Abstract
Purpose of review
Thioredoxin-interacting protein (TXNIP) has emerged as a major factor regulating pancreatic beta cell dysfunction and death, key processes in the pathogenesis of type 1 and type 2 diabetes. Accumulating evidence based on basic, pre-clinical and retrospective epidemiological research suggests that TXNIP represents a promising therapeutic target for diabetes. The present review is aimed at providing an update regarding these developments.
Recent findings
TXNIP has been shown to be induced by glucose and increased in diabetes and to promote beta cell apoptosis, whereas TXNIP deletion protected against diabetes. More recently, TXNIP inhibition has also been found to promote insulin production and glucagon-like peptide 1 signaling via regulation of a microRNA. Beta cell TXNIP expression itself was found to be regulated by hypoglycemic agents, carbohydrate-response-element-binding protein and cytosolic calcium or the calcium channel blocker, verapamil. Retrospective studies now further suggest that verapamil use might be associated with a lower incidence of type 2 diabetes in humans.
Summary
TXNIP has emerged as a key factor in the regulation of functional beta cell mass and TXNIP inhibition has shown beneficial effects in a variety of studies. Thus, the inhibition of TXNIP may provide a novel approach to the treatment of diabetes.
Keywords: TXNIP, diabetes, functional beta cell mass, therapeutic target, microRNA
Introduction
Loss of functional beta cell mass is a hallmark of both type 1 and type 2 diabetes (1-6). Thus, an attractive treatment for diabetes would be to promote functional beta cell mass by decreasing the elevated levels of beta cell apoptosis associated with this disease. A promising target that has recently emerged in this area of research is thioredoxin-interacting protein (TXNIP) (7, 8). In this review, we discuss the physiological role of TXNIP and recent studies regarding the impact of TXNIP on beta cell biology and as a therapeutic target in diabetes.
Physiological Role and Regulation of TXNIP
In 1994, the gene encoding what is most commonly known as TXNIP was first cloned from HL-60 cells stimulated with 1,25-dihydroxyvitamin D-3, thus earning it the name Vitamin-D upregulated protein 1 (VDUP1) (9-11). However, subsequent TXNIP promoter analysis did not uncover a consensus vitamin D response element (10) and vitamin D-induced TXNIP transcription has not been shown in other cell types. Currently, TXNIP is most commonly known as a 50kDa ubiquitously expressed protein that is highly conserved across species (10) and plays a vital role in regulating cellular redox status through binding and negatively regulating thioredoxin (Trx) (11-15). Because of its ability to act as a cellular redox regulator, TXNIP has been thought to be localized in the cytoplasm (13, 16, 17); although, it has been shown that TXNIP can translocate between cellular compartments (18).
In 2002, TXNIP was identified in human pancreatic islets as the highest glucose-induced gene in a gene expression microarray (19). TXNIP’s upregulation by glucose was later confirmed by quantitative real-time RT-PCR as well as immunoblotting in both INS-1 beta cells and primary human islets (20-22). This glucose-induced TXNIP response was found to be mediated by a cis-acting element consisting of a well-conserved E-box repeat contained in the TXNIP promoter and carbohydrate response element-binding protein (ChREBP) was identified as the trans-acting factor (20). In response to glucose, ChREBP becomes dephosphorylated allowing it to translocate from the cytosol into the nucleus and bind to this E-box repeat (23). Furthermore, TXNIP is able to stimulate its own expression via a positive feedback loop involving activation of ChREBP (24). Moreover, type 1 diabetes associated inflammatory cytokines also promote beta cell TXNIP expression primarily via ChREBP (25). On the other hand, mammalian target of rapamycin (mTOR) has recently been observed to decrease TXNIP by regulating ChREBP expression (26). While ChREBP is predominantly expressed in beta cells (23), liver (27, 28), and adipose tissue (28, 29), its paralog, MondoA, is predominantly expressed and responsible for TXNIP induction in skeletal muscle and heart (30). Interestingly, this year TXNIP was also identified by genome-wide gene expression profiling in skeletal muscle to be downregulated by exercise, an effect that seems to be mediated by hypoxia-inducible factor 1a (31).
High glucose has been observed to confer beta cell dysfunction and apoptosis, and TXNIP plays a pivotal role in mediating these detrimental effects of glucose toxicity primarily via the mitochondrial death pathway (18). In fact, TXNIP was found to translocate to the mitochondria, where it competes with ASK1 (apoptosis signaling-regulating kinase 1) for binding of Trx2. The subsequent release and activation of ASK1 initiates a downstream apoptotic cascade, thus leading to the death of the beta cell (18). TXNIP has also been found to lead to NLRP3 inflammasome activation, resulting in caspase-1 activation and IL-1beta production (32, 33). IL-1beta, in turn, has been shown to play an important role in the pathogenesis of both type 1 and type 2 diabetes (32-35). While initially thought to be produced in the beta cell (36), NLRP3 expression and IL-1beta production are primarily observed in innate immune cells (37-39). It is conceivable though that TXNIP-induced IL-1beta production and inflammasome activation is present in resident macrophages of the intact islet, but it is less likely this event is taking place in the beta cells themselves.
