Abstract
In low and middle income countries (LMICs), where the burden of neonatal sepsis is the highest, the spread of extended spectrum beta-lactamase-producing enterobacteriaceae (ESBL-PE) in the community, potentially contributing to the neonatal mortality, is a public health concern. Data regarding the acquisition of ESBL-PE during the neonatal period are scarce. The routes of transmission are not well defined and particularly the possible key role played by pregnant women. This study aimed to understand the neonatal acquisition of ESBL-PE in the community in Madagascar. The study was conducted in urban and semi-rural areas. Newborns were included at birth and followed-up during their first month of life. Maternal stool samples at delivery and six stool samples in each infant were collected to screen for ESBL-PE. A Cox proportional hazards model was performed to identify factors associated with the first ESBL-PE acquisition. The incidence rate of ESBL-PE acquisition was 10.4 cases/1000 newborn-days [95% CI: 8.0–13.4 cases per 1000 newborn-days]. Of the 83 ESBL-PE isolates identified, Escherichia coli was the most frequent species (n = 28, 34.1%), followed by Klebsiella pneumoniae (n = 20, 24.4%). Cox multivariate analysis showed that independent risk factors for ESBL-PE acquisition were low birth weight (adjusted Hazard-ratio (aHR) = 2.7, 95% CI [1.2; 5.9]), cesarean-section, (aHR = 3.4, 95% CI [1.7; 7.1]) and maternal use of antibiotics at delivery (aHR = 2.2, 95% CI [1.1; 4.5]). Our results confirm that mothers play a significant role in the neonatal acquisition of ESBL-PE. In LMICs, public health interventions during pregnancy should be reinforced to avoid unnecessary caesarean section, unnecessary antibiotic use at delivery and low birth weight newborns.
Introduction
Since 2000, the number of neonatal deaths has decreased from 3.9 million to 2.7 million [1]. Nevertheless, this decline has been slower than the post-neonatal under-five mortality [2] and significant improvements in neonatal health still have to be achieved. Bacterial infections are a leading cause of neonatal deaths in countries with very high under five mortality rate [3,4]. In 2014, it has been estimated that 6.9 million cases of neonatal possible severe bacterial infection (pSBI) occurred in low or middle-income countries (LMICs) [5].
In LMICs, neonatal infections are mainly caused by Enterobacteriaceae, more specifically Escherichia coli and Klebsiella pneumoniae [6,7]. One important driver of unfavorable outcome in infections caused by these bacteria is multidrug resistance which challenges appropriate therapy [8]. Of particular concern, the extended-spectrum beta-lactamase-producing enterobacteriaceae (ESBL-PE), are the most frequently isolated multidrug resistant bacteria [6,9–11]. First reported in hospital settings, ESBL-PE emerged in the community since the early 2000s [12]. ESBL-PE are resistant to beta-lactams and cephalosporins [13]. Carbapenems remain the last resort to treat pediatric ESBL-PE infections which is onerous and often unavailable in LMICs [14–16].
Enterobacteriaceae are known to colonize the digestive tract [17]. After birth, the intestinal tract of newborns is colonized by the maternal and environment flora [18] which represents the first step for potential neonatal infections [19]. However, data regarding the acquisition of ESBL-PE during the neonatal period are scarce [20]. Bacteria that first colonize the neonatal gut are from different sources (maternal, health-care facilities, community) and the routes of transmission are not well defined [21].The maternal carriage of ESBL-PE is likely to play a significant role in the colonization and/or infection of newborns in the first week of life [22].
In Madagascar, a recent study among pregnant women at delivery in the community showed a significant prevalence (18.5%) of ESBL-PE carriage, and one strain of Klebsiella pneumoniae isolated was a New Delhi metallo-beta-lactamase-1 producer, indicating that pregnant women may represent a substantial source for transmission of multiresistant Enterobacteriaceae to neonates [23].
The aim of this study was to understand the neonatal acquisition of ESBL-PE colonization in the community in Madagascar.
Methods
The study was reviewed and approved by the Ethics Committee of the Malagasy Public Health Ministry (no. 113-MSANP/CE 03 November 2014) before the study began and was authorized by the Institut Pasteur in Paris. Written informed consents were obtained from all participants.
Study design
This study was nested within the BIRDY program (“Bacterial Infections and antibiotic Resistant Diseases among Young children in low income countries”, http://www.birdyprogram.org). The study design of the BIRDY program has already detailed elsewhere [24]. Briefly, the present study took place between October 1st, 2015 and September 30th, 2016 in two distinct areas in Madagascar: an urban area, Antananarivo, and a semi-rural area, Moramanga (110 km east from Antananarivo) (Fig 1). All pregnant women of the study areas were identified and were enrolled in the study during their third trimester of pregnancy. An active monitoring of the pregnant women was conducted to ensure the enrollment of neonates at birth.
Fig 1. Study areas.

The mother’s sociodemographic, medical and obstetric characteristics and delivery information were also collected as well as the newborn’s anthropometric measurements and APGAR score.
