Abstract
Purpose
Recording vital signs is important in the hospital setting and the quality of this documentation influences clinical decision making. The Modified Early Warning Score (MEWS) uses vital signs to categorise the severity of a patient's physiological derangement and illustrates the clinical impact of vital signs in detecting patient deterioration and making management decisions. This descriptive study measured the quality of vital sign recordings in an acute care trauma setting, and used the MEWS to determine the impact the documentation quality had on the detection of physiological derangements and thus, clinical decision making.
Methods
Vital signs recorded by the nursing staff of all trauma patients in the acute care trauma wards at a regional hospital in South Africa were collected from January 2013 to February 2013. Investigator-measured values taken within 2 hours of the routine observations and baseline patient information were also recorded. A MEWS for each patient was calculated from the routine and investigator-measured observations. Basic descriptive statistics were performed using EXCEL.
Results
The details of 181 newly admitted patients were collected. Completion of recordings was 81% for heart rate, 88% for respiratory rate, 98% for blood pressure, 92% for temperature and 41% for GCS. The recorded heart rate was positively correlated with the investigator's measurement (Pearson's correlation coefficient of 0.76); while the respiratory rate did not correlate (Pearson's correlation coefficient of 0.02). In 59% of patients the recorded respiratory rate (RR) was exactly 20 breaths per minute and 27% had a recorded RR of exactly 15. Seven percent of patients had aberrant Glasgow Coma Scale readings above the maximum value of 15.
The average MEWS was 2 for both the recorded (MEWS(R)) and investigator (MEWS(I)) vitals, with the range of MEWS(R) 0–7 and MEWS(I) 0–9. Analysis showed 59% of the MEWS(R) underestimated the physiological derangement (scores were lower than the MEWS(I)); 80% of patients had a MEWS(R) requiring 4 hourly checks which was only completed in 2%; 86% of patients had a MEWS(R) of less than three (i.e. not necessitating escalation of care), but 33% of these showed a MEWS(I) greater than three (i.e. actually necessitating escalation of care).
Conclusion
Documentation of vital signs aids management decisions, indicating the physiological derangement of a patient and dictating treatment. This study showed that there was a poor quality of vital sign recording in this acute care trauma setting, which led to underestimation of patients' physiological derangement and an inability to detect deteriorating patients. The MEWS could be a powerful tool to empower nurses to become involved in the diagnosis and detection of deteriorating patients, as well as providing a framework to communicate the severity of derangement between health workers. However, it requires a number of strategies to improve the quality of vital sign recording, including continuing education, increasing the numbers of competent staff and administrative changes in vital sign charts.
Keywords: Vital signs recording quality, Modified early warning score, Nursing, Acute trauma care
Introduction
Recording of vital signs is an important role for nurses in the hospital setting. Previous studies have looked for ways to improve the quality of this documentation, such as that recommended by Okaisu et al in 20141, highlighting its important function and impact on clinical decision making.
The clinical impact of the quality of vital signs recording is difficult to quantify. One way is to utilise the Modified Early Warning Score (MEWS) system, a modification of the Early Warning Score proposed by Stenhouse et al in 2000, which uses vital signs to categorise the severity of a patient's physiological deterioration.2 The modified score was validated in medical admissions by Subbe et al in 20013 and shown to be of value in assessment of high care requirements of surgical in-patients by Gardner-Thorpe et all in 2006.4 It is a tool to detect physiological deterioration when it first appears in a patient's observation chart, but also provides a framework to act on any abnormalities found. It is thus an important tool in translating nurse recorded vital signs into clinical decision making by physicians.4 The MEWS determines the need for intervention based on five clinical signs, namely: heart rate (HR), respiratory rate (RR), systolic blood pressure (SBP), temperature and level of consciousness (measured by the AVPU scale – noting whether the patient is alert, responding to voice, responding to pain or unresponsive).2
Each parameter is scored according to the extent of derangement (Table 1) and the total score for all parameters is tallied to give an indication of physiological derangement and act as a guide as to the next step in management. A score of one to two should prompt four hourly vital recordings, and a score of three to six necessitates 30 min vital checks and escalation of care to a doctor's attendance. A MEWS of seven or more is a clinical emergency.2
Table 1.
