Abstract
BACKGROUND
Despite significant progress in primary prevention, the rate of MI has not declined in young adults.
OBJECTIVES
The purpose of this study was to evaluate statin eligibility based on the 2013 American College of Cardiology/American Heart Association guidelines for treatment of blood cholesterol and 2016 U.S. Preventive Services Task Force recommendations for statin use in primary prevention in a cohort of adults who experienced a first-time myocardial infarction (MI) at a young age.
METHODS
The YOUNG-MI registry is a retrospective cohort from 2 large academic centers, which includes patients who experienced an MI at age ≤50 years. Diagnosis of type 1 MI was adjudicated by study physicians. Pooled cohort risk equations were used to estimate atherosclerotic cardiovascular disease risk score based on data available prior to MI or at the time of presentation.
RESULTS
Of 1,685 patients meeting inclusion criteria, 210 (12.5%) were on statin therapy prior to MI and were excluded. Among the remaining 1,475 individuals, the median age was 45 years, there were 294 (20%) women, and 846 (57%) had ST-segment elevation MI. At least 1 cardiovascular risk factor was present in 1,225 (83%) patients. The median 10-year atherosclerotic cardiovascular disease risk score of the cohort was 4.8% (interquartile range: 2.8% to 8.0%). Only 724 (49%) and 430 (29%) would have met criteria for statin eligibility per the 2013 American College of Cardiology/American Heart Association guidelines and 2016 U.S. Preventive Services Task Force recommendations, respectively. This finding was even more pronounced in women, in whom 184 (63%) were not eligible for statins by either guideline, compared with 549 (46%) men (p < 0.001).
CONCLUSIONS
The vast majority of adults who present with an MI at a young age would not have met current guideline-based treatment thresholds for statin therapy prior to their MI. These findings highlight the need for better risk assessment tools among young adults.
Keywords: myocardial infarction, prevention, risk, statin, young adults
Significant progress in prevention of coronary artery disease (CAD) has led to a decrease in the incidence of myocardial infarction (MI) (1). However, recent reports highlight that the reduction in the rate of MI has not extended to young adults, and young women in particular continue to have worse cardiovascular outcomes than men (2,3).
Identifying individuals who are at risk for cardiovascular events is paramount, as such individuals can be targeted for more aggressive primary prevention efforts (4). Nevertheless, predicting risk in young adults is challenging, and most risk calculators fail to identify susceptible young adults as high risk. For instance, a prior study applied the National Cholesterol Education Program (NCEP) III guidelines (5) to a group of young adults with MI and reported that only 25% would have been eligible for statin therapy prior to their MI (6).
However, risk prediction has evolved considerably, and the 2013 American College of Cardiology/American Heart Association (ACC/AHA) guidelines for cholesterol lowering (7) and 2016 U.S. Preventive Services Task Force (USPSTF) recommendations for primary prevention statin use (8) have significantly expanded the number of individuals who are candidates for statin therapy (9).
The underestimation of cardiovascular risk among young individuals and the subsequent lost opportunity to prevent events is concerning, given the disparity in reducing the rate of MI in this population (3). Therefore, we sought to determine how contemporary guidelines perform in identifying the need for statin therapy among a cohort of men and women who experienced a first-time MI at a young age. In addition, within this cohort, we evaluated the prevalence of major cardiovascular risk factors to determine their utility in enhancing the identification of at-risk young individuals.
METHODS
STUDY POPULATION
The design of the YOUNG-MI registry has been previously described (10). In brief, this is a retrospective cohort study from 2 large academic medical centers (Brigham and Women’s Hospital and Massachusetts General Hospital), which included patients who experienced an MI at or before 50 years of age between 2000 and 2016. All records were adjudicated by a team of study physicians, as previously described (10), using the Third Universal Definition of MI (11). For the present analysis, only patients with type 1 MI were included. Individuals with known CAD (defined as prior MI or revascularization) were excluded. Individuals were also excluded if they had missing values for lipid profiles or systolic blood pressure, which are necessary components for the pooled cohort equations (PCE) for estimation of cardiovascular risk, and hence, determination of statin eligibility (12). Online Figure 1 provides a consort diagram of the study population.
RISK FACTORS
The presence of cardiovascular risk factors was ascertained by a detailed review of electronic medical records during or before the index admission. For each risk factor, we also determined whether it was known prior to admission or diagnosed during hospitalization. Diabetes was defined as fasting plasma glucose >126 mg/dl or hemoglobin A1c ≥6.5% or diagnosis/treatment for diabetes. Hypertension was defined as a systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or diagnosis/treatment of hypertension. Dyslipidemia was defined as total cholesterol ≥240 mg/dl, serum triglycerides ≥150 mg/dl, high-density lipoprotein cholesterol <40 mg/dl in men or <50 mg/dl in women, or diagnosis/treatment of dyslipidemia. Obesity was defined as a body mass index ≥30 kg/m2 or a diagnosis of obesity. Smoking was defined as current (tobacco products used within the last month), former, or never. Family history of premature CAD, defined as fatal MI, nonfatal MI, or coronary revascularization occurring before 55 years of age for first-degree male family members and before 65 years of age for first-degree female family members, was captured by a thorough review of the electronic medical records, which included all clinic notes prior to admission, admission history and physical, discharge summaries, and follow-up visit notes.
ASSESSMENT OF CARDIOVASCULAR RISK
To determine whether each individual would qualify for statin therapy prior to his or her MI, we calculated the atherosclerotic cardiovascular disease (ASCVD) risk score based on data available prior to MI or at time of presentation using the PCE. For individuals younger than 40 years of age at presentation, an age of 40 was assigned, as PCE are only applicable to individuals age 40 to 79 years. For those with a triglyceride level >400 mg/dl, the method described by Martin et al. (13) was used to estimate low-density lipoprotein (LDL) cholesterol, as this method has been shown to be more accurate compared with the Friedewald equation in such scenarios. Risk factors that were diagnosed during the index hospitalization for MI were not used for calculating the risk scores, as the intent of our study was to evaluate how many patients would have met criteria for statin therapy prior to presentation.