Newborns were included at birth and systematic home visits were planned twice in the first week of life; the first visit occurring within three days after delivery and then weekly in the first month (day 0, day 3, day 7, day 14, day 21 and day 28). At each visit, stools sample or endorectal swabs were collected. We recorded using standardized questionnaires orally administered to the mothers factors potentially associated with the risk of ESBL-PE acquisition, including habitat type, number of rooms, number of household members, parity, diet and hygiene habits, contact with animals, animal ownership, animal husbandry, hospitalization and consumption of antibiotics in the previous days, latrines [12,25–28].
Maternal fresh stools were collected at delivery or shortly after delivery in case of home delivery to detect ESBL-PE. Six stools samples or endorectal swabs from the newborns were obtained during the first month of life starting with the meconium when available, then 2 others during the first week and weekly for the 3 remaining weeks of the first month of life. In case of hospitalization of the newborn, a sample was taken at the entrance and every 7 days during hospitalization. Another sample was taken before discharge from the hospital if hospitalization was less than 7 days.
Microbiological analysis
All samples were analyzed in the laboratory of Experimental Bacteriology unit at the Institut Pasteur in Madagascar. If stools were collected, 1g of sample was suspended in 9ml of physiologic water and dilution in 1/10 was prepared. If endorectal swabs were collected, the swab was suspended in 1ml of physiologic water then vortexed.
Samples were cultivated on CHROMagar ESBL (CHROMagar, Paris, France). The presence of ESBLs in isolates was confirmed by the double-disk synergy test (DDST) [29]. DDST was performed by placing the disk of cefotaxime (30 μg), ceftazidime (30 μg), and combination of amoxicillin/clavulanic acid (20 μg/10 μg) on a lawn culture of bacteria on Muller-Hinton agar plate, with a 20 mm distance between each disk from center to center. Then, plates were incubated at 37°C for 18–24 hrs. Enhancement of the inhibition zone between the disks containing clavulanic acid and cefotaxime or ceftazidime indicated the presence of ESBL production. E. coli ATCC 25922 and K. pneumoniae ATCC 700603 were used as internal quality control strains. Each colony morphotype was identified by mass spectrometry MALDI-TOF, Bruker. Antimicrobial susceptibility testing was performed on each isolate. Amoxicillin, ticarcillin, ticarcillin-clavulanic acid, cefalotin, amoxicillin-clavulanic acid, aztreonam, cefotaxim, ceftazidime, cefepime, imipenem, ertapenem, cefoxitin, cefuroxim, gentamicin, nalidixic acid, ciprofloxacin were tested. The phenotype interpretation was done according to the Antibiogram Committee of the French Society of Microbiology (CA-SFM) guidelines 2015[29].
Statistical analysis
Stata version no.14 (Stata Corp., College Station, TX) was used for all statistical analyses. Differences in proportions and means were compared using the chi2 and the student test, respectively. A P -value of < 0.05 was considered statistically significant.
We made the assumption that at birth the newborn gut was not colonized by ESBL-PE [18,30]. Also, newborns that had their first sample after the 2 first weeks of life were not included in the survival analysis [31]. We defined low birth weight (LBW) as a birth weight under 2500 g.
Our primary outcome was defined as the first acquisition of ESBL-PE occurring during the first month of life of the newborn; follow-up was thus censored after the first month, or at the date of death, date of withdrawal, or date of last visit for the newborns lost to follow-up, whichever occurred first. We calculated incidence rates of the first acquisition of ESBL-PE per 1000 newborn-days. The ESBL-PE acquisition curves were obtained by the Kaplan–Meier method and compared using the log-rank statistic. To identify factors associated with the first ESBL-PE acquisition, we used a Cox proportional hazard model. We considered variables potentially associated with ESBL-PE acquisition, such as maternal ESBL-PE colonization, antibiotic consumption, and hygiene.
For all factors included in the Cox model, the proportional hazard assumption was validated using a test on Schoenfeld residuals. All factors associated with the outcome with a P-value <0.20 in univariate analysis were entered in the multivariate model. A backward selection procedure was applied to identify factors independently and significantly associated with the outcome. We also tested an interaction between maternal ESBL-PE colonization and cesarean delivery; and antibiotic per-partum, respectively. A P-value <0.05 was considered significant.
