Key Points
Question
What factors contribute to discordance between preoperative parathyroid 4-dimensional computed tomographic scans and intraoperative findings?
Findings
In an analysis of a database that included 411 patients with primary hyperparathyroidism who underwent preoperative 4-dimensional computed tomographic scans followed by parathyroidectomy, we found that the presence of multigland disease, multinodular goiter or thyroid nodule, parathyroid lesion size of 10 mm or less, and parathyroid lesion in the inferior position were associated with discordance between preoperative parathyroid 4-dimensional computed tomographic scans and intraoperative findings.
Meaning
Understanding potential limitations and factors affecting the accuracy of preoperative 4-dimensional computed tomographic scans may enable surgeons to fully leverage this new localization technique in preoperative planning and intraoperative troubleshooting.
Abstract
Importance
Parathyroid 4-dimensional computed tomographic scans (4D-CTs) have emerged as an accurate and cost-effective initial localization study for patients with primary hyperparathyroidism. However, potential limitations and factors affecting the accuracy of preoperative 4D-CTs remain poorly defined.
Objectives
To characterize factors associated with missed parathyroid lesions on preoperative 4D-CTs and to investigate patterns of commonly observed errors.
Design, Setting, and Participants
A prospectively accrued patient database was analyzed from September 1, 2011, through October 31, 2016. The study was performed in a tertiary referral center. Consecutive patients with primary hyperparathyroidism undergoing preoperative 4D-CTs and subsequent parathyroidectomy were included in the study.
Main Outcomes and Measures
Discordance between preoperative 4D-CTs and intraoperative findings in the number and location of abnormal parathyroid lesions.
Results
Of 411 patients studied (mean [SD] age, 59 [14] years; 325 [79.1%] female), 123 (29.9%) had discordance between preoperative 4D-CTs and intraoperative findings. Among the 411 patients, 75 (18.2%) had major discordance, including incorrectly localized adenoma on the contralateral side of the neck, missed double adenoma, and absence of any abnormal lesion detected on 4D-CTs. Compared with concordant cases, discordant cases had higher frequencies of multigland disease (66.7% [82 of 123] vs 24.3% [70 of 288], P < .001) and multinodular goiter or thyroid nodule (40.7% [50 of 123] vs 29.2% [84 of 288], P = .02). Missed parathyroid lesions were smaller (mean [SD], 0.86 [0.29] vs 1.24 [0.50] cm; P < .001) and were more likely to be in the inferior position (65.4% [87 of 133] vs 38.1% [177 of 465], P < .001). Parathyroid lesion size of 10 mm or less (odds ratio [OR], 4.37; 95% CI, 2.24-8.54), multigland disease (OR, 7.63; 95% CI, 3.49-16.69), multinodular goiter or thyroid nodule (OR, 1.82; 95% CI, 1.01-3.28), and parathyroid lesion in the inferior position (OR, 6.82; 95% CI, 3.10-14.99) were independently associated with discordant 4D-CT results.
Conclusions and Relevance
Multigland disease was most strongly associated with discordance between preoperative 4D-CTs and intraoperative findings, followed by parathyroid lesion in the inferior position and parathyroid lesion size of 10 mm or less. Awareness of these potential pitfalls may allow surgeons to better leverage this new localization technique in preoperative planning and intraoperative troubleshooting.
This study of patients with primary hyperparathyroidism characterizes factors associated with missed parathyroid lesions on preoperative 4-dimensional computed tomographic scans and investigates patterns of commonly observed errors.
Introduction
Preoperative imaging in patients with primary hyperparathyroidism guides surgical planning and improves operative outcomes. In addition to conventional localization techniques of ultrasound (US) and sestamibi single-photon emission computed tomography (SPECT), 4-dimensional computed tomographic scans (4D-CTs) have emerged in major hospitals as a highly accurate and cost-effective initial localizing study for patients with parathyroid disease.
Although 4D-CTs have been shown to have superior sensitivity compared with US and sestamibi SPECT, missed lesions can still occur with this technique, which is especially true in cases of multigland disease (MGD), for which 4D-CT sensitivity remains as low as 32% to 53%. In clinical practice, failure of preoperative imaging to identify all abnormal parathyroid glands may increase the risk of failed parathyroidectomy. Unlike well-established localization techniques of US and sestamibi SPECT, 4D-CTs remain a new technique to many surgeons. As such, it is critical that surgeons become aware of potential limitations and factors that may influence the accuracy of 4D-CTs.