In addition to the ASCVD 10-year risk, we also estimated the lifetime cardiovascular risk based on the burden of traditional risk factors (14). The criteria used to define each risk category are provided in Online Table 1. The cohort was also divided into a low lifetime risk group (lifetime risk <39%) and high lifetime risk group (lifetime risk ≥39%), based on thresholds established in prior studies (15).
STATIN ELIGIBILITY
The 2013 ACC/AHA guidelines (7) and the 2016 USPSTF recommendations (8) were used to assess statin eligibility. Individuals were considered to be statin eligible if guidelines indicated that statins are recommended or statins are considered. Although our goal was to evaluate contemporary statin guidelines, we also assessed statin eligibility according to the older NCEP III guidelines (5). Specific criteria that were followed for each guideline are detailed in Online Table 2.
DATA MANAGEMENT
Study-related data for all patients who met inclusion criteria were stored on our customized secure electronic adjudication system and REDCap. REDCap is an encrypted, secure, Health Insurance Portability and Accountability Act–compliant web platform for electronic data capture and serves as an intuitive interface to enter data with real-time validation (16). The YOUNG-MI registry has been approved by the Institutional Review Board at Partners HealthCare.
STATISTICAL ANALYSIS
Categorical variables are reported as frequencies and proportions, and were compared with the chi-square or Fisher exact test, as appropriate. Continuous variables are reported as means or medians and compared with the Student’s t-test or the Mann-Whitney U test, as appropriate.
To determine how the ASCVD risk score or the 2013 ACC/AHA guidelines can be enhanced to identify more individuals prior to their MI, we reclassified all statin-ineligible individuals with LDL cholesterol ≥160 mg/dl or family history of premature cardiovascular disease to statin considered, as these criteria were offered by the guidelines as additional factors that may influence ASCVD risk (7).
Because most patients did not have any available data on lipid values prior to their MI, and because lipid levels can decrease at the time of MI, we performed 2 separate sensitivity analyses to determine the potential effect of using lipid values obtained at the time of MI. First, we performed a sensitivity analysis that only included patients who had available cholesterol measurements prior to their MI. Second, we performed a separate sensitivity analysis where we increased the total cholesterol level of all patients who did not have prior cholesterol values by 12%. This was based on the observed decrease in total cholesterol in our cohort among patients who had measurements of total cholesterol prior to their MI and upon admission. Because blood pressure during hospitalization for MI can be labile, we also performed a sensitivity analysis that only included patients who had available blood pressure measurements prior to their MI. A 2-sided p value <0.05 was considered significant. All analyses were performed using Stata version 14.2 (StataCorp, College Station, Texas).
RESULTS
BASELINE CHARACTERISTICS
The cohort consisted of 1,685 patients who met inclusion criteria, of whom 210 (12.5%) were on statin therapy prior to MI. These patients were excluded from all subsequent analyses. The remaining cohort consisted of 1,475 individuals with a median age of 45 years, of whom 294 (20%) were women and 1,060 (72%) were white. There were 255 patients (17.3%) under the age of 40 years at the time of the MI (range 19 to 39 years). Other baseline characteristics are provided in Table 1.
TABLE 1.
Baseline Characteristics (N = 1,475)
| Age at time of MI, yrs | 45 (41–48) |
|
| |
| Female | 294 (19.9) |
|
| |
| White | 1,060 (71.9) |
|
| |
| ST-segment elevation myocardial infarction | 846 (57.4) |
|
| |
| Diabetes | 246 (16.7) |
|
| |
| Hypertension | 649 (44.0) |
|
| |
| Dyslipidemia | 818 (55.5) |
|
| |
| Current smoking | 772 (52.3) |
|
| |
| Former smoker | 196 (13.2) |
|
| |
| Premature CAD in first-degree relative | 424 (28.7) |
|
| |
| Obesity | 437 (29.6) |
|
| |
| Total cholesterol, mg/dl | 191.3 ± 55.9 |
|
| |
| HDL cholesterol, mg/dl | 37.0 ± 10.6 |
|
| |
| LDL cholesterol, mg/dl | 118.4 ± 45.9 |
|
| |
| Triglycerides, mg/dl | 145 (101–17) |
|
| |
| ASCVD score | 4.8 (2.8–8.0) |
|
| |
| ASCVD risk score | |
| <5% | 770 (52.2) |
| 5–7.5% | 298 (20.2) |
| 7.5–20% | 365 (24.7) |
| >20% | 42 (2.8) |
|
| |
| Recommended/considered for statin therapy by 2013 ACC/AHA | 724 (49.1) |
|
| |
| Recommended/considered for statin therapy by 2016 USPSTF | 430 (29.2) |
|
| |
| Recommended/considered for statin therapy by either guideline | 742 (50.3) |
|
| |
| Recommended/considered for statin therapy by NCEP III | 507 (34.4) |
Values are median (interquartile range), n (%), or mean ± SD.
ACC/AHA = American College of Cardiology/American Heart Association; ASCVD = atherosclerotic cardiovascular disease; CAD = coronary artery disease; HDL = high-density lipoprotein; LDL = low-density lipoprotein; MI = myocardial infarction; NCEP = National Cholesterol Education Panel; USPSTF = U.S. Preventive Services Task Force.
PREVALENCE AND AWARENESS OF RISK FACTORS
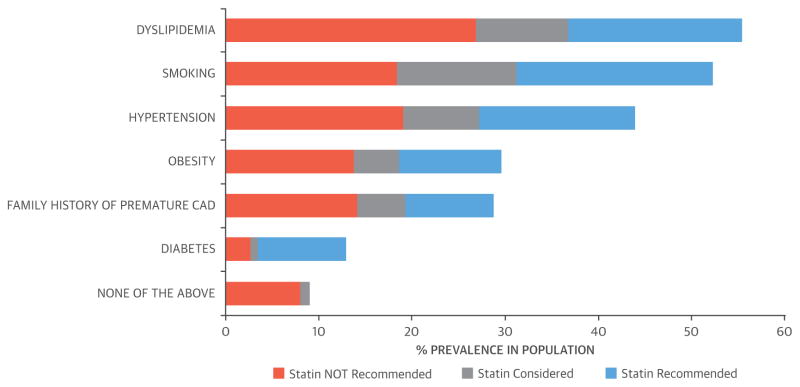
When examining the prevalence of risk factors, 1,225 (83%) patients had at least 1 of the following: diabetes, dyslipidemia, hypertension, or smoking. Dyslipidemia was the most common risk factor, which was present in 818 (55%) patients, followed by smoking in 772 (52%) and hypertension in 649 (44%). Figure 1 shows the distribution of the most common risk factors within our cohort, stratified by the proportion of patients in whom statins are recommended, considered, or not recommended by the 2013 ACC/AHA guideline.
