Abstract
Background
The transanal hemorrhoidal dearterialization (THD) Doppler procedure is a minimally invasive technique to treat symptomatic hemorrhoids. The aim of the study was to assess the clinical efficacy and the satisfaction of patients in a large series treated with THD and to review the relevant literature.
Methods
In this retrospective, single-institution, study consecutive patients with grade 2, 3, or 4 hemorrhoidal disease were treated with the THD Doppler procedure. Dearterialization was performed in all cases and mucopexy in case of prolapse. The dearterialization procedure evolved from “proximal artery ligation” to “distal Doppler-guided dearterialization.” Follow-up was scheduled at 15 days, 1, 3, 12 months, and once a year thereafter. Complications were recorded. Clinical efficacy was assessed comparing both frequency of symptoms and disease grading (Goligher’s classification) at baseline versus last follow-up. Uni-/multivariate analysis evaluated factors affecting the outcome.
Results
There were 1000 patients (619 men; mean age: 48.6 years, range 19–88 years). Acute postoperative bleeding was observed in 14 patients (1.4%), pain/tenesmus in 31 patients (3.1%), and urinary retention in 23 patients (2.3%). At mean follow-up duration of 44 ± 29 months, the symptomatic recurrence rate was 9.5% (95 patients; bleeding in 12 (1.2%), prolapse in 46 (4.6%), and bleeding and prolapse in 37 (3.7%) patients). The recurrence rate was 8.5, 8.7, and 18.1% in patients with grade 2, 3, and 4 hemorrhoids, respectively. Seventy out of 95 patients with recurrence needed surgery (reoperation rate: 7.0%). At final follow-up and taking into account the reoperations, 95.7% of patients had no hemorrhoidal disease on examination. Younger age, grade 4 disease, and high artery ligation affected the outcome negatively.
Conclusions
Our results show that the THD Doppler procedure is safe and effective in patients with hemorrhoidal disease and associated with low morbidity and recurrence rates and a high rate percentage of treatment success.
Keywords: Hemorrhoids, Transanal hemorrhoidal dearterialization, Mucopexy, Surgical management hemorrhoidal disease
Introduction
Hemorrhoidal disease is the most common benign anorectal disorder in Western countries, with an estimated prevalence between 4.4 and 12.8% in the adult population [1].
An accurate patient history, anorectal examination, and anoscopy are mandatory to estimate the degree of disease and to identify patients who are suitable for either medical or surgical treatment.
Among surgical approaches, Milligan–Morgan and Ferguson hemorrhoidectomies are still considered the “gold standard” for the treatment of advanced hemorrhoidal disease, even though there is a significant risk of postoperative complications, particularly pain. In an attempt to reduce the risk of complications, in 1995 Morinaga introduced a new non-excisional procedure providing the Doppler-guided ligation of the hemorrhoidal arteries [2], hemorrhoidal dearterialization. Several modifications of the original technique have been described, and consequently, the indications have been expanded. In particular, the addition of the endorectal plication of the redundant and prolapsing mucosa and submucosa (mucopexy) aimed to treat the hemorrhoidal prolapse, while maintaining the anatomical integrity of the hemorrhoidal piles. Later a more reliable identification of the hemorrhoidal arteries made it possible to perform distal Doppler-guided dearterialization (DDD), with further improvement in clinical results [3, 4].
The primary aim of the present study was to evaluate the clinical results obtained during a 10-year experience of using transanal hemorrhoidal dearterialization (THD) for hemorrhoidal disease in the largest series of patients to date. The secondary aim was to examine the factors related to recurrence.
Materials and methods
A retrospective study was conducted on all consecutive patients with grade 2, 3, or 4 hemorrhoidal disease who had failed conservative treatment (based on diet, fiber supplements, topical ointments, and phlebotonic drugs) and underwent THD Doppler at the University Hospital “A. Gemelli,” Rome, Italy between June 2005 and June 2015. All procedures complete hemorrhoidal dearterialization, while mucopexy was carried out in patients with hemorrhoidal prolapse. All the patients provided written informed consent to undergo the procedure and subsequent follow-up. Ethical approval in our institution is not needed for this type of studies.
Preoperatively, all patients underwent full physical and clinical examination: According to Goligher’s classification [5], 82 cases (8.2%) were classified as grade 2, 835 (83.5%) as grade 3, and 83 (8.3%) as grade 4. A symptoms-based questionnaire (recording bleeding, prolapse, manual reduction, impact on quality of life, discomfort/pain) was administered to all patients, before the operation and at follow-up; this questionnaire was based on five different parameters characterizing the hemorrhoidal disease, with a grading from 0 (no symptom) to 4 (daily presence of the symptom(s)) for each symptom [6]. The total score of all five parameters was used to evaluate the patient’s condition: 0 indicated the total absence of a symptom, while a score of 20 represented the worst clinical scenario. After the patients were examined and the above symptoms were discussed, the examining clinician made a final assessment of symptomatic recurrences that needed to be addressed medically or surgically.
