Abstract
This study was carried out to look for diagnostic and prognostic role of neutrophil gelatinase-associated lipocalin (NGAL) in early diabetic nephropathy (DN) in type 2 diabetes individuals. NGAL was measured in both urinary and serum sample of 144 type 2 diabetes individuals stratified into three categories based on urinary albumin-creatinine ratio and 54 control populations with estimated glomerular filtration rate >60 mL/min/1.73 m2 and serum creatinine <1.2 mg/dl. The serum NGAL (sNGAL), urine NGAL (uNGAL), and uNGAL/urine creatinine were significantly higher in diabetic individuals than in the control populations with significant difference in between the groups (P < 0.05). Difference of above values between control value and normoalbuminuria was also statistically significant (P < 0.05). Again, sNGAL and uNGAL correlate positively with albuminuria (P < 0.05). Tubular injury may precede glomerular injury in diabetic individuals, and NGAL can be used as a biomarker to diagnose DN even earlier to incipient nephropathy. Both sNGAL and uNGAL can predict albuminuria and be used as a noninvasive tool for diagnosis, staging, and progression of DN.
Keywords: Diabetic kidney disease, early predictor, neutrophil gelatinase-associated lipocalin, type 2 diabetes
Introduction
Diabetic nephropathy (DN) is a major microvascular complication of diabetes mellitus, accounting 20%–40% of populations requiring renal replacement therapy.[1,2] Pathologically, it is a diffuse process involving glomerular endothelial cells, tubular epithelial cells, and interstitium. It evolves through glomerular hyperfiltration, silent phase (normoalbuminuria), incipient nephropathy (microalbuminuria), overt nephropathy (macroalbuminuria), and established renal failure.[3] Whether tubular epithelial and interstitial injury in diabetics is primary, that precedes glomerular endothelial injury or secondary to albuminuria, is a subject of debate.[4] Chronological age of appearances of glomerular basement membrane and tubular basement membrane thickening on histopathology of type 1 diabetes suggests that tubular injury is independent of glomerular injury as both appears after similar duration of disease.[5,6] As with other renal diseases, outcome of diabetic kidney disease (DKD) is better determined by tubulointerstitial changes than glomerular changes.[7,8,9] Classically, albuminuria, which is considered as a hallmark of DN, is a marker of glomerular injury (glomerular phase). However, Pun et al. in 1990 and later by many other researchers suggested that tubular injury can occur even at stage that precedes microalbuminuria (tubular phase).[10,11] Low Vitamin-D and erythropoietin in normoalbuminuric diabetic patients imply early involvement of tubulointerstitial component rather than glomerular.[12]
Chronic hyperglycemia leads to increased production of oxidative free radicals, advanced glycosylated end-products,[13] vasoactive amines (angiotensin-II), and cytokines (transforming growth factor-β), which result in functional followed by structural damage to tubulointerstitium.[8,9] Functional damage reflected as tubular hypertrophy due to increased absorption of glucose,[14] dysfunction of transporter proteins such as megalin and cubilin,[15] and defective activity of lysosomal system that leads to increased excretion of protein which can serve as biomarker to diagnose while glomerular function is still normal. Hence, now, investigators are in search of ideal biomarkers to identify DN in the stage of functional damage so that measures can be taken to prevent the progression or retard the disease process.
Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker of renal tubular injury, upregulated in distal tubules and collecting duct, is extensively evaluated for acute kidney injury (AKI).[16] It is a 25 kDa glycoprotein with 178 amino acid belonging to lipocalin superfamily.[17] It is a constituent of specific granules and exists in neutrophil as a part of NGAL-gelatinase complex.[18] It is involved in antimicrobial defense mechanism and upregulated in systemic bacterial infection.[17,18,19,20] It plays a protective role in epithelial injury by its anti-apoptosis effect.[21] As it is not produced by burnt out nephron, it is supposed to be a marker of active injury and represents mass of salvageable nephrons.[22] Its usefulness as a biomarker in chronic kidney disease (CKD) and later in DN has been suggested by Bolignano et al.[23,24] Other than renal parenchyma disease, heart failure, endothelial dysfunction, preeclampsia, infection, inflammation, and malignancy are associated with increase in NGAL level independent of glomerular filtration rate (GFR).[17,25,26,27,28,29]
In our current study, we aimed to compare markers of glomerular injury (urinary albumin) with that of tubular injury (NGAL), in a subset of type 2 diabetics mellitus (T2DM) those never been exposed to angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) and to establish diagnostic role of the later in nonalbuminuric DN. This is to avoid bias as ACEIs or ARBs known to reduce albuminuria and tubular biomarkers.[30] Again, there is no study based on Indian population to decide diagnostic accuracy of NGAL in diabetic populations.
