Abstract
Importance
Unsolicited patient observations are associated with risk of medical malpractice claims. Because lawsuits may be triggered by an unexpected adverse outcome superimposed on a strained patient-physician relationship, a question remains as to whether behaviors that generate patient dissatisfaction might also contribute to the genesis of adverse outcomes themselves.
Objective
To examine whether patients of surgeons with a history of higher numbers of unsolicited patient observations are at greater risk for postoperative complications than patients whose surgeons generate fewer such unsolicited patient observations.
Design, Setting, and Participants
This retrospective cohort study used data from 7 academic medical centers participating in the National Surgical Quality Improvement Program and the Vanderbilt Patient Advocacy Reporting System from January 1, 2011, to December 31, 2013. Patients older than 18 years included in the National Surgical Quality Improvement Program who underwent inpatient or outpatient operations at 1 of the participating sites during the study period were included. Patients were excluded if the attending surgeon had less than 24 months of data in the Vanderbilt Patient Advocacy Reporting System preceding the date of the operation. Data analysis was conducted from June 1, 2015, to October 20, 2016.
Exposures
Unsolicited patient observations for the patient’s surgeon in the 24 months preceding the date of the operation.
Main Outcomes and Measures
Postoperative surgical or medical complications as defined by the National Surgical Quality Improvement Program within 30 days of the operation of interest.
Results
Among the 32 125 patients in the cohort (13 230 men, 18 895 women; mean [SD] age, 55.8 [15.8] years), 3501 (10.9%) experienced a complication, including 1754 (5.5%) surgical and 2422 (7.5%) medical complications. Prior unsolicited patient observations for a surgeon were significantly associated with the risk of a patient having any complication (odds ratio, 1.0063; 95% CI, 1.0004-1.0123; P = .03), any surgical complication (odds ratio, 1.0104; 95% CI, 1.0022-1.0186; P = .01), any medical complication (odds ratio, 1.0079; 95% CI, 1.0009-1.0148; P = .03), and being readmitted (odds ratio, 1.0088, 95% CI, 1.0024-1.0151; P = .007). The adjusted rate of complications was 13.9% higher for patients whose surgeon was in the highest quartile of unsolicited patient observations compared with patients whose surgeon was in the lowest quartile.
Conclusions and Relevance
Patients whose surgeons have large numbers of unsolicited patient observations in the 24 months prior to the patient’s operation are at increased risk of surgical and medical complications. Efforts to promote patient safety and address risk of malpractice claims should continue to focus on surgeons’ ability to communicate respectfully and effectively with patients and other medical professionals.
This cohort study uses data from the American College of Surgeons NSQIP and the Vanderbilt Patient Advocacy Reporting System to examine whether patients of surgeons with a history of higher numbers of unsolicited patient observations are at greater risk for postoperative complications than patients whose surgeons generate fewer such unsolicited patient observations.
Key Points
Question
Are patients of surgeons with a history of higher numbers of unsolicited patient observations at greater risk for postoperative complications than patients whose surgeons generate fewer such unsolicited patient observations?
Findings
Among the 32 125 patients in this cohort study, patients whose surgeons had a history of higher numbers of unsolicited patient observations had a significantly increased risk of surgical and medical complications.
Meaning
Efforts to promote patient safety and address risk of malpractice claims should continue to focus on surgeons’ ability to communicate respectfully and effectively with patients and other medical professionals.
Introduction
The distribution of malpractice claims among physicians is not random; a small number of clinicians account for a disproportionate share of total cases of and expenditures associated with malpractice. Studies designed to understand why some physicians are associated with greater numbers of malpractice claims have identified certain surgical specialties, higher clinical activity relative to peers, and unsolicited patient observations as associated with higher risk. Of the factors identified, however, unsolicited patient observations have the strongest association with risk of malpractice claims. This finding is not surprising in that interviews with families who have filed malpractice lawsuits reveal that factors other than money, such as lost trust in the physician and an unmet need for information, are primary drivers behind patients’ and families’ desire to sue a physician after an unexpected adverse outcome.
An intriguing question remains as to whether factors that generate patient dissatisfaction might also contribute to the genesis of adverse outcomes themselves. Previous studies have shown that failure to model respect affects team performance in a variety of clinical settings, including the operating room. A recent analysis of unsolicited patient observations from a single health care organization found that surgeons with higher numbers of unsolicited patient observations were associated with higher risk of complications, particularly in the most complex surgical cases. Collectively, these studies suggest that the surgeons with the highest number of unsolicited patient observations may interact with team members in the operating room and other perioperative care settings in ways that could negatively affect team performance and contribute to risk for complications. We hypothesized that patients of surgeons with higher numbers of unsolicited patient observations would be at greater risk for postoperative complications than patients whose surgeons generated fewer such unsolicited patient observations.
