Abstract
This study aimed to obtain the prevalence of hyperlipidemia and its related factors in Shanxi Province, China using multivariate logistic regression analysis and tabu search-based Bayesian networks (BNs). A multi-stage stratified random sampling method was adopted to obtain samples among the general population aged 18 years or above. The prevalence of hyperlipidemia in Shanxi Province was 42.6%. Multivariate logistic regression analysis indicated that gender, age, region, occupation, vegetable intake level, physical activity, body mass index, central obesity, hypertension, and diabetes mellitus are associated with hyperlipidemia. BNs were used to find connections between those related factors and hyperlipidemia, which were established by a complex network structure. The results showed that BNs can not only be used to find out the correlative factors of hyperlipidemia but also to analyse how these factors affect hyperlipidemia and their interrelationships, which is consistent with practical theory, is superior to logistic regression and has better application prospects.
Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide, accounting for 30% of all deaths1. As an influencing factor of cardiovascular disease2–5, hyperlipidemia plays an important role in the occurrence and development of CVD6. However, with increased economic development, improvement of living standards, and changes in lifestyle, the prevalence of hyperlipidemia has been gradually increasing in China1,7–9. The results of the 2002 Chinese National Nutrition and Health Survey showed that the prevalence of hyperlipidemia was 18.6%1. In 2007, a survey of 43,368 residents in China over age 18 years demonstrated that the prevalence of hyperlipidemia had increased to 33.97%7. Another report in 2014 showed that the prevalence of hyperlipidemia in China reached as high as 41.9%9. Hyperlipidemia has become an important public health problem; therefore, it is of great importance to comprehensively analyse the related factors of hyperlipidemia to prevent its occurrence.
As shown in previous studies, gender, age, lifestyle, obesity, diabetes mellitus, dietary structure, and other factors directly or indirectly affect the incidence and progress of hyperlipidemia6,7,10,11. Most previous studies on factors related to hyperlipidemia have used logistic regression based on independent variables, and odds ratio values to reflect the degree of association; however, in reality, these factors are often interdependent and may have a complex network structure, which cannot meet the assumptions of a logistic regression model and lead to the failure of logistic regression to describe this relationship. In addition, the relating factors of logistic regression are parallel, which cannot infer the part they play in the occurrence and development of hyperlipidemia. Mancini et al.12,13 stated that traditional statistical methods such as logistic regression, are ineffective for describing the relationship between variables in the biomedical domain because of their limitations of independency. Bayesian networks (BNs) can overcome this shortcoming and has become a popular method for analysing the relationship between variables in biomedical field. The BN method is a technique based on the probability of uncertainty reasoning and has no strict requirements for statistical assumptions. In the BN method, a directed acyclic graph (DAG) is constructed to intuitively reflect the potential relationship between factors, and a conditional probability distribution table is used to reflect the strength of association14. Unlike logistic regression, BNs allow for estimating the subsequent probability of any target variable given any set of conditioning variables15,16, which can predict the probability of having dyslipidemia in a more flexible manner. Tabu search is a metaheuristic approach proposed by Glover and it is one of the most efficient optimization techniques that incorporates adaptive memory to escape local search and find the global optimum17. Hence, we applied BNs optimized with a tabu search algorithm to jointly model dyslipidemia and its related factors and determine how these factors impact dyslipidemia, to offer comprehensive strategies for effectively reducing the incidence of hyperlipidemia.
Results
Characteristics of the study population
Among the 4,776 initial participants in our study, we excluded 671 with incomplete data. Finally, A total of 4,105 participants (1,748 men and 2,357 women) were included in this study; 2,581 (62.9%) participants came from rural regions and 1,524 (37.1%) were from urban areas. The median age was 51.5 years, ranging from age 18 to 108 years.
Detection rate of dyslipidemia
Figure 1 shows the distribution of TC, TG, HDL-C, and LDL-C in participant blood samples. Of 4,105 participants, 1,748 were diagnosed as having dyslipidemia, The detection rate was 42.6% (45.7% for male, 40.3% for female). The detection rates of hypercholesterolemia, hypertriglyceridemia, HDL-C, and LDL-C were 6.1%, 16.4%, 33.8%, and 5.1%, respectively. The main types of hyperlipidemia in Shanxi Province were low HDL-C, followed by hypertriglyceridemia.
Figure 1.
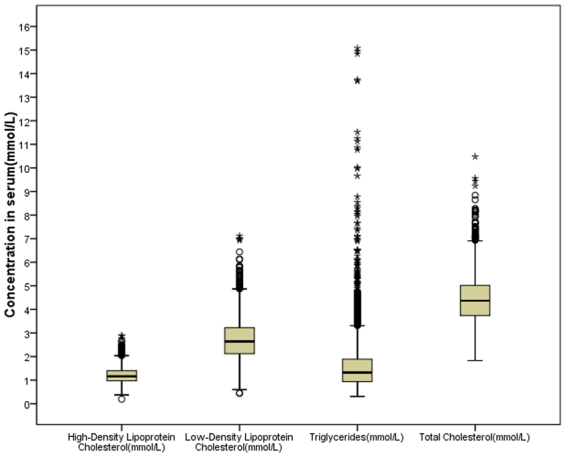
Concentrations of total cholesterol, triglycerides, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol in blood samples among study participants. The figure was plotted using IBM SPSS 22.0 (https://www.ibm.com).