Recently, additional TXNIP-dependent mechanisms of beta cell dysfunction and death have been identified, several of which have been linked to microRNAs. Insulin production was shown to be downregulated by TXNIP as TXNIP induces expression of miR-204, which in turn targets and decreases expression of MafA, the main insulin transcription factor (40). Most recently, miR-204 has also been discovered to target and downregulate glucagon-like peptide 1 receptor (GLP1R) expression and by doing so to inhibit GLP-1 agonist mediated insulin secretion (41). Islet amyloid polypeptide, which promotes beta cell inflammation and toxicity and is found in type 2 diabetic islets (42-44), is upregulated by TXNIP through miR-124a and FoxA2 (45). Also, TXNIP has been shown to increase miR-200 leading to beta cell apoptosis (46). On the other hand, TXNIP is a target of miR-17. Activation of inositol-requiring enzyme 1a (IRE1a) in the context of endoplasmic reticulum (ER) stress and unfolded protein response leads to destabilization of miR-17, which results in upregulation of TXNIP (32). In non-beta cells, similar effects have been observed with miR-20a, a member of the miR-17-92 cluster (47).
Beta cell TXNIP expression is increased in diabetes (20, 40, 48-50) and overexpression of TXNIP has been shown to result in apoptosis, especially in beta cells (20, 51), which is consistent with their particular susceptibility to oxidative stress (52). Elevated TXNIP levels are therefore thought to be an important factor in the pathogenesis of diabetic beta cell loss and the development of diabetic complications. Indeed, mutation or genetic deletion of TXNIP has been shown to prevent diabetes in a variety of mouse models including type 1 and type 2 diabetes (49). TXNIP-deficient HcB-19 mice as well as beta cell-specific TXNIP knockout mice have increased beta cell mass, decreased beta cell apoptosis, elevated insulin levels, and are protected against STZ-induced diabetes (49). In addition, beta cell-specific overexpression of thioredoxin in non-obese diabetic (NOD) mice has also been shown to protect against autoimmune diabetes (53). TXNIP deletion has also been observed to reduce beta cell apoptosis and diabetes in Akita mice, whose diabetes is due to insulin misfolding and ER-stress (32). Even in the stringent, leptin-deficient type 2 diabetic BTBRob/ob mouse model, characterized by severe obesity, insulin resistance and hyperglycemia (54), TXNIP deficiency led to a decrease in beta cell apoptosis, increase in beta cell mass and protection against diabetes (49).
Given these beneficial effects of TXNIP deletion and the many detrimental effects associated with elevated TXNIP, the question arises as to what the physiological role of this protein might be and why we even express it. However, in prehistoric times TXNIP may have provided an evolutionary advantage by contributing to the host’s protective shield. TXNIP-induced oxidative stress could be viewed as a protective cellular defense mechanism against microbes and keeping beta cell mass and insulin production in check would be beneficial during periods of food scarcity and famine to prevent hypoglycemia and assure survival. Consistent with this notion, TXNIP deficient mice are more sensitive to starvation (55). Also, TXNIP has been found to be upregulated in multiple tissues during torpor and prolonged fasting and plays an important role in fuel partitioning and regulation of energy expenditure especially in the hypometabolic state (56-59). In contrast, in more recent times of excess energy- and glucose-rich foods and sedentary life-style, TXNIP expression may easily surpass the very low, if at all present, need for TXNIP under these conditions and start contributing to the metabolic risk and the development of diabetes by promoting beta cell dysfunction and impairing glucose homeostasis. On the other hand, having recognized at least some of the implications that elevated TXNIP has for the pathogenesis of diabetes, may allow us to use TXNIP as a novel drug target for diabetes going forward (Figure 1).
Fig. 1.
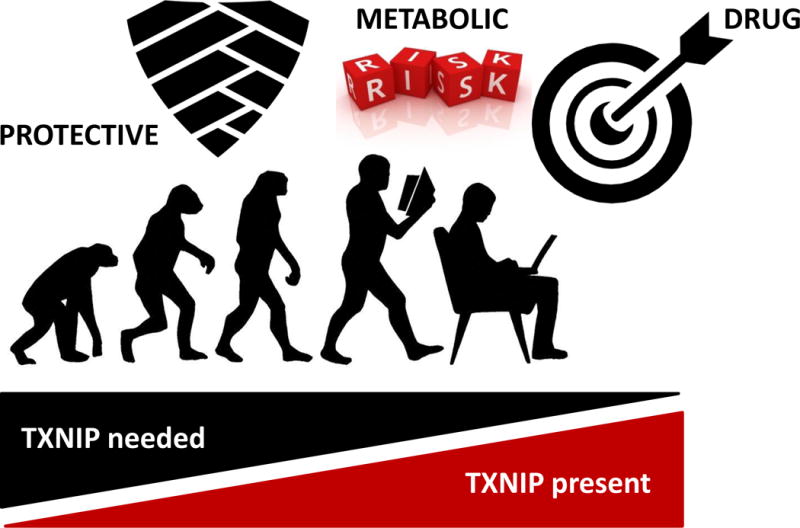
Schematic of the predicted changes in the role of TXNIP over time.
Pharmacological Regulation of TXNIP
A number of hypoglycemic agents have been shown to decrease TXNIP. In fact, insulin has been reported to decrease TXNIP mRNA and protein levels in vitro (50); although, hyperglycemia seems to supersede insulin’s effect on TXNIP in beta cells, as TXNIP continues to remain elevated in diabetes even in the context of in vivo hyperinsulinemia (48, 49). The biguanide metformin, a first-line oral agent to treat type 2 diabetes, has been shown to decrease glucose-induced TXNIP mRNA and protein levels in beta cells through its ability to activate AMPK (60, 61). Furthermore, it has been shown in various cell types that metformin decreases glucose-induced nuclear entry and binding of the TXNIP transcription factor ChREBP (or its paralog MondoA) to the TXNIP promoter, which is thought to be at least partially due to the effects of metformin on AMPK activation (60, 62).
