This cohort study compares the incidence of surgical site infection and noninfectious wound complications after immediate, delayed, and secondary implant and autologous breast reconstruction in patients undergoing mastectomy.
Key Points
Question
Does the incidence of wound complications differ after implant and autologous immediate, delayed, and secondary breast reconstruction?
Findings
In this cohort study of 17 293 patients who underwent mastectomy, the incidence of surgical site infection was significantly higher after immediate (8.9%) compared with delayed (6.0%) and secondary (3.3%) implant reconstructions, with similar results for noninfectious wound complications. In contrast, the incidence of surgical site infection was similar after immediate (9.8%), delayed (13.9%), and secondary (11.6%) autologous reconstructions.
Meaning
Delayed implant rather than immediate implant reconstruction may be beneficial in some high-risk patients to reduce the risk of wound complications.
Abstract
Importance
Few data are available concerning surgical site infection (SSI) and noninfectious wound complications (NIWCs) after delayed (DR) and secondary reconstruction (SR) compared with immediate reconstruction (IR) procedures in the breast.
Objective
To compare the incidence of SSI and NIWCs after implant and autologous IR, DR, and SR breast procedures after mastectomy.
Design, Setting, and Participants
This retrospective cohort study included women aged 18 to 64 years undergoing mastectomy from January 1, 2004, through December 31, 2011. Data were abstracted from a commercial insurer claims database in 12 states and analyzed from January 1, 2015, through February 7, 2017.
Exposures
Reconstruction within 7 days of mastectomy was considered immediate. Reconstruction more than 7 days after mastectomy was considered delayed if the mastectomy did not include IR or secondary if the mastectomy included IR.
Main Outcomes and Measures
International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis codes for SSI and NIWCs.
Results
Mastectomy was performed in 17 293 women (mean [SD] age, 50.4 [8.5] years); 61.4% of women had IR or DR. Among patients undergoing implant reconstruction, the incidence of SSI was 8.9% (685 of 7655 women) for IR, 5.7% (21 of 369) for DR, and 3.2% (167 of 5150) for SR. Similar results were found for NIWCs. In contrast, the incidence of SSI was similar after autologous IR (9.8% [177 of 1799]), DR (13.9% [19 of 137]), and SR (11.6% [11 of 95]) procedures. Compared with women without an SSI after implant IR, women with an SSI after implant IR were significantly more likely to have another SSI (47 of 412 [11.4%] vs 131 of 4791 [2.7%]) and an NIWC (24 of 412 [5.8%] vs 120 of 4791 [2.5%]) after SR. The incidence of SSI (24 of 379 [6.3%] vs 152 of 5286 [2.9%]) and NIWC (22 of 379 [5.8%] vs 129 of 5286 [2.4%]) after implant SR was higher in women who had received adjuvant radiotherapy. Wound complications after IR were associated with significantly more breast surgical procedures (mean of 1.92 procedures [range, 0-9] after implant IR and 1.11 [range, 0-6] after autologous IR) compared with women who did not have a complication (mean of 1.37 procedures [range, 0-8] after implant IR and 0.87 [range, 0-6] after autologous IR).
Conclusions and Relevance
The incidence of SSI and NIWCs was slightly higher for implant IR compared with delayed or secondary implant reconstruction. Women who had an SSI or NIWC after implant IR had a higher risk for subsequent complications after SR and more breast operations. The risk for complications should be carefully balanced with the psychosocial and technical benefits of IR. Select high-risk patients may benefit from consideration of delayed rather than immediate implant reconstruction to decrease breast complications after mastectomy.
Introduction
Breast reconstruction is increasingly performed after mastectomy in women with breast cancer and for prophylaxis in women at high risk for breast cancer. Steadily increasing use of mastectomy in women with early breast cancer has been reported in the past decade, along with increasing use of bilateral mastectomy, even for unilateral disease. Coinciding with this trend is increased use of immediate breast reconstruction (IR), particularly in women undergoing bilateral mastectomy, more than half of whom undergo reconstruction. Using the Nationwide Inpatient Sample, the proportion of women undergoing mastectomy for cancer or prophylaxis with IR increased by almost 1.5-fold from 28.5% in 2005 to 42% in 2011 (M.A.O., unpublished data; November 2015).
Immediate breast reconstruction is often recommended to women undergoing mastectomy because it is thought to confer psychosocial benefits and result in better cosmesis. The true influence of reconstruction on quality of life is difficult to assess, because women who only undergo mastectomy tend to be older, white, have higher educational attainment, and place less importance on body image than women who undergo breast reconstruction. The perceived benefit of IR does not, however, take into account the potential for serious complications, including delays in initiating chemotherapy and radiotherapy that may affect the potential for cure, survival, quality of life, psychosocial well-being, return to work, and overall cost.
The proportion of women with high-risk characteristics undergoing implant IR has increased 3-fold since the late 1990s, driven primarily by increased use of implant reconstruction. Increased use of IR was found in all high-risk groups by Albornoz et al using the National Cancer Database, including the elderly, women with advanced breast cancer, women with comorbidities, and women who required adjuvant radiotherapy.
Few studies with sufficient sample size in the literature compare wound complication rates, including surgical site infection (SSI) and noninfectious wound complications (NIWCs), to make firm conclusions about the relative incidence of complications after IR vs delayed reconstruction (DR). Given this paucity of data, we compared the incidence of wound complications after implant and/or autologous IR, DR, and secondary breast reconstruction (SR) using insurance claims data from nonelderly (aged 18-64 years) women. The goal of this study was to determine and compare complication rates to facilitate discussion of options with women considering breast reconstruction and the timing of reconstructive surgery after mastectomy (ie, IR vs DR).
