Abstract
Introduction
Diarrhoea among children under-five is a serious public health problem in many developing countries, including Nepal. This study aimed to examine the association between health service utilization and diarrhoea management approaches among children under-five years in Nepal.
Methods
The combined 2001, 2006 and 2011 Nepal Demographic and Health Survey (NDHS) data sets were examined and the sample included 2,655 children aged 0–59 months who had diarrhoea 2-weeks prior to the each survey. Multilevel logistic regression analyses that adjust for clustering and sampling weight were used to examine the association between health service utilization and diarrhoea management approaches (Oral Rehydration Solution, increased fluids and/or continued feeding).
Results
The prevalence of extra fluids decreased significantly from 27% in 2001 to 15% in 2011 while that of ORS increased significantly from 32% in 2001 to 40% in 2011. The prevalence of continued feeding fluctuated between 83–89%. Multivariate analysis revealed that caregivers whose children received treatment or advice from health care providers during diarrhoea were 5.78 times more likely to treat diarrhoea with Oral Rehydration Solution (ORS) [adjusted Odds Ratio (aOR) 5.78, 95% confidence interval (CI) 4.50, 7.44], 1.56 (aOR 1.56, 95% CI 1.19, 2.05) times more likely to offer extra fluids, and 2.25 (aOR 2.25, 95% CI 1.50, 3.39) times more likely to use continued feeding than those who did not seek advice.
Conclusions
Our findings indicate that health service utilization significantly improves diarrhoea management among under-five children. However, a broader national diarrhoeal disease control program to further reduce diarrhoea related morbidity and mortality in Nepal should focus on educating caregivers about the importance of the use of ORS as well as increase fluid intake to children under-five years with diarrhoea.
Introduction
Globally, diarrhoea remains a leading cause of under-five mortality and morbidity, particularly in low-and middle-income countries including Nepal [1, 2, 3]. The 2015 global burden of disease study estimated that nearly half a million under-five deaths were caused by diarrhoea, and south Asia (including Nepal) stands second to sub-Saharan Africa with the highest number of these under-five deaths [3].
During the past three decades, international organizations such as World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) have proposed various management approaches for diarrhoea[4]. The first line approaches include: the use of oral rehydration solutions (ORS), increasing fluid intake, use of zinc supplements and continued feeding (including breastfeeding)[4, 5]. The impact of diarrhoeal disease control programs on childhood mortality have been documented in previous studies conducted in Egypt and the Philippines[6, 7]. These studies revealed that the decline in child mortality associated with diarrhoea may be due to increased use of ORS, extra fluids and continued feeding [6, 7], and other research concluded that diarrhoea management approaches are cost effective in reducing the overall burden of diarrhoea [8–14].
In Nepal, the national diarrhoeal disease control program emphasizes the use of the four treatment approaches for childhood diarrhoea; ORS, zinc supplementation, counselling on continued feeding to the caregivers, and the use of extra fluids; which are provided at all levels of the Nepalese health care system [15, 16]. Despite these initiatives, diarrhoea remains a public health concern, particularly in remote regions[17, 18]. Recently, the prevalence estimates for diarrhoea increased from 12% in 2006[19] to 14% in 2011[15]. Almost 50% of Nepalese children who experience diarrhoea do not have access to basic diarrhoea treatment approaches such as ORS or extra fluids[15].
There is substantial variation in uses around ORS, extra fluids and continued feeding as reported in the Nepal Demographic and Health Surveys of 2001, 2006 and 2011[15, 19, 20]. Hence, studies that examine the impact of health service use on ORS, continued feeding and/or extra fluids during childhood diarrhoea would provide important locally-relevant evidence to inform context-specific interventions geared towards reducing diarrhoea-related morbidity and mortality among children under-five years. Therefore, the aim of this study was to examine the association between health service use and diarrhoea management approaches among children aged 0–5 years in Nepal using nationally representative data from the Nepal Demographic and Health Survey (NDHS) for the years 2001, 2006 and 2011. This paper also provide insights into the three main diarrhoeal management approaches used by Nepalese government in order to be able to recommend the changes necessary for the successful implementation of the national diarrheal disease control program.