Modified early warning scoring system.
| Score | 3 | 2 | 1 | 0 | 1 | 2 | 3 |
|---|---|---|---|---|---|---|---|
| Heart rate (Beat/min) | <40 | 41–59 | 51–100 | 101–110 | 111–129 | >130 | |
| Respiratory rate (Breath/min) | <8 | 9–14 | 15–20 | 21–29 | >30 | ||
| Temperature (°C) | <35.0 | 35.1–37.2 | 37.3–37.9 | >38 | |||
| CNS | Confused | Alert | Responds to voice | Responds to pain | Un-responsive | ||
| Systolic blood pressure (mmHg) | <70 | 71–80 | 81–100 | 101–199 | >200 |
The MEWS corresponds with morbidity and mortality, with a score of five or more increasing the risk of High Care or Intensive Care Unit (ICU) admission and death.3 A threshold of four or more is 75% sensitive and 83% specific for the requirement to step up the level of care to High Care or ICU.4 Thus it was designed to detect critically ill patients at risk of serious deterioration.5 It can also be used to predict hospital admission, with independent risk factors of HR more than 130 beats per minute, RR more than 30 breaths per minute, temperature greater than 38.5°C, a decreased level of consciousness and a SBP less than 100 mmHg or over 200 mmHg. It has therefore been recommended as an adjunct in triage.5
The MEWS thus demonstrates the importance of accurate vital sign recording and the impact that the vital signs can have on the management of patients. The importance of good quality recording and derangement detection is illustrated by the fact that physiological deterioration is a common antecedent of cardiac arrest, unplanned ICU admission and unexpected death.6 This means that continuous monitoring of physiological parameters is essential in order to identify acute deterioration in patients, in turn making the accurate recording and interpretation of vital signs crucial to clinical management.
This study aimed to objectively measure the quality of vital signs recording in an acute care trauma setting in a regional hospital and to translate this to a MEWS to determine the impact the documentation quality had on the detection of physiological derangements and clinical decision making.
Materials and methods
This descriptive, cross sectional study was conducted from January 2013 to February 2013 over a six week period at a regional hospital in KwaZulu-Natal, South Africa. The population studied was patients in the acute care trauma wards – this is a step down ward from high care where patients that are too ill for the general ward are monitored.
All newly admitted patients to the ward (admitted the previous evening) were sampled at 8:00 a.m. each day for six consecutive weeks. At this time, the 6:00 a.m. recorded vitals were noted. The vital signs recorded in the patient charts were HR (measured manually), RR (measured manually), SBP (measured with an automated blood pressure cuff), temperature (measured with a reusable thermometer) and Glasgow Coma Scale (GCS) (measured manually). The nursing notes make use of the GCS rather than the AVPU score as in the MEWS system. It was shown by McNarry and Goldhill in 2004 that there is good correlation between the AVPU and GCS systems,7 with each category of AVPU corresponding to GCS scores of 15, 13, 8 and 6 respectively. Thus in this study the GCS was used as a proxy for the AVPU section of the MEWS.
At the same time the RR, HR and GCS of each patient were manually measured by the investigator. These were denoted as recorded vitals (R) and investigator vitals (I). The assumption was made that the investigator recorded vitals were more controlled, with the RR and HR each counted over a full minute and the GCS score calculated after medical practitioner examination of the patient, and used as a standard against which to compare the recorded vitals. The MEWS for the recorded vitals (MEWS(R)) and investigator vitals (MEWS(I)) were calculated and compared.
There was a time delay between the recorded and investigator vitals, however during this time there were no patient-related nursing activities such as bathing, and patient activities were minimal as the nurses conducted their handover during this time. Thus external influences to change the vital signs were minimised.
Another limitation is that vital signs fluctuate constantly, so that recordings taken even directly after one another will vary. However minute to minute variation is still within a normal range, and this study identified vital signs deviating out of this normal range of variation. The MEWS compared whether recorded and investigator vitals were within the same range of derangement.
