Abstract
Lumbar spondylolysis usually occurs as a stress fracture in the pars interarticularis of the vertebra. It is a prevalent sports-related disorder and a common cause of low back pain. We encountered five athletes (4 males, 1 female) with severe low back pain. Mean age was 14.5 years. All five patients were found to have bilateral pars fracture. In all cases, staging based on the findings from computed tomography scan of the right and left pars fracture was different. On short tau inversion recovery magnetic resonance imaging (STIR-MRI) of the comparatively newer more recently injured side, high signal intensity changes were obvious and dominant at the intra- and extraosseous area, which would indicate tissue edema and/or bleeding. Furthermore, the imaging findings corresponded to the side of the low back pain. In conclusion, STIR-MRI can effectively distinguish between painful pars fracture and painless pars fracture.
Keywords: pars fracture, spondylolysis, STIR-MRI, bleeding, edema
Introduction
Lumbar spondylolysis usually occurs as a stress fracture in the pars interarticularis of the vertebra in children and adolescents particularly among active athletes.1–6) During the stage of non-pseudoarthrosis, osseous healing can be achieved with brace treatment; however, with progression to pseudoarthrosis, osseous healing cannot be achieved without surgery.1–5,7)
Magnetic resonance imaging (MRI) has recently been reported to provide useful information for early diagnosis. Yamane et al. first reported that T1-weighted MR images in the coronal plane show a hypointense area in the pars interarticularis before this becomes obvious on computed tomography (CT).8) Sairyo et al. reported that bone marrow edema (low signal on T1 weighted and high signal on T2-weighted images) in the adjacent pedicle is the indicator for the early stage of pars fracture.7) Furthermore, the same group reported that facet joint and pars defect effusion caused by synovitis would be the pain generator in the pseudoarthrosis stage of pars fracture and can be detected by short tau inversion recovery (STIR)-MRI.9) They also emphasized that patients may complain of leg symptoms such as pain and numbness due to nerve root irritation by extraosseous bleeding from the pars fracture, and MRI provides valuable information as to the exact diagnosis.10)
From 2015 April to 2016 March 106 young athletes, who had lumbar spondylolysis, had consulted to our hospital. Among these patients, 13 patients had one side of low back pain and they had examined STIR-MRI. We showed typical 5 cases of bilateral pars fracture in which staging differed between the right and left sides. STIR-MRI was effective to distinguish painful pars fracture from painless pars fracture. We discuss the utility of STIR-MRI for identifying the pain generator of pars fracture.
Case Reports
Relevant background information regarding all five cases is summarized in Table 1.
Table 1.
Summary of five cases
| Age | Gender | Sports | The side of low back pain | CT stage | High-signal change side on MRI | |||
|---|---|---|---|---|---|---|---|---|
| Right | Left | Right | Left | |||||
| Case 1 | 17 | Male | Basketball | Right | Progressive | Terminal | + | − |
| Case 2 | 9 | Male | Baseball | Right | Progressive | Terminal | + | − |
| Case 3 | 20 | Male | Track and field | Left | Terminal | Early | − | + |
| Case 4 | 17 | Male | Soccer | Right | Progressive | Terminal | + | − |
| Case 5 | 11 | Female | Volleyball | Right | Early | Progressive | + | − |
Case 1
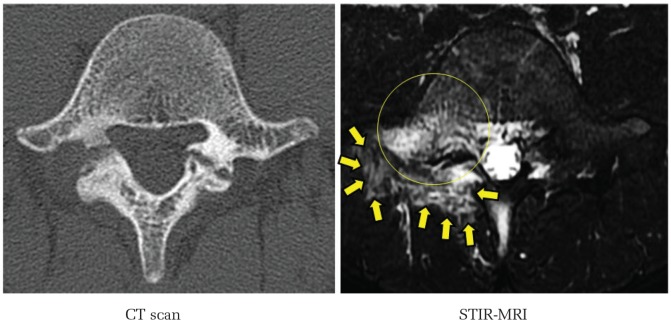
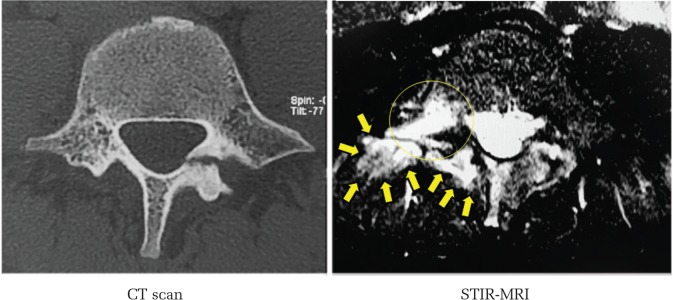
A 17-year-old male basketball player visited us with a complaint of severe right-sided low back pain. CT revealed bilateral pars fracture at L5. Staging based on CT according to the classification of Fujii et al.2) was progressive and terminal for the right and left sides, respectively. On STIR-MRI, there was obvious extraosseous edema and bleeding around the right pars fracture. The MRI findings were in good correlation with the clinical finding of low back pain (Fig. 1).
