This national database study describes the natural history of isolated splenic injuries to determine the association of management strategy with patterns of readmission among these patients.
Key Points
Question
On a national level, what is the natural history of isolated splenic injuries with regard to readmission and delayed splenectomy when a splenectomy is not performed during the index hospitalization for injury?
Findings
In this national database study of 3792 patients with isolated splenic injury, nonoperative management was the most common strategy used for isolated splenic injuries (2673 [70.5%]), whereas splenectomy was used in 825 cases (21.8%). The delayed splenectomy rate for those who did not have a splenectomy at their index admission was 1.2% (36 of 2967 patients).
Meaning
Current practice patterns are associated with low rates of readmission for delayed splenectomy.
Abstract
Importance
Options for managing splenic injuries have evolved with a focus on nonoperative management. Long-term outcomes, such as readmissions and delayed splenectomy rate, are not well understood.
Objective
To describe the natural history of isolated splenic injuries in the United States and determine whether patterns of readmission were influenced by management strategy.
Design, Setting, and Participants
The Healthcare Cost and Utilization Project’s Nationwide Readmission Database is an all-payer, all-ages, longitudinal administrative database that provides data on more than 35 million weighted US discharges yearly. The database was used to identify patients with isolated splenic injuries and the procedures that they received. Adult patients with isolated splenic injuries admitted from January 1 through June 30, 2013, and from January 1 through June 30, 2014, were included. Those who died during the index hospitalization or who had an additional nonsplenic injury with an Abbreviated Injury Score of 2 or greater were excluded. Univariate and mixed-effects logistic regression analysis controlling for center effect were used. Weighted numbers are reported.
Exposures
Initial management strategy at the time of index hospitalization, including nonprocedural management, angioembolization, and splenectomy.
Main Outcomes and Measures
All-cause 6-month readmission rate. Secondary outcome was delayed splenectomy rate.
Results
A weighted sample of 3792 patients (2146 men [56.6%] and 1646 women [43.4%]; mean [SE] age, 48.5 [0.7] years) with 5155 admission events was included. During the index hospitalization, 825 (21.8%) underwent splenectomy, 293 (7.7%) underwent angioembolization, and 2673 (70.5%) had no procedure. The overall readmission rate was 21.1% (799 patients). Readmission rates did not differ based on initial management strategy (195 patients undergoing splenectomy [23.6%], 70 undergoing angioembolism [23.9%], and 534 undergoing no procedure [20%]; P = .33). Splenectomy was performed in 36 of 799 readmitted patients (4.5%) who did not have a splenectomy at their index hospitalization, leading to an overall delayed splenectomy rate of 1.2% (36 of 2967 patients). In mixed-effects logistic regression analysis controlling for patient, injury, clinical, and hospital characteristics, the choice of splenectomy (odds ratio, 0.93; 95% CI, 0.66-1.31) vs angioembolization (odds ratio, 1.19; 95% CI, 0.72-1.97) as initial management strategy was not associated with readmission.
Conclusions and Relevance
This national evaluation of the natural history of isolated splenic injuries from index admission through 6 months found that approximately 1 in 5 patients are readmitted within 6 months of discharge after an isolated splenic injury. However, the chance of readmission for splenectomy after initial nonoperative management was 1.2%. This finding suggests that the current management strategies used for isolated splenic injuries in the United States are well matched to patient need.
Introduction
Management options for splenic injuries resulting from trauma have evolved to include immediate splenectomy, nonoperative management, and splenic artery angioembolization. Nonoperative management has become common, particularly for low-grade injuries. However, angioembolization for selected splenic injuries has also been used increasingly. Some centers using angioembolization in their management algorithms have published high rates of splenic salvage, even in the case of high-grade injuries. However, long-term failure rates for nonoperative management and angioembolization are not well described.