Methods
Data
We conducted a retrospective cohort study using data from 12 Anthem-affiliated plans in the HealthCore Integrated Research Database, including individuals from 12 Anthem-affiliated plans (California, Connecticut, Georgia, Indiana, Kentucky, Maine, Missouri [excluding 30 counties in the Kansas City area], Nevada, New Hampshire, New York, Ohio, and Virginia [excluding the northern suburbs of Washington, DC]). Data include all fully adjudicated claims submitted from clinicians, facilities, and outpatient pharmacies linked to health plan enrollment information. Fully insured women with enrollment in a fee-for-service plan and complete medical coverage were eligible for cohort inclusion. We excluded women with codes for end-stage renal disease, organ transplant, or human immunodeficiency virus owing to unique risk factors for complications. Medical claims were restricted to paid claims. This study was approved by the Washington University Human Research Protection Office, which did not require informed consent for this retrospective review of claims data.
Patient Population
We identified mastectomy operations among women aged 18 to 64 years from January 1, 2004, through December 31, 2011, using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and/or Current Procedural Terminology, 4th edition (CPT-4) procedure codes from inpatient and outpatient facility and clinician claims, as previously described. We limited primary analyses to the first mastectomy per patient and the first subsequent reconstruction procedure within 365 days of mastectomy. We required at least 90 days of insurance coverage after the mastectomy and after the first DR or SR to identify SSIs and NIWCs. Patient characteristics, including demographic features, comorbidities, and cancer-related and operative factors, were defined as previously described.
Procedure Dates and Definitions
Mastectomy and reconstruction dates within 7 days were collapsed into single-surgery dates because of potential date inaccuracy. An implant or autologous breast reconstruction code within 7 days of the index mastectomy was considered IR. Breast reconstruction coded more than 7 days after the mastectomy date was considered to be a subsequent reconstruction, which we defined as delayed if the index mastectomy did not involve IR and secondary if the index mastectomy included IR.
Classification of Procedures
We classified mastectomy and IR as described previously. Implant IR included tissue expander and permanent implant insertion; autologous IR included latissimus dorsi, transverse rectus abdominus myocutaneous, deep inferior epigastric artery perforator, superficial inferior epigastric artery, and gluteal artery perforator flaps. Delayed reconstruction included implant insertion and/or autologous reconstruction; SR included implant insertion, exchange of tissue expander or permanent prosthesis (CPT-4 code 11970 or codes for implant removal plus insertion), and/or autologous reconstruction. Implant DR procedures were excluded if another implant reconstruction code(s) was used, suggesting that the procedures were more likely to be second stage (CPT-4 codes 11970, 11971, 19328, 19370, 19371, or 19380; ICD-9-CM procedure codes 85.93, 85.94, or 85.96). Secondary reconstruction included second-stage or revision ipsilateral reconstruction and symmetry procedures on the contralateral breast. In addition to the implant and autologous procedures captured as part of IR, DR, or SR, other reconstruction procedures were captured within 2 years after the index mastectomy, including implant removal without insertion, revision of reconstruction, mastopexy, capsulectomy, nipple reconstruction, and reduction mammoplasty.
Identification and Timing of SSIs and NIWCs
We identified SSIs using a claims-based adaptation of the Centers for Disease Control and Prevention National Healthcare Safety Network definition of SSI. We identified NIWCs (ie, tissue necrosis, dehiscence, hematoma, and fat necrosis) using ICD-9-CM diagnosis codes, as described previously. The time frame for identifying wound complications was limited to 2 to 90 days after each immediate, delayed, and secondary reconstructive operation (1-90 days for hematoma; hematomas can occur soon after the procedure) because we only required health insurance coverage through 90 days after each procedure. Complications were further categorized by severity. We defined serious complications as those diagnosed during an inpatient admission or within 14 days before or after surgical wound care (incision/drainage codes except ICD-9-CM procedure codes 85.91, 86.01, and 86.28) requiring reoperation (identified by UB-04 medical revenue code[s] for operating room services) or implant removal or exchange (CPT-4 code 11970 or codes for implant removal plus insertion). In the analysis of complications after secondary reconstruction, 198 women with implant IR were excluded because they had an SSI coded more than 90 days after the index mastectomy, of whom 105 underwent SR. Similarly, 136 women with implant IR were excluded because they had an NIWC coded more than 90 days after the index mastectomy, of whom 79 underwent SR.
Identification of Chemotherapy and Radiotherapy
Adjuvant treatment was defined as having 2 or more distinct dates coded for radiotherapy or chemotherapy, as defined previously except for ICD-9-CM diagnosis codes for chemotherapy and radiotherapy and CPT-4 code 96402 for chemotherapy. We examined the association of radiotherapy with complications after DR and SR, including only radiotherapy after mastectomy and before DR or SR. To examine the association of IR complications within 90 days with initiation of adjuvant chemotherapy and radiotherapy, we determined the time to first chemotherapy and/or radiotherapy treatment within 365 days of mastectomy, excluding women who had treatment initiation before a wound complication.
Statistical Analysis
Data were analyzed from January 1, 2015, through February 7, 2017. We compared the incidence of wound complications within 90 days after IR, DR, or SR using a χ2 test or logistic regression for unpaired comparisons. The McNemar test was used for paired comparisons of complications after implant IR vs implant SR within a woman. A Kruskal-Wallis test was used to compare continuous variables. All data management and statistical analyses were performed using SAS software (version 9.3; SAS Institute Inc).
