Abstract
While many studies have identified a significant relation between child maltreatment and adolescent substance use, the developmental pathways linking this relation remain sparsely explored. The current study examines posttraumatic stress (PTS) symptoms, mother-child relationships, and internalizing and externalizing problems as potential longitudinal pathways through which child maltreatment influences adolescent substance use. Structural equation modeling was conducted on 883 adolescents drawn from the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN). The pathways of PTS symptoms linked physical and sexual abuse to substance use, and the pathways of mother-child relationships linked emotional abuse and neglect to substance use. None of the four types of maltreatment affected substance use via internalizing or externalizing problems. The findings suggest that intervention efforts aimed at addressing posttraumatic stress symptoms and improving mother-child relationship quality may be beneficial in reducing substance use among adolescents with child maltreatment histories.
Keywords: Adolescent substance use, Child maltreatment, Posttraumatic stress symptoms, Mother-child relationship, Internalizing and externalizing problems, Adolescence
1. Introduction
Adolescent substance use presents a critical threat to public health. Substance use during adolescence may lead to problematic substance use that disturbs healthy youth development. Furthermore, substance use during adolescence has been found to be a strong predictor of the subsequent development of substance abuse or dependence over a lifespan (Anthony & Petronis, 1995; Patton et al., 2007; Shin, 2012). Negative developmental outcomes associated with adolescent substance use can include low academic achievement, impaired brain functioning, risky sexual behavior, unintended teen pregnancies, depression, suicidal attempts, and criminal involvement (Bava & Tapert, 2010; Danzo, Connell, & Stormshak, 2017; Guo et al., 2002; Marshall, 2014; Slade et al., 2008; Silins et al., 2014; Squeglia, Jacobus, & Tapert, 2009).
Alcohol, tobacco, and marijuana are the most prevalent substances used by adolescents, making them a strategic area of focus for prevention. According to the 2015 Monitoring the Future (MTF) study,39.9% of youth in 8th, 10th, and 12th grades reported drinking alcohol, 20.2% reported using cigarettes, and 23.7% reported using marijuana in the past year (Johnston, O’Malley, Miech, Bachman, & Schulenberg, 2016). Furthermore, evidence from the National Longitudinal Study of Adolescent Health (Add Health) indicated high prevalence (34.1%) of poly-substance use of alcohol, marijuana, and cigarettes (Moss, Chen, & Yi, 2014).
Adolescent substance use is of particular concern among youth who have experienced child maltreatment. While the estimates of substance use among victims of child maltreatment vary depending on how substance use was defined, prior studies have consistently reported higher rates of substance use among youth involved in the child welfare system compared to the general population (e.g., Traube, James, Zhang, & Landsverk 2012). These patterns are particularly pronounced for higher risk forms of substance use and substance use disorder (Braciszewski & Stout, 2012; Traube, James, Zhang, & Landsverk 2012)). In addition, a review on the association between maltreatment and adolescent substance use indicated that the majority of 31 included studies identified an elevated risk of substance use (alcohol, cigarette, and various drugs) among adolescents with a history of child maltreatment, establishing a firm link between maltreatment and substance use (Tonmyr, Thornton, Draca, & Wekerle, 2010).
1.1 Child Maltreatment and Adolescent Substance Use
Substantial research has indicated child maltreatment—including physical abuse, sexual abuse, emotional abuse, and neglect—as a risk factor for adolescent substance use (Bailey & McCloskey, 2005; Moran, Vuchinich, & Hall, 2004; Tonmyr et al., 2010). A robust body of literature supports the association between physical abuse and substance use in adolescence (Dube et al., 2006; Harrison, Fulkerson, & Beebe, 1997; Kobulsky, Holmes, Yoon, & Perzynski, 2016; Lansford, Dodge, Petit, & Bates, 2010; Shin, Miller, & Teicher, 2013). For example, physical abuse has been reported to be a significant predictor of adolescent drug use in a review study that included various school and community samples (Tonmyr et al., 2010). In a nationally representative child welfare-involved sample, physical abuse was associated with concurrent polysubstance use– defined as using more than one substance, including alcohol, cigarettes, marijuana, and other illegal drugs such as inhalants and ecstasy– (Snyder & Smith, 2015) and an increase in illicit substance use over time (Casanueva, Stambauh, Urato, Fraser, & Williams, 2014). Child sexual abuse is another type of maltreatment that has widely been recognized as a strong risk factor for adolescent substance use (Dube et al., 2006; Moran et al., 2004; Harrison et al., 1997; Shin et al., 2013; Tonmyr et al., 2010). For example, in a sample of youth recruited from battered women’s shelters and the general community, childhood sexual abuse has been found to increase the likelihood that girls aged 13-19 will eventually use substances, even after controlling for family dysfunction, maternal substance use, and other internalizing problems (depression and anxiety) (Bailey & McCloskey, 2005). Several studies have suggested emotional abuse as a risk factor for substance use (Highland, Herschl, Klanecky, & McChargue, 2013; Moran et al., 2004; Norman, Byambaa, De, Butchart, Scott, & Vos, 2012). For example, in a retrospective study of adults, Dube and colleagues (2006) found that childhood emotional abuse was associated with 2.5 times higher odds of initiating alcohol use during earlyadolescence . In another study, emotional abuse was significantly associated with higher tobacco, alcohol, and illicit drug use among public high school students, yet the magnitude of the effects of emotional abuse was smaller than that of physical or sexual abuse (Moran et al., 2004). Finally, childhood neglect is also related to an increase risk of substance use during adolescence (Dube et al., 2006; Shin et al., 2013; Tonmyr et al., 2010). Using Add Health data, Hussey and colleagues (2006) found that child neglect was associated with an increased likelihood of past 30-day cigarettes use, regular alcohol use, binge drinking, and marijuana use during adolescence. Finally, a review study found that neglect in childhood was related to an increased risk of drug use, but was not associated with alcohol problem drinking in adolescence (Norman et al., 2012).
1.2 Mechanisms Linking Child Maltreatment and Substance Use
While many studies have identified a significant relation between child maltreatment and adolescent substance use, the developmental pathways linking this relation remain sparsely explored. The developmental traumatology theory (De Bellis, 2001, 2002) and attachment theory (Bowlby, 1969) provide useful theoretical frameworks in exploring potential mechanisms through which child maltreatment influences substance use during adolescence (Hovdestad, Tonmyr, Wekerle, Thornton, 2011). Both the developmental traumatology theory and attachment theory have been widely applied as primary explanatory models explaining the association between childhood maltreatment and adolescent substance use (Hovdestad et al., 2011).
The developmental traumatology theory suggests that adverse psychological reactions that result from a highly traumatic and stressful event including posttraumatic stress (PTS; e.g., intrusive thoughts or memories, avoidance) and other internalizing problems (e.g., social withdrawal, depression, general anxiety), and externalizing problems (e.g., aggression), as important contributory mechanisms that connect childhood adversities and adolescent substance use (De Bellis, 2002). According to the developmental traumatology theory (De Bellis, 2001, 2002), early traumatic experiences—such as child maltreatment—may lead to the dysregulation of biological stress response systems, which may increase problems of emotional and behavioral regulation, leading to PTS symptoms, and internalizing and externalizing problems. These psychiatric symptoms, in turn, contribute to adolescents’ substance use as they seek to alleviate unpleasant psychiatric symptoms (De Bellis 2002).
In line with the developmental traumatology theory, empirical research has suggested the potential PTS connection between childhood maltreatment and adolescent substance use (e.g., Rosenkranz, Muller, & Henderson, 2014). For example, experiencing physical abuse and sexual abuse has been related to increased risk of PTS, and PTS has been reported to be a predictor of substance use (Goldstein et al., 2011; Ullman et al., 2009). Few studies, however, have examined PTS as a mechanism connecting maltreatment and substance use, and these studies have yielded mixed results. One study found a significant indirect pathway from overall maltreatment to adolescent substance use through complex PTS symptoms among youth seeking substance use treatment (Rosenkranz, Muller, & Henderson, 2014).) On the contrary, another study found no significant indirect effect of maltreatment on substance use through PTS (Faulkner, Goldstein, Wekerle, 2014). More research is needed to understand if PTS plays a mediating role in the link between maltreatment and adolescent substance use.