Investigations related to postdischarge outcomes for splenic injuries have been based on institutional findings, limiting the overall generalizability of results. Furthermore, these studies may not capture patients who presented to a different hospital for additional treatment. Two population-based studies in the recent literature have used statewide data from California. One of these studies reported a 30-day readmission rate of 7.4% when nonoperative management was used and a 12.8% readmission rate when angioembolization was used. However, the study included patients who had other injuries in addition to their splenic injuries. Whether a readmission was associated with the splenic or another injury could not be determined from administrative data. Furthermore, the study excluded patients who had undergone a splenectomy at the index hospitalization; thus, comparison of the associations of management strategies with readmissions is difficult. A second study used the same data to analyze readmission rates for nonoperative management with or without adjunctive angioembolization vs operative management. The investigators showed readmission rates among patients who had undergone splenectomy of 11% at 30 days and 21% at 1 year compared with rates of 7.5% at 30 days and 16% at 1 year in the nonoperative management group. Again, the study cohort included patients who had other injuries in addition to splenic injuries, and thus interpretation of the findings is difficult.
An investigation that uses population-level data is needed to determine postdischarge outcomes related to splenic injuries, particularly as the outcomes are associated with the initial management strategy used for the splenic injury. Such a study should focus on isolated splenic injuries, because readmissions and the decision to perform a splenectomy can depend on other injuries and procedures. We hypothesized that readmission rates would be high and that splenectomies would be performed during readmissions for those who did not undergo a procedure at their index hospitalization. To test this hypothesis, we used an all-payer, all-ages, longitudinal database to evaluate 6-month readmission and delayed splenectomy rates among patients who were admitted to hospitals in the United States in 2013 through 2014 with an isolated splenic injury.
Methods
The Nationwide Readmissions Database (NRD) is produced by the Healthcare Cost and Utilization Project (HCUP) by the Agency of Healthcare Research and Quality. The NRD is a nationally representative sample of 15 million unweighted discharges each year, or 35 million weighted discharges from US hospitals. The NRD is unique because it contains readmission data, such that each patient in the database can be followed up longitudinally for the course of 1 year. Furthermore, the NRD is an all-payer database, and thus the generalizability of analysis from the included patient population is increased. This database provides weighted adjustments to produce nationally representative estimates. We used NRD data from 2013 and 2014, which are the only 2 years available. The study was waived from formal review and informed consent by the institutional review board of Stanford University because the NRD data used by HCUP are deidentified. Use of the NRD follows regulations within the data use agreement as defined by the HCUP and Agency of Healthcare Research and Quality.
Diagnoses and procedures were identified using codes from the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM). Splenic injuries were identified using ICD-9-CM codes 865 to 865.2. ICD-9-CM procedure codes used to identify splenectomy included 41.5 and 41.43; codes used to identify angioembolization were 88.4, 88.40, 88.47, and 39.79. Injury characteristics such as Injury Severity Score were derived using the ICDPIC (ICD Programs for Injury Categorization) module in Stata software.
Patients were included in the analysis if they were 18 years or older, had a splenic injury, and were admitted from January 1 through June 30, 2013, or January 1 through June 30, 2014. Admissions in the first half of the year ensured a minimum follow-up period of 6 months. A follow-up period of 6 months was selected because long-term follow-up of consequences of splenic management strategies has never been defined. Of note, patients are not followed up from year to year in this database. Therefore, each year was analyzed separately.
Because readmission or decisions to perform a splenectomy may depend on the totality of a patient’s injuries, we focused only on isolated splenic injuries. Therefore, all patients with an Abbreviated Injury Score greater than or equal to 2 in any nonsplenic body region were excluded. Patients who died during their first hospitalization were also excluded.
The primary outcome was the all-cause 6-month readmission rate. A secondary outcome was delayed splenectomy rate. Delayed splenectomy was defined as a splenectomy that was performed after the index hospitalization. Analyses were performed using a level of statistical significance of P < .05. Unadjusted analysis included the χ2 goodness-of-fit test and univariate regression. Mixed-effects logistic regression controlling for center effect was used to determine factors associated with risk for readmission. Variables used in the regression models included known demographic, injury, and hospital confounding characteristics. The most parsimonious regression models were used. Stata software does not allow for calculations of the area under the curve or Hosmer-Lemeshow statistics when mixed-effects regression is used; thus, the same variables were included in a logistic regression model not controlling for center. Results were compared, and model performance was derived from the matching logistic regression models.