Fig. 1.
Case 1: 17-year-old male basketball player. Axial view of CT and STIR-MRI. Circle shows bone marrow edema, arrows show extraosseous edema and bleeding around right pars fracture.
Case 2
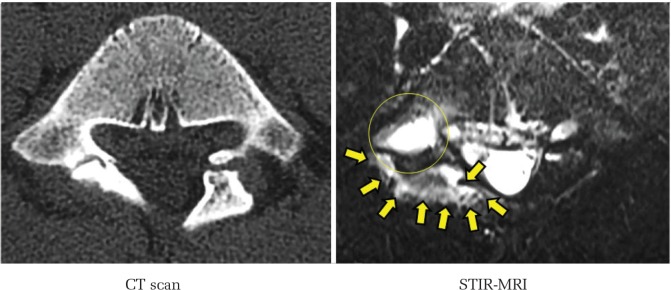
A 9-year-old male baseball player visited us with a complaint of severe right-sided low back pain. CT revealed bilateral pars fracture at L5. The stage based on CT was progressive and terminal stage for the right and left sides, respectively. On STIR-MRI, obvious high signal changes (HSC) were found around the right pars fracture. In the pedicle adjacent to the right pars fracture, marrow edema was also observed. In contrast, no such findings were seen around the terminal stage pars fracture on the left side. The MRI findings were in good correlation with the clinical finding of low back pain (Fig. 2).
Fig. 2.
Case 2: 9-year-old male baseball player. Axial view of CT and STIR-MRI. Circle shows bone marrow edema, arrows show extraosseous edema and bleeding around right pars fracture.
Case 3
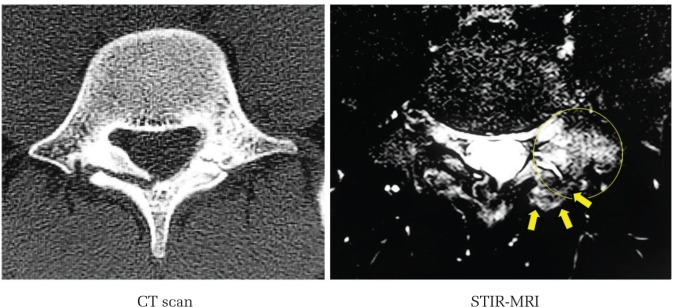
A 20-year-old male hurdler consulted at our sports clinic because of severe left-sided low back pain. CT revealed bilateral pars fracture at L5. Staging based on CT was terminal on the right and progressive stage on the left side. There was obvious HSC around the left pars fracture indicating extraosseous edema and bleeding. In the pedicle adjacent to the left pars fracture, marrow edema was also observed. However, no such findings were noted on the right side. The MRI findings were consistent with the side of severe low back pain (Fig. 3).
Fig. 3.
Case 3: 20-year-old male hurdler (track and field). Axial view of CT and STIR-MRI. Circle shows bone marrow edema, arrows show extraosseous edema and bleeding around right pars fracture.
Case 4
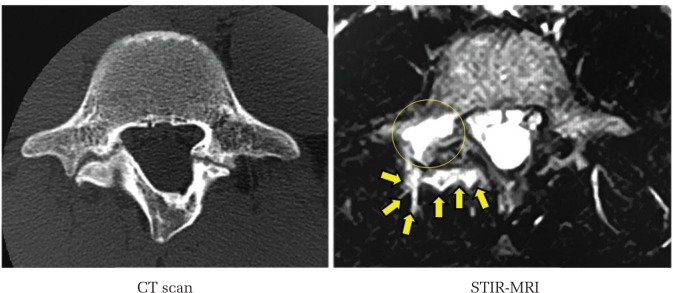
A 17-year-old male soccer player consulted us because of severe right-sided low back pain. CT revealed bilateral pars fracture at L5. Staging based on CT was progressive on the right and terminal stage on the left side. There was obvious HSC around the right pars fracture indicating extraosseous edema and bleeding. In the pedicle adjacent to the right pars fracture, marrow edema was also noted. However, there were no such findings on the left side. The MRI findings were consistent with the side of the severe low back pain (Fig. 4).
