Abstract
Background
Monitoring political and social determinants of delayed or forgone care due to cost is necessary to evaluate efforts to reduce racial and ethnic disparities in access to care. Our objective was to examine the extent to which state Medicaid expansion decisions and personal household income may be associated with individual-level racial and ethnic disparities in delayed or forgone care due to cost, at baseline, prior to the implementation of the Affordable Care Act.
Methods
We used 2012 Behavioral Risk Factor Surveillance System survey data to examine racial and ethnic differences in delayed or forgone care due to cost in states that do and do not plan Medicaid expansion. We examined personal household income as a social factor that could contribute to racial and ethnic disparities in delayed or forgone care.
Results
We found that personal income differences were strongly related to disparities in delayed or forgone care in places with and without plans to expand Medicaid. Additionally, while delayed or forgone care disparities between non-Hispanic whites and non-Hispanic blacks were lowest in places with plans to expand Medicaid access, disparities between non-Hispanic whites and Hispanics did not differ by state Medicaid expansion plans.
Conclusions
As access to insurance improves for diverse groups, health systems must develop innovative strategies to overcome social determinants of health, including income inequities, as barriers to accessing care for Hispanic and non-Hispanic blacks. Additional efforts may be needed to ensure Hispanic groups achieve the benefits of investments in health care access.
Keywords: health policy, health disparities, social determinants of health, income inequality
INTRODUCTION
The Affordable Care Act (ACA), is expected to improve access to care, and reduce racial and ethnic disparities in the number of adults who delay or forgo needed medical care due to cost, particularly, through the expansion of Medicaid.1,2 Racial and ethnic disparities in delayed or forgone care due to cost are likely multifaceted, and disparities may be exacerbated by uneven implementation of reforms, and by the inability to fully address complex root factors that contribute to disparities.
For example, as states tailor plans to expand Medicaid as either a public plan (traditional or managed care plans), as a set of privately administered plans in the case of Arkansas and New Hampshire, or, as states opt out of expanding Medicaid (in the case of Texas, a waiver will allow funds to be used for prevention programs instead of Medicaid), disparities in delayed or forgone care due to cost may be exacerbated by geographic differences in Medicaid coverage.3 Importantly, state decisions on Medicaid expansion may also serve as markers of broader policy decision-making on investments in health care access infrastructure, or other adverse conditions that may affect disparities in delayed or forgone care due to cost. For example, recent prior work has shown that the states that plan to forgo Medicaid expansion tend to have fewer primary care physicians per county, lower Medicaid eligibility thresholds for working adults with children, and higher rates of unemployment and county-level poverty, which are associated with delayed care due to cost.3,4
In addition to insurance and health care access infrastructure, racial and ethnic disparities in delayed care due to cost may also relate to fundamental social determinants of health that influence the ability to access care.5 Of these, our prior work showed personal household income, an indicator of socioeconomic status, was strongly associated with delayed care due to cost, in excess of health care infrastructure differences.4 However, this work did not explore the contribution of personal household income to racial and ethnic disparities in delayed care due to cost.
Our current study explores two questions: at baseline prior to ACA implementation, are there greater racial and ethnic disparities in delayed or forgone care due to cost in policy contexts where Medicaid expansion is not planned, compared to places that do plan expansions? Second, what is the relative contribution of socioeconomic status, particularly household income, to racial and ethnic disparities in delayed or forgone care due to cost, in excess of other factors?
To address these questions, we used national survey data collected prior to ACA implementation (a) to explore maps of the geographic distribution of delayed or forgone care due to cost by race and ethnicity, and (b) to estimate cross-sectional associations among Medicaid expansion decisions, personal household income, and delayed or forgone care due to cost in diverse racial and ethnic groups.
As health systems monitor changes in access to care associated with the ACA, understanding baseline social and demographic patterns in delayed or forgone care due to cost may suggest additional strategies needed to address complex factors underlying racial and ethnic disparities in access to care.