THD technique
THD Doppler technique has been described in detail elsewhere [4, 7]. Patients were treated under general or spinal anesthesia. No antibiotics were administered before, during, or after the operation. With the patient in the lithotomy position, the THD Doppler proctoscope was introduced transanally for its full length to reach the lower rectum. Under Doppler guidance, the signal from six arteries was found in all the patients. During the 10-year study period, the equipment has been progressively improved (all the devices were produced by THD S.p.A., Correggio, Italy) [8]. The first model of the proctoscope (hereafter referred to as “first device”) had a very small operative window that limited the possibilities for mucopexy in very advanced cases. Then, THD Surgery (hereafter referenced to as “second device”) was introduced, improving the first model of the proctoscope by providing a fully opened operative window, to better expose the site of the mucopexy. The last proctoscope model (THD Slide, hereafter referred to as “third device”) was introduced in 2009. It provided an improved Doppler system and a sliding component, which significantly facilitated both a reliable dearterialization and an effective and complete mucopexy.
Up to 2009, the hemorrhoidal arteries were searched for at the higher part of the low rectum, reached by fully introducing the THD proctoscope. However, following the results of a study which highlighted that the arterial hemorrhoidal branches became more superficial and submucosal in the distal rectum [9], artery identification and ligation was targeted to the distal part of the low rectum (within 2 cm of the anorectal junction). This distal Doppler-guided dearterialization (DDD) has been used to perform the dearterialization since 2009 [3]. Using electrocautery, a small marker point was made on the mucosa where the best Doppler signal was obtained. Thereafter, in patients with prolapsing hemorrhoids requiring mucopexy, the proctoscope was fully reintroduced into the low rectum. Mucopexy started at 6–7 cm from the anal verge with a Z-shaped proximal fixation stitch. Then it continued distally with several passages (roughly 5 mm from each other), through the rectal mucosa and submucosa, finally reaching the anorectal junction. The running suture always stopped above the hemorrhoid tissue. Along the continuous suture of mucopexy, the “marker point” was incorporated by passages of suture above and below therefore occluding the hemorrhoidal artery lying in the submucosa. Postoperatively, patients were advised to avoid prolonged straining and heavy physical activity for 1 month, and a fiber- and fluid-rich diet was prescribed for 2 weeks. Stool softeners, analgesics, and anti-inflammatory drugs (paracetamol, nonsteroidal anti-inflammatory drugs) were administered for postoperative days 1–3, and thereafter only if necessary. No antibiotics were administered.
Follow-up
Routine follow-up visits were scheduled at 2 weeks, 1 month and 3 months, and then 1 year after the operation. Patients with a follow-up longer than 1 year were recalled and examined to evaluate the results of the operation at longer follow-up. Postoperative symptoms occurring within 30 days were recorded. The medical or surgical treatment needed to resolve complications and recurrence was also recorded. At the last follow-up visit, the symptom questionnaire was readministered and compared with the preoperative data. If patients suffered from a recurrence, the results from the questionnaire at the time of recurrence were considered final. Recurrence was defined as the presence of recurrent bleeding or recurrent hemorrhoidal prolapse requiring medical or surgical therapy after the first THD surgery. Anatomical recurrence was defined as presence of hemorrhoidal tissue on physical examination and anoscopy at the last visit, including patients who underwent surgical procedures for recurrent disease.
Statistical analysis
The following baseline variables were evaluated as predictive factors of failure: age, gender, hemorrhoid grade, recurrent disease, type of THD procedure performed, morbidity, need for therapy, follow-up period, use of first or second device, and use of “high ligation.” Continuous data were analyzed as means (with SD and range) and compared using the paired samples t test. Categorical data were analyzed as frequencies and percentages, and compared using either the Chi-square test or the marginal homogeneity test, as necessary. To assess factors potentially predictive of failure, univariate and multivariate logistic regression models were applied. A p < 0.05 was considered statistically significant. Analyses were carried out with SPSS—version 21.0 software for Windows—(SPSS, Chicago, IL, USA).
Results
Intra- and postoperative findings
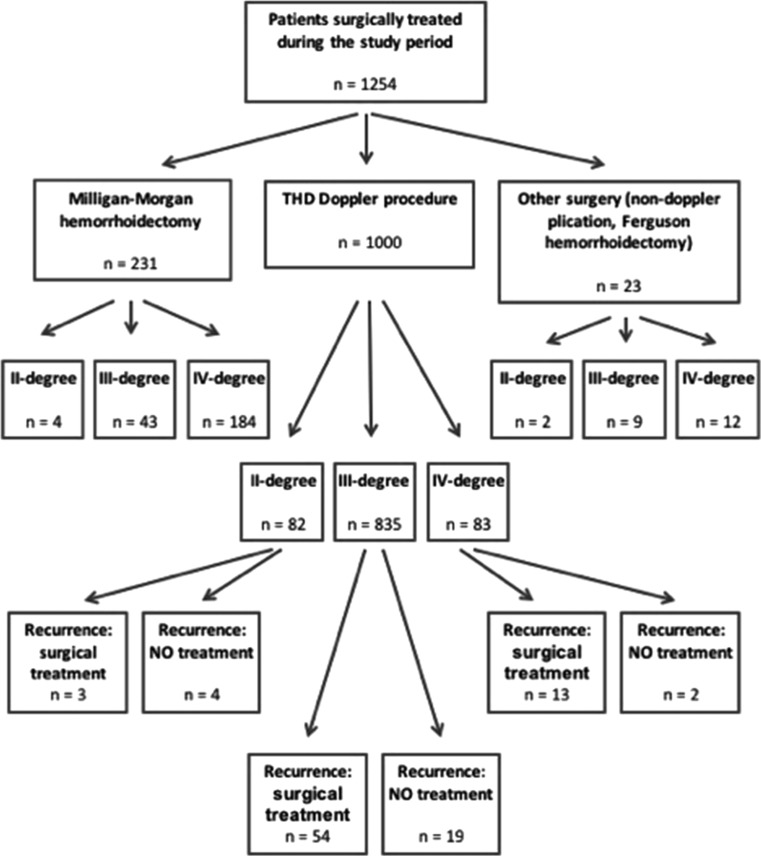
A total of 1000 consecutive patients with symptomatic hemorrhoids (619 men; mean age 48.6 years; range 19–88 years) underwent THD Doppler during the study period (Fig. 1).