The 2014 (but not 2013) NRD also provided data on days to procedure, allowing for a determination of the specific days after admission on which splenectomies were performed. This information could be used to identify patients who initially underwent a nonoperative management strategy, which we defined as patients who did not undergo a splenectomy on hospital days 0 or 1. Therefore, in addition to the delayed splenectomy rate, we determined a rate of failure of nonoperative management, defined as a splenectomy after day 1. A Kaplan-Meier analysis was performed to determine time to splenectomy for those with failure of nonoperative management.
Weighted data are presented to provide nationally representative estimates. Statistical analysis was performed using Stata/SE software (version 14.1; StataCorp).
Results
A weighted sample of 3792 patients (mean [SE] age, 48.5 [0.7] years) with 5155 admissions in the NRD met inclusion and exclusion criteria. Overall, patients were more often male (2146 male [56.6%] vs 1646 female [43.4%]), and low-grade splenic injuries (Abbreviated Injury Score grades 1-3) were the most common (2843 [75%]). Splenectomy was performed in 825 patients (21.8%); angioembolization, in 293 (7.7%); and no procedure, in 2673 (70.5%). For patients with grades 4 to 5 splenic injuries, splenectomy was performed more often compared with patients with low-grade injuries (353 of 948 [37.2%] vs 471 of 2843 [16.6%]; P < .01), and angioembolization was more common in high-grade vs low-grade injuries (143 [14.0%] vs 160 [5.6%]; P < .01).
We found significant differences in patient, injury, hospital, and outcome factors, depending on the management strategy used during the index hospitalization (Table 1). Patients who underwent splenectomy were more often in the lowest 2 income quartiles (541 [65.6%]) compared with those who underwent angioembolization (149 [50.6%]) or no procedure (1408 [52.7%]; P = .02). Patients who underwent splenectomy were also less likely to have private insurance (246 [29.8%]) compared with those who underwent angioembolization (131 [44.7%]) or no procedure (1088 [40.7%]; P = .02). Grade of splenic injury was also associated with procedure. High-grade splenic injuries (grades 4-5) were more common in patients who underwent splenectomy (353 [42.8%]) and angioembolization (133 [45.5%]) than in those who underwent no procedure (461 [17.3%]; P < .01). Hospital characteristics were also associated with initial management. Patients who had splenectomies more often lived in regions with a population of less than 1 million (506 [61.4%]) compared with those who underwent no procedure (1324 [49.5%]; P < .01). The index hospitalization mean (SE) length of stay was longer for patients who had angioembolization or splenectomy (9.7 [0.5] and 6.8 [0.7] days, respectively) vs those who had no procedure (4.7 [0.2] days; P < .01). However, readmission rates did not significantly differ among the 3 groups.
Table 1. Patient, Injury, Hospital, and Outcome Characteristics Based on Primary Management Strategy.
| Characteristic | Primary Management Strategy for Index Admissiona | P Valueb | ||
|---|---|---|---|---|
| No
Procedure (n = 2673) |
Angioembolization (n = 293) |
Splenectomy (n = 825) |
||
| Patient | ||||
| Age in 2013, mean (SE), y | 48 (0.7) | 46 (2.0) | 52 (1.2) | .30 |
| Sex | ||||
| Male | 1494 (55.9) | 171 (58.4) | 480 (58.2) | .75 |
| Female | 1179 (44.1) | 122 (41.6) | 344 (41.7) | |
| Zip code income quartile | ||||
| 0-25th | 698 (26.1) | 63 (21.4) | 288 (34.9) | .02 |
| 26th-50th | 710 (26.6) | 86 (29.2) | 253 (30.7) | |
| 51th-75th | 676 (25.3) | 76 (26.0) | 159 (19.3) | |
| 76th-100th | 546 (20.4) | 64 (21.7) | 115 (13.9) | |