Methods
Data sources
The present study used nationally representative data from the Nepal Demographic and Health Survey (NDHS) for the period (2001–2011). The present analyses is based on publicly available NDHS datasets collected for the years 2001, 2006 and 2011[21]. Using multi-stage cluster sampling design, all NDHS collected data on various socio-demographic and health indicators including diarrhoea prevalence and its management approaches. The average response of three recent NDHS was 98.2% and the sample represents more than 98% of Nepal’s population. The details of survey methodology, sampling techniques and standard questionnaires are described elsewhere[15, 19, 20].
From 17,714 children aged 0–5 years (N = 6978 in 2001 NDHS[15], N = 5545 in 2006 NDHS[19], and N = 5391 in 2011 NDHS[20]), a sample of 2655 children (n = 1320 in 2001 NDHS, n = 624 in 2006 NDHS, and n = 711 in 2011 NDHS) who had diarrhoea 2 weeks prior the interviews of each survey were identified. The sample population was weighted to adjust for the multi stage cluster sampling effect.
Outcome variables
In the NDHS, if a child had diarrhoea two weeks prior to each survey, mothers were asked how much a child was given to drink (including breastmilk), how much a child was given to eat, and was a child given a fluid made from ORS packets during the diarrhoea. The outcome variables are: (a) use of ORS, (b) use of increased fluids, (c) use of continued feeding (d) combination of all treatment approaches (ORS & extra fluids & continued feeding) and (e) combination of any treatment approaches (ORS or extra fluids or continued feeding) during recent diarrhoeal episodes. If a child had diarrhoea and was given fluid made from ORS packets, it was coded as 1, otherwise 0. If a child had diarrhoea and was given more liquids to drink, it was coded as 1, otherwise 0. If a child had diarrhoea and was given more, same as usual, or somewhat less food, it was coded as 1, otherwise 0.
Exposure variable
The exposure variable of the study was derived from the women’s questionnaire for the section of immunization and health (Did you seek advice or treatment for the diarrhoea from any source?). The exposure variable was coded as 1 if the parents or carer of a child with diarrhoea sought treatment or advice from health care providers (except from pharmacies, shops and traditional practitioners), otherwise coded as 0.
Potential confounding factors
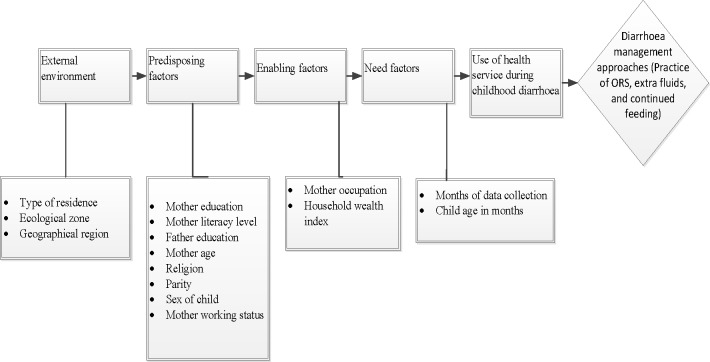
The confounding factors examined in the study were based on the modified Anderson behavioural model[22] to examine the relationship between health service use and diarrhoea management approaches (Fig 1). We analysed 15 key confounding factors and they were classified as: external environment, predisposing factor, enabling factor and need factor. The external environmental factors consisted of: type of residence (Rural and Urban), ecological zone (Mountain, Hill and Terai), and geographical region (Eastern, Central, Western, Mid-Western and Far-Western). Nepal was divided into five Development Regions: Mid-Western, Western, Eastern, Central and Far-Western [15,19,20,23]. The Mid-Western Development Region comprised of three zones (Karnali, Bheri, Rapti) whereas, Western Development Region comprised of three zones (Gandaki. Lumbini, Daulagiri). Similarly, Eastern Development Region and Central Development Region covered three zones (Mechi, Koshi, Sagarmatha) and (Janakpur, Bagmati, Narayani), respectively. Far-Western Development Region only comprised two zones (Seti, Mahakali). Mid-Western, Western, Eastern, Central and Far-Western Development Regions covered 28%, 20%, 19%, 19% and 14%, respectively of the total land of Nepal [15,19,20,23]. The predisposing factors included mother’s current age, mother’s education, mother’s literacy level, father’s education, parity, mother’s religion, and mother’s working status. The enabling factors examined were mother’s occupation, household wealth index and the sex of the child. The household wealth index measures the economic status of the household. We used the wealth index factor scores as calculated by original DHS[15, 19, 20]. The combined original household wealth index factor scores were categorised into three: the bottom, 40% of households was referred to as poor households, the next 40% as the middle households and the top 20% as rich households, consistent with previous studies[24, 25].