Fig. 1.
Flow diagram of the surgical treatment
General anesthesia was given to 915 patients (91.5%), and spinal anesthesia to 85 patients (8.5%). The mean duration of surgical procedure was 20 ± 5 min when only dearterialization was performed and 30 ± 10 min when mucopexy was added. In 931 patients (93.1%), hemorrhoidal dearterialization and mucopexy were performed, while in 69 patients (6.9%) only dearterialization was performed. The mean postoperative hospital stay was 1 ± 0.2 day. Table 1 reports the intra- and postoperative results. One hundred and one patients (10.1%) were treated with the first THD Doppler device, 36 (3.6%) with the THD Surgery, and 863 (86.3%) with the THD Slide. Concomitant surgical procedures were carried out in 243 patients (24.3%): The most frequent was skin tag(s) removal (in 145 patients, 14.5%); internal lateral sphincterotomy was performed in 103 patients (10.3%) with anal fissure, and fistulotomy in 10 patients (1.0%). Morbidity (within 30 days) included mainly pain and/or tenesmus (31 patients, 3.1%), which required medical therapy (anti-inflammatory and/or analgesic drug) for more than 5 days; urinary retention was observed in 23 patients (2.3%) treated with bladder catheterization; and thrombosed external hemorrhoids in eight patients (0.8%). Only 14 cases (1.4%) of acute bleeding were registered, requiring surgical or endoscopic hemostasis. Neither postoperative anal abscess nor anal fissure was reported.
Table 1.
Intra- and postoperative results
| No. of patients | % | |
|---|---|---|
| Device used | ||
| First model device | 101 | 10.1 |
| Second model device (THD Surgy) | 36 | 3.6 |
| Third model device (THD Slide) | 863 | 86.3 |
| Concomitant surgical procedures | ||
| Skin tag(s) removal | 145 | 14.5 |
| Lateral internal sphincterotomy | 103 | 10.3 |
| Fistulotomy | 10 | 1 |
| Total | 243 | 24.3 |
| Mortality | 0 | 0 |
| Morbidity (≤ 30 postop days) | ||
| Pain/tenesmus | 31 | 3.1 |
| Urinary retention | 23 | 2.3 |
| Bleeding | 14 | 1.4 |
| Total | 68 | 6.8 |
Long-term follow-up
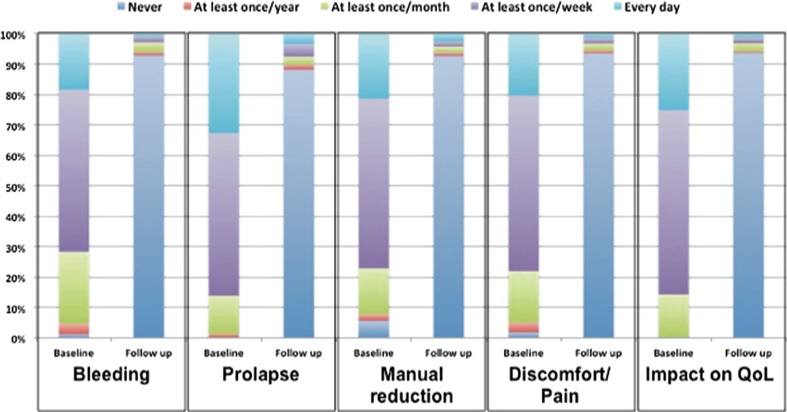
The mean follow-up period was 44 ± 29 months (median 36 months, range 6–124). A significant mean reduction in the symptom-based questionnaire score was calculated following the primary THD Doppler operation when compared with the preoperative values (mean score: 13.8 ± 2.3 at baseline vs. 1.1 ± 0.8 at last follow-up; p < 0.0001). With regard to each component of the questionnaire administered after the primary THD Doppler procedure (Fig. 2), no bleeding was reported by 928 of patients (92.8%), no prolapse by 881 patients (88.1%), no manual reduction of hemorrhoids by 926 patients (92.6%), no anal discomfort/pain by 935 patients (93.5%), and no impact on quality of life (QoL) by 936 patients (93.6%). The comparison between frequency of symptoms preoperatively and during follow-up, as investigated by the questionnaire, revealed a statistical significant difference for every item (p < 0.0001; Fig. 2).
Fig. 2.
Results of symptoms-based questionnaire at preoperative evaluation (baseline) and last visit (follow-up): distribution of patients (percentage). Statistics: marginal homogeneity test; for each item, baseline versus follow-up: p < 0.0001
Recurrence, which was evaluated by taking into account patient examination and severity of symptoms, was 9.5% (95 patients): 12 patients (1.2%) had recurrence of bleeding, 46 (4.6%) of prolapse, and 37 (3.7%) of both bleeding and prolapse. Only 26 patients (2.6%) needed to reduce prolapsing piles every day, 14 (1.4%) had daily anal discomfort/pain, and 12 (1.2%) daily significant impact on their quality of life. The mean time until recurrence was 13 ± 4.3 months. The detailed distribution of the patients with recurrence related to the classification of the primary disease is reported in Table 2. Recurrence occurred in 7 out of 82 grade 2 patients (8.5%), 73 out of 835 grade 3 patients (8.7%), and 15 out of 83 grade 4 patients (18.1%) (p = 0.021). Twenty-five patients (2.5%) having recurrence did not need any further surgery as their symptoms were minimal or very infrequent (Fig. 1). On the other hand, 70 patients (7.0%) underwent a second surgical procedure (performed in either our institution or other hospitals) for symptomatic hemorrhoids: 32 were treated again with the THD Doppler procedure, 23 underwent Milligan–Morgan hemorrhoidectomy, 11 Ferguson hemorrhoidectomy, 2 stapled hemorrhoidopexy, and 2 stapled transanal rectal resection.