FIGURE 1. Prevalence of Cardiovascular Risk Factors Stratified by Statin Eligibility.
Distribution of the most common risk factors within our cohort, stratified by the proportion of patients who are recommended (blue), considered (gray), or not recommended (orange) to use statins by the 2013 American College of Cardiology/American Heart Association guidelines. CAD = coronary artery disease.
Among the patients with dyslipidemia, 163 of 818 (20%) had no prior history of this condition and were first diagnosed during the index hospitalization for MI. Similarly, diabetes and hypertension were first diagnosed in 55 of 246 (22%) and 61 of 649 (9%) patients, respectively. When considering the 3 major cardiovascular risk factors proposed by the USPSTF—namely, diabetes, dyslipidemia, and hypertension, 226 (21%) of 1,069 patients were unaware of having at least 1 of these risk factors.
CARDIOVASCULAR RISK AND STATIN ELIGIBILITY
The median ASCVD risk score of the population was 4.8% (interquartile range: 2.8% to 8%), with 1,068 (72%) having an ASCVD risk score of <7.5%. When considering the lifetime cardiovascular risk of the population, 1,184 (80.3%) were at high risk (Figure 2). Online Figure 2 provides detailed risk factor burden and lifetime risk estimates stratified by sex.
FIGURE 2. Lifetime Cardiovascular Risk.
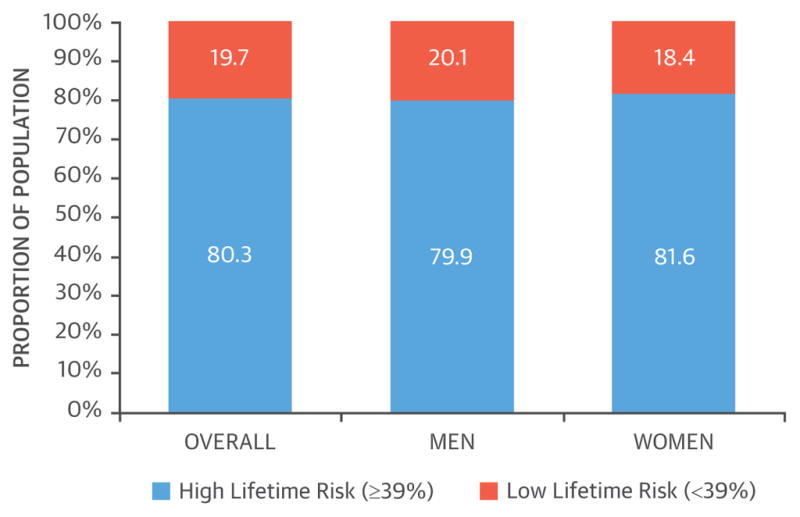
Proportion of patients with high lifetime cardiovascular risk (≥39%) among young adults with myocardial infarction.
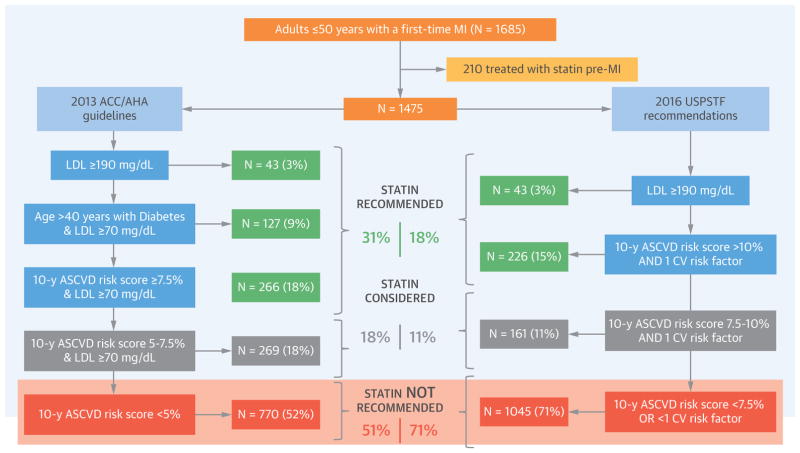
When applying the 2013 ACC/AHA guideline, only 455 (31%) would have met criteria for initiation of statin therapy prior to their MI, an additional 269 (18%) would have met criteria for consideration of statin therapy, and the remaining 751 (51%) would not have been eligible for primary prevention statin therapy (Central Illustration).
CENTRAL ILLUSTRATION. Guideline-Based Statin Eligibility of Young Adults Prior to MI.
Contemporary statin guidelines were applied to 1,475 young adults not on statins prior to myocardial infarction. (Left) The stepwise implementation of the 2013 American College of Cardiology/American Heart Association cholesterol guidelines. (Right) The stepwise implementation of the 2016 United States Preventive Services Task Force statin recommendations. The cohort is stratified by statin eligibility according to specified guideline criteria into 3 groups: statin recommended (green), statin considered (gray), and statin not recommended (orange). The risk factors considered by USPSTF guidelines include diabetes, hypertension, dyslipidemia, and smoking. ACC/AHA = American College of Cardiology/American Heart Association; ASCVD = atherosclerotic cardiovascular disease; CV = cardiovascular; LDL = low-density lipoprotein; MI = myocardial infarction; USPSTF = U.S. Preventive Services Task Force.
When applying the 2016 USPSTF recommendations, only 269 (18%) would have met criteria for initiating statin therapy, an additional 161 (11%) would have met criteria for consideration of statin therapy, and the remaining 1,045 (71%) would not have been eligible for statin therapy (Central Illustration).