Methods
Setting and Data Sources
We performed a retrospective cohort study to examine the association between a patient’s risk of experiencing a complication and their surgeon’s history of unsolicited patient observations in the 24 months prior to the operation. The study used data from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) and the Vanderbilt Patient Advocacy Reporting System (PARS), an established patient reporting system used previously to study concerns about professionalism and risk of malpractice claims. Seven academic health care systems that participate in the NSQIP and the PARS program contributed data to the study. The NSQIP files provided an efficient source for identifying the cohort and supplying information about the operations, patient characteristics, and operative characteristics that might be associated with surgical and medical complications. The NSQIP uses a systematic sampling process to identify cases that is designed to avoid bias in case selection and to ensure a diverse mix of surgical cases. Surgical clinical reviewers at each site, who are trained and undergo regular audits and quality checks, collect data on more than 150 variables using standardized NSQIP definitions, including preoperative risk, intraoperative variables, and 30-day postoperative morbidity and mortality outcomes. After data are uploaded to a central NSQIP site, quality audits are performed to ensure data integrity. One site began contributing data to the NSQIP after 2011; we used data for that site from the first date that the site contributed data to the NSQIP through the end of the study period. The other 6 sites contributed data throughout the study period. The study was reviewed by the institutional review boards at each study site, including Vanderbilt University Medical Center; University of California, Los Angeles Medical Center; University of North Carolina; University of Pennsylvania Health System; Wake Forest University; Emory University School of Medicine; and Stanford University. The study qualified as nonhuman participant research pursuant to CFR 46.102(f)(2) because the deidentified information on individuals in the cohort would not readily be ascertained by the investigators.
The PARS program includes a reliable system to process and code unsolicited observations from patients and families, which allows identification and intervention with physicians at high risk for malpractice claims. Data from the PARS program for the study encompassed all previously coded observations from patients and their families attributed to any cohort member’s attending surgeon, as recorded by the medical center’s patient relations staff. Some unsolicited patient observations described behaviors that might intimidate or deter communication:
“I asked Dr Y how long he thought the operation would take. He said, ‘Look, your wife will die without this procedure. If you want to ask questions instead of allowing me to do my job, I can just go home and not do it.’”
“Dr X rushed us through the appointment so quickly; she didn’t even explain why she was recommending this procedure over other treatment approaches.”
Other unsolicited patient observations included patients’ observations of a physician’s disrespectful or rude interaction with other health care team members that might distract focus:
“I witnessed a tense exchange between Dr Z and a nurse. It was difficult to watch someone try to humiliate another person like that. I was embarrassed and it made me feel vulnerable.”
All unsolicited patient observations were uploaded securely to the PARS program database within the Vanderbilt Center for Patient and Professional Advocacy (CPPA). Individuals trained by the Vanderbilt CPPA in PARS coding reviewed unsolicited patient observations and assigned unique observations to general categories involving care and treatment, communication, respect for the patient and/or family, accessibility, and billing. Interrater reliabilities for PARS reviewers were 73% to 100% across categories. Association of an unsolicited patient observation with a physician required evidence of unequivocal documentation of the physician’s identity by the site. To avoid inclusion of unsolicited observations from patients in the cohort who experienced a complication, only observations about the surgeon from the 24 months (730 days) preceding the date of the operation were used.
To protect physician confidentiality, an independent computer analyst who did not participate in conducting the study’s analyses used a probabilistic linkage algorithm to link the NSQIP record to each surgeon’s PARS data. Once data files were linked, all identifiers for surgeons were removed and a unique number for the site and number for the surgeon were created that could not be linked to an individual.
Cohort and Follow-up
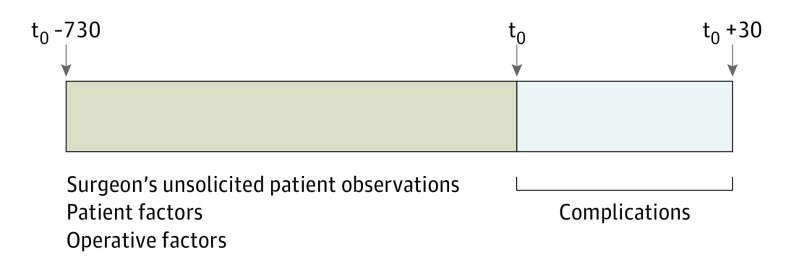
The study cohort included patients in the NSQIP database who underwent inpatient or outpatient operations between January 1, 2011, and December 31, 2013, at 1 of the participating sites. Patients were excluded if they were younger than 18 years on the date of the operation or if the attending surgeon had less than 24 months of PARS data preceding the date of the operation. Follow-up for each patient began on the date of the operation, defined as t0, and continued through the subsequent 30 days or death (Figure 1).
Figure 1. Study Design.
Association between a surgeon’s prior unsolicited patient observations and complications following operations for patients in the National Surgical Quality Improvement Program. t0 Indicates the date of the operation.
Outcomes
The primary outcome was any postoperative complication, as defined by the NSQIP, occurring within 30 days of the operation of interest. Surgical site infections and wound disruptions were considered surgical complications. Pulmonary conditions (pneumonia, reintubation, or mechanical ventilation), renal conditions (renal insufficiency or acute renal failure), stroke, cardiovascular conditions (cardiac arrest or acute myocardial infarction), thromboembolic conditions (pulmonary embolism or deep venous thrombosis), and infectious conditions (sepsis, septic shock, or urinary tract infections) were considered medical complications. Conditions included in the group of possible surgical or medical complications that were present at the time of the operative procedure were excluded. Secondary outcomes included reoperations, readmissions, and 30-day mortality.