Univariate analysis
Supplementary Table S1 shows related factors and their assignment. Supplementary Tables S2–S5 show differences in the prevalence of dyslipidemia among participants with different characteristics. Factors such as old age, male, rural residence, employers, higher educational level, higher BMI value, sufficient intake of vegetables, insufficient physical activity, central obesity, and having a history of hypertension and diabetes mellitus showed a higher prevalence of dyslipidemia (all, P < 0.10). As depicted in Fig. 2 and Table 1, men younger than age 60 years were more inclined to have higher prevalence of dyslipidemia than women in the same age group (P < 0.1), whereas the detection rate of dyslipidemia increased with age in women (P < 0.1); women over age 60 years had a significantly higher detection rate than men in the same age group (P < 0.1).
Figure 2.
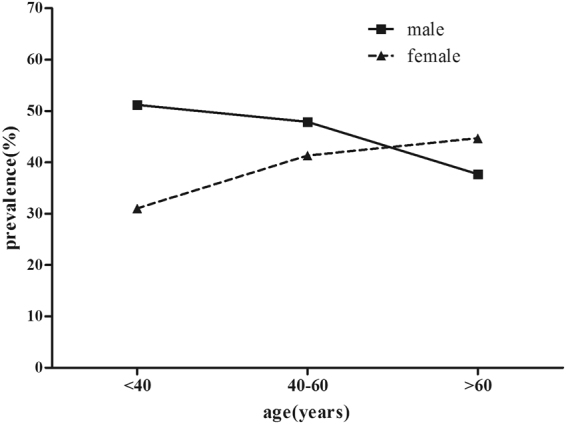
Prevalence of dyslipidemia by age groups. The figure was plotted using GraphPad Prism 5.01 (https://www.graphpad.com/).
Table 1.
Detection rate of dyslipidemia by different age groups and gender.
| Age (years) | Gender | Cases | hyperlipidemia | Prevalence (%) | χ 2 | P |
|---|---|---|---|---|---|---|
| <40 | Male | 326 | 167 | 51.2 | 31.263 | <0.001 |
| Female | 422 | 131 | 31.0 | |||
| 40~ | Male | 934 | 447 | 47.9 | 9.595 | 0.002 |
| Female | 1367 | 565 | 41.3 | |||
| 60~ | Male | 488 | 184 | 37.7 | 5.319 | 0.021 |
| Female | 568 | 254 | 44.7 |
Multivariate analysis
We conducted a multivariate logistic regression analysis using stepwise method (αin = 0.10, αout = 0.20) to select variables, with the presence of dyslipidemia as the dependent variable; independent variables were those that were significantly associated with dyslipidemia in univariate analysis. The multivariate analysis revealed that dyslipidemia was significantly associated with gender (OR 0.716, 95% CI: 0.628–0.817), age (OR 0.906, 95% CI: 0.817–1.005), region (OR 0.875, 95% CI: 0.762–1.005), occupation as a farmer (OR 0.844, 95% CI: 0.725–0.982), vegetable intake level (OR 1.080, 95% CI: 0.992–1.177), sufficient physical activity (OR 0.785, 95% CI: 0.653–0.944), BMI (OR 1.469, 95% CI: 1.327–1.626), central obesity (OR 1.698, 95% CI: 1.433–2.011), hypertension (OR 1.276, 95% CI: 1.109–1.468), and diabetes mellitus (OR 1.318, 95% CI: 1.057–1.643) (Table 2). Central obesity was strongly associated with hyperlipidemia (OR 1.760, 95% CI: 1.491–2.078), followed by BMI (OR 1.529, 95% CI: 1.382–1.692).
Table 2.
Multivariate logistic regression analyses on relaing factors of dyslipidemia.