Materials and Methods
Patients’ selection
This was a prospective, single-center, nonrandomized controlled trial conducted at Sanjay Gandhi Postgraduate Institute of Medical Sciences (SGPGI), Lucknow, India, between June 2014 and December 2015. The study was carried out to look for diagnostic and prognostic role of NGAL in early DN. Only willing patients with T2DM presented to Outpatient Department of Nephrology and Endocrinology were included in this study. Enrolled patients satisfied following inclusion criteria: age between 18 and 60 years, estimated GFR (eGFR) (CKD-epidemiology collaboration [EPI]) >60 mL/min/1.73 m2, and serum creatinine <1.2 mg/dl with stable renal function for at least 1 year (i.e., variation <0.3 mg% from baseline serum creatinine). Patients with a history of usage of renin–angiotensin system inhibitors were strictly excluded from the study. In addition, those with infection; inflammatory disorders; uncontrolled hypertension; history of usage of nonsteroidal anti-inflammatory drug (NSAID), nephrotoxic medications, or immunosuppressant; history of non-DKD; history of coronary artery disease (CAD), stroke, or peripheral vascular disease; malignancy; thyroid disorders; liver dysfunction; and pregnancy were also excluded from the study. All included patients were on diabetic diet without protein restriction and had stable blood pressure and glycemic control for at least for 30 days. They were stratified into three groups based on urinary albumin-creatinine ratio (UACR)– normoalbuminuria (<30 mg/g creatinine), microalbuminuria (30–299 mg/g creatinine), and macroalbuminuria (≥300 mg/g creatinine).
Age- and gender-matched nondiabetic healthy controls were selected randomly from the voluntary kidney donor registry with eGFR >60 mL/min/1.73 m2; and those with history of hypertension (JNC7); dyslipidemia; infections; inflammations; usage of NSAID or nephrotoxic agents; malignancy; renal, pulmonary, cardiovascular, and endocrine disorders were excluded.
This study was approved by the Institutional Ethics Committee, SGPGI, and prior informed consents were obtained from all study subjects.
Measurements
Spot urine (clean-catch midstream urine sample) and fasting blood samples were obtained between 8 and 11 AM. During the same visit, medical history, systolic blood pressure (SBP), diastolic blood pressure (DBP), and body mass index (BMI) were recorded. Blood was centrifuged; serum separated and was stored at −80°C until final analyses were carried out. Similarly, urine was centrifuged and stored at −80°C. uNGAL and sNGAL (catalog #DY1757) were measured using sandwich enzyme linked immunosorbent assay (ELISA, R&D Systems, Inc., USA and Canada). The uNGAL was expressed in absolute value (ng/ml) and also normalized to the urinary creatinine concentration (ng/mg), whereas the sNGAL was expressed in absolute value (ng/ml). The lower detection limit of the assay was 78.1 pg/ml for NGAL. Urinary albumin was measured using a solid phase, sandwich-format, immunometric assay (Alere Technologies AS, Norway) and was expressed as ACR (mcg/mg). The eGFR was calculated using the CKD-EPI equations and expressed in ml/min/1.73 m2. Glycated hemoglobin (HbA1c), creatinine (Jaffe rate-reaction method), albumin, and lipid profile were determined from venous blood sample. Manufacturers’ protocol was followed for all test procedures.
Statistical analysis
Normality of the continuous variables was examined using Kolmogorov–Smirnov test. Data were presented in mean ± standard deviation for normally distributed variables and median (interquartile range) for nonnormal variables. One-way ANOVA/Kruskal–Wallis H-test was used to compare the independent groups. In case P < 0.05 was found statistically significant, post hoc test (multiple comparisons) was used to identify the significant pairs. Categorical variables were reported in frequency and percentage. Pearson's Chi-square test/Fisher's exact test was employed to analyze categorical data as appropriate. Binary logistic regression analysis used to identify the significant predictors of the outcome. All the individual predictors those found significant in univariate analysis were included in multivariate analysis. Area under the curve (AUC) used to identify the best cutoff value of normoalbuminuric DN in terms of their sensitivity and specificity. A P < 0.05 was considered as statistically significant. Statistical Package for Social Sciences version 17 (SPSS 17, IBM, Chicago, IL, USA) was used for statistical analyses.