Past research has also examined internalizing and externalizing problems as paths connecting maltreatment to adolescent substance use and produced mixed results (Jones et al., 2013; Lewis et al., 2011). In general, studies have found that maltreatment leads to adolescent substance use via externalizing problems, but not internalizing problems (Handley, Rogosch, Cuild, & Cicchetti, 2015; Jones et al., 2013; Rogosch, Oshri, & Cicchetti, 2010). For instance, an intervening role was found only for externalizing problems, but not for internalizing problems, in an examination of the relation between sexual abuse by age 12 and alcohol use at age 14 (Jones et al., 2013). Conversely, Lewis and colleague (2011) found that internalizing problems mediate the relationship between child maltreatment and adolescent cigarette smoking. The mixed findings regarding the role of internalizing pathways to substance use warrant further investigation.
Bowlby’s (1969) attachment theory also guides the potential underlying pathways linking child maltreatment and adolescent substance use. Attachment theory posits that a child establishes secure attachment with his or her primary caregiver if the primary caregiver remains accessible and responsive to the child’s needs (Bowlby, 1969). According to this theory, the formation of secure attachment and positive caregiver-child relationships is a vital developmental task that leads to various favorable outcomes, such as adaptive behavioral functioning across the lifespan (Sroufe, 1979). Prior research has suggested that some maltreating parents, especially mothers who are neglecting their children, may be unable to provide sensitive and responsive caregiving that meet their children’s needs (Crittenden & Ainsworth, 1989), and thus, maltreated children may be at increased risk for developing insecure attachment and poor mother-child relationship quality. Those children with poor mother-child relationships may have difficulty in regulating their emotions (e.g., negative affect), which in turn may lead to the development of maladaptive emotion regulation strategies, such as substance use (Cooper, Shaver, & Collins, 1998; Reinert & Edwards, 2009).
The mother-child relationship may be an important mechanism that links child maltreatment and adolescent substance use, but has yet to be fully tested as an intervening variable. Empirical studies indicate that maltreated children are more likely to have insecure attachment and poor mother-child relationship than do non-maltreated children (e.g., Stronach et al., 2011), and poor mother-child relationship has been related to adolescent substance use (e.g., Ledoux, Miller, Choquet, & Plant, 2002). On the other hand, a positive and close mother-child relationship has been found to protect the child from substance use during adolescence (e.g., Branstetter, Furman, & Cottrell, 2009; Zhang, Welte, & Wieczorek, 1999). For example, adolescents with stronger parental attachment and positive relationships have a lower likelihood of initiating cigarette smoking (Foshee & Bauman, 1994) and using alcohol or other substances in adolescence (Kuntsche & Silbereisen, 1996). Further investigation is needed to examine the mother-child relationship as a mechanism through which maltreatment affects substance use in adolescence.
1.3 The Present Study
To date, the developmental pathways through which maltreatment increases risk for adolescent substance use have yet to be fully understood. In particular, little is known about longitudinal pathways from maltreatment to substance use covering the period from early- to mid- adolescence. The developmental psychopathology perspective (Sroufe & Rutter, 1984) suggests that earlier exposure to traumatic experiences can lead to later maladaptation, highlighting the need for investigation of longitudinal effects of childhood maltreatment (e.g., from birth to age 12) on the development of substance use in adolescence. To advance our knowledge regarding the longitudinal developmental pathways and mechanisms connecting maltreatment and substance use, this study addressed the following research question: Are PTS symptoms, mother-child relationships, and internalizing and externalizing problems significant underlying mechanisms of the developmental pathway from child maltreatment to adolescent substance use? It was hypothesized that child maltreatment would be associated with greater PTS symptoms, poor mother-child relationships, and higher levels of internalizing and externalizing problems, which in turn would be related to increased adolescent substance use (see theoretical framework in Figure 1).
Figure 1.
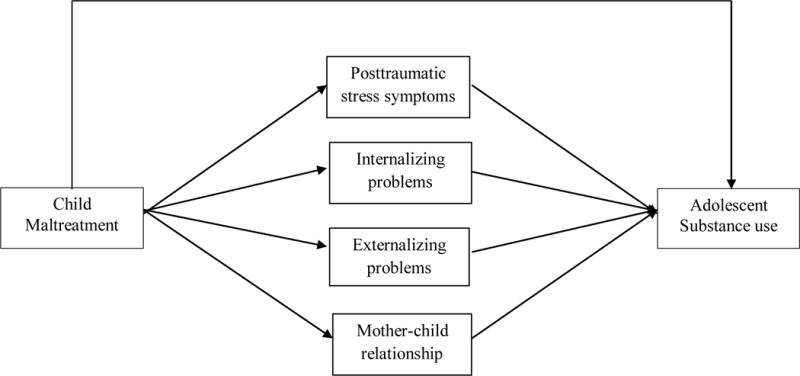
Conceptual model
2. Method
2.1 Data and Sample
This study used data from the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN), a multi-site (Midwest, Southwest, Northwest, South, and East) longitudinal study (N = 1,354) that investigates the etiology and consequences of child abuse and neglect (Larrabee & Lewis, 2014). LONGSCAN includes five pooled cohort samples that represent varying levels of risk or exposure to child maltreatment, ranging from children at high risk of maltreatment to CPS-involved children with substantiated maltreatment cases (Larrabee & Lewis, 2014). Regardless of the location, all children were enrolled when they were four years old or younger and were followed through the age of 18 years. All study sites also share measures, training, data collection methods, data entry, and management (Larrabee & Lewis, 2014). The present study utilizes data from 883 adolescents who had data at the age 12, 14, or 16 assessment, which represents 65% retention of the study participants. Adolescents in the study sample were more likely to be Black, and have mothers with less education and no spouse/partner. No other significant differences were found between the baseline sample and the study sample.
2.2 Measures
2.2.1 Substance use
Substance use was assessed at age 16, using adolescent self-report of tobacco, alcohol, and marijuana use frequency in the past month. Adolescents reported the number of days they smoked cigarettes, the number of days they had at least one drink of alcohol (i.e., beer, wine, wine coolers, malt liquor, or hard liquor), and the number of times they smoked marijuana (weed, pot, or grass) during the past 30 days. For cigarette and alcohol use, response options included: 1= 0 days, 2 = 1 or 2 days, 3 = 3 to 5 days, 4 = 6 to 9 days, 5 = 10 to 19 days, 6 = 20 to 29 days, and 7 = All 30 days. For marijuana use, response options included: 1= 0 times, 2 = 1 or 2 times, 3 = 3 to 9 times, 4 = 10 to 19 times, 5 = 20 to 39 times, and 6 = 40 or more times. Substance use was specified as a latent variable, using log-transformed frequency of alcohol, tobacco, and marijuana use as observed indicators.