Fig 1. Conceptual framework for health service utilization and diarrhoea management approaches among children aged 0–5 years in Nepal, adopted from Anderson behavioural model.
Statistical analysis
As part of the analysis, weighted frequency tabulation and percentage of study variables were first performed for exposure and all confounding factors. This was followed by univariate analyses that independently examined the association of all potential confounding and exposure variables. Multivariate analyses were used to examine the association between health service use and diarrhoea management approaches. As part of the multivariate analyses, staged modelling technique[26] was employed. As a process of staged hierarchical modelling technique, all external environmental factors were first entered into the baseline multivariable model with backward elimination to remove statistically non-significant variables (Model 1). Similarly, in the next stage, predisposing factors were examined with model 1 (Model 2). Next, enabling factors were assessed with model 2 (Model 3). Afterward, need factors were examined with model 3 (Model 4). In the final model (model 5), we examined the use of health service variable with the statistically significant environmental, predisposing, enabling, and need factors identified in the previous model. Variables significantly associated at the 5% significance level with each outcome measure were included in model 5 and reported in the study. We also tested collinearity and reported these findings. The analyses were performed using STATA (version 14.1). The Survey (SVY) function was applied, which allowed for adjustments for sampling weights for cluster sampling. We reported adjusted and unadjusted odds ratios and 95% confidence intervals.
Ethics
The consent statement was read to each respondent in all three surveys and informed verbal consent from each respondent was signed by the interviewer. The Nepal Health Research Council (NHRC) in Kathmandu, Nepal and the ICF Institutional Review Board in Maryland, USA, approved all surveys. The first author sought and obtained permission from Measure DHS/ ICF International to use data as part of his doctoral dissertation within the School of Science and Health at Western Sydney University, Australia.
Results
Of the 2655 children with diarrhoea, only 27% of their caregivers sought treatment or advice from health care providers (Table 1). Of the 27% who sought treatment or advice from the health care providers during diarrhoea, 17% used ORS and sought treatment and 10% sought treatment but did not use ORS. About half (46.5%) of the diarrhoea cases in the study occurred during the high diarrhoea prevalence period (April–August). The majority of children (92%) were rural residents, and 74% were at least two years of age. Nearly half (49%) of the children were from poor socioeconomic households.
Table 1. Characteristics of children under-five years of age with diarrhoea in Nepal, NDHS 2001–2011.
| Study variables | n(%) | Study variables | n(%) |
|---|---|---|---|
| Type of Residence | Parity | ||
| Rural | 2443(92.0) | 6+ | 332(12.5) |
| Urban | 211(8.0) | (4–5) | 505(19.0) |
| Ecological zone | (2–3) | 1144(43.1) | |
| Mountain | 219(8.3) | 1 | 674(25.4) |
| Hill | 1030(38.8) | Sex of child | |
| Terai | 1405(53.0) | Female | 1220(46.0) |
| Geographical region | Male | 1435(54.1) | |
| Central | 948(35.7) | Mother working status (n = 2628) | |
| Eastern | 632(23.8) | Currently working | 1829(68.9) |
| Western | 480(18.1) | Currently not working | 798(31.1) |
| Mid-western | 312(11.8) | Mother occupation (n = 2611) | |
| Far-western | 283(10.7) | Agriculture | 1827(68.8) |
| Mother education | Non- agriculture | 191(7.2) | |
| No education | 1723(64.9) | Not working | 593(23.3) |
| Primary | 442(16.7) | Household wealth index | |
| Some secondary to higher | 489(18.4) | Poor | 1300(49.0) |
| Mother literacy level (n = 2651) | Middle | 577(21.7) | |
| Cannot read at all | 1567(59.0) | Rich | 777(29.3) |
| Able to read | 1084(40.8) | Months of data collection | |
| Father education | January- March | 1420(53.5) | |
| No education | 1288(48.5) | April- August | 1235(46.5) |
| Primary | 869(32.7) | Child age in months | |
| Some secondary to higher | 498(18.7) | (0–11) | 690(26.0) |
| Mother age | (12–23) | 819(30.9) | |
| 30–49 | 787(39.6) | (24–59) | 1145(43.1) |
| 20–29 | 1662(62.6) | Use of health service during diarrhoea | |
| <20 | 206(7.8) | No | 1937(73.0) |
| Religion | Yes | 718(27.0) | |
| Buddhist | 218(8.2) | ||
| Hindu | 2166(81.6) | ||
| Others | 271(10.2) |
n: Weighted counts. Other religion Includes mainly Christian, Muslims and Kirat; Non-agriculture occupation includes skilled and professional jobs; Counts and percentages vary between categories because of missing values.