Results
Comparison of baseline characteristics among different groups
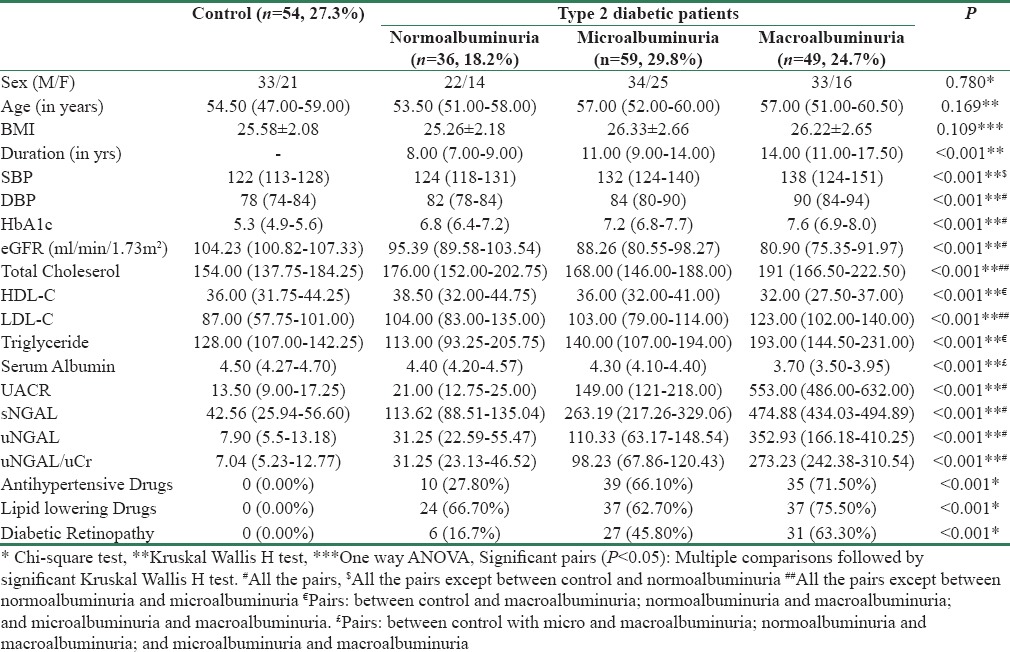
Table 1 shows comparison of baseline characteristics between the study groups. Of 198 study participants, there were 36 normoalbuminuric, 59 microalbuminuric, 49 macroalbuminuric, and 54 control populations. In the baseline characteristics among the four groups, there was no significant difference in the distribution of sex, age, and BMI while significant difference in regard to duration of disease, SBP, DBP, HbA1c, eGFR, total cholesterol (TCH), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglyceride (TG), serum albumin, antihypertensive drugs (AHDs), lipid-lowering agents (LLAs), and diabetic retinopathy (DR). Duration of diabetes and HbA1c were progressively higher among normoalbuminuria, microalbuminuria, and macroalbuminuria while reverse was true for eGFR and HDL-C. There was no significant difference between the control and normoalbuminuria with respect to SBP. Difference between the normoalbuminuria and microalbuminuria groups with regard to TCH and LDL-C was also nonsignificant. Macroalbuminuria group had significantly low serum albumin and higher incidence of DR than other groups. Usage of AHDs and LLAs was more frequently observed in the macroalbuminuria group than in the normoalbuminuria and microalbuminuria groups.
Table 1.
Comparison of clinical characteristics among different groups
Comparison of serum neutrophil gelatinase-associated lipocalin and urine neutrophil gelatinase-associated lipocalin values according to albuminuria
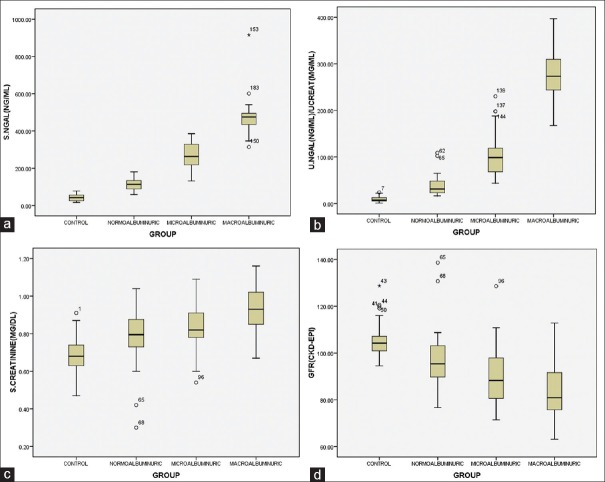
Table 1 and Figure 1 show comparisons in values of uNGAL, sNGAL, uNGAL/urine creatinine (uCr), and other markers among different groups. The sNGAL, uNGAL, and uNGAL/uCr were significantly higher in diabetic individual than in the control. Multiple comparisons indicated the significant difference in sNGAL, uNGAL, and uNGAL/uCr values between the groups (P < 0.05). Difference of above values between control value and normoalbuminuria was also significant (P < 0.05).
Figure 1.
Showing median value of various biomarkers and eGFR in different stage of diabetic nephropathy. (a) Serum NGAL (ng/ml), (b) Urine NGAL/urine creatinine –(ng/mg), (c) Serum creatinine (mg/dl) and (d) GFR (ml/min/1.73m2)
Associations of albuminuria with serum and urinary markers in type 2 diabetic patients
Spearman's rank correlation coefficient (rho; ρ) was calculated between the various serum and urinary marker with each other. The sNGAL showed good (P < 0.05) positive correlation with UACR (ρ = 0.92), uNGAL (ρ = 0.77), uNGAL/uCr (ρ = 0.93). Similarly, uNGAL and uNGAL/uCr showed good (P < 0.05) positive correlation with UACR (ρ = 0.0.77, 0.88) and sNGAL (ρ = 0.77, 0.93).