Results
Characteristics of the study population
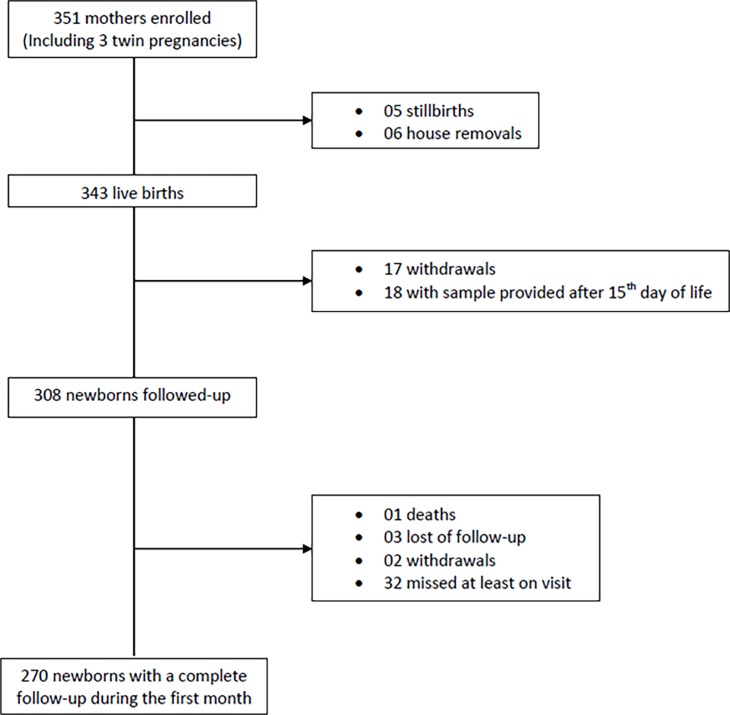
Of the 351 pregnant women included in the study, 340 gave birth to 343 live newborns who were included in the study (Fig 2). At the end of the study, the mean number of visits was 4.96 (standard-deviation (SD) = 0.04) and 270 newborns had a complete follow-up.
Fig 2. Flow-chart of the study participants.
Among the 1755 samples collected in neonates, 678 (39%) were stool samples and 1077 (61%) were endorectal swabs. And among the 275 maternal samples, 177 (64%) were stool samples and 98 (36%) were endorectal swabs.
Table 1 presents the general characteristics of the mothers and newborns. On average, mothers were 27.5 years of age (range 26.8–28.2), 29.1% were primigravidae. More than one-half (54.7%) attended to partial secondary school and more than two third (67.4%) were unemployed. More than 90% used outside toilets and more than one quarter (25.6%) did not have access to electricity. A total of 153 (44.6%) pregnant women gave birth at home. Of the 343 newborns included in the study, 48.1% were male. Their mean birth weight was 3067.6 g (SD = 23.8, range: [1610–4200]); and 7.3% of them had a low birth weight. Among the 308 newborns followed-up, eleven (3.6%) were hospitalized and 5 (1.6%) took antibiotics during their first month of life. Of the 275 mothers with collected stool samples, 54 (19.6%) were colonized with ESBL-PE. The majority were Escherichia coli (n = 28, 49.1%) and Klebsiella pneumoniae (n = 6, 10.5%) S1 Table.
Table 1. Characteristics of the mothers and newborns.
| Total | Urban area | Semi-urban area | Pa | |
|---|---|---|---|---|
| Mothers | 340 (100) | 103 (30.3) | 237 (69.7) | |
| Age | n (%) | n (%) | n (%) | |
| Mean (SDb) | 27.5 (6.5) | 26.7 (5.8) | 27.9 (6.7) | 0.5 |
| Median (IQRc) | 26 (23; 32) | 25 (23; 29) | 26 (23; 32) | |
| Marital status | ||||
| Single or divorced | 18 (5.3) | 2 (1.9) | 16 (6.8) | 0.1 |
| Married or consensual union | 322 (94.7) | 101 (98.1) | 222 (93.3) | |
| ESBL colonisation | 275 (100) | 77 (28) | 198 (72) | 0.7 |
| Yes | 54 (19.6) | 16 (20.8) | 38 (19.2) | |
| No | 221 (80.4) | 61 (79.2) | 160 (80.8) | |
| Education | ||||
| No education or primary | 77 (22.7) | 18 (17.5) | 59 (24.9) | 0.1 |
| Partial secondary | 186 (54.7) | 56 (54.4) | 130 (54.9) | |
| Complete secondary or University | 77 (22.6) | 29 (28.1) | 48 (20.2) | |
| Parity | ||||
| Primigravidae | 99 (29.1) | 33 (32.0) | 66 (27.9) | 0.4 |
| Multigravidae | 241 (70.9) | 70 (68.0) | 171 (72.1) | |
| Toilets facilities | ||||
| Inside access | 24 (7.1) | 13 (12.6) | 11 (4.6) | 0.008 |
| Outside access | 316 (92.9) | 90 (87.4) | 226 (95.4) | |
| Electricity access | ||||
| Yes | 253 (74.4) | 89 (86.4) | 164 (69.2) | 0.001 |
| No | 87 (25.6) | 14 (13.6) | 73 (30.8) | |
| Profession | ||||
| Unemployed | 229 (67.4) | 63 (61.2) | 166 (70.0) | 0.06 |
| Manual employment | 101 (29.7) | 34 (33.0) | 67 (28.3) | |
| Office jobs | 10 (2.9) | 6 (5.8) | 4 (1.7) | |
| Person who followed pregnancy | ||||
| No follow-up | 10 (2.9) | 2 (1.9) | 8 (3.4) | 0.9 |
| Traditional birth attendant | 7 (2.1) | 2 (1.9) | 5 (2.1) | |
| Health care workerd | 323 (95.0) | 99 (96.2) | 224 (94.5) | |
