Abstract
Objectives
To examine the association between numbers of primary care provider (PCP) visits for asthma monitoring (AM) over time and acute asthma visits in the emergency department (ED) and at the PCP for Medicaid-insured children.
Methods
We prospectively enrolled children 2–10 years-old during ED asthma visits. We audited hospital and PCP records for each subject for 3 consecutive years. We excluded subjects also receiving care from asthma subspecialists. PCP AM visits were those with documentation that suggested discussion of asthma management but no acute asthma symptoms or findings. PCP “Acute Asthma” visits were those with documentation of acute asthma symptoms or findings, regardless of treatment. ED asthma visits were those with documented asthma treatment. Generalized liner models were used to analyze the association between numbers of AM visits and acute asthma visits to the ED and PCP.
Results
One hundred three subjects were analyzed. Over the 3 years, the mean number of AM visits/child was 2.5 ± 2.3 (standard deviation), range 0–10. Only 50% of subjects had at least 1 PCP visit with an asthma controller medication documented. The mean number of ED asthma visits/child was 3.2 ± 2.8; range 1–18. The mean number of PCP Acute Asthma visits/child was 0.7 ± 1.6; range 0–11. Increasing AM visits was associated with more ED visits (estimate 0.088; 95% CI 0.001, 0.174), and more PCP Acute Asthma visits (estimate 0.297; 95% CI 0.166, 0.429). Increasing PCP visits for any diagnosis was not associated with ED visits (estimate 0.021; 95% CI −0.018, 0.06).
Conclusions
Asthma monitoring visits and documented controller medication for these urban Medicaid-insured children occurred infrequently over 3 years, and having more asthma monitoring visits was not associated with fewer ED or PCP acute asthma visits.
Keywords: primary care provider, emergency department, visits, morbidity, monitoring
INTRODUCTION
Regular asthma monitoring (AM) visits (every 1–6 months depending on severity) are recommended by the National Asthma Education and Prevention Program (NAEPP) guidelines as opportunities to assess asthma risk and impairment, adjust treatment, and educate and foster collaborative partnerships with patients.[1] Data from national US surveys demonstrate high asthma morbidity including many emergency department (ED) visits, for minority children, those in urban areas, and those with Medicaid insurance.[2–5] Several studies have shown that AM visits at primary care providers (PCPs) occur infrequently, particularly as follow-up from an emergency department visit for asthma.[6–15] When such visits do occur, care often does not meet guideline-based preventive action.[16, 17] However, multiple factors also impact asthma outcomes, including inadequate contact with a health care provider, access to medical care, and maternal psychosocial factors including maternal depression and social isolation.[17–22]
Studies evaluating the effect of AM visits to reduce ED visits and hospitalizations have come to different conclusions. Smith et al. used a retrospective review of Medicaid claims and found that children with a greater number of asthma-related primary care visits were less likely to have asthma-related ED visits.[11] However, Nelson et al. found that while a coaching intervention increased likelihood of at least one future AM visit there was no impact on ED visits.[12] Most concerning was the finding of Cabana et al. that follow-up visits within 30 days after ED visits for asthma were associated with an increased likelihood of an ED visit within 1 year.[9] There are limited studies of the relationship between numbers of PCP AM visits and ED visits over an extended period of time for children at high risk for asthma morbidity.
The objectives of this study were to examine the association between numbers of AM visits to PCPs and morbidity measured as numbers of acute asthma visits over an extended (3-year) period, with a focus on the impact of multiple AM visits on the number of ED visits. Our hypothesis was that increased AM visits is associated with fewer ED visits. Our subjects were children with asthma who had Medicaid insurance and lived in an urban area. By hand-auditing medical records, we were able to clarify visit types beyond the level of billing codes. We also specifically examined characteristics associated with having 6 or more AM visits over 3 years as this represents an average of 2/year, aligned with the minimum frequency recommended in the NAEPP guidelines.[1]
METHODS
Study design and selection of subjects
This study is a secondary analysis of data from a randomized controlled trial of peer asthma coaching to reduce morbidity.[12] The study was conducted through an urban tertiary-care children’s hospital. From 9/1/03 to 5/15/05, during ED visits for acute asthma care, we prospectively enrolled a sample of parents and children and followed them for 2 years. Recruitment was limited to two 8-hour shifts of the two recruiters five days a week. Parents were the primary subjects and were eligible if they attested to being primary caregivers of eligible children, spoke English, had working telephones, and agreed to study procedures. Eligible children were age 2–10 years; had, by parent report, an asthma diagnosis and reported at least 1 other acute asthma visit in either an ED or the PCP office during the preceding 15 months; resided in local urban zip codes; had Medicaid insurance; and received at least 1 albuterol dose during the enrollment ED visit. Enrollment was limited to one parent-child dyad per household. Our affiliated University Human Research Protection Office approved study procedures, and informed consent was obtained from all subjects.
