Abstract
A consistent relationship has been demonstrated between obesity and absenteeism in the workplace. However, most studies have focused on primarily sedentary occupational groups. Firefighting is a physically demanding profession that involves significant potential for exposure to dangerous situations and strenuous work. No studies to date have evaluated the impact of obesity on risk for absenteeism among firefighters. We examined the cross-sectional association between BMI and obesity and injury-related absenteeism. BMI, body fat percentage (BF%), waist circumference (WC), injury, and injury-related absenteeism were assessed in 478 career male firefighters. One hundred and fifteen firefighters reported an injury in the previous year and the number of days absent from work due to their injury. BMI was an independent predictor of absenteeism due to injury even after adjustment for confounding variables. Firefighters meeting the definition of class II and III obesity had nearly five times (odds ratio (OR) = 4.89; 95% confidence interval (CI) = 3.63–6.58) the number missed work days due to injury when compared to their normal weight counterparts and their elevated risk was greater than firefighters with class I obesity (OR = 2.71; 95% CI = 2.01–3.65) or those who were overweight (OR = 2.55; 95% CI = 1.90–3.41). The attributable per capita costs of class II and III obesity-related absenteeism over the last year were $1,682.90 per firefighter, $254.00 per firefighter for class I obesity, and $74.41 per firefighter for overweight. Our findings suggest that class II and III obesity were associated with substantial attributable costs to employers and our cost estimates probably underestimate the actual financial burden.
INTRODUCTION
Nonfatal occupational injuries represent a significant health problem for firefighters in the United States, with nearly 80,000 line of duty injuries reported in 2009 (1). The most common cause and type of injury is overexertion resulting in strain or sprain and the annual estimated costs for preventing and addressing firefighter injuries at a national level are estimated to $2.7–$7.8 billion dollars (2,3). Because of the ongoing epidemic of obesity in the United States (4), there has been great interest in determining whether obesity represents a significant risk factor for injury among workers and for firefighters in particular. Obese individuals may be a greater risk for occupational injury due to a number of factors including impaired mobility and fitness and apnea-related fatigue.
However, the association between body weight or obesity and risk of nonfatal occupational injury is only modest in the limited number of studies available (5,6). A more clear and significant relationship has been established between increasing BMI and/ or obesity and missed work days or “absenteeism” (7–14). The costs of missed work days also are higher among obese workers or with increasing BMI (9,12,15–18) and the national economic burden of obesity-related absenteeism has been estimated to be $4 billion annually in the United States (19).
Firefighting is a physically demanding profession that involves greater potential for exposure to dangerous situations. However, obesity and low fitness levels are a growing problem for the US fire service (20–24). Thus, it is not surprising that obesity has been found to be a significant risk factor for disability among firefighters (25). Unfortunately, no studies to date have been conducted examining the impact of increasing BMI or obesity on risk for nonfatal occupational injury-related absenteeism among firefighters. This lack of research on obesity and loss of work productivity, including absenteeism, represents a significant gap in the scientific literature (26), particularly among occupational groups engaging in strenuous and dangerous work activities such as firefighters. The purpose of this study was to examine the association between nonfatal occupational injury-related absenteeism and obesity. We were limited to injury-related absenteeism and not other forms of lost productivity (e.g., sickness-related absenteeism and presenteeism) due to the primary focus of the parent study on risk factors for occupational injuries among firefighters.
METHODS AND PROCEDURES
Participants and procedures
The protocol for the protection of human subjects for this study was approved by the institutional review board of National Development and Research Institutes. Data for this study are from the baseline evaluation of an ongoing longitudinal cohort study examining risk factors for injury and cardiovascular impairment in both career and volunteer firefighters (“A prospective evaluation of health behavior risk for injury among firefighters—the Firefighter Injury Risk Evaluation (FIRE) study”; EMW-2007-FP-02571; (20)). Firefighters from 11 randomly selected career and 13 randomly selected volunteer departments in the International Association of Fire Chief ’s Missouri Valley Region (Colorado, Iowa, Kansas, Missouri, North Dakota, Nebraska, South Dakota and Wyoming) comprised the sample for this study. Of the firefighters who were available and solicited (N = 736), 97% (N = 714) agreed to participate and were consented. Data from the volunteer firefighters (N = 214) were not used because of the focus on firefighter-related occupational injury and absenteeism and its association with obesity. In addition, data from 21 women career firefighters also were excluded due to their low number and the resulting inability to examine the potential moderating impact of gender. Thus, a total 478 career male firefighters had complete anthropometric and injury-related data, of which 115 reported any injury during the last 12 months. This group comprised the primary sample which was used to evaluate the relationship between obesity and injury-related absenteeism for this study. Greater details about the selection and recruitment process can be found in Poston and colleagues (20).
