Abstract
Background
Routine influenza vaccination of health care personnel (HCP) can reduce influenza related illness and its potentially serious consequences among HCP and their patients. Influenza vaccination has been routinely recommended for HCP since 1984.
Methods
Data from the 2013 and 2014 National Health Interview Survey (NHIS) were analyzed in 2015. The Kaplan-Meier survival analysis procedure was used to estimate the cumulative proportion of HCP reporting 2013–14 season influenza vaccination. Vaccination coverage by work setting and occupation were assessed. Multivariable logistic regression and predictive marginal analyses were conducted to identify factors independently associated with vaccination among HCP.
Results
Overall, influenza vaccination coverage was 64.9% among HCP aged ≥18 years (95% confidence interval [CI] = 60.5%–69.3%), which was significantly higher compared with non-HCP among the same age group (41.0%; 95% CI = 39.8%–42.1%) (p<0.05). Vaccination coverage was higher among physicians (82.3%) and nurses (77.5%) compared with other types of HCP (range: 50.2% to 65.6%). Coverage was higher among HCP working in hospitals (76.9%) compared with other settings (range: 53.9%–60.2%). Characteristics independently associated with an increased likelihood of vaccination among HCP were higher age, higher education, having more physician contacts, and having health insurance. Having never been married was independently associated with a decreased likelihood of vaccination among HCP.
Conclusions
Influenza vaccination coverage was higher among HCP than non-HCP but still below the national target of 90%. Vaccination coverage varied widely by occupation type, work settings, and demographic characteristics. Evidence-based interventions such as making vaccine available at no cost at the workplace along with active promotion of vaccination are needed to increase influenza vaccination among HCP in all health-care settings.
Keywords: influenza vaccine, vaccination, coverage, health-care personnel
Introduction
All paid and unpaid persons working in health-care settings who have potential for exposure to patients or to infectious materials, including body substances, contaminated medical supplies and equipment, contaminated environmental surfaces, or contaminated air are considered to be health-care personnel (HCP).1, 2 HCP include staff involved in direct patient care (e.g., physicians, nurses, clinical laboratory staff, health technologists, and medical assistants), and staff not involved in direct patient care (e.g., clerical, dietary, house-keeping, laundry, security, maintenance, billing, and volunteers).1, 2. Because of their contact with patients or infective material from patients, HCP are at risk for exposure to influenza or possible transmission of influenza.1, 2 Annual influenza vaccination of HCP has been recommended by the Advisory Committee on Immunization Practices (ACIP) since 1984 (3) and remains the most effective intervention to reduce transmission of influenza in health-care settings.1–2, 4–5 Influenza outbreaks in healthcare settings have been associated with low vaccination coverage among HCP.4, 6–8 Influenza vaccination has been shown to lower the number of sick days taken by HCP during influenza season.9, 10
In addition to the ACIP, medical and health professional organizations, including the American Academy of Family Physicians, American College of Physicians, and the Society for Post-Acute and Long-Term Care Medicine have published position statements that support influenza vaccination of healthcare personnel.11 The Healthy People 2020 (HP2020) objectives call for raising influenza vaccination levels among HCP to at least 90%.12 However, even though levels of influenza vaccination among HCP have risen slowly over the past ten years, vaccination coverage of HCP has not been optimal, ranging from 36% to 62%.1–2, 4, 13–14
Data from the 2013 and 2014 National Health Interview Surveys (NHIS) were used to assess influenza vaccination coverage among HCP in the United States overall, by work setting, and by occupation, and to identify factors independently associated with vaccination. The NHIS is the only population-based source of data on influenza vaccination coverage among all U.S. HCP, and is the official data source for tracking progress towards the HP2020 target.12
Methods
Data from the 2013 and 2014 NHIS were analyzed in 2015. NHIS is a probability-based annual household survey conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention.15–16 The survey has four main modules: the household composition section, family core, sample adult core, and sample child core. In the sample adult core, one adult per sampled family from each household was randomly selected and asked to complete the sample adult questionnaire, including questions about receipt of influenza vaccination. In 2013 and 2014, the final response rates for the sample adult core were 61.2% and 58.9%, respectively.15–16
Respondents were asked “During the past 12 months, have you had a flu shot?” and “During what month and year did you receive your most recent seasonal flu shot?” “During the past 12 months, have you had a seasonal flu vaccine that was sprayed in your nose?” and “During what month and year did you receive your most recent seasonal flu vaccine that was sprayed in your nose?” For this study, persons self-reporting receipt of either vaccine (shot or spray) were considered to have received influenza vaccination. Respondents were also asked “Do you currently volunteer or work in a hospital, medical clinic, doctor’s office, dentist’s office, nursing home or some other health-care facility? This includes part-time and unpaid work in a health care facility as well as professional nursing care provided in the home.” and “Do you provide direct patient care as part of your routine work?” Those with an affirmative answer to either question were considered HCP. Regarding occupation type and work settings, respondents were asked “What kind of work were you doing?” and “What kind of business or industry was this?” Occupation type and work settings are based on standard occupation and industry categories recoded into groups by the National Center for Health Statistics and released through CDC’s Research Data Center (RDC).