METHODS
Study Population
We analyzed data on non-Hispanic white, non-Hispanic black and Hispanic adults aged 18 – 64 from the 2012 Behavioral Risk Factor Surveillance System (BRFSS), a state-administered telephone survey of non-institutionalized US households. The BRFSS is a cross-sectional, random digit-dial telephone survey of the non-institutionalized civilian population aged 18 years and older. The survey is administered by the states and the Centers for Disease and Control and Prevention, and is fielded annually by state health departments in each of the 50 states, the District of Columbia and select US territories. In the BRFSS, raking weights are used to produce state-specific and population estimates that adjust for survey non-coverage, non-response, and the probability of being sampled given the geographic location, age, race, and sex of the participant.6
Outcome variable
To assess delayed or forgone care due to cost, we constructed a binary (“yes”/”no”) variable to code responses to the BRFSS survey question: “Was there a time in the past 12 months when you needed to see a doctor but could not because of cost?”
Predictor and modifying variables
Race and ethnicity were defined by self-report as non-Hispanic white, non-Hispanic Black and Hispanic ethnicity of any race. Annual household income was categorized as ≥$75,000, $50,000–74,999, $25,000–49,999, or <$25,000. For these analyses, states were classified as planning to expand Medicaid if, by December 2014, state legislative and federal approval had been granted either for extending traditional Medicaid to low-income groups at 133% of the federal poverty line (plus a 5% income offset), for providing coverage through Section 1115 waivers, or for alternative structures, including using federal funding to provide coverage through exchanges. States that were still debating at that time were classified as not expanding Medicaid. We conducted sensitivity analyses and found that our results did not change when we re-classified four states with pending implementation plans (Indiana, Pennsylvania, Utah, Montana) as planning to expand Medicaid.
Area-level covariates
We assessed county-level poverty (for the population aged 18 to 64), and county-level unemployment (for the population aged 16 years and older), using the 2008–2012 US Census American Community Survey. County-level primary care physician concentration per 100,000 population was compiled from the 2011 Area Health Resource File. State Medicaid income eligibility thresholds for working adults with children as of January 2012 were obtained from the Henry J. Kaiser Family Foundation.7
Individual-level covariates
We examined self-reported individual-level BRFSS participant characteristics that we hypothesized were related to delayed or forgone care due to cost, including age and sex, educational attainment (categorized as “college graduate or more,” “some college,” “high school graduate,” or attained “less than high school education,”) employment status (categorized as “employed for wages,” “unemployed ≥1 year,” “unemployed <1year,” “retired” or “other,”) self-rated health (classified as “excellent,” “very good,” “good,” or “fair/poor,”) smoking status (classified as “current,” “former” or “never smokers,”) physical activity status in the past thirty days (the BRFSS used a “yes/no” indicator in answer to the question:”During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?”), body mass index (classifed as low: <18.5, normal: 18-5-24.9, overweight: 25–29.9, or obese: ≥30) and physician’s reported diagnosis of diabetes, asthma (classified as “never,” “former,” “current” by the BRFSS) and cardiovascular disease (determined from reported myocardial infarction, stroke or coronary heart disease). Self-reported insurance status in the 2012 BRFSS does not capture specific sources of insurance, and participants were defined as “insured” or “uninsured.”
Don’t know, refused and item non-response values for all covariates were set to missing and excluded from the analysis. The largest source of missing individual-level data was income (9.9%), body mass index (4.9%), diabetes (2.4%) and smoking status (1.4%). Other missing covariates had between 0.02% and 0.6% missing data.
Mapping Delayed Care Due to Cost by Race/Ethnicity
We described geographic patterns in delayed or forgone care due to cost by race and ethnicity with 2012 BRFSS data from non-Hispanic whites (N=205,557 individuals in 2,229 counties), non-Hispanic blacks (N=27,215 individuals in 1,335 counties), and Hispanic groups (N=21,993 individuals in 1,472 counties). The goal of the small-area map analysis was to describe the magnitude of racial and ethnic disparities in delayed care due to cost across geographic areas in which Medicaid expansion is planned, or not planned. We estimated the county-level prevalence of delayed or forgone care due to cost for non-elderly adult BRFSS participants aged 18–64 who had complete data on delayed care in the 2012 data. Estimates were produced using Poisson log-linear regression models with county-level random effects, as implemented by the glmmPQL function in the MASS package of the statistical software R, version 3.0.1. For outcome count Yi from county i with population count ni, the exact model is Yi ~ Poisson(μi)
where ui are county-specific normally distributed random effects with Gaussian spatial correlation structure with the correlation between a pair of counties depending on the distance between the county centroids.