Measures
Body composition—weight, BMI, body fat percentage (BF%), and waist circumference (WC)
Height was assessed using a portable stadiometer. Body weight and BF% were determined using foot-to-foot bioelectrical impedance using the Tanita 300 (Tanita, Arlington Heights, IL). The Tanita 300 demonstrated strong concurrent validity (r = 0.94; P < 0.001; (27)) with Dual-Energy X-ray Absorptiometry for body fat assessment. The Tanita 300 is a commonly used bioelectrical impedance field measure because of its portability and accuracy in determining BF%. WC was determined using a spring-loaded nonstretchable tape measure in accordance with recommendations by US Government Obesity Guidelines (4,28,29). BMI (kg/m2) and weight status categories for BMI were computed using these standards (4,28,29).
Injury and missed work days (absenteeism) due to injury
While many studies of injury take into account only administratively reported injury and days out due to injury (i.e., injury days, workers compensation claims data, other insurance information), Pole et al. (30) found that administrative reports often underestimate the rates of injury and days of missed work. Thus, we developed an injury survey that combined questions from the National Health Interview Survey (31) and fire service-specific injury questions from the National Institute of Standards and Technology (3). Injury questions included injury type (e.g., abrasion, fracture, concussion, sprains, strains or dislocation, burns, etc.), location on body, how, when, where injury occurred, and whether any types of injury reports were filed.
Absenteeism was specifically assessed by asking firefighters how many days of work they missed in the last year due to injuries, an approach similar to that used in previous studies (e.g., refs. 7,9,12,13). Two-week test–retest reliability of this variable was very high (r = 0.925; P < 0.001) in a subset of career firefighters. Because there is no straightforward method for determining injury severity in a self-report survey, we examined participants’ responses to whether they sought medical treatment for their injury, whether they completed a department report, and/or whether they filed a Worker’s Compensation claim. We then constructed a variable combining whether or not they reported their injury to the Worker’s Compensation, their department, both, or neither. We did not include whether or not they sought medical treatment because this item largely overlapped with whether or not they filed a departmental injury report (i.e., only 5.3% of those reporting seeking medical treatment did not complete an injury report).
Depression and perceived stress, job satisfaction, and general health
The Center for Epidemiological Studies Short Depression Scale (10) was used to assess depressive symptoms (32). The 10-item version was found to have comparable reliability estimates to those reported for the original Center for Epidemiological Studies Short Depression Scale (33). For example, it had strong internal consistency (Cronbach’s α = 0.92) and test–retest reliability (r = 0.83) (32). The Perceived Stress Scale (34,35) is a 10-item measure that queries how unpredictable, overloaded, and uncontrollable individuals perceive their lives with a 5-item Likert scale response ranging from “Never” to “Very Often”.
Participants were asked to indicate their level of job satisfaction on the following item: “I am satisfied with my job at the fire department.” Response options were a five-point Likert scale ranging from “Very much disagree” to “Very much agree.” Participants also were asked to rate their current health with the item: “In general, would you say your health is:” Possible responses were “excellent”, “very good,” “good,” “fair,” and “poor.” This measure has been used in studies of self-rated health in related occupations (36).
Demographics and smoking status
Standard individual (e.g., age, marital status, educational level, etc.) and occupational history (e.g., current rank and position, years in the fire service, etc.) data were collected. Smoking status questions were modeled after national surveys such as the BRFSS (37) and smoking status was validated using breath carbon monoxide analysis (Bedront Micro III Smokerlyzer, Bedfont Scientific, Kent, England). A carbon monoxide level ≥10 ppm was used to indicate possible false negatives. The rate of false negatives in our sample was 1.3%.
Statistical analyses
All statistical analyses were conducted using IBM SPSS Statistics version 19 (SPSS, Chicago, IL) and SAS 9.2 (SAS Institute, Cary, NC). As noted earlier, female firefighters in our sample were excluded from analysis because of their small numbers in the larger study (n = 21) and the resulting inability to examine the potential moderating impact of gender. Weight status categories (4,28,29) based on BMI were computed in the following manner: (i) normal weight (18.3%; BMI ≥18 kg/ m2 but <25 kg/m2); (ii) overweight (48.7%; BMI ≥25 kg/m2 but <30 kg/ m2); (iii) class I obesity (21.7%; BMI ≥30 kg/m2 but <35 kg/m2); and (iv) class II and III obesity (10.4%; BMI ≥35 kg/m2).