2.2.2 Child maltreatment type
Lifetime history of child physical, sexual, and emotional abuse (i.e., abuse ever experienced over the lifetime) were assessed at age 12, using a set of LONGSCAN-developed self-report measures. The youth self-reported data of maltreatment collected at age 12 was chosen over official reports because the CPS data had a considerable amount of missing information (e.g., no CPS maltreatment type given: 8.9%; don’t know: 3.6%) on the type of maltreatment, which may bias the study results. In addition, youth self-reported measures of child maltreatment may have the advantage over official data of improved detection, given evidence from the National Incidence (Sedlak et al. 2010) and LONGSCAN (Everson et al., 2008) studies suggesting that much child maltreatment goes undetected by Child Protective Services. The physical abuse scale consisted of 15 dichotomous items (e.g., kicked, punched, choked) that assess a child’s lifetime experience of physical harm and threat of harm perpetrated by any caregiver. Responses were summed to create a total physical abuse score, with higher scores indicating more physical abuse experienced over the lifetime. Similarly, the child emotional abuse scale consisted of 18 dichotomous items (e.g., threatened to be hurt, humiliated badly) that assess a child’s experience of psychologically abusive parental behaviors. A total score was created by summing the responses to the items, with higher scores indicating more emotional abuse experienced during the lifetime. The sexual abuse scale comprised of four subscales that assess a child’s lifetime history of child sexual abuse perpetrated by any adults. The four subscales include the non-contact scale (3 items; e.g., having ever been forced to look at something sexual), fondling scale (4 items; e.g., having ever been touched their private parts), oral-genital contact scale (2 items; e.g., having ever been made to put mouth on others’ private parts), and penetration scale (2 items; e.g., having anyone ever put some part of their body inside my private parts or bottom). Higher scores on each subscale indicate more severe and broader sexual abuse experiences. Child sexual abuse was specified as a latent variable using the four subscales. Although psychometric data on the self-report measures are currently not available, there is preliminary evidence of superior predictive validity of the LONGSCAN child self-report measures in comparison to CPS determinations (Everson et al., 2008). Cronbach’s alphas for the physical abuse scale and emotional abuse scale are .70 and .82, respectively in this sample. Internal consistency for the sexual abuse subscales were acceptable, ranging from .67 (penetration) to .96 (fondling).
Child neglect was measured at age 12, using a modified version of the Multi-dimensional Neglectful Behavior Scale, Form A (MNBS-A) (Straus, Kinard, & Williams, 1995). The youth self-report neglect scale comprised of four subscales that assess neglectful parenting behaviors during the elementary school years and in the last year. Child neglect was specified as a latent variable using the four subscales: 1) physical neglect (7 items; e.g. not giving enough food to eat), 2) inadequate supervision (5 items; e.g., not knowing what the child is doing when he or she is not at home), 3) lack of emotional support (7 items; e.g., not comforting the child when he/she is upset) and 4) educational neglect (4 items; e.g., not making sure the child goes to school). The response categories included: 0 = never, 1 = almost never, 2 = sometimes, 3 = a lot. The positively worded items were reverse coded so that higher scores in this measure indicate more neglectful parenting behavior. The revised MNBS-A has been reported to have good internal consistency and modest to moderate convergent validity (Dubowitz et al., 2011). Cronbach’s alphas for the neglect subscales in the study sample were acceptable (physical neglect = .80; lack of emotional support = .82; inadequate supervision = .70; educational neglect = .71).
2.2.3 Posttraumatic stress symptoms
Posttraumatic stress (PTS) symptoms were measured at age 12 by youth self-report, using the PTS scale of the Trauma Symptoms Checklist for Children – Alternate Version (TSCC-A; Briere, 1996). The 10 items of the PTS scale include nightmares, intrusive thoughts, remembrances of scary or unwanted things, recollections of traumatic events, fears, and dissociative avoidance of painful feelings. For each item, youth reported the frequency of the experience in the past month, using a four-point Likert scale ranging from 0 = never to 3 = almost all the time. Scores were summed and transformed into standardized T scores (Briere, 1996), with higher scores indicating greater symptoms. The TSCC scales have demonstrated good internal consistency reliability and has also been found to have good concurrent validity, indicated by congruent results derived from similar measures such as Child Behavior Checklist (CBCL) (Briere, 1996). T scores greater equal to or greater than 65 are considered clinically elevated (Briere, 1996). Cronbach’s alpha for the PTS scale in this sample is .88.
2.2.4 Mother-child relationship
The mother-child relationship was measured at age 14 by youth self-report, using a six-item scale that assesses the quality of the relationship with the current mother/mother figure (i.e., someone who acts like a mother to the youth) on a five-point Likert scale ranging from 1 = never/not at all to 5 = always/very much. The items were adapted from the Add Health Study (Resnick et al., 1997) and include level of closeness, understanding, trust, shared decision-making, caring, and getting along well (e.g., “how close do you feel to your mother?” “how much you think she cares about you?”). A score of overall quality of the mother-child relationship was created summing the responses to these items, with a higher score indicating higher quality of the mother-child relationship. Preliminary evidence of reliability (i.e., good internal consistency) and convergent validity of the measure has been suggested (Knight, Smith, Martin, Lewis, & the LONGSCAN investigators, 2010). Cronbach’s alpha for the mother-child relationship scale in this sample is .83.
2.2.5 Internalizing and externalizing problems
Internalizing and externalizing problems were measured at age 14, using the Child Behavior Checklist/4-18 (CBCL: Achenbach, 1991), a standardized, caregiver-report measure of children’s social competences and behavior problems. Internalizing problems were measured using the internalizing behavior subscale which combines the social withdrawal, somatic complaints, and anxiety/depression scales. Externalizing behaviors were measured using the externalizing behavior subscale which combines the scores of the delinquency and aggressive behavior scales. Caregivers rated the extent to which each item applied to their child during the past 6 months, using the following response options: 0 = not true, 1 = somewhat or sometimes true, 2 = very true or often true. Standardized T scores were used with higher scores indicating greater behavior problems. T scores less than 60 represent the normal range, 60 to 63 represent the borderline, and scores greater than 63 are considered the clinical range (Achenbach, 1991). Cronbach’s alphas in this study were acceptable (internalizing: .87, externalizing: .93).
2.2.6 Control variables
Child’s age, race, and household income were reported by the caregiver at baseline (age 4 for the child). Child’s gender was coded as 0 = male, 1 = female. Child race was dummy-coded for Black, using Non-Black as the reference group. Household income was measured on an 11-point scale, ranging from 1 = < $5,000 per year to 11 = > $50,000 per year. Family substance use and peer substance use was measured at age 12. Family substance use was reported by youth using nine dichotomous items (e.g., use cocaine or crack, inject drugs) that assess substance use by household members. For peer substance, youth were asked if any of their friends used substance use (7 items: e.g., cigarette, alcohol, marijuana, other drugs). Peer substance use was coded as a dichotomous variable (0 = no, 1= yes; indicated yes on at least one item). To minimize the problem of recall bias in self-report and to better capture childhood maltreatment, this study accounted for early childhood maltreatment using official reports of maltreatment. Early childhood (≤ age 5) maltreatment type was measured using the child’s CPS records from birth to 5 years of age. For each maltreatment type (i.e., physical, sexual, emotional, neglect), no allegations was coded as 0 and at least one allegation was coded as 1.
2.3 Analysis Plan
Preliminary analyses, including univariate descriptive statistics and bivariate correlations, were performed using SPSS v.23. Skewed data were normalized using a log transformation prior to analyses in order to meet structural equation modeling assumptions of multivariate normality with Maximum Likelihood Estimation. Before conducting structural equation modeling, measurement modeling was performed using confirmatory factor analysis (CFA) to examine the appropriateness of the factor structure of the latent variables (i.e., substance use, sexual abuse, neglect). Model fit was evaluated using the following fit indices: Comparative Fit Index (CFI), Root Mean Square Error of Approximation (RMSEA), and Standardized Root Mean Square Residual (SRMR). CFI > .95, RMSEA ≤ .05, and SRMR < .06 (Hu & Bentler, 1999) indicate a good model fit. The measurement model fit the data well, as indicated by a CFI of .986, RMSEA of .040 (90% CI= .030−.050), and SRMR of .024. Structural equation modeling (SEM) was conducted using Mplus version 7.32 to test the direct and indirect effects of child maltreatment on adolescent substance use. The following paths were estimated in the initial model (see Figure 1): (1) direct paths from each maltreatment type to adolescent substance use; (2) pathways from each maltreatment type to four mediators (i.e., PTS symptoms, mother-child relationships, internalizing problems, externalizing problems) to substance use; and (3) paths from PTS symptoms to internalizing and externalizing problems. All endogenous variables were regressed on the control variables. Missing data were handled using full information maximum likelihood (FIML) method. The comparison of study participants with complete data (i.e., no missing data) versus participants missing one or more variables revealed that children who had complete data had greater PTS symptoms, t (868) = 3.111, p = .002. No other significant differences were found between groups with and without missing data. For ease of interpretation, parameter estimates are presented in standardized form.