These models yield smoothed prevalence estimates in geographic areas with small sample sizes.8 Models incorporated spatially-correlated, state-level random effects to account for clustering imposed by similarities among individuals within the same state. County-level estimates from the BRFSS have been obtained previously in other studies using small-area estimation techniques that produce smoothed prevalence estimates.9,10
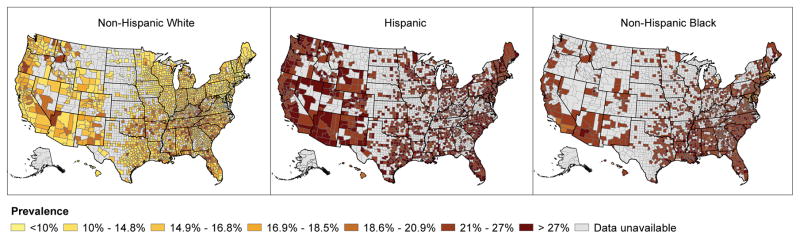
Smoothed county-level prevalence estimates of delayed or forgone care due to cost were mapped by race and ethnicity in Figure 1 with ArcGIS 10.0 (ESRI®, Redlands, California). Due to small numbers within county, 11.3% of BRFSS participants were missing geographic identifiers. Hispanic ethnic groups were overrepresented in the population missing geographic identifiers (19.6%) compared to the population with geographic identifiers (16.1%). However, those missing geographic identifiers did not differ with respect to delayed or forgone care due to cost.
Figure 1.
County-Level Smoothed Prevalence of Delayed or Forgone Care Due to Cost among Adults between the Ages of 18 and 64 Years by Race/Ethnicity
Source: Authors’ calculations based on data from the 2012 Behavioral Risk Factor Surveillance System. Notes: Smoothed prevalence estimates of delayed or forgone care were generated via Poisson mixed effect models via the glmmPQL function in the MASS package of R version 3.0.1. We estimated delayed or forgone care within three ethnic groups including: 205,557 non-Hispanic whites within 2,229 counties, 27,215 non-Hispanic blacks within 1,335 counties and 21,993 Hispanics within 1,472 counties.
Descriptive statistics
We used Wald F-tests to compare differences between non-Hispanic whites, and non-Hispanic blacks and Hispanic groups, on individual-level and area-level covariates thought be associated with delayed or forgone care due to cost, including demographics, socioeconomic indicators, health status indicators, and contextual factors (primary care physician concentration, county poverty, county unemployment rate, state Medicaid eligibility threshold pre-ACA, and status of decisions on Medicaid implementation).
Multivariable model statistical analysis
To examine the potential modifying effect of Medicaid expansion decisions on racial disparities in delayed or forgone care due to cost for individuals living in states that planned and did not plan to expand Medicaid, we obtained model-based (a) point estimates and (b) prevalence ratios of delayed care due to cost with 95% confidence intervals, by race and Medicaid expansion decisions, all estimated via average marginal predictions fit in logistic regression models.11 Finally, to understand the relative contribution of personal household income to racial and ethnic disparities in delayed or forgone care due to cost, in excess of other factors, we report model-based point estimates and prevalence ratios associated with race and ethnicity adjusting for (a) personal household income, (b) all measured socioeconomic status conditions, (c) all measured health care policy and access variables, and (d) all measured covariates. The model of all measured covariates includes statistically significant interaction terms between household income and model covariates (education, physical activity), and between race and ethnicity and Medicaid expansion plans. Interaction terms did not change main effects associated with household income, race or Medicaid expansion decisions.