Statistical Analysis
Statistical analysis was conducted from June 1, 2015, to October 20, 2016. Multivariable logistic regression was used to create separate models of the association between the surgeon’s total unsolicited patient observations in the 24 months preceding the date of the operation and the patient’s risk for any complication, any surgical complication, and any medical complication. Regression models using the patient as the unit of analysis included variables thought to be the most important potential confounders. Models included total unsolicited patient observations, patient factors (age, sex, race/ethnicity, body mass index, functional status, American Society of Anesthesiologists class, ventilator dependence, chronic obstructive pulmonary disease, congestive heart failure, diabetes, renal failure, and disseminated cancer), operative characteristics (surgeon specialty, number of cases contributed to the study cohort by the surgeon [as a surrogate for surgical volume], case urgency, wound classification [ie, clean vs contaminated], operative time >75th percentile for each Current Procedural Terminology code), and deidentified study site. We also analyzed the risk of complications by quartile of unsolicited patient observations (quartile 1, 0-4 observations; quartile 2, 5-9 observations; quartile 3, 10-13 observations; and quartile 4, 14-60 observations) and calculated the adjusted incidence of complications for each quartile by multiplying the unadjusted incidence rate by the rate ratio obtained from logistic regression models. We performed power calculations a priori and anticipated that, with 80% power, we would have the ability to detect an increase in complications of 1.7% between patients whose surgeons had lower numbers of unsolicited patient observations relative to patients whose surgeons had higher numbers of unsolicited patient observations.
We used R statistical software, version 3.2.3 (R Foundation for Statistical Computing) to perform all analyses. For all comparisons, α = .05 denoted a statistically significant difference.
Results
The cohort included 32 125 patients who underwent an operation performed by 1 of 817 surgeons during the study period. Patients in the cohort underwent 17 255 general surgical, 4583 orthopedic, 2288 vascular, 2139 gynecologic, 1810 plastic surgery, 1272 neurosurgical, 1118 otolaryngologic, 1046 urologic, 606 cardiothoracic, and 8 other specialty (not specified by the NSQIP) operations. In the 24 months preceding the date of the operations, surgeons of cohort patients received a mean of 10.6 unsolicited patient observations (range, 0-60) (Table 1).
Table 1. Characteristics of the Cohort Across Quartiles of the Operating Surgeon’s Unsolicited Patient Observations in the 24 Months Preceding the Operation.
| Patient Characteristic | Surgeons’ Unsolicited Patient Observations in the 24 mo Preceding the Operation, by Quartilea | ||||
|---|---|---|---|---|---|
| All (N = 32 125) |
Quartile 1 (n = 6501) |
Quartile 2 (n = 9535) |
Quartile 3 (n = 7985) |
Quartile 4 (n = 8104) |
|
| Age, mean (SD), y | 55.8 (15.8) | 55.6 (16.0) | 55.4 (16.0) | 56.1 (16.0) | 56.2 (15.4) |
| Male sex, No. (%) | 13 230 (41.2) | 2308 (35.5) | 3749 (39.3) | 3504 (43.9) | 3669 (45.3) |
| Race/ethnicity, No. (%) | |||||
| White | 23 867 (74.3) | 4717 (72.6) | 6974 (73.1) | 6018 (75.4) | 6158 (76.0) |
| Black | 5249 (16.3) | 1063 (16.4) | 1580 (16.6) | 1262 (15.8) | 1344 (16.6) |
| Other | 1112 (3.5) | 274 (4.2) | 370 (3.9) | 251 (3.1) | 217 (2.7) |
| Unknown | 1897 (5.9) | 447 (6.9) | 611 (6.4) | 454 (5.7) | 385 (4.8) |
| Dyspnea, No. (%) | |||||
| None | 29 156 (90.8) | 6083 (93.6) | 8867 (93.0) | 7129 (89.3) | 7077 (87.3) |
| With moderate exertion | 2704 (8.4) | 359 (5.5) | 604 (6.3) | 771 (9.7) | 970 (12.0) |
| At rest | 264 (0.8) | 59 (0.9) | 63 (0.7) | 85 (1.1) | 57 (0.7) |
| Functional status, No. (%) | |||||
| Independent | 31 063 (96.7) | 6296 (96.8) | 9248 (97.0) | 7727 (96.8) | 7792 (96.2) |
| Partially independent | 889 (2.8) | 168 (2.6) | 247 (2.6) | 213 (2.7) | 261 (3.2) |
| Totally dependent | 160 (0.5) | 34 (0.5) | 38 (0.4) | 41 (0.5) | 47 (0.6) |
| Unknown | 13 (0.04) | 3 (0.05) | 2 (0.02) | 4 (0.1) | 4 (0.05) |
| Diabetes, No. (%) | |||||
| None | 27 073 (84.3) | 5565 (85.6) | 8109 (85.0) | 6664 (83.5) | 6735 (83.1) |
| Type 2 | 3030 (9.4) | 542 (8.3) | 891 (9.3) | 791 (9.9) | 806 (9.9) |
| Type 1 | 2021 (6.3) | 394 (6.1) | 534 (5.6) | 530 (6.6) | 563 (6.9) |
| Ventilator dependent, No. (%) | 157 (0.5) | 35 (0.5) | 41 (0.4) | 35 (0.4) | 46 (0.6) |
| History of chronic obstructive pulmonary disease, No. (%) | 1433 (4.5) | 242 (3.7) | 339 (3.6) | 405 (5.1) | 447 (5.5) |