Very recent work has shown that TXNIP downregulation promotes GLP1R signaling in the beta cell (41). Furthermore, GLP-1 agonists, such as exendin-4, have been shown to reduce TXNIP levels and protect against beta cell death (63, 64). Exendin-4 activates cAMP signaling, as well as protein kinase A, resulting in TXNIP ubiquitination and proteasomal degradation (64). This reduction of TXNIP results in decreased susceptibility of beta cells to glucotoxicity (64). Dipeptidyl-4 inhibitors, such as sitagliptin have also recently been reported to decrease cytokine-induced TXNIP and caspase 3/7 activity in INS-1E cells by preserving sarco-endoplasmic reticulum calcium ATPase (SERCA) activity and decreasing cytosolic calcium levels (65).
Interestingly, TXNIP had previously been found to be downregulated in response to a decrease in cytosolic calcium levels and by calcium channel blockers such as the widely used blood pressure medication, verapamil (66). These effects were not agent or class specific, were not restricted to L-type calcium channel blockers such as verapamil, and could be mimicked by calcium chelators. As such, verapamil is believed to decrease beta cell TXNIP expression by reducing cytosolic calcium, which in turn controls calcineurin/calcium-dependent protein phosphatase 2B signaling and leads to increased phosphorylation and nuclear exclusion of ChREBP and results in decreased ChREBP mediated TXNIP transcription. Indeed, the calcineurin inhibitor, cyclosporine A effectively mimicked the effects of verapamil on TXNIP transcription and ChREBP nuclear exclusion. In vivo, verapamil was found to not only prevent multiple low-dose STZ-induced diabetes, but also to rescue overtly diabetic mice by decreasing beta cell apoptosis, increasing beta cell mass and elevating insulin levels. Similar effects were also observed when verapamil was administered to BTBRob/ob mice as a model of type 2 diabetes (66).
While these findings raised the question as to why such beneficial effects of calcium channel blockers had not been described in diabetic patients before, it is important to remember that for antihypertensive medications, the primary and secondary outcomes monitored are most commonly mortality and cardiovascular complications, not metabolic regulation or diabetes. However, several intriguing retrospective epidemiological findings have recently emerged. The International Verapamil SR-Trandolapril Study (INVEST) trial found that participants in the verapamil arm had a lower risk of developing diabetes (67, 68). In an association study using the Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort, it was further revealed that diabetic verapamil users had fasting blood glucose levels that were up to 37mg/dL lower as compared to diabetic subjects not on calcium channel blockers (69). Most recently, using Taiwan’s National Health Insurance Research Database, it was observed that verapamil use was associated with reduced incidence of newly diagnosed type 2 diabetes especially in patients older than 65 years (70). While these observations combined with all the pre-clinical data make it tempting to speculate that verapamil may also have beneficial effects in human diabetes, only the results of properly controlled prospective studies such as the currently ongoing randomized double-blind placebo controlled phase II trial in type 1 diabetic patients will be able to determine whether verapamil also promotes functional beta cell mass and has protective effects in human diabetes. If so, this obviously would provide a completely novel, yet easily translatable and cost-effective additional approach to diabetes management.
Considerations of Targeting TXNIP as a Novel Approach to Diabetes
While verapamil provides a realistic investigational possibility for in vivo TXNIP inhibition as it is already FDA approved as an antihypertensive medication, this also might limit its use in some diabetic patient populations, such as children and adult subjects with severe ventricular dysfunction or hypotension. Also, the possibility of potential adverse effects due to inhibition of a ubiquitously expressed pro-apoptotic protein has to be considered. However, TXNIP inhibition has been shown to have beneficial effects beyond the beta cell including various extrapancreatic tissues (71-74), such as the cardiovascular system (75-80), kidney (81, 82), and retina (83, 84), making a beta cell-specific approach unnecessary and even undesirable. Furthermore, while complete whole body TXNIP deficiency has been associated with an elevated risk later in life of developing hepatocellular carcinomas in the HcB-19 mice (85), it does not seem to lead to other malignancies typically associated with inhibition of a pro-apoptotic tumor-suppressor gene such as lymphomas or leukemias. Importantly, since the goal of any pharmacological TXNIP inhibition is to normalize pathologically elevated TXNIP levels back to physiological levels, side effects from low TXNIP expression would be extremely unlikely. The most recent findings that TXNIP and/or miR-204 inhibition can specifically induce expression of GLP1R in the beta cell also raises the intriguing possibility that TXNIP inhibition could be used in combination with GLP-1 agonists to amplify their desired effects on the beta cell, reduce the necessary dose and thereby possibly avoid some of the common dose-dependent GLP-1 side effects.
Conclusion
The emergence of TXNIP as a viable therapeutic target to promote functional beta cell mass has been strongly supported by numerous studies showing its impact on beta cell biology and diabetes development. TXNIP is rapidly induced by glucose, is elevated in diabetes, and results in beta cell apoptosis, whereas normalizing TXNIP to basal levels reverses these deleterious effects. Much about TXNIP biology has been learned over the last 15 years since it was found to be induced by glucose in human pancreatic islets. TXNIP has gone from a hit in an oligonucleotide gene expression microarray, to being a recognized factor linking glucotoxicty and beta cell apoptosis, preventing and reversing diabetes in mice, regulating insulin production and secretion via microRNAs, and serving as the therapeutic target in a phase II diabetes trial. Together, these recent advances have positioned TXNIP as an exciting and promising candidate for diabetes drug discovery and development.
Key Points.
TXNIP expression is induced by glucose and TXNIP levels are pathologically elevated in diabetes.
TXNIP downregulation has beneficial effects on functional beta cell mass as well as on extrapancreatic tissues in the context of diabetes.
Multiple TXNIP-dependent mechanisms of beta cell dysfunction and death are mediated by microRNAs.
TXNIP inhibition has emerged as a viable therapeutic target for promoting functional beta cell mass in humans and is currently being evaluated in pre-clinical and clinical trials.