To account for clustering at the county-level we use scaled survey weights as described by Carle.12 To account for the complex survey design, we fit models with the SAS (version 9.3, SAS Institute, Cary, NC) callable version of statistical package SUDAAN (version 11.0.0, Research Triangle Institute, Research Triangle Park, NC). Tests of statistical significance use two-tailed significance tests at the 0.05 alpha level from Wald F tests calculated in SUDAAN software to account for the complex survey design. Tests of significance for additive interaction terms from predicted marginal models were calculated on the risk difference scale as detailed by Bieler et al.11
RESULTS
Disparities by County-Level Geography and Individual-level Characteristics
Figure 1 shows broad racial and ethnic disparities in county-level prevalence estimates of delayed or forgone care due to cost. In 2012, the magnitude of delayed or forgone care due to cost ranged between 5.7% and 27.6% among non-Hispanic whites, 12.9% and 35.8% among non-Hispanic blacks, and 16.4% to a high of 42.9% among Hispanic groups.
Within-county racial and ethnic disparities in delayed or forgone care were not specific to areas that did not plan to expand Medicaid, but instead, were seen throughout the US, including disparities within counties with low overall delayed care (Figure 1). For example, in Suffolk County Massachusetts, with one of the lowest percentages of delayed care in the US, the prevalence was 7.2% higher for Hispanics than non-Hispanic whites (16.4% vs. 9.2%) and 5.5% higher for non-Hispanic blacks (14.7%).
Compared to non-Hispanic whites, non-Hispanic blacks and Hispanic groups were younger, had lower incomes, lower educational attainment, were less likely to be insured, more frequently had fair or poor self-rated health, and lived in counties with higher poverty, higher unemployment rates, and lower Medicaid eligibility thresholds. Non-Hispanic blacks were less likely to live in states that were planning Medicaid expansion, while Hispanic groups were more likely to live in states planning to implement expansion than other groups (see Supplemental Table A). Populations living in states with plans to implement Medicaid expansion were exposed to higher concentrations of primary care physicians per county, lower county poverty, lower county unemployment, and higher pre-ACA Medicaid eligibility thresholds for working adults with children (Supplemental Table B).
Individual-level Racial and Ethnic Disparities by State Decisions to Expand or not to Expand Medicaid
Table 1 shows racial and ethnic differences in delayed or forgone care due to cost by state decisions to expand Medicaid. Adjusted for age and sex, for all three racial and ethnic groups, delayed or forgone care due to cost pre-ACA expansion was lower in states planning to expand Medicaid than in states not planning expansions.
Table 1.
Model Adjusted Percentage of Individuals with Delayed or Forgone Care due to Cost among Non-Elderly Adults in the United States, BRFSS 2012
| Model Adjusted Estimates of Delayed or Forgone Care Due to Cost* (95% CI) | |||
|---|---|---|---|
| N=209,760 | Non-Hispanic White N=171,066 |
Non-Hispanic Black N=21,900 |
Hispanic N=16,794 |
| Differences by State Decision to Expand Medicaid† | |||
| All states | 15.2 (14.9, 15.4) | 24.4 (23.6, 25.2) | 27.6 (26.6, 28.5) |
| States Expanding Medicaid | 14.2 (13.9, 14.5) | 20.8 (19.7, 22.0) | 26.6 (25.6, 27.7) |
| States Not Expanding Medicaid | 17.1 (16.7, 17.5) | 27.8 (26.7, 29.0) | 30.1 (28.1, 32.1) |
| Personal Household Income-adjusted Differences by State Decision to Expand Medicaid‡ | |||
| All states | 17.0 (16.7, 17.2) | 18.1 (17.5, 18.7) | 20.4 (19.7, 21.2) |
| States Expanding Medicaid | 15.7 (15.4, 16.1) | 15.8 (15.0, 16.7) | 19.1 (18.3, 19.9) |
| States Not Expanding Medicaid | 19.2 (18.8, 19.7) | 20.7 (19.8, 21.7) | 23.5 (21.9, 25.2) |
Source: Data from Centers for Disease Control and Prevention 2012 Behavioral Risk Factor Surveillance System unless otherwise noted. Analyses performed among the N = 209,760 participants with complete data on all covariates.
Notes:
Multivariable logistic regression weighted using scaled weights to account for clustering at the county level with rlogist function in SUDAAN.
Models adjusted for age and sex.
Models adjusted for age, sex and income. Medicaid expansion status classified as of 2014.
