Abstract
Direct-current cardioversion is an important means of managing arrhythmias. During treatment, carefully synchronizing energy delivery to the QRS complex is necessary to avoid ventricular fibrillation caused by a shock during the vulnerable period of ventricular repolarization, that is, a shock on the T wave. The presence of an accessory pathway and ventricular preexcitation can lead to difficulty in distinguishing the QRS complex from the T wave because of bizarre, wide, irregular QRS complexes and prominent repolarization. We present the cases of 2 patients who had iatrogenic ventricular fibrillation from inappropriate T-wave synchronization during direct-current cardioversion of preexcited atrial fibrillation. Our experience shows that rapidly recognizing the iatrogenic cause of VF and immediate treatment with unsynchronized defibrillation can prevent adverse clinical outcomes.
Keywords: Atrial fibrillation/complications, electric countershock/adverse effects/standards, pre-excitation syndromes/complications, treatment outcome, ventricular fibrillation/etiology/prevention & control, Wolff-Parkinson-White syndrome/complications/drug therapy
Terminating arrhythmias by applying external direct-current (DC) cardioversion requires appropriate synchronization to the QRS complex to avoid ventricular fibrillation (VF) from a shock delivered during the vulnerable period of ventricular repolarization, known as a shock on the T wave. However, distinguishing the QRS from the T wave can be particularly difficult during preexcited atrial fibrillation (AF) because of the bizarre, irregular, wide QRS complexes with prominent repolarization waveforms. We present the cases of 2 patients who had iatrogenic VF resulting from inadvertent T-wave synchronization during attempted DC cardioversion of preexcited AF.
Case Reports
Patient 1
Emergency medical service providers were called to evaluate a 23-year-old man whose palpitations, chest pain, and dyspnea had awakened him from sleep. He had a history of a Wolff-Parkinson-White pattern on a previous surface electrocardiogram (ECG) but had been asymptomatic. On evaluation, the patient was tachycardic (heart rate, 250 beats/min). He received a 6-mg intravenous (IV) bolus of adenosine, and then a 12-mg dose, but there was no change in heart rate. He was then given IV amiodarone (dose unknown), without effect. On arrival at the emergency department, the patient's ECG showed preexcited AF (Fig. 1A). He was started on an IV procainamide drip, and sinus rhythm was restored (Fig. 1B). Results of a diagnostic electrophysiologic study revealed a left posteroseptal accessory pathway. During the intraprocedural period, the patient's AF recurred. A synchronized 360-J shock was delivered; however, because of inappropriate synchronization of the external defibrillator, a shock on the T wave induced VF (Fig. 1C). Ventricular fibrillation was recognized immediately, and an unsynchronized shock resulted in successful defibrillation. The patient's left posteroseptal accessory pathway was then ablated, after which he did well. At follow-up one month later, he had no clinical sequelae.
Fig. 1.
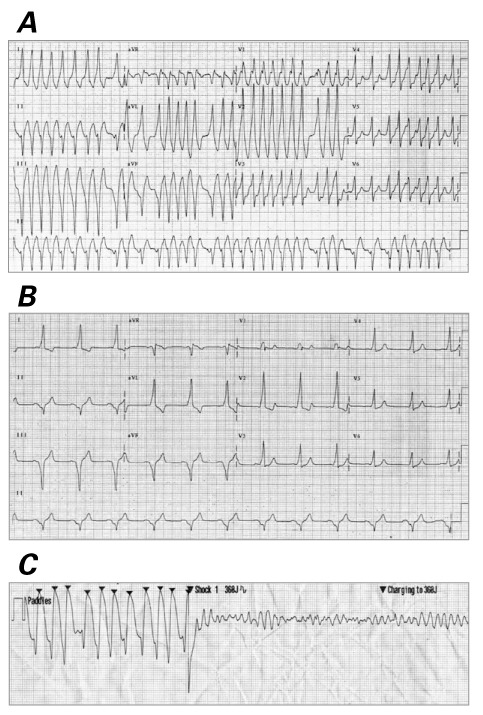
Patient 1. A) Electrocardiogram on presentation shows atrial fibrillation with preexcitation and rapid ventricular response. B) Electrocardiogram shows sinus rhythm. C) Telemetry strip shows inappropriate synchronization and shock on the T wave, which induced ventricular fibrillation. Arrowheads are synchronization markers placed by the external defibrillator.