Poisson regression models were used to explore associations between weight status and absenteeism due to injury because missed work days represent count outcomes with distributions that are typically skewed and with zeros representing the modal count (“0” or no missed days representing 49.6% of distribution of missed work days due to injury; (38,39)). Models were developed to examine the independent effect of BMI and the BMI categories outlined above. Potential confounding variables that have been identified in the literature or that were conceptually important were included in all models (e.g., age, years of education, race, smoking status, self-reported health, job satisfaction, perceived stress, depression, and injury severity; e.g., refs. 7,8,11,14). Injury severity was operationalized by whether the firefighter reported the injury to Worker’s Compensation and their department (34.3%), only their department (34.3%), or neither (31.4%). Output includes both β-weights for each variable and the corresponding odds ratio (OR) for each variable’s association with missed the number of missed work days due to injury.
Costs associated with missed work days due to injury were computed using standard approaches (3,15–17,40). In this case, we derived very conservative cost estimates by using a national hourly rate ($17.25; (3)) for firefighters multiplied by the number of days missed in hours + the cost “backfilling” (i.e., cost of personnel to replace the absentee injured firefighter; (3)) at time and a half (1.5 × $17.25 × the number of days missed in hours). The following formula represents how the costs of missed work days/absenteeism due to injury were computed:
The overall costs of missed work days due to injury were computed for each weight category (i.e., normal weight, overweight, obese class I, and obese class II and III) and then the excess costs attributable to overweight and obesity were calculated by subtracting the costs of missed days for the normal weight group from each of the other weight status groups. The excess costs per individual firefighter for firefighters who were overweight, class I obese, or class II and III obese were computed by dividing their total excess costs by the number of firefighters in each group.
RESULTS
Firefighters in this study (N = 478) were predominantly white (86.4%), in their late thirties (M ± s.d.; 38.2 ± 9.9), married or living with a partner (72.6%), had completed at least some college or were college graduates (82.4%) and, on average, had over one decade of service (14.0 ± 9.1 years). Most held the rank or job title of firefighter (31.8%); other ranks included firefighter/paramedic (16.9%), driver/operator (18.8%), officer (e.g., Lieutenant, Captain, etc.; 21.8%), Chief (e.g., Chief, Deputy/Assistant/Battalion Chief; 6.5%). The average weight, BMI, WC, and BF% for firefighters were 91.3 ± 15.6 kg, 28.6 ± 4.6 kg/m2, 97.2 ± 12.2 cm (38.3 ± 4.8 inches), and 25.3 ± 6.6%, respectively. Thirteen percent were current smokers.
There were 115 (24.1%) firefighters reporting an injury in the previous 12 months and this subsample is the focus of all subsequent analyses. There were no significant differences between injured and noninjured firefighters on any of the demographic characteristics or body composition indices and their demographic and body composition characteristics were nearly identical to those of the whole sample. Most of the injuries reported were musculoskeletal (77.4%) in nature and resulted in the majority of firefighters seeking medical treatment (64.6%) or completing an injury report for the department (69.3%). However, only about one-third of firefighters reported their injury to Worker’s Compensation if that was available to them. Nearly 50% of injured firefighters reported missing some work days (10.2 ± 20.4; range = 0–90) as a result of their injuries. There were no significant differences in the types of injuries reported based on BMI category or BMI.
There was no association between BMI and whether or not firefighters reported an injury. For example, the average BMI for injured (BMI = 28.7 ± 4.4) and noninjured firefighters (BMI = 28.6 ± 4.6) were statistically equivalent (BMI-F = 0.00, P = 0.988) and the proportions of obese (23.7%) vs. nonobese (25.2%) firefighters reporting any injury were similar (P = 0.719). There also was no relationship between the number of injuries reported and BMI (r = −0.041, P = 0.383). The results were unchanged after adjusting analyses for potential confounders. Finally, among those injured (n = 115), there was no relationship between whether or not they reported any missed work days due to injury and BMI (rpb = 0.153, P = 0.108) and the associations were weaker after adjustment for confounding factors.
In contrast, there was a significant relationship between number of injury-related missed work days reported and BMI using Poisson regression analysis (see Table 1).
Table 1.