| Newborns | 343 (100) | 105 (30.6) | 238 (69.4) | |
| Sex | ||||
| Male | 165 (48.1) | 52 (49.5) | 113 (47.5) | 0.7 |
| Place of delivery | ||||
| Health care center | 190 (55.4) | 74 (70.5) | 116 (48.7) | >0.001 |
| Home | 153 (44.6) | 31 (29.5) | 122 (51.3) | |
| Cesarean delivery | ||||
| Yes | 29 (8.5) | 17 (16.2) | 12 (5.0) | 0.001 |
| No | 314 (91.5) | 88 (83.8) | 226 (95.0) | |
| Difficult birth | ||||
| Yes | 25 (7.3) | 13 (12.4) | 12 (5.0) | 0.016 |
| No | 318 (92.7) | 92 (87.6) | 226 (95.0) | |
| Weight at delivery (gr) | 329 (100) | 101 (30.7) | 228 (69.3) | |
| < 2500 | 24 (7.3) | 15 (14.9) | 9 (3.9) | >0.001 |
| > = 2500 | 305 (92.7) | 86 (85.1) | 219 (96.1) | |
| Hospitalization during the first month of life | 308 (100) | 89 (28.9) | 219 (71.1) | |
| No | 297 (96.4) | 82 (92.1) | 215 (98.2) | 0.01 |
| Yes | 11 (3.6) | 7 (7.9) | 4 (1.8) | |
| Antibiotics intake during the first month of life | 308 (100) | 89 (28.9) | 219 (71.1) | |
| No | 303 (98.4) | 88 (98.9) | 215 (98.2) | 1 |
| Yes | 5 (1.6) | 1 (1.1) | 4 (1.8) |
ap, p-value
bSD, Standard deviation
cIQR, Interquartile range.
dHealth care worker: a doctor, a midwife or a nurse.
ESBL-PE acquisition in newborns
A total of 83 ESBL-PE isolates were identified during the follow-up. Escherichia coli was the most frequent species (n = 28, 34.1%), followed by Klebsiella pneumoniae (n = 20, 24.4%). Eleven strains remained unidentified. When we considered the first acquisition only (n = 55), Escherichia coli and Klebsiella pneumoniae remained the most prevalent pathogens (n = 17, 30.9% and n = 14, 25.5%, respectively) (see S2 and S3 Tables). Overall, thirty five newborns were excluded from the survival analysis (18 with sample provided after 15th day of life, 17 withdrawls (Fig 2). There was no statistical difference between the characteristics of these newborns and those included in the survival analysis.
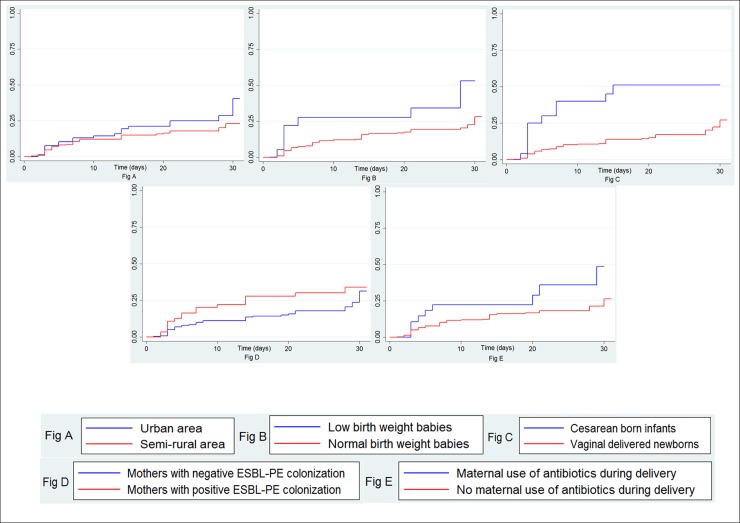
The overall incidence of ESBL-PE first acquisition was 10.4 per 1000 newborn-days [95% confident interval (CI) = 8.0; 13.4]. The incidences were 13.7 [8.8; 21.3] and 9, 2 [6.7; 12.7] in the urban and semi-rural areas, respectively. We did not find any difference in the incidence of acquisition between the urban and semi-rural areas (log rank test, p = 0.22). ESBL-PE acquisition curves according to study areas, newborn’s weight, mode of delivery, maternal ESBL-PE colonization status and antibiotics use during delivery are shown in Fig 3A, Fig 3B, Fig 3C, Fig 3D and Fig 3E, respectively. In univariate Cox analysis (Table 2), cesarean-born babies (Hazard-ratio (HR) = 3.5, 95% CI [1.7; 6.8]) or newborn from a mother who received an antibiotic during delivery (HR = 2.1, 95% CI [1.0; 4.2]) were at higher risk of ESBL-PE acquisition than vaginally born babies or newborn from a mother who did not receive an antibiotic during delivery, respectively. Compared to babies born from a mother not colonized with ESBL-PE, children born from an ESBL-PE colonized mother had an increased risk of acquiring ESBL-PE (HR = 1.7, 95% CI [1.0; 3.0]). Low birth weight was significantly associated with a higher risk of ESBL-PE acquisition (HR = 2.6, 95% CI [1.2; 5.5]) compared to normal weight babies at birth.
