Abstract
BACKGROUND:
The Medical Council of India (MCI) has envisioned a change in the undergraduate medical curriculum by encouraging integrated teaching and Problem Based Learning (PBL).
METHODS:
In this cross-sectional study 110 medical teachers of Kasturba Medical College, Mangalore were assessed regarding their perception on PBL. Independent t-test was applied to find out the difference in the mean perception scores regarding PBL among the teachers in pre/para-clinical and clinical departments and P < 0.05 was considered statistically significant.
RESULTS:
PBL as a teaching method was preferred by 65.2% medical teachers. The teachers from clinical departments (Mean 4.1, SD 0.8) perceived PBL sessions to be more effective than the traditional methods than those from the pre-clinical and para clinical departments (Mean 3.7, SD 3.7) and this difference was found to be statistically significant. (P =0.028).
CONCLUSION:
PBL can complement integrated teaching and motivates students towards self-learning, and apply the learnt concepts of basic specialties to clinical problem solving.
Keywords: Medical education, medical teachers, problem-based learning, South India, undergraduate teaching
Introduction
Medical education focuses on training the medical students to have appropriate professional attitudes, acquire appropriate clinical skills and to prepare them to handle real-life situations. It should motivate students toward active, self-directed learning, rather than just being passive recipients of information in the classrooms.[1] The need for modifying the existing conventional method of undergraduate teaching in India has been recognized in recent years. Problem-based learning (PBL) is one such innovative approach to teaching that has international credibility.[2] PBL motivates students to frame learning objectives by identifying key areas or triggers from the clinical exercises provided to them which in turn encourages them to read and understand in depth. Learning by PBL method is not limited by any subject boundaries and promotes student-centered learning and concerted learning which are the hallmarks of PBL.[3,4] The Medical Council of India (MCI) has envisioned a change in the undergraduate medical curriculum by encouraging innovative teaching methods which aim to make the medical training more exciting and challenging to the students[5] and incorporating PBL into the curriculum seems to be the right path in this direction. However, the transition from the traditional didactic teaching to a role of a facilitator might be difficult for the most senior teachers. There is limited literature from India assessing the perceptions of teachers toward PBL and its inclusion into the existing curriculum. This cross-sectional study aimed to assess the perception of medical teachers regarding benefits and drawbacks of PBL.
Materials and Methods
Approval was obtained from the Institutional Ethics Committee of Kasturba Medical College, Mangalore (IEC/KMCMLR/2/2013). One hundred and ten medical teachers of Kasturba Medical College, Mangalore and its associated teaching hospitals were included in this cross-sectional study. Data were collected using an author designed questionnaire which was pilot tested on few teachers and was further modified based on their inputs. The teachers were chosen using nonrandom sampling. A written informed consent was obtained from those willing to participate in the study. Data collected was analyzed using SPSS (Statistical Package for Social Sciences, Chicago, IL, USA) version 11.5. Mean with the corresponding standard deviation (SD) and proportions were used to express the results. Perception of faculty toward PBL was assessed using a 5-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = not sure, 4 = agree, and 5 = strongly agree). Independent t-test was then applied to find out the difference in the mean perception scores regarding PBL among the medical teachers in pre/paraclinical and clinical departments. After applying Bonferroni corrections, P < 0.007 was considered to be a significant difference in perception scores regarding benefits of PBL among clinical and nonclinical teachers, and P < 0.008 was considered to be statistically significant difference in perception regarding drawbacks of PBL among the two groups.
Results
The mean (±SD) age of the teachers was 40.4 (±9.5) years. Medical teachers from the preclinical, para-clinical, and clinical specialties accounted for 24.5%, 29.1%, and 46.4% of the total participants, respectively. More than half (n = 65, 59.1%) of the medical teachers had a teaching experience of 10 years or less. The majority (n = 68, 61.8%) had prior exposure to PBL, with 35.5% of teachers having participated as a facilitator.
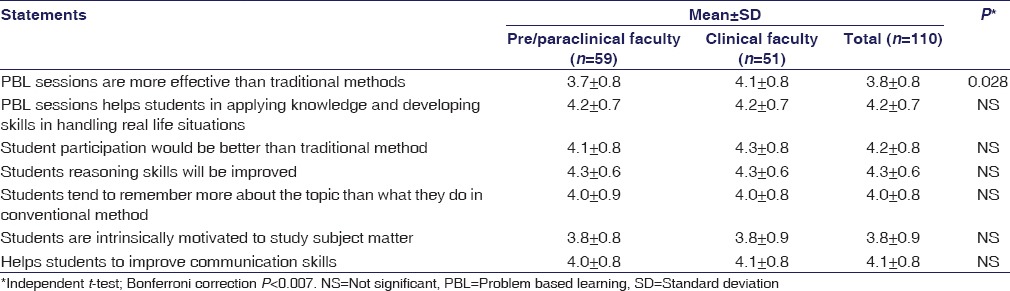
The differences in mean perception scores regarding benefits of PBL across the subgroups of medical teachers was assessed using the independent t-test. The teachers from clinical departments perceived PBL sessions to be more effective than the traditional methods (mean = 4.1, SD ± 0.8) than those from the preclinical and paraclinical departments (mean 3.7, SD ± 3.7) and this difference was found to be statistically significant (P = 0.028). Table 1 shows the comparison of perceived benefits of PBL among clinical and nonclinical faculties.