Results
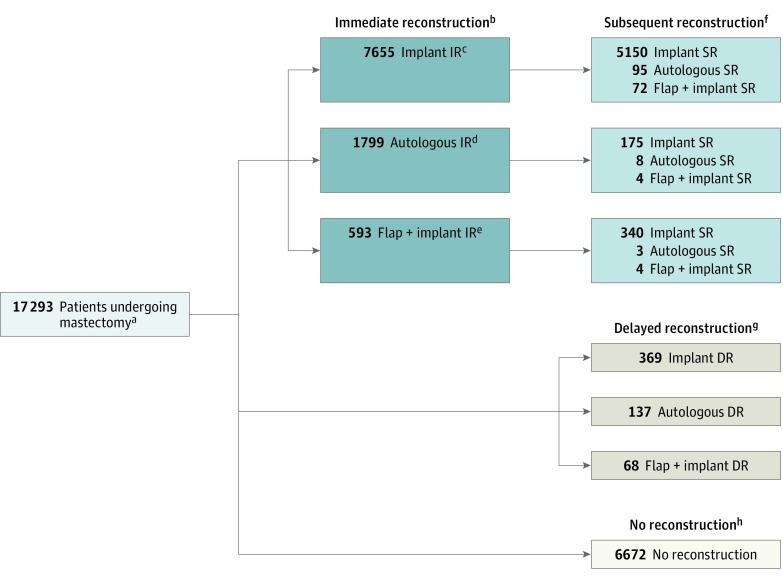
A total of 17 293 women (mean [SD] age, 50.4 [8.5] years) with mastectomy met study eligibility criteria (Figure 1). Mastectomy procedures included IR in 10 047 women (58.1%), of which 7655 (76.2%) involved an implant only; 1799 (17.9%), autologous reconstruction; and 593 (5.9%), autologous plus implant reconstruction. A total of 6425 women had at least 1 subsequent breast reconstruction procedure within 1 year after mastectomy; the breakdown of DR vs SR and type of reconstructive procedure is shown in Figure 1. Most implant IR and implant DR procedures involved tissue expanders (7102 [92.8%] and 349 [94.6%], respectively), whereas most implant SR procedures involved a permanent implant (5207 [91.9%]).
Figure 1. Diagram of Study Population, Including Index Mastectomy and Immediate and Subsequent Reconstruction After Mastectomy.
aWe required all women included in the study population to have at least 90 days of insurance coverage after mastectomy. The women with subsequent breast reconstruction procedure(s) were more likely to have at least 1 year of health insurance coverage after mastectomy than those without a subsequent reconstruction procedure (5763 [89.7%] vs 8194 [75.4%]; P < .001). Among women with less than 1 year of coverage after mastectomy, those with a subsequent procedure had a greater median number of days of health insurance coverage (295 vs 227 days; P < .001).
bImmediate reconstruction (IR) occurred within 7 days of mastectomy.
cIncludes tissue expander or permanent implant.
dIncludes use of an autologous tissue flap (abdominal, buttock, and back tissue transferred on its vascular pedicle or by free tissue transfer microsurgical anastomosis techniques).
eIncludes use of an implant and autologous tissue flap, as defined above.
fIncludes a woman’s first subsequent reconstruction 8 to 365 days after the index mastectomy. The first subsequent implant reconstruction (secondary reconstruction [SR] or delayed reconstruction [DR]) was performed a median of 156 days after mastectomy (interquartile range [IQR], 112-210 days); the first subsequent autologous reconstruction (with or without implant), a median of 232 days (IQR, 157-294 days) after mastectomy (P < .001). Implant DR was performed at a later date after mastectomy than was implant SR (181 days [IQR, 113-252 days] vs 155 days [IQR, 112-207 days]; P < .001), and autologous DR was performed at a later date than was autologous SR (250 days [IQR, 189-299 days] vs 209 days [IQR, 133-279 days]; P = .007).
gPerformed in patients without IR.
hIndicates no implant or flap reconstruction within 365 days of mastectomy. Implant procedures consistent with contralateral procedures were included in this group (eg, implant insertion in a woman with unilateral mastectomy without immediate reconstruction but with other code[s] consistent with secondary implant procedures [eg, capsulectomy]). Because we only required 90 days of health insurance enrollment after mastectomy, some women may have had DR at 91 to 365 days that we could not identify owing to cessation of insurance coverage.
Women who had DR (vs IR) were more likely to live in a rural (vs urban) location (69 [18.8%] vs 667 [9.7%]; P < .001); have tobacco use disorder (62 [16.8%] vs 831 [12.1%]; P = .007); use oral corticiosteroids (54 [14.7%] vs 695 [10.1%]; P = .01); have anemia (29 [7.9%] vs 379 [5.5%]; P = .05); have a higher cancer stage, defined as regional or metastatic cancer (135 [23.5%] vs 1734 [17.3%]; P < .001); and were less likely to have had previous breast cancer (45 [12.2%] vs 1170 [17.0%]; P = .02). Women with DR were also more likely to have undergone modified radical mastectomy (163 [44.3%] vs 2227 [32.4%]; P < .001) and unilateral mastectomy (240 [65.2%] vs 3118 [45.3%]; P < .001).
Overall Wound Complication Incidence After Reconstruction
The incidence of SSI and NIWCs within 90 days after IR, DR, and SR are shown in Table 1. Overall, 865 SSIs (74.9%) and 734 NIWCs (59.0%) were categorized as serious complications. The incidence of SSI and NIWCs were significantly higher after implant IR (373 of 5150 [7.2%] and 420 of 5150 [8.2%], respectively) compared with implant SR (167 of 5150 [3.2%] and 134 of 5150 [2.6%]; P < .001 for both in matched comparisons within a woman) (Table 1). The 90-day SSI incidence was significantly higher after implant IR (685 of 7655 [8.9%]) compared with implant DR (21 of 369 [5.7%]; P = .04) (Table 1). The SSI incidence was also significantly higher after implant IR compared with implant SR after autologous tissue flap plus implant IR (6 of 340 [1.8%]; P < .001) and with implant SR after autologous IR (3 of 175 [1.7%]; P = .003). Similarly, the 90-day NIWC rates were significantly higher after implant IR (717 of 7655 [9.4%]) compared with implant DR (15 of 369 [4.1%]) and implant SR after autologous tissue flap plus implant IR (9 of 340 [2.7%]; P < .001) and with implant SR after autologous tissue flap IR (8 of 175 [4.6%]; P = .03). In contrast, the 90-day wound complication rates were similar in women who underwent autologous tissue flap reconstruction regardless of the timing of reconstruction (Table 1). In women undergoing IR, we found no difference in the incidence of SSI (629 of 7102 [8.9%] vs 56 of 553 [10.1%]; P = .31) or NIWC (664 of 7102 [9.3%] vs 53 of 553 [9.6%]; P = .86) based on the use of tissue expanders vs permanent implants.