| Factors | β | SE | wald χ2 | P | OR(95%CI) |
|---|---|---|---|---|---|
| Gender | −0.334 | 0.067 | 24.490 | <0.001 | 0.716(0.628,0.817) |
| Age | −0.098 | 0.053 | 3.489 | 0.062 | 0.906(0.817,1.005) |
| Region | −0.133 | 0.070 | 3.574 | 0.059 | 0.875(0.762,1.005) |
| vegetable intake level | 0.077 | 0.044 | 3.126 | 0.077 | 1.080(0.992,1.177) |
| hypertension | 0.244 | 0.072 | 11.589 | 0.001 | 1.276(1.109,1.468) |
| diabetes mellitus | 0.276 | 0.112 | 6.025 | 0.014 | 1.318(1.057,1.643) |
| BMI(kg/m2) | 0.385 | 0.052 | 54.841 | <0.001 | 1.469(1.327,1.626) |
| Central obesity | 0.529 | 0.086 | 37.442 | <0.001 | 1.698(1.433,2.011) |
| insufficient physical activity | 7.741 | 0.021 | |||
| Normal physical activity | −0.048 | 0.080 | 0.359 | 0.549 | 0.953(0.814,1.116) |
| sufficient physical activity | −0.242 | 0.094 | 6.654 | 0.010 | 0.785(0.653,0.944) |
| Other | 5.843 | 0.119 | |||
| Farmer | −0.170 | 0.077 | 4.828 | 0.028 | 0.844(0.725,0.982) |
| Retirees or unemployers | −0.099 | 0.137 | 0.520 | 0.471 | 0.906(0.693,1.185) |
| Employers | −0.013 | 0.105 | 0.016 | 0.899 | 0.987(0.804,1.212) |
| constant | −0.853 | 0.162 | 27.918 | <0.001 | 0.426 |
Bayesian networks model
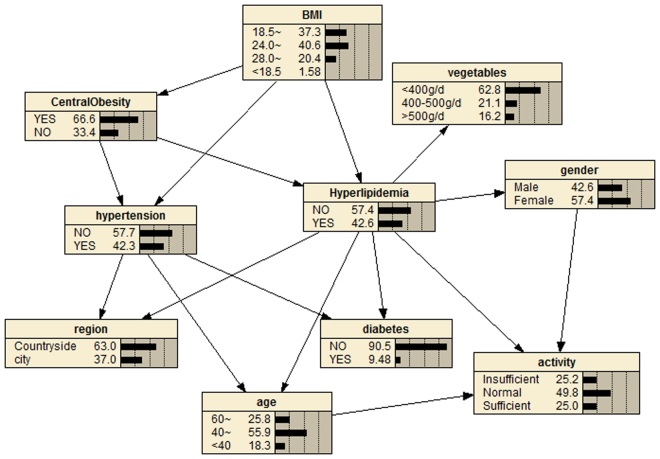
A probabilistic model with 10 nodes and 16 directed edges was built using BNs, considering those variables with significant differences in the multivariate logistic regression analysis (Fig. 3). Directed edges represent probabilistic dependencies between the nodes that are connected rather than the causal relationship between hyperlipidemia and the factors. Figure 3 shows that connections between hyperlipidemia and its related factors were established by a complex network structure, in which a direct connection between gender, age, region, occupation, vegetable intake level, physical activity, BMI, central obesity, diabetes mellitus, and hyperlipidemia were found (Fig. 3); in addition, hypertension was indirectly linked to hyperlipidemia through diabetes mellitus. We can also figure out the interrelationship between the related factors of hyperlipidemia from Fig. 3. For example, physical activity is related to gender and age; hypertension is associated with region, age, BMI, central obesity, and diabetes; BMI is also associated with central obesity. Supplementary Table S6 shows the CPT of hyperlipidemia, which quantitatively describes the relationship between the hyperlipidemia node and its parent nodes.
Figure 3.
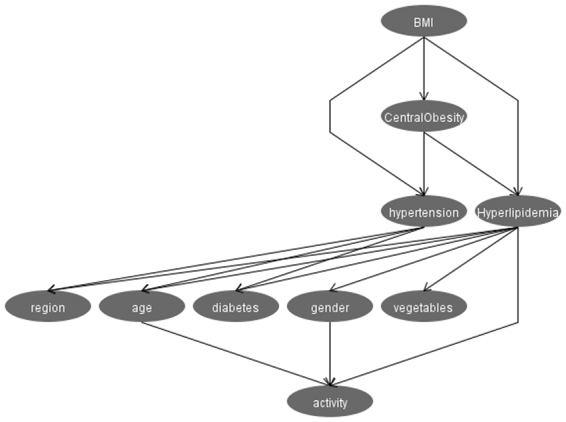
Bayesian Network model of factors relating to dyslipidemia. The figure was plotted using Weka 3.8.0 (https://www.cs.waikato.ac.nz/ml/weka/).
Reasoning model
Marginal probabilities of the variables are shown in Fig. 4. It can be seen that the marginal probability of hyperlipidemia was 42.6%. The resulting probabilistic model can be used to quantitatively analyse the impact of these factors on hyperlipidemia by computing the conditional probabilities P(y|xi). For example, Supplementary Fig. S1 shows that if a person has insufficient exercise, the detection rate of hyperlipidemia increases from the marginal value of 42.6% to P(hyperlipidemia|Lack of exercise) = 45.1%, and the detection rate of hyperlipidemia reaches 55.2% if this person has central obesity (Supplementary Fig. S2). We can see from Supplementary Fig. S3 that if this person is also obese (according to BMI), then they have a 59.4% probability of having hyperlipidemia; the probability increases to 65.0% when this person has concurrent diabetes mellitus (Supplementary Fig. S4). Bayesian networks can also be used to study the interrelationship between related factors. For example, we can see from Supplementary Figs S5 and S6 that if a person has diabetes mellitus, the probability of developing hypertension increases to 60%, and if he has hypertension, the probability of having diabetes mellitus increases to 13.4%. In addition, if a person has insufficient exercise, the probability of having central obesity, diabetes mellitus, and hypertension is increased to 67.6%, 9.73%, and 44.9%, respectively.