Table 2.
Recurrence following THD Doppler procedure: distribution based on the preoperative Goligher classification of hemorrhoidal disease
| Type of failure | Hemorrhoidal disease grade No. of patients (%) |
p valuea | |||
|---|---|---|---|---|---|
| II | III | IV | Overall | ||
| Bleeding | 2 (2.4) | 10 (1.2) | 0 | 12 (1.2) | 0.355 |
| Prolapse | 1 (1.2) | 37 (4.4) | 8 (9.6) | 46 (4.6) | 0.030 |
| Bleeding and prolapse | 4 (4.9) | 26 (3.1) | 7 (8.4) | 37 (3.7) | 0.042 |
| Overall failure | 7 (8.5) | 73 (8.7) | 15 (18.1) | 95 (9.5) | 0.021 |
aChi-square test
As far as anatomical recurrence at the final evaluation, taking into account reoperations, 95.7% of patients (957/1000) was free of hemorrhoidal disease, while 0.2% (2 patients) had grade 1 hemorrhoids, 1.1% (11 patients) grade 2, 2.5% (25 patients) grade 3, and 0.5% (5 patients) grade 4. Residual skin tags were present in 53 patients (5.3%). No patient reported defecatory urgency, fecal incontinence, or chronic pain.
At univariate analysis, high ligation of hemorrhoidal arteries, age < 40 years, and grade 4 hemorrhoidal disease were all variables associated with a significantly higher recurrence rate. These three variables have proven their value as independent factors affecting the outcome of the disease also at multivariate analysis (Table 3).
Table 3.
Uni-/multivariate analysis of factors affecting the final outcome following THD Doppler procedure
| Factors | Univariate analysis Relative risk (95% CI) |
p value | Multivariate analysis Relative risk (95% CI) |
p value |
|---|---|---|---|---|
| Age < 40 years | 2.004 (1.284–3.128) | 0.002 | 1.945 (1.234–3.065) | 0.004 |
| Male | 1.010 (0.653–1.561) | 0.965 | ||
| Baseline grade 4 hemorrhoidal diseasea | 2.308 (1.261–4.223) | 0.005 | 2.367 (1.261–4.442) | 0.007 |
| First device usage | 1.472 (0.788–2.750) | 0.223 | ||
| Second device usage | 1.966 (0.797–4.852) | 0.135 | ||
| Third device usage | 0.600 (0.350–1.028) | 0.060 | 0.949 (0.485–1.855) | 0.878 |
| High ligation of arteries | 2.155 (1.375–3.377) | 0.001 | 1.881 (1.083–3.269) | 0.025 |
| No morbidity within 30 days | 1.508 (0.694–3.279) | 0.296 | ||
| Follow-up < 12 months | 0.447 (0.160–1.249) | 0.115 | 0.613 (0.216–1.744) | 0.359 |
aGoligher classification
Discussion
In recent years, several studies have legitimized the THD Doppler procedure as an effective non-excisional operation for symptomatic hemorrhoidal disease. Progressively, the improvement in targeted hemorrhoidal artery ligation [3, 4, 9] and the addition of the appropriate mucopexy in those patients presenting hemorrhoidal/muco-hemorrhoidal prolapse [4, 7] have obtained high success rates in treating the symptoms of hemorrhoidal disease (mainly bleeding and prolapse). The literature on this subject includes studies conducted during the first period of THD Doppler use, with only the hemorrhoidal dearterialization, and several, more recent, papers that have reported data about the addition of mucopexy (Table 4). There are also papers reporting trials comparing THD Doppler to other procedures: Table 5 summarizes the data and lists some critical points concerning the results. In four studies, THD was compared to hemorrhoidectomy (in 2 with the Milligan–Morgan procedure [19, 20], in 1 with the Ferguson procedure [17, 18], and 1 with hemorrhoidectomy using LigaSure™ [16]. In four other studies [11, 13, 15, 23], THD was compared to stapled hemorrhoidopexy.
Table 4.