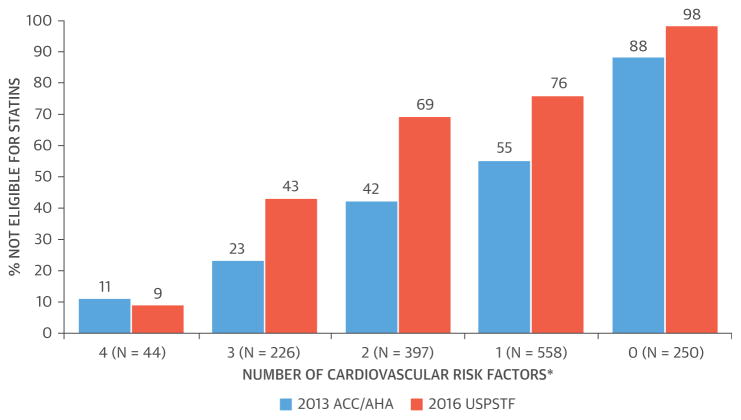
When applying both the 2013 ACC/AHA and the 2016 USPSTF recommendations to our entire study population, only 742 (50%) patients would have been categorized as statin eligible—that is, categorized as statin recommended or statin considered by either guideline—prior to their MI. Furthermore, 23% (52 of 226) and 43% (98 of 226) of patients with at least 3 of the following risk factors—diabetes, hypertension, dyslipidemia, and smoking—would not have been eligible for statin therapy according to the 2013 ACC/AHA guidelines and 2016 USPSTF recommendations, respectively (Figure 3).
FIGURE 3. Burden of Risk Factors and Statin Ineligibility.
Proportion of patients not eligible for statin therapy stratified by cumulative burden of cardiovascular risk factors by 2013 ACC/AHA (blue) and 2016 USPSTF (orange) recommendations. *Cardiovascular risk factors considered include diabetes, hypertension, dyslipidemia, and smoking. ACC/AHA = American College of Cardiology/American Heart Association; USPSTF = U.S. Preventive Services Task Force.
The number of patients in which the variables required for calculating the ASCVD risk score were available pre-presentation are provided in Online Table 3. When we increased the total cholesterol of all patients without prior lipid values, we observed a similar proportion eligible for statin therapy (56% by 2013 ACC/AHA and 34% by 2016 USPSTF) (Online Table 4). When we limited our analyses to patients who had available cholesterol levels prior to their MI, we observed that a greater proportion of these patients were eligible for statins compared with the overall study population (63% vs. 48% by 2013 ACC/AHA) (Online Table 5). This was driven by the fact that this group had more risk factors, including a higher prevalence of diabetes and hypertension, than those who did not have lipid values obtained prior to their MI (Online Table 6). When we limited our analysis to patients who had available blood pressure measurements prior to MI, there was no significant difference in statin eligibility (Online Table 7).
We also evaluated the NCEP III guidelines, according to which 347 (23%) patients would have met criteria for initiating statin therapy, 160 (11%) would have met criteria for consideration of statin therapy, and the remaining 968 (66%) would not have been eligible for statin therapy (Online Table 8). Figure 4 depicts the proportion of statin eligibility and the overlap between the 3 guidelines.
FIGURE 4. Statin Eligibility of Young Adults Prior to Myocardial Infarction by Various Guidelines.
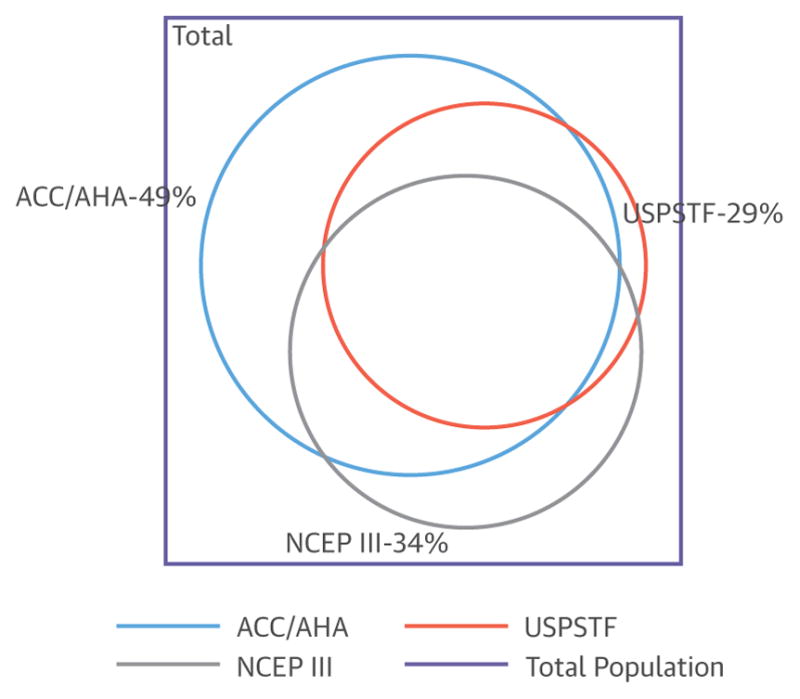
The square represents the total population (n = 1,475) of patients who experienced a myocardial infarction at a young age. The colored circles represent the proportion of statin eligible (statins considered/statin recommended) individuals. The size is directly proportional to magnitude of statin eligibility, with the 2013 ACC/AHA guidelines (blue), 2016 USPSTF recommendations (orange), and NCEP III guidelines (gray). Overlap between circles represents individuals that were eligible by multiple respective guidelines. NCEP = National Cholesterol Education Panel; other abbreviations as in Figure 3.
SEX DIFFERENCES
When considering the prevalence of risk factors by sex, there were significant differences. When compared with men, women had a lower prevalence of hyperlipidemia (30% vs. 59%; p < 0.001), as well as lower total cholesterol, LDL cholesterol, and triglycerides, but higher high-density lipoprotein cholesterol. Women also had a higher prevalence of obesity (37% vs. 28%; p = 0.003) and a trend toward a higher prevalence of smoking (57% vs. 51%; p = 0.068). The median ASCVD risk score was significantly lower in women (3.2 vs. 5.2; p < 0.001), and 244 (83%) women had an ASCVD score of <7.5% compared with 824 (70%) men (p < 0.001) (Table 2).
TABLE 2.