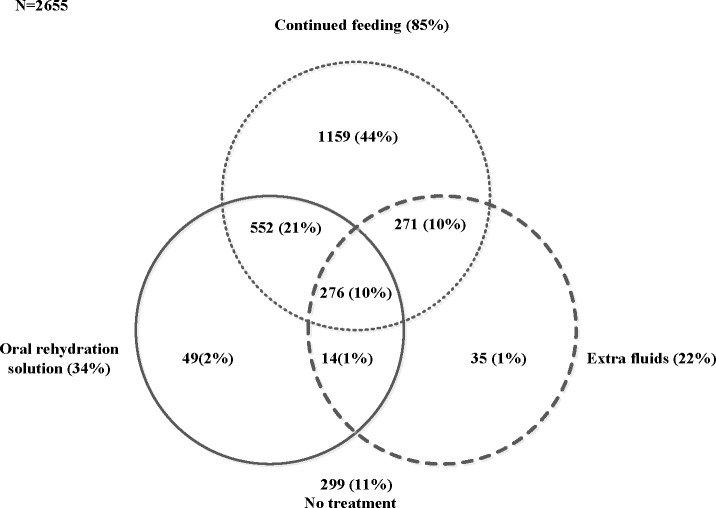
The Venn diagram shows all the three treatment approaches in Nepal, 2001–2011 (Fig 2). In the figure, 21%, 10% and 1% of children aged 0–59 months were given ORS and continued feeding, continued feeding and extra fluids, and ORS and extra fluids, respectively. 10% of children were given ORS, extra fluids and continued feeding and 11% of children did not use any of three treatment approaches.
Fig 2. Number and percentage of children who received ORS, continued feeding and/or extra fluids during diarrhoea in Nepal (2001–2011).
Trends in diarrhoea management approaches
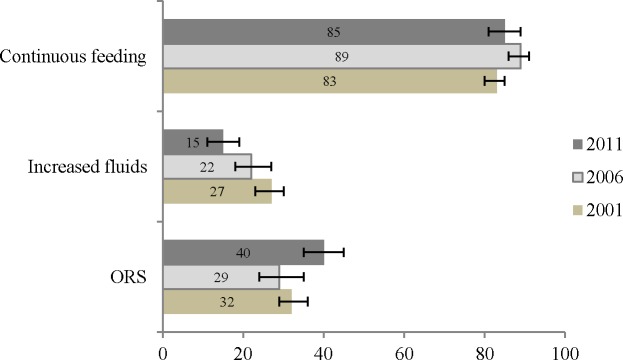
We found that the prevalence of ORS use increased significantly from 29% in 2006 to 40% in 2011, whereas the use of extra fluids decreased significantly from 27% in 2001 to 15% in 2011 (Fig 3). Over the 10 years, the prevalence of continued feeding fluctuated from between 83% in 2001, 89% in 2006, and 85% in 2011, and the prevalence of continued feeding significantly increased by 6% in 2006 compared to 2001, and a non-statistically significant reduction of 4% in 2011 compared to 2006.
Fig 3. Trends in prevalence of Oral Rehydration Solution (ORS), increased fluids, and continued feeding during childhood diarrhoea in Nepal (2001–2011).