The aim of this study was to characterize factors associated with discordant results between preoperative 4D-CTs and intraoperative findings during parathyroidectomy. Furthermore, we sought to identify commonly observed error patterns, including locations of abnormal parathyroid glands that are more likely to be missed on 4D-CTs.
Methods
Study Participants
Patients with biochemical evidence of primary hyperparathyroidism who underwent 4D-CTs were included in a prospective database between September 1, 2011, and October 31, 2016. The study was performed in a tertiary referral center. Relevant clinical information, CT-derived data, and operative findings were recorded. Consecutive patients with primary hyperparathyroidism undergoing preoperative 4D-CTs and subsequent parathyroidectomy were analyzed in the present study, including primary and reoperative patients with parathyroidectomy. Patients who subsequently underwent a successful parathyroidectomy, defined as an intraoperative parathyroid hormone (PTH) level drop of 50% or more from the baseline value, were included in this study. For patients with available follow-up information, calcium levels were checked to assess for eucalcemia at or beyond 6 months after surgery. This study was performed with approval from the University of California, Los Angeles (UCLA) Institutional Review Board and with a waiver of informed consent and a waiver of Health Insurance Portability and Accountability Act of 1996 authorization.
Preoperative Localization of Parathyroid Lesions With 4D-CTs
The 4D-CT protocol included noncontrast, arterial phase, and delayed phase images from the hard palate to the carina as previously described. Parathyroid lesions were characterized using a system based on anteroposterior location relative to the expected course of the recurrent laryngeal nerve in the tracheoesophageal groove. Lesions posterior to the expected course of the nerve were defined as superior parathyroid glands, and those anterior to the recurrent laryngeal nerve were defined as inferior parathyroid glands. Location along a superoinferior axis was also described using the thyroid isthmus and the lower edge of the thyroid gland as landmarks. Radiology reports were generated by one of us (A.R.S.), who is a subspecialty-certified neuroradiologist with more than 10 years of experience in CT interpretation, including 6 years of experience in interpretation of 4D-CTs.
Determination of Concordance Between Preoperative 4D-CTs and Intraoperative Findings
All parathyroid lesions were classified as correctly or incorrectly localized on 4D-CTs by correlating the operative notes with the original radiology reports and using anatomic landmarks reported in the operative and radiology reports. Gland sizes were obtained from the operative notes and were based on the largest dimension measured. Determination of single-gland disease (SGD) (ie, 1 abnormal gland) or MGD (ie, 2-3 abnormal glands or 4-gland hyperplasia) was made based on operative findings (size, color, and overall appearance) in conjunction with sufficient drop in PTH level (intraoperative PTH level drop ≥50%). Based on surgeon preference, patients included in the study underwent either routine 4-gland exploration with direct visual inspection of all parathyroid glands or focused image-guided parathyroidectomy. To avoid the surgical approach from confounding the evaluation of 4D-CT accuracy, only those glands that were removed for high clinical suspicion with pathological confirmation of hypercellular parathyroid tissue were considered for determination of 4D-CT accuracy. Correct localization of all abnormal glands on 4D-CTs was defined as concordant, while those with 1 or more missed or incorrectly localized lesions were defined as discordant. Surgical findings were considered to be the criterion standard for identifying abnormal parathyroid glands.
Discordant 4D-CTs were further classified as having major or minor discordance based on potential implications for the surgical approach and outcomes. Major discordance included the following types of errors: (1) abnormal gland found on the opposite side of the neck (right vs left), (2) SGD indicated by 4D-CTs but MGD found at surgery, (3) MGD indicated by 4D-CTs but SGD found at surgery, and (4) no abnormal lesions found on 4D-CTs. These types of discordance can either lead to failed unilateral neck exploration (1 and 2) or influence surgeons to choose 4-gland exploration when focused parathyroidectomy was in fact possible (3 and 4). Minor discordance included abnormal gland found on the same side of the neck but in the wrong location (superior vs inferior) and MGD found on both 4D-CTs and surgery but with the wrong number or location of abnormal lesions noted on 4D-CTs. These errors were deemed minor because they have minimal influence on surgical planning and outcomes.