Table 1. Incidence of Complications Within 90 Days After Immediate, Delayed, and Secondary Breast Reconstruction Procedures.
| Reconstruction Type | No. of Patients | Complication | |||||
|---|---|---|---|---|---|---|---|
| SSI | NIWC | SSI or NIWC | |||||
| No. (%) | P Valuea | No. (%) | P Valuea | No. (%) | P Valuea | ||
| Implant IR | 7655 | 685 (8.9) | NA | 717 (9.4) | NA | 1180 (15.4) | NA |
| Subsequent implant | |||||||
| Implant SR after implant IR | 5150 | 167 (3.2) | <.001b | 134 (2.6) | <.001b | 268 (5.2) | <.001b |
| Implant DR | 369 | 21 (5.7) | .04 | 15 (4.1) | .001 | 31 (8.4) | <.001 |
| Implant SR after autologous IR | 175 | 3 (1.7) | .003 | 8 (4.6) | .03 | 11 (6.3) | .001 |
| Implant SR after autologous tissue flap plus implant IR | 340 | 6 (1.8) | <.001 | 9 (2.6) | <.001 | 15 (4.4) | <.001 |
| Autologous tissue flap | |||||||
| Autologous IR | 1799 | 177 (9.8) | NA | 250 (13.9) | NA | 342 (19.0) | NA |
| Autologous tissue flap plus implant IR | 593 | 52 (8.8) | .44 | 63 (10.6) | .04 | 98 (16.5) | .18 |
| Subsequent autologous flapc | |||||||
| Autologous DR | 137 | 19 (13.9) | .13 | 23 (16.8) | .35 | 32 (23.4) | .22 |
| Autologous tissue flap plus implant DR | 68 | 4 (5.9) | .29 | 4 (5.9) | .07 | 7 (10.3) | .08 |
| Autologous SR after implant IR | 95 | 11 (11.6) | .58 | 11 (11.6) | .52 | 18 (18.9) | .99 |
| Autologous tissue flap plus implant SR after implant IR | 72 | 8 (11.1) | .72 | 6 (8.3) | .18 | 11 (15.3) | .43 |
Abbreviations: DR, delayed reconstruction; IR, immediate reconstruction; NA, not applicable; NIWC, noninfectious wound complication; SR, secondary reconstruction; SSI, surgical site infection.
Calculated using logistic regression, unless otherwise noted. For implant procedures, all P values refer to comparison with the results of implant IR. For autologous procedures, all P values refer to comparison with the results of autologous tissue flap IR.
Calculated using the McNemar test. For the matched comparisons, the population was restricted to women who had implant IR followed by implant SR (n = 5150).
The following SR procedures were not included owing to small numbers: 8 autologous tissue SR procedures after autologous IR, 4 autologous tissue SR procedures with implant after autologous IR, 3 autologous tissue SR procedures after autologous tissue flap plus implant IR, and 4 flap with implant SR procedures after autologous tissue flap plus implant IR.
Failed implant reconstruction, defined as implant removal or exchange within 60 days of insertion, occurred in 532 women (7.0%) after IR and 30 women (8.1%) after DR (P = .39). Among women with SSI, implant failure occurred in 300 IR (43.8%) and 12 DR procedures (57.1%; P = .23).
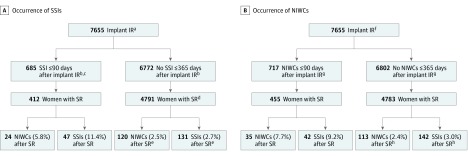
Influence of Wound Complications After IR
The association of SSI after implant IR with wound complications after SR is shown in Figure 2A. The incidence of SSI after SR (implant or autologous) in women who had an SSI after implant IR was significantly higher than in women who did not have an SSI within 365 days after implant IR (47 of 412 [11.4%] vs 131 of 4791 [2.7%]; P < .001). An analogous result was obtained for NIWCs, with significantly higher incidence of NIWCs in women who had an SSI after implant IR compared with women without an SSI after implant IR (24 of 412 [5.8%] vs 120 of 4791 [2.5%]; P < .001). When the analysis was restricted to women who had only implant SR (excluding women with autologous SR after implant IR), the SSI rate after implant SR remained significantly higher in women who had an SSI after implant IR compared with women without an SSI after implant IR (42 of 373 [11.3%] vs 117 of 4673 [2.5%]; P < .001). Similar to the results depicted in Figure 2A, the rates of NIWC and SSI after SR were significantly higher in women with an NIWC after implant IR (35 of 455 [7.7%] and 42 of 455 [9.2%], respectively; P < .001) (Figure 2B).
