adult obesity. Eat Weight Disord 2003;8:157–63. 10.1007/BF03325006 [DOI] [PubMed] [Google Scholar]
- 159.Caulfield T, Obesity CT. Obesity, legal duties, and the family physician. Can Fam Physician 2007;53:1129–30. [PMC free article] [PubMed] [Google Scholar]
- 160.Cerveny R. Approaching the obese patients in primary health care in the Czech Republic. Bratisl Lek Listy 2007;108:425–7. [PubMed] [Google Scholar]
- 161.Fitzpatrick SL, Wischenka D, Appelhans BM, et al. An Evidence-based Guide for Obesity Treatment in Primary Care. Am J Med 2016;129:115.e1–115.e7. 10.1016/j.amjmed.2015.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Frank A. A multidisciplinary approach to obesity management: the physician’s role and team care alternatives. J Am Diet Assoc 1998;98:S44–8. [DOI] [PubMed] [Google Scholar]
- 163.Gandjour A, Westenhöfer J, Wirth A, et al. Development process of an evidence-based guideline for the treatment of obesity. Int J Qual Health Care 2001;13:325–32. 10.1093/intqhc/13.4.325 [DOI] [PubMed] [Google Scholar]
- 164.Grief SN. Strategies to facilitate weight loss in patients who are obese. Am Fam Physician 2010;82:1434. [PubMed] [Google Scholar]
- 165.Grima M, Dixon JB. Obesity-recommendations for management in general practice and beyond. Aust Fam Physician 2013;42:532–41. [PubMed] [Google Scholar]
- 166.Hagaman M. FP’s patients are successful “losers”. The Journal of Family Practice 2010;59:488. [PubMed] [Google Scholar]
- 167.Hill JO. Dealing with obesity as a chronic disease. Obes Res 1998;6 Suppl 1:34S–8. 10.1002/j.1550-8528.1998.tb00686.x [DOI] [PubMed] [Google Scholar]
- 168.Hill JO, Wyatt H. Outpatient management of obesity: a primary care perspective. Obes Res 2002;10 Suppl 2:124S–30. 10.1038/oby.2002.205 [DOI] [PubMed] [Google Scholar]
- 169.Iacobucci G. Pay GPs to tackle obesity, doctors urge UK government. BMJ 2014;348:g232 10.1136/bmj.g232 [DOI] [PubMed] [Google Scholar]
- 170.Kausman R, Bruere T, dieting Inot. now what? Australian family physician 2006;35:572–5. [PubMed] [Google Scholar]
- 171.Kolasa K. Summary of clinical guidelines on the identification, evaluation, and treatment of overweight and obesity. J Nutr Educ 1999;31:114 10.1016/S0022-3182(99)70404-8 [DOI] [Google Scholar]
- 172.Kushner RF. Tackling obesity: is primary care up to the challenge? Arch Intern Med 2010;170:121–3. 10.1001/archinternmed.2009.479 [DOI] [PubMed] [Google Scholar]
- 173.Landau C, Moulton AW. General principles in the primary care of obesity. R I Med 1992;75:527–30. [PubMed] [Google Scholar]
- 174.Lenfant C. Physicians need practical tools to treat the complex problems of overweight and obesity. Am Fam Physician 2001;63:2139–46. [PubMed] [Google Scholar]
- 175.Maryon-Davis A. Weight management in primary care: how can it be made more effective? Proc Nutr Soc 2005;64:97–103. 10.1079/PNS2004414 [DOI] [PubMed] [Google Scholar]
- 176.Mogul HR, Rau J, Weinstein BI, et al. New perspectives on diagnosis and treatment of obesity. Heart Dis 1999;1:295–304. [PubMed] [Google Scholar]
- 177.Newton RL, Milsom VA, Nackers LM, et al. Supporting behavior change in overweight patients: a guide for the primary care physician. JCOM 2007;15:536–44. [Google Scholar]
- 178.Nichols J, Bazemore A. Winnable battles: family physicians play an essential role in addressing tobacco use and obesity. Am Fam Physician 2014;89:872. [PubMed] [Google Scholar]
- 179.Nonas CA. A model for chronic care of obesity through dietary treatment. J Am Diet Assoc 1998;98:S16–22. 10.1016/S0002-8223(98)00705-6 [DOI] [PubMed] [Google Scholar]
- 180.Orzano AJ, Scott JG. Diagnosis and treatment of obesity in adults: an applied evidence-based review. J Am Board Fam Pract 2004;17:359–69. 10.3122/jabfm.17.5.359 [DOI] [PubMed] [Google Scholar]
- 181.Ossolinski G, Jiwa M, McManus A. Weight management practices and evidence for weight loss through primary care: a brief review. Curr Med Res Opin 2015;31:2011–20. 10.1185/03007995.2015.1082993 [DOI] [PubMed] [Google Scholar]