Univariate and multivariate logistic analyses
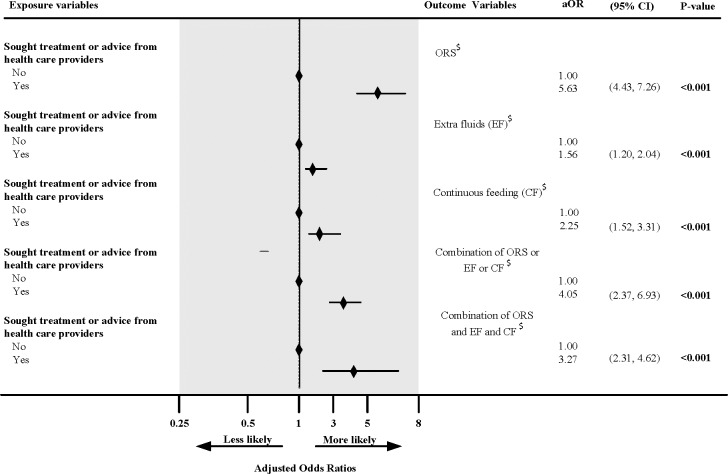
Univariate analyses revealed that caregivers who sought treatment or advice from the health care providers were significantly more likely to use at least one the three prescribed approaches, ORS or extra fluids or continued feeding (OR 3.64, 95% CI 2.24, 5.90) for the treatment of childhood diarrhoea compared to those who did not seek treatment or advice from the health care providers (S1 Table). We also found increasing use of all approaches, ORS (OR 5.48, 95% CI 4.36, 6.88), extra fluids (OR 1.67, 95% CI 1.30, 2.15), continued feeding (OR 2.04, 95%CI 1.49, 2.80) among caregivers who sought treatment or advice from health care providers compared to those who did not seek treatment or advice from health care providers. This result was also found for the combination of all treatment approaches, ORS and extra fluids and continued feeding (OR 3.44, 95% CI 2.52, 4.72). These results remained significant in the adjusted model: ORS or extra fluids or continued feeding (aOR 4.05, 95% CI 2.37, 6.93), ORS (aOR 5.63, 95% CI 4.43, 7.26), extra fluids (aOR 1.56, 95% CI 1.20, 2.04), continued feeding (aOR 2.25, 95% CI 1.52, 3.31), ORS and extra fluids and continued feeding (aOR 3.27, 95% CI 2.31, 4.62) (Fig 4).
Fig 4. Impact of health service use on diarrhoea treatment approaches among children aged 0–59 months in Nepal (2001–2011).
$Adjusted for type of residence, ecological zone, geographical region, mother education, mother literacy level, father education, mother age, religion, parity, sex of child, mother working status, mother occupation, household wealth, months of data collection, age of child, and use of health service during diarrhoea.
There were several socio-demographic variables that were important determinants of use of the management approaches, including geographical area of residence, maternal education, paternal education, and household wealth index. The use of all treatment approaches was significantly higher among mothers residing in the eastern geographical region (aOR 1.88, 95% CI 1.09, 3.26) compared to mothers residing in the central geographical region, mothers with primary education (aOR 1.48, 95% CI 1.00, 2.19) or secondary to higher education (aOR 2.93, 95% CI 1.86, 4.63) compared to uneducated mothers, fathers with primary education (aOR 1.55, 95% CI 1.11, 2.17) or secondary to higher education (aOR 1.58, 95% CI 1.01, 2.49) compared to uneducated fathers, and the family with middle household wealth index (aOR 2.25, 95% CI 1.53, 3.32) or rich household wealth index (aOR 1.63, 95% CI 1.02, 2.60) compared to the family with poor household wealth index. Among mothers who reported childhood diarrhoea, the majority (24%) of the illiterate women were from Central Geographical Region compared to 14% in Eastern, 7% in Mid-western, 6% in Far-western, and 8% in Western Geographical Region.
Discussion
Despite the established benefits of using ORS, extra fluids and continued feeding as strategies to reduce mortality and morbidity from diarrhoea [6, 7, 11], optimal management is still not universally adopted in Nepal. Our study found that caregivers who sought treatment or advice from the health care providers were more likely to use treatment approaches (ORS, extra fluids and/or continued feeding) for childhood diarrhoea compared to those who did not seek treatment or advice from the health care providers.
The knowledge of ORS is almost universal in Nepal [27, 20]. However, this study found that the aggregate prevalence of ORS was about one-third whereas approximately a quarter of the sample reported extra fluids. The difference between knowledge and practice may be as a result of socio-cultural values related to help seeking for childhood illness and different ethnical views about causes and consequences of diarrhoea which prevented mothers from accessing modern healthcare for management of diarrhoea[28]. Similarly, the study conducted in a rural part of Nigeria reported that large improvements in knowledge of Oral Rehydration Therapy (ORT) from about 6 to 47 percent did not translate into practice with only 10 percent using ORT during diarrhoeal episodes[29]. The gap between knowledge and ORS use was also reported in hospital based studies in India, and a hospital based cross-sectional study in Pakistan [30–32]. These studies recommended that community outreach programs[30], widespread health education for mothers[31], and awareness programs around diarrhoea management approaches can bridge the knowledge and practice gap among mothers.