There was a statistically significant additive interaction contrast by race and Medicaid expansion plans for non-Hispanic blacks versus non-Hispanic whites (p < 0.001), but not between non-Hispanic whites and Hispanic groups (p = 0.08). For non-Hispanic blacks, there was a greater racial disparity compared to non-Hispanic whites in states that were not planning Medicaid expansion (27.8% vs. 17.1%) than in states planning expansion (20.8% vs. 14.2%.) However, Hispanic versus non-Hispanic white differences in delayed or forgone care due to cost were equally large, and not significantly different in states not planning Medicaid expansion (30.1% vs.17.1%), compared to states planning expansion (26.6.% vs. 14.2%)
Racial and Ethnic Disparities Adjusted for Income Differences
Adjusting for personal household income either eliminated or significantly reduced the absolute racial or ethnic difference in delayed or forgone care between non-Hispanic whites and non-Hispanic black or Hispanic groups in states where Medicaid expansions were and were not being planned (Table 1).
Multivariable Models
Table 2 shows the prevalence ratio associated with race and ethnicity, adjusted for age and sex. Adjusting for personal household income reduced the prevalence ratio associated with race and ethnicity to 1.07 (95% CI 1.03, 1.11) for non-Hispanic blacks and 1.20 (95% CI 1.16, 1.25) for Hispanic groups, compared to non-Hispanic whites (not presented in tables). Full adjustment for socioeconomic conditions at the individual and county-level fully attenuated disparities among non-Hispanic whites and non-Hispanic blacks (1.02, 95% CI 0.98, 1.06), and substantially attenuated disparities between non-Hispanic white and Hispanic groups (1.14, 95% CI 1.10, 1.19). Models adjusting for all measured health policy and access variables (health insurance status, concentration of primary care physicians, state Medicaid income eligibility thresholds pre-ACA, and status on Medicaid expansion decisions) also significantly attenuated differences by race and ethnicity (Table 2). After adjustment for socioeconomic conditions, health policy access, health status and health behaviors, racial and ethnic differences in delayed or forgone care due to cost were substantially attenuated, though residual disparities were seen between non-Hispanic whites and Hispanic groups (Table 2.)
Table 2.
Data Tables of Prevalence Ratios for Delayed or Forgone Care due to Cost among Non-Elderly Adults in the United States, BRFSS 2012
| Prevalence Ratios* (95% CI) | ||||
|---|---|---|---|---|
| Disparities by Race and Ethnicity and the Role of SES Inequities | ||||
| N= 209,760 | Age and Sex Adjusted‡ | Socioeconomic Status§ | Health Policy and Access|| | Fully Adjusted¶ |
| Race† | ||||
| Non-Hispanic White | 1.00 | 1.00 | 1.00 | 1.00 |
| Non-Hispanic Black | 1.61 (1.55, 1.67) | 1.02 (0.98, 1.06) | 1.29 (1.22, 1.36) | 1.03 (0.97, 1.09) |
| Hispanic | 1.82 (1.75, 1.89) | 1.14 (1.10, 1.19) | 1.27 (1.21, 1.33) | 1.06 (1.01, 1.12) |
Source: Data from Centers for Disease Control and Prevention 2012 Behavioral Risk Factor Surveillance System unless otherwise noted. Analyses performed among the N = 209,760 participants with complete data on all covariates. Concentration of primary care doctors from the Area Health Resource File. State Medicaid income eligibility limits and Medicaid Expansion Status from the Kaiser Family Foundation. County percent in poverty and unemployment rate from the 2008–2012 US Census American Community Survey.
Notes:
Multivariable logistic regression weighted using scaled weights to account for clustering at the county level with rlogist function in SUDAAN.
Race/ethnicity includes Hispanics of any race in the Hispanic category.
Model adjusted for age and sex.
Socioeconomic status model adjusted for age, sex, income, education, employment status, county unemployment rate, county percent in poverty and statistical significant interactions between education and income.
Health policy and access model adjusted for health insurance status, county concentration of primary care doctors, state Medicaid income eligibility threshold, state Medicaid expansion status and statistical significant interactions between race/ethnicity and Medicaid expansion status.