Figure 2. Incidence of Surgical Site Infection (SSI) and Noninfectious Wound Complications (NIWCs) After Secondary Reconstruction (SR) Stratified by SSI and NIWC After Immediate Implant Reconstruction .
aSSIs attributable to the immediate implant reconstruction (implant IR) were identified within 90 days of the index procedure. Follow-up to identify SR was performed through 365 days after mastectomy.
bIndicates attributable to implant IR.
cOf these, 273 (39.9%) did not have a secondary reconstructive procedure within 365 days of the index surgery.
dExcludes 9 women with an SSI or cellulitis within 30 days before SR, not attributable to implant IR.
eIf we included the 105 women with SSI more than 90 days after implant IR who had SR in the uninfected category, an additional 8 women had an SSI and 6 women had an NIWC after SR, bringing the total number of SSIs attributable to SR to 139 (2.9%) and the total number of NIWCs attributable to SR to 126 (2.6%). Compared with the incidence of SSI and NIWCs for women who had SSI within 90 days after implant IR, the differences remain statistically significant (P < .001).
fNIWCs attributable to the immediate implant reconstruction were identified within 90 days of the index procedure. Follow-up to identify SR was performed through 365 days after mastectomy.
gIndicates attributable to implant IR.
hIf we included the 79 women with NIWCs more than 90 days after implant IR who had SR into the uncomplicated category, an additional 2 women had an SSI and 3 women had an NIWC after SR, bringing the total number of SSIs attributable to SR to 144 (3.0%) and the total number of NIWCs attributable to SR to 116 (2.4%). Compared with the incidence of SSI and NIWCs for women who had NIWCs within 90 days after implant IR, the differences remain statistically significant (P < .001).
Compared with women without a wound complication after IR, women with IR-associated wound complications underwent significantly more breast procedures within 2 years after the index operation (Table 2). The difference in number of procedures after implant IR was greater in women with SSI (mean, 2.08; range, 0-9) and NIWCs (mean, 1.88; range, 0-9) vs women without a wound complication (1.37; range, 0-8) than in women after autologous IR with SSI (mean, 1.14; range, 0-6) and NIWCs (mean, 1.12; range, 0-6) vs women without a wound complication (mean of 0.87; range, 0-6). Women who had a wound complication after IR started chemotherapy 2 weeks later than women who did not have an IR wound complication (median start of chemotherapy, 53 vs 39 days after mastectomy; P < .001). Similarly, women who had a wound complication after IR had a median 3-week delay in initiation of radiotherapy compared with women who did not have a wound complication after IR (median start of radiotherapy, 162 vs 142 days after mastectomy; P < .001).
Table 2. Subsequent Breast Reconstruction and Revision Procedures Within 2 Years of Immediate Reconstruction According to 90-Day Complications After Immediate Implant or Autologous Reconstructiona.
| Type of IR, Complication | No. of Complications ≤90 d After Mastectomyb | No. of Subsequent Reconstruction or Revision Procedures, Mean (Range)c | P Valued | |
|---|---|---|---|---|
| Implant (n = 7655) | ||||
| None | 6475 | 1.37 (0-8) | Reference | |
| SSI | 685 | 2.08 (0-9) | <.001 | |
| NIWC | 717 | 1.88 (0-9) | <.001 | |
| SSI or NIWC | 1180 | 1.92 (0-9) | <.001 | |
| Autologous flap only (n = 1799) | ||||
| None | 1457 | 0.87 (0-6) | Reference | |
| SSI | 177 | 1.14 (0-6) | .002 | |
| NIWC | 250 | 1.12 (0-6) | .002 | |
| SSI or NIWC | 342 | 1.11 (0-6) | <.001 | |
| Autologous flap plus implant (n = 593) | ||||
| None | 495 | 1.30 (0-7) | Reference | |
| SSI | 52 | 1.58 (0-5) | .34 | |
| NIWC | 63 | 1.41 (0-4) | .64 | |
| SSI or NIWC | 98 | 1.51 (0-5) | .22 | |
Abbreviations: IR, immediate reconstruction; NIWC, noninfectious wound complication; SSI, surgical site infection.
Subsequent reconstruction or revision procedures included the first secondary implant or autologous procedure; implant removal without insertion, revision of reconstruction, mastopexy, capsulectomy, nipple reconstruction, reduction mammoplasty, and any additional subsequent autologous or implant procedures (ie, autologous and implant insertion codes in addition to the following: Current Procedural Terminology, 4th edition codes 11970, 11971, 19316, 19318, 19328, 19350, 19370, 19371, and 19380; International Classification of Diseases, Ninth Revision, Clinical Modification procedure codes 85.31, 85.32, 85.6, 85.87, 85.89, 85.93, 85.94, and 85.96). Of all procedures within 2 years after mastectomy and before any subsequent mastectomy, 5851 (43.0%) were the first secondary implant or autologous procedure. Overall, the most common follow-up procedure was implant exchange or insertion (8212 [60.4%] of all procedures within 2 years), followed by nipple reconstruction (with or without revision or mastopexy, 2565 [18.9%]), revision or mastopexy only (1063 [7.8%]), implant removal only (806 [5.9%]), and autologous flap reconstruction without an implant (230 [1.7%]).
SSI and NIWC categories are not mutually exclusive; thus, the sum of the number of women by complication category is greater than the number of women with IR.
Includes subsequent procedures up to 2 years after mastectomy and before any subsequent mastectomy. Among women with IR, 8172 (81%) had at least 1 year of enrollment and 5683 (57%) had at least 2 years of health insurance enrollment after mastectomy.
Calculated using the Kruskal-Wallis test comparing SSI vs no complication and NIWC vs no complication.
Association of Adjuvant Radiotherapy With Incidence of Wound Complications
Adjuvant radiotherapy was administered after mastectomy to 34 of 369 women before implant DR (9.2%) and 379 of 5665 women before implant SR (6.7%) (Table 3). Prior receipt of adjuvant radiotherapy was associated with approximately 2-fold higher incidence of wound complications after implant SR but was not associated with higher complication rates in women who underwent implant DR after adjuvant radiotherapy (Table 3). Among women who had subsequent autologous tissue reconstruction, 85 of 205 (41.5%) with autologous DR and 51 of 186 (27.4%) with autologous SR received adjuvant radiotherapy before the reconstruction. The incidence of any wound complication was not significantly different when comparing implant DR, autologous DR, or autologous SR according to receipt of adjuvant radiotherapy, although the number of women with complications in individual comparisons was very small (Table 3).