Acknowledgments
None.
Financial support and sponsorship
A.S. is supported by grants from the National Institutes of Health (R01DK078752, UC4DK104204) and JDRF (3-SRA-2014-302-M-R).
Footnotes
Conflicts of interest
There are no conflicts of interest.
References and recommended reading
Papers of particular interest, published within the annual period of review, have been highlighted as:
● of special interest
●● of outstanding interest
- 1.Mathis D, Vence L, Benoist C. beta-Cell death during progression to diabetes. Nature. 2001;414(6865):792–8. doi: 10.1038/414792a. [DOI] [PubMed] [Google Scholar]
- 2.Bonner-Weir S. Life and death of the pancreatic beta cells. Trends Endocrinol Metab. 2000;11(9):375–8. doi: 10.1016/s1043-2760(00)00305-2. [DOI] [PubMed] [Google Scholar]
- 3.Mandrup-Poulsen T. beta-cell apoptosis: stimuli and signaling. Diabetes. 2001;50(Suppl 1):S58–63. doi: 10.2337/diabetes.50.2007.s58. [DOI] [PubMed] [Google Scholar]
- 4.Mandrup-Poulsen T. Apoptotic signal transduction pathways in diabetes. Biochem Pharmacol. 2003;66(8):1433–40. doi: 10.1016/s0006-2952(03)00494-5. [DOI] [PubMed] [Google Scholar]
- 5.Pick A, Clark J, Kubstrup C, Levisetti M, Pugh W, Bonner-Weir S, et al. Role of apoptosis in failure of beta-cell mass compensation for insulin resistance and beta-cell defects in the male Zucker diabetic fatty rat. Diabetes. 1998;47(3):358–64. doi: 10.2337/diabetes.47.3.358. [DOI] [PubMed] [Google Scholar]
- 6.Poitout V, Robertson RP. Minireview: Secondary beta-cell failure in type 2 diabetes–a convergence of glucotoxicity and lipotoxicity. Endocrinology. 2002;143(2):339–42. doi: 10.1210/endo.143.2.8623. [DOI] [PubMed] [Google Scholar]
- 7.Shalev A. Minireview: Thioredoxin-interacting protein: regulation and function in the pancreatic beta-cell. Mol Endocrinol. 2014;28(8):1211–20. doi: 10.1210/me.2014-1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alhawiti NM, Al Mahri S, Aziz MA, Malik SS, Mohammad S. TXNIP in Metabolic Regulation: Physiological Role and Therapeutic Outlook. Curr Drug Targets. 2017;18(9):1095–103. doi: 10.2174/1389450118666170130145514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen KS, DeLuca HF. Isolation and characterization of a novel cDNA from HL-60 cells treated with 1,25-dihydroxyvitamin D-3. Biochim Biophys Acta. 1994;1219(1):26–32. doi: 10.1016/0167-4781(94)90242-9. [DOI] [PubMed] [Google Scholar]
- 10.Ludwig DL, Kotanides H, Le T, Chavkin D, Bohlen P, Witte L. Cloning, genetic characterization, and chromosomal mapping of the mouse VDUP1 gene. Gene. 2001;269(1-2):103–12. doi: 10.1016/s0378-1119(01)00455-3. [DOI] [PubMed] [Google Scholar]
- 11.Nishiyama A, Matsui M, Iwata S, Hirota K, Masutani H, Nakamura H, et al. Identification of thioredoxin-binding protein-2/vitamin D(3) up-regulated protein 1 as a negative regulator of thioredoxin function and expression. J Biol Chem. 1999;274(31):21645–50. doi: 10.1074/jbc.274.31.21645. [DOI] [PubMed] [Google Scholar]
- 12.Nishiyama A, Masutani H, Nakamura H, Nishinaka Y, Yodoi J. Redox regulation by thioredoxin and thioredoxin-binding proteins. IUBMB Life. 2001;52(1-2):29–33. doi: 10.1080/15216540252774739. [DOI] [PubMed] [Google Scholar]
- 13.Junn E, Han SH, Im JY, Yang Y, Cho EW, Um HD, et al. Vitamin D3 up-regulated protein 1 mediates oxidative stress via suppressing the thioredoxin function. J Immunol. 2000;164(12):6287–95. doi: 10.4049/jimmunol.164.12.6287. [DOI] [PubMed] [Google Scholar]
- 14.Yamanaka H, Maehira F, Oshiro M, Asato T, Yanagawa Y, Takei H, et al. A possible interaction of thioredoxin with VDUP1 in HeLa cells detected in a yeast two-hybrid system. Biochem Biophys Res Commun. 2000;271(3):796–800. doi: 10.1006/bbrc.2000.2699. [DOI] [PubMed] [Google Scholar]
- 15.Patwari P, Higgins LJ, Chutkow WA, Yoshioka J, Lee RT. The interaction of thioredoxin with Txnip. Evidence for formation of a mixed disulfide by disulfide exchange. J Biol Chem. 2006;281(31):21884–91. doi: 10.1074/jbc.M600427200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schulze PC, De Keulenaer GW, Yoshioka J, Kassik KA, Lee RT. Vitamin D3-upregulated protein-1 (VDUP-1) regulates redox-dependent vascular smooth muscle cell proliferation through interaction with thioredoxin. Circ Res. 2002;91(8):689–95. doi: 10.1161/01.res.0000037982.55074.f6. [DOI] [PubMed] [Google Scholar]
- 17.Schulze PC, Yoshioka J, Takahashi T, He Z, King GL, Lee RT. Hyperglycemia promotes oxidative stress through inhibition of thioredoxin function by thioredoxin-interacting protein. J Biol Chem. 2004;279(29):30369–74. doi: 10.1074/jbc.M400549200. [DOI] [PubMed] [Google Scholar]
- 18.Saxena G, Chen J, Shalev A. Intracellular shuttling and mitochondrial function of thioredoxin-interacting protein. J Biol Chem. 2010;285(6):3997–4005. doi: 10.1074/jbc.M109.034421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shalev A, Pise-Masison CA, Radonovich M, Hoffmann SC, Hirshberg B, Brady JN, et al. Oligonucleotide microarray analysis of intact human pancreatic islets: identification of glucose-responsive genes and a highly regulated TGFbeta signaling pathway. Endocrinology. 2002;143(9):3695–8. doi: 10.1210/en.2002-220564. [DOI] [PubMed] [Google Scholar]