One goal of the main randomized controlled trial was to improve AM visits to the PCP and subsequently reduce ED visits and hospitalizations.[12] The primary results of the trial have been published and demonstrated that peer asthma coaching did increase the proportion with ≥1AM visits over the 2 years, but did not have the subsequent effect of decreasing ED visits and hospitalization.[12]
In this current study, we focused the analysis on how partnership between the parent and the PCP (assessed by the number of AM visits) relates to the number of acute asthma visits over time, including all three years of data (1 year pre-enrollment and 2 years post-enrollment). In order to remove the potential confounding of asthma coaching, we limited this analysis to subjects in the control group (n=121). Also, as the focus of this analysis was the impact of care by PCPs, we excluded subjects who had visits to the hospital sub-specialty asthma clinic in addition to their PCP (n=18), yielding 103 subjects for analysis.
Outcomes and Covariates: Definition and Measurement
Health care visits
Each child’s hospital and PCP medical records were audited for visits over three consecutive years (1 year before and 2 years after enrollment). Investigators trained research assistants to audit the medical records and identify asthma-related terminology. Parents were contacted every 6 months and reported health care visits were verified by audit of medical records. There were 20 PCP practices involved with the study. Each child had records at their PCP clinic during all 3 years of the study, indicating ongoing contact and suggesting continuity of care. PCP visits with documentation of acute asthma symptoms or examination findings were coded as "acute asthma" regardless of treatment administered or prescribed. Asthma Monitoring (AM) visits were those with documentation suggesting asthma management had been discussed, but no acute asthma symptoms or findings listed (i.e. not acute visits). AM visits included "well-child" visits with asthma listed as a diagnosis and/or any asthma medication documented, and included visits labeled as asthma "check-up" or "follow-up." ED Asthma visits were those with documentation of asthma medication administered or prescribed. ED visits that ended in hospitalization were counted as ED visits. After study completion, investigators masked to research assistants' assessments verified the visit categorizations. The primary outcome was number of ED asthma visits.
Parent and child characteristics
Factors that are often considered as important in outcomes of childhood asthma, including child race, symptom severity, and parental education, employment, income, social isolation, and quality of life, were included in the analyses (see Tables 1 and 2). During enrollment, parents completed questionnaires assessing asthma disease characteristics and demographic information. Asthma severity was measured using a score representing the frequency of asthma symptoms in the 7 days preceding the increased symptoms resulting in the index ED visit. This symptom score was derived from three questions based on the constructs for measuring asthma impairment in the NAEPP guidelines.[1] This score was the sum of a) days with any asthma symptoms (cough, wheeze, shortness of breath, or chest tightness), b) nights awakened due to symptoms, and c) days with activity limitations due to symptoms; maximum score was 21. To aid recall, the research assistant asked the parent when the child had started to become ill with the current exacerbation, noting the day on a calendar, and then referred to the calendar when asking the 3 questions concerning symptoms during the week before this date. Social support was assessed by answers parents gave to four questions: 1) number of friends you can call on when you need a favor, 2) number of friends with whom you feel at ease and can talk about a private matter; 3) number of relatives you can call on when you need a favor, and 4) number of relatives with whom you feel at ease and can talk about a private matter.[22, 23] A composite score was calculated based on responses to the 4 questions and “social isolation” was defined as reporting < median number of friends and relatives. The Pediatric Caregivers Quality of Life Questionnaire was given to the primary caregiver present in the ED at the time of enrollment.[24] The poverty level as assessed from the zip code of the family with reference to the 2000 United States Census Block Group data.
Table 1.