Our study found that attending a health service improved the management of diarrhoea (Fig 4). We found a strong association between health service utilization and the use of ORS, extra fluids and/or continued feeding during diarrhoea treatment. This finding is similar to a study conducted in a poor neighbourhood in Nicaragua[33] which reported that that ORS use was significantly associated to health service utilization. The authors concluded that mothers did not use ORS until they visited the health professional. A study conducted in Uganda by Nanyonjo et al [34] revealed that Integrated Community Case Management attendance for diarrhoea was associated with ORS use. It is useful to note that studies from developing countries including Nepal have documented some beliefs such as high fluid intake worsened diarrhoea, children with diarrhoea should be given only water due to teething, some forms of diarrhoea require traditional methods like exorcism, and intensity of diarrhoea is decreased with food restriction [28, 35–37]. These beliefs might have negatively affected the management of diarrhoea. Hence, knowledge, attitude and practice, which are deeply rooted into local cultural values and norms, appear to be important and health professionals can change cultural beliefs and improve knowledge about the use of diarrhoea treatment approach. For example, health care workers proving information to caregivers were found to improve the use of ORS and extra fluids as indicated in a study conducted in Ethiopia[38]. The government of Nepal policy to provide counselling on continued feeding during diarrhoea while patients are sought treatment or advice from health care providers may have contributed for the significant role for patient’s adherence to continued feeding[15]. Hence, widespread heath education for caregivers as well as awareness programs to improve knowledge, attitude and practice could bridge the widening gap and motivate caregivers to use recommended treatment approaches during diarrhoea. Past studies [34, 38, 39] have also suggested that a proper interaction between health worker and patient/care giver is crucial to improve the rate of treatment use and recovery. These findings suggest the need for educating family members particularly, mothers, their husbands and mother in-law about the importance and how to adequately use complementary and ORS to the children during diarrhoea.
Our study found that caregivers of children aged 0–59 months who received treatment or advice from health care provider reported higher odds of practicing ORS compared to other diarrhoea management approaches (extra fluids, continued feeding, combination of ORS & extra fluids & continued feeding, and combination of ORS or extra fluids or continued feeding). This finding was supported by a recent systematic review that estimated the effectiveness of ORS on diarrhoea mortality and the study concluded that ORS is more effective in reducing mortality related childhood diarrhoea in home, community and facility settings[11].
The major strengths of this study include the use of a nationally representative pooled sample, with an average response of 97%, use of standardised survey questionnaires, and the adjustment for the cluster sampling design with sampling weight. However, findings from this study do not accurately capture changes in diarrhoea management in Nepal as the Nepalese government introduced zinc in the treatment protocol for the management of childhood diarrhoea in 2007. We could not retain the use of the zinc variable into our pooled study because NDHS 2001 had no zinc related data. Similarly, the use of antibiotics or other medicine, an important confounder was excluded from this study due to no observations recorded in 2001 NDHS dataset.
Conclusions
Our study concludes that caregivers of children aged 0–59 months of age are more likely to adhere with all three treatment approaches if they seek care or advice from health care providers. However, community based complete intervention packages such as the use of ORS, extra fluids and continued feeding are needed to further manage childhood diarrhoea in Nepal and such intervention should target caregivers of children from low socioeconomic disadvantaged group.
Supporting information
(DOCX)
Acknowledgments
The authors are grateful to Measure DHS, ICF International, Rockville, Marylands, USA for providing all the three NDHS data for this analysis.
Data Availability
The data underlying this study belong to the Demographic and Health Surveys (DHS) Program. The data can be accessed using the following link: https://www.dhsprogram.com/data/available-datasets.cfm. The authors did not have any special access privileges that others would not have.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Santosham M, Chandran A, Fitzwater S, Fischer-Walker C, Baqui AH, Black R. Progress and barriers for the control of diarrhoeal disease. The Lancet. 2010. July 3; 376: 63–7. doi: 10.1016/S0140-6736(10)60356-X [DOI] [PubMed] [Google Scholar]
- 2.Walker CL, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta ZA, et al. Global burden of childhood pneumonia and diarrhoea. The Lancet. 2013. April 12; 381: 1405–16. doi: 10.1016/S0140-6736(13)60222-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collaborators, Global Burden of Diseases. Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: A systematic analysis for the global burden of disease study. The Lancet Infectious Diseases. 2017. June 1 http://dx.doi.org/10.1016/.S1473-3099(17)30276-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UNICEF. Pneumonia and diarrhoea: tackling the deadliest diseases for the world’s poorest children. New York: UNICEF; 2014. June. [Google Scholar]
- 5.The World Health Organization. The treatment of diarrhoea: a manual for physicians and other senior health workers, 2005.