Poisson regression models evaluating associations between number of missed work days and BMI and weight status categories
| Variable | β | P value | OR |
|---|---|---|---|
| Model for BMI (continuous) | |||
| Age (years) | 0.060 | <0.001 | 1.06 |
| Education (years) | −0.126 | <0.001 | 0.88 |
| Race | |||
| Minority | RG | — | 1.00 |
| White | 1.05 | <0.001 | 2.86 |
| Smoking status | |||
| Never, experimental, or former | RG | — | 1.00 |
| Current | −1.12 | <0.001 | 0.33 |
| General health | −0.588 | <0.001 | 0.56 |
| Job satisfaction | −0.122 | <0.001 | 0.89 |
| Perceived stress | 0.062 | <0.001 | 1.06 |
| Depression | −0.042 | 0.031 | 0.96 |
| Reported injury to department and/or workers compensation | |||
| Neither | RG | — | 1.00 |
| Department only | 4.702 | <0.001 | 110.17 |
| Workers compensation and department | 4.43 | <0.001 | 83.69 |
| BMI (kg/m2) | 0.085 | <0.001 | 1.09 |
| Model for BMI categories | |||
| Age (years) | 0.063 | <0.001 | 1.07 |
| Education (years) | −0.124 | 0.001 | 0.88 |
| Race | |||
| Minority | RG | — | 1.00 |
| White | 0.420 | 0.004 | 1.52 |
| Smoking status | |||
| Never, experimental, or former | RG | — | 1.00 |
| Current | −1.251 | <0.001 | 0.29 |
| General health | −0.599 | <0.001 | 0.55 |
| Job satisfaction | −0.118 | <0.001 | 0.89 |
| Perceived stress | 0.076 | <0.001 | 1.08 |
| Depression | −0.029 | 0.146 | 0.97 |
| Reported injury to department and/or workers compensation | |||
| Neither | RG | — | 1.00 |
| Department only | 4.750 | <0.001 | 115.55 |
| Workers compensation and department | 4.379 | <0.001 | 79.72 |
| Weight status categories | 0.101 | <0.001 | 1.11 |
| Normal weight | RG | — | 1.00 |
| Overweight | 0.936 | <0.001 | 2.55 |
| Obese class I | 0.995 | <0.001 | 2.71 |
| Obese class II and III | 1.586 | <0.001 | 4.89 |
Weight status categories: (i) normal weight (BMI ≥18 kg/m2 but <25 kg/m2); (ii) overweight (BMI ≥25 kg/m2 but <30 kg/m2); (iii) class I obesity (BMI ≥30 kg/m2 but <35 kg/m2); and (iv) class II and III obesity (BMI ≥35 kg/m2), were computed using current standards (4,28,29).
OR, odds ratio; RG, reference group.
BMI was an independent and significant predictor of number of missed work days due to injury even after adjustment for a number of theoretically important variables that also have been found to be associated with absenteeism. For each one unit increase in BMI, there was a corresponding 9% increase in missed work days due to injury. When we substituted other continuous body composition measures (e.g., WC and BF%), the magnitude of effect for the parameter estimates were similar to those for BMI suggesting that BMI provides a robust, easy, and accurate method for examining the association between body composition and risk of missed work days due to injury.
We also modeled BMI categorically using standard criteria (4,28,29) in our sample of 115 firefighters who reported any injury: (i) normal weight (n = 21); (ii) overweight (n = 54); (iii) class I obesity (n = 26); and (iv) class II and III obesity (n = 12; we grouped these categories together because of the small numbers in each). Firefighters meeting the definition of class II and III obesity had nearly five times (OR = 4.89; 95% confidence interval (CI) =3.63–6.58) the number injury-related missed work days when compared to their normal weight counterparts and their elevated risk was greater than firefighters with class I obesity (OR = 2.71; 95% CI = 2.01–3.65) or those who were overweight (OR = 2.55; 95% CI= 1.90–3.41).
While all groups were statistically different from the normal weight firefighters, the overlap in the confidence intervals indicates that class II and III obese and class I obese were not statistically different from each other and class I obese and overweight firefighters also were not statistically different. However, class II and III obese were significantly different from overweight firefighters. Figure 1 illustrates the number of work days due to injury missed by weight status.
Figure 1.
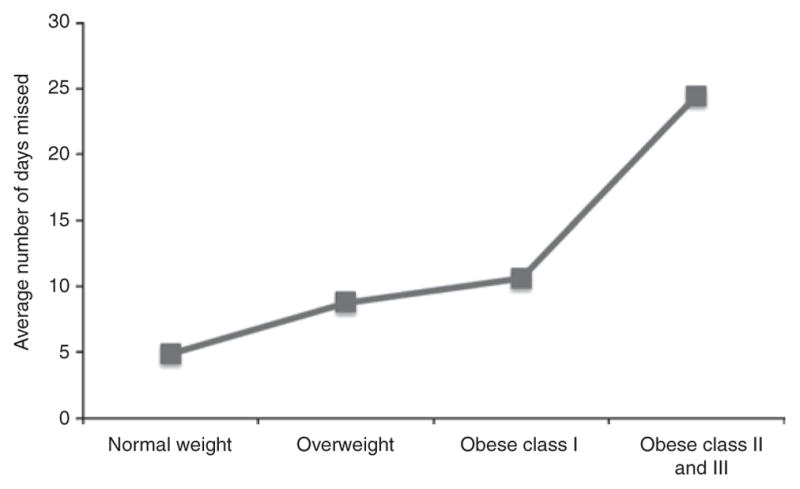
Average number of missed days due to injury by weight status.