Table 3. Incidence of 90-Day Complications After Delayed and Secondary Breast Reconstruction According to Receipt of Adjuvant Radiotherapya.
| Reconstruction Type | No. of Patients | Complication | |||||
|---|---|---|---|---|---|---|---|
| SSI | NIWC | SSI or NIWC | |||||
| No. (%) | P Valueb | No. (%) | P Valueb | No. (%) | P Valueb | ||
| Implant DR | |||||||
| Radiotherapy | 34 | 4 (11.8) | .12c | 2 (5.9) | .64c | 4 (11.8) | .51c |
| No radiotherapy | 335 | 17 (5.1) | 13 (3.9) | 27 (8.1) | |||
| Autologous tissue flap ± implant DR | |||||||
| Radiotherapy | 85 | 5 (5.9) | .04 | 9 (10.6) | .36 | 14 (16.5) | .43 |
| No radiotherapy | 120 | 18 (15) | 18 (15) | 25 (20.8) | |||
| Implant SR | |||||||
| Radiotherapy | 379 | 24 (6.3) | <.001 | 22 (5.8) | <.001 | 41 (10.8) | <.001 |
| No radiotherapy | 5286 | 152 (2.9) | 129 (2.4) | 253 (4.8) | |||
| Autologous tissue flap ± implant SR | |||||||
| Radiotherapy | 51 | 5 (9.8) | .69 | 1 (2) | .01 | 6 (11.8) | .19 |
| No radiotherapy | 135 | 16 (11.9) | 20 (14.8) | 27 (20) | |||
Abbreviations: DR, delayed reconstruction; NIWC, noninfectious wound complication; SR, secondary reconstruction; SSI, surgical site infection.
Adjuvant radiotherapy was administered after mastectomy and before DR or SR.
Calculated using the χ2 test, unless otherwise indicated.
Calculated using the Fisher exact test.
Discussion
To our knowledge, this study is the largest to date comparing rates of SSI and NIWCs after immediate, delayed, and secondary breast reconstruction. We found that the incidence of wound complications was higher after implant IR than after implant DR or SR. In contrast, no difference was found in the incidence of complications after autologous IR compared with autologous DR or SR, although the number of procedures was smaller. Our finding of lower rates of wound complications after DR compared with IR is important because the women who had DR were more likely to have characteristics associated with a higher risk for SSI than were women who underwent IR (eg, tobacco use disorder, rural residence). Thus, these women likely would have had even higher wound complication rates if they underwent immediate rather than delayed reconstruction. Wound complications after implant IR were associated with high rates of implant failure, and women who had wound complications after implant IR were also more likely have additional wound complications after secondary reconstructive procedures. Women who had a wound complication after IR underwent more subsequent breast procedures and had delayed adjuvant treatment initiation compared with women who did not have a wound complication after IR.
Consensus is lacking in the literature regarding differences in complication rates after IR vs DR for autologous tissue flap and implant reconstructions. Several small studies have reported similar wound complication rates after autologous IR vs DR, whereas others have found higher complication rates after autologous IR. Sullivan and colleagues reported a higher incidence of overall complications after implant IR compared with DR procedures, whereas 2 other groups reported no difference, although these studies included only a small number of implant DR procedures. Consistent with our finding of increased incidence of wound complications after implant IR vs implant SR, Lovecchio et al and Cordeiro and McCarthy reported significantly higher complication rates after implant IR compared with SR exchange procedures. In contrast to studies that did not find a difference in complication rates, our study was larger and we compared wound complication rates after implant IR vs SR within a woman using matched-pairs analysis to account for lack of independence of events.
Several investigators have used the National Surgical Quality Improvement Program database to analyze 30-day complication rates after IR compared with DR. Gart and colleagues reported a decreased risk for SSI and total complications associated with immediate compared with delayed autologous reconstruction, although these findings varied by tissue flap type. Chung et al found no difference in SSI rates between IR and DR microvascular autologous tissue flap procedures. More recently, Sanati-Mehrizy et al found an increased risk for 30-day complications after autologous DR and implant DR using tissue expanders compared with IR. In contrast to the National Surgical Quality Improvement Program studies, we compared SSI and NIWC rates after IR, DR, and SR procedures and identified complications within 90 days of operation rather than 30 days, based on a previous finding that only 50% of SSIs were identified within 30 days of mastectomy with implant IR but almost 90% were identified within 90 days.
One possible explanation for increased complication rates after implant IR is the substantial dead space and hypovascular field in which the initial implant is placed, compared with the surgical field at the time of delayed or second-stage implant insertion. Another explanation for the higher complication rates is the longer operation times often required for IR owing to the performance of 2 sequential procedures.
Women who developed an SSI after implant IR were more likely to have another SSI and/or an NIWC after any SR procedure. Similarly, NIWCs after implant IR were associated with a higher incidence of NIWCs and SSI after SR. Adkinson and colleagues reported higher rates of complications and permanent implant loss after implant SR in women who had a complication after tissue expander insertion, although they did not report the secondary procedure complication risk according to the specific type of wound complication after the initial surgery. Thus, wound complications after implant IR appear to result in a prolonged risk for complications after subsequent procedures, possibly because of a poor soft-tissue envelope or continued low-level infection. An additional explanation may be that women who had a complication after their initial procedure had an inherently higher risk for complications and thus were more likely to have another complication after SR.
We found that adjuvant radiotherapy was associated with higher SSI and NIWC rates after implant SR. Several investigators have reported higher rates of total complications with second-stage implants, infection and wound breakdown, and reconstruction failure in women who received adjuvant radiotherapy after tissue expander or implant IR. In contrast, among women undergoing subsequent autologous reconstruction, we did not find increased rates of SSI or NIWCs after adjuvant radiotherapy. This finding is consistent with reports in the literature of the lack of association between radiotherapy and outcomes of autologous reconstruction.