- 182.Plourde G, Prud’homme D. Managing obesity in adults in primary care. Can Med Assoc J 2012;184:1039–44. 10.1503/cmaj.111640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Rao G, Burke LE, Spring BJ, et al. New and emerging weight management strategies for busy ambulatory settings: a scientific statement from the American Heart Association endorsed by the Society of Behavioral Medicine. Circulation 2011;124:1182–203. 10.1161/CIR.0b013e31822b9543 [DOI] [PubMed] [Google Scholar]
- 184.Robinson BE, Gjerdingen DK, Houge DR. Obesity: a move from traditional to more patient-oriented management. J Am Board Fam Pract 1995;8:99–108. [PubMed] [Google Scholar]
- 185.Ruser CB, Federman DG, Kashaf SS. Whittling away at obesity and overweight. Small lifestyle changes can have the biggest impact. Postgrad Med 2005;117:37–40. [DOI] [PubMed] [Google Scholar]
- 186.Scherger J. Primary care physicians: On the front line in the fight against obesity. Cardiovascular reviews and reports 1999;20:268–70. [Google Scholar]
- 187.Schlair S, Moore S, McMacken M, et al. How to deliver high-quality obesity counseling in primary care using the 5As framework. JCOM 2012;19:221–9. [Google Scholar]
- 188.Spira M. Managing obesity in general practice. Practitioner 1983;227:625–9. [PubMed] [Google Scholar]
- 189.Thompson WG, Cook DA, Clark MM, et al. Treatment of obesity. Mayo Clin Proc 2007;82:93–102. quiz 01-2 10.1016/S0025-6196(11)60971-3 [DOI] [PubMed] [Google Scholar]
- 190.Tsai AG, Carvajal R, Egner R, et al. Obesity : DiTomasso R, Golden B, Morris H, Handbook of cognitive behavioral approaches in primary care. New York: Springer Publishing Company, 2010:595–630. [Google Scholar]
- 191.Yanovski SZ. A practical approach to treatment of the obese patient. Arch Fam Med 1993;2:309–16. 10.1001/archfami.2.3.309 [DOI] [PubMed] [Google Scholar]
- 192.Australian Medical Association. Your family doctor – keeping you healthy. Ama Family Doctor Week 20142014:20–6. [Google Scholar]
- 193.Zwar N, Harris M. The conversation are GPs doing enough to help patients lose weight? Australia: The Conversation, 2013. [Google Scholar]
- 194.Hainer V. How should the obese patient be managed? Possible approaches to a national obesity management network. Int J Obes Relat Metab Disord 1999;23 (Suppl 4):S14–S19. discussion S18-9 10.1038/sj.ijo.0800915 [DOI] [PubMed] [Google Scholar]
- 195.Seidell JC, Halberstadt J, Noordam H, et al. An integrated health care standard for the management and prevention of obesity in The Netherlands. Fam Pract 2012;29 (Suppl 1):i153–6. 10.1093/fampra/cmr057 [DOI] [PubMed] [Google Scholar]
- 196.Anderson P. Reducing overweight and obesity: closing the gap between primary care and public health. Fam Pract 2008;25 Suppl 1:i10–i16. 10.1093/fampra/cmn060 [DOI] [PubMed] [Google Scholar]
- 197.Jarvis S. Obesity and the overworked GP. Br J Gen Pract 2006;56:654–5. [PMC free article] [PubMed] [Google Scholar]
- 198.Lowery B. Medical home concept: policy implications for an integrated approach in obesity management. Bariatric Nursing and Surgical Patient Care 2010;5:89–91. 10.1089/bar.2009.9933 [DOI] [Google Scholar]
- 199.van Avendonk MJ, Mensink PA, Drenthen AJ, et al. Primary care and public health a natural alliance? The introduction of the guidelines for obesity and undernutrition of the Dutch College of General Practitioners. Fam Pract 2012;29 Suppl 1(Suppl 1):i31–i35. 10.1093/fampra/cmr095 [DOI] [PubMed] [Google Scholar]
- 200.Al-Quaiz AJ. Current concepts in the management of obesity. An evidence based review. Saudi Med J 2001;22:205–10. [PubMed] [Google Scholar]
- 201.Carvajal R, Wadden TA, Tsai AG, et al. Managing obesity in primary care practice: a narrative review. Ann N Y Acad Sci 2013;1281:191–206. 10.1111/nyas.12004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Kushner RF, Ryan DH. Assessment and lifestyle management of patients with obesity: clinical recommendations from systematic reviews. JAMA 2014;312:943–52. 10.1001/jama.2014.10432 [DOI] [PubMed] [Google Scholar]
- 203.Australia O. The mission of Obesity Australia is to drive change in the public perceptions of obesity, its prevalence and its treatment. Action Agenda. Australia 2013. [Google Scholar]
- 204.Bourn J. General CaA Tackling Obesity in England : London: National Audit Office, 2001. [Google Scholar]