Fully adjusted model includes all covariates in the socioeconomic status model, health policy and access model and self rated health, cardiovascular disease, diabetes, asthma, smoking status, physical activity, body mass index, and statistical significant interactions between: education and income, race/ethnicity and Medicaid expansion status, and physical activity and income.
DISCUSSION
At this writing, it is still early to assess the impact of the ACA on racial and ethnic disparities in access to care. Recent Gallup data give cause for optimism, and show insurance coverage gains among non-Hispanic blacks and Hispanics that are associated with Medicaid expansion and established insurance exchanges.13 Additionally, there are early improvements in racial and ethnic disparities in the ability to access medications during the early phases of ACA enrollment.14 However, our data show that the context of ACA implementation differs by race and ethnicity, and that personal household income differences are strongly related to excess delayed or forgone care due to cost among non-Hispanic black and Hispanic groups. Moreover, though Hispanic groups are more likely to live in places with more generous access policies pre-ACA, delayed or forgone care due to cost were highest among Hispanics compared to any other group. Disparate results for Hispanic groups pre-ACA raise concern that these groups may not achieve the full benefits of general policies that enhance access to care. As improved efforts are employed to reach uninsured Hispanics and other uninsured groups, additional access strategies, including continued preservation and use of safety-net funding, may be needed to promote access to care.15 For example, prior data in Massachusetts showed that during the implementation of insurance coverage expansions in 2006, safety-net funds were used successfully to preserve the use of women’s cancer screening for some low-income groups.16
Importantly, our analyses suggest that racial and ethnic differences in household income may be under-appreciated and under-addressed contributors to disparities in health care access.17 In the 2012 BRFSS data, income differences largely accounted for disparities in delayed or forgone care between non-Hispanic blacks and whites, after adjusting for related factors including educational attainment. As Medicaid expansion and other ACA provisions are implemented, sustainable approaches to addressing disparities in delayed or forgone care may need to address income inequality directly. ACA provisions may be expected to contribute to reducing income inequality, chiefly by reducing out-of-pocket health care spending, and by supporting more efficient care through investments in primary care infrastructure (e.g. reduced wait times for physician appointments).18 However, prior data show that in even places that have had established policies for improving health status 19 access to insurance, and health care infrastructure, delayed or forgone care due to cost is associated with income differences.4 Our current analysis suggests a strong potential for reducing racial and ethnic disparities in delayed or forgone care by addressing income inequality primarily. To this end, the Institute of Medicine (IOM) has called for health systems to address social determinants of health, for example, by using electronic health records (EHRs) to gather data on income and other social factors, to assist in developing population health intervention strategies.20 Additionally, Accountable Care Organizations (ACOs) are uniquely positioned to try innovative strategies to address social determinants as a part of population health management. For example, in Hennepin County Minnesota, multifaceted health sector providers, social services and payer groups have developed an ACO model with capacity to address social service needs of patients, including vocational services to address patient unemployment and other issues.21 Similar innovative strategies that address income inequality may be important components of multifaceted approaches to health equity promotion.17
Our study has important limitations that should be noted. Our design is cross sectional and we cannot draw causal conclusions from the findings we report. Importantly, our findings related to income could reflect endogeneity, where high costs of care reduce income. Data from the Medical Panel Expenditure Survey show that as incomes fell during the Great Recession, total medical expenditures tended to fall as well, making endogeneity less likely as an explanation for our results.22 Second, racial differences in chronic illness may be associated with differential demand for care that could affect care seeking behavior. To better isolate the relation between personal household income and Medicaid expansion decisions as contributors to delayed care, we have included potential confounders in multivariable models, including adjustment for self-rated health and chronic health conditions that might be expected to influence demand for care. However, our results must be viewed in light of the potential for unmeasured factors to explain the associations we observed.