Figure 4.
Bayesian network model. Marginal probabilities. The figure was plotted using Netica (www.norsys.com).
Discussion
The increasing prevalence of dyslipidemia had become a worldwide public health problem. We found a detection rate of dyslipidemia was 42.6% in Shanxi Province of China, which is considerably higher than the nationally reported prevalence of dyslipidemia9 (41.9%) as well as those reported in other provinces of China1,3,11,18. Therefore, Shanxi Province should give more attention to the prevention and control of hyperlipidemia, as studies have shown that preventing and controlling hyperlipidemia can play a major role in both primary prevention and secondary prevention of CVD19,20.
In our study, the main types of dyslipidemia in Shanxi Province were low HDL-C, followed by hypertriglyceridemia, findings that are consistent with those from other studies in Asian countries18. This phenomenon probably reflects the growing high intake of simple carbohydrates and high-fat diets that have emerged in recent decades, which clearly affect serum triglyceride concentrations18. In addition, the hyperlipidemia prevalence varies widely with different demographic characteristics and lifestyles. It is noteworthy that we found that the detection rate of hyperlipidemia in participants with excessive intakes of fresh vegetables was unexpectedly high, which may be related to a conscious increase of vegetable consumption among these participants upon konwing that they had hyperlipidemia. The prevalence of hyperlipidemia in the population over the age 60 years has been reduced, probably because more people over the age of 60 years with hyperlipidemia have died from hyperlipidemia complications or other diseases. As shown in Fig. 2 and Table 1, men under age 60 years were more inclined to have higher prevalence of dyslipidemia than women in the same age group (P < 0.10) whereas the detection rate of dyslipidemia increased with age in women (P < 0.10); women over 60 years old had a significantly higher detection rate than men in the same age group (P < 0.10), which may be associated with reduced sex hormones.
At the same time, hyperlipidemia was found to be closely related to hypertension and diabetes mellitus. A total 52.2% of diabetes mellitus patients and 49.1% of patients with hypertension had dyslipidemia, whereas the prevalence of dyslipidemia among their counterparts without diabetes mellitus or hypertension was 41.6%, 37.8%, respectively. Previous studied have showed that diabetes mellitus and hypertension are associated with dyslipidemia, even after adjusting for other relative variables21,22. Although the relevant factors of hyperlipidemia have been identified, how these related factors are associated with hyperlipidemia have rarely been studied.
The Bayesian network model shows connections between hyperlipidemia and those related factors that were established by a complex network structure. Of these, direct connections between gender, age, region, occupation, vegetable intake level, physical activity, BMI, central obesity, diabetes mellitus, and hyperlipidemia were found (Fig. 3) whereas hypertension was indirectly linked to hyperlipidemia. The BN model can also be used to figure out the interrelationship between related factors of hyperlipidemia whereas multivariate logistic regression cannot for its limitations of independency23. The results summarized above show that the BNs model can be used to assess the dependency of hyperlipidemia on all factors included in the model, as well as the interrelationships between these factors, which makes it convenient for exploring the internal relationships between factors, to thereby improve hyperlipidemia prevention.
BNs can infer the probability of an unknown node (hyperlipidemia) based on the state of known nodes16. For example, according to the reasoning model of hyperlipidemia, we know that if a person engages in insufficient exercise, the detection rate of hyperlipidemia increases from 42.6% to 45.1% (Supplementary Fig. S1) whereas the prevalence reaches 55.2% if this person has central obesity (Supplementary Fig. S2). If this person is also obese, then he has a 59.4% probability of having hyperlipidemia (Supplementary Fig. S3); the probability increases to 65.0% when this person has diabetes mellitus concurrently (Supplementary Fig. S4). Therefore, maintaining body weight within a reasonable range, getting sufficient physical exercise, and diabetes prevention should be given priority, to reduce the occurrence of hyperlipidemia.
Although they are current method of choice for evaluating factors related to dyslipidemia, multivariable logistic regression models are often constrained by issues such as an inability to find how factors impact on outcome variable, inability to assess the interrelationships between factors, and independent restrictions of variables, which contribute to the conundrum of implementation to comprehensively analyse the factors affecting dyslipidemia. However, BNs can solve this problem and have their own merits. BNs can combine prior information with sample information to avoid subjective bias by only using prior knowledge, as well as avoiding bias by only using sample knowledge24. BNs can also predict the probability of an unknown node by the state of known nodes25, deal with problems of incomplete data26, handle situations of uncertain information and excessive variables using probability theory with a solid mathematical basis, and can display results as an intuitive graphic27. However, BNs also have some limitations, for example, the direct arcs of the constructed BNs do not provide cause–effect relationships but rather show how the various parameters are influenced (statistically) by each other. Only the BNs established by causal relationship with directed edges indicate cause–effect relationships28.
