In September 2011, the Centers for Disease Control and Prevention (CDC) convened a Ventilator-Associated Pneumonia (VAP) Surveillance Definition Working Group to organize a formal process for leaders and experts of key stakeholder organizations to discuss the challenges of VAP surveillance definitions and to propose new approaches to VAP surveillance in adult patients (Table 1). The charges to the Working Group were to:
-
1
Critically review a draft, streamlined VAP surveillance definition developed for use in adult patients;
-
2
Suggest modifications to enhance the reliability and credibility of the surveillance definition within the critical care and infection prevention communities;
-
3
Propose a final adult surveillance definition algorithm, to be implemented in the CDC's National Healthcare Safety Network (NHSN), taking into consideration the potential future use of the definition algorithm in public reporting, interfacility comparisons, and pay-for-reporting and pay-for-performance programs.
Table 1.
VAP Surveillance Definition Working Group Organizations, Representatives and Federal Participants
| Organization | Representative(s) |
|---|---|
| American Association of Critical-Care Nurses | Suzanne Burns and Beth Hammer |
| American Association for Respiratory Care | Dean Hess |
| American College of Chest Physicians | Robert Balk and David Gutterman |
| American Thoracic Society | Nicholas Hill and Mitchell Levy |
| Association of Professionals in Infection Control and Epidemiology | Linda Greene |
| Council of State and Territorial Epidemiologists | Carole VanAntwerpen |
| Healthcare Infection Control Practices Advisory Committee Surveillance Working Group | Daniel Diekema |
| Infectious Diseases Society of America | Edward Septimus |
| Society for Healthcare Epidemiology of America | Michael Klompas |
| Society of Critical Care Medicine | Clifford Deutschman, Marin Kollef, and Pamela Lipsett |
| U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion | Don Wright |
| National Institutes of Health | David Henderson |
| Centers for Disease Control and Prevention, Division of Healthcare Quality Promotion | Scott Fridkin, Alice Guh, Shelley Magill, Teresa Horan, others |
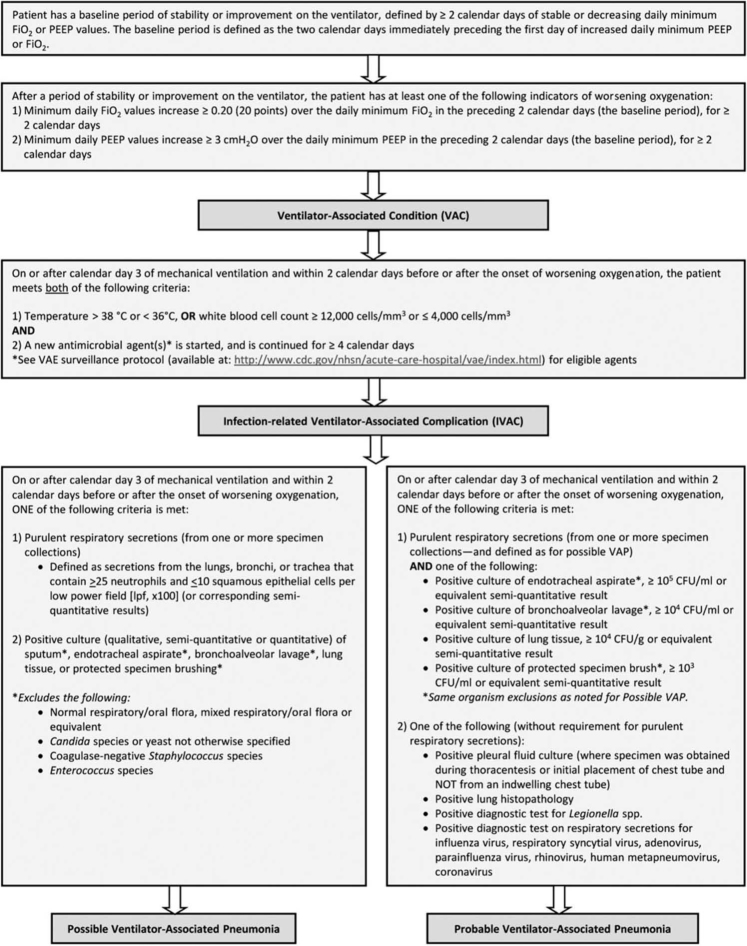
The Working Group's surveillance definition algorithm, which is referred to as the ventilator-associated events or VAE surveillance definition algorithm, represents a purposeful departure from VAP toward more general, objective measures of conditions and complications occurring in patients on mechanical ventilation (Figure 1; VAE surveillance protocol available at: http://www.cdc.gov/nhsn/acute-care-hospital/vae/index.html). The VAE surveillance definition algorithm uses a tiered approach, moving from measures of ventilator-associated conditions (VAC), to infection-related ventilator-associated complications (IVAC), to possible and probable VAP.