High-risk persons were defined as individuals who self-reported one or more of the following: having ever being told by a physician they had diabetes, emphysema, chronic obstructive pulmonary disease (COPD), coronary heart disease, angina, heart attack or other heart condition; being diagnosed with cancer in the past 12 months (excluding non-melanoma skin cancer) or ever being told by a physician they have lymphoma, leukemia or blood cancer; during the past 12 months, being told by a physician they have chronic bronchitis or weak or failing kidneys; or reporting an asthma episode or attack in the past 12 months. Poverty thresholds used in the 2014 NHIS were estimated from: weighted average Census poverty thresholds from 2012, the average Consumer Price Index from 2012; actual Consumer Price Index values for January–July 2013, and projected Consumer Price Index values for August–December 2013. The poverty thresholds used in the 2013 NHIS were estimated from several sources: weighted average Census poverty thresholds from 2011, the average Consumer Price Index from 2011, actual Consumer Price Index values for January–July, 2012, and projected Consumer Price Index values for August–December, 2012.15, 16
SAS (Statistical analysis software) version 9.3 and SUDAAN (Software for the statistical analysis of correlated data, Research Triangle Institute, Research Triangle Park, NC, version 10.01) was used to calculate point estimates and 95% confidence intervals (CIs). Influenza vaccination among HCP stratified by demographic and access-to-care characteristics was assessed in bi-variable analyses. Chi-square tests were used to determine differences between groups with statistical significance defined as p< 0.05. To better assess cumulative seasonal influenza vaccination coverage, analysis of season-specific coverage was restricted to individuals interviewed during August 2013 through June 2014 and vaccinated during July 2013 through May 2014 using the Kaplan-Meier survival analysis procedure, and the results based on this procedure are presented in Table 2 (The end of season coverage is an independent categorical rate and the Chi-square test is used to determine differences between groups). For the Kaplan-Meier survival analysis, time-to-event variable is month of vaccination. Time-to-event variable considered censored if person not vaccinated by date of interview. Time-to-event variable is considered not censored if person was vaccinated in a month prior to month of interview. The main interest for most reporting will be the cumulative coverage rate for the most recent month (e.g., if using data through June to estimate vaccinations through May, the Kaplan-Meier estimate of cumulative vaccination rate for May could be reported). Multivariable analyses were restricted to individuals interviewed during August 2013 through June 2014, and vaccinated in the last 12 months. Multivariable logistic regression and predictive marginal models were used to generate adjusted prevalence ratios and identify variables independently associated with influenza vaccination. All variables used in the bi-variable analysis were included in the full multivariable model.
TABLE 2.
Influenza vaccination coverage by healthcare personnel status, demographic and access-to-care variables among persons ≥18 years in the United States – National Health Interview Survey (NHIS), 2013–14 influenza season
| Characteristic | Healthcare personnel | Non-HCP |
|---|---|---|
|
| ||
| % (95% CI) | % (95% CI) | |
| Total | 64.9 (60.5, 69.3) | 41.0 (39.8, 42.1)* |
| Age (years) | ||
| 18–49a | 60.9 (54.6, 67.3) | 28.2 (26.8, 29.6)* |
| 50–64 | 71.1 (65.8, 76.3)** | 45.5 (43.5, 47.6)*,** |
| ≥65 | 75.2 (66.6, 83.0)** | 71.4 (69.5, 73.2) ** |
| Sex | ||
| Malea | 67.9 (60.2, 75.3) | 37.1 (35.5, 38.9)* |
| Female | 63.8 (59.0, 68.5) | 44.8 (43.4, 46.3)*,** |
| Race/ethnicityb | ||
| Non-Hispanic Whitea | 66.9 (61.1, 72.6) | 44.4 (42.9, 45.9)* |
| Non-Hispanic Black | 50.2 (42.8, 58.0)** | 34.9 (32.4, 37.6)*,** |
| Hispanic | 65.6 (53.3, 77.7) | 31.5 (29.2, 33.9)*,** |
| Asian | 77.7 (63.9, 89.0) | 41.7 (37.2, 46.5)* |
| Other | 60.3 (37.1, 84.1) | 36.9 (30.9, 43.8)** |
| Marital Status | ||
| Marrieda | 71.6 (66.7, 76.3) | 45.0 (43.3, 46.7)* |
| Widowed/divorced/separated | 63.7 (56.2, 71.2) | 50.7 (48.6, 52.8)*,** |
| Never married | 54.0 (44.6, 63.9)** | 28.4 (26.6, 30.4)*,** |
| Education | ||
| High school or lessa | 54.0 (46.0, 62.3) | 38.0 (36.6, 39.5)* |
| Some college or college graduate | 64.4 (57.7, 71.0) | 40.4 (39.0, 42.0)*,** |
| Above college graduate | 76.5 (70.1, 82.4)** | 55.1 (51.8, 58.5)*,** |
| Poverty level | ||
| At or above poverty | 65.1 (60.3, 69.8) | 42.3 (41.0, 43.6)*,** |
| Below povertya | 66.4 (46.1, 85.4) | 32.4 (30.1, 34.8)* |
| Region | ||
| Northeasta | 66.6 (58.7, 74.5) | 44.1 (41.2, 47.1)* |
| Midwest | 63.1 (52.2, 73.9) | 42.9 (40.4, 45.5)* |
| South | 64.1 (58.7, 69.5) | 39.9 (38.1, 41.7)*,** |
| West | 67.9 (60.9, 74.7) | 38.6 (36.4, 40.9)*,** |
| US born status | ||
| U.S. borna | 63.4 (58.8, 68.0) | 42.1 (40.9, 43.4)* |
| Born outside U.S. -- In U.S. < 10 yrs | 70.6 (50.9, 87.8) | 29.7 (25.1, 34.9)*,** |
| Born outside U.S. -- In U.S. ≥ 10 yrs | 71.2 (63.0, 79.0) | 37.5 (35.0, 40.0)*,** |
| High-risk statusc | ||
| High risk | 68.4 (61.5, 75.1) | 57.2 (55.2, 59.2)*,** |
| Not high riska | 63.9 (58.4, 69.3) | 35.4 (34.2, 36.7)* |
| Physician contacts within past year | ||
| Nonea | 53.0 (39.7, 67.6) | 14.9 (13.2, 16.7)* |
| 1 | 58.4 (50.6, 66.3) | 31.9 (29.6, 34.3)*,** |
| 2–3 | 69.8 (64.0, 75.5)** | 44.5 (42.4, 46.6)*,** |
| 4–9 | 67.3 (57.0, 77.3) | 56.8 (54.6, 59.0)*,** |
| ≥10 | 68.6 (59.6, 77.3) | 57.9 (55.2, 60.6)*,** |
| Hospitalization within past year | ||
| Yes | 67.4 (55.5, 78.9) | 57.5 (54.5, 60.6)** |
| Noa | 64.8 (60.2, 69.3) | 39.4 (38.2, 40.6)* |
| Usual place for health care | ||
| Yes | 66.2 (61.6, 70.8) | 45.5 (44.3, 46.7)*,** |
| Noa | 52.9 (38.7, 68.6) | 14.6 (12.8, 16.7)* |
| Health insurance | ||
| Yes | 67.6 (62.7, 72.3)** | 45.7 (44.5, 46.9)*,** |
| Noa | 40.6 (30.7, 52.3) | 14.6 (12.9, 16.5)* |
| Direct patient care | ||
| Yes | 65.1 (58.6, 71.5) | NA |
| Noa | 64.7 (58.7, 70.6) | NA |
Note: Boldface indicates significance.