Sex Differences
| Male (n = 1,181, 80%) | Female (n = 294, 20%) | p Value | |
|---|---|---|---|
| Age at time of MI, yrs | 45 (41–48) | 46 (42–48) | 0.24 |
|
| |||
| White | 856 (72.5) | 204 (69.4) | 0.31 |
|
| |||
| Diabetes | 190 (16.1) | 56 (19.0) | 0.22 |
|
| |||
| Hypertension | 517 (43.8) | 132 (44.9) | 0.74 |
|
| |||
| Hyperlipidemia | 702 (59.4) | 116 (39.5) | <0.001 |
|
| |||
| Current smoking | 604 (51.1) | 168 (57.1) | 0.068 |
|
| |||
| Former smoker | 167 (28.9) | 29 (23.0) | 0.19 |
|
| |||
| Premature CAD in first-degree relative | 334 (28.3) | 90 (30.6) | 0.43 |
|
| |||
| Obesity | 329 (27.9) | 108 (36.7) | 0.003 |
|
| |||
| Total cholesterol, mg/dl | 193.1 ± 57.0 | 184.1 ± 50.9 | 0.014 |
|
| |||
| HDL cholesterol, mg/dl | 36.1 ± 9.5 | 40.9 ± 13.8 | <0.001 |
|
| |||
| LDL cholesterol, mg/dl | 119.8 ± 45.9 | 112.8 ± 45.6 | 0.02 |
|
| |||
| Triglycerides, mg/dl | 153 (104–230) | 122 (86–177) | <0.001 |
|
| |||
| ASCVD score | 5.2 (3.2–8.5) | 3.2 (1.2–6.0) | <0.001 |
|
| |||
| ASCVD risk group | |||
| <5% | 571 (48.3) | 199 (67.7) | <0.001 |
| 5.0–7.5% | 253 (21.4) | 45 (15.3) | |
| 7.5–20.0% | 326 (27.6) | 39 (13.3) | |
| >20% | 31 (2.6) | 11 (3.7) | |
|
| |||
| Recommended/considered for statin therapy by 2013 ACC/AHA | 603 (51.1) | 102 (34.7) | <0.001 |
|
| |||
| Recommended/considered for statin therapy by 2016 USPSTF | 377 (31.9) | 53 (18.0) | <0.001 |
|
| |||
| Recommended/considered for statin therapy by either guideline | 632 (53.5) | 110 (37.4) | <0.001 |
|
| |||
| Recommended/considered for statin therapy by NCEP III guidelines | 378 (32.0) | 129 (43.9) | <0.001 |
Values are median (interquartile range), n (%), or mean ± SD.
Abbreviations as in Table 1.
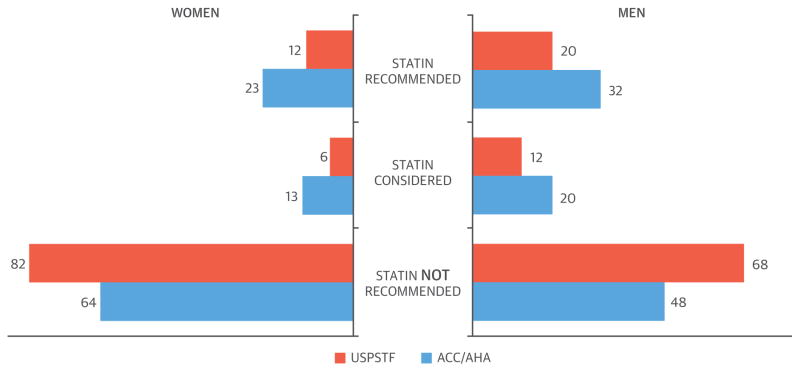
When applying the 2013 ACC/AHA guidelines, over 64% of women would not have been eligible for statin therapy compared with 49% of men (p < 0.001) (Figure 5). When applying the USPSTF recommendations, 82% of women would not have been eligible compared with 68% of men (p = 0.002). Overall, only 37% of women would have been eligible for statin therapy by either the 2013 ACC/AHA or USPSTF guidelines compared with 54% of men (p < 0.001) (Table 2).
FIGURE 5. Sex Differences in Statin Eligibility.
Classification of statin eligibility by the 2013 ACC/AHA guidelines (blue) and 2016 USPSTF recommendations (orange) for women (left) and men (right). Abbreviations as in Figure 3.
ENHANCEMENT OF STATIN ELIGIBILITY
We estimated the effect of modifying the risk prediction and incorporating additional risk factors to increase statin eligibility; these are provided in the Online Appendix and Online Figure 3.
DISCUSSION
To the best of our knowledge, this study is the first to apply the 2013 ACC/AHA cholesterol guidelines and 2016 USPSTF primary prevention recommendations for statin therapy to a large cohort of adults who experienced an MI at a young age, and is 1 of the largest to look at distributions of risk factors prior to MI among adults under the age of 50 years. We found that despite the expanded use of statins advocated by these recommendations (9,17), current guidelines did not identify most young adults who experienced an MI to be eligible for statins at the time of or prior to their event. In our study, 51% of subjects would not have been eligible for statin therapy prior to their MI if the 2013 ACC/AHA guidelines were implemented, and 71% would not have been eligible by the 2016 USPSTF recommendations. Our findings were more striking in women, where only 36% and 18% were determined to be eligible by the 2013 ACC/AHA guidelines and 2016 USPSTF recommendations, respectively. It is notable that the underestimation of risk in this cohort exists despite the high prevalence of traditional cardiovascular risk factors (with 4 of every 5 patients having at least 1 major cardiovascular risk factor). Furthermore, in calculating the ASCVD risk score, we conservatively increased the minimum age to 40 years, and reclassified all patients in the statin considered category (i.e., ASCVD risk score of 5% to 7.5%) as statin eligible, as has been suggested by others as a method for improving the applicability of these criteria to young adults (18).
RISK PREDICTION IN YOUNG ADULTS
In 2002, Akosah et al. (6) evaluated the statin eligibility of 222 “young adults” (men age ≤55 years and women age ≤65 years) hospitalized for MI using the then current NCEP III guidelines, and found that 82% of women and 59% of men did not meet thresholds for pharmacotherapy prior to their MI, despite a high prevalence of cardiovascular risk factors, particularly among women. The authors concluded that there is a need for better risk prediction in young adults. Although various guidelines have subsequently been developed, no studies have been performed applying the various proposed criteria to young adults. When applied to other populations, the ASCVD risk calculator based on the PCE has been shown to overestimate risk (19–21); however, our findings suggest that this risk score, which is highly dependent on age (19,22), also has the potential to underestimate risk in younger individuals. Although the 2016 USPSTF recommendations and 2001 NCEP III guidelines each identify a small proportion of individuals that was not eligible by 2013 ACC/AHA guidelines, even when considering patients who may be eligible by any of the 3 guidelines, a significant proportion of at-risk population would not have been categorized as statin eligible (Figure 4).