Methods
Study participants
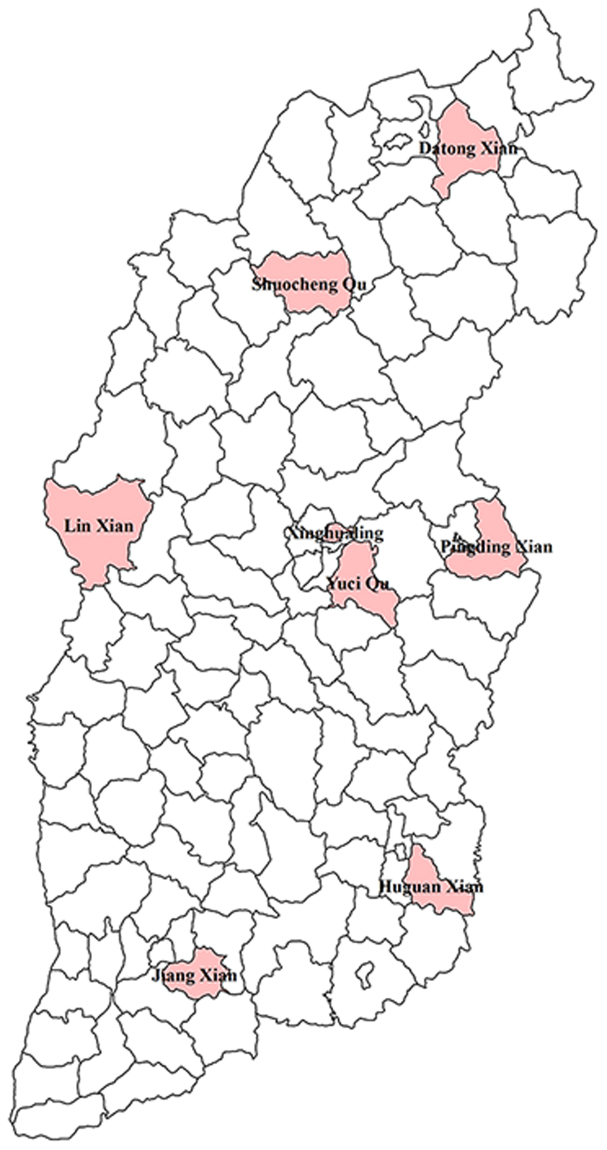
Participants were included in the China National Chronic Diseases Survey, which was conducted in Shanxi Province in 2013. In this survey, a multi-stage stratified random sampling method was used to obtain representative samples. In the first stage, eight representative monitoring points were randomly selected in Shanxi Province. Figure 5 shows the distribution of these monitoring points in the province; it can be seen that the monitoring points are evenly distributed in Shanxi Province. In the second stage, four townships or streets were randomly selected from each monitoring point. In the third stage, three villages/committees/organizations were randomly selected from each township/street. The fourth stage involved random selection of one group containing 50 households from each selected residential committee/village/organization. In the final stage, a standard Kish table was adopted to randomly select one person aged 18 years or above from each household. If the selected individual was unable or ineligible to participate, a similar household in the same or an adjacent neighbourhood or village was randomly selected as a replacement. Finally, a total of 4,776 participants completed the survey and physical examination. This study was approved by the China Chronic Disease Center Ethics Committee, with reference number 201307. Informed consent was signed by all study participants or their agents. All experiments were performed according to the relevant guidelines and regulations.
Figure 5.
The distribution of monitoring points in Shanxi Province. The figure was plotted using ArcGIS 10.2 (www.esri.com/).
The eligibility criteria for the study was all residents aged 18 years or above who had been living in the monitoring area for more than 6 of the previous 12 months. Exclusion criteria for this study were those residents who lived in functional areas, such as sheds, military or student dormitories, nursing homes, and so on.
Data collection
Questionnaire interview
A written informed consent was given to all participants before the collection of data. After signing the informed consent, all participants received a questionnaire established by the China Center for Disease Control and Prevention (CDC) on chronic disease. A direct face-to-face questionnaire interview was carried out by uniformly trained investigators. The questionnaire included information on general demographic characteristics (such as region, age, sex, level of education, and occupation), lifestyles (such as smoking, drinking, dietary habits, and physical activity), and past medical history (such as hypertension and diabetes mellitus).
Anthropometric measures
Anthropometric measurements including height, weight, waist circumference and blood pressure were taken. Height and weight were measured with participants wearing light indoor clothing and no shoes, following a standardized protocol, to the nearest 0.1 cm and 0.1 kg, respectively. Waist circumference was measured twice at the midpoint level of the midaxillary line between the lower edge of the ribcage and the iliac crest. After ensuring that the difference between the two measurements was less than 2 cm, the second measured value was then recorded. Blood pressure were measured while participants were in a seated position following a 5-min rest period. Third consecutive blood pressure (BP) readings were taken using an electronic sphygmomanometer (OMRON HEM-7071 or HEM-770A), with an accuracy of 1 mmHg; the averages were then calculated for a final blood pressure reading.