Analysis of Factors Associated With Discordant 4D-CTs
Concordant and discordant cases were compared to identify factors contributing to inaccurate lesion localization by 4D-CTs. Clinical factors included age, sex, body mass index (BMI), SGD vs MGD, lesion size and location, multinodular goiter or thyroid nodule (>5 mm), prior thyroid or parathyroid surgery, and history of hypothyroidism. These factors were further evaluated using univariate and multivariable logistic regression analysis. The χ2 test was used to evaluate categorical data, and the t test was used for continuous variables. Two-sided P < .05 was the threshold used for statistical significance for all tests. Statistical analyses were performed using a software program (SAS Enterprise, version 4.2; SAS Institute Inc).
Results
Study Cohort
During the study period, there were 640 patients with primary hyperparathyroidism who underwent a total of 660 4D-CTs. Patients were excluded if they did not have a parathyroidectomy performed at UCLA (n = 227) or if their parathyroidectomy was not successful (intraoperative PTH level drop <50%) (n = 2). The final study cohort consisted of the remaining 411 patients (mean [SD] age, 59 [14] years; 325 [79.1%] female), 123 (29.9%). Follow-up information of at least 6 months was available for 165 of 411 patients (40.1%). For patients with 6-month follow-up data available, all had remained eucalcemic at or beyond the 6-month benchmark.
4D-CT Localization Performance
Discordance between preoperative 4D-CTs and intraoperative findings was noted in 123 of 411 patients (29.9%). Among these patients, 107 cases were associated with 1 or more missed parathyroid adenomas. Preoperative, surgeon-performed US was done in all patients. The US and 4D-CT results were similar in 184 of 411 patients (44.8%). When US and 4D-CT findings did not match, most intraoperative findings were concordant with the 4D-CT findings as opposed to the US findings (178 of 227 [78.4%] vs 20 of 227 [8.8%]); in the remaining cases (12.7%), the intraoperative finding matched with neither US nor 4D-CTs (eFigure in the Supplement). In 20 cases, preoperative US had identified the parathyroid lesion missed on 4D-CTs. The sensitivity and specificity for quadrant localization in SGD were 90.7% and 94.7%, respectively. For MGD detection, the sensitivity and specificity were 45.3% and 87.2%, respectively. When defining an accurate 4D-CT localization study as lacking major discordance, the overall accuracy was 81.7%. Using a stricter definition for accurate localization (ie, lack of major and minor discordances), the overall accuracy was 70.0%.
Clinical Factors Associated With Discordant 4D-CT Findings
Compared with concordant cases, discordant cases were associated with higher frequencies of MGD (66.7% [82 of 123] vs 24.3% [70 of 288], P < .001) and multinodular goiter or thyroid nodule (40.7% [50 of 123] vs 29.2% [84 of 288], P = .02). Abnormal glands missed on 4D-CTs were smaller compared with those that were identified before surgery (mean [SD], 0.86 [0.29] vs 1.24 [0.50] cm; P < .001) and were more likely to be in the inferior position (65.4% [87 of 133] vs 38.1% [177 of 465], P < .001). Patients with prior thyroid or parathyroid surgery were observed less frequently in the discordant group. Intended surgical approach was not associated with concordance between preoperative 4D-CTs and intraoperative findings (Table 1).
Table 1. Clinical Characteristics of Patients With Discordant vs Concordant Parathyroid 4-Dimensional Computed Tomographic Scans.
| Variable | Discordant (n = 123) |
Concordant (n = 288) |
P Value |
|---|---|---|---|
| Age, mean (SD), y | 58.8 (13.2) | 60.9 (14.8) | .38 |
| Female, No. (%) | 97 (78.9) | 228 (79.2) | .95 |
| BMI, mean (SD) | 27.3 (6.4) | 27.6 (5.9) | .54 |
| Multigland disease, No. (%) | 82 (66.7) | 70 (24.3) | <.001 |
| Multinodular goiter or thyroid nodule, No. (%) | 50 (40.7) | 84 (29.2) | .02 |
| Prior thyroid or parathyroid surgery, No. (%) | 14 (11.4) | 82 (28.5) | <.001 |
| History of hypothyroidism, No. (%) | 30 (24.4) | 67 (23.3) | .06 |
| Parathyroid lesion size, mean (SD), cm | 0.86 (0.29) | 1.24 (0.50) | <.001 |
| Parathyroid lesion in the inferior position, No./total No. (%) | 87/133 (65.4) | 177/465 (38.1) | <.001 |
| Intended surgical approach, No. (%) | |||
| Focused parathyroidectomy | 39 (31.7) | 109 (37.8) | .24 |
| 4-Gland exploration | 84 (68.3) | 179 (62.2) |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
In univariate analysis, factors associated with discordant 4D-CT findings included parathyroid lesion size of 10 mm or less (odds ratio [OR], 8.27; 95% CI, 4.62-14.82), MGD (OR, 5.68; 95% CI, 3.59-8.98), multinodular goiter or thyroid nodule (OR, 1.66; 95% CI, 1.07-2.58), and parathyroid lesion in the inferior position (OR, 4.85; 95% CI, 2.57-9.15). Prior thyroid or parathyroid surgery was protective against discordant 4D-CT findings (OR, 0.32; 95% CI, 0.18-0.60), while BMI and intended surgical approach were not statistically significant predictors (Table 2).