Abbreviations: CI=Confidence interval; NA=Not applicable.
Reference level.
Race/ethnicity was defined based on individuals self-identifying as non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic Asian, and non-Hispanic other race (including American Indian/Alaska Native, and multiple races).
Individuals who self-reported one or more of the following: ever being told by a physician they had diabetes, emphysema, COPD, coronary heart disease, angina, heart attack or other heart condition; being diagnosed with cancer in the past 12 months (excluding non-melanoma skin cancer) or ever being told by a physician they have lymphoma, leukemia or blood cancer; during the past 12 months, being told by a physician they have chronic bronchitis or weak or failing kidneys; or reporting an asthma episode or attack in the past 12 months.
p<0.05 by chi-square test for comparisons between healthcare personnel and non-healthcare personnel within each level of each characteristic.
p<0.05 by chi-square test for comparisons within each covariate category with the indicated reference level.
Results
Of the 32,584 respondents in the NHIS sample adult core interviewed August 2013 through June 2014, 8.2% (2,651) were HCP. Demographic characteristics of the study population are given in Table 1. The majority of HCP were 18–49 years (62.6%), female (72.5%), non-Hispanic white (70.7%), married (56.1%), had some college education or higher (81.5%), were living at or above poverty (92.7%), born in the United States (85.3%), had no high-risk conditions (79.7%), had a usual place for health care (90.5%), and had health insurance (90.4%). HCP differed significantly from non-HCP for all characteristics assessed. Additionally, of the 2,651 HCP, 60.4% reported direct patient care.
TABLE 1.
Sample characteristics of participants ≥18 years in the United States, by healthcare personnel status, demographic, and access-to-care variables--National Health Interview Survey (NHIS), 2013–14 influenza season
| Characteristic | Healthcare personnel | Non-HCP | ||
|---|---|---|---|---|
|
| ||||
| Sample | Weighted % | Sample | Weighted % | |
| Total | 2,651 | 100.0 | 29,933 | 100.0 |
| Age (years) | ||||
| 18–49 | 1,603 | 62.6 | 15,152 | 54.9* |
| 50–64 | 770 | 29.4 | 7,624 | 25.6 |
| ≥65 | 278 | 8.0 | 7,157 | 19.5 |
| Sex | ||||
| Male | 652 | 27.5 | 13,887 | 49.8* |
| Female | 1,999 | 72.5 | 16,046 | 50.2 |
| Race/ethnicitya | ||||
| Non-Hispanic White | 1,742 | 70.7 | 18,248 | 65.6* |
| Non-Hispanic Black | 408 | 13.3 | 4,049 | 11.3 |
| Hispanic | 288 | 9.1 | 5,139 | 15.7 |
| Asian | 157 | 5.6 | 1,698 | 5.4 |
| Other | 56 | 1.4 | 799 | 2.1 |
| Marital status | ||||
| Married | 1,221 | 56.1 | 12,931 | 52.7* |
| Widowed/divorced/separated | 606 | 14.2 | 8,017 | 17.7 |
| Never married | 816 | 29.6 | 8,919 | 29.6 |
| Education | ||||
| High school or less | 547 | 18.5 | 12,789 | 41.4* |
| Some college or college graduate | 1,655 | 63.5 | 14,084 | 48.7 |
| Above college graduate | 446 | 18.0 | 2,921 | 9.9 |
| Poverty level | ||||
| At or above poverty | 2,284 | 92.7 | 22,780 | 85.6* |
| Below poverty | 241 | 7.3 | 5,235 | 14.4 |
| Region | ||||
| Northeast | 526 | 19.7 | 4,700 | 17.0* |
| Midwest | 613 | 28.2 | 6,159 | 22.7 |
| South | 847 | 33.0 | 10,804 | 37.3 |
| West | 665 | 19.0 | 8,270 | 23.0 |
| US born status | ||||
| U.S. born | 2,258 | 85.3 | 24,306 | 81.8* |
| Born outside U.S. -- In U.S. < 10 yrs | 71 | 2.0 | 1,135 | 3.7 |
| Born outside U.S. -- In U.S. ≥ 10 yrs | 316 | 12.7 | 4,421 | 14.5 |
| High-risk statusb | ||||
| High risk | 544 | 20.3 | 8,271 | 25.2* |
| Not high risk | 2,104 | 79.7 | 21,604 | 74.8 |
| Physician contacts within past year | ||||
| None | 338 | 12.0 | 5,655 | 19.5* |
| 1 | 489 | 17.9 | 5,341 | 18.8 |
| 2–3 | 805 | 30.6 | 7,646 | 25.7 |
| 4–9 | 688 | 27.4 | 7,118 | 23.3 |
| ≥10 | 328 | 12.1 | 4,067 | 12.7 |
| Hospitalization within past year | ||||
| Yes | 195 | 6.9 | 2,886 | 8.7* |
| No | 2,454 | 93.1 | 27,030 | 91.3 |
| Usual place for health care | ||||
| Yes | 2,382 | 90.5 | 25,449 | 85.1* |
| No | 269 | 9.5 | 4,477 | 14.9 |
| Health insurance | ||||
| With health insurance | 2,337 | 90.4 | 25,095 | 84.1* |
| Without health insurance | 309 | 9.6 | 4,739 | 15.9 |
| Direct patient care | ||||
| Yes | 1,627 | 60.4 | NA | NA |
| No | 1,024 | 39.6 | NA | NA |
Note: Boldface indicates significance.
Abbreviation: NA=Not applicable.
Race/ethnicity was defined based on individuals self-identifying as non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic Asian, and non-Hispanic other race (including American Indian/Alaska Native, and multiple races).
Individuals who self-reported one or more of the following: ever being told by a physician they had diabetes, emphysema, COPD, coronary heart disease, angina, heart attack or other heart condition; being diagnosed with cancer in the past 12 months (excluding non-melanoma skin cancer) or ever being told by a physician they have lymphoma, leukemia or blood cancer; during the past 12 months, being told by a physician they have chronic bronchitis or weak or failing kidneys; or reporting an asthma episode or attack in the past 12 months.
p<0.05, by chi-square test for comparisons between healthcare personnel and non-healthcare personnel of the distribution of each covariate category.