Table 1.
Perceived benefits of problem based learning among medical teachers from pre/para-clinical versus clinical departments (n=110)
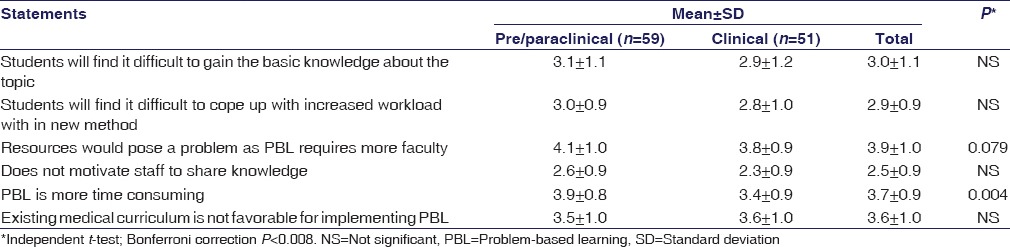
The comparison of perceived difficulties of PBL among clinical and nonclinical faculties is shown in Table 2. The pre/para clinical faculties perceived PBL as more time consuming (mean 3.9, SD ± 0.8) compared to clinical faculties (mean 3.4, SD ± 0.9) and this difference was found to be statistically significant (P = 0.004).
Table 2.
Perceived difficulties of problem-based learning among medical teachers from pre/paraclinical versus clinical departments (n=110)
Discussion
PBL has been incorporated in the medical curriculum with the objective of training medical students to focus their attention on patient needs rather than gathering mere theoretical knowledge.[6] However, the curriculum in the majority of the medical schools in India is handled in a customary class room gathering in the form of monotonous didactic lectures given subject wise and the outcome assessed on the basis of examination which tests a student's recall power rather than the knowledge he/she has gained. Most medical students consider the lectures and laboratory methods taught in basic sciences to be of no use in their clinical practice. Use of clinical case scenarios admixed with aspects of basic sciences in PBL exercises generates interest among students and motivates them to study basic sciences and its application in clinical practice making it more interesting.[7]
In this cross-sectional study, the majority of the medical teachers from various specialties were in favor of PBL as a method of teaching. Nearly one-fifth of these participants, however, preferred PBL in combination with the traditional method of teaching. This might be due to the great diversity of medical teachers, and hence, the method of teaching may depend on the topics taught. In a study from Bangladesh, a higher percentage of faculty members supported the inclusion of PBL in the undergraduate curriculum.[8] In another study from Canada[9] the faculty tutors involved in PBL sessions rated PBL higher than the traditional methods of teaching. In a study conducted in Hong Kong,[10] all the faculties were in favor of PBL since it matched with their philosophy of teaching and learning. In a study done in Pakistan,[11] 46.22% of the faculties were in favor of the implementation of PBL. Studies in the past have reported that PBL helps students in the application of basic sciences knowledge, to develop reasoning and problem-solving skills, self-directed learning, and promotion of teamwork.[12] The popularity of PBL as a favored teaching method is quite evident from our results as well as the above-mentioned studies. This can be attributed to the acceptance of newer technologies in learning by the students which compel the teachers to try innovative teaching methods.
In this study, the medical teachers perceived that PBL helps the students understand the topic easily and inculcates problem-solving skills among them. In a study done in Chennai among medical students, almost 50% of them agreed that PBL helps them to understand the concept and develop communication skills.[13] Similar observations were made in studies from Iran,[14] Malaysia,[15] and Pakistan[16] where the teachers found PBL to be more beneficial to the students when compared to the traditional method of teaching. It was observed in our study that the medical teachers with >10 years of teaching experience were more in favor of PBL. Comparable results were obtained in a study in Hong Kong[10] where 70% of the senior lecturers were in favor of PBL, who felt that it would help students learn effectively and develop critical thinking ability.
Teaching in between busy hospital schedule has always been a problem for clinicians, and PBL method of teaching has its time constraints. However, it was encouraging that half of the medical teachers from the clinical departments in our study were in favor of PBL. No significant differences existed between the medical teachers of clinical and nonclinical specialties in terms of perceived benefits of PBL among students and difficulties in implementation of PBL. The participants were of the opinion that the academic environment in the college favored implementation of PBL. This is further substantiated by the fact that in a study among medical students from the same setting reported PBL as the most preferred method by the students as they felt it enhanced lateral thinking.[17] The limitation of the study would be that it's a single center study with opinions of medical teachers from one institution which cannot be generalized. Similar studies from other medical colleges in India have to be conducted to generate an opinion of medical teachers toward PBL.