| Payer status at first admission | ||||
| Medicare | 693 (25.9) | 70 (23.9) | 271 (32.9) | .02 |
| Medicaid | 369 (13.8) | 43 (14.7) | 121 (14.7) | |
| Private insurance | 1088 (40.7) | 131 (44.7) | 246 (29.8) | |
| Splenic injury gradec | ||||
| 1-3 | 2212 (82.7) | 160 (54.7) | 471 (57.1) | <.01 |
| 4-5 | 461 (17.3) | 133 (45.5) | 353 (42.9) | |
| Hospital | ||||
| Population setting | ||||
| ≥1 Million | 1350 (50.5) | 174 (59.4) | 318 (38.6) | <.01 |
| <1 Million | 1324 (49.5) | 119 (40.7) | 506 (61.4) | |
| Ownership | ||||
| Government | 446 (16.7) | 53 (18.0) | 109 (13.2) | .29 |
| Private | 2228 (83.3) | 241 (82.0) | 716 (86.8) | |
| Bed size | ||||
| Small | 904 (33.8) | 76 (25.8) | 329 (40.0) | <.01 |
| Large | 1769 (66.2) | 218 (74.2) | 495 (60.0) | |
| Teaching status | ||||
| Nonteaching | 1087 (40.7) | 75 (25.5) | 385 (46.7) | <.01 |
| Teaching | 1586 (59.3) | 219 (74.5) | 440 (53.3) | |
| Outcome | ||||
| Discharge destinationd | ||||
| Routine | 2142 (80.1) | 234 (79.8) | 585 (70.9) | <.01 |
| Discharged with services | 531 (19.9) | 59 (20.2) | 239 (29.0) | |
| Length of stay, mean (SE), d | 4.7 (0.2) | 6.8 (0.7) | 9.7 (0.5) | <.01 |
| ≥1 Readmission within 6 mo | 534 (20) | 70 (23.9) | 195 (23.6) | .33 |
Unless otherwise indicated, data are expressed as number (percentage) of patients. All numbers and percentages are accounted for by weight.
Calculated using univariate linear regression for continuous variables and Pearson χ2 test for binary variables.
Calculated using the Abbreviated Injury Score for splenic injury (range, 1-5, with higher scores indicating greater severity of injury).
Cell size is too small to report for some subcategories, per the Healthcare Cost and Utilization Project data use agreement.
Mixed-effects logistic regression controlling for center effect was performed to determine factors associated with undergoing splenectomy at the index admission. Variables included in the analysis were age, sex, payer status, zip code income quartile, number of chronic diseases, splenic injury grade, hospital characteristics, and discharge status and length of stay from the index hospitalization. The only variables associated with undergoing a splenectomy were age, splenic injury grade, and hospital characteristics. Increasing age was associated with an increased odds ratio (OR) for splenectomy (1.48; 95% CI, 1.02-2.14; P = .04) The OR for undergoing a splenectomy at the index hospitalization for patients with a high-grade vs a low-grade splenic injury was 3.60 (95% CI, 2.74-4.73; P < .01). Characteristics associated with lower ORs for a splenectomy at index admission included hospitals in regions with a population of 1 million or greater (0.67; 95% CI, 0.51-0.88; P < .01), metropolitan teaching hospitals (0.74; 95% CI, 0.56-0.96; P = .02), and hospitals with large bed sizes (0.75; 95% CI, 0.57-0.97; P = .03).
Overall, 799 patients with an isolated splenic injury (21.1%) were readmitted within 6 months. For patients who were readmitted, 504 (63.1%) experienced 1 readmission, whereas 168 (21%) experienced 2 and 127 (15.9%) experienced 3 or more readmissions. The mean time until readmission was 44.0 days (95% CI, 38.2-49.7 days). Among patients who were readmitted, 562 (70.3%) were admitted to the same hospital as in the index hospitalization, whereas 237 (29.7%) were admitted to a different hospital. Among the 799 patients who did not have a splenectomy at their index hospitalization and were readmitted within 6 months, 36 (4.5%) had a splenectomy at readmission. Because most patients were not readmitted, patients who did not undergo a splenectomy at the index hospitalization had a low delayed splenectomy rate (36 of 2967 [1.2%]).