Fig. 4.
Case 4: 17-year-old male soccer player. Axial view of CT and STIR-MRI. Circle shows bone marrow edema, arrows show extraosseous edema and bleeding around right pars fracture.
Case 5
An 11-year-old female volleyball player visited us with a complaint of severe low back pain on both sides; the pain was more severe on the right side than on the left side. CT revealed bilateral pars fracture at L5. Staging based on CT was early and progressive stage for the right and left sides, respectively. On STIR-MRI, there was obvious extraosseous edema and bleeding around both pars fractures. However, the area of the HSC was larger on the right side. The MRI findings were in good correlation with the clinical finding of low back pain (Fig. 5).
Fig. 5.
Case 5: 11-year-old female volleyball player. Axial view of CT and STIR-MRI. Circle shows bone marrow edema, arrows show extraosseous edema and bleeding around right pars fracture.
Discussion
In this paper, we describe 5 cases of bilateral pars fracture at the level of L5. In all five cases, the staging based on CT of the right and left sides was different. For such asymmetrical staging of lumbar spondylolysis, we performed STIR-MRI to investigate which would be the more painful side. On STIR-MRI, extraosseous bleeding or edema, which was identified as HSC was demonstrated around the pars fracture in all 5 cases. The findings were also asymmetric. The side showing the HSC was well correlated with the painful side. Thus, STIR-MRI can provide useful information that can help to understand the painful side in bilateral pars fractures.
Mirowitz et al. explained the strengths of STIR-MRI stating that the procedure enabled clear visualization of bone marrow lesions by fat suppression and that depicting the extent of bone marrow edema was more sensitive on STIR than on other types of MRI.11) It has also been reported that STIR-MRI is sufficiently sensitive to visualize effusion and that indistinct bone marrow edema could possibly be indicated as hyperintensity relative to the background of suppressed fat.12) Here, we present several images of a variety of spinal disorders, and discuss the significance of STIR on accurate diagnosis such as metastatic tumor, acute fracture, insufficiency fracture, infection, and inflammatory arthritis.12)
Regarding spinal disorders, it has been reported that high-signal intensity on STIR-MRI would be a good indicator to help distinguish between acute and old compression fracture.13,14) Borg et al. reported cases with high signal intensity at the posterior spine structures, and suggested an association with clinically observable pain and functional limitation.15) Mineta et al. reported a case of painful type I Modic change in the lumbar spine16) in which STIR-MRI was useful to demonstrate inflammatory changes around the endplate. These reports in the literature indicate the importance of STIR in understanding pain generators in the spine in conditions such as fractures, inflammatory disorders, tumors, and other conditions.
Concerning STIR-MRI for lumbar spondylolysis, Sairyo et al.3) utilized this modality to elucidate the pain generator among pediatric patients with spondylolysis. All spondylolysis was of the terminal (pseudoarthrosis) stage. Because STIR can demonstrate indistinct joint effusion, the authors described synovitis in pars fracture as the pain mechanism. Early-stage spondylolysis in children is particularly difficult to diagnose on plain radiographs. Thus, in 2006, Sairyo et al. first proposed bone marrow edema in the adjacent pedicle as the indicator of early-stage spondylolysis.7) Subsequently in 2012, the group reported that marrow edema of the pedicle would be obvious on STIR-MRI.4) Borg et al. analyzed pedicle bone marrow in 646 cases, and found that marrow edema on STIR-MRI was apparent in 1.7%.15) The associated disorders were pars fractures, pedicle fractures, and degenerative facets.
In this case series, we presented asymmetric MRI findings in pars fractures with asymmetric staging. Our results show that extraosseous HSC was obvious in the comparatively early stage of pars fracture. This information would be indicative of the pain generator for the patient. Moreover, we previously reported abnormal extraosseous findings on T2-weighted MRI in pars fracture10) where we demonstrated the possibility of radiculopathy due to extraosseous hematoma or bleeding from pars fracture. We, however, failed to discuss the asymmetric changes on MRI. We then performed further evaluation mainly by T2-weighted MRI. In the present study, by using STIR-MRI, HSC which is indicative of extraosseous bleeding, hematoma, or edema around a painful pars fracture was clearly shown.
In conclusion, we presented 5 cases of bilateral pars fracture with asymmetric STIR-MRI findings. STIR-MRI is effective for distinguishing painful pars fracture from painless pars fracture.