Verbal consent from each patient was obtained. Patients were not identified in the notes, rather using patient numbers, and no names were used or published. The nursing staff in the ward were not aware of the study so that the quality of observations would not be consciously or subconsciously altered, minimising observer effect on the results.
The recorded vitals and investigator vitals were compared using basic EXCEL statistical analysis, including mean, range, percentage, mode, difference and Pearson's correlation coefficient.
Results
Quality of vital sign recordings
The details of 181 patients were collected. Table 2 shows the completion of recordings as well as the average recorded values and calculated MEWS(R). The completion rates for vital signs were 81% for HR, 88% for RR, 98% for SBP, 92% for temperature and 40% for GCS. The percentage of recorded vitals that were in the normal range was 80% for HR, 3% for RR, 79% for SBP, 89% for temperature and 92% for GCS.
Table 2.
Results of recorded results.
| Physiological parameter | Percentage recorded | Percentage of those recorded that are in the normal range | Average value recorded | Range of values recorded | Average MEWS(R) | Range of MEWS(R) |
|---|---|---|---|---|---|---|
| Heart rate | 81.22 | 80.27 | 88 | 60–119 | 0 | 0–2 |
| Respiratory rate | 87.85 | 2.52 | 19 | 15–30 | 1 | 0–3 |
| Systolic blood pressure | 98.34 | 78.65 | 115.06 | 51–163 | 0 | 0–3 |
| Temperature | 92.27 | 88.62 | 36.5 | 34.8–39.1 | 0 | 0–2 |
| Glasgow Coma Scale | 40.33 | 91.78 | 15 | 14–18 | 0 | 0–1 |
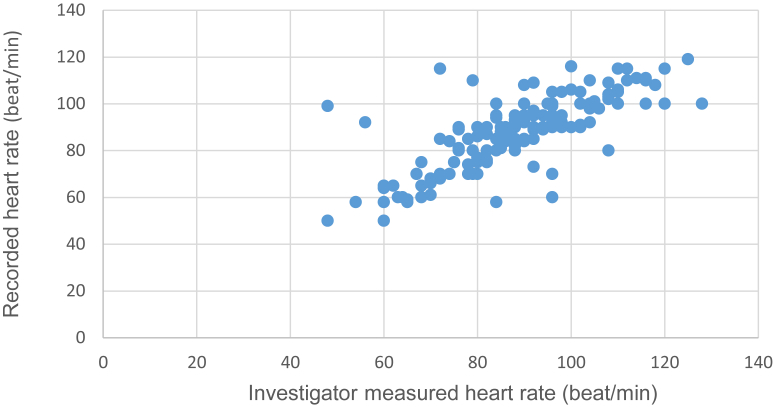
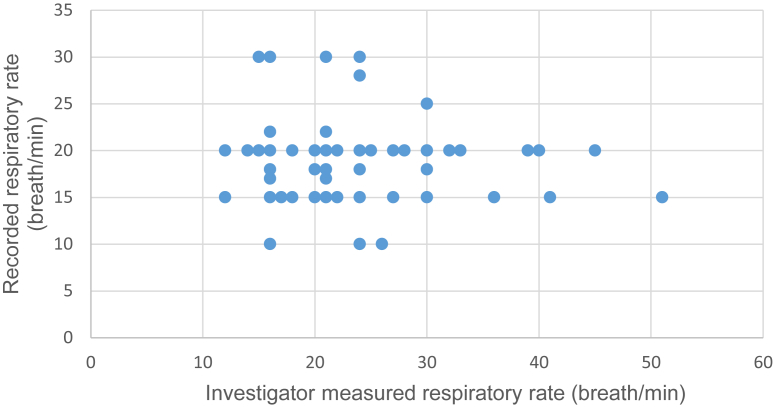
Fig. 1 shows the positive correlation of the recorded HR and investigator HR, with a Pearson correlation coefficient of 0.76. The recorded RR and investigator RR were uncorrelated, with a Pearson correlation coefficient of 0.02, as shown in Fig. 2.
Fig. 1.
Correlation of recorded and investigator measured heart rate.
Fig. 2.
Correlation of recorded and investigator measured respiratory rate.
