Genetics determine only a small proportion of common disease risk, but the potential to motivate health behavior change remains a proposed benefit of genetic susceptibility testing. Evidence supporting this benefit is scant (1), and studies of long-term clinical outcomes are absent. Type 2 diabetes is heritable yet preventable by behavior change. Although genetic scores predict incident diabetes (2), we demonstrated in the Genetic Counseling/Lifestyle Change (GC/LC) Study that learning one’s genetic risk did not impact short-term weight loss or behavior change motivation among participants in a diabetes prevention program (3). Here, we examine 6-year diabetes incidence among participants.
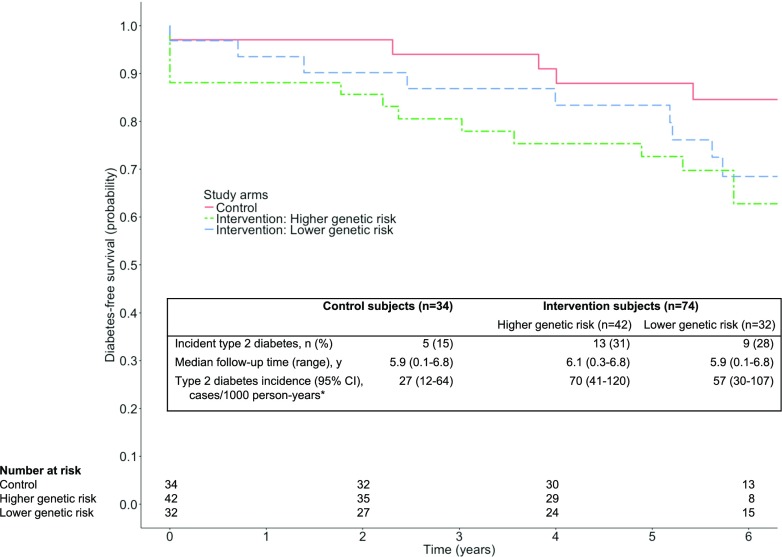
The GC/LC Study was a randomized trial of diabetes genetic risk counseling among primary care patients (3). Eligible participants did not have diabetes but were at high phenotypic risk for diabetes in that they were overweight and met at least one other metabolic syndrome criterion. Participants were randomized to undergo genotyping for a diabetes genetic risk score (tested) versus no genotyping (control). Tested participants in the highest and lowest quartiles of genetic risk (intervention) remained in the study. A genetic counselor delivered genetic risk results along with a counseling intervention emphasizing the behavioral and genetic risk factors for diabetes. All control and intervention participants were enrolled in a 12-week version of the Diabetes Prevention Program (DPP) (4). Although 33 (31%) participants lost ≥5% of their body weight, weight loss and motivation for behavior changes did not differ between study arms (3). In this exploratory follow-up study, we identified incident diabetes among participants using electronic health records and a validated diabetes algorithm (5). Log-rank tests compared time to diabetes among study arms through the date diabetes criteria were met or the last visit in the electronic health records through 2016 (median 6 years). Figure 1 shows diabetes incidence by study group. Time to diabetes did not differ between groups (overall log-rank P = 0.18), but the results suggested lower diabetes incidence among control versus intervention participants (27 [95% CI 12–64] vs. 64 [42–97]) per 1,000 person-years, respectively; log-rank P = 0.08).
Figure 1.
Diabetes-free survival among GC/LC Study participants. y, years. *Log-rank tests comparing time-to-diabetes: intervention vs. control, P = 0.08; higher vs. control, P = 0.07; lower vs. control, P = 0.18; higher vs. lower, P = 0.63.
The promise of precision prevention depends in part on its ability to motivate health behavior change. However, a recent systematic review found no evidence that genetic testing for common diseases motivates risk-reducing behavior (1). Likewise, we previously demonstrated that diabetes genetic risk testing did not impact short-term weight loss or preventive behaviors (3). Still, the hypothesis that genetic risk information acts subtly over a longer period to motivate prevention remains largely untested. Here, we find no evidence that a genetic risk testing and counseling intervention reduced 6-year diabetes incidence among patients at high phenotypic risk for diabetes. Diabetes incidence might actually have been higher among intervention participants, regardless of genetic risk; the relative roles of pathophysiology, health behavior, and ascertainment bias in this observation merit further investigation, ideally in populations with greater diversity. Limited statistical power necessitates that the present findings be considered hypothesis generating.
Context is key for any prevention intervention. Having features of metabolic syndrome, study participants were already known to have high phenotypic diabetes risk. We found no evidence that receiving counseling about genetic diabetes risk as an adjunct to participation in an evidence-based prevention program impacts long-term diabetes incidence. Whether information about genetic risk can lower disease incidence among other clinical and nonclinical populations remains an open question.
Article Information
Funding. The GC/LC Study was funded by a grant from the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (R21-DK084527). J.L.V. is an employee of the VA Boston Healthcare System and is supported by a Career Development Award from the U.S. Department of Veterans Affairs Clinical Science Research and Development Service (IK2-CX001262). J.C.F. is partially supported by NIDDK grant K24-DK110550. R.W.G. is partially supported by NIDDK grant K24-DK109114.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. J.L.V. researched data and wrote the manuscript. W.H. researched data and reviewed/edited the manuscript. J.C.F. and J.B.M. contributed to discussion and reviewed/edited the manuscript. R.W.G. researched data, contributed to discussion, and reviewed/edited the manuscript. J.L.V. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Clinical trial reg. no. NCT01034319, clinicaltrials.gov.
The contents of this article do not necessarily represent the views of the Department of Veterans Affairs, the U.S. Government, or the National Institutes of Health.
References
- 1.Hollands GJ, French DP, Griffin SJ, et al. . The impact of communicating genetic risks of disease on risk-reducing health behaviour: systematic review with meta-analysis. BMJ 2016;352:i1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bao W, Hu FB, Rong S, et al. . Predicting risk of type 2 diabetes mellitus with genetic risk models on the basis of established genome-wide association markers: a systematic review. Am J Epidemiol 2013;178:1197–1207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grant RW, O’Brien KE, Waxler JL, et al. . Personalized genetic risk counseling to motivate diabetes prevention: a randomized trial. Diabetes Care 2013;36:13–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diabetes Prevention Program (DPP) Research Group The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care 2002;25:2165–2171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hivert MF, Grant RW, Shrader P, Meigs JB. Identifying primary care patients at risk for future diabetes and cardiovascular disease using electronic health records. BMC Health Serv Res 2009;9:170. [DOI] [PMC free article] [PubMed] [Google Scholar]