Results of the analyzed cohort studies
| Study | No. patients | Operation time (min.) | No. ligatedarteries | Postoperative complications | Follow-up (months) | Recurrence rate (%) | Symptoms at follow-up | Reoperation rate (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pain (%) | Bleeding (%) | Thrombosis (%) | Fissure (%) | Bleeding (%) | Prolapse (%) | Pain (%) | |||||||
| Dal Monte [10] | 330 (grades 2–3–4) | n.a. | n.a. | 19† | 2 | 1.5 | 0.6 | 46 (22–79) | 7.5 | 3 | 2.7 | n.a. | n.a. |
| Festen et al. [11] | 23 (grades 2–3) | 34 | n.a. | n.a. | n.a. | n.a. | n.a. | 1.5 | 17 | 4.3 | n.a. | n.a. | n.a. |
| Ratto et al. [8] | 170 (grades 2–3–4) | 20 ± 5.30 ± 10 (with RAR) | 6 | 15.9 | 1.2 | 2.3 | n.a. | 11.5 ± 12 (1–41) | n.a. | 6.5 | 10.5 | 0 | 4.1 |
| Infantino [12] | 112 (grades 2–3) | 33.9 ± 8.8 | 7.2 ± 1.5 | 28.6 | 0.9 | 2.7 | n.a. | 15.6 ± 6.5 (6–32) | 14.3 | 20 | 6.3 | 3.6 | 12.5 |
| Rattoet al. [6] | 35 (grade 4) | 33 ± 12 | 6 | 14.3 | 5.7 | 8.6 | n.a. | 10 (6–28) | n.a. | 25.7 | 28.6 | 8.6 | 5.7 |
| Giordano et al. [13] | 28 (grades 2–3) | 30 (20–45) | n.a. | 0 | 0 | n.a. | n.a. | 38 (33–48) | 14 | 4 | 11 | n.a. | n.a. |
| Schuurman et al. [14] | 38 (grades 2–3) | n.a. | 5.2 ± 0.71 | 0 | 2.6 | 2.6 | n.a. | 6 | n.a. | n.a. | n.a. | n.a. | 13.2 |
| Infantino et al. [15] | 85 (grade 3) | n.a. | n.a. | 5.9 | 2.4 | n.a. | 17 ± 0.4 (15–20) | 14 | n.a. | n.a. | n.a. | 11.3 | |
| Zampieriet al. [16] | 46 (grades 3–4) | 20 ± 5.1 | n.a. | 6.5 | 0 | 0 | 0 | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. |
| Denoya et al. [17, 18] | 20 (grades 3–4) | 36.6 ± 12.7 | 6 | 10 | 10 | 0 | 0 | 35 (27–43) | 16.7 | 16.7 | 16.7 | 8.3 | 8.3 |
| Elmér et al. [19] | 20 (grades 2–3) | 36 (30–45) | 6 | 5 | 0 | 5 | 0 | 12 | 20.0 | 15.0 | 20.0 | 10–0 | 10.0 |
| De Nardi et al. [20] | 25 (grade 3) | 25 ± 10 | 6 | 0 | 0 | 0 | 0 | 24 | 12.5 | 4.2 | 0 | 16.6 | 4.2 |
| Giordano et al. [21] | 31 (grade 4) | 32 (23–47) | 6 (5–8) | 71 | 0 | 3.2 | 0 | 32 (6–58) | 3.2 | n.a. | n.a. | n.a. | 3.2 |
| Tempel et al. [22] | 216 (grade n.a.) | n.a. | n.a. | 10.4 | 0 | 0 | 0 | 23 (1–42) | n.a. | n.a. | n.a. | n.a. | n.a. |
| Béliard et al. [23] | 54 (grades 2–3) | n.a. | n.a. | 0 | 0 | 0 | 0 | 24 | 9.3 | n.a. | n.a. | n.a. | n.a. |
| Ratto et al. [24] | 803 (grades: 2–3–4) | 34.3 ± 5.9 (24–47) | 6 | 13 | 2.2 | 0.5 | 0.1 | 11.1 ± 9.2 (3–57) | 9.3 | 3.0 | 6.9 | 0 | 5.6 |
| LaBella et al. [25] | 108 (grades 2–3–4) | n.a. | 6 | 8 | 13 | 0 | 0 | 12 | 10.3 | 0 | 10.3 | 0 | 10.3 |
| Rubbini et al. [26] | 106 (grades 3–4) | 25 (16–65) | n.a. | 35 | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. |
Table 5.
Comparative trials comparing THD Doppler procedure with other techniques
| Study | No. patients, grade | Compared procedure | Outcome |
|---|---|---|---|
| Festen et al. [11] | Total: 23 Grade 3: 19 Grade 4: 4 |
PPH | No significant difference in complications. However, significantly shorter operative time for DGHL (23 vs. 34 min, p < 0.001) and less pain (pain score at day 7: 1.6 vs. 3.2, p < 0.01) |
| Giordano et al. [13] | Total: 28 Grade 2: 16 Grade 2: 12 |
PPH | No significant difference in pain, operative time, complications, or recurrence rate. Patients returned to normal activities faster after DGHL (3.2 vs. 6.3 days, p < 0.01) |
| Schuurman et al. [14] | Total: 38 (grades 2–3) | HL | No significant difference in patient-reported severity of bleeding, pain, defecation problems, and discomfort. Greater improvement in prolapse symptoms in non-Doppler group (p = 0.047). Higher rate of complications for DGHL (p < 0.0005) |
| Infantino et al. [15] | Total: 85 (grade 3) | PPH | No significant difference in pain, postoperative complications, recurrence, or reoperation rates. Higher rate of late complications for PPH (p = 0.028). Shorter length of stay and lower equipment cost for DGHL |
| Zampieriet al. [16] | Total: 46 Grade 3: 21 Grade 4: 25 |
Ligasure hemorrhoidectomy | In DGHL group, lower length of procedure (20 ± 5.1 vs. 28 ± 4.2 min, p < 0.05), higher pain resolution rate (87 vs. 81%, p < 0.05), better QoL, lower number of constipation days |
| Elmér et al. [19] | Total: 20 Grade 2: 3 Grade 3: 17 |
MMH | Postop peak pain lower in DGHL during first week (p < 0.05), but no difference in overall pain. More patients with normal well-being in DGHL (p = 0.05). Pain, bleeding, and manual reduction in prolapse improved in all DGHL pts. At 1-year follow-up, grade of hemorrhoids reduced for both methods (more patients with remaining grade II for DGHL (p = 0.06) |
| Denoya et al. [17] | Total: 20 Grade 3: 16 Grade 4: 4 |
Ferguson hemorrhoidectomy | In DGHL group, lower postop narcotics use (25 vs. 100%, p < 0.001), shorter postop analgesics use (0 vs. 7 days, p = 0.001), earlier first bowel movement (1.3 ± 0.9 vs. 4.6 ± 3.1 days, p = 0.001), lower pain intensity rate (2.9 ± 3.5 vs. 7.6 ± 2.9, p = 0.001), less frequent urinary retention (0 vs. 23.5%, p = 0.012), less laxative use (8.3 vs. 23.5%, p = 175), less anal pain (8.3 vs. 64.7%, p = 0.001) |
| Denoya et al. [18] | Total: 12 | Ferguson hemorrhoidectomy | In DGHL group, similar recurrence rate (16.7 vs. 6.7%, p = 0.411), reintervention rate (8.3 vs. 6,7%, p = 809), no chronic complications (0 vs. 13.3%, p = 0.189), similar rate of recurrent symptoms (50 vs. 26.7%, p = 0.212), similar pain severity, similar QoL, similar incontinence-related QoL |