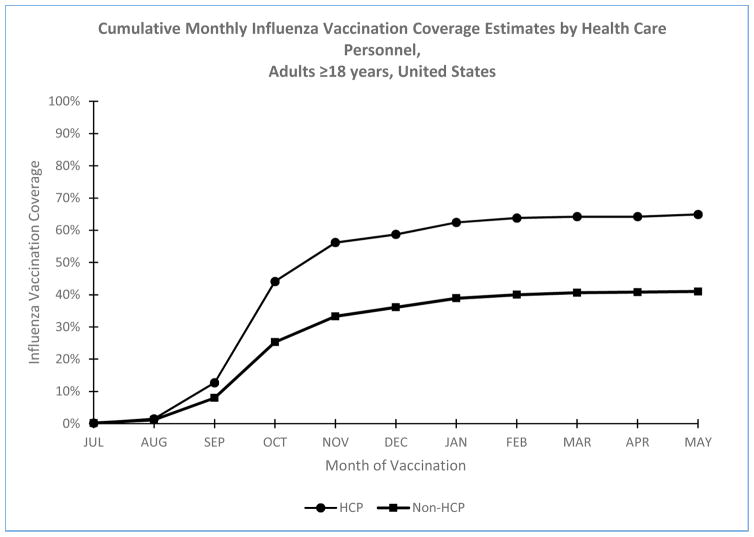
Influenza vaccination coverage among HCP was 64.9% (95% confidence interval (CI) = 60.5%–69.3%), significantly higher than among non-HCP (41.0%: 95% CI=39.8%–42.1%) (Table 2). Monthly vaccination coverage substantially increased from August to January and then increase slowed down from February to May (Figure). Influenza vaccination coverage was significantly higher among HCP compared with non-HCP across all subgroups except those ≥65 years, and those who were hospitalized in the past year (Table 2). Influenza vaccination coverage was similar among HCP with direct patient contact (65.1% [95% CI = 58.6% to 71.5%]) and HCP without direct patient contact (64.7% [95% CI = 58.7% to 70.6%]) (p>0.05).
Figure.
Cumulative Monthly Influenza Vaccination Coverage Estimates by Health Care Personnel Status based on Kaplan-Meier Survival Analysis among Adults ≥18 Years, United States
In bi-variable analysis, influenza vaccination coverage was significantly higher among HCP aged 50–64 years (71.1%) and those aged ≥65 years (75.2%) compared with HCP aged 18–49 years (60.9%) (Table 2). Influenza vaccination coverage among HCP was significantly higher among those who reported having education beyond college compared with those who had high school or less than high school education, having 2–3 physician contacts in the past year compared with those who did not have physician contacts in the past year, and having health insurance compared with those who do not have health insurance (Table 2). Influenza vaccination coverage was significantly lower among non-Hispanic black HCP compared with non-Hispanic white HCP, and those who reported never having been married compared with those who were married (Table 2). Influenza vaccination coverage among non-HCP was significantly higher among persons who were: aged ≥50 years, female, widowed, divorced, or separated, those who had education beyond high school graduation, were living at or above poverty level, reported high-risk conditions, reported at least one or more physician contacts in the past year, reported having been hospitalized within past year, having a usual place for health care; and having health insurance (Table 2). Influenza vaccination coverage among non-HCP was significantly lower among persons who were non-Hispanic black, Hispanic, never married, those living in the South or West regions, and those who were born outside the United States (Table 2).
In multivariable analysis, characteristics independently associated with an increased likelihood of vaccination among HCP were: age ≥50 years, education beyond college graduation, having two or more physician contacts in the past year, and having health insurance. Never having been married was independently associated with a decreased likelihood of vaccination among HCP (Table 3). Characteristics independently associated with an increased likelihood of vaccination among non-HCP were: age ≥50 years, being female, education beyond high school graduation, living at or above poverty level, having high-risk conditions, having one or more physician contacts in the past year, having been hospitalized in the past year, having a usual place for health care, and having health insurance. Being non-Hispanic black and widowed, divorced, separated, or never married were independently associated with a decreased likelihood of vaccination among non-HCP (Table 3).
TABLE 3.
Multivariable logistic regression analyses of persons 18–64 years who reported receiving influenza vaccination, by healthcare personnel status, demographic and access-to-care variables, United States – National Health Interview Survey (NHIS), 2013–14 influenza season
| Characteristic | Healthcare personnel | Non healthcare personnel |
|---|---|---|
|
| ||
| Prevalence Ratio (PR) (adjusted) (95% CI) | Prevalence Ratio (PR) (adjusted) (95% CI) | |
| Age (years) | ||
| 18–49a | Reference | Reference |
| 50–64 | 1.14 (1.04–1.26)* | 1.28 (1.21–1.35)* |
| ≥65 | 1.18 (1.04–1.34)* | 1.86 (1.77–1.95)* |
| Sex | ||
| Malea | Reference | Reference |
| Female | 0.96 (0.87–1.05) | 1.09 (1.04–1.13)* |
| Race/ethnicityb | ||
| Non-Hispanic whitea | Reference | Reference |
| Non-Hispanic black | 0.91 (0.80–1.03) | 0.88 (0.83–0.94)* |
| Hispanic | 1.02 (0.88–1.17) | 1.02 (0.96–1.09) |
| Asian | 1.13 (0.96–1.34) | 1.06 (0.97–1.16) |
| Other | 1.08 (0.81–1.45) | 0.96 (0.85–1.09) |
| Marital Status | ||
| Marrieda | Reference | Reference |
| Widowed/divorced/separated | 0.94 (0.84–1.05) | 0.93 (0.88–0.97)* |
| Never married | 0.82 (0.73–0.93)* | 0.93 (0.88–0.98)* |
| Education | ||
| High school or lessa | Reference | Reference |
| Some college or college graduate | 1.11 (0.99–1.24) | 1.10 (1.06–1.15)* |
| Above college graduate | 1.27 (1.11–1.46)* | 1.34 (1.26–1.42)* |
| Poverty level | ||
| At or above poverty | 1.06 (0.90–1.26) | 1.08 (1.02–1.14)* |
| Below povertya | Reference | Reference |
| Region | ||
| Northeasta | Reference | Reference |
| Midwest | 0.94 (0.82–1.08) | 0.99 (0.93–1.06) |