Table 1 also presents the relationships between injury-related missed work days and the other potentially confounding variables for both models. For example, for the categorical BMI model, age, race (white vs. minority), perceived stressed, and injury severity were all positively associated with missed work days due to injury. White firefighters experienced nearly three times more missed work days due to injury when compared to their minority counterparts and for each one unit increase on the perceived stress measure, there was an 8% increased in missed work days due to injury. In contrast, greater education, higher job satisfaction and self-reported health, and current smoking all were associated with fewer missed work days due to injury and the relationship between absenteeism and depression was not significant.
The costs of absenteeism associated with excess weight were calculated by subtracting the cost of injury-related missed work days for normal weight firefighters in the last year ($5,076.43) from the costs for overweight ($9,094.58), class I obese ($11,426.40) and class II and III obese firefighters ($25,271.25), respectively. Thus, the excess costs injury-related missed work days attributable to class II and III obesity over the last year was $20,194.82 ($1,682.90 per firefighter), $6,349.97 for class I obesity ($254.00 per firefighter), and $4,018.15 for overweight ($74.41 per firefighter).
DISCUSSION
Popkin and colleagues (26) reviewed the literature on economic costs associated with obesity and concluded that there was a dearth of scientific studies evaluating the impact of obesity on productivity losses, including absenteeism, in workplace. In fact, we could only locate one study among firefighters evaluating the relationship between obesity in the workplace and a component of productivity loss (i.e., disability; (25)). This is a particularly poignant issue for firefighters, an occupational group that engages in strenuous, stressful, and often dangerous activities (e.g., rescue operations, fire suppression, and medical emergencies) and experiences high risk for exposure to dangerous environments and toxic agents.
There are a number of occupational factors that might increase firefighters risk for weight gain, obesity, and subsequent injury-related absenteeism. For example, firefighters engage in shift work and may have unhealthy diets or eating patterns structured by responding to emergencies. Shift work has been associated with weight gain and obesity risk in a number of studies (41–43) and it has been suggested that eating patterns may be negatively impacted by chronic sleep deprivation and irregular meal times (41,42). In addition, shift work and sleep disruption also may disrupt or interfere with regular physical activity (42). Currently, there are no nationally or widely agreed upon or enforced fitness or physical activity standards for firefighters, which may lead to substandard fitness levels and greater obesity risk (20,23). Finally, firefighting is a stressful career and it has been characterized as a high demand but low control profession (42). A number of studies have found positive associations between job strain/stress and BMI (41,42).
BMI and obesity, particularly class II and III combined, were significant independent predictors of injury-related absenteeism during the last year in our population-based cohort of male firefighters, even after adjustment for a number of potential confounding factors. For example, firefighters meeting the definition of class II or III obesity (BMI ≥35 kg/m2) missed nearly five times the number of work days due to injury when compared to normal weight firefighters and this is in the context that there were no substantial differences in injury frequency and type among the weight status groups. In addition, the excess costs attributable to obesity overall and per firefighter were substantial for both class I obesity and class II and III obesity combined when compared to normal weight firefighters even though the rates and types of injury were similar across weight status groups.
Our data are consistent with other studies that examined the relationship between obesity and absenteeism among other groups of workers in the United States and other western nations (7–19,44). For example, Jans and associates (10) found that obese employees in the Netherlands were absent from work 14 days more per year than normal weight employees. Similarly, workers who were class II or III obese were found to experience significantly higher probability of any missed work and more total injury-related missed work days when compared to workers in the normal weight range (9,17,19).
Similar to our cost per worker estimates of obesity-related absenteeism, several studies have demonstrated higher total costs and costs per worker associated with obesity-related absenteeism (9,12,15–18,44,45). For example, Cawley et al. (9) found that the incremental costs of obesity overall were $380 for women and $268 for men in 2004 USD, and Gates et al. (45) demonstrated that the excess costs of class II and III obesity was $433. However, it should be noted that the majority of workers in these studies were in occupations with substantially less hazards than firefighting (e.g., sales, managers, professionals, office workers, manufacturing, etc.). Average annual costs per worker associated with significant obesity have been found to be even higher in some studies and more comparable to our findings, with estimates ranging from $1191–$1683 to $1329–$1921 for class II and III obese males and female workers, respectively (16,17). Similarly, Robbins and associates (44) found that male military service personnel who exceeded their maximum allowable weights accrued 17,117 lost work days over 12 months totaling to $2.2 million annually, resulting in excess weight attributable costs of approximately $2,809.70 per male service member.