Table 2. Patient and Parathyroid Lesion Factors Associated With Discordant Parathyroid 4-Dimensional Computed Tomographic Scans.
| Variable | Odds Ratio (95% CI) | P Value |
|---|---|---|
| Univariate Analysis | ||
| Age | 0.99 (0.98-1.01) | .33 |
| Female | 1.24 (0.71-2.18) | .44 |
| BMI | 0.99 (0.97-1.02) | .61 |
| Parathyroid lesion size ≤10 mm | 8.27 (4.62-14.8) | <.001 |
| Multigland disease | 5.68 (3.59-8.98) | <.001 |
| Multinodular goiter or thyroid nodule | 1.66 (1.07-2.58) | .02 |
| Prior thyroid or parathyroid surgery | 0.32 (0.18-0.60) | <.001 |
| Hypothyroidism | 1.06 (0.65-1.74) | .81 |
| Inferior parathyroid glands | 4.85 (2.57-9.15) | <.001 |
| Intended surgical approach | ||
| Focused parathyroidectomy | 1 [Reference] | .24 |
| 4-Gland exploration | 1.31 (0.84-2.07) | |
| Multivariable analysis | ||
| Parathyroid lesion size ≤10 mm | 4.37 (2.24-8.54) | <.001 |
| Multigland disease | 7.63 (3.49-16.69) | <.001 |
| Multinodular goiter or thyroid nodule | 1.82 (1.01-3.28) | .046 |
| Prior thyroid or parathyroid surgery | 0.41 (0.17-0.98) | .045 |
| Inferior parathyroid glands | 6.82 (3.10-14.99) | <.001 |
Abbreviation: BMI, body mass index.
In multivariable analysis, parathyroid lesion size of 10 mm or less (OR, 4.37; 95% CI, 2.24-8.54), MGD (OR, 7.63; 95% CI, 3.49-16.69), multinodular goiter or thyroid nodule (OR, 1.82; 95% CI, 1.01-3.28), and parathyroid lesion in the inferior position (OR, 6.82; 95% CI, 3.10-14.99) remained associated with discordance between preoperative 4D-CTs and intraoperative findings. Prior thyroid or parathyroid surgery remained protective against discordant 4D-CT results (Table 2).
Reasons for Major and Minor Discordances
We analyzed the 4D-CT results and corresponding surgical findings of the 123 discordant cases. We found major discordances in 75 cases, of which 41.3% (n = 31) occurred in patients with SGD found at the time of surgery (Table 3). The most common errors included SGD incorrectly identified as MGD on 4D-CTs (n = 16) and no abnormal glands detected on 4D-CTs (n = 12). Finding a single abnormal gland on the side opposite from 4D-CT localization was rare, occurring in only 3 patients. Errors leading to missed MGD were also common, occurring in 58.7% (44 of 75). These cases were frequently misdiagnosed as SGD on preoperative imaging when in fact patients had MGD identified during surgery.
Table 3. Major and Minor Discordance Between Parathyroid 4-Dimensional Computed Tomographic Scans (4D-CTs) and Surgical Findings.
| Variable | No. |
|---|---|
| Reasons for Major Discordance | |
| Single-gland disease (n = 31) | |
| Single-gland disease on 4D-CTs, but incorrect laterality (right vs left) found in surgery | 3 |
| Multigland disease on 4D-CTs, but single-gland disease found in surgery | 16 |
| No abnormal gland on 4D-CTs, but single-gland disease found in surgery | 12 |
| Multigland disease (n = 44) | |
| Single-gland disease on 4D-CTs, but multigland disease found in surgery | 34 |
| No abnormal gland on 4D-CTs, but multigland disease found in surgery | 10 |
| Reasons for Minor Discordance | |
| Single-gland disease (n = 9) | |
| Single-gland disease on 4D-CTs, but incorrect location (superior vs inferior) found in surgery | 9 |
| Multigland disease (n = 39) | |
| Multigland disease on 4D-CTs, but incorrect number of abnormal glands and/or locations found in surgery | 39 |
Minor discordance was identified in 48 cases (Table 3). Most minor discordances were in patients with MGD, occurring in 81.3% (n = 39). These discordances were due to correct identification of MGD on 4D-CTs but incorrect numbers or locations of abnormal glands.