| South | 1.01 (0.91–1.12) | 0.99 (0.93–1.04) |
| West | 1.01 (0.89–1.15) | 0.97 (0.91–1.03) |
| US born status | ||
| U.S. borna | Reference | Reference |
| Born outside U.S. -- In U.S. < 10 yrs | 1.11 (0.91–1.36) | 1.09 (0.98–1.21) |
| Born outside U.S. -- In U.S. ≥ 10 yrs | 0.93 (0.80–1.08) | 0.98 (0.91–1.04) |
| High-risk statusc | ||
| High risk | 0.95 (0.85–1.07) | 1.13 (1.09–1.17)* |
| Not high riska | Reference | Reference |
| Physician contacts within past year | ||
| Nonea | Reference | Reference |
| 1 | 1.09 (0.90–1.31) | 1.40 (1.27–1.55)* |
| 2–3 | 1.30 (1.08–1.57)* | 1.66 (1.51–1.82)* |
| 4–9 | 1.26 (1.05–1.53)* | 1.86 (1.69–2.05)* |
| ≥10 | 1.34 (1.10–1.64)* | 1.93 (1.74–2.14)* |
| Hospitalization within past year | ||
| Yes | 1.07 (0.93–1.24) | 1.12 (1.05–1.18)* |
| Noa | Reference | Reference |
| Usual place for health care | ||
| Yes | 1.06 (0.91–1.23) | 1.35 (1.23–1.48)* |
| Noa | Reference | Reference |
| Health insurance | ||
| Yes | 1.38 (1.12–1.69)* | 1.43 (1.31–1.55)* |
| Noa | Reference | Reference |
| Direct patient care | ||
| Yes | 1.06 (0.96–1.18) | NA |
| Noa | Reference | NA |
Note: Boldface indicates significance.
Abbreviations: CI=Confidence interval. NA=Not applicable.
Reference level.
Race/ethnicity was defined based on individuals self-identifying as non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic Asian, and non-Hispanic other race (including American Indian/Alaska Native, and multiple races).
Individuals who self-reported one or more of the following: ever being told by a physician they had diabetes, emphysema, COPD, coronary heart disease, angina, heart attack or other heart condition; being diagnosed with cancer in the past 12 months (excluding non-melanoma skin cancer) or ever being told by a physician they have lymphoma, leukemia or blood cancer; during the past 12 months, being told by a physician they have chronic bronchitis or weak or failing kidneys; or reporting an asthma episode or attack in the past 12 months.
p<0.05 by chi-square test for comparisons within each covariate category with the indicated reference level.
Influenza vaccination coverage was 82.3% (95% CI=71.5%–89.6%) for physicians, 77.5% (95% CI=72.1%–82.1%) for nurses, 70.5% (95% CI=64.1%–76.1%) for health technologists, 65.6% (95% CI= 57.3%–73.0%) for other groups besides physicians and nurses, 61.5% (95% CI=46.1%–74.9%) for clinical laboratory staff, 58.5% (95% CI=48.0%–68.2%) for healthcare support occupations, and 50.2% (95% CI=44.5%–55.8%) for nursing, psychiatric and home health aides (Table 4). Vaccination coverage was higher among HCP working in hospitals (76.9%) compared with other settings (53.9% for ambulatory healthcare service settings, and 60.2% for nursing and residential care facilities).
TABLE 4.
Influenza vaccination coverage by types of healthcare personnel and facilities among persons ≥18 years in the United States, National Health Interview Survey, 2014
| Sample | Influenza vaccination coverage | ||||
|---|---|---|---|---|---|
| Occupations | N | Total % (95% CI) | Ambulatory health care services % (95% CI) | Hospitals % (95% CI) | Nursing and residential care facilities % (95% CI) |
| Total | 2195a | 66.6 (63.7–69.3) | 60.2 (55.9–64.4) | 76.9 (72.3–81.0) | 53.9 (47.1–60.5) |
| Physicians | 130 | 82.3 (71.5–89.6) | 79.2 (64.7–88.8) | 88.7 (72.0–96.0) | b |
| Nurses | 580 | 77.5 (72.1–82.1) | 72.0 (61.5–80.6) | 80.0 (74.3–84.7) | 69.1 (49.9–83.4) |
| Other groups besides physicians and nursesc | 214 | 65.6 (57.3–73.0) | 50.7 (39.1–62.3)* | 85.3 (72.7–92.7) | b |
| Clinical laboratory | 77 | 61.5 (46.1–74.9) | b | 64.6 (43.6–81.2) | b |
| Health technologistsd | 401 | 70.5 (64.1–76.1) | 63.9 (52.7–73.8) | 79.8 (71.9–85.9) | b |
| Nursing, psychiatric, and home health aides | 552 | 50.2 (44.5–55.8)* | 50.1 (42.2–58.0)* | 60.2 (41.4–76.4) | 44.7 (35.7–54.0) |
| Healthcare support occupationse | 235 | 58.5 (48.0–68.2)* | 56.0 (43.1–68.1) | 62.6 (43.3–78.6) | b |
Note: Boldface indicates significance.
Abbreviations: CI=Confidence interval.
This sample size is less than the sample size in Table 1 since some HCP could not be categorized into occupations and work settings based on standard occupation and industry codes.
Estimates are not reliable due to sample size less than 30.
Including chiropractors, dentists, dietitians and nutritionists, optometrists, pharmacists, physician assistants, podiatrists, audiologists, occupational therapists, physical therapists, radiation therapists, and respiratory therapists.
Including dental hygienists, diagnostic related technologists and technicians, emergency medical technicians and paramedics, health diagnosing treating practitioner support technicians, medical records and health information technicians, opticians, and dispensing staff.
Including occupational therapist assistants and aides, physical therapist assistants, massage therapists, dental assistants, and medical assistants.
p<0.05 by chi-square for comparisons within each healthcare setting with physicians as the reference level.