Characteristics of children and parents
| n=103 | |
|---|---|
| CHILDREN | |
|
| |
| Gender, male | 58% |
| Age, years | 5.4 (2.6) |
| Race | |
| African American | 95% |
| White | 1.0% |
| African American & White | 3.9% |
| Symptom score a | 5.7 (4.3) |
| Admitted at enrollment visit | 20% |
| Attends federally-funded clinic | 59% |
|
| |
| PARENTS | |
|
| |
| Gender, female | 97% |
| Age, years | 29.2 (7.3) |
| Race | |
| African American | 95% |
| White | 5% |
| Relationship to child, Mother | 93% |
| No. of children in house | 2.8 (1.4) |
| No. of adults in house | 1.6 (0.7) |
| High school graduate or equivalent | 76% |
| Employed (full, part, or self-employed) | 64% |
| Social isolation b | 43% |
| PACQLQ, total score c | 4.5 (1.3) |
| % below federal poverty level d | 28 (13) |
Data is presented as number (%) and mean (standard deviation). Categorical data were compared using Fisher's exact test; continuous data using analysis of variance.
3 questions regarding # of days with symptoms [a) at any point during day, b) awakening from sleep, and c) interfering with play] that occurred in the week preceding current exacerbation; possible maximum score = 21.
Number of subjects reporting < 7 (median) friends or relatives they feel that they may “talk with” or “ask a favor”.
Pediatric Asthma Caregivers Quality of Life Questionnaire. Juniper et al, Qual Life Res. 1996;5:27–34
Based on address at enrollment and 2000 United States Census Block Group data.
Table 2.
Characteristics of children and parents according to having 6 or more asthma monitoring visits over 3 years
| < 6 AM visits (n=90) |
≥ 6 AM visits (n=13) |
P-value | |
|---|---|---|---|
| CHILDREN | |||
|
| |||
| Gender, male | 58% | 62% | 0.80 |
| Age, years | 5.6 (2.6) | 3.7 (2.2) | 0.02 |
| Race | |||
| African American | 98% | 76% | <0.001 |
| White | 0% | 8% | <0.01 |
| African American & White | 2% | 15% | 0.02 |
| Symptom score a | 5.6 (4.3) | 6.1 (3.7) | 0.69 |
| Admitted at enrollment visit | 20% | 23% | 0.79 |
| Attends federally-funded clinic | 62% | 38% | 0.10 |
| Health Care Visits over 3 years | |||
| ED visits for asthma | 3.0 (2.5) | 4.5 (4.4) | 0.09 |
| Hospitalizations for asthma | 0.6 (1.0) | 0.6 (1.0) | 0.95 |
| Acute asthma PCP visits | 0.5 (1.0) | 2.2 (3.3) | < 0.05 |
| Asthma controller medication documented in ≥1 PCP visit | 43% | 100% | <0.001 |
|
| |||
| PARENTS | |||
|
| |||
| Gender, female | 97% | 100% | 0.50 |
| Age, years | 29.6 (7.5) | 26.6 (5.2) | 0.18 |
| Race | |||
| African American | 97% | 85% | 0.06 |
| White | 3% | 15% | 0.06 |
| Relationship to child, Mother | 92% | 100% | 0.30 |
| No. of children in house | 2.9(1.4) | 2.8 (1.6) | 0.76 |
| No. of adults in house | 1.6 (0.7) | 1.6 (0.7) | 0.86 |
| High school graduate or equivalent | 79% | 54% | 0.05 |
| Employed (full, part, or self-employed) | 66% | 54% | 0.41 |
| Social isolation b | 40% | 61% | 0.14 |
| PACQLQ, total score c | 4.5 (1.3) | 4.3 (0.8) | 0.66 |
| % below federal poverty level d | 28 (14) | 25 (12) | 0.49 |
Data is presented as number (%) and mean (standard deviation). Categorical data were compared using Fisher's exact test; continuous data using analysis of variance.
ED = emergency department, PCP = primary care provide
3 questions regarding # of days with symptoms [a) at any point during day, b) awakening from sleep, and c) interfering with play] that occurred in the week preceding current exacerbation; possible maximum score = 21.
Number of subjects reporting < 7 (median) friends or relatives they feel that they may “talk with” or “ask a favor”.
Pediatric Asthma Caregivers Quality of Life Questionnaire. Juniper et al, Qual Life Res. 1996;5:27–34
Based on address at enrollment and 2000 United States Census Block Group data.