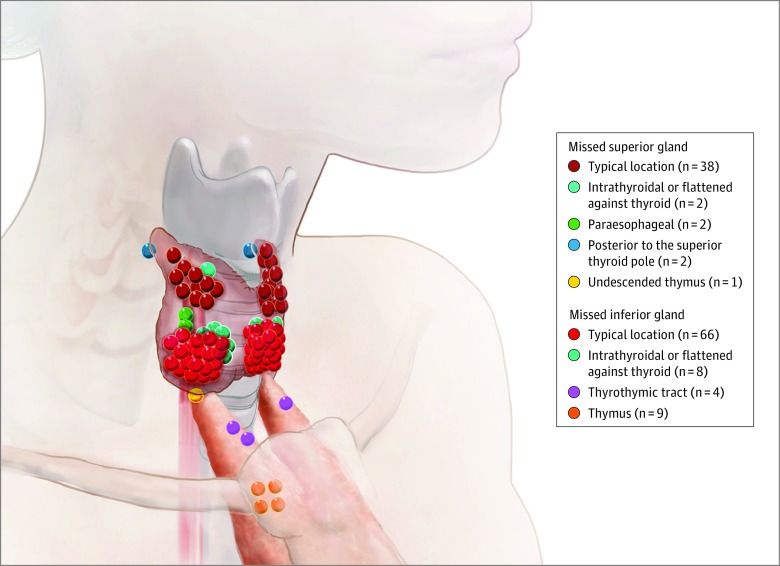
Locations of Missed Parathyroid Lesions
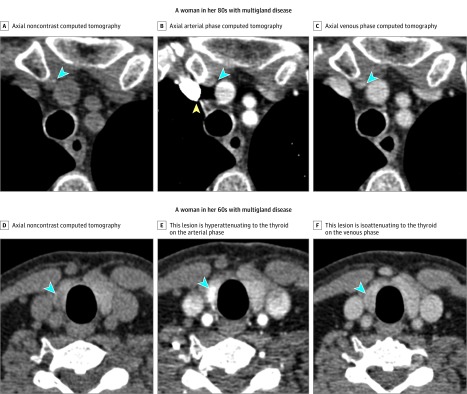
Locations of missed parathyroid lesions were determined by correlating the operative notes with the corresponding original radiology reports. Most missed glands were found in the expected anatomic location at the time of surgery (Figure 1). Missed glands were more common in the inferior position (34.5% [46 of 133] superior vs 65.4% [87 of 133] inferior). Glands that were either intrathyroidal or flattened against the thyroid comprised 7.5% (2 of 133) of all missed glands. Figure 2 (top panel) shows a missed inferior mediastinal lesion in a patient with MGD. Figure 2 (bottom panel) shows a missed right inferior intrathyroidal lesion that was mistaken for a thyroid nodule in a patient with MGD.
Figure 1. Locations of Missed Parathyroid Adenomas.
All parathyroid lesions that were missed on preoperative 4-dimensional computed tomographic scans are shown. Most missed glands were found in the expected anatomic location at the time of surgery. Missed glands were more common in the inferior position.
Figure 2. Examples of Discordant Parathyroid 4-Dimensional Computed Tomographic Scans.
The arrowheads point to the location of a candidate intrathyroidal lesion. The top panel shows that an ectopic right inferior gland in the mediastinum was missed on initial review. A, Axial noncontrast computed tomography through the superior mediastinum shows a small nodule anteromedial to the right brachiocephalic vein, just deep to the manubrium of the sternum. B, Axial arterial phase computed tomography shows some enhancement in this lesion, the degree of which is not well determined due to streak artifact from the adjacent inflowing contrast bolus (arrowhead). C, Axial venous phase computed tomography shows similar or slightly greater attenuation in this lesion compared with the arterial phase. This finding was misinterpreted as a reactive lymph node. Two other candidate lesions were identified on this study reflecting hyperplastic orthotopic right superior and left superior glands (not shown), both of which were also abnormal at surgery. The bottom panel shows that a right inferior intrathyroidal parathyroid lesion was mistaken on initial review as a thyroid nodule. D, Axial noncontrast computed tomography is shown. E, This lesion is hyperattenuating to the thyroid on the arterial phase. F, This lesion is isoattenuating to the thyroid on the venous phase. Although this enhancement pattern is also typical of parathyroid adenoma, the lesion was initially dismissed as a likely benign thyroid nodule due to the presence of 2 other high-suspicion candidates, both of which were also abnormal at surgery.