In terms of the generalizability of our findings, the BRFSS is a telephone based survey that is largely based on landline telephone samples, with response rates of 49.1% for landline telephones and 35.3% for cellular telephones. The response rate is comparable to that of other national telephone based surveys, and the inclusion of cellular telephones is expected to increase generalizability of the BRFSS by increasing sampling of populations with lower incomes, lower educational levels, and younger age groups.23 Our data also have limitations related to measurement. The BRFSS measures delayed or forgone care due to cost with a single question, and does not distinguish between those who delay or do not at all see a doctor (have forgone care) due to cost. Additionally, the BRFSS does not report specific sources of costs that may delay care, including out-of-pocket costs for prescription drugs, office visit co-payments, or logistical and opportunity costs associated with visiting a physician, such as transportation or time missed from work. Because of this limitation, we cannot report on the specific cost-related barriers that may contribute to any disparities we observe. Recent data suggest that for nonelderly adults, out-of-pocket prescription drug costs, for example, have declined in recent years.24 An important focus for policy and surveillance research going forward will be to collect and track specific cost barriers to monitor impacts of policy changes on racial and ethnic disparities as health care reform policies are implemented.
With respect to small-area estimation, we note that eleven percent of BRFSS participants were missing geographic identifiers. Those missing identifiers were more likely to be Hispanic, but did not differ by delayed or forgone care due to cost. As a result, our estimates may underestimate the experience of Hispanic populations, but are unlikely to bias the associations between race/ethnicity and delayed or forgone care that we report.
Importantly, we report data for non-Hispanic whites, non-Hispanic black, and Hispanic groups, but not for other racial and ethnic groups or for specific Hispanic subgroups. Existing national surveillance data are limited in sampling design, and additional strategies must be employed to identify trends in other populations with diverse experiences.25
CONCLUSIONS
In summary, we find that baseline racial and ethnic disparities in delayed or forgone care due to cost are associated with state decisions to expand Medicaid for some groups, as well as lower personal household incomes for Hispanics and non-Hispanic blacks. As Medicaid expansion is implemented over time, greater surveillance is required to ensure that racial gaps in delayed or forgone care are not widened. For Hispanic groups, additional strategies may be required to shore up access to care, above and beyond access provided by Medicaid.
We note that both the issues of racial and ethnic disparities in health care access, and racial and ethnic disparities in socioeconomic status may be viewed as longstanding, and perhaps, intractable problems in the US. However, as the country becomes increasingly diverse, and confronts both the growing pressure to contain health care costs, and the need to encourage early access to preventive care, there is a pressing need to develop and implement innovative strategies that address root causes of poor access disparities, including income inequities.26 The surveillance data we present here underscore this need, and we suggest that income differences be addressed directly to promote sustainable reductions in racial and ethnic disparities in access to care.
Supplementary Material
Acknowledgments
Funders: This research was conducted with support from the National Institute on Aging (K08 AG 032357) and the Harvard Catalyst | The Harvard Clinical and Translational Science Center (NIH Grant #1 UL1 RR 025758-01 and financial contributions from participating institutions). The funding organizations were not involved in the design or conduct of the study, interpretation of the data, or preparation of the manuscript.
References
- 1.The Kaiser Commission on Medicaid and the Uninsured. Key Facts about the Uninsured Population. Kaiser Family Foundation; 2014. [Last accessed: 8-28-2015]. [Google Scholar]
- 2.Kaiser Commission on Medicaid and the Uninsured. [Last accessed: 8-28-2015];Impact of the Medicaid Expansion for Low-Income Communities of Color Across States. 2013 http://www.kff.org/minorityhealth/upload/8435.pdf.