Fig 3.
Cumulative incidencesaccording to study areas (Fig 3A), newborn’s weight at birth (Fig 3B), mode of delivery (Fig 3), maternal ESBL-PE colonization status (Fig 3D) and antibiotics use during delivery (Fig 3E).
Table 2. Cox proportional hazard analysis of ESBL-PE acquisition.
| Variable | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|
| Person-days | Crude HRa [95% CIb] | Pc | Adjusted HR [95% CI] | p | |
| Low birth weight | 0.01 | 0.01 | |||
| No (> = 2500gr) | 5300 | Ref.d | Ref. | ||
| Yes (<2500gr) | 324 | 2.6 [1.2; 5.5] | 2.7 [1.2 ; 5.9] | ||
| Maternal job | 0.21 | ||||
| No Job | 3900 | Ref. | |||
| Manual job | 1500 | 1.0 [0.6; 1.9] | |||
| Office job | 199 | 2.5 [1.0; 6.5] | |||
| Latrine type | 0.41 | ||||
| Outside without flush | 5100 | Ref. | |||
| Outside with flush | 137 | 0.7 [0.1; 5.4] | |||
| Inside without flush | 176 | 0.5 [0.1; 3.8] | |||
| Inside with flush | 232 | 2.1 [0.9; 5.3] | |||
| Habitat type | 0.46 | ||||
| Room shared with other household | 4389 | Ref. | |||
| House shared with other household | 500 | 0.8 [0.4; 1.4] | |||
| Individual house | 410 | 1.3 [0.2; 2.5] | |||
| Number of rooms | 0.63 | ||||
| 1 room | Ref. | ||||
| 2 rooms and more | 1.1 [0.6; 1.9] | ||||
| Number of household members | 0.16 | ||||
| Less than 5 members | 4500 | Ref. | |||
| 5 members and more | 1097 | 1.01 [0.5; 1.7] | |||
| Animal ownership | 0.32 | ||||
| No | 5370 | Ref. | |||
| Yes | 214 | 1.7 |0.2; 10.6] | |||
| Site | 0.19 | 0.96 | |||
| Semi-rural site | 4100 | Ref. | Ref. | ||
| Urban site | 1500 | 1.4 [0.8; 2.5] | 1.0 [0.5; 1.8] | ||
| Mode of delivery | <0.001 | 0.001 | |||
| Vaginal delivery | 5300 | Ref. | Ref. | ||
| Cesarean | 320 | 3.5 [1.8; 6.8] | 3.4 [1.7 ; 7.1] | ||
| Supervising person at delivery | 0.14 | ||||
| Non medical staff | 1700 | Ref. | |||
| Medical staff | 3800 | 1.6 [0.8 ; 2.9] | |||
| Maternal ESBL-carriage | 0.06 | 0.09 | |||
| No | 4000 | Ref. | Ref. | ||
| Yes | 1100 | 1.7 [1.0 ; 3.0] | 1.6 [0.9 ; 2.9] | ||
| Antibiotic during delivery | 0.04 | 0.04 | |||
| No | 5200 | Ref. | Ref. | ||
| Yes | 423 | 2.1 [1.0; 4.2] | 2.2 [1.1; 4.5] | ||
| Place of delivery | 0.09 | ||||
| Home | 2600 | Ref. | |||
| Health-care facilities | 3000 | 1.6 [0.9 ; 2.7] | |||
| Hospitalization during the first month of life | 0.23 | ||||
| No | 5500 | Ref. | |||
| Yes | 84 | 2.7 |0.62; 11.2] | |||
| Antibiotics intake during the first month of life | 0.54 | ||||
| No | 5500 | Ref. | |||
| Yes | 58 | 2.0 [0.27;14.7] | |||
aHR, Hazard Ratio
b95% CI, 95% Confidence Interval
cp, p-value
dRef., reference.
In multivariate analysis (Table 2), factors independently associated with a higher risk of first ESPL-PE acquisition included low birth weight (adjusted Hazard-ration (aHR) = 2.7, 95% CI [1.2; 5.9]), cesarean delivery (aHR = 3.4, 95% CI [1.7; 7.1]) and maternal use of antibiotics at delivery (aHR = 2.2, 95% CI [1.1; 4.5]). Maternal ESBL-PE colonization status was no longer statistically significant after adjustment. We found no statistically significant interactions.