- 20.Minn AH, Hafele C, Shalev A. Thioredoxin-interacting protein is stimulated by glucose through a carbohydrate response element and induces beta-cell apoptosis. Endocrinology. 2005;146(5):2397–405. doi: 10.1210/en.2004-1378. [DOI] [PubMed] [Google Scholar]
- 21.Chen J, Fontes G, Saxena G, Poitout V, Shalev A. Lack of TXNIP protects against mitochondria-mediated apoptosis but not against fatty acid-induced ER stress-mediated beta-cell death. Diabetes. 2010;59(2):440–7. doi: 10.2337/db09-0949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kibbe C, Chen J, Xu G, Jing G, Shalev A. FOXO1 competes with carbohydrate response element-binding protein (ChREBP) and inhibits thioredoxin-interacting protein (TXNIP) transcription in pancreatic beta cells. J Biol Chem. 2013;288(32):23194–202. doi: 10.1074/jbc.M113.473082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cha-Molstad H, Saxena G, Chen J, Shalev A. Glucose-stimulated expression of Txnip is mediated by carbohydrate response element-binding protein, p300, and histone H4 acetylation in pancreatic beta cells. J Biol Chem. 2009;284(25):16898–905. doi: 10.1074/jbc.M109.010504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen J, Jing G, Xu G, Shalev A. Thioredoxin-interacting protein stimulates its own expression via a positive feedback loop. Mol Endocrinol. 2014;28(5):674–80. doi: 10.1210/me.2014-1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hong K, Xu G, Grayson TB, Shalev A. Cytokines Regulate beta-Cell Thioredoxin-interacting Protein (TXNIP) via Distinct Mechanisms and Pathways. J Biol Chem. 2016;291(16):8428–39. doi: 10.1074/jbc.M115.698365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26●.Chau GC, Im DU, Kang TM, Bae JM, Kim W, Pyo S, et al. mTOR controls ChREBP transcriptional activity and pancreatic beta cell survival under diabetic stress. J Cell Biol. 2017;216(7):2091–105. doi: 10.1083/jcb.201701085. This study found that mTOR decreases beta cell TXNIP expression in the context of diabetes again by associating with and inhibiting the transcriptional activity of ChREBP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yamashita H, Takenoshita M, Sakurai M, Bruick RK, Henzel WJ, Shillinglaw W, et al. A glucose-responsive transcription factor that regulates carbohydrate metabolism in the liver. Proc Natl Acad Sci U S A. 2001;98(16):9116–21. doi: 10.1073/pnas.161284298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iizuka K, Bruick RK, Liang G, Horton JD, Uyeda K. Deficiency of carbohydrate response element-binding protein (ChREBP) reduces lipogenesis as well as glycolysis. Proc Natl Acad Sci U S A. 2004;101(19):7281–6. doi: 10.1073/pnas.0401516101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Letexier D, Pinteur C, Large V, Frering V, Beylot M. Comparison of the expression and activity of the lipogenic pathway in human and rat adipose tissue. J Lipid Res. 2003;44(11):2127–34. doi: 10.1194/jlr.M300235-JLR200. [DOI] [PubMed] [Google Scholar]
- 30.Stoltzman CA, Peterson CW, Breen KT, Muoio DM, Billin AN, Ayer DE. Glucose sensing by MondoA:Mlx complexes: a role for hexokinases and direct regulation of thioredoxin-interacting protein expression. Proc Natl Acad Sci U S A. 2008;105(19):6912–7. doi: 10.1073/pnas.0712199105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31●.Gorgens SW, Benninghoff T, Eckardt K, Springer C, Chadt A, Melior A, et al. Hypoxia in Combination With Muscle Contraction Improves Insulin Action and Glucose Metabolism in Human Skeletal Muscle via the HIF-1alpha Pathway. Diabetes. 2017;66(11):2800–7. doi: 10.2337/db16-1488. In this paper TXNIP was identified as an exercise/HIF-1alpha-regulated gene in skeletal muscle suggesting that it may also play a role in exercise-mediated effects on peripheral regulation of glucose homeostasis. [DOI] [PubMed] [Google Scholar]
- 32.Lerner AG, Upton JP, Praveen PV, Ghosh R, Nakagawa Y, Igbaria A, et al. IRE1alpha induces thioredoxin-interacting protein to activate the NLRP3 inflammasome and promote programmed cell death under irremediable ER stress. Cell Metab. 2012;16(2):250–64. doi: 10.1016/j.cmet.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oslowski CM, Hara T, O’Sullivan-Murphy B, Kanekura K, Lu S, Hara M, et al. Thioredoxin-interacting protein mediates ER stress-induced beta cell death through initiation of the inflammasome. Cell Metab. 2012;16(2):265–73. doi: 10.1016/j.cmet.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou R, Tardivel A, Thorens B, Choi I, Tschopp J. Thioredoxin-interacting protein links oxidative stress to inflammasome activation. Nat Immunol. 2010;11(2):136–40. doi: 10.1038/ni.1831. [DOI] [PubMed] [Google Scholar]