Laboratory assays
Laboratory assays included blood glucose, blood lipids, glycosylated haemoglobin, and so on. Samples for detecting blood sugar were kept in cold storage at 2–8 °C until they were sent to a local laboratory for measurement of fasting glucose and 2-h postprandial plasma glucose in 48 hours. Other samples were stored at −60 to −80 °C in specialized areas, or at −20 °C in areas that did not have cryopreservation facilities, until being transported to the medical inspection organizations designated by the state for blood lipid and glycosylated haemoglobin testing within one month.
Bayesian networks (BNs)
A Bayesian network is a directed acyclic graph (DAG) based on probability theory and graph theory29, which consists of nodes representing the variables U = {Xi, …, Xn} and directed edges symbolizng the relationships between the variables13,27,30,31. If there is an edge from Xi to Xj, then we say that node is the parent of Xj and Xj is the child of Xi. Each node has a conditional probability distribution table (CPT), which quantitatively describes the probability dependence of the nodes and its parent nodes28. From the perspective of probability theory, a BN represents the joint distribution of a set of random variables, according to the chain rule and conditional independence, the joint distribution of a series of random variables X = { can be written as:
| 1 |
is the collection of the parent of Xi, ⊆ , given the value of is conditionally independent of other variables32 in .
Tabu search algorithm
A tabu search (TS) algorithm starts from a feasible initial solution; the neighbour solutions are generated through a sequence of moves. If a movement in a certain direction is found that makes the objective function value change the most, it will be placed into the tabu list and is considered one of the optimal solutions in the local area, unless it was in the tabu list. Then the initial solution is replaced with this new optimal solution and it continues to move to its neighbourhood, looking for the next optimal solution nearest the previous optimal solution, repeating the cycle continuously until the convergence criteria are met, at which point the search process is stopped33.
Definitions
In accordance with Chinese Guidelines on Prevention and Treatment of Dyslipidemia in Adults published in 2007, hyperlipidemia was defined as the presence of any one of the following four conditions: hypercholesterolemia (total cholesterol (TC; ≥ 6.22 mmol/L); hypertriglyceridemia (triglycerides (TG) ≤ 2.26 mmol/L); low levels of high-density lipoprotein cholesterol (HDL-C; < 1.04 mmol/L); or high levels of low-density lipoprotein cholesterol (LDL-C; ≥ 4.14 mmol/L)9.
According to Guidance on Prevention and Control of Hypertension in Chinese Residents, hypertension was defined as individuals with an average measured systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg, or who reported having been diagnosed with hypertension or receiving BP-lowering treatment34. Diabetes mellitus was defined as fasting glucose ≥ 7.0 mmol/L or 2-h postprandial plasma glucose ≥ 11.1 mmol/L or who reported having been diagnosed with diabetes mellitus35.
Participants who reported smoking ≥ 1 cigarette a day for the previous 6 months were defined as smokers. Body weight was categorized as normal weight (body mass index (BMI) ≥ 18.5 kg/m2 and < 24 kg/m2), overweight (BMI ≥ 24 kg/m2 and < 28 kg/m2), and obese (BMI ≥ 28 kg/m2)36. Central obesity refers to waist circumference ≥ 85 cm for male and ≥ 80 cm for female37. Bradycardia means heart rate less than 60 beats/min, tachycardia refers to heart rate greater than 100 beats/min, and normal heart rate is between 60 and 100 beats/min38. Physical activity was categorized into low, moderate, and high groups based on the upper quartile and lower quartile of weekly metabolic equivalent.
Statistical analyses
Categorical variables were summarized as proportions, and chi-square tests were applied to compare categorical variables. Multivariate logistic regression and Bayesian networks were used to explore the factors related to hyperlipidemia.
Statistical description, chi-square tests, and multivariate logistic regression were performed using IBM SPSS Version 22 (IBM Corp., Armonk, NY, USA). Significance for all statistical tests was a priori at P < 0.10 and all P values were two-tailed; Weka 3.8.0 (Waikato Environment for Knowledge Analysis; the University of Waikato, New Zealand) was used for structural learning and parametric learning of BNs. The BN models and reasoning models were drawn using Netica (Norsys Software Corp., Vancouver, BC, Canada). In addition, the maximum likelihood method was used to obtain the values for CPT.
Data availability
All data generated or analyzed during this study are included in its Supplementary Information files.