We compared patients who were readmitted at least once with those who were never readmitted (Table 2). Patients who were readmitted differed on several measures. Readmitted patients were older (mean [SE] age, 58.1 [1.0] vs 46.4 [0.7] years; P < .01) and were more often female (415 of 799 [51.9%] vs 1231 of 2993 [41.1%]; P < .01). Patients who were readmitted had lower rates of high-grade splenic injuries compared with those without any readmissions (145 of 799 [18.2%] vs 803 of 2993 [26.8%]; P < .01). We found no difference between those who were readmitted and those who were not in terms of initial management strategy (ie, splenectomy, angioembolization, or no procedure). To determine whether initial management strategy was associated with lower rate of readmission in patients with high-grade splenic injuries, we also conducted multivariate logistic regression with the inclusion of an interaction term for splenic injury grade and management strategy. Inclusion of the interaction variable did not affect the results (OR, 0.93; 95% CI, 0.24-3.64).
Table 2. Patient, Injury, Hospital, and Outcome Characteristics at the Time of Index Admission for Trauma Based on Readmission Status.
| Characteristic | Readmission Statusa | P Valueb | |
|---|---|---|---|
| None (n = 2993) |
≥1
Readmission (n = 799) |
||
| Patient | |||
| Age, mean (SE), y | 46.4 (0.7) | 58.1 (1.0) | <.01 |
| Sex | |||
| Male | 1762 (58.9) | 384 (48.1) | <.01 |
| Female | 1231 (41.1) | 415 (51.9) | |
| Zip code income quartile | |||
| 0-25th | 803 (26.8) | 246 (30.8) | .43 |
| 26th-50th | 828 (27.7) | 221 (27.6) | |
| 51th-75th | 744 (24.8) | 168 (21.1) | |
| 76th-100th | 578 (19.3) | 147 (18.4) | |
| Payer status at first admissionc | |||
| Medicare | 690 (23.1) | 345 (43.2) | <.01 |
| Medicaid | 406 (13.6) | 127 (15.9) | |
| Private insurance | 1243 (41.5) | 223 (27.9) | |
| Injury details | |||
| Splenic injury graded | |||
| 1-3 | 2190 (73.2) | 654 (81.8) | <.01 |
| 4-5 | 803 (26.8) | 145 (18.2) | |
| Management strategy | |||
| No procedure | 2139 (71.5) | 534 (66.9) | .62 |
| Splenectomy | 630 (21.0) | 195 (24.4) | |
| Angioembolization | 224 (7.5) | 70 (8.8) | |
| Hospital | |||
| Population setting | |||
| ≥1 Million | 1406 (47) | 437 (54.7) | .02 |
| <1 Million | 1587 (53) | 362 (45.3) | |
| Ownership | |||
| Government | 508 (17) | 99 (12.4) | .03 |
| Private | 2485 (83) | 700 (87.6) | |
| Bed size | |||
| Small | 1039 (34.7) | 270 (33.8) | .77 |
| Large | 1953 (65.3) | 529 (66.2) | |
| Teaching status | |||
| Nonteaching | 1191 (39.8) | 356 (44.6) | .14 |
| Teaching | 1802 (60.2) | 442 (55.4) | |
| Outcome | |||
| Discharge destination | |||
| Routine | 2492 (83.3) | 469 (58.8) | <.01 |
| Discharge with service | 500 (16.7) | 329 (41.2) | |
| Length of stay, mean (SE), d | 5 (0.2) | 9 (0.6) | <.01 |
| Died at readmission | NA | 50 (6.3) | NA |
Abbreviation: NA, not applicable.
Unless otherwise indicated, data are expressed as number (percentage) of patients. All numbers and percentages are accounted for by weight.
Calculated using univariate linear regression for continuous variables and Pearson χ2 test for binary variables.
Cell size is too small to report for some subcategories, per Healthcare Cost and Utilization Project data use agreement.
Calculated using the Abbreviated Injury Score for splenic injury (range, 1-5, with higher scores indicating greater severity of injury).
The adjusted risk for readmission was determined using mixed-effects regression to control for center effect. Variables included in the analysis were the same as listed above (Table 3). The adjusted risk for admission was not associated with the initial management strategy at the index admission. High-grade splenic injuries were associated with a lower OR for readmission compared with low-grade injuries (0.68; 95% CI, 0.49-0.96; P = .03). Other characteristics associated with high ORs for readmissions included number of chronic conditions (1.18; 95% CI, 1.12-1.23; P < .01) and evidence of a more complicated initial length of stay, including a higher OR for nonroutine discharge (1.18; 95% CI, 1.12-1.23; P < .01) and longer length of stay (1.03 per day; 95% CI, 1.01-1.04; P < .01).