Statistical Analyses
SAS statistical software 9.3 (Cary, North Carolina, US) was used for analysis. Numbers of health care visits are reported with simple descriptive statistics. Generalized linear regression models (GENMOD procedure with a Negative Binomial distribution and log link) were used to examine the associations between visits of different types (AM visits and ED visits, hospitalizations, and PCP acute asthma visits). Considering the possibility of missed AM visits, we examined the association between ED visits and number of PCP visits for any diagnosis, which included AM visits. To examine the impact on venue of acute care, we also explored the difference in relationship between number of AM visits and ED visits and number of AM visits and PCP acute asthma visits. For comparison of characteristics based on having ≥ 6 AM visits, we used Fisher’s exact test for categorical variables, and analysis of variance for continuous variables.
RESULTS
Child and parent characteristics (Table 1)
The children were predominantly early school age and African American race. They had significant asthma symptoms before the index exacerbations. The severity of the index exacerbations is indicated by 20% admission at that visit. Over 50% attended federally-funded clinics. The caregivers were predominantly the children’s’ mothers, had completed high school, and were employed. They had a significantly decreased quality of life (4.5 on a scale of 1–7, with 7 being best). Twenty-eight percent had household incomes below the federal poverty level.
Frequency of Primary Care Provider visits
Over the 3 year study period, the mean number of AM visits per child was 2.5 ± 2.3 (standard deviation (SD)), with a range from 0–10. The mean number of PCP visits for any diagnosis per child was 5.5 ± 6.5 (SD), with a range up to 52. Only 50% of subjects had ≥ 1 PCP visit over the 3 year period that included documentation of any controller medication (inhaled corticosteroid or leukotriene receptor antagonist), whether as a current medication or part of the documented treatment plan. “Only 6% of children had 3 or more visits with documented controller medication over the 3 years. The mean number of PCP acute asthma visits was 0.7 ± 1.6 (SD), with a range from 0–11.
Frequency of hospital-based visits for acute asthma care
The mean number of ED asthma visits per child over 3 years was 3.2 ± 2.8 (SD) with a range from 1–18. The mean number of asthma hospitalizations was 0.6 ± 1.0 (SD) with a range from 0–4.
Relationship between Asthma Monitoring visits and acute asthma visits
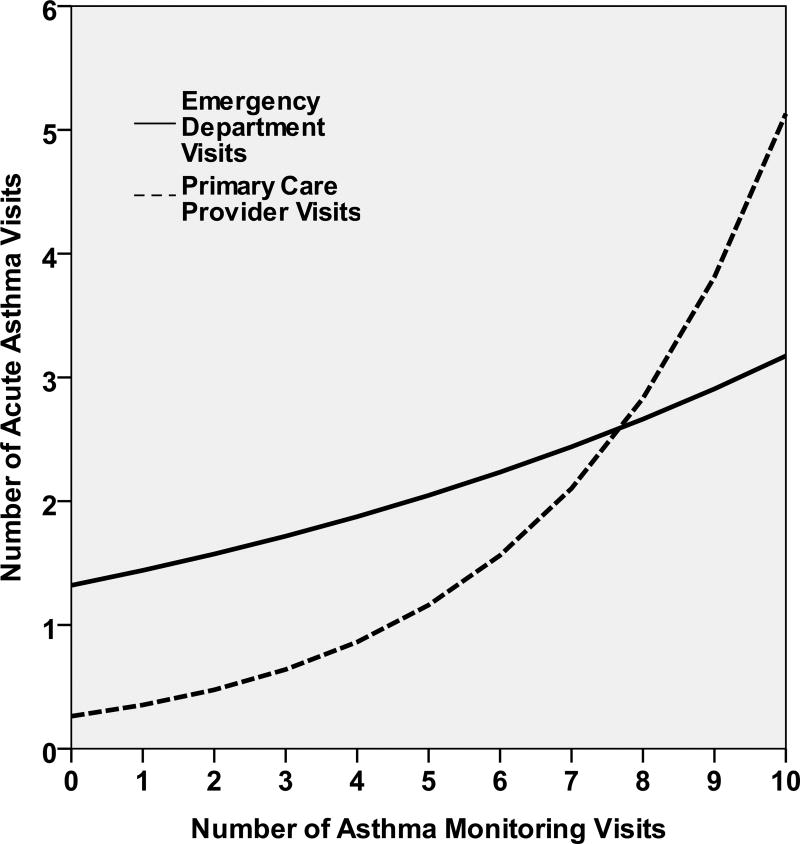
Increasing AM visits was associated with more, not fewer, asthma ED visits. Figure1. In a simple generalized linear model examining the relationship between numbers of AM visits and ED visits, the estimate was 0.088 with a 95% CI of 0.001, 0.174. When this model was adjusted for asthma symptom score and child age, increasing AM visits was not associated with number of ED visits (estimate 0.089; 95% CI −0.001, 0.177). Increasing AM visits was not associated with number of asthma hospitalizations (estimate 0.027; 95% CI −0.12, 0.163). While increasing AM visits was associated both with more PCP acute asthma visits (estimate 0.297; 95% CI 0.166, 0.429) as well as with more ED visits, the slope appears steeper with respect to PCP acute asthma visits. Figure1. Increasing PCP visits for any diagnosis (which included AM visits) was not associated with number of ED visits (estimate 0.021; 95% CI −0.018, 0.060).