- 35.Schroder K, Zhou R, Tschopp J. The NLRP3 inflammasome: a sensor for metabolic danger? Science. 2010;327(5963):296–300. doi: 10.1126/science.1184003. [DOI] [PubMed] [Google Scholar]
- 36.Maedler K, Sergeev P, Ris F, Oberholzer J, Joller-Jemelka HI, Spinas GA, et al. Glucose-induced beta cell production of IL-1beta contributes to glucotoxicity in human pancreatic islets. J Clin Invest. 2002;110(6):851–60. doi: 10.1172/JCI15318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hoffman HM, Mueller JL, Broide DH, Wanderer AA, Kolodner RD. Mutation of a new gene encoding a putative pyrin-like protein causes familial cold autoinflammatory syndrome and Muckle-Wells syndrome. Nat Genet. 2001;29(3):301–5. doi: 10.1038/ng756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.March CJ, Mosley B, Larsen A, Cerretti DP, Braedt G, Price V, et al. Cloning, sequence and expression of two distinct human interleukin-1 complementary DNAs. Nature. 1985;315(6021):641–7. doi: 10.1038/315641a0. [DOI] [PubMed] [Google Scholar]
- 39.Westwell-Roper CY, Ehses JA, Verchere CB. Resident macrophages mediate islet amyloid polypeptide-induced islet IL-1beta production and beta-cell dysfunction. Diabetes. 2014;63(5):1698–711. doi: 10.2337/db13-0863. [DOI] [PubMed] [Google Scholar]
- 40.Xu G, Chen J, Jing G, Shalev A. Thioredoxin-interacting protein regulates insulin transcription through microRNA-204. Nat Med. 2013;19(9):1141–6. doi: 10.1038/nm.3287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41●.Jo S, Chen J, Xu G, Grayson TB, Thielen LA, Shalev A. miR-204 controls glucagon-like peptide 1 receptor expression and agonist function. Diabetes. 2017:db170506. doi: 10.2337/db17-0506. Ahead of print. These studies discovered that inhibition of TXNIP and/or miR-204 specifically induces GLP1R expression in the beta cell, thus uncovering a novel link between TXNIP and GLP-1 signaling. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Westermark P, Andersson A, Westermark GT. Islet amyloid polypeptide, islet amyloid, and diabetes mellitus. Physiol Rev. 2011;91(3):795–826. doi: 10.1152/physrev.00042.2009. [DOI] [PubMed] [Google Scholar]
- 43.Zhu T, Wang Y, He B, Zang J, He Q, Zhang W. Islet amyloid polypeptide acts on glucose- stimulated beta cells to reduce voltage-gated calcium channel activation, intracellular Ca(2+) concentration, and insulin secretion. Diabetes Metab Res Rev. 2011;27(1):28–34. doi: 10.1002/dmrr.1140. [DOI] [PubMed] [Google Scholar]
- 44.Howard CF., Jr Longitudinal studies on the development of diabetes in individual Macaca nigra. Diabetologia. 1986;29(5):301–6. doi: 10.1007/BF00452067. [DOI] [PubMed] [Google Scholar]
- 45.Jing G, Westwell-Roper C, Chen J, Xu G, Verchere CB, Shalev A. Thioredoxin-interacting protein promotes islet amyloid polypeptide expression through miR-124a and FoxA2. J Biol Chem. 2014;289(17):11807–15. doi: 10.1074/jbc.M113.525022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Filios SR, Xu G, Chen J, Hong K, Jing G, Shalev A. MicroRNA-200 is induced by thioredoxin-interacting protein and regulates Zeb1 protein signaling and beta cell apoptosis. J Biol Chem. 2014;289(52):36275–83. doi: 10.1074/jbc.M114.592360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li XF, Shen WW, Sun YY, Li WX, Sun ZH, Liu YH, et al. MicroRNA-20a negatively regulates expression of NLRP3-inflammasome by targeting TXNIP in adjuvant-induced arthritis fibroblast-like synoviocytes. Joint Bone Spine. 2016;83(6):695–700. doi: 10.1016/j.jbspin.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 48.Chen J, Saxena G, Mungrue IN, Lusis AJ, Shalev A. Thioredoxin-interacting protein: a critical link between glucose toxicity and beta-cell apoptosis. Diabetes. 2008;57(4):938–44. doi: 10.2337/db07-0715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen J, Hui ST, Couto FM, Mungrue IN, Davis DB, Attie AD, et al. Thioredoxin-interacting protein deficiency induces Akt/Bcl-xL signaling and pancreatic beta-cell mass and protects against diabetes. FASEB J. 2008;22(10):3581–94. doi: 10.1096/fj.08-111690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shaked M, Ketzinel-Gilad M, Ariav Y, Cerasi E, Kaiser N, Leibowitz G. Insulin counteracts glucotoxic effects by suppressing thioredoxin-interacting protein production in INS-1E beta cells and in Psammomys obesus pancreatic islets. Diabetologia. 2009;52(4):636–44. doi: 10.1007/s00125-009-1274-2. [DOI] [PubMed] [Google Scholar]
- 51.Minn AH, Pise-Masison CA, Radonovich M, Brady JN, Wang P, Kendziorski C, et al. Gene expression profiling in INS-1 cells overexpressing thioredoxin-interacting protein. Biochem Biophys Res Commun. 2005;336(3):770–8. doi: 10.1016/j.bbrc.2005.08.161. [DOI] [PubMed] [Google Scholar]
- 52.Robertson RP, Harmon J, Tran PO, Tanaka Y, Takahashi H. Glucose toxicity in beta-cells: type 2 diabetes, good radicals gone bad, and the glutathione connection. Diabetes. 2003;52(3):581–7. doi: 10.2337/diabetes.52.3.581. [DOI] [PubMed] [Google Scholar]