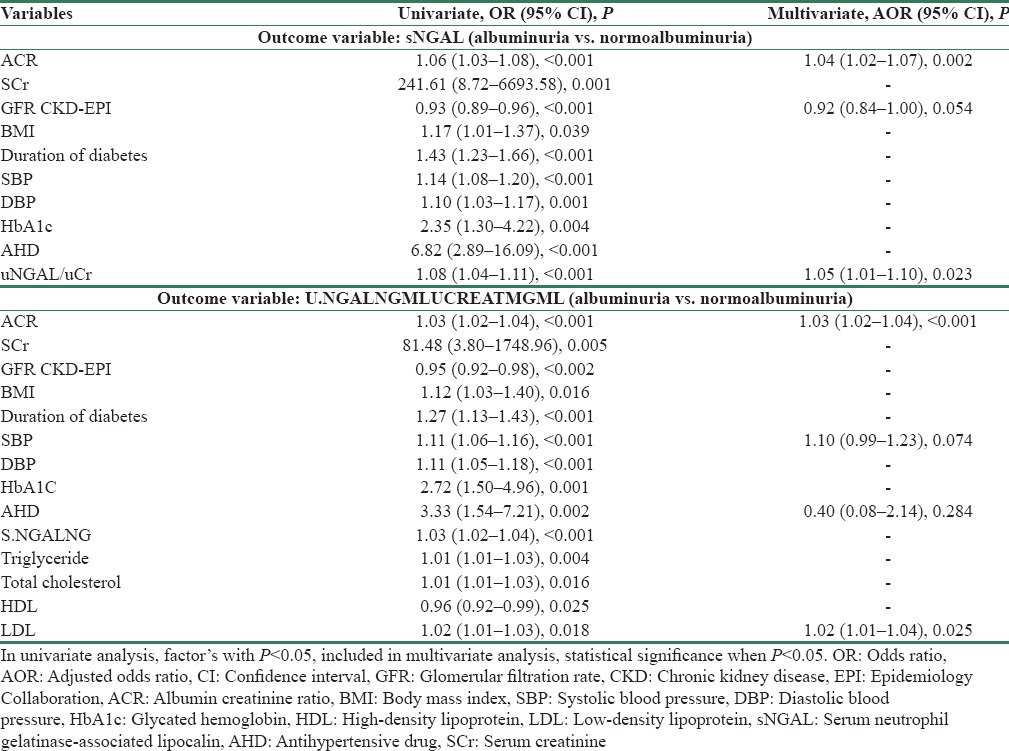
Univariate binary logistic regression analysis showed that predictors, i.e., ACR, serum creatinine, GFR, BMI, duration of diabetes, SBP, DBP, HbA1c, AHD, and uNGAL/uCr, were found individually significant with sNGAL (P < 0.05). In the multivariate analysis, variables included were ACR (adjusted odds ratio [AOR] = 1.04, 95% confidence interval [CI] = 1.02–1.07, P = 0.002), GFR (AOR = 0.92, 95% CI = 0.84–1.00, P = 0.054), and uNGAL/uCr (AOR = 1.05, 95% CI = 1.01–1.10, P = 0.023). Similarly, univariate analysis, for uNGAL/uCr, predictors, i.e., ACR, serum creatinine, GFR, BMI, duration of diabetes, SBP, DBP, HbA1c, AHD, sNGAL, TG, TCH, HDL, and LDL, were found individually significant (P < 0.05), but in the multivariate model, variables included were ACR (AOR = 1.03, 95% CI = 1.02–1.04, P < 0.001), SBP (AOR = 1.10, 95% CI = 0.99–1.23, P = 0.074), AHD (AOR = 0.40, 95% CI = 0.08–2.14, P = 0.284), and LDL (AOR = 1.02, 95% CI = 1.01–1.04, P = 0.025) [Table 2].
Table 2.
Univariate and multivariate binary logistic regression analysis
Receiver operating characteristics curve analysis of serum neutrophil gelatinase-associated lipocalin, urine neutrophil gelatinase-associated lipocalin, urine neutrophil gelatinase-associated lipocalin/urine creatinine, and urinary albumin-creatinine ratio
Receiver operating characteristics (ROC) curve analyses were performed to define the diagnostic value of sNGAL, uNGAL, uNGAL/uCr, and UACR in identifying DN with or without proteinuria [Table 3 and Figure 2]. The uNGAL showed a very good diagnostic profile, describing an AUC of 0.996 (95% CI: 0.991–1.000, P < 0.001) with a best cutoff value of 21.31 ng/ml (sensitivity 95.1%; specificity 100%). This is followed by sNGAL, showing an AUC of 0.993 (95% CI: 0.998–1.000, P < 0.001) and a best cutoff value of 78.73 ng/ml (sensitivity 95.1%; specificity 100.0%) [Table 3]. Similarly, uNGAL/uCr had a good diagnostic profile, showing an AUC of 0.996 (95% CI: 0.992–1.00, P < 0.001) and a best cutoff value of 24.96 ng/g (sensitivity 93.1%; specificity 100.0%). UACR had least diagnostic profile among four with an AUC of 0.926 (95% CI: 0.89–0.96, P < 0.001) and a best cutoff value of 29.5 mg/g (sensitivity 75.5%; specificity 100.0%).
Table 3.
Receiver operating characteristics curve analysis of serum neutrophil gelatinase-associated lipocalin, urine neutrophil gelatinase-associated lipocalin, urine neutrophil gelatinase-associated lipocalin/urine creatinine and urinary albumin-creatinine ratio

Figure 2.