Table 3. Adjusted Analysis for Variables Associated With Readmission.
| Variablea | OR (95% CI) | P Valueb |
|---|---|---|
| No. of chronic conditions | 1.18 (1.12-1.23) | <.01 |
| High- vs low-grade splenic injuryc | 0.68 (0.49-0.96) | .03 |
| Population of region ≥1 million vs <1 million | 1.42 (1.07-1.87) | .01 |
| Non-routine discharge after index admission vs routine | 1.18 (1.12-1.23) | <.01 |
| Length of stay, d | 1.03 (1.01-1.04) | <.01 |
Abbreviation: OR, odds ratio.
Only significant variables are shown.
Calculated using univariate linear regression for continuous variables and Pearson χ2 test for binary variables.
High-grade injury indicates an Abbreviated Injury Score grade of 4 to 5; low-grade injury, 3 or less.
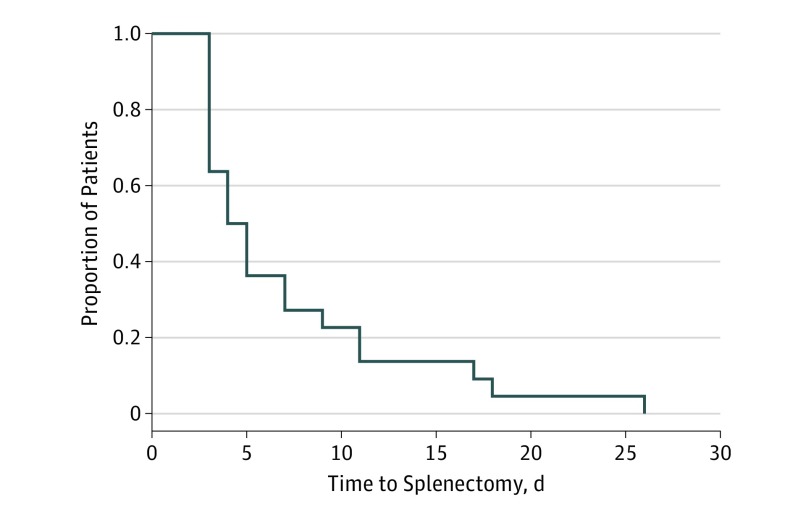
The 2014 data (but not the 2013 data) contained information on day to procedure. This information could be used to identify the exact day from the index admission day for injury to splenectomy for the cohort in 2014 who had nonmissing data. We defined patients as having an initial plan for nonoperative management for an isolated splenic injury if a splenectomy was not performed on day 0 or 1. For the subset of patients who initially underwent nonoperative management but who ultimately required splenectomy, we performed Kaplan-Meier analysis (Figure). For patients who underwent splenectomy, 446 of 558 (79.9%) had their procedures on day 0 or 1. Of the remaining 112 patients, 53 (47.3%) underwent a splenectomy within 5 days and 59 (52.7%) underwent a splenectomy after 5 days.
Figure. Kaplan-Meier Curve for Time to Splenectomy for Patients Who Underwent Initial Nonoperative Management.
Data from admission year 2014 are presented because the timing variable was not included in 2013 admission year data.
Discussion
This analysis is the first, to our knowledge, to describe the management of isolated splenic injuries and the long-term consequences in a longitudinal all-payer, all-ages national database that also includes all acute care hospitals (ie, not just trauma centers). By focusing the study on isolated splenic injuries, we could assess splenectomy rates and readmissions independently of other confounding injuries.