| History of congestive heart failure, No. (%) | 202 (0.6) | 45 (0.7) | 59 (0.6) | 57 (0.7) | 41 (0.5) |
| Preoperative renal failure, No. (%) | 94 (0.3) | 18 (0.3) | 27 (0.3) | 19 (0.2) | 30 (0.4) |
| Disseminated cancer at time of operation, No. (%) | 1448 (4.5) | 338 (5.2) | 431 (4.5) | 354 (4.4) | 325 (4.0) |
| Preoperative infection, No. (%) | 1458 (4.5) | 257 (4.0) | 430 (4.5) | 334 (4.2) | 437 (5.4) |
| Preoperative transfusion, No. (%) | 355 (1.1) | 79 (1.2) | 93 (1.0) | 73 (0.9) | 110 (1.4) |
| ASA classification, No. (%) | |||||
| No disturbance | 1875 (5.8) | 486 (7.5) | 624 (6.5) | 424 (5.3) | 341 (4.2) |
| Mild disturbance | 11 530 (35.9) | 2469 (38.0) | 3652 (38.3) | 2776 (34.8) | 2633 (32.5) |
| Severe disturbance | 16 431 (51.1) | 3088 (47.5) | 4654 (48.8) | 4192 (52.5) | 4497 (55.5) |
| Life threatening | 2177 (6.8) | 434 (6.7) | 567 (5.9) | 569 (7.1) | 607 (7.5) |
| Moribund | 83 (0.3) | 13 (0.2) | 27 (0.3) | 20 (0.3) | 23 (0.3) |
| Missing | 28 (0.1) | 11 (0.2) | 11 (0.1) | 4 (0.1) | 3 (0.04) |
| Wound class, No. (%) | |||||
| Clean | 17 029 (53.0) | 3320 (51.1) | 5078 (53.3) | 4065 (50.9) | 4566 (56.3) |
| Clean-contaminatedb | 11 667 (36.3) | 2576 (39.6) | 3467 (36.4) | 2938 (36.8) | 2686 (33.1) |
| Contaminated | 1900 (5.9) | 335 (5.2) | 560 (5.9) | 571 (7.2) | 434 (5.4) |
| Dirty-infectedc | 1528 (4.8) | 270 (4.2) | 429 (4.5) | 411 (5.1) | 418 (5.2) |
| Emergency case, No. (%) | 1716 (5.3) | 411 (6.3) | 479 (5.0) | 403 (5.0) | 423 (5.2) |
| Operating room time, mean (SD), min | 164.0 (185.0) | 161.4 (125.2) | 162.8 (122.7) | 166.6 (304.0) | 164.2 (121.9) |
| Total unsolicited patient observations prior to surgery, mean (SD) | 10.6 (7.5) | 2.3 (1.4) | 7.1 (1.4) | 11.3 (1.1) | 20.5 (7.1) |
Abbreviation: ASA, American Society of Anesthesiologists.
Quartile 1, 0-4 observations; quartile 2, 5-9 observations; quartile 3, 10-13 observations; and quartile 4, 14-60 observations.
Defined by the National Surgical Quality Improvement Program as operative wounds in which the respiratory, alimentary, genital, or urinary tracts are entered under controlled conditions and without unusual contamination.
Defined by the National Surgical Quality Improvement Program as old traumatic wounds with retained devitalized tissue and those that involve existing clinical infection or perforated viscera.
Across quartiles of unsolicited patient observations, patients were comparable in terms of age, race/ethnicity, functional status, and ventilator dependence at the time of the procedure (Table 1). Patients whose surgeons were in the highest quartile (n = 8104; 14-60 observations) were more likely than those whose surgeons were in the lowest quartile (n = 6501; 0-4 observations) to have type 1 or 2 diabetes (1369 [16.9%] vs 936 [14.4%]), dyspnea (1027 [12.7%] vs 418 [6.4%]), chronic obstructive pulmonary disease (447 [5.5%] vs 242 [3.7%]), and renal failure (30 [0.4%] vs 18 [0.3%]) but less likely to have congestive heart failure (41 [0.5%] vs 45 [0.7%]) or disseminated cancer (325 [4.0%] vs 338 [5.2%]). Patients whose surgeons were in the highest quartile were more likely than those whose surgeons were in the lowest quartile to be classified with higher preoperative American Society of Anesthesiologists risk (severe, life-threatening, or moribund: 5127 [63.3%] vs 3535 [54.4%]), but their cases were less likely to be emergency cases (423 [5.2%] vs 411 [6.3%]), and their surgical wounds were more likely to be classified by the NSQIP as clean (4566 [56.3%] vs 3320 [51.1%]) vs contaminated (434 [5.4%] vs 335 [5.2%]).
Among the patients in the cohort, 3501 (10.9%) experienced any complication, including 1754 (5.5%) surgical and 2422 (7.5%) medical complications (Table 2). Within 30 days, 1326 patients (4.1%) had to return to the operating room, 2436 (7.6%) were readmitted, and 427 (1.3%) died. Patients whose surgeons were named in more unsolicited patient observations had a higher number of complications of any type (948 of 8104 [11.7%]) than patients whose surgeons generated fewer unsolicited patient observations (622 of 6501 [9.6%]) (P = .007) (Table 2). Among surgical complications, surgical site infections had a greater increase across quartiles (lowest quartile, 279 of 6501 [4.3%]; highest quartile, 442 of 8104 [5.5%]; P = .001) than did wound disruptions (lowest quartile, 39 of 6501 [0.6%]; highest quartile, 45 of 8104 [0.6%]; P = .79). Among medical complications, sepsis (lowest quartile, 156 of 6501 [2.4%]; highest quartile, 315 of 8104 [3.9%]; P = .003) and urinary tract infection (lowest quartile, 94 of 6501 [1.4%]; highest quartile, 142 of 8104 [1.8%]; P = .003) were significantly more likely in the higher quartiles.