Discussion
This study showed an overall incidence of 10.4 ESBL-PE acquisitions per 1000 newborn-days within a cohort of newborns in the community in Madagascar. Also, we found that low birth weight, cesarean delivery and maternal use of antibiotic at delivery were major risk factors of acquiring ESBL-PE during the first month of life.
To our best knowledge, this is the first community-based estimate of the incidence of ESBL-PE acquisition in newborns in a LMIC. In these settings, there are very few data from the community and the majority of published studies estimated a prevalence (ranging from 10.0% to 46.0%) which is less accurate than an incidence [12,23,26,32–36]. In addition, most studies [37–40] on the acquisition of ESBL-PE were conducted in neonatal intensive care units where ESBL-PE are more likely to be hospital-acquired and where neonates have serious illness, are more exposed to broad-spectrum antibiotics and are thus not representative of the general population. In these studies, two swabs were usually performed: the first one at admission and the second one at discharge which does not allow an accurate incidence estimation. Our estimate is just below the lower limit of monthly incidence of ESPL-PE acquisition [12 and 53 cases per 1000 patient-days] estimated by Mammina et al. in a neonatal intensive care unit in Italy [31]. Thus, this finding highlights that, even in neonates not particularly exposed to hospital environment, ESBL-PE spread is significant and very fast from the very beginning of life.
We found that cesarean delivery is a risk factor of ESBL-PE acquisition which is concordant with others studies on ESBL-PE infection or carriage [32,41]. Babies delivered by cesarean section are more at risk of handling by health personnel and have generally longer stay in hospital than vaginally delivered newborns. These two factors might increase the risk of acquiring ESBL-PE. Moreover, birth by cesarean section deprives newborns from maternal vaginal and gut flora exposure and may influence the newborn microbiome development [42,43]. Recent studies show that the microbiota play a key role in the protection against infectious diseases [44]. One plausible explanation to our finding is that the maternal microbiota might also play a role in the ESBL-PE acquisition during the first month of life. Concordantly, it has been shown that infants delivered by cesarean section have longer ESBL-PE carriage compared to those vaginally delivered [45].
The rate of cesarean section in low-income countries remains low compared to those observed in high- and middle-income countries [46–49]. However, in LMICs also, cesarean section might be performed while it is not medically indicated, with negative consequences [50]. Our result provides an additional argument to avoid unnecessary cesarean sections.
In the present study, pregnant women were included in their third trimester of pregnancy, which rendered difficult an accurate measurement of gestational age, as none of the included women had a first-trimester ultrasound. Therefore, in our analysis, we used LBW instead, which can be either the consequence of prematurity or intra-uterine growth retardation, or both. We showed that low birth weight babies were at increased risk of acquiring ESBL-PE whatever the ESBL-PE status of the mother. Among the 18 LBW babies with collected stool samples, seven were colonized by ESBL-PE, and only one had been hospitalized among the seven colonized babies, suggesting that the colonization was likely not hospital-acquired. Prematurity has been shown to be a risk factor for acquisition of ESBL-PE [51], whereas to our knowledge the role of intra-uterine growth retardation has never been studied. More studies are then needed to understand which is the underlying pathway of ESBL-PE acquisition in LBW babies, who are consequently more at risk to develop a potentially fatal drug-resistant infection.
Antibiotics during delivery are administered for various reasons [52], including for preventing the transmission of maternal group B streptococcus (GBS) to newborns. However, in our study, all mothers (n = 28) who received antibiotics during delivery had fetid amniotic fluid and/or premature rupture of the membrane and/or fever during delivery. Although these factors did not indicate that the mother was definitively infected, the delivery of these women might occurred in a septic context, which might increases the risk of an earlier ESBL-PE acquisition in newborns.
It is the first time, to our knowledge, that maternal use of antibiotics at delivery has been shown as a risk factor of ESBL-PE acquisition in newborns. Penicillin A, the most common antibiotics used [53], is able to cross the placenta and thus to be transmitted to the fetus. Consequently, it is likely that the newborn also received a part of maternal antibiotic and may explain why infants born from mothers who had antibiotics during delivery might be at increased risk of an earlier ESBL-PE acquisition in newborns.
It is well known that unnecessary use of antibiotics has subsequent impact on drug resistance and cost of healthcare in both LMICs and high-resource countries [54–58]. Measures to prevent it are currently under development (rapid diagnostic test) or have already been implemented, for example: through integrated community case management [59]. Thus, our findings support that reinforcing antibiotic stewardship is of the utmost importance. We did not find that hospitalization or antibiotic intake was associated with an increased risk of the first acquisition of ESBL-PE in newborns. As our study was community-based, few newborns were hospitalized (3.6%) or took antibiotics during their first month of life (1.6%) and therefore less exposed compared to neonates of the studies which are for the majority hospital-based [51,60–63]. In community-settings, risk factors might therefore be different and the mother and more specifically pregnancy conditions are predominant for ESBL-PE acquisition in neonates.