Patient 2
A 30-year-old man with a history of hypertension presented at a small community hospital after he experienced weakness and dizziness while driving. A surface ECG revealed an irregularly irregular wide-complex tachycardia with varying QRS widths (Fig. 2A), but the patient's medical team did not recognize the preexcited AF pattern. Direct-current cardioversion was attempted with the external defibrillator intermittently synchronized to the T wave, and a 100-J shock caused VF (Fig. 2B), which went unrecognized. Instead of immediately delivering an unsynchronized shock, the team performed chest compressions; administered 1 mg of IV epinephrine (twice), IV atropine, and 300 mg of IV amiodarone; and intubated the patient. A 200-J shock, delivered 11 minutes after VF began, failed to restore sinus rhythm. Then, 20 minutes after VF began, a 300-J shock finally led to successful defibrillation. The patient was subsequently transferred to another medical facility. No other ventricular arrhythmia was observed after this event. Nevertheless, a subcutaneous implantable cardioverter-defibrillator was placed for the indication of polymorphic VT.
Fig. 2.
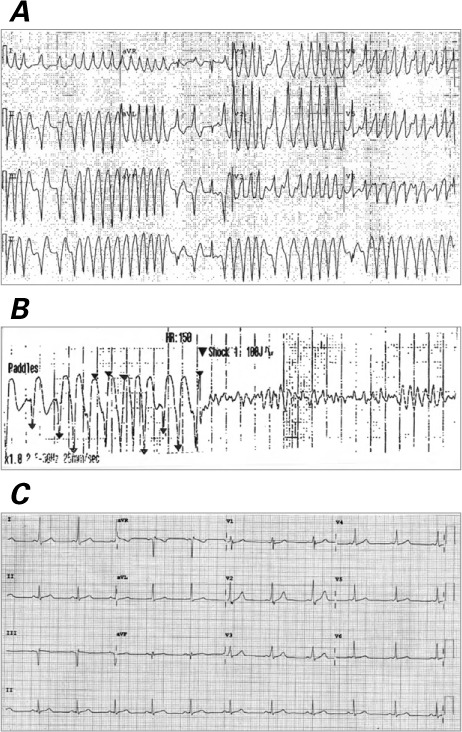
Patient 2. A) Electrocardiogram on presentation shows atrial fibrillation with preexcitation and rapid ventricular response. B) Telemetry strip shows inappropriate synchronization and shock on the T wave, which induced ventricular fibrillation. Arrowheads are synchronization markers placed by the external defibrillator. C) Electrocardiogram shows sinus rhythm.
One month later, the patient presented at our clinic, and his 12-lead ECG showed ventricular preexcitation (Fig. 2C). Results of an electrophysiologic study revealed a rapidly conducting left posteroseptal accessory pathway; the shortest preexcited R-R interval was 240 ms. The preexcited QRS morphology was identical to that of the patient's original presenting arrhythmia (Fig. 2A). Radiofrequency ablation was performed, eliminating the accessory pathway. The patient did well and had no sequelae.
Discussion
Atrial fibrillation in a patient with ventricular preexcitation can cause rapid ventricular activation via the accessory pathway and lead to an irregular wide-QRS tachycardia with varying degrees of QRS width. This is known as preexcited AF. Identifying this ECG pattern is crucial because administering IV adenosine or amiodarone,1 as well as IV or oral digoxin, β-blockers, or nondihydropyridine calcium blockers,2 is specifically contraindicated. These agents can increase the rate of ventricular activation via the accessory pathway because of preferential conduction over the accessory pathway, a reflexive increase in sympathetic stimulation from acute vasodilation and hypotension, or both.1–3 Accelerating rates of ventricular activation in the presence of hemodynamic collapse can induce VF. Whereas a hemodynamically stable patient can be safely treated with IV procainamide or IV ibutilide, an unstable patient should undergo emergency synchronized DC cardioversion.
We found 3 previous reports of VF caused by synchronization failure during electrical cardioversion of preexcited AF.4–6 Our additional cases show that rapidly recognizing iatrogenic VF and performing unsynchronized cardioversion (Patient 1) can prevent an adverse clinical outcome. On the other hand, failure to recognize the diagnosis or to rapidly defibrillate VF caused by inadvertent T-wave synchronization (Patient 2) can potentially cause substantial harm to the patient.
In the 3 previous reports,4–6 VF was induced with 50-, 70-, and 100-J synchronous T-wave shocks. One author6 suggested that selecting a higher energy could help prevent VF induction. However, in our first patient, VF was induced with a 360-J shock (Fig. 1C), showing that high-energy shocks do not necessarily compensate for poor synchronization. We postulate that iatrogenic VF from failed synchronization during electrical cardioversion of preexcited AF might occur more often than is recognized, and, along with inappropriate pharmacologic management, may account for some occurrences of VF in patients with preexcited AF.