- 205.Alexander SC, Cox ME, Boling Turer CL, et al. Do the five A’s work when physicians counsel about weight loss? Fam Med 2011;43:179–84. [PMC free article] [PubMed] [Google Scholar]
- 206.Alexander SC, Cox ME, Yancy WS, et al. Weight-loss talks: what works (and what doesn’t). J Fam Pract 2011;60:213–9. [PMC free article] [PubMed] [Google Scholar]
- 207.Klumbiene J, Petkeviciene J, Vaisvalavicius V, et al. Advising overweight persons about diet and physical activity in primary health care: Lithuanian health behaviour monitoring study. BMC Public Health 2006;6:30 10.1186/1471-2458-6-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Linné Y, Rooth P, Rössner S. Success rate of Orlistat in primary-care practice is limited by failure to follow prescribing recommendations: the referral letter content vs clinical reality. Int J Obes Relat Metab Disord 2003;27:1434–5. 10.1038/sj.ijo.0802401 [DOI] [PubMed] [Google Scholar]
- 209.Patterson L, Patterson C, Kee F, et al. Prescribing for weight loss in primary care: evidence from a population based study. J Epidemiol Community Health 2013;67:530–2. 10.1136/jech-2012-201995 [DOI] [PubMed] [Google Scholar]
- 210.Person HA. place, and prevention in primary care: a multilevel analysis of variation in the delivery of mental health, substance-use disorder, and obesity services dissertation abstracts international section A. Humanities and Social Sciences 2013;73. [Google Scholar]
- 211.Fransen GA, Hiddink GJ, Koelen MA, et al. The development of a minimal intervention strategy to address overweight and obesity in adult primary care patients in The Netherlands. Fam Pract 2008;25 (Suppl 1):i112–5. 10.1093/fampra/cmn083 [DOI] [PubMed] [Google Scholar]
- 212.Cohen R, Pinheiro JS, Correa JL, et al. Laparoscopic Roux-en-Y gastric bypass for BMI < 35 kg/m(2): a tailored approach. Surg Obes Relat Dis 2006;2:401–4. Discussion 04 10.1016/j.soard.2006.02.011 [DOI] [PubMed] [Google Scholar]
- 213.Fobi M, Lee H, Igwe D, et al. Gastric bypass in patients with BMI < 40 but > 32 without life-threatening co-morbidities: preliminary report. Obes Surg 2002;12:52–6. 10.1381/096089202321144586 [DOI] [PubMed] [Google Scholar]
- 214.Kloek CJ, Tol J, Veenhof C, et al. Dutch General Practitioners' weight management policy for overweight and obese patients. BMC Obes 2014;1 10.1186/2052-9538-1-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Antognoli EL, Smith KJ, Mason MJ, et al. Direct observation of weight counselling in primary care: alignment with clinical guidelines. Clin Obes 2014;4:69–76. 10.1111/cob.12050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. GPs failing to offer weight-loss advice to people who need it. Nursing Standard 2015;29:16. [Google Scholar]
- 217.Binnie GA. Ten-year follow-up of obesity. J R Coll Gen Pract 1977;27:492–5. [PMC free article] [PubMed] [Google Scholar]
- 218.Bramlage P, Wittchen HU, Pittrow D, et al. Recognition and management of overweight and obesity in primary care in Germany. Int J Obes Relat Metab Disord 2004;28:1299–308. 10.1038/sj.ijo.0802752 [DOI] [PubMed] [Google Scholar]
- 219.Kraschnewski JL, Sciamanna CN, Stuckey HL, et al. A silent response to the obesity epidemic: decline in US physician weight counseling. Med Care 2013;51:186–92. 10.1097/MLR.0b013e3182726c33 [DOI] [PubMed] [Google Scholar]
- 220.Morris SE, Lean ME, Hankey CR, et al. Who gets what treatment for obesity? A survey of GPs in Scotland. Eur J Clin Nutr 1999;53 (Suppl 2):S44–8. [DOI] [PubMed] [Google Scholar]
- 221.Sammut D, Sammut D, Bonnici J. Audit of the diagnosis and management of adult obesity in a Maltese general practice. Malta Medical Journal 2012;24:16–20. [Google Scholar]
- 222.Smith AW, Borowski LA, Liu B, et al. U.S. primary care physicians' diet-, physical activity-, and weight-related care of adult patients. Am J Prev Med 2011;41:33–42. 10.1016/j.amepre.2011.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Sonntag U, Henkel J, Renneberg B, et al. Counseling overweight patients: analysis of preventive encounters in primary care. Int J Qual Health Care 2010;22:486–92. 10.1093/intqhc/mzq060 [DOI] [PubMed] [Google Scholar]