- 53.Hotta M, Tashiro F, Ikegami H, Niwa H, Ogihara T, Yodoi J, et al. Pancreatic beta cell-specific expression of thioredoxin, an antioxidative and antiapoptotic protein, prevents autoimmune and streptozotocin-induced diabetes. J Exp Med. 1998;188(8):1445–51. doi: 10.1084/jem.188.8.1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Clee SM, Nadler ST, Attie AD. Genetic and genomic studies of the BTBR ob/ob mouse model of type 2 diabetes. Am J Ther. 2005;12(6):491–8. doi: 10.1097/01.mjt.0000178781.89789.25. [DOI] [PubMed] [Google Scholar]
- 55.Oka S, Liu W, Masutani H, Hirata H, Shinkai Y, Yamada S, et al. Impaired fatty acid utilization in thioredoxin binding protein-2 (TBP-2)-deficient mice: a unique animal model of Reye syndrome. FASEB J. 2006;20(1):121–3. doi: 10.1096/fj.05-4439fje. [DOI] [PubMed] [Google Scholar]
- 56.Sheth SS, Castellani LW, Chari S, Wagg C, Thipphavong CK, Bodnar JS, et al. Thioredoxin-interacting protein deficiency disrupts the fasting-feeding metabolic transition. J Lipid Res. 2005;46(1):123–34. doi: 10.1194/jlr.M400341-JLR200. [DOI] [PubMed] [Google Scholar]
- 57.Hand LE, Saer BR, Hui ST, Jinnah HA, Steinlechner S, Loudon AS, et al. Induction of the metabolic regulator Txnip in fasting-induced and natural torpor. Endocrinology. 2013;154(6):2081–91. doi: 10.1210/en.2012-2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Blouet C, Schwartz GJ. Nutrient-sensing hypothalamic TXNIP links nutrient excess to energy imbalance in mice. J Neurosci. 2011;31(16):6019–27. doi: 10.1523/JNEUROSCI.6498-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Blouet C, Liu SM, Jo YH, Chua S, Schwartz GJ. TXNIP in Agrp neurons regulates adiposity, energy expenditure, and central leptin sensitivity. J Neurosci. 2012;32(29):9870–7. doi: 10.1523/JNEUROSCI.0353-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chai TF, Hong SY, He H, Zheng L, Hagen T, Luo Y, et al. A potential mechanism of metformin-mediated regulation of glucose homeostasis: inhibition of Thioredoxin-interacting protein (Txnip) gene expression. Cell Signal. 2012;24(8):1700–5. doi: 10.1016/j.cellsig.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 61.Shaked M, Ketzinel-Gilad M, Cerasi E, Kaiser N, Leibowitz G. AMP-activated protein kinase (AMPK) mediates nutrient regulation of thioredoxin-interacting protein (TXNIP) in pancreatic beta-cells. PLoS One. 2011;6(12):e28804. doi: 10.1371/journal.pone.0028804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li X, Kover KL, Heruth DP, Watkins DJ, Moore WV, Jackson K, et al. New Insight Into Metformin Action: Regulation of ChREBP and FOXO1 Activities in Endothelial Cells. Mol Endocrinol. 2015;29(8):1184–94. doi: 10.1210/ME.2015-1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen J, Couto FM, Minn AH, Shalev A. Exenatide inhibits beta-cell apoptosis by decreasing thioredoxin-interacting protein. Biochem Biophys Res Commun. 2006;346(3):1067–74. doi: 10.1016/j.bbrc.2006.06.027. [DOI] [PubMed] [Google Scholar]
- 64.Shao W, Yu Z, Fantus IG, Jin T. Cyclic AMP signaling stimulates proteasome degradation of thioredoxin interacting protein (TxNIP) in pancreatic beta-cells. Cell Signal. 2010;22(8):1240–6. doi: 10.1016/j.cellsig.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 65.Clark AL, Kanekura K, Lavagnino Z, Spears LD, Abreu D, Mahadevan J, et al. Targeting Cellular Calcium Homeostasis to Prevent Cytokine-Mediated Beta Cell Death. Sci Rep. 2017;7(1):5611. doi: 10.1038/s41598-017-05935-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Xu G, Chen J, Jing G, Shalev A. Preventing beta-cell loss and diabetes with calcium channel blockers. Diabetes. 2012;61(4):848–56. doi: 10.2337/db11-0955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cooper-Dehoff R, Cohen JD, Bakris GL, Messerli FH, Erdine S, Hewkin AC, et al. Predictors of development of diabetes mellitus in patients with coronary artery disease taking antihypertensive medications (findings from the INternational VErapamil SR-Trandolapril STudy [INVEST]) Am J Cardiol. 2006;98(7):890–4. doi: 10.1016/j.amjcard.2006.04.030. [DOI] [PubMed] [Google Scholar]
- 68.Cooper-DeHoff RM, Aranda JM, Jr, Gaxiola E, Cangiano JL, Garcia-Barreto D, Conti CR, et al. Blood pressure control and cardiovascular outcomes in high-risk Hispanic patients–findings from the International Verapamil SR/Trandolapril Study (INVEST) Am Heart J. 2006;151(5):1072–9. doi: 10.1016/j.ahj.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 69●.Khodneva Y, Shalev A, Frank SJ, Carson AP, Safford MM. Calcium channel blocker use is associated with lower fasting serum glucose among adults with diabetes from the REGARDS study. Diabetes Res Clin Pract. 2016;115:115–21. doi: 10.1016/j.diabres.2016.01.021. Using diabetic adults from the REGARDS cohort this study found that verapamil use was associated with an up to 37mg/dL lower fasting glucose as compared to subjects not on calcium channel blockers. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70●●.Yin T, Kuo SC, Chang YY, Chen YT, Wang KK. Verapamil Use Is Associated With Reduction of Newly Diagnosed Diabetes Mellitus. J Clin Endocrinol Metab. 2017;102(7):2604–10. doi: 10.1210/jc.2016-3778. This large retrospective analysis of Taiwan’s National Health Insurance Research Database observed that verapamil use was associated with a lower incidence of type 2 diabetes. [DOI] [PubMed] [Google Scholar]