This study has a number of important strengths that should be noted. It is the first population-based study of obesity-related absenteeism and its attributable costs among firefighters. In addition, the BMI and weight status categories in our studies are based on measured weights and heights. We also assessed BF% and WC and found that the rate of false positives for BMI-based obesity classification was very low (20), thus providing us with strong assurance that our BMI data were an accurate representation of body composition in our sample. Most previous studies of obesity-related absenteeism (e.g., refs. 8,9,12,13,16,17) used self-report weight and height and had no way to determine the accuracy of the BMI-based obesity classification. Finally, absenteeism was determined in a manner comparable to other published studies (e.g., refs. 7,9,12,13,18,19) and our method of assessing it demonstrated strong test–retest reliability in this sample.
Study limitations include the fact that our sample was not ethnically diverse and the low number of women necessitated removing them from the current analysis. However, the proportions of minorities and women in our sample are representative of the fire service nationally (46). Next, we only examined absenteeism associated with an injury; however, absenteeism also can be associated with illness and other medical conditions (9,12,16,17,47). Also, the concept of lost productivity often includes presenteeism (i.e., reduced productivity at work; refs. 12,17,18,45). Therefore our conservative estimates of work days missed only due to injury and the associated costs probably underestimated the extent of the problem and financial impact in the fire service. Future studies on obesity-related absenteeism in the fire service should attempt to quantify the extent of absenteeism for reasons other than injury and also include some measure of presenteeism to ensure thorough assessments of productivity losses.
While our models were robust and adjusted for a number of potential confounding variables, we did not have a straightforward method for categorizing injury severity in our self-report survey. Nevertheless, we developed a composite variable that readily addressed the issue and still found that BMI and weight status were robust correlates of missed work days due to injury. Finally, the generalizability of our findings is potentially limited with regard to most other occupational groups because of the unique mission carried out by firefighters. Firefighters play one of the most critical roles in the United States with regard to responding to domestic emergencies, disasters, and medical crises. Thus, it is important to know how the obesity epidemic is affecting their readiness, fitness for duty, and risk for injury-related absenteeism and its associated costs. However, despite the unique and critical nature of firefighting, our attributable cost estimates were similar in magnitude to those computed for other occupational groups, some of which have similarities in job demands with firefighting (e.g., the military) and some that do not (16,17,44).
In conclusion, this is the first population-based study of obesity-related absenteeism in the US Fire Service. We demonstrated a strong and significant relationship between increasing BMI and/or weight status and the number of missed work days due to injury during the last year. In addition, we found that both class I obesity and class II and III obesity were associated with substantially greater weight-related attributable costs to employers, even though the rates and types of injuries were similar across groups. It should be noted that our cost estimates probably underestimated the actual financial impacts due to the fact that we only assessed absenteeism related to injuries during the last 12 months. Had we also been able to include missed work days/absenteeism due to other health problems and illnesses, as well as presenteeism, it is likely that the BMI and obesity-related attributable costs would have been substantially higher.
Future research should focus on replicating these results in a larger, nationally representative sample of firefighters using more liberal conceptions of lost productivity to provide more comprehensive costs estimates. Finally, interventions will need to be developed to reduce firefighter absenteeism following injuries or illness in order to ultimately improve the probability of return to work and reduce the likelihood of long-term obesity-related risk for disability (25).
Acknowledgments
This study was funded by a grant from the Assistance to Firefighters Grants program managed by the Federal Emergency Management Agency in the Department of Homeland Security (“A prospective evaluation of health behavior risk for injury among firefighters—the Firefighter Injury Risk Evaluation (FIRE) study”; EMW-2007-FP-02571). We would like to thank the departments that participated in this study.