Table 2. Complications Across Quartiles of the Operating Surgeon’s Unsolicited Patient Observations in the 24 Months Preceding the Operation.
| Outcome | Surgeons’ Unsolicited Patient Observations in the 24 mo Preceding the Operation, by Quartile, No. (%)a | P Value | ||||
|---|---|---|---|---|---|---|
| All (N = 32 125) |
Quartile 1 (n = 6501) |
Quartile 2 (n = 9535) |
Quartile 3 (n = 7985) |
Quartile 4 (n = 8104) |
||
| Any complications | 3501 (10.9) | 622 (9.6) | 992 (10.4) | 939 (11.8) | 948 (11.7) | .007 |
| Surgical complications | ||||||
| Any surgical complication | 1754 (5.5) | 305 (4.7) | 489 (5.1) | 497 (6.2) | 463 (5.7) | .01 |
| Surgical site infection | 1640 (5.1) | 279 (4.3) | 458 (4.8) | 461 (5.8) | 442 (5.5) | .001 |
| Wound disruption | 200 (0.6) | 39 (0.6) | 56 (0.6) | 60 (0.8) | 45 (0.6) | .79 |
| Medical complications | ||||||
| Any medical complication | 2422 (7.5) | 410 (6.3) | 687 (7.2) | 633 (7.9) | 692 (8.5) | .006 |
| Pulmonary | 922 (2.9) | 143 (2.2) | 276 (2.9) | 250 (3.1) | 253 (3.1) | .25 |
| Renal | 300 (0.9) | 38 (0.6) | 94 (1.0) | 76 (1.0) | 92 (1.1) | .38 |
| Central nervous system | 77 (0.2) | 19 (0.3) | 23 (0.2) | 23 (0.3) | 12 (0.1) | .88 |
| Cardiovascular | 237 (0.7) | 38 (0.6) | 72 (0.8) | 61 (0.8) | 66 (0.8) | .88 |
| Thromboembolic | 363 (1.1) | 52 (0.8) | 119 (1.2) | 96 (1.2) | 96 (1.2) | .92 |
| Infectious sepsis | 1017 (3.2) | 156 (2.4) | 282 (3.0) | 264 (3.3) | 315 (3.9) | .003 |
| Urinary tract infection | 518 (1.6) | 94 (1.4) | 147 (1.5) | 135 (1.7) | 142 (1.8) | .003 |
| Other complications within 30 d | ||||||
| Death | 427 (1.3) | 62 (1.0) | 127 (1.3) | 116 (1.5) | 122 (1.5) | .10 |
| Reoperation | 1326 (4.1) | 250 (3.8) | 365 (3.8) | 333 (4.2) | 378 (4.7) | .28 |
| Readmission | 2436 (7.6) | 474 (7.3) | 681 (7.1) | 641 (8.0) | 640 (7.9) | .69 |
Quartile 1, 0-4 observations; quartile 2, 5-9 observations; quartile 3, 10-13 observations; and quartile 4, 14-60 observations.
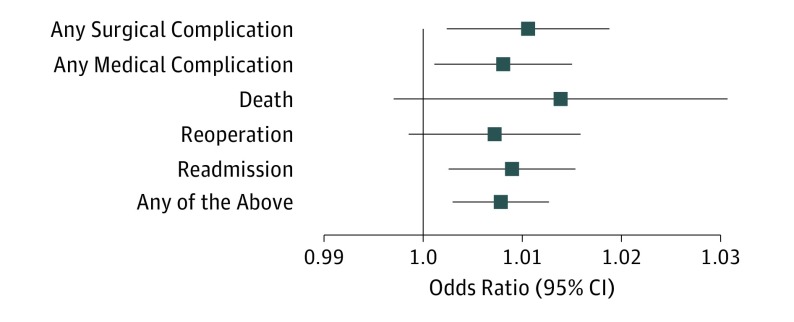
In multivariable analyses controlling for patient, surgeon, and operative characteristics, a surgeon’s prior unsolicited patient observations were significantly associated with the risk of a patient having any complication (odds ratio, 1.0063; 95% CI, 1.0004-1.0123; P = .03), any surgical complication (odds ratio, 1.0104; 95% CI, 1.0022-1.0186; P = .01), any medical complication (odds ratio, 1.0079; 95% CI, 1.0009-1.0148; P = .03), and readmission (odds ratio, 1.0088, 95% CI, 1.0024-1.0151; P = .007) (Figure 2). Each unsolicited patient observation with which the surgeon was associated in the 24 months preceding the operation significantly increased the risk for surgical and medical complications in the statistical models. There was no statistically significant association between a surgeon’s prior unsolicited patient observations and reoperation, readmission, or patient death within 30 days in multivariable models.
Figure 2. Adjusted Odds Ratios for Surgical Complications.
Adjusted for total unsolicited patient observations, patient factors (age, sex, race/ethnicity as recorded in the site’s medical record, body mass index, functional status, American Society of Anesthesiologists class, ventilator dependence, history of severe chronic obstructive pulmonary disease, history of severe congestive heart failure, diabetes prior to the procedure, hypertension requiring medication in the prior 30 days, preoperative renal failure, or disseminated cancer at the time of the operation), operative characteristics (surgeon specialty, number of cases contributed to the study cohort by the surgeon, case urgency, wound classification, long operative time [calculated as operative time >75th percentile for each Current Procedural Terminology code]), and deidentified study site. Horizontal lines indicate 95% CIs.