Receiver operating characteristics curve analysis of serum neutrophil gelatinase-associated lipocalin, urine neutrophil gelatinase-associated lipocalin, urine neutrophil gelatinase-associated lipocalin/urine creatinine, and urinary albumin-creatinine ratio
Discussion
Diabetics are continuously exposed to metabolic and hemodynamic stress. Metabolic stress is related to hyperglycemia and hyperlipidemia. Hemodynamic stress includes hypertension. Hyperglycemia, hyperlipidemia, and hypertension together lead to inflammation and atherosclerosis resulting endothelial dysfunction and tubulointerstitial damage. While tubular damage leads to increase in tubular biomarkers, endothelial dysfunction progresses to albuminuria. In 1993, Yaqoob et al. concluded that endothelial dysfunction and tubular injury may precede microalbuminuria.[31] Hence, even diabetics with preserved eGFR are at increased risk for AKI in comparison to healthy individuals, indicating decreased renal reserve. Hence, several tubular markers such as NGAL, KIM-1, NAG, MCP, and urinary liver-type fatty acid-binding protein (uLFABP) may act as clinical indicators of onset and progression of DN.[32]
In our study, we observed sNGAL and uNGAL values across nondiabetic control and three groups of diabetics with normal serum creatinine – normoalbuminuria, microalbuminuria, and macroalbuminuria. There was significant difference in median value of sNGAL and uNGAL between diabetes patients compared to well-matched control, suggesting that NGAL can be a useful marker of onset of DN even when serum creatinine is normal range. This may be due to protective response of NGAL in response to metabolic and hemodynamic stress. Intergroup comparison among three groups of T2DM patients shows that difference was significant with highest median value in macroalbuminuria and lowest in normoalbuminuria, which suggest that sNGAL and uNGAL can be used to predict progression of DN. Again, sNGAL and uNGAL correlates positively with albuminuria suggesting that former correlates with severity of renal involvement. This concludes that NGAL can be used as a marker to stratify diabetes nephropathy into different stages.
Results obtained above were in agreement with previous studies which reported similar tendency for NGAL[33] and other biomarkers of tubular injury such as NAG, MCP, uLFABP, and KIM-1 whose level corresponds with degree of proteinuria[24,34,35,36,37] but contradicted by Kim et al., where there were no significant differences in NGAL value between normoalbuminuria and microalbuminuria groups.[38]
Normoalbuminuric diabetes patients had significantly higher median sNGAL and uNGAL value than control group, suggesting that tubular injury may precede glomerular injury and NGAL can serve as an early laboratory marker of DN, supporting the previous study.[24,32,37,39,40,41] This also suggested that tubular dysfunction in early DN is not secondary to albuminuria, but consequences of metabolic and hemodynamic stress are associated with chronic hyperglycemia contradicting previous hypothesis.[4,7,9] As NGAL is a marker of distal tubule injury, it is not going to be affected by albuminuria or proteinuria, which again supports our earlier hypothesis that tubular injury may precede glomerular injury.[36] Markers of tubular injury predicting onset of albuminuria and progression of disease have been observed in various other studies using other biomarkers such as uLFABP, KIM-1.[30,32,42] In 2012, Kim et al. suggested in their trial that differences in NGAL value between control, normoalbuminuria, and microalbuminuria were nonsignificant, contradicting NGAL as an early marker of DN.[38]
In our study, sNGAL, uNGAL, and uNGAL/uCr show strong positive correlation with one another and that with albuminuria and duration of DM but negative correlation with eGFR which is supported by other study also.[33,37,40,43] However, in multivariate binary logistic regression, only UACR and uNGAL/uCr were predictors of sNGAL whereas UACR and LDL-C were predictors of uNGAL/uCr. A strong correlation between NGAL and albuminuria suggests glomerular and tubular injury may occur as parallel processes. Lacquaniti et al. and Zachwieja et al. in their studies found no correlation between sNGAL and uNGAL. They also found no correlation NGAL with renal function such as eGFR and creatinine.[39,41] Bolignano et al., Zachwieja et al., and Fathimah et al. concluded that NGAL value does not correlate with glycemic control (HbA1c) which is supported by our study but contradicted to the study by Lacquaniti et al.[24,33,37,39,41] Nauta et al. concluded that it is not NGAL but uLFABP that predicts decline in renal function (eGFR) in diabetic individuals, whereas Nielsen et al. suggested that none of the tubular markers can predict decrease in renal function (true GFR-51Cr-EDTA).[36,44]
Advantage of our study is that we have included patients with better control of blood sugar and blood pressure; normal serum creatinine and GFR >60 ml/min/1.73 m2. As NGAL might be elevated in nonrenal causes, we have excluded those with cardiac dysfunction and malignancy. On the contrary to other study, we have excluded those who are already on ACEI and/or ARB as protective role of both of them on glomerular and tubulointerstitial compartments has already been proved in both animal and human study.[30,44,45] Some trials conducted also showed protecting role of ACEI and/or ARB in DN using NGAL as a marker.