3. Results
3.1. Sample Characteristics
Table 1 summarizes sample demographics and descriptive statistics for study variables. Participants in this study were 883 adolescents who were age 12 at baseline. Approximately half (49.3%) of the sample was male and a little over half (55.3%) was Black. Neglect was the most prevalent form of maltreatment (67.9%) experienced by adolescents, followed by emotional abuse (40.7%), physical abuse (22.9%), and sexual abuse (15.9%). The score of the quality of the mother-child relationship ranged from 6 to 30, with a mean of 25.11 (SD = 4.97), indicating relatively strong mother-child relationships. Of these mothers, 72.2% were biological mothers, 12% were step or adoptive mothers, 10% were grandmothers, and 2.7% were foster mothers. The mean score of the PTS scale was 41.32 (SD = 8.51), with 3% of adolescents showing clinically elevated levels of PTS symptoms. For internalizing problems, 12.7% of adolescents showed scores in the borderline and 16.8% showed scores in the clinical range (M = 50.15, SD = 11.49). For externalizing problems, 12.2% of adolescents showed scores in the borderline and 18.5% showed scores in the clinical range (M = 54.56, SD = 11.46). In terms of substance use, at age 16, 21.6% of adolescents reported drinking alcohol, 17.4% reported smoking cigarettes, and 15.4% reported using or trying marijuana in the past year. Bivariate correlations between study variables are presented in Table 2.
Table 1.
Descriptive Statistics of Study Variables (N = 883)
| N (%) | M (SD) | |
|---|---|---|
| Past 30-day substance use frequencyc | ||
| Alcohol | 1.55 (1.48) | |
| Cigarette | 1.29 (.78) | |
| Marijuana | 1.29 (.92) | |
| Posttraumatic stress symptomsa | 41.32 (8.51) | |
| Mother-child relationship qualityb | 25.11 (4.97) | |
| Internalizing problemsb | 50.15 (11.49) | |
| Externalizing problemsb | 54.56 (11.46) | |
| Youth self-reports of child maltreatmenta | ||
| Physical abuse | .43 (1.04) | |
| Emotional abuse | 1.23 (2.18) | |
| Sexual abuse | ||
| Non-contact subscale | .13 (.44) | |
| Fondling subscale | .18 (.58) | |
| Oral-genital contact subscale | .05 (.25) | |
| Penetration subscale | .06 (.28) | |
| Neglect | ||
| Physical neglect subscale | 1.06 (2.21) | |
| Emotional support subscale | 3.48 (3.68) | |
| Inadequate supervision subscale | 1.57 (2.29) | |
| Educational neglect subscale | 2.44 (2.24) | |
| CPS reports of child maltreatment (age ≤ 5) | 3.13 (3.90) | |
| Physical abuse | 128 (14.50) | |
| Sexual abuse | 63 (7.2) | |
| Emotional abuse | 44 (5.0) | |
| Neglect | 222 (25.2) | |
| Child’s age | 11.93 (0.53) | |
| Child’s gender (male) | 438 (49.30) | |
| Child’s race (Black) | 488 (55.30) | |
| Annual household income | $20,000 - $24,999* | |
| Family substance usea | 1.27 (1.19) | |
| Peer substance usea | 100 (11.30) |
Note.
Assessed at age 12 years;
Assessed at age 14 years;
Assessed at age 16 years;
median
Table 2.
Correlations among Study Variables (N = 883)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Physical abuse | --- | |||||||||||||||
| 2. Emotional abuse | .55** | --- | ||||||||||||||
| 3. Non-contact SA | .27** | .34** | --- | |||||||||||||
| 4. Fondling | .30** | .36** | .52** | --- | ||||||||||||
| 5. Oral-genital contact | .21** | .18** | .43** | .46** | --- | |||||||||||
| 6. Penetration | .24** | .22** | .45** | .51** | .46** | --- | ||||||||||
| 7. Physical neglect | .24** | .16** | .10** | .09** | .06 | .04 | --- | |||||||||
| 8. Low emotional support | .29** | .29** | .12** | .11** | .04 | .09** | .70** | --- | ||||||||
| 9. Inadequate supervision | .21** | .20** | .12** | .10** | .02 | .07* | .77** | .72** | --- | |||||||
| 10. Educational neglect | .30** | .29** | .09* | .10** | .04 | .02 | .66** | .78** | .66** | --- | ||||||
| 11. PTS | .26** | .23** | .23** | .25** | .19** | .16** | .11** | .08* | .07* | .12** | --- | |||||
| 12. Mother-child relation | −.13** | −.27** | −.08* | −.15** | −.06 | −.08* | −.08* | −.25** | −.12** | −.24** | −.12 | --- | ||||
| 13. Internalizing | .15** | .12** | .12** | .14** | .13** | .12** | .01 | .05 | .06 | .08* | .15** | −.19** | --- | |||
| 14. Externalizing | .14** | .16** | .07 | .11** | .05 | .07 | .01 | .05 | .05 | .06 | .11** | −.25** | .71** | --- | ||
| 15. Alcohol | .01 | .06 | −.01 | .03 | −.02 | −.01 | .01 | .03 | .02 | .10* | .04 | −.13** | .06 | .08* | --- | |
| 16. Cigarette | .07* | .13** | .07* | .10** | .03 | .10** | .04 | .06 | .04 | .08* | .12** | −.17** | .12** | .20** | .48** | --- |
| 17. Marijuana | .01 | .06 | .03 | .04 | −.03 | .01 | .02 | .02 | .05 | .05 | .03 | −.14** | .09** | .13** | .56** | .55** |
Note.
SA = sexual abuse;
p < .05.
p < .01.
3.2 SEM Analysis for Pathways from Child Maltreatment to Adolescent Substance Use
The SEM model (presented in Figure 2) had a good fit, CFI = .957, RMSEA = .036 (90% CI = .031−.040), and SRMR = .043. The model explained 16% of the variance in substance use, 12% of the variance in the mother-child relationship, 10% of the variance in PTS symptoms, 10% of the variance in internalizing behavior, and 10% of the variance in externalizing problems. No maltreatment type was directly associated with adolescent substance use in path analysis, but all four maltreatment types had significant indirect effects on adolescent substance use (see Table 3). This study found two distinctive pathways through which four types of maltreatment influence adolescent substance use: 1) via PTS symptoms (indirect effects: sexual: β = .05, p < .001; physical: β = .03, p = .009) and 2) via mother-child relationships (indirect effects: emotional: β = .02, p = .025; neglect: β = .03, p = .016). Specifically, sexual abuse and physical abuse were each associated with greater PTS symptoms, which in turn, were associated with adolescent substance use. Emotional abuse and neglect were associated with poorer mother-child relationships, which in turn, were related to adolescent substance use. None of the four types of maltreatment had significant indirect effects on substance use via internalizing or externalizing problems. Female sex, Black race, and official report of child physical abuse in childhood (≤ age 5) were associated with increased internalizing and externalizing problems. Peer substance use was associated with higher substance use frequency in adolescence.
Figure 2.