Discussion
By the 2013–14 influenza season, influenza vaccination coverage among HCP was only 64.9%, well below the HP2020 target of 90% (12). HCP are exposed to influenza both at work and in the community.1–2, 4 Vaccination of HCP is especially important given their exposure to many high risk patients, patients with influenza-like illness, and the fact that HCP often work while ill.17–19 While HCP were more likely to be vaccinated with influenza vaccine than those who were non-HCP, even among HCP, about 1 in 3 (35.1%) reported not receiving influenza vaccination, including those with direct patient care. By occupation, vaccination coverage was the highest among physicians (82.3%), followed by nurses (77.5%), and lowest among nursing, psychiatric, and home health aide staff (50.2%). By work setting, coverage was highest among physicians who work in hospitals (88.7%), where influenza vaccination levels were close to the HP2020 target of 90%. However, coverage was the lowest among HCP working in nursing and residential care facilities (53.9%). Effective interventions should be provided for occupations and settings with low coverage.
A comprehensive employer influenza vaccination program that includes education about the benefits of vaccination, convenient access to vaccination services, the provision of influenza vaccination at no cost, and vaccination requirements can help improve vaccination coverage.20–22 Institutional requirements for influenza vaccination have led to higher vaccination levels.20 One study conducted in 2011 showed that mean reported institutional-level influenza vaccination coverage among HCP in a national sample of acute care hospitals rose from 62.0% in the pre-requirement season to 76.6% in the post-requirement season, representing a single-season increase of 14.7 percentage points.20 Influenza vaccination coverage rates of >98% have been reported in many health care organizations that have instituted mandatory vaccination policies.23–24 In the absence of vaccination requirements, increased influenza vaccination coverage among HCP has been associated with the provision of free vaccine at the workplace and multifaceted programs that combine education with active promotion of vaccine.25–27
Tetanus, diphtheria and acellular pertussis (Tdap) vaccination is also recommended for all HCP.28 Policies requiring vaccination with Tdap vaccine have also improved vaccination levels.21, 22 In 2010, a large public university made employment of HCP with direct patient contact conditional upon Tdap vaccination. After implementation of the policy, a nearly 100% compliance rate was achieved.21 One recent example used a multimodal HCP vaccination campaign consisting of a mandatory declination policy, mask wearing for non-vaccinated HCP, highly visible “I’m vaccinated” hanging badges, improved vaccination tracking, weekly compliance reports to managers and vice presidents, disciplinary measures for noncompliant HCP, vaccination stations at facility entrances, and inclusion of a target employee vaccination rate in the annual employee bonus program. The result of this study showed that compared with vaccination rates of 57%–72% in the 3 years prior to the intervention, employee vaccination coverage increased to 92% in year 1 and 93% in years 2–4.29 Such programs may provide a model for behavioral change within healthcare organizations.29
Vaccination coverage varied by occupation and work setting. Coverage was the highest among physicians and nurses, and lowest among nursing, psychiatric, and home health aide staff. Coverage was the highest among HCP working in hospitals and lowest among HCP working in nursing and residential care facilities. These patterns are consistent with the results from one previous study though vaccination coverage among HCP was lower (49% in 2008).30 These patterns are also similar to coverage estimates reported from non-probability based Internet panel surveys of HCP that have been conducted by CDC since the 2009–10 influenza season.25, 31 Though actual estimates from the Internet panel surveys are higher than those from the NHIS, likely due to methodological differences in the surveys, the Internet panel surveys have consistently shown higher vaccination coverage among physicians, nurses, and other clinical professionals compared with other groups of HCP, and lowest coverage among HCP working in long-term care settings.25–27, 29, 31 Compared with HCP working in hospital and ambulatory care settings, HCP in the Internet panel sample working in nursing and residential care facilities were most likely to report that their employer neither required nor promoted vaccination and least likely to report that their employer made vaccination available onsite at no cost for multiple days.25 In addition, performance measures implemented for HCP in hospitals may contribute to higher coverage in that work setting across occupation groups. The Centers for Medicare and Medicaid Services (CMS) required hospitals to report HCP influenza vaccination levels as part of its hospital quality reporting programs in 2013 and the coverage results are publicly available, providing an incentive for hospitals to support employee vaccination.32 The Internet panel survey also showed that influenza vaccination knowledge and awareness were higher among physicians and physician assistants/nurse practitioners compared with other HCP and among HCP working in hospital settings compared with those working in long-term care settings, indicating that vaccination knowledge and awareness among other clinical and non-clinical personnel and those working in long-term care settings could be further improved.33 While the NHIS does not collect data on vaccination-related knowledge and attitudes or employer vaccination policies, the similar pattern of coverage estimates to those found in the Internet panel surveys suggest that vaccination policies including employee education along with free access to vaccination and other vaccine promotion could be effective in increasing influenza vaccination coverage, particularly among nursing, psychiatric, and home health aide staff and HCP working in long-term care settings.
We found that vaccination coverage among HCP who have more physician contacts during the previous year and who had health insurance was significantly higher than that among those who had no physician contacts or without health insurance, and these differences remained after controlling for other demographic factors. The association of these access-to-care factors with vaccination uptake among HCP has been described previously in 2002 and in the 2004–05 influenza season, though the magnitude of effect of these factors was smaller among HCP than among non-HCP.34, 35 Among HCP, access barriers to vaccination might be overcome by providing vaccination at the workplace free of charge. Additionally, our study found that age and education were independently associated with vaccination. Those findings were consistent with previous studies.34, 35
Several limitations should be considered in interpreting these results. First, information on influenza vaccination was self-reported and may be subject to recall bias. However, self-reported seasonal influenza vaccination status has been shown to have relatively high agreement with vaccination status ascertained from medical records.36–39 Second, high-risk conditions were self-reported and not validated by medical record. Finally, to assess factors associated with vaccination (multivariable analyses), logistic regression model was used and the analysis was restricted to individuals interviewed during August 2013 through June 2014, and vaccinated in the last 12 months. The logistic regression approach may ignore the time-to-event and censoring characteristics of the influenza data. However, one study showed that the results based on a logistic regression model are similar compared with the results based on a Cox proportional hazards model which could take into account of the time-to-event and censoring issues.40
Vaccination of HCP is an important component of influenza prevention programs in the United States. Vaccination of HCP could reduce transmission of influenza in health-care settings, staff illness and absenteeism, and influenza-related morbidity and mortality.1–2, 4 Despite the availability of safe and effective influenza vaccines, influenza vaccination coverage among HCP remains suboptimal. Employers and health care administrators should make use of the Guide to Community Preventive Services, which has found evidence to support on-site vaccination at no or low cost to HCP to increase influenza vaccination coverage among HCP.27 LTC employers can also use the LTC web-based toolkit developed by CDC and the National Vaccine Program Office, which provides access to resources, strategies, and educational materials for increasing influenza vaccination among HCP in LTC settings.41 Additional approaches include: electronic tracking of coverage levels by ward, unit, and occupation, a mandatory declination policy, mask-wearing for non-vaccinated HCP, highly visible acknowledgement of vaccinated HCP, weekly compliance reports to managers and other administrators, disciplinary measures for noncompliant HCP, vaccination stations at facility entrances, and employee financial incentives for achieving high facility vaccination rates. 1–2, 4, 6–7, 27, 29, 42–43
Acknowledgments
We thank Ajay Yesupriya, Karon Lewis, and Dr. Carolyn S. Neal of the Research Data Center, National Center for Health Statistics; and Drs. Stacie M. Greby and James A. Singleton of the Immunization Services Division, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, for their important contributions.