Although marginally significant in the univariate analysis, we did not found that maternal ESBL-PE colonization significantly increases the risk of ESBL-PE carriage for the newborns in the multivariate model. When we considered the acquisition of ESBL-PE during the first week of life, only 3 pairs of mother/infant carried the same pathogen. Although other studies found that maternal ESBL-PE was associated with ESBL-PE colonization in newborns [64,65], this finding suggests that mother to child transmission during delivery might not play such a significant role in the acquisition of colonization in the first week of life.
However, we cannot exclude that the none statistically significant associations between hospitalization, use of antibiotics during the first month of life, maternal ESBL-PE carriage and ESBL-PE acquisition in neonates, may be due to a lack of statistical power. Therefore, the interpretation of these results must be cautious.
Our study had some limitations. Six anal swabs were planned during the follow-up. For ethical reasons, it was not possible to perform more frequent swabs. Therefore, the time of acquisition of ESBL-PE might have occurred earlier than at the time of the positive ESBL-PE swab, within the span-time of two consecutive swabs. However, this inaccurate estimation of the acquisition date concerns all included newborns in the same way and is not likely to have had an impact on the risk factors we found associated with a higher risk of ESBL-acquisition. Also, the exposures to LBW, cesarean section and maternal carriage do not change over time and occur before and at the time of birth.
A great majority of the newborns (75.6%) had their first swab within the 3 first days. However, due to logistical issues, 75 newborns could not have their sample taken during this period. Among them, seven had only one sample during their whole follow-up (missed visits or lost-to follow-up). In the 68 remaining newborns, all subsequent samples were negative, suggesting that the missing sample within the three first days of life was likely negative. We are then confident that these limitations may not impact the associations we found.
Eleven Gram negative bacteria (GNB) in newborns stool samples and 14 GNB in mothers stool samples could not be identified by the MALDI-TOF SM. They were all Gram-negative, oxidase-negative, aerobic rods. The scores provided by the MALDI-TOF mass spectrometer were too low (1.2–1.7) and did not allow us to identify the species but gave us an idea about the bacteria genus (Enterobacteriaceae: Acinetobacter sp., Enterobacter sp., Kluyvera sp., Raoultella sp. and other Gram negative rods such as Stenotrophomonas sp.).
We did not have collect data on ESBL-PE colonization in household members. However, characteristics reflecting a potential transmission from the household members (habitat type, number of room, number of household members) were not significantly associated with ESBL-PE acquisition in newborns.
Conclusions
To our knowledge, we provide the first community-based estimate of the incidence of ESBL-PE acquisition in newborn in LMICs. This incidence is substantial; one other striking result of our study is the key role played by the mother in the acquisition of ESBL-PE by the neonates. We highlight that the course of pregnancy, including delivery and the previous months before birth, may influence the ESBL-PE acquisition and consequently potential subsequent neonatal infection. Our results reinforce that enhancing public-health interventions to promote antibiotic stewardship and to better monitor pregnancy to avoid unnecessary caesarean section, unnecessary antibiotic use at delivery and low birth weight newborns is of utmost importance.
Supporting information
(DOCX)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Acknowledgments
We would like to thank all the families who participated in this study. We would also like to thank the members of the BIRDY Study Group, physicians, field investigators and community workers for their involvement in this project. This work was supported by the funding of the Department of International Cooperation of the Principality of Monaco.
Data Availability
The data underlying this study are legally restricted by both French and Malagasy regulations. The procedures carried out with the French data privacy authority (CNIL, Commission nationale de l'informatique et des libertés) do not provide for public availability of the database. Requests for data may be sent to the following points of contact: Dr. Ravelomanantena Hantamalala Vololoniaina (Ethics Committee of the Malagasy Public Health Ministry) at hanta.agmed@blueline.mg, or Dr. Gwenaelle Carn (quality assurance manager at Institut Pasteur in Madagascar) at Gwenaelle@pasteur.mg.
Funding Statement
This work was undertaken as part of the Bacterial Infections and antibiotic Resistant Diseases among Young children (BIRDY) project (http://www.birdyprogram.org/), which is made possible by the funding of the Department of International Cooperation of the Principality of Monaco. Also this work was supported by the Institut Pasteur (PTR call). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Liu L, Hill K, Oza S, Hogan D, Chu Y, et al. (2016) Levels and Causes of Mortality under Age Five Years. In: Black RE, Laxminarayan R, Temmerman M, Walker N, editors. Reproductive, Maternal, Newborn, and Child Health: Disease Control Priorities, Third Edition (Volume 2). Washington (DC). [PubMed]
- 2.UNICEF (New York 2015) Levels & Trends in Child Mortality, Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation, Report 2015.