- 3.Stephens J, Artiga S, Lyons B, Jankiewicz A, Rousseau D. Understanding the Effect of Medicaid Expansion Decisions in the South. JAMA. 2014;311:2471. [Google Scholar]
- 4.Clark CR, Ommerborn MJ, Coull BA, Pham DQ, Haas J. State Medicaid Eligibility and Care Delayed Because of Cost. New England Journal of Medicine. 2013;368:1263–1265. doi: 10.1056/NEJMc1214874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annual review of public health. 2011;32:381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- 6.Methodologic Changes in the Behavioral Risk Factor Surveillance System in 2011 and Potential Effects on Prevalence Estimates. Morbidity and Mortality Weekly Report. 2012:61. [PubMed] [Google Scholar]
- 7.The Kaiser Commission on Medicaid and the Uninsured. Performing Under Pressure: Annual Findings of a 50-State Survey of Eligibility, Enrollment, Renewal, and Cost-Sharing Policies in Medicaid and CHIP, 2011–2012. The Henry J. Kaiser Family Foundation; 2012. [Last accessed: 8-28-2015]. [Google Scholar]
- 8.Bivand RS, Pebesma EJ, Gómez-Rubio V. Applied Spatial Data Analysis with R. Springer-Verlag; New York, LLC: 2008. New Edition ed. [Google Scholar]
- 9.Parsons VL, Schenker N. County-Level Small Area Estimation using the National Health Interview Survey (NHIS) and the Behavioral Risk Factor Surveillance System (BRFSS) Section on Survey Research Methods - JSM. 2008 [Google Scholar]
- 10.Jia H, Muennig P, Borawski E. Comparison of small-area analysis techniques for estimating county-level outcomes. American journal of preventive medicine. 2004;26:453–460. doi: 10.1016/j.amepre.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. American journal of epidemiology. 2010;171:618–623. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- 12.Carle A. Fitting multilevel models in complex survey data with design weights: Recommendations. BMC Medical Research Methodology. 2009;9:49. doi: 10.1186/1471-2288-9-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levy Jenna. [Last accessed: 8-28-2015];US Uninsured Rate Holds Steady at 13.4%: Uninsured rate declining most among blacks and Hispanics. 2014 http://www.gallup.com/poll/170882/uninsured-rate-holds-steady.
- 14.Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in Self-reported Insurance Coverage, Access to Care, and Health Under the Affordable Care Act. JAMA. 2015;314:366–374. doi: 10.1001/jama.2015.8421. [DOI] [PubMed] [Google Scholar]
- 15.Hall MA. Rethinking safety-net access for the uninsured. New England Journal of Medicine. 2011;364:7–9. doi: 10.1056/NEJMp1011502. [DOI] [PubMed] [Google Scholar]
- 16.Clark CR, Soukup J, Riden H, et al. Preventive Care for Low-Income Women in Massachusetts Post-Health Reform. Journal of Women’s Health. 2014 doi: 10.1089/jwh.2013.4612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lichtenstein R. The Vexing Problem of Health Inequalities in the United States: What is to be Done? Medical care. 2015;53:215–217. doi: 10.1097/MLR.0000000000000332. [DOI] [PubMed] [Google Scholar]
- 18.Collins Sara R, Robertson Ruth, Garber Tracy, Doty Michelle M. The Income Divide in Health Care: How the Affordable Care Act will Help Restore Fairness to the U.S. Health System. The Commonwealth Fund; 2012. [Last accessed: 8-28-2015]. [PubMed] [Google Scholar]
- 19.Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. New England Journal of Medicine. 2012;367:1025–1034. doi: 10.1056/NEJMsa1202099. [DOI] [PubMed] [Google Scholar]
- 20.Adler NE, Stead WW. Patients in context - EHR capture of social and behavioral determinants of health. New England Journal of Medicine. 2015;372:698–701. doi: 10.1056/NEJMp1413945. [DOI] [PubMed] [Google Scholar]
- 21.Hennepin County Projects and Initiatives. 2015. [Last accessed: 8-28-2015]. Hennepin: Health Care Reform. [Google Scholar]
- 22.Chen J, Vargas-Bustamante A, Mortensen K, Thomas SB. Using quantile regression to examine health care expenditures during the great recession. Health services research. 2014;49:705–730. doi: 10.1111/1475-6773.12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Behavioral Risk Factor Surveillance System: 2012 Summary Data Quality Report. Centers for Disease Control and Prevention; 2013. [Last accessed: 8-28-2015]. [Google Scholar]
- 24.Gellad WF, Donohue JM, Zhao X, Zhang Y, Banthin JS. The financial burden from prescription drugs has declined recently for the nonelderly, although it is still high for many. Health Affairs. 2012;31:408–416. doi: 10.1377/hlthaff.2011.0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bitton A, Ayanian JZ. Health risks, chronic diseases, and access to care among US Pacific Islanders. Journal of general internal medicine. 2010;25:435–440. doi: 10.1007/s11606-009-1241-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: how interventions that address the social determinants of health can improve health and reduce disparities. Journal of public health management and practice: JPHMP. 2008;14:S8. doi: 10.1097/01.PHH.0000338382.36695.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.