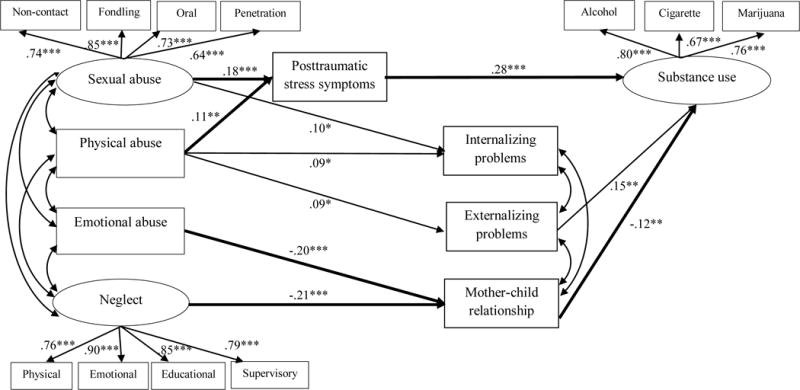
Observed path model of the effects of child maltreatment on adolescent substance use.
Note. Standardized β estimates are presented for significant paths only. Bolded lines indicate significant indirect effects. Standardized β estimates for control variables and non-significant paths are not shown for clarity of the figure.
Model fit: CFI = .957, RMSEA = .036 [90% CI: .031, .040], SRMR = .043
*p<.05, ** p <.01, ***p <.001
Table 3.
Direct and Indirect Effects of Child Maltreatment on Substance Use (N = 883)
| β | 95% CI | |
|---|---|---|
| Sexual Abuse on substance use | ||
| Direct | −.09 | [−.18, .00] |
| Total indirect | .06** | [.02, .09] |
| By posttraumatic stress symptoms (PTS) | .05*** | [.03, .08] |
| By mother-child relationship | .00 | [−.01, .01] |
| By internalizing problems | .00 | [−.01, .01] |
| By externalizing problems | .00 | [−.01, .01] |
| By PTS, internalizing problems | .00 | [.00, .00] |
| By PTS, externalizing problems | .00 | [.00, .00] |
| Physical Abuse on substance use | ||
| Direct | −.06 | [−.15, .02] |
| Total indirect | .05** | [.02, .08] |
| By posttraumatic stress symptoms (PTS) | .03* | [.01, .05] |
| By mother-child relationship | .00 | [−.01, .05] |
| By internalizing problems | .00 | [−.01, .01] |
| By externalizing problems | .02 | [−.01, .03] |
| By PTS, internalizing problems | .00 | [.00, .00] |
| By PTS, externalizing problems | .00 | [.00, .00] |
| Emotional Abuse on substance use | ||
| Direct | .03 | [−.06, .12] |
| Total indirect | .05** | [.02, .09] |
| By posttraumatic stress symptoms (PTS) | .02 | [.00, .04] |
| By mother-child relationship | .02* | [.01, .04] |
| By internalizing problems | .00 | [.00, .00] |
| By externalizing problems | .01 | [−.01, .02] |
| By PTS, internalizing problems | .00 | [.00, .00] |
| By PTS, externalizing problems | .00 | [.00, .00] |
| Neglect on substance use | ||
| Direct | −.03 | [−.11, .05] |
| Total indirect | .03* | [.00, .06] |
| By posttraumatic stress symptoms (PTS) | .00 | [−.01, .03] |
| By mother-child relationship | .03* | [.01, .05] |
| By internalizing problems | .00 | [.00, .00] |
| By externalizing problems | .00 | [−.01, .01] |
| By PTS, internalizing problems | .00 | [.00, .00] |
| By PTS, externalizing problems | .00 | [.00, .00] |
Note. β = standardized coefficient, CI= confidence interval;
p < .05,
p < .01,
p < .001.
4. Discussion
The current study extends previous research by examining PTS symptoms, internalizing problems and externalizing problems, and mother-child relationships as underlying mechanisms of the developmental pathway to adolescent substance use. This study found no direct effects of self-reported maltreatment on adolescent substance use, contrasting with some past cross-sectional research reporting direct relationships between maltreatment and adolescent substance use (Moran et al., 2004; Snyder & Smith, 2015; Wall & Kohl, 2007). The discrepancy in findings may reflect the variation in the timeframe used to assess maltreatment (e.g.., current vs. lifetime; early childhood vs. middle childhood vs. adolescense) as well as differences in study design (i.e., cross sectional vs. longitudinal). In fact, our findings are in line with longitudinal studies that report no direct association between maltreatment and substance use (Cheng & Lo 2011; Faulkner et al., 2014; Kobulsky et al., 2016; Lansford et al., 2010). These findings suggest that substance use in middle adolescence may not be a direct consequence of maltreatment exposure during childhood but rather, a secondary result of more proximate maltreatment sequelae.
Although no significant direct effects were found, all four maltreatment types had significant indirect effects on adolescent substance use. The pathways of PTS symptoms linked physical and sexual abuse to substance use. These findings corroborate past research identifying indirect effects from overall maltreatment, to PTS, to adolescent substance use (Rosenkranz et al., 2014). Consistent with past research (Pelcovitz et al., 1994; Ullman et al., 2009), physical and sexual abuse were related to higher PTS symptoms, which in turn, were related to higher substance use. These findings align with developmental traumatology theory, which purports that events such as physical and sexual abuse that threaten injury, death, or physical harm while causing shock, terror, or helplessness (APA, 2000) disrupt brain regulation, leading to PTS symptoms which in turn, may increase risk for substance use as youth seek to “self-medicate” (DeBellis 2000, 2001).
Further, emotional abuse and neglect were associated with poor mother-child relationship quality, which predicted adolescent substance use. An emotionally abusive and neglectful mother’s unresponsive and non-sensitive parenting may prevent the development of secure and intimate relationships between the mother and the child. Emotional abuse and neglect may be related to poor mother-child relationship quality because emotional abuse and neglect tend to be chronic and occur/ recur more frequently than physical abuse and sexual abuse (DePanfilis & Zuravin, 1999). Alternatively, perpetrators of emotional abuse and neglect may more often be the mothers of the children, making these types of maltreatment particularly detrimental to the mother-child relationship. Our findings of mother-child relationships predicting adolescent substance use are consistent with numerous studies that have indicated that having positive, strong, close relationships with parents serve as a protective factor for adolescent substance use (e.g., Branstetter, Furman, Cottrell, 2009). Adolescents who have poor relationships with their mother may use substances as a coping mechanism to deal with their feelings of isolation (Johnson & Pandina, 1991).
None of the four types of maltreatment had significant indirect effects on substance use via internalizing or externalizing problems. It is possible that the indirect effects of externalizing problems were drowned out by the relatively large and comprehensive list of control variables and mediators included in this study (Walter, 2017). The prominence of PTS over externalizing problems may also be related to developmental timing. PTS were measured during early adolescence (12 years) versus externalizing problems at 14 years. Early adolescence may be a developmentally sensitive period for experiencing these symptoms that put youth at particularly high risk for later substance use. The null findings for internalizing pathways are consistent with prior research that found no indirect effects of maltreatment on substance use via internalizing problems (e.g., Handley et al., 2015; Jones et al., 2013). Internalizing problems such as lack of energy, timid and shy personality, and socially withdrawal may be protective of substance use, counterbalancing other internalizing problems, such as depression and anxiety associated with risk, leading to null results (Tandon, Cardeli, & Luby, 2009). Alternatively, it is possible that caregivers, abusive and neglectful caregivers in particular, failed to detect internalizing problems of their children, given the hidden and unobservable nature of internalizing problems (Tandon et al., 2009). Non-findings for internalizing problems contradict the study by Lewis and colleagues (2011) findings. A likely explanation for this discrepancy is that Lewis and colleagues assessed internalizing problems as a sole mediator.