In this study, 70.5% of patients did not undergo any procedure at their index admission, whereas 21.8% underwent splenectomy. The estimate for the number of patients being treated with a nonoperative therapy at the index admission is likely to be an underestimate because the day of the procedure is not coded for the entire data set (only 2014). Because these data were not available, we can only identify whether a splenectomy was performed at some point during the hospitalization. Therefore, some patients who initially were assigned to a nonoperative management arm likely experienced treatment failure during their index admission, as suggested by the 2014 data, which include procedure days. In 2014, 50.1% of patients experienced nonoperative management failure within a 5-day window. Together, these findings suggest that the number of patients who underwent initial nonoperative management was likely to have been higher than 70%.
Injury and hospital factors were associated with the particular management strategy used at the index hospitalization. Almost 40% of patients with higher-grade injuries (Abbreviated Injury Score grades 4-5) underwent splenectomy during the initial hospitalization. In adjusted regression, the OR for having a splenectomy at the index admission for high-grade injuries remained high at 3.60. However, our findings suggest that hospital factors also play a role. We also found that large, metropolitan teaching hospitals were less likely to perform splenectomy, after controlling for known confounders. Although this result may be secondary to differences in patient factors, the findings may represent cultural or protocol differences. This possibility is further suggested by differences observed in hospitals where angioembolization was performed at the index admission. Among patients who underwent angioembolization, 219 (74.5%) were at teaching hospitals, compared with 440 (53.3%) who underwent splenectomy and 1586 (59.3%) who did not undergo a procedure. Further work should determine whether patient factors, practice patterns, or a combination of both result in the observed patterns of management for splenic injury.
Given the longitudinal nature of this database, we also determined downstream use of health care services based on initial management strategy. Overall, 6-month readmission rates were approximately 20%. This rate is consistent with those of other studies of trauma readmissions that show rates of 30-day and 1-year readmission ranging from 7.6% to 21%. High rates of readmission did not appear to be associated with the need for splenectomy. The overall rate of delayed splenectomy was only 1.2%. This rate suggests that readmissions occurred for reasons other than splenic rebleeding.
Rates of readmission were higher among patients who had low-grade injuries. Given the low rates of delayed splenectomy, readmissions are likely attributable to other factors unrelated to management of the spleen. Furthermore, the unadjusted and adjusted analyses suggest that some of these factors may be patient related. Patients who were readmitted were older and had more chronic conditions. Readmission may be associated with these chronic conditions or perhaps a worsening status for their chronic condition resulting from injury. Furthermore, patients who were ultimately readmitted appeared to have longer, perhaps more complicated, index hospitalizations. Patients who were readmitted had a mean length of stay that was 4 days longer than that for those who were not readmitted. Because patients with significant other injuries were excluded from the analysis, patient factors rather than injury factors may have played a role.
Limitations
This study has several limitations. Retrospective observational reviews are subject to the limitations inherent to such studies. Although results of studies from the national databases such as the NRD provide important insights into management trends, causal associations cannot be determined. Specifically, for this study, we were limited by ICD-9-CM procedure codes, because those coding for angioembolization are not specific to body location. The ICD-10 Procedure Coding System may benefit overall analysis because procedural data are coded for body part. Such granularity would allow for more specific identification of angioembolization location and allow analysis of all patients with splenic injuries, including those with concomitant injuries. Other limitations include those inherent to the NRD. These include the lack of information on out-of-hospital deaths, trauma center status, and clinical treatment variables such as transfusion data. Future studies should incorporate these variables to further evaluate risk factors for readmission. Despite these limitations, this study is the first, to our knowledge, to evaluate long-term readmission rates in a national, all-payer, all-ages database.
Conclusions
This study is the first, to our knowledge, to describe national management patterns for isolated splenic injuries and to include 6-month follow-up. Nonoperative management is commonly used in the United States, and use of this strategy does not appear to be associated with high rates of delayed splenectomy. Almost half of patients who underwent an initial trial of nonoperative management, if they experienced treatment failure, did so within 5 days, suggesting that inpatient hospitalization or quick follow-up should be considered for those deemed to be at high risk. Future work should distinguish clinical factors responsible for these findings.