OPPORTUNITIES FOR ENHANCING RISK PREDICTION
In the current era of generic statins that are generally well tolerated, several mechanisms have been suggested for better identification of more at-risk individuals. For instance, Navar-Boggan et al. (18) suggested that decreasing the treatment threshold to include the statin-considered group (i.e., ASCVD risk score of 5% to 7.5%) would improve the sensitivity of identifying individuals who ultimately experienced cardiovascular events. In our cohort, this increased statin eligibility by 18% for the ACC/AHA guideline. In addition to performing these measures, we also evaluated how including other risk factors proposed by the 2013 ACC/AHA statin guidelines may further enhance risk prediction. Specifically, we found that reclassifying all patients with LDL cholesterol >160 mg/dl and a family history of premature CAD as statin eligible would increase the proportion of treated patients from 49% to 66%. However, any criteria that would identify more at-risk individuals would lead to a higher proportion of treated patients across the population who would not necessarily experience events. Thus, although our findings suggest that incorporating the previously mentioned risk factors in making decisions regarding the role of statins in young individuals may be important, future investigations should further elucidate the population-level effect of such approaches aimed at expanding the number of individuals treated.
Any effort to expand the number of treated young individuals should also incorporate the following considerations: 1) although no randomized studies have assessed the role of statins for primary prevention among young adults, Mendelian randomization studies suggest that a longer exposure to low LDL cholesterol may provide long-term benefits (23); 2) although the overall risk of most young patients is low, younger individuals represent the largest proportion of the population who are at risk (24); and 3) patients who experience an MI at a younger age have a larger economic impact, as their lifetime earnings and societal contributions are affected to a greater extent. Ultimately, in the absence of randomized data (25), and given the need to balance the risks and benefits of treatment together with patients’ disutility from being on statin therapy, there is an important need to incorporate shared decision making between patients and physicians (26).
In addition to the aforementioned efforts in identifying at-risk patients, our study also reinforces the need for more primordial prevention (27–29). In fact, >80% of the patients who had an MI at a young age had at least 1 modifiable risk factor, with dyslipidemia, smoking, and hypertension being the most prevalent. The USPSTF has established guidelines for screening for traditional cardiovascular risk factors in adults, and current recommendations include: screening for hypertension annually in patients age ≥40 years, and every 3 to 5 years in patients 18 to 40 years of age (30); screening overweight or obese adults age 40 to 70 years for diabetes (31); and providing pharmacotherapy or behavioral interventions to adults for smoking cessation (32). The USPSTF recommends screening for dyslipidemia every 5 years in patients age ≥40 years, but was neither for nor against screening patients age 21 to 39 years, citing lack of evidence in this age group (8). The 2013 ACC/AHA cholesterol guidelines have expanded the number of individuals eligible for statin therapy, and accordingly, recent data suggests that there has been a gradual but sustained increase in statin use for primary preventions (33).
SEX DIFFERENCES IN STATIN ELIGIBILITY
Women had significantly lower statin eligibility compared with men, even though there were no significant differences in age or the burden of risk factors between men and women. Although the more pronounced underestimation of risk in women in our cohort cannot be explained by differences in age or risk factors alone, it is noteworthy that the PCE has been shown to overestimate risk in women (34). Further research is required to better identify risk and prevent cardiovascular disease in women, particularly as women have worse outcomes post-MI compared with similarly aged men (35).
STUDY LIMITATIONS
Our study is retrospective in nature and thus subject to limitations regarding uniformity of data collection. However, our retrospective cohort design is ideal for studying less frequent conditions, such as MI in young individuals. In addition, we performed a manual review of all admission notes, rather than rely on billing or other coded information, to both adjudicate the presence of MI as well as determine the prevalence of various risk factors. Although our findings reinforce the need for better identification of risk among young individuals, a limitation of our study is that we only evaluated individuals who experienced an MI, without considering the overall at-risk population for this age group. As a result, we were not able to determine the prevalence of various risk factors across the population of at-risk patients who did not experience an MI, as has previously been done by other population-based cohorts (36). In the future, the use of machine learning algorithms may facilitate other study designs, such as retrospective case-control studies, which may provide further information in this regard.
Lipid levels may be falsely lowered at the time of MI; however, one of the largest studies examining this did not find a clinically meaningful change (37). Nevertheless, we analyzed the change in total cholesterol for patients who had available measurements before their MI and during the index admission. In these patients, the total cholesterol decreased by 12%. Consequently, we performed a sensitivity analysis by increasing the total cholesterol of all patients who did not have prior cholesterol values by 12%, and our findings remained robust, suggesting that any potential changes in lipid values peri-MI did not have a significant effect on our findings.
Guidelines recommend considering factors such as high-sensitivity C-reactive protein, coronary artery calcium, and ankle brachial pressure index, but results from such testing were not available for our cohort. Finally, our risk estimates may be too conservative, as we increased the age of some of the patients by more than 10 years, and it is likely that we would have observed an even higher proportion of patients who were not statin eligible if we used actual age in calculating the ASCVD risk score from PCE. However, the PCE are derived from and thereby applicable only to those who are 40 to 79 years of age (12).
Despite the fact that this study was conducted across 2 large academic medical centers, our results remain generalizable to other settings, as our study examines baseline risk level and is not related to the treatment received. Although there may be geographical differences in some cardiovascular risk factors, these are unlikely to influence our main results, as our population had a high prevalence of underlying risk factors, and it was their younger age, rather than failure to capture these risk factors, that contributed to them being classified as statin ineligible. Our study population was mostly white, and we recognize that certain groups such as South Asians may have a higher predisposition to develop premature CAD, and risk scores may further underestimate their risk (38–40); however, we did not have sufficient power to analyze subgroups based on race or ethnicity.