4.1 Strengths and Limitations
This study has several noteworthy strengths which enhance its contribution to knowledge. First, it used a longitudinal design which enhanced the study’s support for the theoretical temporal sequencing of relationships among study variables. Second, it examined multiple, theoretically-chosen intervening variables simultaneously using SEM, a sophisticated analytic technique. Third, this study used youth self-reported measures of lifetime exposure to child maltreatment. Because of the hidden nature of child maltreatment, many incidents may go undetected by CPS agencies and the rate of child maltreatment is most likely underestimated in official reports (Sedlack et al., 2010). This non-detection can lead to problems of contamination, resulting in underestimated effect sizes in examinations of maltreatment effects (Shenk et al., 2016). Youth self-reports provide more direct access to the child’s experience of maltreatment; in fact, previous studies have suggested that children tend to report higher rates of maltreatment experiences than the rates documented in their CPS case file (Everson et al., 2008; Hambrick, Tunno, Gabrielli, Jackson & Belz, 2014; Knight et al., 2000).
Despite notable strengths, this study has several limitations that warrant caution in interpreting and applying its results. First, this study consisted of adolescents who were at risk of maltreatment; therefore, the findings of the study may not be generalizable to the general population. Developmental paths to adolescent substance use may vary in higher- and lower-risk populations. Second, although this study has the strength of a longitudinal design, reverse or bidirectional relationships are possible. For example, externalizing problems and poor mother-child relationships may result from maltreatment or act as a risk factor for maltreatment (Lansford et al., 2011). Relatedly, this study did not adjust for possible maltreatment between ages 12 and the age of the outcome of interest (substance use at age 16). Although beyond the scope of the current study, the impact of maltreatment on substance use may vary by the developmental stage during which the maltreatment occurred and future research should address the timing of maltreatment and its relation to substance use during adolescence. Third, although this study had the strength of simultaneously examining four types of maltreatment, this study was limited in that it did not account for the interactive effects among multiple subtypes of maltreatment. A growing body of evidence suggests that children are often exposed to different forms of maltreatment rather than to a single form of maltreatment, with co-occurrence rates of multi-type maltreatment ranging from 8% (Price-Robertson, Smart, & Bromfield, 2010) to over 60% (e.g., Arata, Langhinrichsen-Rohling, Bowers, & O’Farrill-Swails, 2005; Sesar, Zivcic-Becirevic, & Sesar, 2008). Although multiple types of childhood maltreatment may co-occur, this study examined the individual types together in order to determine whether each type of maltreatment constructs a distinctive pathway to adolescent substance use. Few studies have examined all four major maltreatment types simultaneously. This analytic approach has been shown to provide valuable information about the unique influence of individual subtype maltreatment variables on their outcomes, after accounting for the effects of other maltreatment subtypes (Petrenko, Friend, Garrido, Taussig, & Culhane, 2012). Future research should consider multiple maltreatment characteristics, such as maltreatment co-occurrence, severity, and timing when examining pathways to adolescent substance use. Fourth, the findings should be interpreted with caution because approximately 35% of the sample dropped out of the study and the results may be biased by attrition. Relatedly, the variances of mediating and outcome variables explained by the model were relatively small; therefore, the findings need to be replicated and further verified in future research. Finally, our outcome was restricted to three types of substances: alcohol, tobacco, and marijuana. Future research should examine how developmental paths to substance use may differ for other substances (e.g., hard drugs) or substance use outcomes (e.g., substance use disorder, polysubstance use).
4.2 Practice Implications
This study adds to the existing literature by identifying multiple pathways through which different types of child maltreatment influence adolescent substance use. Targeted interventions addressing posttraumatic stress symptoms and enhancing the quality of the mother-child relationship may be effective in preventing adolescent substance use and promoting healthy youth development among adolescents with child maltreatment histories. In particular, children exposed to emotional abuse and neglect may benefit from interventions focused on improving the mother-child relationship, such as communication coaching and therapeutic, mutually enjoyable activities aimed to improve the mother-child bond. In addition to strengthening the parent-child relationship, maternal coaching on effective child supervision and communication may be beneficial in curtailing substance use in adolescence. Maltreatedd children, particularly those exposed to sexual and physical abuse, may also benefit from individual, trauma-informed therapies to address PTS symptoms in order to prevent substance use. Therapies may include assistance in coping with PTS symptoms, with a specific focus on healthy alternatives to substance use, and psychotropic medication to help reduce PTS symptoms.
Acknowledgments
This document includes data from the Consortium of Longitudinal Studies of Child Abuse and Neglect (LONGSCAN), which was funded by the Office on Child Abuse and Neglect (OCAN), Children's Bureau, Administration for Children and Families, Dept. of Health and Human Services (The National Center on Child Abuse and Neglect (NCCAN)). The data were made available by the National Data Archive on Child Abuse and Neglect, Cornell University, Ithaca, NY, and have been used with permission. The collector of the original data, the funder, NDACAN, Cornell University and their agents or employees bear no responsibility for the analyses or interpretations presented here.
This research was funded by the Ohio State University Institute for Population Research through a grant from the Eunice Kennedy Shriver NICHD of NIH, P2CHD058484. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver NICHD or the NIH.
References
- Achenbach TM. Manual for the child behavior Checklist/4-18 and 1991 profile. Department of Psychiatry, University of Vermont; Burlington, VT: 1991. [Google Scholar]
- American Psychiatric Association, & American Psychiatric Association. DSM-IV-TR: Diagnostic and statistical manual of mental disorders, text revision. Washington, DC: American Psychiatric Association; 2000. p. 75. [Google Scholar]
- Anthony JC, Petronis KR. Early-onset drug use and risk of later drug problems. Drug and Alcohol Dependence. 1995;40(1):9–15. doi: 10.1016/0376-8716(95)01194-3. [DOI] [PubMed] [Google Scholar]
- Arata CM, Langhinrichsen-Rohling J, Bowers D, O'Farrill-Swails L. Single versus multi-type maltreatment: An examination of the long-term effects of child abuse. Journal of Aggression, Maltreatment & Trauma. 2005;11(4):29–52. [Google Scholar]
- Bailey JA, McCloskey LA. Pathways to adolescent substance use among sexually abused girls. Journal of Abnormal Child Psychology. 2005;33(1):39–53. doi: 10.1007/s10802-005-0933-0. [DOI] [PubMed] [Google Scholar]
- Bava S, Tapert SF. Adolescent brain development and the risk for alcohol and other drug problems. Neuropsychology Review. 2010;20(4):398–413. doi: 10.1007/s11065-010-9146-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss: vol. 1. Attachment. New York: Basic Books; 1969. [Google Scholar]