Figure 1.
Acute care asthma visits at the Emergency Department and at Primary Care Provider according to number of Asthma Monitoring Visits over 3 Years (n=103)
Characteristics associated with ≥ 6 Asthma Monitoring visits
Only 13% (95% CI 7% to 20%) of our subjects had ≥ 6 AM visits over 3 years. Results of univariate analysis of covariates associated with having ≥ 6 AM visits are listed in Table 2. Children with ≥ 6 AM visits were more likely to be younger and have parents without education beyond high school, and were less likely to be African American. There was no association between having ≥ 6 AM visits and the number of children or adults in the household, income below the federal poverty level, parent age, social isolation, symptom score in the week before the exacerbation leading to the index ED visit, admission to hospital at the index visit, and attending a federally-funded clinic. All children with ≥ 6 AM visits over these 3 years had ≥ 1 PCP visit with a controller medication documented during the 3 years, compared to 43% of children with < 6 AM visits. Overall, only 6% of children had ≥ 3 visits with documentation of controller medication over the 3 years.
DISCUSSION
We examined the association between PCP AM visits and asthma morbidity over time for a population of children with significant asthma risk and impairment. We found that, over a 3 year period, AM visits occurred infrequently; fewer than 20% of the children had 6 or more, while NAEPP guidelines recommend at least 2/year. Furthermore having more AM visits was not associated with fewer acute asthma visits in the ED or at the PCP.
Asthma monitoring visits are recommended as an important part of effective asthma management.[1] These visits are opportunities to assess asthma status and management and to not only prevent, but also prepare for future exacerbations. Ideally such visits would occur consistently over time, not only following acute exacerbations but also when the child was well. However, findings from studies evaluating the effect of AM visits on asthma morbidity have been inconsistent. Interventions that have focused on improved PCP follow-up after ED visits have generally not shown reduction in subsequent ED visits or hospitalizations over the subsequent 6–12 months.[8–10,13] The only publication examining a relationship between the total number of PCP visits for asthma over time and ED visits was by Smith et al., who examined a Medicaid database in Hartford, CT. They found that a greater number of “asthma-related” PCP visits (determined by use of an ICD-9 code 493.xx; and which included visits for monitoring or acute care) seemed to be protective against having ED visits.[11] There are differences between our study and that of Smith et al. to consider. Smith et al. examined a broader patient population including children in the Medicaid database regardless of whether or not they had an ED visit, although the subjects were identified as having persistent asthma; and they included a larger sample size than our study. We focused on children with high asthma morbidity that were users of the ED. In our study we did not use ICD-9 codes to identify asthma visits, but instead, hand audited records and distinguished asthma monitoring from acute asthma visits. Interestingly, in each of the 2 years of their study, Smith et al. found the percentages of children with 3 or more “asthma related PCP visits” were 17.6% and 10.9%, low for children with persistent asthma and similar to our results.[11] Collectively, these results highlight the lack of consistent primary care for many children at risk for asthma morbidity.