Subgroup Analysis for Patients With Available 6-Month Follow-up Information
We performed a subgroup analysis among only patients with confirmed eucalcemia at or beyond 6 months after surgery (n = 165). A multivariable analysis within this subgroup identified the same variables as found above (Clinical Factors Associated With Discordant 4D-CT Findings subsection in the Results section) to be independent risk factors of discordant 4D-CT results, including the following: parathyroid lesion size of 10 mm or less (OR, 6.52; 95% CI, 2.59-18.45), MGD (OR, 5.27; 95% CI, 1.85-16.38), multinodular goiter or thyroid nodule (OR, 2.28; 95% CI, 1.05-5.09), and parathyroid lesion in the inferior position (OR, 7.41; 95% CI, 2.73-22.76).
Discussion
Parathyroid 4D-CTs have emerged as one of the most accurate preoperative imaging modalities to localize abnormal parathyroid glands. Despite this use, missed lesions and incorrect localization still occur. To our knowledge, the present study represents the largest series to date evaluating factors associated with discordance between preoperative 4D-CTs and intraoperative findings. Parathyroid lesion size of 10 mm or less, MGD, multinodular goiter or thyroid nodule, and parathyroid lesion in the inferior position were found to be risk factors for discordant 4D-CT findings.
The discordance rate between preoperative 4D-CTs and intraoperative findings was 29.9% (123 of 411) in our study. Most were cases of major discordance that could potentially influence the surgical approach and outcome. Multigland disease was most strongly associated with discordance between preoperative 4D-CTs and intraoperative findings, which is consistent with previous reports that suggest suboptimal sensitivities of 4D-CTs for MGD at 32% to 53%. While some studies have shown superior sensitivity of 4D-CTs in detecting MGDs over US or sestamibi SPECT, our findings indicate that MGD remains a major source of error in 4D-CTs. This result is reflected in the finding that 67.4% (83 of 123) of all errors in 4D-CT localization occurred in patients with MGD. Furthermore, MGD was the most common source of error in 4D-CT localization studies overall, suggesting that the reported relative superiority of 4D-CTs over US and sestamibi SPECT in MGD detection is only modest. Although 4D-CTs may be the least operator dependent compared with US or sestamibi SPECT, detection of MGD continues to remain a significant challenge similar to other existing localization techniques. Our group and others have previously developed a prospectively validated scoring system to predict the risk of MGD using data from 4D-CTs and biochemical factors. Routine use of the scoring system in conjunction with 4D-CTs may improve preoperative identification of patients with MGD, in whom surgeons must be aware of the important limitations of 4D-CTs in guiding surgical planning.
Multinodular goiter or thyroid nodule was also associated with a higher risk of 4D-CT discordance. A prior study by Galvin et al also identified thyroid nodules as a potential risk factor for missed parathyroid lesions on 4D-CTs. Thyroid goiters show nodular projections of thyroid tissue that may be intrinsically low density yet demonstrate a wash-in or washout pattern of enhancement, making it difficult to distinguish between thyroid tissue and a juxtathyroidal parathyroid adenoma. Thyroid nodules can mimic parathyroid adenomas because they can occur in similar locations and appear oval or round, and they can have enhancement characteristics similar to those of parathyroid adenomas. The addition of US may enable correct identification of abnormal parathyroid glands in a patient with thyroid nodules.