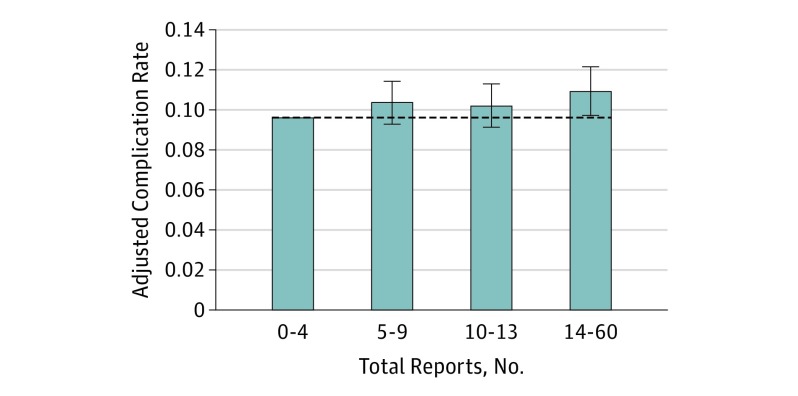
The adjusted complication rate was 13.9% higher for patients whose surgeon was in the highest quartile compared with patients whose surgeon was in the lowest quartile (Figure 3). If surgeons in the highest 3 quartiles had performed at the level of those in the first quartile, the cohort would have experienced 426 fewer complications.
Figure 3. Adjusted Complication Rate by Quartiles of the Operating Surgeon’s Unsolicited Patient Observations in the 24 Months Preceding the Operation.
Adjusted for total unsolicited patient observations, patient factors (age, sex, race/ethnicity as recorded in the site’s medical record, body mass index, functional status, American Society of Anesthesiologists class, ventilator dependence, history of severe chronic obstructive pulmonary disease, history of severe congestive heart failure, diabetes prior to the procedure, hypertension requiring medication in the prior 30 days, preoperative renal failure, or disseminated cancer at the time of the operation), operative characteristics (surgeon specialty, number of cases contributed to the study cohort by the surgeon, case urgency, wound classification, long operative time [calculated as operative time >75th percentile for each Current Procedural Terminology code]), and deidentified study site. Vertical lines indicate 95% CIs. Dashed horizontal line indicates the complication rate for the lowest quartile of unsolicited patient observations (9.6%).
Discussion
Patients whose surgeons were associated with higher numbers of unsolicited patient observations in the 24 months prior to their operation experienced more surgical and medical complications than did patients receiving care from surgeons with fewer unsolicited patient observations. The differences remained when controlling for a variety of patient, operative, and surgeon factors. The study cohort included 32 125 patients at 7 geographically diverse sites across the United States. If extrapolated to the entire United States, where 27 000 000 surgical procedures are performed annually, failures to model respect, communicate effectively, and be available to patients could contribute to more than 350 000 additional complications and more than $3 billion in additional costs to the US health care system each year.
Our study follows a previous single NSQIP site study of surgical outcomes and unsolicited patient observations, which found that patients of surgeons with high numbers of unsolicited patient observations had a greater risk of complications in more complex surgical cases than did patients of their colleagues with low numbers of unsolicited patient observations. Our study assessed risk for individual patients and controlled for several factors associated with the patient, the operation, and the surgeon. A surgeon’s unsolicited patient observations were limited to those from the 24 months prior to the operation to avoid the bias that might be introduced by including observations from patients in the cohort who experienced complications associated with the operation included in the NSQIP data. Our study was adequately powered to detect clinically relevant differences in outcomes and included a geographically diverse population, increasing the generalizability of the findings.
Patients and families are uniquely positioned to observe physicians’ behavior and performance. Although anesthetized patients cannot observe what happens in the operating arena or outside their hospital room, analysis of their collective stories offers insight into how physicians may also interact with other medical professionals. Disrespect and rudeness toward other professionals affect willingness to share information and seek help and, in turn, may affect both procedural and diagnostic performance. Concerns about a surgeon who previously lashed out at an anesthesiologist during an intraoperative emergency may distract the anesthesiologist from recognizing a change in the patient’s status or inhibit him or her from speaking up about a change in status if he or she fears the surgeon’s response. If a nurse notes a break in the sterile field or violation of safety protocols, such as surgical time-outs (a process performed immediately before the operation in which the team stops and verbally reviews pertinent information to ensure accurate patient identity, surgical site, and planned procedure), the nurse may be less likely to share his or her concerns with the team if he or she has been ignored or disrespected by the surgeon when he or she raised similar concerns in previous situations.
Our study provides additional insight into why a small subset of surgeons attracts a disproportionate share of malpractice claims. Study findings confirm that surgeons who generate more unsolicited patient observations also have patients who experience more complications. Thus, not only are patients whose surgeons fail to communicate clearly or model respect more likely to file a malpractice claim in the face of any adverse outcome but that same surgeon may be nonrandomly contributing to the unexpected adverse outcomes that lead to claims.
Our findings reinforce the importance of work to identify and address surgeons who are associated with a disproportionate share of unsolicited patient observations. Previous work using peer messengers to share comparative data with physicians who have a high amount of unsolicited patient observations reveals that most respond by generating fewer unsolicited patient observations after the intervention. It remains to be seen, but surgeons who improve their interactions, communication, and accessibility for patients may also favorably alter the work environment, contributing to enhanced team performance and reducing the likelihood of complications. Other future lines of inquiry might focus on the analysis of different types of unsolicited patient observations.