We defined AM visits as those with documentation suggesting discussion of asthma management, but acute symptoms were not present. This definition was used to be inclusive of visits during which chronic asthma management was presumed to have been discussed to some degree (e.g., scheduled visits to discuss asthma, ED follow-up visits and well-child visits with asthma documented as a problem) and allowed distinction from acute asthma visits. Even with this broad definition of AM visits, they occurred infrequently, less than once per year on average for most children. Acknowledging the possibility of classification bias for the AM visits, we also analyzed the data including all PCP visits for any diagnosis, and still found no decrease in ED visits if PCP visits for any reason or diagnosis increased. It is possible that more AM visits was not associated with fewer acute asthma visits because of insufficient chronic care that lacked controller therapy, parental misunderstanding of the disease process, non-adherence to appropriate treatment plan, or parental stress driving parents to seek help everywhere. It is also possible that AM visits in our sample occurred at a rate too low to see an effect on ED visits even if these PCP visits were of high quality. However, based on the high asthma impairment and risk demonstrated in our study population, it is likely that these families would require more frequent AM visits to support effective chronic disease management. Strategies to augment the patient-PCP relationship are important considerations for this population. As an alternative strategy, some investigators have examined the impact of models that provide chronic asthma care outside of the PCP. Community-based approaches have been studied, and, while some have been successful in improving outcomes, not all attempts have had equal success.[25] In Washington, DC, an ED-based asthma follow-up clinic has been associated with some improved outcomes.[26]
We found that the proportion of children with ≥ 6 AM visits over 3 years was quite low, and this limited our power to detect significant differences from those with < 6 visits. However, we analyzed for distinguishing features that might provide ideas for future research. Younger children, those of non-African-American race, and those with parents who did not report education beyond high school were more likely to have ≥ 6 AM visits. It may be that these younger children had more severe disease or disease that more rapidly progressed to a level needing acute care, however adjustment of the generalized linear model for child age and asthma symptom score at presentation did not change the relationship. It may also be that parents with lower levels of education did not have plans in place to prevent progression of symptoms so that acute care was not needed. No other characteristics of parents, families, and children, including attendance at a federally funded clinic suggested distinguishing characteristics for children/families that had more AM visits. Documentation of asthma controller medications was one of the study definitions for AM visits, and, therefore, more frequent for children with ≥ 6 AM visits. However, only 50% had 1 or more visits with a controller medication documented. In fact, only 6% of children had ≥ 3 visits with documentation of controller medication over the 3 years. It is possible that use of controller medication was more commonly encouraged for children with ≥ 6 AM visits and may have occurred during all PCP visits (for any diagnosis) but was not documented. However, children with more PCP visits for any diagnosis did not have reduced morbidity, suggesting that prescription of asthma medications did not occur at PCP visits for reasons other than asthma. There were a large number of PCPs used by patients in this study. We did not control for clustering of PCP and have no information about prescribing patterns of the individual PCPs, a limitation of the study. Other studies of nationally representative samples of children with asthma have also found low rates of asthma controller medication use.[27, 28] Characteristics such as parental employment, and number of children or adults in the household, often thought to reflect competing priorities that might interfere with effective acute and chronic asthma care were similar whether or not ≥ 6 AM visits occurred.
We also examined the venue of acute care (ED or PCP). Interestingly, increasing AM visits was associated both with more ED visits and with more PCP visits for acute asthma. This suggests that those with more AM visits may not only have more exacerbations but may be more likely to seek acute care at their PCP, perhaps indicating an ongoing relationship or partnership with their PCP. This was also suggested in the study by Smith et al, in their finding that 3 or more PCP asthma visits was associated with lower odds of an ED. Unfortunately we do not have data to determine if this pattern of behavior reflects a stronger collaborative relationship with the PCP or simply increased severity of their asthma or other co-morbid acute conditions.
There are other limitations of our study not yet mentioned. We enrolled a convenience cohort of children with asthma and had a relatively small sample size which limits the power of the analysis and generalizability of results. However, our population is an important group to study, as these urban Medicaid insured children with high asthma morbidity are clearly in need of better outcomes. Further, we do not have objective information on controller medication use even when prescribed. We also did not assess details of parent-physician interactions, including shared decision-making and parent or PCP perception of the frequency or quality of partnership in care. Non-documented dialogue about asthma care may have occurred during other visits leading to underestimated frequency of AM visits, although we think this unlikely. We measured ED visits and hospitalizations at one hospital, and our city has another children's hospital with an ED. While it is possible that children had visits at this other hospital, data from another study in this city suggest this rate is <5% for users of our hospital.[29] We also did not measure outcomes besides ED visits and hospitalizations, which may be positively affected by AM visits with the PCP and of interest in future studies.