In 59% of patients the RR(R) was exactly 20 breaths per minute and 27% of the patients had a RR(R) of exactly 15 breaths per minute. Less than 3% of patients had a GCS(R) less than 15 but 7% of the patients had aberrant readings above the maximum value of 15; 4% had a GCS of 16, 1.4% had a GCS of 17, and 1.4% had a GCS of 18.
Clinical consequences of the quality of vital signs recording
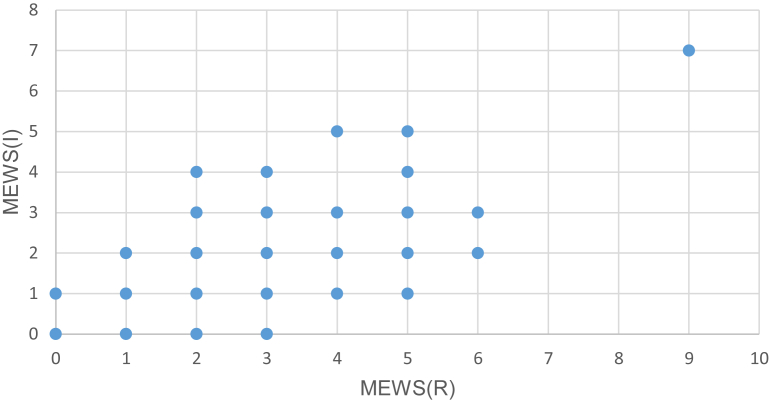
The average MEWS was 2 for both the recorded and investigator vitals, with the MEWS(R) ranging from 0 to 7 and MEWS(I) from 0 to 9. In 33% of patients, the MEWS(R) were the same as the MEWS(I), 7% of the MEWS(R) were higher than the MEWS(I), from 1 to 2 points difference, and 59% of the MEWS(R) were lower than the MEWS(I), from 1 to 4 points difference, as shown in Fig. 3.
Fig. 3.
Correlation between the MEWS(R) and MEWS(I).
Eighty percent of patients had a MEWS(R) requiring 4 hourly checks; 2% of them did have 4 hourly recordings and 98% had recordings done more than 4 hours apart.
There were 86% of patients with a MEWS(R) of less than 3 (i.e. not necessitating escalation of care); however, the MEWS(I) in 33% of them were 3 or greater (i.e. necessitating escalation of care). One patient had a MEWS(R) of 7 (i.e. necessitating emergency intervention); but the MEWS(I) for this patient was 9. No emergency escalation of care, including increased frequency of vital signs recording or obtaining a review by a doctor, was implemented.
Discussion
Quality of vital signs recording
The completion rates of vital signs recording varied greatly from 40% for GCS(R) to 98% for SBP(R). It appeared from the charts that parameters that were better completed were associated with visual cues (such as graphs for SBP and temperature) compared to the poorer completion of those that required a figure to be written in (such as GCS).
The fact that the HR(R) and HR(I) are positively correlated while the RR(R) and RR(I) are uncorrelated suggests that parameters measured by a machine (such as a pulse oximeter used to measure the HR(R)) are more accurate than those measured manually (such as RR(R)). The reasons for this are not conclusive but understaffing and nurses being pressed for time could contribute. The vital signs are also generally measured by the most junior nursing staff, often the students, who 1) may not yet be as competent as the senior staff is at measuring vital signs and 2) may not have the same appreciation of the importance of vital signs recording as the senior staff.
Eighty-six percent of patients had RR(R) of exactly 15 or 20 breaths per minute. This suggests that these values were estimated rather than manually measured. Again the reasons are unclear, but the authors postulate that time constraints and a lack of understanding of the importance of accuracy may be factors.
The aberrant GCS readings over the maximum of 15, possibly indicate a lack of understanding of the GCS system. As junior nursing staff are completing the charts, they may not have a complete knowledge of the GCS scoring system leading to the recording of unobtainable values. Education or a tick box GCS section on the chart may remedy this error.
Clinical consequences of the quality of vital signs
An important purpose of recording the vital signs is to help clinicians make management decisions. The vital signs give an indication of the physiological derangement of a patient, which in turn leads to changes in treatment and shifting of the level of care (i.e. whether or not to upscale care to an ICU setting or downscale care to the general trauma ward). The impact of the quality of vital signs is shown by the gross underestimation of physiological derangements, illustrated by the consistently lower MEWS(R) in nearly 60% of patients.