Limitations
Claims data were designed for administrative purposes and have limitations, including misclassification of diagnoses and likely undercoding of SSIs and NIWCs, especially minor complications treated without additional procedures during the 90-day global surgical reimbursement period. A previous study reported the positive predictive values for identification of SSIs and NIWCs in this same population based on medical record review. Although the positive predictive value for SSI (57.5%) was lower than for a composite NIWC group (dehiscence or fat or tissue necrosis, 86.8%), most of the patients coded in error for SSI had a documented wound complication (most often cellulitis or an NIWC). Some of the procedures that we identified as SR may have been symmetry procedures on the contralateral side. Because the duration of continuous private insurance enrollment was variable, we limited our study to subsequent breast reconstruction within 1 year and complications within 90 days to limit loss to follow-up. Therefore, we are missing later complications and subsequent procedures and may be underestimating these rates. The incidence of complications after procedures performed from 2004 to 2011 may also underestimate the burden in the current era because of increased use of skin- and nipple areola complex–sparing mastectomy to optimize cosmesis, with a potentially increased risk for complications.
Conclusions
We found an increased incidence of infectious and noninfectious wound complications after immediate compared with delayed implant reconstruction, despite the higher risk profile of the population undergoing DR. Confirmation of these results in a prospective multicenter study that tracks individual outcomes in all settings will be important to verify the increased risk for wound complications after IR. Our finding of poorer outcomes associated with IR complications, including increased wound complication rates after the next reconstruction procedure, more subsequent breast procedures, and delay of the start of adjuvant treatment, underscores the need to communicate individualized complication risk to women considering IR. Consideration of the timing of implant reconstruction in relation to radiotherapy is also important. Our results suggest that some high-risk patients may benefit from delayed rather than immediate implant reconstruction or from the use of autologous reconstruction to decrease their risk for serious wound complications. Given trends of patients with increasingly medically complex problems undergoing breast reconstruction, tailoring of preventive measures to patients’ unique risk factors and/or careful consideration of the best timing of reconstruction may be needed to prevent complications after immediate and subsequent breast reconstruction procedures.
References
- 1.Jagsi R, Jiang J, Momoh AO, et al. Trends and variation in use of breast reconstruction in patients with breast cancer undergoing mastectomy in the United States. J Clin Oncol. 2014;32(9):919-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in US breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131(1):15-23. [DOI] [PubMed] [Google Scholar]
- 3.Kummerow KL, Du L, Penson DF, Shyr Y, Hooks MA. Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg. 2015;150(1):9-16. [DOI] [PubMed] [Google Scholar]
- 4.Merchant SJ, Goldstein L, Kruper LL. Patterns and trends in immediate postmastectomy reconstruction in California: complications and unscheduled readmissions. Plast Reconstr Surg. 2015;136(1):10e-19e. [DOI] [PubMed] [Google Scholar]
- 5.Serletti JM, Fosnot J, Nelson JA, Disa JJ, Bucky LP. Breast reconstruction after breast cancer. Plast Reconstr Surg. 2011;127(6):124e-135e. [DOI] [PubMed] [Google Scholar]
- 6.Parker PA, Youssef A, Walker S, et al. Short-term and long-term psychosocial adjustment and quality of life in women undergoing different surgical procedures for breast cancer. Ann Surg Oncol. 2007;14(11):3078-3089. [DOI] [PubMed] [Google Scholar]
- 7.Morrow M, Li Y, Alderman AK, et al. Access to breast reconstruction after mastectomy and patient perspectives on reconstruction decision making. JAMA Surg. 2014;149(10):1015-1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jagsi R, Li Y, Morrow M, et al. Patient-reported quality of life and satisfaction with cosmetic outcomes after breast conservation and mastectomy with and without reconstruction: results of a survey of breast cancer survivors. Ann Surg. 2015;261(6):1198-1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ananian P, Houvenaeghel G, Protière C, et al. Determinants of patients’ choice of reconstruction with mastectomy for primary breast cancer. Ann Surg Oncol. 2004;11(8):762-771. [DOI] [PubMed] [Google Scholar]
- 10.Albornoz CR, Cordeiro PG, Pusic AL, et al. Diminishing relative contraindications for immediate breast reconstruction: a multicenter study. J Am Coll Surg. 2014;219(4):788-795. [DOI] [PubMed] [Google Scholar]
- 11.Olsen MA, Nickel KB, Fox IK, et al. Incidence of surgical site infection following mastectomy with and without immediate reconstruction using private insurer claims data. Infect Control Hosp Epidemiol. 2015;36(8):907-914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Olsen MA, Nickel KB, Margenthaler JA, et al. Development of a risk prediction model to individualize risk factors for surgical site infection after mastectomy. Ann Surg Oncol. 2016;23(8):2471-2479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. National Healthcare Safety Network (NHSN) procedure-associated (PA) module: surgical site infection (SSI) event. 2017. https://www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf. Published January 2017. Accessed January 30, 2017.