Limitations
This study has several limitations. The NSQIP uses a systematic sampling algorithm designed to avoid bias in case selection to select each participating site’s cases, so it is possible that the cases included for an individual surgeon may not reflect his or her overall experience. It is possible that some patients in the cohort had incomplete follow-up in the 30-day postoperative period, but data quality checks performed by the NSQIP are designed to reduce incomplete data, and we do not anticipate that loss to follow-up would be differentially distributed among our exposure categories. We did have complete follow-up data for all surgeons included in the study. To account for possible changes in the complexity of cases sampled by the NSQIP over time, we created an individualized 2-year time window to sample a surgeon’s unsolicited patient observations for each case. Environment and systems issues beyond a surgeon’s immediate control (eg, lost laboratory results) may lead to unsolicited patient observations. However, we included surgeons from the same institutions who presumably practice in the same environments and do not generate as many unsolicited patient observations. We also included sites in our multivariable models to account for other unmeasured factors by site (eg, types of cases sampled, variation in capture of unsolicited patient observations). Patient and operative characteristics differed across the quartiles, but patients in the higher quartiles did not consistently have a higher likelihood of having characteristics associated with risk for surgical complications. It is also possible that unmeasured factors contributed to the associations between unsolicited patient observations and complications. For example, surgeons who are more aggressive and who might offer surgery inappropriately or operate on higher-risk patients might also generate more unsolicited patient observations. However, the analysis included several variables thought to be the most important potential confounders. Another limitation arises from the fact that the study was performed at 7 large academic medical centers. Thus, the generalizability of the results to other settings, including nonteaching hospitals, is potentially limited. Nonetheless, previous work assessing the association of the risk of malpractice claims and large numbers of unsolicited patient observations found strikingly similar results between academic and community hospital settings from all regions of the country.
Conclusions
A surgeon’s pattern of generating a large number of unsolicited patient observations in the 24 months prior to a patient’s operation was associated with an increased risk of surgical and medical complications, even when controlling for patient, surgeon, and operative factors. Efforts to promote patient safety and address the risk of malpractice claims should continue to focus on surgeons’ ability to communicate respectfully and effectively with patients and other medical professionals.
References
- 1.Studdert DM, Bismark MM, Mello MM, Singh H, Spittal MJ. Prevalence and characteristics of physicians prone to malpractice claims. N Engl J Med. 2016;374(4):354-362. [DOI] [PubMed] [Google Scholar]
- 2.Moore IN, Pichert JW, Hickson GB, Federspiel C, Blackford JU. Rethinking peer review: detecting and addressing medical malpractice claims risk. Vanderbilt Law Rev. 2006;59(4):1175-1206. [Google Scholar]
- 3.Fullam F, Garman AN, Johnson TJ, Hedberg EC. The use of patient satisfaction surveys and alternative coding procedures to predict malpractice risk. Med Care. 2009;47(5):553-559. [DOI] [PubMed] [Google Scholar]
- 4.Hickson GB, Federspiel CF, Pichert JW, Miller CS, Gauld-Jaeger J, Bost P. Patient complaints and malpractice risk. JAMA. 2002;287(22):2951-2957. [DOI] [PubMed] [Google Scholar]
- 5.Stelfox HT, Gandhi TK, Orav EJ, Gustafson ML. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133. [DOI] [PubMed] [Google Scholar]
- 6.Bismark MM, Spittal MJ, Gurrin LC, Ward M, Studdert DM. Identification of doctors at risk of recurrent complaints: a national study of healthcare complaints in Australia. BMJ Qual Saf. 2013;22(7):532-540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hickson GB, Clayton EW, Githens PB, Sloan FA. Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA. 1992;267(10):1359-1363. [PubMed] [Google Scholar]
- 8.Vincent C, Young M, Phillips A. Why do people sue doctors? a study of patients and relatives taking legal action. Lancet. 1994;343(8913):1609-1613. [DOI] [PubMed] [Google Scholar]
- 9.Mitchell P, Wynia M, Golden R, et al. . Core Principles & Values of Effective Team-Based Healthcare. Washington, DC: Institute of Medicine; 2012. [Google Scholar]
- 10.Mazzocco K, Petitti DB, Fong KT, et al. . Surgical team behaviors and patient outcomes. Am J Surg. 2009;197(5):678-685. [DOI] [PubMed] [Google Scholar]
- 11.Sexton JB, Paine LA, Manfuso J, et al. . A check-up for safety culture in “my patient care area.” Jt Comm J Qual Patient Saf. 2007;33(11):645, 699-703. [DOI] [PubMed] [Google Scholar]
- 12.Fan CJ, Pawlik TM, Daniels T, et al. . Association of safety culture with surgical site infection outcomes. J Am Coll Surg. 2016;222(2):122-128. [DOI] [PubMed] [Google Scholar]
- 13.Makary MA, Sexton JB, Freischlag JA, et al. . Patient safety in surgery. Ann Surg. 2006;243(5):628-632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Profit J, Sharek PJ, Amspoker AB, et al. . Burnout in the NICU setting and its relation to safety culture. BMJ Qual Saf. 2014;23(10):806-813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wahr JA, Prager RL, Abernathy JH III, et al. ; American Heart Association Council on Cardiovascular Surgery and Anesthesia, Council on Cardiovascular and Stroke Nursing, and Council on Quality of Care and Outcomes Research . Patient safety in the cardiac operating room: human factors and teamwork: a scientific statement from the American Heart Association. Circulation. 2013;128(10):1139-1169. [DOI] [PubMed] [Google Scholar]
- 16.Catron TF, Guillamondegui OD, Karrass J, et al. . Patient complaints and adverse surgical outcomes. Am J Med Qual. 2016;31(5):415-422. [DOI] [PubMed] [Google Scholar]
- 17.Makary MA, Sexton JB, Freischlag JA, et al. . Operating room teamwork among physicians and nurses: teamwork in the eye of the beholder. J Am Coll Surg. 2006;202(5):746-752. [DOI] [PubMed] [Google Scholar]
- 18.Cochran A, Elder WB. Effects of disruptive surgeon behavior in the operating room. Am J Surg. 2015;209(1):65-70. [DOI] [PubMed] [Google Scholar]
- 19.Hickson GB, Pichert JW, Federspiel CF, Clayton EW. Development of an early identification and response model of malpractice prevention. Law Contemp Probl. 1997;60(1-2):7-29. [Google Scholar]
- 20.Pichert JW, Moore IN, Karrass J, et al. . An intervention model that promotes accountability: peer messengers and patient/family complaints. Jt Comm J Qual Patient Saf. 2013;39(10):435-446. [DOI] [PubMed] [Google Scholar]
- 21.Guillamondegui OD, Gunter OL, Hines L, et al. . Using the National Surgical Quality Improvement Program and the Tennessee Surgical Quality Collaborative to improve surgical outcomes. J Am Coll Surg. 2012;214(4):709-714. [DOI] [PubMed] [Google Scholar]
- 22.American College of Surgeons User Guide for the 2012 ACS NSQIP Participant Use Data File https://www.facs.org/~/media/files/quality%20programs/nsqip/2012pedsuserguide.ashx Published October 2013. Accessed January 12, 2017.