Strengths of this study are the prospective enrollment and hand audit of visit records instead of review simply by visit codes or billing data as must be done in a large database. Determination of AM visits was based on review of documentation within visit records that suggested asthma management was discussed.
Conclusion
In conclusion, AM visits at PCPs and documented controller medication for these urban Medicaid-insured children occurred infrequently over a 3 year period. More frequent AM visits was not associated with fewer ED visits or fewer PCP visits for acute asthma, and number AM visit rates were not aligned with guideline recommendations for most of these children. These results highlight the need for asthma interventions that facilitate an ongoing partnership between provider and patient and enable regular monitoring of the child’s asthma control and exacerbation history, with treatment adjustment as needed.
Acknowledgments
This study was funded by a grant from the National Heart Lung Blood Institute (HL 072919).
Footnotes
Declaration of Interest
The authors report no conflicts of interest.
References
- 1.National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the diagnosis and management of asthma - summary report 2007. J Allergy Clin Immunol. 2007;120:S94–138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 2.Miller JE. The effects of race/ethnicity and income on early childhood asthma prevalence and health care use. Am J Public Health. 2000;90:428–430. doi: 10.2105/ajph.90.3.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akinbami L. Centers for Disease Control and Prevention National Center for Health Statistics. The state of childhood asthma, United States, 1980–2005. Adv Data. 2006;381:1–24. [PubMed] [Google Scholar]
- 4.Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980–2007. Pediatrics. 2009;123(suppl 3):S131–S145. doi: 10.1542/peds.2008-2233C. [DOI] [PubMed] [Google Scholar]
- 5.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005–2009. Natl Health Stat Report. 2011;12(32):1–14. [PubMed] [Google Scholar]
- 6.Leickly FE, Wade SL, Crain E, et al. Self-reported adherence, management behavior, and barriers to care after an emergency department visit by inner city children with asthma. Pediatrics. 1998;101(5):1–8. doi: 10.1542/peds.101.5.e8. [DOI] [PubMed] [Google Scholar]
- 7.Petersen DL, Murphy DE, Jaffe DM, et al. A tool to organize instructions at discharge after treatment of asthmatic children in an emergency department. J Asthma. 1999;36(7):597–603. doi: 10.3109/02770909909087297. [DOI] [PubMed] [Google Scholar]
- 8.Zorc JJ, Scarfone RJ, Li Y, et al. Scheduled follow-up after a pediatric emergency department visit for asthma: a randomized trial. Pediatrics. 2003;111:495–502. doi: 10.1542/peds.111.3.495. [DOI] [PubMed] [Google Scholar]
- 9.Cabana MD, Bruckman D, Bratton SL, Kemper AR, Clark NM. Association between outpatient follow-up and pediatric emergency department asthma visits. J Asthma. 2003;40:741–749. doi: 10.1081/jas-120023499. [DOI] [PubMed] [Google Scholar]
- 10.Smith SR, Jaffe DM, Fisher EB, Trinkaus KM, Highstein G, Strunk RC. Improving follow-up for children with asthma after an acute emergency department visit. J Pediatr. 2004;145:772–777. doi: 10.1016/j.jpeds.2004.08.029. [DOI] [PubMed] [Google Scholar]
- 11.Smith SR, Wakefield DB, Cloutier MM. Relationship between pediatric primary provider visits and acute asthma ED visits. Pediatr Pulmonol. 2007;42:1041–1047. doi: 10.1002/ppul.20694. [DOI] [PubMed] [Google Scholar]
- 12.Nelson KA, Highstein G, Garbutt J, et al. A randomized controlled trial of parental asthma coaching to improve outcomes in urban minority children. Arch Pediatr Adolesc Med. 2011;165(6):520–526. doi: 10.1001/archpediatrics.2011.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li p, To T, Guttmann A. Follow-up care after an emergency department visit for asthma and subsequent healthcare utilization in a universal-access healthcare system. J Pediatr. 2012;161(2):208–13. doi: 10.1016/j.jpeds.2012.02.038. [DOI] [PubMed] [Google Scholar]