Figure 1.
Ventilator-associated events surveillance definition algorithm. Available at: http://www.cdc.gov/nhsn/acute-care-hospital/vae/index.html). Abbreviations: CFU = colony-forming units; Fio 2 = fraction of inspired oxygen; PEEP = positive end-expiratory pressure; VAP=ventilator-associated pneumonia.
The first tier of VAE surveillance, VAC, seeks to identify episodes of sustained respiratory deterioration, and will capture both infectious and non-infectious conditions and complications occurring in mechanically ventilated patients. VAC is defined by a sustained period of worsening oxygenation that immediately follows a baseline period of stability or improvement on the ventilator. To meet the VAC definition, a mechanically ventilated patient must have at least 2 calendar days of stable or decreasing daily minimum positive end-expiratory pressure (PEEP) or fraction of inspired oxygen (Fio 2), followed by at least 2 days of increased daily minimum PEEP or Fio 2, where the increase in the daily minimum PEEP is ≥ 3 cm H2O greater than the daily minimum PEEP during the baseline period, or where the increase in the daily minimum Fio 2 is ≥ 0.20 (or 20 percentage points in oxygen concentration) greater than the daily minimum Fio 2 during the baseline period. For example, if a patient's daily minimum Fio 2 requirement on days 4 and 5 of mechanical ventilation is 0.40, then the patient's daily minimum Fio 2 requirement would need to be at least 0.60 on days 6 and 7 of mechanical ventilation for the VAC definition to be met. The Working Group's decisions to set specific thresholds of 3 cm H20 and 0.20 (20 points) for the increases in PEEP and Fio 2, respectively, and to define a “sustained” increase as an increase persisting for at least 2 calendar days, were based on expert opinion of what criteria would likely identify clinically important events, while minimizing inadvertent inclusion of other types of events resulting in transient changes in oxygenation—such as surgery or performance of other procedures. Thresholds were also selected based upon published data indicating that increases of ≥ 2.5 cm H2O in PEEP or ≥ 0.15 (15 points) in Fio 2 sustained for at least 2 days were associated with longer duration of mechanical ventilation, ICU and hospital stays, and increased mortality. 1 Subsequently, additional data have been published that support the Working Group's approach to VAC. 2
The second tier, IVAC, attempts to identify the subset of VACs that are potentially related to infection, as evidenced by an abnormal white blood cell count or temperature and initiation of a new antimicrobial agent. IVAC will likely capture patients with pulmonary infections and extrapulmonary infections of sufficient severity to trigger respiratory deterioration. The Working Group recognized the low predictive value of an abnormal temperature or white blood cell count in ICU patients, and Klompas and colleagues have shown that the addition of fever or abnormal white blood cell count to a VAC definition does not substantially enhance the definition's predictive value for death. 2 Nevertheless, these are objective and readily available signs that are frequently used at the bedside to assess for the presence of infection. The additional required criterion of starting a new antimicrobial, where the new agent is continued for at least 4 days, may add specificity and clinical credibility to the IVAC definition, although data are needed.