CONCLUSIONS
The vast majority of adults who present with an MI at a young age would not have met current guideline-based treatment thresholds for statin therapy prior to their MI. These findings highlight the need to develop better risk assessment tools among young adults.
Supplementary Material
PERSPECTIVES.
COMPETENCY IN MEDICAL KNOWLEDGE
Most patients presenting with MI before age 50 years would not have met current guideline-based treatment thresholds for statin therapy prior to their event.
COMPETENCY IN PATIENT CARE AND PROCEDURAL SKILLS
Low ASCVD risk scores may be falsely reassuring in patients younger than 50 years of age, leading to under-treatment in certain clinical situations. In addition to the risk score, additional factors such as a family history of premature CAD or clustering of risk factors, should be considered in determining the potential benefit of statin therapy.
TRANSLATIONAL OUTLOOK
Further research is needed to optimally estimate cardiovascular risk in young adults.
Acknowledgments
Dr. Gupta is supported by National Institutes of Health grant number 5T32HL094301. Dr. Qamar is supported by National Institutes of Health grant number T32HL007604. Dr. Bhatt has served on Advisory Board of Cardax, Elsevier Practice Update Cardiology, Medscape Cardiology, and Regado Biosciences; has served on the Board of Directors of Boston VA Research Institute and the Society of Cardiovascular Patient Care; is Chair of the American Heart Association Quality Oversight Committee; has served on Data Monitoring Committees for Cleveland Clinic, Duke Clinical Research Institute, Harvard Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine, and Population Health Research Institute; has received honoraria from American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org), Belvoir Publications (Editor-in-Chief, Harvard Heart Letter), HMP Communications (Editor-in-Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), Slack Publications (Chief Medical Editor, Cardiology Today’s Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), and WebMD (CME steering committees); has received honoraria for serving on clinical trial steering committees of Duke Clinical Research Institute, Harvard Clinical Research Institute, and Population Health Research Institute; has served as Deputy Editor of Clinical Cardiology; has served as chair of the NCDR-ACTION Registry Steering Committee and VA CART Research and Publications Committee; has received research funding from Amarin, Amgen, AstraZeneca, Bristol-Myers Squibb, Chiesi, Eisai, Ethicon, Forest Laboratories, Ironwood, Ischemix, Lilly, Medtronic, Pfizer, Roche, Sanofi, and The Medicines Company; has received royalties from Elsevier (Editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease); has served as site coinvestigator for Biotronik, Boston Scientific, and St. Jude Medical (now Abbott); has served as a trustee of American College of Cardiology; and has performed unfunded research for FlowCo, Merck, PLx Pharma, and Takeda. Dr. Blankstein has served on the advisory board of Amgen; and has received research support from Amgen and Gilead Sciences. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose. This paper was presented on November 14, 2017, at the Ancel Keys Cardiovascular Disease Prevention Session, American Heart Association 2017 Scientific Sessions, Anaheim, California.
ABBREVIATIONS AND ACRONYMS
- ASCVD
atherosclerotic cardiovascular disease
- CAD
coronary artery disease
- LDL
low-density lipoprotein
- MI
myocardial infarction
- NCEP
National Cholesterol Education Panel
- PCE
pooled cohort equations
- USPSTF
U.S. Preventive Services Task Force
Footnotes
APPENDIX For supplemental figures and tables, please see the online version of this paper.
References
- 1.Eisen A, Giugliano RP, Braunwald E. Updates on acute coronary syndrome: a review. JAMA Cardiol. 2016;1:718–30. doi: 10.1001/jamacardio.2016.2049. [DOI] [PubMed] [Google Scholar]
- 2.Bucholz EM, Strait KM, Dreyer RP, et al. Sex differences in young patients with acute myocardial infarction: a VIRGO study analysis. Eur Heart J Acute Cardiovasc Care. 2017;6:610–22. doi: 10.1177/2048872616661847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta A, Wang Y, Spertus JA, et al. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol. 2014;64:337–45. doi: 10.1016/j.jacc.2014.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gidding SS. Why cholesterol testing in children and adolescents matters. JAMA Cardiol. 2016;1:859–61. doi: 10.1001/jamacardio.2016.2871. [DOI] [PubMed] [Google Scholar]
- 5.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 6.Akosah KO, Schaper A, Cogbill C, Schoenfeld P. Preventing myocardial infarction in the young adult in the first place: how do the National Cholesterol Education Panel III guidelines perform? J Am Coll Cardiol. 2003;41:1475–9. doi: 10.1016/s0735-1097(03)00187-6. [DOI] [PubMed] [Google Scholar]
- 7.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889–934. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Force USPST. Bibbins-Domingo K, Grossman DC, et al. Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;316:1997–2007. doi: 10.1001/jama.2016.15450. [DOI] [PubMed] [Google Scholar]
- 9.Miedema MD, Garberich RF, Schnaidt LJ, et al. Statin eligibility and outpatient care prior to ST-segment elevation myocardial infarction. J Am Heart Assoc. 2017;6:e005333. doi: 10.1161/JAHA.116.005333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh A, Collins B, Qamar A, et al. Study of young patients with myocardial infarction: design and rationale of the YOUNG-MI Registry. Clin Cardiol. 2017 Aug 14; doi: 10.1002/clc.22774. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012;60:1581–98. doi: 10.1016/j.jacc.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Goff DC, Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2935–59. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martin SS, Blaha MJ, Elshazly MB, et al. Comparison of a novel method vs the Friedewald equation for estimating low-density lipoprotein cholesterol levels from the standard lipid profile. JAMA. 2013;310:2061–8. doi: 10.1001/jama.2013.280532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lloyd-Jones DM, Leip EP, Larson MG, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–8. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 15.Berry JD, Liu K, Folsom AR, et al. Prevalence and progression of subclinical atherosclerosis in younger adults with low short-term but high lifetime estimated risk for cardiovascular disease: the Coronary Artery Risk Development in Young Adults Study and Multi-Ethnic Study of Atherosclerosis. Circulation. 2009;119:382–9. doi: 10.1161/CIRCULATIONAHA.108.800235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Informat. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pencina MJ, Navar-Boggan AM, D’Agostino RB, Sr, et al. Application of new cholesterol guidelines to a population-based sample. N Engl J Med. 2014;370:1422–31. doi: 10.1056/NEJMoa1315665. [DOI] [PubMed] [Google Scholar]