- 71.Parikh H, Carlsson E, Chutkow WA, Johansson LE, Storgaard H, Poulsen P, et al. TXNIP regulates peripheral glucose metabolism in humans. PLoS Med. 2007;4(5):e158. doi: 10.1371/journal.pmed.0040158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chutkow WA, Patwari P, Yoshioka J, Lee RT. Thioredoxin-interacting protein (Txnip) is a critical regulator of hepatic glucose production. J Biol Chem. 2008;283(4):2397–406. doi: 10.1074/jbc.M708169200. [DOI] [PubMed] [Google Scholar]
- 73.Ishrat T, Mohamed IN, Pillai B, Soliman S, Fouda AY, Ergul A, et al. Thioredoxin-interacting protein: a novel target for neuroprotection in experimental thromboembolic stroke in mice. Mol Neurobiol. 2015;51(2):766–78. doi: 10.1007/s12035-014-8766-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Byon CH, Han T, Wu J, Hui ST. Txnip ablation reduces vascular smooth muscle cell inflammation and ameliorates atherosclerosis in apolipoprotein E knockout mice. Atherosclerosis. 2015;241(2):313–21. doi: 10.1016/j.atherosclerosis.2015.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Xiang G, Seki T, Schuster MD, Witkowski P, Boyle AJ, See F, et al. Catalytic degradation of vitamin D up-regulated protein 1 mRNA enhances cardiomyocyte survival and prevents left ventricular remodeling after myocardial ischemia. J Biol Chem. 2005;280(47):39394–402. doi: 10.1074/jbc.M502966200. [DOI] [PubMed] [Google Scholar]
- 76.Yoshioka J, Chutkow WA, Lee S, Kim JB, Yan J, Tian R, et al. Deletion of thioredoxin-interacting protein in mice impairs mitochondrial function but protects the myocardium from ischemia-reperfusion injury. J Clin Invest. 2012;122(1):267–79. doi: 10.1172/JCI44927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yoshioka J, Imahashi K, Gabel SA, Chutkow WA, Burds AA, Gannon J, et al. Targeted deletion of thioredoxin-interacting protein regulates cardiac dysfunction in response to pressure overload. Circ Res. 2007;101(12):1328–38. doi: 10.1161/CIRCRESAHA.106.160515. [DOI] [PubMed] [Google Scholar]
- 78●.Chen J, Young ME, Chatham JC, Crossman DK, Dell’Italia LJ, Shalev A. TXNIP regulates myocardial fatty acid oxidation via miR-33a signaling. Am J Physiol Heart Circ Physiol. 2016;311(1):H64–75. doi: 10.1152/ajpheart.00151.2016. In this study, TXNIP deficiency was found to promote myocardial beta-oxidation by signaling through miR-33a providing another example of how some TXNIP effects on metabolism are mediated by microRNAs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cha-Molstad H, Xu G, Chen J, Jing G, Young ME, Chatham JC, et al. Calcium channel blockers act through nuclear factor Y to control transcription of key cardiac genes. Mol Pharmacol. 2012;82(3):541–9. doi: 10.1124/mol.112.078253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chen J, Cha-Molstad H, Szabo A, Shalev A. Diabetes induces and calcium channel blockers prevent cardiac expression of proapoptotic thioredoxin-interacting protein. Am J Physiol Endocrinol Metab. 2009;296(5):E1133–9. doi: 10.1152/ajpendo.90944.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shi Y, Ren Y, Zhao L, Du C, Wang Y, Zhang Y, et al. Knockdown of thioredoxin interacting protein attenuates high glucose-induced apoptosis and activation of ASK1 in mouse mesangial cells. FEBS Lett. 2011;585(12):1789–95. doi: 10.1016/j.febslet.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 82.Shah A, Xia L, Masson EA, Gui C, Momen A, Shikatani EA, et al. Thioredoxin-Interacting Protein Deficiency Protects against Diabetic Nephropathy. J Am Soc Nephrol. 2015 doi: 10.1681/ASN.2014050528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Perrone L, Devi TS, Hosoya KI, Terasaki T, Singh LP. Inhibition of TXNIP expression in vivo blocks early pathologies of diabetic retinopathy. Cell Death Dis. 2010;1:e65. doi: 10.1038/cddis.2010.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.El-Azab MF, Baldowski BR, Mysona BA, Shanab AY, Mohamed IN, Abdelsaid MA, et al. Deletion of thioredoxin-interacting protein preserves retinal neuronal function by preventing inflammation and vascular injury. Br J Pharmacol. 2014;171(5):1299–313. doi: 10.1111/bph.12535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sheth SS, Bodnar JS, Ghazalpour A, Thipphavong CK, Tsutsumi S, Tward AD, et al. Hepatocellular carcinoma in Txnip-deficient mice. Oncogene. 2006;25(25):3528–36. doi: 10.1038/sj.onc.1209394. [DOI] [PubMed] [Google Scholar]