- 23.Ko CY, Hall BL, Hart AJ, Cohen ME, Hoyt DB. The American College of Surgeons National Surgical Quality Improvement Program: achieving better and safer surgery. Jt Comm J Qual Patient Saf. 2015;41(5):199-204. [DOI] [PubMed] [Google Scholar]
- 24.Hickson GB, Federspiel CF, Blackford J, et al. . Patient complaints and malpractice risk in a regional healthcare center. South Med J. 2007;100(8):791-796. [DOI] [PubMed] [Google Scholar]
- 25.Stimson CJ, Pichert JW, Moore IN, et al. . Medical malpractice claims risk in urology: an empirical analysis of patient complaint data. J Urol. 2010;183(5):1971-1976. [DOI] [PubMed] [Google Scholar]
- 26.Hickson G, Pichert JW. Identifying and addressing physicians at high risk for medical malpractice claims In: Youngberg B, ed. Principles of Risk Management and Patient Safety. Sudbury, Massachusetts: Jones & Bartlett Publishers Inc; 2012:347-368. [Google Scholar]
- 27.Hayden AC, Pichert JW, Fawcett J, Moore IN, Hickson GB. Best practices for basic and advanced skills in health care service recovery: a case study of a re-admitted patient. Jt Comm J Qual Patient Saf. 2010;36(7):310-318. [DOI] [PubMed] [Google Scholar]
- 28.Mukherjee K, Pichert JW, Cornett MB, Yan G, Hickson GW, Diaz JJ Jr. All trauma surgeons are not created equal: asymmetric distribution of malpractice claims risk. J Trauma. 2010;69(3):549-556. [DOI] [PubMed] [Google Scholar]
- 29.Kohanim S, Sternberg P Jr, Karrass J, Cooper WO, Pichert JW. Unsolicited patient complaints in ophthalmology: an empirical analysis from a large national database. Ophthalmology. 2016;123(2):234-241. [DOI] [PubMed] [Google Scholar]
- 30.Murff HJ, France DJ, Blackford J, et al. . Relationship between patient complaints and surgical complications. Qual Saf Health Care. 2006;15(1):13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim BD, Edelstein AI, Hsu WK, Lim S, Kim JY. Spine surgeon specialty is not a risk factor for 30-day complication rates in single-level lumbar fusion: a propensity score–matched study of 2528 patients. Spine (Phila Pa 1976). 2014;39(15):E919-E927. [DOI] [PubMed] [Google Scholar]
- 32.Cooper WO, Habel LA, Sox CM, et al. . ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365(20):1896-1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.National Center for Health Statistics, Centers for Disease Control and Prevention, US Department of Health and Human Services National Hospital Discharge Survey 2010. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHDS/NHDS_2010_Documentation.pdf. Published March 2012. Accessed January 12, 2017.
- 34.Dimick JB, Weeks WB, Karia RJ, Das S, Campbell DA Jr. Who pays for poor surgical quality? building a business case for quality improvement. J Am Coll Surg. 2006;202(6):933-937. [DOI] [PubMed] [Google Scholar]
- 35.Carayon P, Schoofs Hundt A, Karsh BT, et al. . Work system design for patient safety: the SEIPS model. Qual Saf Health Care. 2006;15(suppl 1):i50-i58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carayon P, Wood KE. Patient safety—the role of human factors and systems engineering. Stud Health Technol Inform. 2010;153:23-46. [PMC free article] [PubMed] [Google Scholar]
- 37.Shouhed D, Gewertz B, Wiegmann D, Catchpole K. Integrating human factors research and surgery: a review. Arch Surg. 2012;147(12):1141-1146. [DOI] [PubMed] [Google Scholar]
- 38.Riskin A, Erez A, Foulk TA, et al. . The impact of rudeness on medical team performance: a randomized trial. Pediatrics. 2015;136(3):487-495. [DOI] [PubMed] [Google Scholar]
- 39.Rosenstein AH, O’Daniel M. Impact and implications of disruptive behavior in the perioperative arena. J Am Coll Surg. 2006;203(1):96-105. [DOI] [PubMed] [Google Scholar]
- 40.Lingard L, Espin S, Whyte S, et al. . Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care. 2004;13(5):330-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hickson GB, Pichert JW, Webb LE, Gabbe SG. A complementary approach to promoting professionalism: identifying, measuring, and addressing unprofessional behaviors. Acad Med. 2007;82(11):1040-1048. [DOI] [PubMed] [Google Scholar]