- 18.Navar-Boggan AM, Peterson ED, D’Agostino RB, Sr, Pencina MJ, Sniderman AD. Using age- and sex-specific risk thresholds to guide statin therapy: one size may not fit all. J Am Coll Cardiol. 2015;65:1633–9. doi: 10.1016/j.jacc.2015.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeFilippis AP, Young R, McEvoy JW, et al. Risk score overestimation: the impact of individual cardiovascular risk factors and preventive therapies on the performance of the American Heart Association-American College of Cardiology-Atherosclerotic Cardiovascular Disease risk score in a modern multi-ethnic cohort. Eur Heart J. 2017;38:598–608. doi: 10.1093/eurheartj/ehw301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013;382:1762–5. doi: 10.1016/S0140-6736(13)62388-0. [DOI] [PubMed] [Google Scholar]
- 21.Miedema MD, Lopez FL, Blaha MJ, et al. Eligibility for statin therapy according to new cholesterol guidelines and prevalent use of medication to lower lipid levels in an older US Cohort: the Atherosclerosis Risk In Communities study cohort. JAMA Intern Med. 2015;175:138–40. doi: 10.1001/jamainternmed.2014.6288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karmali KN, Goff DC, Jr, Ning H, Lloyd-Jones DM. A systematic examination of the 2013 ACC/AHA pooled cohort risk assessment tool for atherosclerotic cardiovascular disease. J Am Coll Cardiol. 2014;64:959–68. doi: 10.1016/j.jacc.2014.06.1186. [DOI] [PubMed] [Google Scholar]
- 23.Ference BA, Majeed F, Penumetcha R, Flack JM, Brook RD. Effect of naturally random allocation to lower low-density lipoprotein cholesterol on the risk of coronary heart disease mediated by polymorphisms in NPC1L1, HMGCR, or both: a 2 × 2 factorial Mendelian randomization study. J Am Coll Cardiol. 2015;65:1552–61. doi: 10.1016/j.jacc.2015.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sniderman AD, Thanassoulis G, Williams K, Pencina M. Risk of premature cardiovascular disease vs the number of premature cardiovascular events. JAMA Cardiol. 2016;1:492–4. doi: 10.1001/jamacardio.2016.0991. [DOI] [PubMed] [Google Scholar]
- 25.Domanski MJ, Fuster V, Diaz-Mitoma F, et al. Next steps in primary prevention of coronary heart disease: rationale for and design of the ECAD trial. J Am Coll Cardiol. 2015;66:1828–36. doi: 10.1016/j.jacc.2015.08.857. [DOI] [PubMed] [Google Scholar]
- 26.Krumholz HM. Treatment of cholesterol in 2017. JAMA. 2017;318:417–8. doi: 10.1001/jama.2017.6753. [DOI] [PubMed] [Google Scholar]
- 27.Fuster V. Stratified approach to health: integration of science and education at the right time for each individual. J Am Coll Cardiol. 2015;66:1627–9. doi: 10.1016/j.jacc.2015.08.039. [DOI] [PubMed] [Google Scholar]
- 28.Vaduganathan M, Venkataramani AS, Bhatt DL. Moving toward global primordial prevention in cardiovascular disease: the heart of the matter. J Am Coll Cardiol. 2015;66:1535–7. doi: 10.1016/j.jacc.2015.08.027. [DOI] [PubMed] [Google Scholar]
- 29.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s Strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 30.Siu AL for the U S. Preventive Services Task Force. Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163:778–86. doi: 10.7326/M15-2223. [DOI] [PubMed] [Google Scholar]
- 31.Siu AL for the U S. Preventive Services Task Force. Screening for abnormal blood glucose and type 2 diabetes mellitus: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2015;163:861–8. doi: 10.7326/M15-2345. [DOI] [PubMed] [Google Scholar]
- 32.Siu AL for the U S. Preventive Services Task Force. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2015;163:622–34. doi: 10.7326/M15-2023. [DOI] [PubMed] [Google Scholar]
- 33.Olufade T, Zhou S, Anzalone D, et al. Initiation patterns of statins in the 2 years after release of the 2013 American College of Cardiology/American Heart Association (ACC/AHA) Cholesterol Management Guideline in a large US health plan. J Am Heart Assoc. 2017;6:e005205. doi: 10.1161/JAHA.116.005205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cook NR, Ridker PM. Further insight into the cardiovascular risk calculator: the roles of statins, revascularizations, and underascertainment in the Women’s Health Study. JAMA Intern Med. 2014;174:1964–71. doi: 10.1001/jamainternmed.2014.5336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bangalore S, Fonarow GC, Peterson ED, et al. Age and gender differences in quality of care and outcomes for patients with ST-segment elevation myocardial infarction. Am J Med. 2012;125:1000–9. doi: 10.1016/j.amjmed.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 36.Patel KK, Taksler GB, Hu B, Rothberg MB. Prevalence of elevated cardiovascular risks in young adults: a cross-sectional analysis of National Health and Nutrition Examination Surveys. Ann Intern Med. 2017;166:876–82. doi: 10.7326/M16-2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pitt B, Loscalzo J, Ycas J, Raichlen JS. Lipid levels after acute coronary syndromes. J Am Coll Cardiol. 2008;51:1440–5. doi: 10.1016/j.jacc.2007.11.075. [DOI] [PubMed] [Google Scholar]
- 38.Palaniappan L, Wang Y, Fortmann SP. Coronary heart disease mortality for six ethnic groups in California, 1990–2000. Ann Epidemiol. 2004;14:499–506. doi: 10.1016/j.annepidem.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 39.Kanjilal S, Rao VS, Mukherjee M, et al. Application of cardiovascular disease risk prediction models and the relevance of novel biomarkers to risk stratification in Asian Indians. Vasc Health Risk Manag. 2008;4:199–211. doi: 10.2147/vhrm.2008.04.01.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kandula NR, Kanaya AM, Liu K, et al. Association of 10-year and lifetime predicted cardiovascular disease risk with subclinical atherosclerosis in South Asians: findings from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. J Am Heart Assoc. 2014;3:e001117. doi: 10.1161/JAHA.114.001117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.