References
- 1.Peitzman AB, Heil B, Rivera L, et al. Blunt splenic injury in adults: multi-institutional study of the Eastern Association for the Surgery of Trauma. J Trauma. 2000;49(2):177-187. [DOI] [PubMed] [Google Scholar]
- 2.Dent D, Alsabrook G, Erickson BA, et al. Blunt splenic injuries: high nonoperative management rate can be achieved with selective embolization. J Trauma. 2004;56(5):1063-1067. [DOI] [PubMed] [Google Scholar]
- 3.Haan JM, Biffl W, Knudson MM, et al. ; Western Trauma Association Multi-Institutional Trials Committee . Splenic embolization revisited: a multicenter review. J Trauma. 2004;56(3):542-547. [DOI] [PubMed] [Google Scholar]
- 4.Jeremitsky E, Kao A, Carlton C, Rodriguez A, Ong A. Does splenic embolization and grade of splenic injury impact nonoperative management in patients sustaining blunt splenic trauma? Am Surg. 2011;77(2):215-220. [PubMed] [Google Scholar]
- 5.Zarzaur BL, Kozar R, Myers JG, et al. The splenic injury outcomes trial: an American Association for the Surgery of Trauma multi-institutional study. J Trauma Acute Care Surg. 2015;79(3):335-342. doi: 10.1097/TA.0000000000000782 [DOI] [PubMed] [Google Scholar]
- 6.Miller PR, Chang MC, Hoth JJ, et al. Prospective trial of angiography and embolization for all grade III to V blunt splenic injuries: nonoperative management success rate is significantly improved. J Am Coll Surg. 2014;218(4):644-648. doi: 10.1016/j.jamcollsurg.2014.01.040 [DOI] [PubMed] [Google Scholar]
- 7.Capecci LM, Jeremitsky E, Smith RS, Philp F. Trauma centers with higher rates of angiography have a lesser incidence of splenectomy in the management of blunt splenic injury. Surgery. 2015;158(4):1020-1024. doi: 10.1016/j.surg.2015.05.025 [DOI] [PubMed] [Google Scholar]
- 8.Zarzaur BL, Savage SA, Croce MA, Fabian TC. Trauma center angiography use in high-grade blunt splenic injuries: timing is everything. J Trauma Acute Care Surg. 2014;77(5):666-673. doi: 10.1097/TA.0000000000000450 [DOI] [PubMed] [Google Scholar]
- 9.Clancy AA, Tiruta C, Ashman D, Ball CG, Kirkpatrick AW. The song remains the same although the instruments are changing: complications following selective non-operative management of blunt spleen trauma: a retrospective review of patients at a level I trauma centre from 1996 to 2007. J Trauma Manag Outcomes. 2012;6(1):4. doi: 10.1186/1752-2897-6-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zarzaur BL, Vashi S, Magnotti LJ, Croce MA, Fabian TC The real risk of splenectomy after discharge home following nonoperative management of blunt splenic injury. J Trauma. 2009;66(6):1531-1536-1538. doi: 10.1097/TA.0b013e3181a4ed11 [DOI] [PubMed]
- 11.Freitas G, Olufajo OA, Hammouda K, et al. Postdischarge complications following nonoperative management of blunt splenic injury. Am J Surg. 2016;211(4):744-749.e1. doi: 10.1016/j.amjsurg.2015.11.018 [DOI] [PubMed] [Google Scholar]
- 12.Olufajo OA, Rios-Diaz A, Peetz AB, et al. Comparing readmissions and infectious complications of blunt splenic injuries using a statewide database. Surg Infect (Larchmt). 2016;17(2):191-197. doi: 10.1089/sur.2015.137 [DOI] [PubMed] [Google Scholar]
- 13.Healthcare Cost and Utilization Project. Overview of the Nationwide Readmissions Database. https://www.hcup-us.ahrq.gov/nrdoverview.jsp. April 5, 2017. Accessed June 27, 2017.
- 14.Clark DE, Osler TM, Hahn DR ICDPIC: STATA module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores. 2010. http://econpapers.repec.org/software/bocbocode/s457028.htm. October 29, 2010. Accessed February 4, 2017.
- 15.Centers for Medicare & Medicaid Services 2017 ICD-10-PCS and GEMs. https://www.cms.gov/Medicare/Coding/ICD10/2017-ICD-10-PCS-and-GEMs.html. Modified August 22, 2016. Accessed June 27, 2017.