Electronic supplementary material
Acknowledgements
The authors thank Analisa Avila, ELS, of Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Author Contributions
J.H.P. and Z.P.R. conceived the study; J.H.P., Z.P.R., Y.L.H., C.L.L., and X.J.Y. conducted the survey and collected data; W.H.L. and Z.W. processed the data; J.H.P., H.R., Z.Z., and W.M.S. analysed the results; J.H.P. and Z.P.R. wrote the main manuscript text; and L.X.Q. and L.M.C. gave constructive suggestions for the manuscript. All authors revised the manuscript for important intellectual content and approved the final version.
Competing Interests
The authors declare no competing interests.
Footnotes
Jinhua Pan and Zeping Ren contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-22167-2.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
LiMin Chen, Email: sxchenlimin@163.com.
Lixia Qiu, Email: qlx_1126@163.com.
References
- 1.Cai L, Zhang L, Liu A, Li S, Wang P. Prevalence, awareness, treatment, and control of dyslipidemia among adults in Beijing, China. Journal of atherosclerosis and thrombosis. 2012;19:159–168. doi: 10.5551/jat.10116. [DOI] [PubMed] [Google Scholar]
- 2.Degano IR, et al. The association between education and cardiovascular disease incidence is mediated by hypertension, diabetes, and body mass index. Scientific reports. 2017;7:12370. doi: 10.1038/s41598-017-10775-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.He H, et al. Dyslipidemia awareness, treatment, control and influence factors among adults in the Jilin province in China: a cross-sectional study. Lipids in health and disease. 2014;13:122. doi: 10.1186/1476-511X-13-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang FL, et al. The prevalence, awareness, treatment, and control of dyslipidemia in northeast China: a population-based cross-sectional survey. Lipids in health and disease. 2017;16:61. doi: 10.1186/s12944-017-0453-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mooradian AD. Dyslipidemia in type 2 diabetes mellitus. Nat Clin Pract End Met. 2009;5:150–159. doi: 10.1038/ncpendmet1066. [DOI] [PubMed] [Google Scholar]
- 6.Gao N, et al. Dyslipidemia in rural areas of North China: prevalence, characteristics, and predictive value. Lipids in health and disease. 2016;15:154. doi: 10.1186/s12944-016-0328-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan L, et al. The prevalence, awareness, treatment and control of dyslipidemia among adults in China. Atherosclerosis. 2016;248:2–9. doi: 10.1016/j.atherosclerosis.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Luo JY, et al. Prevalence, awareness, treatment and control of dyslipidemia among adults in northwestern China: the cardiovascular risk survey. Lipids in health and disease. 2014;13:4. doi: 10.1186/1476-511X-13-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang Y, Gao L, Xie X, Tan SC. Epidemiology of dyslipidemia in Chinese adults: meta-analysis of prevalence, awareness, treatment, and control. Population health metrics. 2014;12:28. doi: 10.1186/s12963-014-0028-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang S, et al. Prevalence and associated factors of dyslipidemia in the adult Chinese population. PloS one. 2011;6:e17326. doi: 10.1371/journal.pone.0017326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun GZ, et al. High prevalence of dyslipidemia and associated risk factors among rural Chinese adults. Lipids in health and disease. 2014;13:189. doi: 10.1186/1476-511X-13-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang KJ, Makond B, Wang KM. Modeling and predicting the occurrence of brain metastasis from lung cancer by Bayesian network: a case study of Taiwan. Computers in biology and medicine. 2014;47:147–160. doi: 10.1016/j.compbiomed.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 13.Mancini F, et al. Classification of postural profiles among mouth-breathing children by learning vector quantization. Methods of information in medicine. 2011;50:349–357. doi: 10.3414/ME09-01-0039. [DOI] [PubMed] [Google Scholar]
- 14.Wei Z, et al. Application of Bayesian network model based on Tabu Search Algorithm in the analysis of influencing factors of coronary heart disease. Chinese Journal of Epidemiology. 2016;37:895–899. doi: 10.3760/cma.j.issn.0254-6450.2016.06.031. [DOI] [PubMed] [Google Scholar]
- 15.Kaewprag P, et al. Predictive models for pressure ulcers from intensive care unit electronic health records using Bayesian networks. BMC medical informatics and decision making. 2017;17:65. doi: 10.1186/s12911-017-0471-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hughes RE. Using a Bayesian Network to Predict L5/S1 Spinal Compression Force from Posture, Hand Load, Anthropometry, and Disc Injury Status. Applied bionics and biomechanics. 2017;2017:2014961. doi: 10.1155/2017/2014961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Satya Eswari J, Kavya K. Optimal feed profile for the Rhamnolipid kinetic models by using Tabu search: metabolic view point. AMB Express. 2016;6:116. doi: 10.1186/s13568-016-0279-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qi L, et al. Prevalence and Risk Factors Associated with Dyslipidemia in Chongqing, China. International journal of environmental research and public health. 2015;12:13455–13465. doi: 10.3390/ijerph121013455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Janus ED, et al. Dyslipidaemia in rural Australia: prevalence, awareness, and adherence to treatment guidelines in the Greater Green Triangle Risk Factor Study. The Medical journal of Australia. 2010;192:127–132. doi: 10.5694/j.1326-5377.2010.tb03449.x. [DOI] [PubMed] [Google Scholar]