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
References
- 1.Karter MJ, Molis JL. U.S. Firefigher Injuries – 2009. National Fire Protection Association; Quincy, MA: 2010. NFPA No. FF109. [Google Scholar]
- 2.Walton SM, Conrad KM, Furner SE, Samo DG. Cause, type, and workers’ compensation costs of injury to fire fighters. Am J Ind Med. 2003;43:454–458. doi: 10.1002/ajim.10200. [DOI] [PubMed] [Google Scholar]
- 3.National Institutes of Standards and Technology (NIST) Final report (NIST GCR 05-874) US Department of Commerce and National Institute of Standards and Technology; Gaithersberg, MD: 2005. The Economic Consequences of Firefighter Injuries and Their Prevention. [Google Scholar]
- 4.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 5.Pollack KM, Cheskin LJ. Obesity and workplace traumatic injury: does the science support the link? Inj Prev. 2007;13:297–302. doi: 10.1136/ip.2006.014787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pollack KM, Sorock GS, Slade MD, et al. Association between body mass index and acute traumatic workplace injury in hourly manufacturing employees. Am J Epidemiol. 2007;166:204–211. doi: 10.1093/aje/kwm058. [DOI] [PubMed] [Google Scholar]
- 7.Australian Institute of Health and Welfare (AIHW) Obesity and workplace absenteeism among older Australians. AIHW; Canberra: 2005. Bulletin No. 31. AIHW Cat. No. AUS 67. [Google Scholar]
- 8.Bungum T, Satterwhite M, Jackson AW, Morrow JR., Jr The relationship of body mass index, medical costs, and job absenteeism. Am J Health Behav. 2003;27:456–462. doi: 10.5993/ajhb.27.4.17. [DOI] [PubMed] [Google Scholar]
- 9.Cawley J, Rizzo JA, Haas K. Occupation-specific absenteeism costs associated with obesity and morbid obesity. J Occup Environ Med. 2007;49:1317–1324. doi: 10.1097/JOM.0b013e31815b56a0. [DOI] [PubMed] [Google Scholar]
- 10.Jans MP, van den Heuvel SG, Hildebrandt VH, Bongers PM. Overweight and obesity as predictors of absenteeism in the working population of the Netherlands. J Occup Environ Med. 2007;49:975–980. doi: 10.1097/JOM.0b013e31814b2eb7. [DOI] [PubMed] [Google Scholar]
- 11.Pronk NP, Martinson B, Kessler RC, et al. The association between work performance and physical activity, cardio respiratory fitness, and obesity. J Occup Environ Med. 2004;46:19–25. doi: 10.1097/01.jom.0000105910.69449.b7. [DOI] [PubMed] [Google Scholar]
- 12.Ricci JA, Chee E. Lost productive time associated with excess weight in the U.S. workforce. J Occup Environ Med. 2005;47:1227–1234. doi: 10.1097/01.jom.0000184871.20901.c3. [DOI] [PubMed] [Google Scholar]
- 13.Robroek SJW, van den Berg TIJ, Plat JF, Burdorf A. The role of obesity and lifestyle behaviors in a productive workforce. Occup Environ Med. 2011;68:134–139. doi: 10.1136/oem.2010.055962. [DOI] [PubMed] [Google Scholar]
- 14.Tucker LA, Friedman GM. Obesity and absenteeism: an epidemiologic study of 10,825 employed adults. Am J Health Promot. 1998;12:202–207. doi: 10.4278/0890-1171-12.3.202. [DOI] [PubMed] [Google Scholar]
- 15.Dor A, Ferguson C, Langwith C, Tan E. A heavy burden: The individual costs of being overweight an obese in the United States (Research Report) The George Washington School of Public Health and Health Services; Washington, DC: 2010. [Google Scholar]
- 16.Finkelstein E, Fiebelkorn C, Wang G. The costs of obesity among full-time employees. Am J Health Promot. 2005;20:45–51. doi: 10.4278/0890-1171-20.1.45. [DOI] [PubMed] [Google Scholar]
- 17.Finkelstein EA, DiBonaventura M, Burgess SM, Hale BC. The costs of obesity in the workplace. J Occup Environ Med. 2010;52:971–976. doi: 10.1097/JOM.0b013e3181f274d2. [DOI] [PubMed] [Google Scholar]
- 18.Trogdon JG, Finkelstein EA, Hylands T, Dellea PS, Kamal-Bahl SJ. Indirect costs of obesity: a review of the current literature. Obes Rev. 2008;9:489–500. doi: 10.1111/j.1467-789X.2008.00472.x. [DOI] [PubMed] [Google Scholar]
- 19.Sullivan PW, Ghushchyan V, Ben-Joseph RH. The effect of obesity and cardiometabolic risk factors on expenditures and productivity in the United States. Obesity (Silver Spring) 2008;16:2155–2162. doi: 10.1038/oby.2008.325. [DOI] [PubMed] [Google Scholar]
- 20.Poston WS, Haddock CK, Jahnke SA, et al. The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. J Occup Environ Med. 2011;53:266–273. doi: 10.1097/JOM.0b013e31820af362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kales SN, Polyhronopoulos GN, Aldrich JM, Leitao EO, Christiani DC. Correlates of body mass index in hazardous materials firefighters. J Occup Environ Med. 1999;41:589–595. doi: 10.1097/00043764-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Clark S, Rene A, Theurer WM, Marshall M. Association of body mass index and health status in firefighters. J Occup Environ Med. 2002;44:940–946. doi: 10.1097/00043764-200210000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Donovan R, Nelson T, Peel J, et al. Cardiorespiratory fitness and the metabolic syndrome in firefighters. Occup Med (Lond) 2009;59:487–492. doi: 10.1093/occmed/kqp095. [DOI] [PubMed] [Google Scholar]