Major limitation of our project was small sample size, single-center study with cross-sectional design. Small sample size is probably related to strict criteria of excluding those who are already on ACEI or ARBs. Other than DN, AKI, infection, inflammation, and malignancy are responsible for raise sNGAL and uNGAL value suspecting specificity of NGAL as diagnostic marker of DN. Elevated circulating NGAL could also be due to endothelial dysfunction of glomerular capillaries or extra-renal blood vessels.[26] As diabetes is a metabolic disease affecting multisystem and endothelium of blood vessel is main target organ, extra-renal source of NGAL due to endothelial dysfunction leading to elevated circulating NGAL cannot be ruled. Again, high uNGAL could be the consequences of elevated circulating NGAL. Hence, along with NGAL, we should use other marker of tubular injury for better assessment of renal function. We can interpret our limitation in better way that NGAL, particularly sNGAL, can be marker of endothelial dysfunction that can be predictor of microvascular and macrovascular complication in diabetes individuals in early stage. Other limitation of our study was that we did not collect 24 h sample which was due to technical infeasibility to collect sample.
Conclusion
Tubular injury may precede glomerular injury in diabetic patients, and NGAL can be used as biomarker to diagnosed DN even earlier to incipient nephropathy. Both sNGAL and uNGAL can predict albuminuria and be used as a noninvasive tool for diagnosis, staging, and progression of DN.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Atkins RC. The epidemiology of chronic kidney disease. Kidney Int Suppl. 2005;94:S14–8. doi: 10.1111/j.1523-1755.2005.09403.x. [DOI] [PubMed] [Google Scholar]
- 2.Ghaderian SB, Hayati F, Shayanpour S, BeladiMousavi SS. Diabetes and end-stage renal disease; a review article on new concepts. J Renal Inj Prev. 2015;4:28–33. doi: 10.12861/jrip.2015.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mogensen CE, Christensen CK, Vittinghus E. The stages in diabetic renal disease. With emphasis on the stage of incipient diabetic nephropathy. Diabetes. 1983;32(Suppl 2):64–78. doi: 10.2337/diab.32.2.s64. [DOI] [PubMed] [Google Scholar]
- 4.Abbate M, Zoja C, Remuzzi G. How does proteinuria cause progressive renal damage? J Am Soc Nephrol. 2006;17:2974–84. doi: 10.1681/ASN.2006040377. [DOI] [PubMed] [Google Scholar]
- 5.Brito PL, Fioretto P, Drummond K, Kim Y, Steffes MW, Basgen JM, et al. Proximal tubular basement membrane width in insulin-dependent diabetes mellitus. Kidney Int. 1998;53:754–61. doi: 10.1046/j.1523-1755.1998.00809.x. [DOI] [PubMed] [Google Scholar]
- 6.Tyagi I, Agrawal U, Amitabh V, Jain AK, Saxena S. Thickness of glomerular and tubular basement membranes in preclinical and clinical stages of diabetic nephropathy. Indian J Nephrol. 2008;18:64–9. doi: 10.4103/0971-4065.42336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Phillips AO, Steadman R. Diabetic nephropathy: The central role of renal proximal tubular cells in tubulointerstitial injury. Histol Histopathol. 2002;17:247–52. doi: 10.14670/HH-17.247. [DOI] [PubMed] [Google Scholar]
- 8.Gilbert RE, Cooper ME. The tubulointerstitium in progressive diabetic kidney disease: More than an aftermath of glomerular injury? Kidney Int. 1999;56:1627–37. doi: 10.1046/j.1523-1755.1999.00721.x. [DOI] [PubMed] [Google Scholar]
- 9.Phillips AO. The role of renal proximal tubular cells in diabetic nephropathy. Curr Diab Rep. 2003;3:491–6. doi: 10.1007/s11892-003-0013-1. [DOI] [PubMed] [Google Scholar]
- 10.Kern EF, Erhard P, Sun W, Genuth S, Weiss MF. Early urinary markers of diabetic kidney disease: A nested case-control study from the Diabetes Control and Complications Trial (DCCT) Am J Kidney Dis. 2010;55:824–34. doi: 10.1053/j.ajkd.2009.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pun KK, Ho P, Lau P, Wong FH. Eight-month longitudinal study of urinary excretion of albumin and tubular proteins in diabetic subjects. Am J Nephrol. 1990;10:475–81. doi: 10.1159/000168172. [DOI] [PubMed] [Google Scholar]
- 12.Singh DK, Winocour P, Summerhayes B, Viljoen A, Sivakumar G, Farrington K. Are low erythropoietin and 1,25-dihydroxyvitamin D levels indicative of tubulo-interstitial dysfunction in diabetes without persistent microalbuminuria? Diabetes Res Clin Pract. 2009;85:258–64. doi: 10.1016/j.diabres.2009.06.022. [DOI] [PubMed] [Google Scholar]