- 224.Timmerman GM, Reifsnider E, Allan JD. Weight management practices among primary care providers. J Am Acad Nurse Pract 2000;12:113–6. [DOI] [PubMed] [Google Scholar]
- 225.Gaglioti A, Petterson SM, Bazemore AW, et al. Primary care’s ecologic impact on obesity. Am Fam Physician 2009;79:446. [PubMed] [Google Scholar]
- 226.Morris S, Gravelle H. GP supply and obesity. J Health Econ 2008;27:1357–67. 10.1016/j.jhealeco.2008.02.012 [DOI] [PubMed] [Google Scholar]
- 227.Huber CA, Mohler-Kuo M, Zellweger U, et al. Obesity management and continuing medical education in primary care: results of a Swiss survey. BMC Fam Pract 2011;12:140 10.1186/1471-2296-12-140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Asselin J, Osunlana AM, Ogunleye AA, et al. Missing an opportunity: the embedded nature of weight management in primary care. Clin Obes 2015;5:325–32. 10.1111/cob.12115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Smoking, nutrition, alcohol, physical activity (SNAP). A population health guide to behavioural risk factors in general practice. Second Edn Melbourne: Royal Australian College of General Practitioners, 2015. [Google Scholar]
- 230.Managing adults who are overweight or obese. NICE guidelines. United Kingdom: National Institute for Health and Care Excellence, 2015. [Google Scholar]
- 231.Brauer P, Connor Gorber S, Shaw E, et al. Recommendations for prevention of weight gain and use of behavioural and pharmacologic interventions to manage overweight and obesity in adults in primary care. CMAJ 2015;187:184–95. 10.1503/cmaj.140887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Institute for Clinical Systems Improvement Health Care. Institute for Clinical Systems Improvement Health Care Prevention and management of obesity for adults. In: ed Sixth Edn, 2013. https://www.icsi.org/guidelines__more/catalog_guidelines_and_more/catalog_guidelines/catalog_endocrine_guidelines/obesity__adults/
- 233.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation 20142014;129:S102–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.New Zealand Guidelines Group. New Zealand Primary Care Handbook 2012. 2012 Third Edn Wellington, New Zealand: New Zealand Guidelines Group, 2012. [Google Scholar]
- 235.U.S. Preventive Services Task Force: Screening for and Management of Obesity in Adults: Recommendation Statement. Am Fam Physician 2012;86. [PubMed] [Google Scholar]
- 236.Moyer VA. U.S. Preventive Services Task Force. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2012;157:373–8. 10.7326/0003-4819-157-5-201209040-00475 [DOI] [PubMed] [Google Scholar]
- 237.Overweight. Guidelines for preventive activities in general practice. 8th Edn Melbourne: edRoyal Australian College of General Practitioners, 2012. [Google Scholar]
- 238.National Aboriginal Community Controlled Health Organisation (NACCHO) and The Royal Australian College of General Practitioners (RACGP). Overweight/Obesity National guide to a preventive health assessment for Aboriginal and Torres Strait Islander people. Second Edn Melbourne: Royal Australian College of General Practitioners, 2012. [Google Scholar]
- 239.Committee GaPA. Association BCM Overweight and obese adults: diagnosis and management. : British Columbia: British Columbia Medical Association, 2011. [Google Scholar]
- 240.Mathus-Vliegen L, Toouli J, Fried M, et al. Organisation WG Obesity, In: ed 2011. http://www.worldgastroenterology.org/guidelines/global-guidelines/obesity/obesity-english
- 241.Scottish Intercollegiate Guidelines Network. Scottish Intercollegiate Guidelines Network Management of obesity: a national clinical guideline. : Edinburgh: Scottish Intercollegiate Guidelines Network, 2010. [Google Scholar]
- 242.Binsbergen JV, Langens F, Dapper A, et al. Dutch College of General Practitioners Obesity. In: ed 2010. https://guidelines.nhg.org/product/obesity
- 243.World Health Organisation. Interventions on Diet and Physical Activity: What works. Geneva, Switzerland: World Health Organisation, 2009. http://www.who.int/dietphysicalactivity/summary-report-09.pdf?ua=1 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-019367supp001.pdf (235.1KB, pdf)