| De Nardi et al. [20] | Total: 25 (grade 3) | MMH | Similar pain level by 30th postop day. In DGH, shorter work resumption and higher patient satisfaction, but not significantly. Similar recurrence rates needing additional surgery (4.2 vs. 4.2%, p = 0.55) at 1-year follow-up |
| Béliard et al. [23] | Total: 54 (grade 2) | PPH | In DGHL group, shorter disability for work (4.4 ± 6.6 vs. 18.6 ± 13.7, p < 0.001), significantly more improved prolapse, similar improvement of bleeding, significant improvement of tenesmus at 3 months, similar incontinence score, lower pain level at 1 month, significantly higher patient satisfaction, higher recurrence rate, similar reoperation rate |
PPH procedure for prolapse and hemorrhoids (stapled hemorrhoidopexy); HL hemorrhoidal artery ligation (without Doppler guidance); DGHL Doppler-guided hemorrhoidal artery ligation; MMH Milligan–Morgan hemorrhoidectomy; QoL quality of life
To our knowledge, this is the first study showing a 10-year experience using the THD Doppler procedure in a single institution, with the largest series of patients ever published.
In other studies (Table 4), the reported operating time was 20–45 min; the number of arteries ligated 5–8. In the present series, the operating time was 20–30 min, and the number of arteries ligated was always 6.
In the previous series (Table 4), pain was the most often reported postoperative complication following THD in up to 35% of patients. However, in the majority of papers, less than 10% of patients complained of significant postoperative pain. In a selected subset of grade 4 patients, Giordano et al. [21] reported pain in 71% (severe pain in only 16%). In the few studies which reported tenesmus following the operation, it was more frequent in patients who underwent mucopexy. Postoperative bleeding was reported in up to 13% of patients; the majority of the published papers report an incidence rate below 6%. Moreover, not all the patients having postoperative bleeding needed surgical reintervention for hemostasis. Hemorrhoidal thrombosis was observed in up to 8.6% of patients but was less than 3% in the majority of papers. Anal fissure was considered a postoperative complication in up to 1.5% of patients.
Urinary retention was reported only in a few papers, possibly because it was not considered an actual postoperative complication. The urge to defecate is infrequently described as a transient postoperative symptom, possibly related to both tenesmus and acute inflammation. In the literature, there is no mention of any life-threatening complication, nor other morbidity observed after different surgical procedures (i.e., rectovaginal fistula, rectal necrosis, retrorectal hematoma, events requiring stoma formation).
In the present study, the overall morbidity rate was below 7%; however, no complication had long-term effects. Pain and tenesmus occurred only within the first few postoperative weeks. Very few cases of postoperative bleeding required reoperation for hemostasis.
In 11 of the 18 papers that report THD Doppler data (Table 4), the follow-up period was longer than 12 months. The overall recurrence rate was 3–20%; no series showed a recurrence rate ≥ 20%. Recurrence of bleeding was reported in 3–16.7% of patients. Recurrent prolapse was observed in 2.7–16.7% of patients. Only in a two-center study (which included our institution) on grade 4 patients was the prolapse recurrence rate higher (28.6%) [6]. During follow-up, anal pain was reported in up to 10% of patients; only De Nardi et al. [20] reported a higher incidence rate of 16.6%. Reoperation, due to the recurrence of symptoms, was necessary in 4.1–17.8% of cases.
The present series has the longest mean follow-up in the literature (44 ± 29 months), with the exception of one other series [10]. The clinical efficacy of the THD Doppler procedure was demonstrated by the subjective improvement of symptoms (as reported by the results of the symptoms-based questionnaire showing a significant decrease in the score from 13.8 to 1.1, p < 0.0001). Less than 10% of patients in the present series experienced recurrence of hemorrhoidal disease following the primary THD Doppler procedure, and recurrence mainly concerned hemorrhoidal prolapse. Recurrence was significantly more frequent in patients treated with high ligation of the arteries (used in the first period of the present series), demonstrating that DDD was effective (Table 3). Grade 4 disease predisposed to the worst outcome, as shown by the multivariate analysis, mainly due to prolapse recurrence (15 cases). However, it was possible to treat the recurrence with a single procedure (12 patients) or conservative management only (3 cases). Almost half the patients with recurrence (32 out of 70) were treated with a redo THD procedure, mainly aimed at repositioning the prolapsing hemorrhoids inside the anal canal. The other 38 patients underwent different operations (including hemorrhoid excision in 34 cases). It is interesting that, at last follow-up visit, 95.7% of the patients were disease-free, and only 30 out of 1000 patients had grade 3 (25 cases) or grade 4 (5 cases) disease.