Footnotes
Conflicts of Interest Disclosure
One of the authors, Koichi Sairyo has conflict of interest (Japan MDM, Senko Medical, Surgical Spine). However, these companies are not concerned with the content of this manuscript. Other authors report no conflicts of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- 1).Morita T, Ikata T, Katoh S, Miyake R: Lumbar spondylolysis in children and adolescents. J Bone Joint Surg Br 77: 620–625, 1995 [PubMed] [Google Scholar]
- 2).Fujii K, Katoh S, Sairyo K, Ikata T, Yasui N: Union of defects in the pars interarticularis of the lumbar spine in children and adolescents. The radiological outcome after conservative treatment. J Bone Joint Surg Br 86: 225–231, 2004 [DOI] [PubMed] [Google Scholar]
- 3).Sairyo K, Sakai T, Yasui N: Conservative treatment of lumbar spondylolysis in childhood and adolescence: the radiological signs which predict healing. J Bone Joint Surg Br 91: 206–209, 2009 [DOI] [PubMed] [Google Scholar]
- 4).Sairyo K, Sakai T, Yasui N, Dezawa A: Conservative treatment for pediatric lumbar spondylolysis to achieve bone healing using a hard brace: what type and how long?: Clinical article. J Neurosurg Spine 16: 610–614, 2012 [DOI] [PubMed] [Google Scholar]
- 5).Sakai T, Tezuka F, Yamashita K, et al. : Conservative treatment for bony healing in pediatric lumbar spondylolysis. Spine (Phila Pa 1976) 42: E716–E720, 2017 [DOI] [PubMed] [Google Scholar]
- 6).Nitta A, Sakai T, Goda Y, et al. : Prevalence of symptomatic lumbar spondylolysis in pediatric patients. Orthopedics 39: e434–e437, 2016 [DOI] [PubMed] [Google Scholar]
- 7).Sairyo K, Katoh S, Takata Y, et al. : MRI signal changes of the pedicle as an indicator for early diagnosis of spondylolysis in children and adolescents: a clinical and biomechanical study. Spine (Phila Pa 1976) 31: 206–211, 2006 [DOI] [PubMed] [Google Scholar]
- 8).Yamane T, Yoshida T, Mimatsu K: Early diagnosis of lumbar spondylolysis by MRI. J Bone Joint Surg Br 75: 764–768, 1993 [DOI] [PubMed] [Google Scholar]
- 9).Sairyo K, Sakai T, Mase Y, et al. : Painful lumbar spondylolysis among pediatric sports players: a pilot MRI study. Arch Orthop Trauma Surg 131: 1485–1489, 2011 [DOI] [PubMed] [Google Scholar]
- 10).Sairyo K, Sakai T, Amari R, Yasui N: Causes of radiculopathy in young athletes with spondylolysis. Am J Sports Med 38: 357–362, 2010 [DOI] [PubMed] [Google Scholar]
- 11).Mirowitz SA, Apicella P, Reinus WR, Hammerman AM: MR imaging of bone marrow lesions: relative conspicuousness on T1-weighted, fat-suppressed T2-weighted, and STIR images. AJR American J Roentgenol 162: 215–221, 1994 [DOI] [PubMed] [Google Scholar]
- 12).Long SS, Yablon CM, Eisenberg RL: Bone marrow signal alteration in the spine and sacrum. AJR Am J Roentgenol 195: W178–W200, 2010 [DOI] [PubMed] [Google Scholar]
- 13).Lenski M, BüSer N, Scherer M: Concomitant and previous osteoporotic vertebral fractures. Acta Orthop 88: 192–197, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Wang B, Fintelmann FJ, Kamath RS, Kattapuram SV, Rosenthal DI: Limited magnetic resonance imaging of the lumbar spine has high sensitivity for detection of acute fractures, infection, and malignancy. Skeletal Radiol 45: 1687–1693, 2016 [DOI] [PubMed] [Google Scholar]
- 15).Borg B, Modic MT, Obuchowski N, Cheah G: Pedicle marrow signal hyperintensity on short tau inversion recovery- and t2-weighted images: prevalence and relationship to clinical symptoms. AJNR Am J Neuroradiol 32: 1624–1631, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).Mineta K, Higashino K, Sakai T, Fukui Y, Sairyo K: Recurrence of type I Modic inflammatory changes in the lumbar spine: effectiveness of intradiscal therapy. Skeletal Radiol 43: 1645–1649, 2014 [DOI] [PubMed] [Google Scholar]