The third tier, possible and probable VAP, attempts to zero in on the subset of IVAC patients with respiratory infections as manifested by objective evidence of purulent respiratory secretions (where purulence is defined using quantitative or semiquantitative criteria for the number of neutrophils on Gram stain) and/or positive results of microbiological tests performed on respiratory tract specimens. The possible VAP definition is met with the presence of purulent secretions or a positive lower respiratory tract culture (showing any growth); the probable VAP definition requires purulent secretions in addition to a positive lower respiratory tract culture meeting certain quantitative or semiquantitative thresholds of pathogen growth. Organisms that are uncommonly regarded as true VAP pathogens are excluded from possible and probable VAP culture criteria (with the exception of lung tissue cultures): Candida spp., coagulase-negative staphylococci, and Enterococcus spp. The probable VAP definition can also be met based upon the presence of a positive pleural fluid culture, lung tissue with histopathological evidence of infection, or positive diagnostic tests for Legionella or selected respiratory tract viruses, without the concomitant requirement for purulent secretions. Although data have shown that requiring purulent secretions or positive cultures in patients who have met a VAC definition actually diminishes the association between mortality and VAC, 2 the Working Group felt that it was important to provide definitions within the VAE algorithm that more closely resemble VAP diagnostic criteria used at the bedside.
This tiered approach is believed to be the most appropriate approach in the current environment. It acknowledges limitations in the ability to accurately identify VAP for surveillance purposes—simply labeling an event “VAP” does not make it so—and focuses instead on a more general measure of complications of mechanical ventilation. This approach may also reduce the likelihood of definition gaming or manipulation that could artificially lower event rates.
Two features of the VAE surveillance definition algorithm are of particular note. First, radiographic evidence of pneumonia is not included as a criterion in any tier of the algorithm because of lack of specificity, and the subjectivity inherent in facilities' and individual providers' practices in ordering, performing, interpreting and reporting results of chest radiographs. Second, only VAC and IVAC (and therefore the overall VAE rate—the rate of all events meeting at least the VAC definition—and the rate of all events meeting at least the IVAC definition) are intended to be possible candidates for future use in public reporting, interfacility comparisons, and pay-for-performance programs. The VAC and IVAC definitions use criteria based on data anticipated to be available from most mechanically ventilated patients and less subject to manipulation or gaming. By contrast, the third definition tier, possible and probable VAP, was developed to be used only in internal quality improvement. These VAP definitions include criteria based on documentation of purulent secretions and/or microbiological findings and are more in keeping with traditional clinical constructs of VAP. Because of the substantial variability in the ordering and collection of lower respiratory tract specimens, and in laboratory processing of specimens and reporting of results, the Working Group determined that it was not appropriate to include these data elements in the VAC and IVAC definitions.
An iterative process for refining the definitions must be ensured as experience using the definition algorithm accumulates in the coming years. Although there was clearly a need to establish a new surveillance approach in the NHSN, there is also an urgent need to advance the science of surveillance for VAP and other VAE. The VAE surveillance definition algorithm should be studied, validated, and improved in an ongoing manner. Evaluation and refinement of the definitions should be conducted in collaboration with members of the Working Group and other members of stakeholder communities and organizations. The Working Group is already discussing potential modifications based on user feedback received during the first 3 months of VAE surveillance.
The VAP Surveillance Definition Working Group's new approach to surveillance in mechanically ventilated adults acknowledges the current limitations in VAP diagnosis and the potential benefit in focusing surveillance on an objective, reliable, but more general measure of significant conditions and complications that occur in patients on ventilators. VAE surveillance was implemented by the CDC's NHSN in January 2013. While much work remains, we believe this innovative approach to surveillance has significant potential to increase the validity of comparisons among healthcare facilities and, more importantly, to improve measurement and patient safety in the ICU.