Footnotes
Disclaimer: The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of CDC.
Conflict of Interest Statement:
All authors have no conflicts of interest to be stated.
References
- 1.Centers for Disease Control and Prevention (CDC) Immunization of health-care personnel: Recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2011;60( RR-07):1–45. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Immunization of health-care workers: Recommendations of the Advisory Committee on Immunization Practices (ACIP) and the Hospital Infection Control Practices Advisory Committee (HICPAC) MMWR Morb Mortal Wkly Rep. 1997;46(RR-18):1–42. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Prevention and control of influenza. MMWR. 1984;33(19):253–60. 265–266. [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Influenza vaccination of health-care personnel. MMWR. 2006;55(RR02):1–16. [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP) — United States, 2014–15 Influenza Season. MMWR. 2014;63(32):692–697. [PMC free article] [PubMed] [Google Scholar]
- 6.Potter J, Stott DJ, Roberts MA, Elder AG, O’Donnell B, Knight PV, et al. Influenza vaccination of health care workers in long-term-care hospitals reduces the mortality of elderly patients. J Infect Dis. 1997;175:1–6. doi: 10.1093/infdis/175.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salgado CD, Giannetta ET, Hayden FG, Farr BM. Preventing nosocomial influenza by improving the vaccine acceptance rate of clinicians. Infect Control Hosp Epidemiol. 2004;25:923–928. doi: 10.1086/502321. [DOI] [PubMed] [Google Scholar]
- 8.National Foundation for Infectious Diseases (NFID) [Accessed July 23, 2015];Influenza immunization among health care workers. Available at: http://www.nfid.org/content-conversion/pdf/publications/calltoaction.pdf.
- 9.Lemaitre M, Meret T, Rothan-Tondeur M, Belmin J, Lejonc JL, Luquel L, et al. Effect of influenza vaccination of nursing home staff on mortality of residents: a cluster-randomized trial. J Am Geriatr Soc. 2009;57:1580–1586. doi: 10.1111/j.1532-5415.2009.02402.x. [DOI] [PubMed] [Google Scholar]
- 10.Saxen H, Virtanen M. Randomized, placebo-controlled double blind study on the efficacy of influenza immunization on absenteeism of healthcare workers. Pediatr Infect Dis J. 1999;18:779–783. doi: 10.1097/00006454-199909000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Immunization Action Coalition. [Accessed July 23, 2015];Influenza vaccination honor roll. Available at: http://www.immunize.org/honor-roll/influenza-mandates.
- 12.US Department of Health and Human Services. [Accessed August 4, 2015];Immunization and infectious diseases. http://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives.
- 13.Lu PJ, Bridges CB, Euler GL, Singleton JA. Influenza vaccination of recommended adult populations, U.S., 1989–2005. Vaccine. 2008;26(14):1786–1793. doi: 10.1016/j.vaccine.2008.01.040. [DOI] [PubMed] [Google Scholar]
- 14.Lu PJ, Singleton JA, Euler GL, Williams WW, Bridges CB. Seasonal influenza vaccination of adult populations, U.S., 2005–2011. Am J Epidemiol. 2013 Nov 1;178( 9):1478–1487. doi: 10.1093/aje/kwt158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention (CDC) [Accessed July 31, 2015];National Health Interview Survey. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2013/srvydesc.pdf.
- 16.Centers for Disease Control and Prevention (CDC) [Accessed July 31, 2015];National Health Interview Survey. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2014/srvydesc.pdf.
- 17.Salgado CD, Farr BM, Hall KK, et al. Influenza in the acute hospital setting. Infect Dis. 2002;2:145–155. doi: 10.1016/s1473-3099(02)00221-9. [DOI] [PubMed] [Google Scholar]
- 18.Hayward AC, Harling R, Wetten S, Johnson AM, Munro S, Smedley J, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ. 2006;333(7581):1241. doi: 10.1136/bmj.39010.581354.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilde JA, McMillan JA, Serwint J, Butta J, O’Riordan MA, Steinhoff MC. Effectiveness of influenza vaccine in health care professionals: a randomized trial. JAMA. 1999 Mar 10;281(10):908–913. doi: 10.1001/jama.281.10.908. [DOI] [PubMed] [Google Scholar]
- 20.Miller BL, Ahmed F, Lindley MC, Wortley PM. Increases in vaccination coverage of healthcare personnel following institutional requirements for influenza vaccination: a national survey of U.S. hospitals. Vaccine. 2011;29( 50):9398–9403. doi: 10.1016/j.vaccine.2011.09.047. [DOI] [PubMed] [Google Scholar]
- 21.Weber DJ, Consoli SA, Sickbert-Bennett E, Rutala WA. Assessment of a mandatory tetanus, diphtheria, and pertussis vaccination requirement on vaccine uptake over time. Infect Control Hosp Epidemiol. 2012;33( 1):81–83. doi: 10.1086/663337. [DOI] [PubMed] [Google Scholar]
- 22.Lindley MC, Lorick SA, Spinner JR, Krull AR, Mootrey GT, Ahmed F, Myers R, Bednash GP, Cymet TC, Maeshiro R, Raines CF, Shannon SC, Sondheimer HM, Strikas RA. Student vaccination requirements of U.S. health professional schools: a survey. Ann Intern Med. 2011;154( 6):391–400. doi: 10.7326/0003-4819-154-6-201103150-00004. [DOI] [PubMed] [Google Scholar]
- 23.Babcock HM, Gemeinhart N, Jones M, Dunagan WC, Woeltje KF. Mandatory influenza vaccination of health care workers: translating policy to practice. Clin Infect Dis. 2010;50:459–464. doi: 10.1086/650752. [DOI] [PubMed] [Google Scholar]
- 24.Rakita RM1, Hagar BA, Crome P, Lammert JK. Mandatory influenza vaccination of healthcare workers: a 5-year study. Infect Control Hosp Epidemiol. 2010 Sep;31(9):881–888. doi: 10.1086/656210. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC) Influenza Vaccination Coverage Among Health-Care Personnel — United States, 2013–14 Influenza Season. MMWR. 2014;63(37):805–811. [PMC free article] [PubMed] [Google Scholar]
- 26.Hollmeyer H, Hayden F, Mounts A, Buchholz U. Review: interventions to increase influenza vaccination among healthcare workers in hospitals. Influenza Other Respir Viruses. 2013;7:604–621. doi: 10.1111/irv.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guide to Community Preventive Services. [Accessed August 8, 2015]; Available at: http://www.thecommunityguide.org/index.html.