- 13.Simm A, Münch G, Seif F, Schenk O, Heidland A, Richter H, et al. Advanced glycation endproducts stimulate the MAP-kinase pathway in tubulus cell line LLC-PK1. FEBS Lett. 1997;410:481–4. doi: 10.1016/s0014-5793(97)00644-3. [DOI] [PubMed] [Google Scholar]
- 14.Jones SC, Saunders HJ, Pollock CA. High glucose increases growth and collagen synthesis in cultured human tubulointerstitial cells. Diabet Med. 1999;16:932–8. doi: 10.1046/j.1464-5491.1999.00174.x. [DOI] [PubMed] [Google Scholar]
- 15.Thrailkill KM, Nimmo T, Bunn RC, Cockrell GE, Moreau CS, Mackintosh S, et al. Microalbuminuria in type 1 diabetes is associated with enhanced excretion of the endocytic multiligand receptors megalin and cubilin. Diabetes Care. 2009;32:1266–8. doi: 10.2337/dc09-0112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bonventre JV. Diagnosis of acute kidney injury: From classic parameters to new biomarkers. Contrib Nephrol. 2007;156:213–9. doi: 10.1159/000102086. [DOI] [PubMed] [Google Scholar]
- 17.Cowland JB, Borregaard N. Molecular characterization and pattern of tissue expression of the gene for neutrophil gelatinase-associated lipocalin from humans. Genomics. 1997;45:17–23. doi: 10.1006/geno.1997.4896. [DOI] [PubMed] [Google Scholar]
- 18.Borregaard N, Sehested M, Nielsen BS, Sengeløv H, Kjeldsen L. Biosynthesis of granule proteins in normal human bone marrow cells. Gelatinase is a marker of terminal neutrophil differentiation. Blood. 1995;85:812–7. [PubMed] [Google Scholar]
- 19.Flo TH, Smith KD, Sato S, Rodriguez DJ, Holmes MA, Strong RK, et al. Lipocalin 2 mediates an innate immune response to bacterial infection by sequestrating iron. Nature. 2004;432:917–21. doi: 10.1038/nature03104. [DOI] [PubMed] [Google Scholar]
- 20.Venge P, Douhan-Håkansson L, Garwicz D, Peterson C, Xu S, Pauksen K. Human neutrophil lipocalin as a superior diagnostic means to distinguish between acute bacterial and viral infections. Clin Vaccine Immunol. 2015;22:1025–32. doi: 10.1128/CVI.00347-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mishra J, Mori K, Ma Q, Kelly C, Yang J, Mitsnefes M, et al. Amelioration of ischemic acute renal injury by neutrophil gelatinase-associated lipocalin. J Am Soc Nephrol. 2004;15:3073–82. doi: 10.1097/01.ASN.0000145013.44578.45. [DOI] [PubMed] [Google Scholar]
- 22.Mori K, Nakao K. Neutrophil gelatinase-associated lipocalin as the real-time indicator of active kidney damage. Kidney Int. 2007;71:967–70. doi: 10.1038/sj.ki.5002165. [DOI] [PubMed] [Google Scholar]
- 23.Bolignano D, Lacquaniti A, Coppolino G, Donato V, Campo S, Fazio MR, et al. Neutrophil gelatinase-associated lipocalin (NGAL) and progression of chronic kidney disease. Clin J Am Soc Nephrol. 2009;4:337–44. doi: 10.2215/CJN.03530708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bolignano D, Lacquaniti A, Coppolino G, Donato V, Fazio MR, Nicocia G, et al. Neutrophil gelatinase-associated lipocalin as an early biomarker of nephropathy in diabetic patients. Kidney Blood Press Res. 2009;32:91–8. doi: 10.1159/000209379. [DOI] [PubMed] [Google Scholar]
- 25.Damman K, Van Veldhuisen DJ, Navis G, Vaidya VS, Smilde TD, Westenbrink BD, et al. Tubular damage in chronic systolic heart failure is associated with reduced survival independent of glomerular filtration rate. Heart. 2010;96:1297–302. doi: 10.1136/hrt.2010.194878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.D’Anna R, Santamaria A, Interdonato ML, Licata G, Giordano D. L9. NGAL, an early marker of endothelial dysfunction in preeclampsia. Pregnancy Hypertens. 2011;1:243. doi: 10.1016/j.preghy.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 27.Kim SM, Park JS, Norwitz ER, Jung HJ, Kim BJ, Park CW, et al. Circulating levels of neutrophil gelatinase-associated lipocalin (NGAL) correlate with the presence and severity of preeclampsia. Reprod Sci. 2013;20:1083–9. doi: 10.1177/1933719113477480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Petla LT, Chikkala R, Ratnakar KS, Kodati V, Sritharan V. Biomarkers for the management of pre-eclampsia in pregnant women. Indian J Med Res. 2013;138:60–7. [PMC free article] [PubMed] [Google Scholar]