- 6.Baltazar JC, Nadera DP, Victora CG. Evaluation of the national control of diarrhoeal disease programme in the philippines, 1980–93. Bulletin of World Health Organization. 2002. August; 80: 637–643. [PMC free article] [PubMed] [Google Scholar]
- 7.Miller P, Hirschhorn N. The effect of a national control of diarrheal diseases program on mortality: the case of Egypt. Social Science and Medicine.1995. May; 40, S1–S30. [DOI] [PubMed] [Google Scholar]
- 8.Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? The Lancet. 2013. August 9; 382: 452–477. doi: 10.1016/S0140-6736(13)60996-4 [DOI] [PubMed] [Google Scholar]
- 9.Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS, Bellagio Child Survival Study Group. How many child deaths can we prevent this year? The Lancet. 2003. July 5; 362: 65–71, doi: 10.1016/S0140-6736(03)13811-1 [DOI] [PubMed] [Google Scholar]
- 10.Bhutta ZA, Das JK, Walker N, Rizvi A, Campbell H, Rudan I et al. Interventions to address deaths from childhood pneumonia and diarrhoea equitably: what works and at what cost? The Lancet. 2013. April 26; 381: 1417–1429, doi: 10.1016/S0140-6736(13)60648-0 [DOI] [PubMed] [Google Scholar]
- 11.Munos MK, Walker CLF, Black RE. The effect of oral rehydration solution and recommended home fluids on diarrhoea mortality. International Journal of Epidemiology. 2010. March 23; 39: i75–i87. doi: 10.1093/ije/dyq025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duggan C, Nurko S. Feeding the gut: the scientific basis for continued enteral nutrition during acute diarrhea. The Journal of Pediatrics. 1997. December 1; 131: 801–808. [DOI] [PubMed] [Google Scholar]
- 13.Nel E. Diarrhoea and malnutrition. South African Journal of Clinical Nutrition. 2010. January 1; 23: 15–18. [Google Scholar]
- 14.Rohde J, Northrup R. Diarrhea is a nutritional disease. Indian pediatrics. 1988; 25: 914–929. [PubMed] [Google Scholar]
- 15.Ministry of Health and Population (MOHP) [Nepal], New ERA, ICF International Inc. 2012. Nepal Demographic and Health Survey 2011. Kathmandu, Nepal: Ministry of Health and Population, New ERA, and ICF International, Calverton, Maryland.
- 16.Ghimire M, Pradhan YV, Maskey MK. Community-based interventions for diarrhoeal diseases and acute respiratory infections in nepal. Bulletin of the World Health Organization. 2010. March; 88: 216–221. doi: 10.2471/BLT.09.065649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhandari G, Bhusal C. Cholera outbreak in far-western region of nepal. Journal of Nepal Health Research Council. 2013. May 10; 11: 6–8. [PubMed] [Google Scholar]
- 18.International Federation of Red Cross and Red Crescent Socities. Diarrhoea outbreak kills hundreds, 2009. Available from: http://www.ifrc.org/en/nouvelles/nouvelles/asia-pacific/nepal/nepal-diarrhoea-outbreak-kills-hundreds/.
- 19.Ministry of Health and Population (MOHP) [Nepal], New ERA, and Macro International Inc. 2007. Nepal Demographic and Health Survey 2006. Kathmandu, Nepal: Ministry of Health and Population, New ERA, and ICF International, Calverton, Maryland.
- 20.Ministry of Health [Nepal], New ERA, and ORC Macro. 2002. Nepal Demographic and Health Survey 2001. Calverton, Maryland, USA: Family Health Division, Ministry of Health; New ERA; and ORC Macro.
- 21.The Demographic and health survey. Available from: http://dhsprogram.com/data/available-datasets.cfm. Accessed 10 March 2013.