- Braciszewski JM, Stout RL. Substance use among current and former foster youth: A systematic review. Children and Youth Services Review. 2012;34(12):2337–2344. doi: 10.1016/j.childyouth.2012.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branstetter SA, Furman W, Cottrell L. The influence of representations of attachment, maternal–adolescent relationship quality, and maternal monitoring on adolescent substance use: a 2‐Year Longitudinal Examination. Child Development. 2009;80(5):1448–1462. doi: 10.1111/j.1467-8624.2009.01344.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briere J. Trauma symptom checklist for children. Odessa, FL: Psychological Assessment Resources; 1996. [Google Scholar]
- Casanueva C, Stambaugh L, Urato M, Fraser JG, Williams J. Illicit drug use from adolescence to young adulthood among child welfare-involved youths. Journal of Child and Adolescent Substance Use. 2014;23:29–48. [Google Scholar]
- Cheng TC, Lo CC. A longitudinal analysis of some risk and protective factors in marijuana use by adolescents receiving child welfare services. Children and Youth Services Review. 2011;33(9):1667–1672. [Google Scholar]
- Crittenden PM, Ainsworth MD. Child maltreatment and attachment theory. In: DF, Carlson V, editors. Child maltreatment: Theory and research on the causes and consequences of child abuse and neglect. London, England: Cambridge University Press; 1989. pp. 432–463. [Google Scholar]
- Cooper ML, Shaver PR, Collins NL. Attachment styles, emotion regulation, and adjustment in adolescence. Journal of Personality and Social Psychology. 1998;74(5):1380–1397. doi: 10.1037//0022-3514.74.5.1380. [DOI] [PubMed] [Google Scholar]
- Danzo S, Connell AM, Stormshak EA. Associations between alcohol-use and depression symptoms in adolescence: Examining gender differences and pathways over time. Journal of Adolescence. 2017;56:64–74. doi: 10.1016/j.adolescence.2017.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bellis MD, Clark DB, Beers SR, Soloff PH, Boring AM, Hall J, Keshavan MS. Hippocampal volume in adolescent-onset alcohol use disorders. American Journal of Psychiatry. 2000;157(5):737–744. doi: 10.1176/appi.ajp.157.5.737. [DOI] [PubMed] [Google Scholar]
- De Bellis MD. Developmental traumatology: The psychobiological development of maltreated children and its implications for research, treatment, and policy. Development and Psychopathology. 2001;13(3):539–564. doi: 10.1017/s0954579401003078. [DOI] [PubMed] [Google Scholar]
- De Bellis MD. Developmental traumatology: A contributory mechanism for alcohol and substance use disorders. Psychoneuroendocrinology. 2002;27(1):155–170. doi: 10.1016/s0306-4530(01)00042-7. [DOI] [PubMed] [Google Scholar]
- DePanfilis D, Zuravin SJ. Epidemiology of child maltreatment recurrences. Social Service Review. 1999;73(2):218–239. [Google Scholar]
- Dube SR, Miller JW, Brown DW, Giles WH, Felitti VJ, Dong M, Anda RF. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. Journal of Adolescent Health. 2006;38(4):444.e1–444.e10. doi: 10.1016/j.jadohealth.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Dubowitz H, Kim J, Black MM, Weisbart C, Semiatin J, Magder LS. Identifying children at high risk for a child maltreatment report. Child Abuse & Neglect. 2011;35(2):96–104. doi: 10.1016/j.chiabu.2010.09.003. [DOI] [PubMed] [Google Scholar]
- Everson MD, Smith JB, Hussey JM, English D, Litrownik AJ, Dubowitz H, Runyan DK. Concordance between adolescent reports of childhood abuse and child protective service determinations in an at-risk sample of young adolescents. Child Maltreatment. 2008;13(1):14–26. doi: 10.1177/1077559507307837. [DOI] [PubMed] [Google Scholar]
- Faulkner B, Goldstein AL, Wekerle C. Pathways from childhood maltreatment to emerging adulthood: Investigating trauma-mediated substance use and dating violence outcomes among child protective services-involved youth. Child Maltreatment. 2014;19(3–4):219–232. doi: 10.1177/1077559514551944. [DOI] [PubMed] [Google Scholar]
- Foshee V, Bauman KE. Parental attachment and adolescent cigarette smoking initiation. Journal of Adolescent Research. 1994;9(1):88–104. [Google Scholar]
- Goldstein AL, Wekerle C, Tonmyr L, Thornton T, Waechter R, Pereira J, MAP Research Team. The relationship between post-traumatic stress symptoms and substance use among adolescents involved with child welfare: Implications for emerging adulthood. International Journal of Mental Health and Addiction. 2011;9(5):507–524. [Google Scholar]
- Guo J, Chung IJ, Hill KG, Hawkins JD, Catalano RF, Abbott RD. Developmental relationships between adolescent substance use and risky sexual behavior in young adulthood. Journal of Adolescent Health. 2002;31(4):354–362. doi: 10.1016/s1054-139x(02)00402-0. [DOI] [PubMed] [Google Scholar]
- Hambrick EP, Tunno AM, Gabrielli J, Jackson Y, Belz C. Using multiple informants to assess child maltreatment: concordance between case file and youth self-report. Journal of Aggression, Maltreatment, & Trauma. 2014;23(7):751–771. doi: 10.1080/10926771.2014.933463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handley ED, Rogosch FA, Guild DJ, Cicchetti D. Neighborhood disadvantage and adolescent substance use disorder: The moderating role of maltreatment. Child Maltreatment. 2015;20(3):193–202. doi: 10.1177/1077559515584159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison PA, Fulkerson JA, Beebe TJ. Multiple substance use among adolescent physical and sexual abuse victims. Child Abuse & Neglect. 1997;21(6):529–539. doi: 10.1016/s0145-2134(97)00013-6. [DOI] [PubMed] [Google Scholar]
- Highland KB, Herschl LC, Klanecky A, McChargue DE. Biopsychosocial pathways to Alcohol‐Related problems. The American Journal on Addictions. 2013;22(4):366–372. doi: 10.1111/j.1521-0391.2013.12012.x. [DOI] [PubMed] [Google Scholar]
- Hovdestad WE, Tonmyr L, Wekerle C, Thornton T. Why is childhood maltreatment associated with adolescent substance abuse? A critical review of explanatory models. International Journal of Mental Health and Addiction. 2011;9(5):525. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- Hussey JM, Chang JJ, Kotch JB. Child maltreatment in the United States: prevalence, risk factors, and adolescent health consequences. Pediatrics. 2006;118(3):933–942. doi: 10.1542/peds.2005-2452. [DOI] [PubMed] [Google Scholar]
- Johnson V, Pandina RJ. Effects of the family environment on adolescent substance use, delinquency, and coping styles. The American Journal of Drug and Alcohol Abuse. 1991;17(1):71–88. doi: 10.3109/00952999108992811. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the future national survey results on drug use, 1975–2015: Overview, key findings on adolescent drug use. Ann Arbor, MI: Institute for Social Research; 2016. [Google Scholar]
- Jones DJ, Lewis T, Litrownick A, Thompson R, Proctor LJ, Isbell T, Runyun D. Linking sexual abuse and early adolescent risk behavior: The intervening role of internalizing and externalizing problems. Journal of Abnormal Child Psychology. 2013;41(1):139–150. doi: 10.1007/s10802-012-9656-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight ED, Runyan DK, Dubowitz H, Brandford C, Kotch J, Litrownik A, Hunter W. Methodological and ethical challenges associated with child self-report of maltreatment solutions implemented by the LONGSCAN consortium. Journal of Interpersonal Violence. 2000;15(7):760–775. [Google Scholar]
- Knight ED, Smith JS, Martin L, Lewis T, the LONGSCAN Investigators Measures for Assessment of Functioning and Outcomes in Longitudinal Research on Child Abuse Volume 3: Early Adolescence (Ages 12-14) 2010 Retreived from the LONGSCAN web site: http://www.iprc.unc.edu/longscan/
- Kobulsky JM, Holmes MR, Yoon S, Perzynski AT. Physical abuse after child protective services investigation and adolescent substance use. Children and Youth Services Review. 2016;71:36–44. [Google Scholar]
- Kuntsche EN, Silbereisen RK. Parental closeness and adolescent substance use in single and two-parent families in Switzerland. Swiss Journal of Psychology. 1996;63(2):85–92. [Google Scholar]