Supplementary Material
A New Approach to Surveillance for Ventilator-Associated Events
Duration: 44 min
Moderator: D. Kyle Hogarth, MD, FCCP, Podcast Editor, CHEST
Participants: Shelley S. Magill, MD, PhD; Craig M. Lilly, MD, FCCP
Acknowledgments
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts: Dr Klompas received grant support from the CDC, US Food and Drug Administration, and the Office of the National Co-ordinator for Health IT. Dr Balk received grant support from the CDC and bioMérieux for participation in the EPIC CAP study (CDC) and the Procalcitonin in ICU antibiotic stewardship study (CDC and bioMérieux). Dr Deutschman received grant support from the National Institute of General Medical Sciences. Dr Diekema received grant support from Merck, Cerexa, bioMériuex, PurThread Technologies, and Pfizer. Dr Klompas received support for travel from the CDC, Society of Healthcare Epidemiologists of America, Association of Professionals in Infection Control, and the Duke University Infection Control Outreach Network. Dr Balk received support for travel from the CDC and Critical Care Societies Collaborative. Dr Burns received support for travel from the American Association of Critical-Care Nurses (AACN; meeting unrelated to this study). Drs Deutschman and Lipsett received support for travel from the Society of Critical Care Medicine. Ms Greene received support for travel from the Department of Health and Human Services/CDC. Ms Greene consults for INC. Dr Hess consulted for Philips Respironics, ResMed, Pari, and Breathe and received honorarium from Covidien and Maquet. Ms Greene lectured for Premier, Advanced Sterilization Products, and APIC. Dr Burns lectured for AACN (annual national conference). Ms Greene presented speeches for Covidien and Maquet. Dr Septimus received an honorarium for a lecture. Dr Klompas received support from the Society of Healthcare Epidemiologists of America for the development of educational presentations. Ms Greene is employed by the Rochester General Hospital. Dr Lipsett has board membership with the Society of Critical Care Medicine. Dr Deutschman received a stipend for his Presidency with the Society of Critical Care Medicine. Dr Deutschman received royalties from Elsevier for the textbook, Evidence-based Practice of Critical Care Medicine. Dr Burns receives royalties from McGraw-Hill for books endorsed by AACN. Ms Greene receives royalties from Up-To-Date, Jones and Bartlett, and McGraw-Hill. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Footnotes
Editor's Note: This article is an executive summary of a report from the Centers for Disease Control and Prevention Ventilator-Associated Pneumonia Surveillance Definition Working Group, entitled “Developing a new, national approach to surveillance for ventilator-associated events” and published in Critical Care Medicine (Magill SS, Klompas M, Balk R, et al. Developing a new, national approach to surveillance for ventilator-associated events. Crit Care Med. 2013;41(11):2467–2475.). The full report provides a comprehensive description of the Working Group process and outcome.
For editorial comment see page 1429
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, the American Association for Respiratory Care, the Association of Professionals in Infection Control and Epidemiology, the Council of State and Territorial Epidemiologists, or the Infectious Diseases Society of America.
Funding/Support: The work described herein was supported by the Centers for Disease Control and Prevention (CDC).
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Klompas M, Khan Y, Kleinman K, CDC Prevention Epicenters Program Multicenter evaluation of a novel surveillance paradigm for complications of mechanical ventilation. PLoS ONE. 2011;6(3):e18062. doi: 10.1371/journal.pone.0018062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klompas M, Magill S, Robicsek A, CDC Prevention Epicenters Program Objective surveillance definitions for ventilator-associated pneumonia. Crit Care Med. 2012;40(12):3154–3161. doi: 10.1097/CCM.0b013e318260c6d9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A New Approach to Surveillance for Ventilator-Associated Events
Duration: 44 min
Moderator: D. Kyle Hogarth, MD, FCCP, Podcast Editor, CHEST
Participants: Shelley S. Magill, MD, PhD; Craig M. Lilly, MD, FCCP