Prior results have indicated that parathyroid lesion size may be an important factor in predicting successful preoperative localization, but the size limit of detection with 4D-CTs is largely unknown. Our findings suggest that the risk of missed glands increases below 10 mm. Because small lesions (<7 mm) occur more frequently in MGD, detection of a small abnormal lesion or no lesions should alert surgeons to the increased possibility of MGD. In addition, parathyroid lesions in the inferior position, especially partially or fully intrathyroidal glands or those flattened against the surface of the thyroid gland, were more likely to be missed on 4D-CTs. Inferior parathyroid adenomas are often in close proximity to inferior thyroid veins. As a result, vascular enhancement can obscure these inferior parathyroid lesions. Streak artifact from the inflowing contrast bolus, beam hardening artifact from the bony structures and soft tissues near the thoracic inlet, and residual thymic tissue can also obscure inferior parathyroid lesions. It is important to note that these potential “blind spots” on 4D-CTs are areas that are easily accessible and straightforward to evaluate during surgery. On the other hand, lesions that are missed by US and sestamibi SPECT are often located in areas that are more difficult to explore surgically, such as the posterior or retroesophageal location. The upshot of this finding in our practice has been that 4D-CTs, even when nonlocalizing or discordant, are highly predictive of surgical success because lesions that are difficult to access have been effectively ruled out.
Although BMI has been shown to reduce the accuracy of US and sestamibi SPECT for parathyroid localization, it did not influence 4D-CT performance in our analysis. Therefore, obese patients may benefit from having 4D-CTs as the initial localization study. Furthermore, patients with prior thyroidectomy or parathyroidectomy were less likely to have discordant 4D-CTs in our analysis. The 4D-CTs provide superior preoperative localization in reoperative cases over sestamibi scintigraphy. Although prior surgery can distort normal anatomy, previous thyroidectomy or parathyroidectomy can also simplify radiographic interpretation. Given that multinodular goiter or thyroid nodule was found to be a predisposing factor for discordant 4D-CTs, it follows that their removal can improve localization. Removal of parathyroid glands reduces the number of potential targets, and information gained from a prior neck operation may facilitate subsequent 4D-CT interpretation. Finally, due to the increased risk of reoperative parathyroidectomy, patients without a convincing target on 4D-CTs may not be offered surgery, which may also explain why fewer discordant results were noted in patients with a prior neck operation.
In the present analysis, we have identified several important risk factors associated with potential inaccuracies in 4D-CT localization. These findings afford a more thorough understanding of 4D-CT performance characteristics, which can help surgeons improve their preoperative planning and intraoperative troubleshooting. In the case of a negative 4D-CT, the surgeon may elect to allot additional operative time for what may be a more difficult case. Or, after considering the likelihood of MGD based on biochemical values and the 4D-CT result, the surgeon may consider having a more detailed discussion with the patient regarding the potential need for subtotal parathyroidectomy. During surgery, if the surgeon is either not finding the culprit glands or if the PTH level is not dropping, he or she should recall that discordance between intraoperative findings and the 4D-CT results is likely to be explained by MGD, an inferior gland that is flattened against the surface of the thyroid gland, or, less commonly, an intrathyroidal gland.
Limitations
We acknowledge some limitations to this study. First, given the retrospective study design, follow-up calcium levels were not available in all patients. Consistent with prior studies, we used the intraoperative PTH level to define a successful parathyroidectomy. We found that all patients who had at least a 50% drop in the intraoperative PTH level and available follow-up data at 6 months or beyond remained eucalcemic. Second, our study was performed within a single institution with one highly experienced neuroradiologist reading all studies. The 4D-CT technique remains novel; therefore, variations in imaging protocol and quality frequently exist among different centers. These factors may limit the generalizability of our results. The evaluation of 4D-CTs in a multi-institutional setting with several interpreting radiologists may further elucidate the potential of this localization technique.
Conclusions
We identified MGD, multinodular goiter or thyroid nodule, small parathyroid lesion size, and parathyroid lesion in the inferior position as factors associated with discordance between parathyroid preoperative 4D-CTs and intraoperative findings. Increased awareness of patterns of potentially missed lesions on 4D-CTs may improve preoperative planning and intraoperative troubleshooting.