- 14.Liberman DB, Shelef DQ, Hi J, McCarter R, Teach SJ. Low rates of follow-up with primary care providers after pediatric emergency department visits for respiratory tract illnesses. Pediatr Emer Care. 2012;28:756–861. doi: 10.1097/PEC.0b013e31826c6dde. [DOI] [PubMed] [Google Scholar]
- 15.Schatz M, Rachelefsky G, Krishnan JA. Follow-up after acute asthma episodes: what improves future outcomes? J Allerg Clin Immunol. 2009;124:S35–S42. doi: 10.1016/j.jaci.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 16.Yee AB, Fagnano M, Halterman JS. Preventive asthma care delivery in the primary care office: missed opportunities for children with persistent asthma symptoms. Acad Pediatr. 2013;13:98–104. doi: 10.1016/j.acap.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Butz AM, Riekert KA, Eggleston P, Winkelstein M, Thompson RE, Rand C. Factors associated with preventive asthma care in inner-city children. Clin Pediatr. 2004;43:709–719. doi: 10.1177/000992280404300804. [DOI] [PubMed] [Google Scholar]
- 18.Halterman JS, Yoos HL, Sidora K, et al. Medication use and health care contacts among symptomatic children with asthma. Ambul Pediatr. 2001;1:275–279. doi: 10.1367/1539-4409(2001)001<0275:muahcc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 19.Halfon N, Newacheck PW. Childhood asthma and poverty: differential impacts and utilization of health services. Pediatrics. 1993;91:56–61. [PubMed] [Google Scholar]
- 20.Bartlett SJ, Kolodner K, Butz AM, et al. Maternal depressive symptoms and emergency department use among inner-city children with asthma. Arch Pediatr Adolesc Med. 2001;155:347–353. doi: 10.1001/archpedi.155.3.347. [DOI] [PubMed] [Google Scholar]
- 21.Eisner MD, Ackerson LM, Chi F, et al. Health-related quality of life and future health care utlization for asthma. Ann Allergy Asthma Immunol. 2002;89:46–55. doi: 10.1016/S1081-1206(10)61910-2. [DOI] [PubMed] [Google Scholar]
- 22.Fisher EB, Strunk RC, Sussman LK, Sykes RK, Walker MS. Community organization to reduce the need for acute care for asthma among African American children in low-income neighborhoods: the Neighborhood Asthma Coalition. Pediatrics. 2004;114(1):116–123. doi: 10.1542/peds.114.1.116. [DOI] [PubMed] [Google Scholar]
- 23.Fisher E, Strunk R, Sussman L, et al. Acceptability and feasibility of a community approach to asthma management: the Neighborhood Asthma Coalition (NAC) J Asthma. 1996;33:367–383. doi: 10.3109/02770909609068182. [DOI] [PubMed] [Google Scholar]
- 24.Juniper EF, Guyatt GH, Feeny DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in the parents of children with asthma. Qual Life Res. 1996;5:27–34. doi: 10.1007/BF00435966. [DOI] [PubMed] [Google Scholar]
- 25.Clark NM. Community-based approaches to controlling asthma. Annu Rev Pub Hlth. 2012;33:193–208. doi: 10.1146/annurev-publhealth-031811-124532. [DOI] [PubMed] [Google Scholar]
- 26.Teach SJ, Crain EF, Quint DM, et al. Improved asthma outcomes in a high-morbidity pediatric population: results of an emergency department-based randomized clinical trial. Arch Pediatr Adolesc Med. 2006;160(5):535–541. doi: 10.1001/archpedi.160.5.535. [DOI] [PubMed] [Google Scholar]
- 27.Mangione-Smith R, DeCristofaro AH, Setodji CM, et al. The quality of ambulatory care delivered to children in the United States. NEJM. 2007;357:1515–1523. doi: 10.1056/NEJMsa064637. [DOI] [PubMed] [Google Scholar]
- 28.Kit BK, Simon AE, Ogden CL, et al. Trends in preventive asthma medication use among children and adolescents, 1988-2008. Pediatrics. 2012;129(1):62–69. doi: 10.1542/peds.2011-1513. [DOI] [PubMed] [Google Scholar]
- 29.Bloomberg GR, Goodman G, Fisher EB, Jr, Strunk RC. The profile of single admissions and readmissions for childhood asthma over a six year period at St. Louis children’s Hospital [abstract] JACI. 1997;99(1 part 2):S69. [Google Scholar]