Another predictive factor of failure was age below 40 years, and the reason for this is not clear. However, we can speculate that younger patients’ failure to fully respect the recommendations to avoid straining and physical activity may partly explain this result. A similar result, even if not confirmed at the multivariate analysis, emerged in another multicenter trial [24].
Main limitations of the study are: (1) retrospective design; (2) single-institution series: The results could be different in other patient populations, although our results are similar to those of a multicenter trial which includes our experience [24]; (3) variable technique and equipment: To better evaluate this limitation, we have analyzed the impact of the adoption of different devices and techniques on the results; (4) in our center, rubber band ligation or sclerosing injections are not used as a first-line approach, so it is possible that in a practice that includes these ambulatory treatments the results of THD may be different because of patient selection.
Conclusions
Data from this 10-year retrospective study support the safety and the clinical efficacy of the THD procedure in patients with hemorrhoidal disease. The procedure is associated with a high level of treatment success, significant QoL benefits, a low recurrence rate, and good long-term outcome; THD Doppler therefore seems a valid therapeutic option for primary hemorrhoidal disease and selected recurrences.
Authors contribution
CR contributed to study conception and design; analysis and interpretation of data; drafting the article and revising it critically for important intellectual content; and final approval of the version to be published. PC contributed to study conception and design; acquisition and interpretation of data; drafting the article; and final approval of the version to be published. FP helped in study conception and design; acquisition, analysis, and interpretation of data; drafting the article; and final approval of the version to be published. LD contributed to acquisition of data; drafting the article; and final approval of the version to be published. FL helped in study conception, acquisition, analysis, and interpretation of data; drafting the article; and final approval of the version to be published. AP helped in study conception, acquisition, and interpretation of data; revision of the article critically for important intellectual content; and final approval of the version to be published.
Compliance with ethical standards
Conflict of interest
Carlo Ratto was, for 1 year, a member of the THD Advisory Board; no personal salary was received. The other authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
This paper has been presented as Podium Presentation (S62a) at the American Society of the Colon and Rectal Surgeons (ASCRS) Annual Scientific Meeting in Los Angeles, CA, April 30–May 4, 2016.
A correction to this article is available online at https://doi.org/10.1007/s10151-018-1765-6.
References
- 1.Ganz RA. The evaluation and treatment of hemorrhoids: a guide for the gastroenterologist. Clin Gastroenterol Hepatol. 2013;11:593–603. doi: 10.1016/j.cgh.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 2.Morinaga K, Hasuda K, Ikeda T. A novel therapy for internal hemorrhoids: ligation of the hemorrhoidal artery with a newly devised instrument (Moricorn) in conjunction with a Doppler flowmeter. Am J Gastroenterol. 1995;90:610–613. [PubMed] [Google Scholar]
- 3.Ratto C, Donisi L, Parello A, Litta F, Zaccone G, De Simone V. ‘Distal doppler-guided dearterialization’ is highly effective in treating by transanal haemorrhoidal dearterialization. Colorectal Dis. 2012;14:e786–e789. doi: 10.1111/j.1463-1318.2012.03146.x. [DOI] [PubMed] [Google Scholar]
- 4.Ratto C. THD Doppler procedure for hemorrhoids: the surgical technique. Tech Coloproctol. 2014;18:291–298. doi: 10.1007/s10151-013-1062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goligher JC, Leacock AG, Brossy JJ. The surgical anatomy of the anal canal. Br J Surg. 1955;43:51–61. doi: 10.1002/bjs.18004317707. [DOI] [PubMed] [Google Scholar]
- 6.Ratto C, Giordano P, Donisi L, Parello A, Litta F, Doglietto GB. Transanal haemorrhoidal dearterialization (THD) for selected fourth-degree haemorrhoids. Tech Coloproctol. 2011;15:191–197. doi: 10.1007/s10151-011-0689-1. [DOI] [PubMed] [Google Scholar]
- 7.Ratto C, de Parades V. Doppler-guided ligation of hemorrhoidal arteries with mucopexy: a technique for the future. J Visc Surg. 2015;152(2 Suppl):S15–S21. doi: 10.1016/j.jviscsurg.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Ratto C, Donisi L, Parello A, Litta F, Doglietto GB. Evaluation of transanal hemorrhoidal dearterialization as a minimally invasive therapeutic approach to hemorrhoids. Dis Colon Rectum. 2010;53:803–811. doi: 10.1007/DCR.0b013e3181cdafa7. [DOI] [PubMed] [Google Scholar]