- 29.Nielsen BS, Borregaard N, Bundgaard JR, Timshel S, Sehested M, Kjeldsen L. Induction of NGAL synthesis in epithelial cells of human colorectal neoplasia and inflammatory bowel diseases. Gut. 1996;38:414–20. doi: 10.1136/gut.38.3.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nielsen SE, Sugaya T, Tarnow L, Lajer M, Schjoedt KJ, Astrup AS, et al. Tubular and glomerular injury in diabetes and the impact of ACE inhibition. Diabetes Care. 2009;32:1684–8. doi: 10.2337/dc09-0429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yaqoob M, Patrick AW, McClelland P, Stevenson A, Mason H, White MC, et al. Relationship between markers of endothelial dysfunction, oxidant injury and tubular damage in patients with insulin-dependent diabetes mellitus. Clin Sci (Lond) 1993;85:557–62. doi: 10.1042/cs0850557. [DOI] [PubMed] [Google Scholar]
- 32.Nielsen SE, Schjoedt KJ, Astrup AS, Tarnow L, Lajer M, Hansen PR, et al. Neutrophil gelatinase-associated lipocalin (NGAL) and kidney injury molecule 1 (KIM1) in patients with diabetic nephropathy: A cross-sectional study and the effects of lisinopril. Diabet Med. 2010;27:1144–50. doi: 10.1111/j.1464-5491.2010.03083.x. [DOI] [PubMed] [Google Scholar]
- 33.Fathimah M, Alicezah MK, Thevarajah M. Neutrophil gelatinase-associated lipocalin (NGAL): An early marker for diabetic nephropathy. Int J Diabetes Dev Ctries. 2012;32:19–24. [Google Scholar]
- 34.Morii T, Fujita H, Narita T, Shimotomai T, Fujishima H, Yoshioka N, et al. Association of monocyte chemoattractant protein-1 with renal tubular damage in diabetic nephropathy. J Diabetes Complications. 2003;17:11–5. doi: 10.1016/s1056-8727(02)00176-9. [DOI] [PubMed] [Google Scholar]
- 35.Panee J. Monocyte Chemoattractant Protein 1 (MCP-1) in obesity and diabetes. Cytokine. 2012;60:1–12. doi: 10.1016/j.cyto.2012.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nauta FL, Boertien WE, Bakker SJ, van Goor H, van Oeveren W, de Jong PE, et al. Glomerular and tubular damage markers are elevated in patients with diabetes. Diabetes Care. 2011;34:975–81. doi: 10.2337/dc10-1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Assal HS, Tawfeek S, Rasheed EA, El-Lebedy D, Thabet EH. Serum cystatin C and tubular urinary enzymes as biomarkers of renal dysfunction in type 2 diabetes mellitus. Clin Med Insights Endocrinol Diabetes. 2013;6:7–13. doi: 10.4137/CMED.S12633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim SS, Song SH, Kim IJ, Yang JY, Lee JG, Kwak IS, et al. Clinical implication of urinary tubular markers in the early stage of nephropathy with type 2 diabetic patients. Diabetes Res Clin Pract. 2012;97:251–7. doi: 10.1016/j.diabres.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 39.Lacquaniti A, Donato V, Pintaudi B, Di Vieste G, Chirico V, Buemi A, et al. “Normoalbuminuric” diabetic nephropathy: Tubular damage and NGAL. Acta Diabetol. 2013;50:935–42. doi: 10.1007/s00592-013-0485-7. [DOI] [PubMed] [Google Scholar]
- 40.Papadopoulou-Marketou N, Skevaki C, Kosteria I, Peppa M, Chrousos GP, Papassotiriou I, et al. NGAL and cystatin C: Two possible early markers of diabetic nephropathy in young patients with type 1 diabetes mellitus: One year follow up. Hormones (Athens) 2015;14:232–40. doi: 10.14310/horm.2002.1520. [DOI] [PubMed] [Google Scholar]
- 41.Zachwieja J, Soltysiak J, Fichna P, Lipkowska K, Stankiewicz W, Skowronska B, et al. Normal-range albuminuria does not exclude nephropathy in diabetic children. Pediatr Nephrol. 2010;25:1445–51. doi: 10.1007/s00467-010-1443-z. [DOI] [PubMed] [Google Scholar]
- 42.Nielsen SE, Sugaya T, Hovind P, Baba T, Parving HH, Rossing P. Urinary liver-type fatty acid-binding protein predicts progression to nephropathy in type 1 diabetic patients. Diabetes Care. 2010;33:1320–4. doi: 10.2337/dc09-2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wu J, Ding Y, Zhu C, Shao X, Xie X, Lu K, et al. Urinary TNF-a and NGAL are correlated with the progression of nephropathy in patients with type 2 diabetes. Exp Ther Med. 2013;6:1482–8. doi: 10.3892/etm.2013.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nielsen SE, Andersen S, Zdunek D, Hess G, Parving HH, Rossing P. Tubular markers do not predict the decline in glomerular filtration rate in type 1 diabetic patients with overt nephropathy. Kidney Int. 2011;79:1113–8. doi: 10.1038/ki.2010.554. [DOI] [PubMed] [Google Scholar]
- 45.Kelly DJ, Cox AJ, Tolcos M, Cooper ME, Wilkinson-Berka JL, Gilbert RE. Attenuation of tubular apoptosis by blockade of the renin-angiotensin system in diabetic Ren-2 rats. Kidney Int. 2002;61:31–9. doi: 10.1046/j.1523-1755.2002.00088.x. [DOI] [PubMed] [Google Scholar]