Thirty-three percent of the patients who needed upscaling of care were missed by the recorded vital signs. This means that a large population of sick patients were not detected and the severity of their physiological status would have been missed when the clinician looked at the vital sign chart. These patients would not have received the required interventions that were indicated by more accurate measurements, and this could potentially lead to poor outcomes.
Overall there was a poor quality of vital sign recording in this acute care trauma setting. This has significant implications in clinical practice, illustrated by the underestimation of physiological derangements and the inability to detect deteriorating patients.
Recommendations and conclusion
There is a need for further research into the reasons why the quality of vital sign recordings is poor, so that this can be addressed. The authors postulate time constraints and lack of knowledge as potential contributing factors, but these ideas need to be further investigated.
It appears that the charts themselves have a role to play in both the levels of completion and accuracy of vital signs recording. Dedicated areas to be filled in and graphs to be completed highlight deficiencies when they are empty, encouraging better completion rates. This administrative change would make it easier to record vitals correctly.
As highlighted by the recording of GCS values above the maximum of 15, there is a lack of understanding of the parameters being measured. Thus educational interventions are also required to provide a knowledge base to understand not only the importance of correct and complete recordings, but also to have the knowledge and skills to act on abnormal recordings. This may be the basis for future research.
The MEWS could be a powerful tool to empower nurses to be involved in the diagnosis of sick patients and the detection of deteriorating physiological states. It also provides a framework for objective measurement of the severity of the derangement and a way to easily communicate this severity between health care workers – both between nurses on different shifts and between nurses and doctors. This could go some way to improving medical record and patient care continuity. A dedicated check box on the vital signs chart could contribute to encouraging the completion of this calculation. Technology could also play a role to improve completion and quality: with the widespread use of smart phones, applications could be used to calculate the MEWS.
As explained by Okaisu et al in 20141, training of nurses alone was not sufficient to improve nursing documentation. They suggested broader changes including increasing numbers of competent staff, continuing education, redesign of documentation forms, changes in the mix of nursing skills and continuous leadership support. These changes could contribute to remedying the poor quality of vital signs and underestimation of patient deterioration found in this study.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Okaisu E., Kalikwani F., Wanyana G. Improving the quality of nursing documentation: an action research project. Curationis. 2014;37:E1–E11. doi: 10.4102/curationis.v37i2.1251. [DOI] [PubMed] [Google Scholar]
- 2.Stenhouse C., Coates S., Tivey M. Prospective evaluation of a modified early warning score to aid earlier detection of patients developing critical illness on a general surgical ward. Br J Anaesth. 2000;663:84. [Google Scholar]
- 3.Stubbe C.P., Kruger M., Rutherford P. Validation of a modified early warning score in medical admissions. QJM Int J Med. 2001;94:521–526. doi: 10.1093/qjmed/94.10.521. [DOI] [PubMed] [Google Scholar]
- 4.Gardner-Thorpe J., Love N., Wrightson J. The value of modified early warning score (MEWS) in surgical in-patients: a prospective observational study. Ann Roy Coll Surg. 2006;88:571–575. doi: 10.1308/003588406X130615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burch V.C., Tarr G., Morroni C. Modified early warning score predicts the need for hospital admission and inhospital mortality. Emerg Med J. 2008;25:674–678. doi: 10.1136/emj.2007.057661. [DOI] [PubMed] [Google Scholar]
- 6.Kause J., Smith G., Prytherch D. A comparison of antecedents to cardiac arrests, deaths and emergency intensive care admissions in Australia and New Zealand, and the United Kingdom – the ACADEMIA study. Resuscitation. 2004;62:275–282. doi: 10.1016/j.resuscitation.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 7.McNarry A.F., Goldhill D.R. Simple bedside assessment of level of consciousness: comparison of two simple assessment scales with the Glasgow Coma Scale. Anaesthesia. 2004;59:34–37. doi: 10.1111/j.1365-2044.2004.03526.x. [DOI] [PubMed] [Google Scholar]