- 9.Ratto C, Parello A, Donisi L, Litta F, Zaccone G, Doglietto GB. Assessment of haemorrhoidal artery network using colour duplex imaging and clinical implications. Br J Surg. 2012;99:112–118. doi: 10.1002/bjs.7700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dal Monte PP, Tagariello C, Sarago M, et al. Transanal haemorrhoidal dearterialisation: nonexcisional surgery for the treatment of haemorrhoidal disease. Tech Coloproctol. 2007;11:333–338. doi: 10.1007/s10151-007-0376-4. [DOI] [PubMed] [Google Scholar]
- 11.Festen S, Van Hoogstraten MJ, Van Geloven AA, Gerhards MF. Treatment of grade III and IV haemorrhoidal disease with PPH or THD. A randomized trial on postoperative complications and short-term results. Int J Colorectal Dis. 2009;24:1401–1405. doi: 10.1007/s00384-009-0803-2. [DOI] [PubMed] [Google Scholar]
- 12.Infantino A, Bellomo R, Dal Monte PP, et al. Transanal haemorrhoidal artery echodoppler ligation and anopexy (THD) is effective for II and III degree haemorrhoids: a prospective multicentric study. Colorectal Dis. 2010;12:804–809. doi: 10.1111/j.1463-1318.2009.01915.x. [DOI] [PubMed] [Google Scholar]
- 13.Giordano P, Nastro P, Davies A, Gravante G. Prospective evaluation of stapled haemorrhoidopexy versus transanal haemorrhoidal dearterialisation for stage II and III haemorrhoids: three-year outcomes. Tech Coloproctol. 2011;15:67–73. doi: 10.1007/s10151-010-0667-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schuurman JP, Rinkes I, Go P. Hemorrhoidal artery ligation procedure with or without doppler transducer in grade II and III hemorrhoidal disease. Ann Surg. 2012;255:840–845. doi: 10.1097/SLA.0b013e31824e2bb5. [DOI] [PubMed] [Google Scholar]
- 15.Infantino A, Altomare DF, Bottini C, et al. Prospective randomized multicentre study comparing stapler haemorrhoidopexy with Doppler-guided transanal haemorrhoid dearterialization for third-degree haemorrhoids. Colorectal Dis. 2012;14:205–211. doi: 10.1111/j.1463-1318.2011.02628.x. [DOI] [PubMed] [Google Scholar]
- 16.Zampieri N, Castellani R, Andreoli R, Geccherle A. Long-term results and quality of life in patients treated with hemorrhoidectomy using two different techniques: ligasure versus transanal hemorrhoidal dearterialization. Am J Surg. 2012;204:684–688. doi: 10.1016/j.amjsurg.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 17.Denoya PI, Fakhoury M, Chang K, Fakhoury J, Bergamaschi R. Dearterialization with mucopexy versus haemorrhoidectomy for grade III or IV haemorrhoids: short-term results of a double-blind randomized controlled trial. Colorectal Dis. 2013;15:1281–1288. doi: 10.1111/codi.12303. [DOI] [PubMed] [Google Scholar]
- 18.Denoya P, Tam J, Bergamaschi R. Hemorrhoidal dearterialization with mucopexy versus hemorrhoidectomy: 3-year follow-up assessment of a randomized controlled trial. Tech Coloproctol. 2014;18:1081–1085. doi: 10.1007/s10151-014-1219-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elmér SE, Nygren JO, Lenander CE. A randomized trial of transanal hemorrhoidal dearterialization with anopexy compared with open hemorrhoidectomy in the treatment of hemorrhoids. Dis Colon Rectum. 2013;56:484–490. doi: 10.1097/DCR.0b013e31827a8567. [DOI] [PubMed] [Google Scholar]
- 20.De Nardi P, Capretti G, Corsaro A, Staudacher C. A prospective, randomized trial comparing the short- and long-term results of doppler-guided transanal hemorrhoid dearterialization with mucopexy versus excision hemorrhoidectomy for grade III hemorrhoids. Dis Colon Rectum. 2014;57:348–353. doi: 10.1097/DCR.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 21.Giordano P, Tomasi I, Pascariello A, Mills E, Elahi S. Transanal dearterialization with targeted mucopexy is effective for advanced haemorrhoids. Colorectal Dis. 2014;16:373–376. doi: 10.1111/codi.12574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tempel MB, Pearson EG, Page M, et al. Survey of patient satisfaction after Doppler-guided transanal hemorrhoidal dearterialization performed in ambulatory settings. Tech Coloproctol. 2014;18:607–610. doi: 10.1007/s10151-013-1104-x. [DOI] [PubMed] [Google Scholar]
- 23.Béliard A, Labbé F, de Faucal D, Fabreguette JM, Pouderoux P, Borie F. A prospective and comparative study between stapled hemorrhoidopexy and hemorrhoidal artery ligation with mucopexy. J Visc Surg. 2014;151:257–262. doi: 10.1016/j.jviscsurg.2014.03.009. [DOI] [PubMed] [Google Scholar]
- 24.Ratto C, Parello A, Veronese E, et al. Doppler-guided transanal haemorrhoidal dearterialization for haemorrhoids: results from a multicentre trial. Colorectal Dis. 2015;17:10–19. doi: 10.1111/codi.12779. [DOI] [PubMed] [Google Scholar]
- 25.LaBella GD, Main WPL, Hussain LR. Evaluation of transanal hemorrhoidal dearterialization: a single surgeon experience. Tech Coloproctol. 2015;19:153–157. doi: 10.1007/s10151-015-1269-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rubbini M, Tartari V. Doppler-guided hemorrhoidal artery ligation with hemorrhoidopexy: source and prevention of postoperative pain. Int J Colorect Dis. 2015;30:625–630. doi: 10.1007/s00384-015-2148-3. [DOI] [PubMed] [Google Scholar]