- 20.Ni WQ, et al. Serum lipids and associated factors of dyslipidemia in the adult population in Shenzhen. Lipids in health and disease. 2015;14:71. doi: 10.1186/s12944-015-0073-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cai L, Liu A, Zhang L, Li S, Wang P. Prevalence, awareness, treatment, and control of hypertension among adults in Beijing, China. Clinical and experimental hypertension. 2012;34:45–52. doi: 10.3109/10641963.2011.618206. [DOI] [PubMed] [Google Scholar]
- 22.Sun Z, et al. Prevalence of prehypertension, hypertension and, associated risk factors in Mongolian and Han Chinese populations in Northeast China. International journal of cardiology. 2008;128:250–254. doi: 10.1016/j.ijcard.2007.08.127. [DOI] [PubMed] [Google Scholar]
- 23.Deeter A, Dalman M, Haddad J, Duan ZH. Inferring gene and protein interactions using PubMed citations and consensus Bayesian networks. PloS one. 2017;12:e0186004. doi: 10.1371/journal.pone.0186004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sperotto A, Molina JL, Torresan S, Critto A, Marcomini A. Reviewing Bayesian Networks potentials for climate change impacts assessment and management: A multi-risk perspective. Journal of environmental management. 2017;202:320–331. doi: 10.1016/j.jenvman.2017.07.044. [DOI] [PubMed] [Google Scholar]
- 25.Rathnam C, Lee S, Jiang X. An algorithm for direct causal learning of influences on patient outcomes. Artificial intelligence in medicine. 2017;75:1–15. doi: 10.1016/j.artmed.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hall DC, Le QB. Use of Bayesian networks in predicting contamination of drinking water with E. coli in rural Vietnam. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2017;111:270–277. doi: 10.1093/trstmh/trx043. [DOI] [PubMed] [Google Scholar]
- 27.Shim Y, Chen S, Sengupta A, Roy K. Stochastic Spin-Orbit Torque Devices as Elements for Bayesian Inference. Scientific reports. 2017;7:14101. doi: 10.1038/s41598-017-14240-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garcia-Herrero S, Mariscal MA, Gutierrez JM, Ritzel DO. Using Bayesian networks to analyze occupational stress caused by work demands: preventing stress through social support. Accident; analysis and prevention. 2013;57:114–123. doi: 10.1016/j.aap.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 29.Liao Y, Xu B, Wang J, Liu X. A new method for assessing the risk of infectious disease outbreak. Scientific reports. 2017;7:40084. doi: 10.1038/srep40084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Myte R, et al. Untangling the role of one-carbon metabolism in colorectal cancer risk: a comprehensive Bayesian network analysis. Scientific reports. 2017;7:43434. doi: 10.1038/srep43434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu, S. et al. Cognition, quality-of-life and symptom clusters in breast cancer: using Bayesian networks to elucidate complex relationships. Psycho-oncology, 10.1002/pon.4571 (2017). [DOI] [PMC free article] [PubMed]
- 32.Marvin HJP, et al. A holistic approach to food safety risks: Food fraud as an example. Food research international. 2016;89:463–470. doi: 10.1016/j.foodres.2016.08.028. [DOI] [PubMed] [Google Scholar]
- 33.Kumar BS, Venkateswarlu C. Inverse modeling approach for evaluation of kinetic parameters of a biofilm reactor using tabu search. Water environment research: a research publication of the Water Environment Federation. 2014;86:675–686. doi: 10.2175/106143014X13975035525708. [DOI] [PubMed] [Google Scholar]
- 34.Hu M, et al. Prevalence, awareness, treatment, and control of hypertension and associated risk factors among adults in Xi’an, China: A cross-sectional study. Medicine. 2016;95:e4709. doi: 10.1097/MD.0000000000004709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rao H, et al. The higher prevalence of truncal obesity and diabetes in American than Chinese patients with chronic hepatitis C might contribute to more rapid progression to advanced liver disease. Alimentary pharmacology & therapeutics. 2017;46:731–740. doi: 10.1111/apt.14273. [DOI] [PubMed] [Google Scholar]
- 36.Liu X, et al. Prevalence, awareness, treatment, control of type 2 diabetes mellitus and risk factors in Chinese rural population: the RuralDiab study. Scientific reports. 2016;6:31426. doi: 10.1038/srep31426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huang X, et al. Prevalence, awareness, treatment, and control of hypertension among China’s Sichuan Tibetan population: A cross-sectional study. Clinical and experimental hypertension. 2016;38:457–463. doi: 10.3109/10641963.2016.1163369. [DOI] [PubMed] [Google Scholar]
- 38.Tian Q, Hou F, liu X, Wang L. Resting state normal heart rate range of healthy people in Anyang Steel Corp. Chinese Journal of Tissue Engineering. 2005;9:13–15. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in its Supplementary Information files.