- 14.Nickel KB, Fox IK, Margenthaler JA, Wallace AE, Fraser VJ, Olsen MA. Effect of noninfectious wound complications after mastectomy on subsequent surgical procedures and early implant loss. J Am Coll Surg. 2016;222(5):844-852.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sullivan SR, Fletcher DR, Isom CD, Isik FF. True incidence of all complications following immediate and delayed breast reconstruction. Plast Reconstr Surg. 2008;122(1):19-28. [DOI] [PubMed] [Google Scholar]
- 16.Miller RB, Reece G, Kroll SS, et al. Microvascular breast reconstruction in the diabetic patient. Plast Reconstr Surg. 2007;119(1):38-45. [DOI] [PubMed] [Google Scholar]
- 17.DeBono R, Thompson A, Stevenson JH. Immediate versus delayed free TRAM breast reconstruction: an analysis of perioperative factors and complications. Br J Plast Surg. 2002;55(2):111-116. [DOI] [PubMed] [Google Scholar]
- 18.Giacalone PL, Rathat G, Daures JP, Benos P, Azria D, Rouleau C. New concept for immediate breast reconstruction for invasive cancers: feasibility, oncological safety and esthetic outcome of post-neoadjuvant therapy immediate breast reconstruction versus delayed breast reconstruction: a prospective pilot study. Breast Cancer Res Treat. 2010;122(2):439-451. [DOI] [PubMed] [Google Scholar]
- 19.Carlson GW, Page AL, Peters K, Ashinoff R, Schaefer T, Losken A. Effects of radiation therapy on pedicled transverse rectus abdominis myocutaneous flap breast reconstruction. Ann Plast Surg. 2008;60(5):568-572. [DOI] [PubMed] [Google Scholar]
- 20.Alderman AK, Wilkins EG, Kim HM, Lowery JC. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2002;109(7):2265-2274. [DOI] [PubMed] [Google Scholar]
- 21.Nahabedian MY, Tsangaris T, Momen B, Manson PN. Infectious complications following breast reconstruction with expanders and implants. Plast Reconstr Surg. 2003;112(2):467-476. [DOI] [PubMed] [Google Scholar]
- 22.Cordeiro PG, McCarthy CM. A single surgeon’s 12-year experience with tissue expander/implant breast reconstruction: part I—a prospective analysis of early complications. Plast Reconstr Surg. 2006;118(4):825-831. [DOI] [PubMed] [Google Scholar]
- 23.Lovecchio F, Jordan SW, Lim S, Fine NA, Kim JY. Risk factors for complications differ between stages of tissue-expander breast reconstruction. Ann Plast Surg. 2015;75(3):275-280. [DOI] [PubMed] [Google Scholar]
- 24.Gart MS, Smetona JT, Hanwright PJ, et al. Autologous options for postmastectomy breast reconstruction: a comparison of outcomes based on the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2013;216(2):229-238. [DOI] [PubMed] [Google Scholar]
- 25.Chung CU, Wink JD, Nelson JA, Fischer JP, Serletti JM, Kanchwala SK. Surgical site infections after free flap breast reconstruction: an analysis of 2899 patients from the ACS-NSQIP datasets. J Reconstr Microsurg. 2015;31(6):434-441. [DOI] [PubMed] [Google Scholar]
- 26.Sanati-Mehrizy P, Massenburg BB, Rozehnal JM, et al. A comparison of postoperative outcomes in immediate versus delayed reconstruction after mastectomy. Eplasty. 2015;15:e44. [PMC free article] [PubMed] [Google Scholar]
- 27.Lankiewicz JD, Yokoe DS, Olsen MA, et al. Beyond 30 days: does limiting the duration of surgical site infection follow-up limit detection? Infect Control Hosp Epidemiol. 2012;33(2):202-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Adkinson JM, Miller NF, Eid SM, Miles MG, Murphy RX Jr. Tissue expander complications predict permanent implant complications and failure of breast reconstruction. Ann Plast Surg. 2015;75(1):24-28. [DOI] [PubMed] [Google Scholar]
- 29.Wang F, Peled AW, Chin R, et al. The impact of radiation therapy, lymph node dissection, and hormonal therapy on outcomes of tissue expander-implant exchange in prosthetic breast reconstruction. Plast Reconstr Surg. 2016;137(1):1-9. [DOI] [PubMed] [Google Scholar]
- 30.Spear SL, Seruya M, Rao SS, et al. Two-stage prosthetic breast reconstruction using AlloDerm including outcomes of different timings of radiotherapy. Plast Reconstr Surg. 2012;130(1):1-9. [DOI] [PubMed] [Google Scholar]
- 31.Nava MB, Pennati AE, Lozza L, Spano A, Zambetti M, Catanuto G. Outcome of different timings of radiotherapy in implant-based breast reconstructions. Plast Reconstr Surg. 2011;128(2):353-359. [DOI] [PubMed] [Google Scholar]
- 32.Eriksson M, Anveden L, Celebioglu F, et al. Radiotherapy in implant-based immediate breast reconstruction: risk factors, surgical outcomes, and patient-reported outcome measures in a large Swedish multicenter cohort. Breast Cancer Res Treat. 2013;142(3):591-601. [DOI] [PubMed] [Google Scholar]
- 33.Cordeiro PG, Albornoz CR, McCormick B, et al. What is the optimum timing of postmastectomy radiotherapy in two-stage prosthetic reconstruction: radiation to the tissue expander or permanent implant? Plast Reconstr Surg. 2015;135(6):1509-1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ho A, Cordeiro P, Disa J, et al. Long-term outcomes in breast cancer patients undergoing immediate 2-stage expander/implant reconstruction and postmastectomy radiation. Cancer. 2012;118(9):2552-2559. [DOI] [PubMed] [Google Scholar]
- 35.Berry T, Brooks S, Sydow N, et al. Complication rates of radiation on tissue expander and autologous tissue breast reconstruction. Ann Surg Oncol. 2010;17(suppl 3):202-210. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Medicare & Medicaid Services Global surgery fact sheet. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/GloballSurgery-ICN907166.pdf. Published March 2015. Accessed August 5, 2015.
- 37.Olsen MA, Ball KE, Nickel KB, Wallace AE, Fraser VJ. Validation of ICD-9-CM diagnosis codes for surgical site infection and noninfectious wound complications after mastectomy. Infect Control Hosp Epidemiol. 2017;38(3):334-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peled AW, Wang F, Foster RD, et al. Expanding the indications for total skin-sparing mastectomy: is it safe for patients with locally advanced disease? Ann Surg Oncol. 2016;23(1):87-91. [DOI] [PubMed] [Google Scholar]
- 39.Hieken TJ, Boolbol SK, Dietz JR. Nipple-sparing mastectomy: indications, contraindications, risks, benefits, and techniques. Ann Surg Oncol. 2016;23(10):3138-3144. [DOI] [PubMed] [Google Scholar]