eFigure. Comparison of Preoperative US and 4D-CT Findings
References
- 1.Carty SE, Worsey J, Virji MA, Brown ML, Watson CG. Concise parathyroidectomy: the impact of preoperative SPECT 99mTc sestamibi scanning and intraoperative quick parathormone assay. Surgery. 1997;122(6):1107-1114. [DOI] [PubMed] [Google Scholar]
- 2.Siperstein A, Berber E, Mackey R, Alghoul M, Wagner K, Milas M. Prospective evaluation of sestamibi scan, ultrasonography, and rapid PTH to predict the success of limited exploration for sporadic primary hyperparathyroidism. Surgery. 2004;136(4):872-880. [DOI] [PubMed] [Google Scholar]
- 3.Bergenfelz AO, Jansson SK, Wallin GK, et al. . Impact of modern techniques on short-term outcome after surgery for primary hyperparathyroidism: a multicenter study comprising 2,708 patients. Langenbecks Arch Surg. 2009;394(5):851-860. [DOI] [PubMed] [Google Scholar]
- 4.Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol. 2012;19(2):577-583. [DOI] [PubMed] [Google Scholar]
- 5.Eichhorn-Wharry LI, Carlin AM, Talpos GB. Mild hypercalcemia: an indication to select 4-dimensional computed tomography scan for preoperative localization of parathyroid adenomas. Am J Surg. 2011;201(3):334-338. [DOI] [PubMed] [Google Scholar]
- 6.Hunter GJ, Schellingerhout D, Vu TH, Perrier ND, Hamberg LM. Accuracy of four-dimensional CT for the localization of abnormal parathyroid glands in patients with primary hyperparathyroidism. Radiology. 2012;264(3):789-795. [DOI] [PubMed] [Google Scholar]
- 7.Lubitz CC, Stephen AE, Hodin RA, Pandharipande P. Preoperative localization strategies for primary hyperparathyroidism: an economic analysis. Ann Surg Oncol. 2012;19(13):4202-4209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Starker LF, Mahajan A, Björklund P, Sze G, Udelsman R, Carling T. 4D parathyroid CT as the initial localization study for patients with de novo primary hyperparathyroidism. Ann Surg Oncol. 2011;18(6):1723-1728. [DOI] [PubMed] [Google Scholar]
- 9.Galvin L, Oldan JD, Bahl M, Eastwood JD, Sosa JA, Hoang JK. Parathyroid 4D CT and scintigraphy: what factors contribute to missed parathyroid lesions? Otolaryngol Head Neck Surg. 2016;154(5):847-853. [DOI] [PubMed] [Google Scholar]
- 10.Rodgers SE, Hunter GJ, Hamberg LM, et al. . Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery. 2006;140(6):932-940. [DOI] [PubMed] [Google Scholar]
- 11.Kukar M, Platz TA, Schaffner TJ, et al. . The use of modified four-dimensional computed tomography in patients with primary hyperparathyroidism: an argument for the abandonment of routine sestamibi single-positron emission computed tomography (SPECT). Ann Surg Oncol. 2015;22(1):139-145. [DOI] [PubMed] [Google Scholar]
- 12.Hoang JK, Sung WK, Bahl M, Phillips CD. How to perform parathyroid 4D CT: tips and traps for technique and interpretation. Radiology. 2014;270(1):15-24. [DOI] [PubMed] [Google Scholar]
- 13.Sepahdari AR, Bahl M, Harari A, Kim HJ, Yeh MW, Hoang JK. Predictors of multigland disease in primary hyperparathyroidism: a scoring system with 4D-CT imaging and biochemical markers. AJNR Am J Neuroradiol. 2015;36(5):987-992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sho S, Yilma M, Yeh MW, et al. . Prospective validation of two 4D-CT–based scoring systems for prediction of multigland disease in primary hyperparathyroidism. AJNR Am J Neuroradiol. 2016;37(12):2323-2327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mazeh H, Chen H, Leverson G, Sippel RS. Creation of a “Wisconsin Index” nomogram to predict the likelihood of additional hyperfunctioning parathyroid glands during parathyroidectomy. Ann Surg. 2013;257(1):138-141. [DOI] [PubMed] [Google Scholar]
- 16.Kebebew E, Hwang J, Reiff E, Duh QY, Clark OH. Predictors of single-gland vs multigland parathyroid disease in primary hyperparathyroidism: a simple and accurate scoring model. Arch Surg. 2006;141(8):777-782. [DOI] [PubMed] [Google Scholar]
- 17.Berber E, Parikh RT, Ballem N, Garner CN, Milas M, Siperstein AE. Factors contributing to negative parathyroid localization: an analysis of 1000 patients. Surgery. 2008;144(1):74-79. [DOI] [PubMed] [Google Scholar]
- 18.McCoy KL, Chen NH, Armstrong MJ, et al. . The small abnormal parathyroid gland is increasingly common and heralds operative complexity. World J Surg. 2014;38(6):1274-1281. [DOI] [PubMed] [Google Scholar]
- 19.Mortenson MM, Evans DB, Lee JE, et al. . Parathyroid exploration in the reoperative neck: improved preoperative localization with 4D-computed tomography. J Am Coll Surg. 2008;206(5):888-895. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Comparison of Preoperative US and 4D-CT Findings