The MCI has envisioned a curriculum change with an emphasis on integrated teaching and self-learning.[5] PBL can complement this and motivate students toward self-learning and assist them in applying the concepts acquired from basic specialties in clinical problem-solving. In this direction, rather than a full-scale implementation of PBL in the curriculum it would be prudent to use a combination of traditional teaching methods with PBL which is especially required for nonclinical specialties to make it more interesting as well as to make the students understand the importance of these subjects in their clinical curriculum. However, for PBL to gain a strong foothold, medical teachers first need to be trained in this method and should develop a favorable attitude toward it and create a suitable academic environment for its implementation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Papinczak T, Young L, Groves M, Haynes M. An analysis of peer, self, and tutor assessment in problem-based learning tutorials. Med Teach. 2007;29:e122–32. doi: 10.1080/01421590701294323. [DOI] [PubMed] [Google Scholar]
- 2.Borhan MT. Problem Based Learning (PBL) in Malaysian higher education: A review of research on learners experience and issues of implementations. ASEAN J Eng Educ. 2012;1:48–53. [Google Scholar]
- 3.Distlehorst LH, Dawson E, Robbs RS, Barrows HS. Problem-based learning outcomes: The glass half-full. Acad Med. 2005;80:294–9. doi: 10.1097/00001888-200503000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Lewis AD, Menezes DA, McDermott HE, Hibbert LJ, Brennan SL, Ross EE, et al. Acomparison of course-related stressors in undergraduate problem-based learning (PBL) versus non-PBL medical programmes. BMC Med Educ. 2009;9:60. doi: 10.1186/1472-6920-9-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vision 2015 – Medical Council of India. [Last accessed on 2015 Dec 12]. Available from: http://www.mciindia.org/tools/announcement/MCI_booklet.pdf .
- 6.Adams K. Introducing problem based learning to third year B.Ed. Student their tutors. J Teach Educ. 2009;1:31, 45. [Google Scholar]
- 7.Shankar PR. Integrating subjects through problem-based learning: A South Asian perspective. [Last accessed on 2015 Dec 12];Med Educ. 2006 12:1–3. Available from: http://www.med-ed-online.org/pdf/l0000015.pdf . [Google Scholar]
- 8.Rahman ME, Rahman S, Musa KM, Shuvra MR. Knowledge and attitude of faculty members on problem based learning. Mymensingh Med J. 2004;13:20–4. [PubMed] [Google Scholar]
- 9.Kaufman DM, Holmes DB. Tutoring in problem-based learning: Perceptions of teachers and students. Med Educ. 1996;30:371–7. doi: 10.1111/j.1365-2923.1996.tb00850.x. [DOI] [PubMed] [Google Scholar]
- 10.Lai P. Obstacles to the Implementation of Problem-Based Learning (PBL) in Local universities of Hong Kong. [Last accessed on 2015 Nov 12]. Available from: http://www.alumni.tp.edu.sg/pbl_patricklaictang.pdf .
- 11.Usmani A, Sultan ST, Ali S, Fatima N, Babar S. Comparison of students and facilitators' perception of implementing problem based learning. J Pak Med Assoc. 2011;61:332–5. [PubMed] [Google Scholar]
- 12.Al-Naggar RA, Bobryshe YV. Acceptance of Problem Based Learning among Medical Students. J Community Med Health Educ. 2012;2:5. [Google Scholar]
- 13.Thirunavukkarasu J, Latha K, Nalini A. Assessing the acceptance of problem based learning methodology (PBL) by II MBBS students. Rec Res Sci Technol. 2012;4:17–2. [Google Scholar]
- 14.Khaki AA, Tubbs RS, Zarrintan S, Khamnei HJ, Shoja MM, Sadeghi H, et al. The first year medical students' perception of and satisfaction from problem-based learning compared to traditional teaching in gross anatomy: Introducing problem-based anatomy into a traditional curriculum in Iran. Int J Health Sci (Qassim) 2007;1:113–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Ommar N. Perception of first and second year medical students on problem-based learning in university Malaysia Sarawak. World Appl Sci J. 2011;14:1628–34. [Google Scholar]
- 16.Sultana A, Riaz R, Tehseen I. Comparison of problem based learning with traditional teaching as perceived by the students of Rawalpindi Medical College. RMJ. 2010;35:238–41. [Google Scholar]
- 17.Papanna KM, Kulkarni V, Tanvi D, Lakshmi V, Kriti L, Unnikrishnan B, et al. Perceptions and preferences of medical students regarding teaching methods in a medical college, Mangalore India. Afr Health Sci. 2013;13:808–13. doi: 10.4314/ahs.v13i3.41. [DOI] [PMC free article] [PubMed] [Google Scholar]