- Lansford JE, Criss MM, Laird RD, Shaw DS, Pettit GS, Bates JE, Dodge KA. Reciprocal relations between parents' physical discipline and children's externalizing behavior during middle childhood and adolescence. Development and Psychopathology. 2011;23(1):225–238. doi: 10.1017/S0954579410000751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansford JE, Dodge KA, Pettit GS, Bates JE. Does physical abuse in early childhood predict substance use in adolescence and early adulthood? Child Maltreatment. 2010;15(2):190–194. doi: 10.1177/1077559509352359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larrabee HM, Lewis T. Longitudinal studies of child abuse and neglect (LONGSCAN) Assessments 0–18: User’s Guide. Ithaca, NY: National Data Archive on Child Abuse and Neglect, Cornell University; 2014. [Google Scholar]
- Ledoux S, Miller P, Choquet M, Plant M. Family structure, parent–child relationships, and alcohol and other drug use among teenagers in France and the United Kingdom. Alcohol and Alcoholism. 2002;37(1):52–60. doi: 10.1093/alcalc/37.1.52. [DOI] [PubMed] [Google Scholar]
- Lewis TL, Kotch J, Wiley TRA, Litrownik AJ, English DJ, Thompson R, Dubowitz H. Internalizing problems: A potential pathway from child maltreatment to adolescent smoking. Journal of Adolescent Health. 2011;48(3):247–252. doi: 10.1016/j.jadohealth.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall EJ. Adolescent alcohol use: risks and consequences. Alcohol and Alcoholism. 2014;49(2):160–164. doi: 10.1093/alcalc/agt180. [DOI] [PubMed] [Google Scholar]
- Moran PB, Vuchinich S, Hall NK. Associations between types of maltreatment and substance us during adolescence. Child Abuse and Neglect. 2004;28(5):565–574. doi: 10.1016/j.chiabu.2003.12.002. [DOI] [PubMed] [Google Scholar]
- Moss HB, Chen CM, Yi H. Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug and Alcohol Dependence. 2014;136:51–62. doi: 10.1016/j.drugalcdep.2013.12.011. [DOI] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9(11):e1001349. doi: 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, Coffey C, Lynskey MT, Reid S, Hemphill S, Carlin JB, Hall W. Trajectories of adolescent alcohol and cannabis use into young adulthood. Addiction. 2007;102(4):607–615. doi: 10.1111/j.1360-0443.2006.01728.x. [DOI] [PubMed] [Google Scholar]
- Pelcovitz D, Kaplan S, Goldenberg B, Mandel F, Lehane J, Guarrera J. Post-traumatic stress disorder in physically abused adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33(3):305–312. doi: 10.1097/00004583-199403000-00002. [DOI] [PubMed] [Google Scholar]
- Petrenko CL, Friend A, Garrido EF, Taussig HN, Culhane SE. Does subtype matter? Assessing the effects of maltreatment on functioning in preadolescent youth in out-of-home care. Child Abuse & Neglect. 2012;36(9):633–644. doi: 10.1016/j.chiabu.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price-Robertson R, Smart D, Bromfield L. Family is for life connections between childhood family experiences and wellbeing in early adulthood. Family Matters. 2010;(85):7. [Google Scholar]
- Reinert DF, Edwards CE. Childhood physical and verbal mistreatment, psychological symptoms, and substance use: sex differences and the moderating role of attachment. Journal of Family Violence. 2009;24(8):589–596. [Google Scholar]
- Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, Ireland M. Protecting adolescents from harm: findings from the national longitudinal study on adolescent health. JAMA. 1997;278(10):823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- Rogosch FA, Oshri A, Cicchetti D. From child maltreatment to adolescent cannabis abuse and dependence: A developmental cascade model. Development and Psychopathology. 2010;22(04):883–897. doi: 10.1017/S0954579410000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenkranz SE, Muller RT, Henderson JL. The role of complex PTSD in mediating childhood maltreatment and substance abuse severity among youth seeking substance abuse treatment. Psychological Trauma: Theory, Research, Practice, and Policy. 2014;6(1):25–33. [Google Scholar]
- Sedlak AJ, Mettenburg J, Basena M, Peta I, McPherson K, Greene A. Fourth national incidence study of child abuse and neglect (NIS-4) Washington, DC: US Department of Health and Human Services; 2010. [Google Scholar]
- Sesar K, Zivcic-Becirevic I, Sesar D. Multi-type maltreatment in childhood and psychological adjustment in adolescence: Questionnaire study among adolescents in Western Herzegovina Canton. Croatian Medical Journal. 2008;49(2):243–256. doi: 10.3325/cmj.2008.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shenk CE, Noll JG, Peugh JL, Griffin AM, Bensman HE. Contamination in the prospective study of child maltreatment and female adolescent health. Journal of Pediatric Psychology. 2016;41(1):37–45. doi: 10.1093/jpepsy/jsv017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin SH. A Longitudinal Examination of the Relationships between Childhood Maltreatment and Patterns of Adolescent Substance Use among High‐Risk Adolescents. The American Journal on Addictions. 2012;21(5):453–461. doi: 10.1111/j.1521-0391.2012.00255.x. [DOI] [PubMed] [Google Scholar]
- Shin SH, Miller DP, Teicher MH. Exposure to childhood neglect and physical abuse and developmental trajectories of heavy episodic drinking from early adolescence into young adulthood. Drug and Alcohol Dependence. 2013;127(1):31–38. doi: 10.1016/j.drugalcdep.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silins E, Horwood LJ, Patton GC, Fergusson DM, Olsson CA, Hutchinson DM, Coffey C. Young adult sequelae of adolescent cannabis use: an integrative analysis. The Lancet Psychiatry. 2014;1(4):286–293. doi: 10.1016/S2215-0366(14)70307-4. [DOI] [PubMed] [Google Scholar]
- Snyder SM, Smith RE. Do physical abuse, depression, and parental substance use influence patterns of substance use among child welfare involved youth? Substance Use & Misuse. 2015;50(2):226–235. doi: 10.3109/10826084.2014.966845. [DOI] [PubMed] [Google Scholar]
- Sroufe LA. The coherence of individual development: early care, attachment, and subsequent developmental issues. American Psychologist. 1979;34(10):834–841. [Google Scholar]
- Sroufe LA, Rutter M. The domain of developmental psychopathology. Child Development. 1984;55:17–29. [PubMed] [Google Scholar]
- Straus MA, Kinard EM, Williams LM. The multidimensional neglectful behavior scale, Form A: Adolescent and adult-recall version. Durham, NH: University of New Hapshire: Family Research Laboratory; 1995. [Google Scholar]
- Stronach EP, Toth SL, Rogosch F, Oshri A, Manly JT, Cicchetti D. Child maltreatment, attachment security, and internal representations of mother and mother-child relationships. Child Maltreatment. 2011;16(2):137–145. doi: 10.1177/1077559511398294. [DOI] [PubMed] [Google Scholar]
- Squeglia LM, Jacobus J, Tapert SF. The influence of substance use on adolescent brain development. Clinical EEG and Neuroscience. 2009;40(1):31–38. doi: 10.1177/155005940904000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandon M, Cardeli E, Luby J. Internalizing disorders in early childhood: A review of depressive and anxiety disorders. Child and Adolescent Psychiatric Clinics of North America. 2009;18(3):593–610. doi: 10.1016/j.chc.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonmyr L, Thornton T, Draca J, Wekerle C. A review of childhood maltreatment and adolescent substance use relationship. Current Psychiatry Reviews. 2010;6(3):223–234. [Google Scholar]
- Traube DE, James S, Zhang J, Landsverk J. A national study of risk and protective factors for substance use among youth in the child welfare system. Addictive Behaviors. 2012;37(5):641–650. doi: 10.1016/j.addbeh.2012.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE, Najdowski CJ, Filipas HH. Child sexual abuse, post-traumatic stress disorder, and substance use: Predictors of revictimization in adult sexual assault survivors. Journal of Child Sexual Abuse. 2009;18(4):367–385. doi: 10.1080/10538710903035263. [DOI] [PubMed] [Google Scholar]
- Wall AE, Kohl PL. Substance use in maltreated youth: findings from the national survey of child and adolescent well-being. Child Maltreatment. 2007;12(1):20–30. doi: 10.1177/1077559506296316. [DOI] [PubMed] [Google Scholar]
- Zhang L, Welte JW, Wieczorek WF. The influence of parental drinking and closeness on adolescent drinking. Journal of Studies on Alcohol. 1999;60(2):245–251. doi: 10.15288/jsa.1999.60.245. [DOI] [PubMed] [Google Scholar]