The Association for the Advancement of Medical Instrumentation has published minimum standards for detecting QRS on cardiac monitors.7 Of importance, the authors recognized that tall T waves can be misidentified as the QRS complex.7 Differentiating QRS complexes from T waves in preexcited AF can be especially difficult because of the irregular rhythm, as well as the large-amplitude T waves that are often present. Appreciating the potential for VF from an inappropriate shock on the T wave during preexcited AF should prompt the clinician to carefully verify appropriate synchronization before delivering a shock, to immediately recognize iatrogenic postshock VF, and to rapidly deliver potentially life-saving unsynchronized defibrillation. The astute clinician is aware of the vagaries of QRS synchronization in preexcited AF and reviews the location of the synchronization markers before cardioversion to ensure that energy is delivered synchronous to the QRS complex and not the T wave. If the external defibrillator is inappropriately synchronizing to the T waves, selecting a different lead for sensing can improve QRS resolution and increase the likelihood of appropriate synchronization.
Of note, during a very rapid and irregular rhythm such as preexcited AF, even a shock appropriately synchronized to the QRS complex has the potential to induce VF if it is delivered after a very short R-R interval (≤300 ms) following a long R-R interval, especially if lower-energy shocks are used.8,9 This occurs when one region of the ventricles is still repolarizing because of the regional delay after the long-short sequence, while the remaining myocardium begins to depolarize. Consequently, even a QRS-synchronized shock may land in a portion of the ventricular myocardium during a vulnerable period. If iatrogenic VF results from inappropriate (or even appropriate) synchronization during DC cardioversion, the operator must recognize the rhythm, disable synchronization on the external defibrillator, and deliver an immediate unsynchronized high-energy DC shock to defibrillate the patient. Delaying diagnosis and therapy can result in substantial harm to the patient or death.
References
- 1. Boriani G, Biffi M, Frabetti L, Azzolini U, Sabbatini P, Bronzetti G, . et al. Ventricular fibrillation after intravenous amiodarone in Wolff-Parkinson-White syndrome with atrial fibrillation. Am Heart J 1996; 131( 6: 1214– 6. [DOI] [PubMed] [Google Scholar]
- 2. Kim RJ, Gerling BR, Kono AT, Greenberg ML.. Precipitation of ventricular fibrillation by intravenous diltiazem and metoprolol in a young patient with occult Wolff-Parkinson-White syndrome. Pacing Clin Electrophysiol 2008; 31( 6: 776– 9. [DOI] [PubMed] [Google Scholar]
- 3. January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, . et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society [published erratum appears in Circulation 2014;130(23):e270–1]. Circulation 2014; 130( 23: 2071– 104. [DOI] [PubMed] [Google Scholar]
- 4. Ebrahimi R, Rubin SA.. Electrical cardioversion resulting in death from synchronization failure. Am J Cardiol 1994; 74( 1: 100– 2. [DOI] [PubMed] [Google Scholar]
- 5. Adlam D, Azeem T.. Ventricular fibrillation during electrical cardioversion of pre-excited atrial fibrillation. Postgrad Med J 2003; 79( 931: 297– 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Taylor N. Direct current cardioversion causing ventricular fibrillation in Wolff-Parkinson-White syndrome. Emerg Med Australas 2013; 25( 6: 612– 4. [DOI] [PubMed] [Google Scholar]
- 7. Association for the Advancement of Medical Instrumentation: American national standard for cardiac monitors, heart rate meters, and alarms (EC 13:2002). Arlington (VA): ANSI/AAMI; 2002. Available at: http://pauljbennett.com/pbennett/work/ec13/ec13.pdf. [Google Scholar]
- 8. Barold HS, Wharton JM.. Ventricular fibrillation resulting from synchronized internal atrial defibrillation in a patient with ventricular preexcitation. J Cardiovasc Electrophysiol 1997; 8( 4: 436– 40. [DOI] [PubMed] [Google Scholar]
- 9. Ayers GM, Alferness CA, Ilina M, Wagner DO, Sirokman WA, Adams JM, Griffin JC.. Ventricular proarrhythmic effects of ventricular cycle length and shock strength in a sheep model of transvenous atrial defibrillation. Circulation 1994; 89( 1: 413– 22. [DOI] [PubMed] [Google Scholar]