- 28.Centers for Disease Control and Prevention (CDC) Preventing Tetanus, Diphtheria, and Pertussis Among Adults: Use of Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine-- Recommendations of the Advisory Committee on Immunization Practices (ACIP) and Recommendation of ACIP, supported by the Healthcare Infection Control Practices Advisory Committee (HICPAC), for Use of Tdap Among Health-Care. MMWR. 2006;55(RR17):1–33. [PubMed] [Google Scholar]
- 29.Drees M, Wroten K, Smedley M, Mase T, Schwartz JS. Carrots and sticks: achieving high healthcare personnel influenza vaccination rates without a mandate. Infect Control Hosp Epidemiol. 2015 Jun;36(6):717–724. doi: 10.1017/ice.2015.47. [DOI] [PubMed] [Google Scholar]
- 30.Caban-Martinez AJ, Lee DJ, Davila EP, LeBlanc WG, Arheart KL, McCollister KE, et al. Sustained low influenza vaccination rates in US healthcare workers. Prev Med. 2010 Apr;50(4):210–212. doi: 10.1016/j.ypmed.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention (CDC) Interim Results: Influenza A (H1N1) 2009 Monovalent and Seasonal Influenza Vaccination Coverage Among Health-Care Personnel --- United States, August 2009–January 2010. MMWR. 2010;59(12):357–362. [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention (CDC) Influenza Vaccination Coverage Among Health-Care Personnel — United States, 2014–15 Influenza Season. MMWR. 2015;64(36):993–999. doi: 10.15585/mmwr.mm6436a1. [DOI] [PubMed] [Google Scholar]
- 33.Lu PJ, Santibanez TA, Williams WW, Zhang J, Ding H, Bryan L, et al. Surveillance of influenza vaccination coverage - United States, 2007–08 through 2011–12 influenza seasons. MMWR Surveill Summ. 2013 Oct 25;62( Suppl 4):1–29. [PubMed] [Google Scholar]
- 34.Walker FJ, Singleton JA, Lu PJ, Wooten KG, Strikas RA. Influenza vaccination of health care workers in the United States, 1989–2002. Infect Control Hosp Epidemiol. 2006;27:257–265. doi: 10.1086/501538. [DOI] [PubMed] [Google Scholar]
- 35.Lorick SA, Wortley PM, Lindley MC, Bardenheier BH, Euler GL. U.S. Healthcare personnel and influenza vaccination during the 2004–2005 vaccine shortage. Am J Prev Med. 2008 Jun;34(6):455–462. doi: 10.1016/j.amepre.2008.01.031. [DOI] [PubMed] [Google Scholar]
- 36.Donald RM, Baken L, Nelson A, Nichol KL. Validation of self-report of influenza and pneumococcal vaccination status in elderly outpatients. Am J Prev Med. 1999;16(3):173–177. doi: 10.1016/s0749-3797(98)00159-7. [DOI] [PubMed] [Google Scholar]
- 37.Zimmerman RK, Raymund M, Janosky JE, Nowalk MP, Fine MJ. Sensitivity and specificity of patient self-report of influenza and pneumococcal polysaccharide vaccinations among elderly outpatients in diverse patient care strata. Vaccine. 2003;21:1486–1491. doi: 10.1016/s0264-410x(02)00700-4. [DOI] [PubMed] [Google Scholar]
- 38.Mangtani P, Shah A, Roberts JA. Validation of influenza and pneumococcal vaccine status in adults based on self-report. Epidemiol Infect. 2007 Jan;135(1):139–143. doi: 10.1017/S0950268806006479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rolnick SJ, Parker ED, Nordin JD, Hedblom BD, Wei F, Kerby T, et al. Self-report compared to electronic medical record across eight adult vaccines: do results vary by demographic factors? Vaccine. 2013;31(37):3928–3935. doi: 10.1016/j.vaccine.2013.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhai Y, Kahn KE, O’Halloran A, Santibanez TA. Comparing Results from Cox Proportional Hazards Models using SUDAAN® and SAS® Survey Procedures to a Logistic Regression Model for Analysis of Influenza Vaccination Coverage. SESUG Proceedings. 2015 Available at: http://www.lexjansen.com/sesug/2015/42_Final_PDF.pdf.
- 41. [Accessed January 11, 2016];The long-term care web-based toolkit. Available at: http://www.cdc.gov/flu/toolkit/long-term-care/index.htm.
- 42.Poland GA, Shefer AM, McCauley M, Webster PS, Whitely-Williams PN, Peter G, et al. Standards for adult immunization practice. Am J Prev Med. 2003;25(2):144–150. doi: 10.1016/s0749-3797(03)00120-x. [DOI] [PubMed] [Google Scholar]
- 43.Lindley MC, Horlick GA, Shefer AM, Shaw FE, Gorji M. Assessing state immunization requirements for healthcare workers and patients. Am J Prev Med. 2007 Jun;32(6):459–465. doi: 10.1016/j.amepre.2007.02.009. [DOI] [PubMed] [Google Scholar]