- 22.Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior.1995. March 1; 36: 1–10. [PubMed] [Google Scholar]
- 23.Gurung H, Nepal Regional Strategy for Development. 2005 [Google Scholar]
- 24.Agho KE, Dibley MJ, Odiase JI, Ogbonmwan SM. Determinants of exclusive breastfeeding in nigeria. BMC Pregnancy and Childbirth 2011. January 11; 11: 2 doi: 10.1186/1471-2393-11-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghimire PR, Agho KE, Renzaho A, Christou A, Nisha MK, Dibley M et al. Socio-economic predictors of stillbirths in nepal (2001–2011). PloS One. 2017. July 13; 12: e0181332, doi: 10.1371/journal.pone.0181332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Victora CG, Huttly SR, Fuchs SC, Olinto M. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. International Journal of Epidemiology. 1997. February 1; 26: 224–227. [DOI] [PubMed] [Google Scholar]
- 27.Jha N, Singh R, Baral D. Knowledge, attitude and practices of mothers regarding home management of acute diarrhoea in Sunsari, Nepal. Nepal Medical College Journal. 2006. March; 8: 27–30. [PubMed] [Google Scholar]
- 28.Ansari M, Ibrahim MIM, Hassali MA, Shankar PR, Koirala A,Thapa NJ. Mothers’ beliefs and barriers about childhood diarrhea and its management in Morang district, Nepal. BMC Research Notes. 2012. October 24; 5: 576 doi: 10.1186/1756-0500-5-576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jinadu MK, Olusi S, Alade O, Ominiyi C. Effectiveness of primary health-care nurses in the promotion of oral rehydration therapy in a rural area of nigeria. International Journal of Nursing Studies. 1988. January 1; 25: 185–190. [DOI] [PubMed] [Google Scholar]
- 30.Pahwa S, Kumar GT, Toteja GS. Performance of a community-based health and nutrition-education intervention in the management of diarrhoea in a slum of delhi, India. Journal of Health, Population, and Nutrition. 2010. December; 28: 553–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Datta V, John R, Singh VP, Chaturvedi P. Maternal knowledge, attitude and practices towards diarrhea and oral rehydration therapy in rural maharashtra. Indian Journal of Pediatrics. 2001. November 1; 68: 1035–7. [DOI] [PubMed] [Google Scholar]
- 32.Masiha SA, Khalid A, Malik B, Shah SMA. Oral rehydration therapy-knowledge, attitude and practice (kap) survey of pakistani mothers. J. Rawal Med. Coll. 2015; 19: 51–54. [Google Scholar]
- 33.Hudelson PM. ORS and the treatment of childhood diarrhea in managua, Nicaragua. Social Science and Medicine. 1993. July 1; 37: 97–103. [DOI] [PubMed] [Google Scholar]
- 34.Nanyonjo A, Ssekitooleko J, Counihan H, Makumbi F, Tomson G, Källander K. Impact of an integrated community case management programme on uptake of appropriate diarrhoea and pneumonia treatments in uganda: a propensity score matching and equity analysis study. International Journal for Equity in Health 2015. September 4; 14: 74 doi: 10.1186/s12939-015-0202-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Olango P, Aboud F. Determinants of mothers' treatment of diarrhea in rural ethiopia. Social Science and Medicine. 1990. January 1; 31: 1245–1249. [DOI] [PubMed] [Google Scholar]
- 36.Kumar V, Clements C, Marwah K, Diwedi P. Beliefs and therapeutic preferences of mothers in management of acute diarrhoeal disease in children. Journal of Tropical Pediatrics. 1985. April 1; 31: 109–12. [DOI] [PubMed] [Google Scholar]
- 37.Pokhrel D, Viraraghavan T. Diarrhoeal diseases in Nepal vis-à-vis water supply and sanitation status. Journal of Water and Health. 2004. June 1; 2: 71–81. [PubMed] [Google Scholar]
- 38.Mengistie B, Berhane Y, Worku A. Predictors of oral rehydration therapy use among under-five children with diarrhea in eastern ethiopia: a community based case control study. BMC public health. 2012. November 24; 12: 1029 doi: 10.1186/1471-2458-12-1029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Olson CK, Blum LS, Patel KN, Oria PA, Feikin DR, Laserson KF, et al. Community case management of childhood diarrhea in a setting with declining use of oral rehydration therapy: findings from cross-sectional studies among primary household caregivers, kenya, 2007. The American Journal of Tropical Medicine and Hygiene. 2011. December 1; 85: 1134–1140. doi: 10.4269/ajtmh.2011.11-0178 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
The data underlying this study belong to the Demographic and Health Surveys (DHS) Program. The data can be accessed using the following link: https://www.dhsprogram.com/data/available-datasets.cfm. The authors did not have any special access privileges that others would not have.