- 24.Tsismenakis AJ, Christophi CA, Burress JW, et al. The obesity epidemic and future emergency responders. Obesity (Silver Spring) 2009;17:1648–1650. doi: 10.1038/oby.2009.63. [DOI] [PubMed] [Google Scholar]
- 25.Soteriades ES, Hauser R, Kawachi I, Christiani DC, Kales SN. Obesity and risk of job disability in male firefighters. Occup Med (Lond) 2008;58:245–250. doi: 10.1093/occmed/kqm153. [DOI] [PubMed] [Google Scholar]
- 26.Popkin BM, Kim S, Rusev ER, Du S, Zizza C. Measuring the full economic costs of diet, physical activity and obesity-related chronic diseases. Obes Rev. 2006;7:271–293. doi: 10.1111/j.1467-789X.2006.00230.x. [DOI] [PubMed] [Google Scholar]
- 27.Rubiano F, Nuñez C, Heymsfield SB. A comparison of body composition techniques. Ann N Y Acad Sci. 2000;904:335–338. doi: 10.1111/j.1749-6632.2000.tb06477.x. [DOI] [PubMed] [Google Scholar]
- 28.U.S. Department of Health and Human Services. The Surgeon General’s call to action to prevent and decrease overweight and obesity. U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General; Rockville, MD: 2001. [PubMed] [Google Scholar]
- 29.National Institutes of Health (NIH), National Heart, Lung, and Blood Institute (NHLBI) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity: The evidence report. US Government Press; Washington, DC: 1998. [Google Scholar]
- 30.Pole JD, Franche RL, Hogg-Johnson S, Vidmar M, Krause N. Duration of work disability: a comparison of self-report and administrative data. Am J Ind Med. 2006;49:394–401. doi: 10.1002/ajim.20300. [DOI] [PubMed] [Google Scholar]
- 31.National Center for Health Statistics. [Accessed 10 September 2010];National Health Interview Survey. 2007 < http://www.cdc.gov/nchs/nhis/quest_data_related_1997_forward.htm>.
- 32.Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Arch Intern Med. 1999;159:1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- 33.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 34.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 35.Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Sage; Newbury Park, CA: 1988. pp. 31–65. [Google Scholar]
- 36.Haddock CK, Poston WS, Pyle SA, et al. The validity of self-rated health as a measure of health status among young military personnel: evidence from a cross-sectional survey. Health Qual Life Outcomes. 2007;4:57. doi: 10.1186/1477-7525-4-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention (CDC) [Accessed 23 November 2010];Behavioral Risk Factor Surveillance System Questionnaire. 2010 < http://www.cdc.gov/brfss/questionnaires/pdf-ques/2010brfss.pdf>.
- 38.Cameron AC, Trivedi P. Regression Analysis of Count Outcomes. Cambridge University Press; New York: 1998. [Google Scholar]
- 39.Slymen DJ, Ayala GX, Arredondo EM, Elder JP. A demonstration of modeling count data with an application to physical activity. Epidemiol Perspect Innov. 2006;3:3. doi: 10.1186/1742-5573-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lawrence B, Bhattacharya S, Zaloshnja E, et al. Medical and Work Loss Costs Estimation Methods for the WISQARS Cost of Injury Module. Pacific Institute for Research and Evaluation (PIRE); Calverton, MD: 2009. [Google Scholar]
- 41.Schulte PA, Wagner GR, Ostry A, et al. Work, obesity, and occupational safety and health. Am J Public Health. 2007;97:428–436. doi: 10.2105/AJPH.2006.086900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kales SN, Tsismenakis AJ, Zhang C, Soteriades ES. Blood pressure in firefighters, police officers, and other emergency responders. Am J Hypertens. 2009;22:11–20. doi: 10.1038/ajh.2008.296. [DOI] [PubMed] [Google Scholar]
- 43.Karlsson B, Knutsson A, Lindahl B. Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27,485 people. Occup Environ Med. 2001;58:747–752. doi: 10.1136/oem.58.11.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robbins AS, Chao SY, Russ CR, Fonseca VP. Costs of excess body weight among active duty personnel, U.S. Air Force, 1997. Mil Med. 2002;167:393–397. [PubMed] [Google Scholar]
- 45.Gates DM, Succop P, Brehm BJ, Gillespie GL, Sommers BD. Obesity and presenteeism: the impact of body mass index on workplace productivity. J Occup Environ Med. 2008;50:39–45. doi: 10.1097/JOM.0b013e31815d8db2. [DOI] [PubMed] [Google Scholar]
- 46.Fox KA, Hornick CW, Hardin E. International Association of Fire Fighters Diversity Initiative. Achieving and Retaining a Diverse Fire Service Workforce. International Association of Fire Fighters and CWH Research, Inc; Washington, DC: 2006. [Google Scholar]
- 47.Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive work time costs from health conditions in the United States: results from the American Productivity Audit. J Occup Environ Med. 2003;45:1234–1246. doi: 10.1097/01.jom.0000099999.27348.78. [DOI] [PubMed] [Google Scholar]