- 3.Liu L, Oza S, Hogan D, Chu Y, Perin J, et al. (2016) Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet 388: 3027–3035. doi: 10.1016/S0140-6736(16)31593-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oza S, Lawn JE, Hogan DR, Mathers C, Cousens SN (2015) Neonatal cause-of-death estimates for the early and late neonatal periods for 194 countries: 2000–2013. Bull World Health Organ 93: 19–28. doi: 10.2471/BLT.14.139790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seale AC, Blencowe H, Manu AA, Nair H, Bahl R, et al. (2014) Estimates of possible severe bacterial infection in neonates in sub-Saharan Africa, south Asia, and Latin America for 2012: a systematic review and meta-analysis. Lancet Infect Dis 14: 731–741. doi: 10.1016/S1473-3099(14)70804-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zaidi AK, Huskins WC, Thaver D, Bhutta ZA, Abbas Z, et al. (2005) Hospital-acquired neonatal infections in developing countries. Lancet 365: 1175–1188. doi: 10.1016/S0140-6736(05)71881-X [DOI] [PubMed] [Google Scholar]
- 7.Huynh BT, Padget M, Garin B, Herindrainy P, Kermorvant-Duchemin E, et al. (2015) Burden of bacterial resistance among neonatal infections in low income countries: how convincing is the epidemiological evidence? BMC Infect Dis 15: 127 doi: 10.1186/s12879-015-0843-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cosgrove SE (2006) The relationship between antimicrobial resistance and patient outcomes: mortality, length of hospital stay, and health care costs. Clin Infect Dis 42 Suppl 2: S82–89. [DOI] [PubMed] [Google Scholar]
- 9.Baral P, Neupane S, Marasini BP, Ghimire KR, Lekhak B, et al. (2012) High prevalence of multidrug resistance in bacterial uropathogens from Kathmandu, Nepal. BMC Res Notes 5: 38 doi: 10.1186/1756-0500-5-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Basu S (2015) Neonatal sepsis: the gut connection. Eur J Clin Microbiol Infect Dis 34: 215–222. doi: 10.1007/s10096-014-2232-6 [DOI] [PubMed] [Google Scholar]
- 11.Bhattacharya S (2013) Early diagnosis of resistant pathogens: how can it improve antimicrobial treatment? Virulence 4: 172–184. doi: 10.4161/viru.23326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Woerther PL, Burdet C, Chachaty E, Andremont A (2013) Trends in human fecal carriage of extended-spectrum beta-lactamases in the community: toward the globalization of CTX-M. Clin Microbiol Rev 26: 744–758. doi: 10.1128/CMR.00023-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paterson DL, Bonomo RA (2005) Extended-spectrum beta-lactamases: a clinical update. Clin Microbiol Rev 18: 657–686. doi: 10.1128/CMR.18.4.657-686.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vardakas KZ, Tansarli GS, Rafailidis PI, Falagas ME (2012) Carbapenems versus alternative antibiotics for the treatment of bacteraemia due to Enterobacteriaceae producing extended-spectrum beta-lactamases: a systematic review and meta-analysis. J Antimicrob Chemother 67: 2793–2803. doi: 10.1093/jac/dks301 [DOI] [PubMed] [Google Scholar]
- 15.Hsu AJ, Tamma PD (2014) Treatment of multidrug-resistant Gram-negative infections in children. Clin Infect Dis 58: 1439–1448. doi: 10.1093/cid/ciu069 [DOI] [PubMed] [Google Scholar]
- 16.Stoesser N, Xayaheuang S, Vongsouvath M, Phommasone K, Elliott I, et al. (2015) Colonization with Enterobacteriaceae producing ESBLs in children attending pre-school childcare facilities in the Lao People's Democratic Republic. J Antimicrob Chemother. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koleva PT, Kim JS, Scott JA, Kozyrskyj AL (2015) Microbial programming of health and disease starts during fetal life. Birth Defects Res C Embryo Today 105: 265–277. doi: 10.1002/bdrc.21117 [DOI] [PubMed] [Google Scholar]
- 18.Bourlioux P, Koletzko B, Guarner F, Braesco V (2003) The intestine and its microflora are partners for the protection of the host: report on the Danone Symposium "The Intelligent Intestine," held in Paris, June 14, 2002. Am J Clin Nutr 78: 675–683. [DOI] [PubMed] [Google Scholar]
- 19.Carl MA, Ndao IM, Springman AC, Manning SD, Johnson JR, et al. (2014) Sepsis from the gut: the enteric habitat of bacteria that cause late-onset neonatal bloodstream infections. Clin Infect Dis 58: 1211–1218. doi: 10.1093/cid/ciu084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nordberg V, Quizhpe Peralta A, Galindo T, Turlej-Rogacka A, Iversen A, et al. (2013) High proportion of intestinal colonization with successful epidemic clones of ESBL-producing Enterobacteriaceae in a neonatal intensive care unit in Ecuador. PLoS One 8: e76597 doi: 10.1371/journal.pone.0076597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Collado MC, Cernada M, Bauerl C, Vento M, Perez-Martinez G (2012) Microbial ecology and host-microbiota interactions during early life stages. Gut Microbes 3: 352–365. doi: 10.4161/gmic.21215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan GJ, Lee AC, Baqui AH, Tan J, Black RE (2013) Risk of early-onset neonatal infection with maternal infection or colonization: a global systematic review and meta-analysis. PLoS Med 10: e1001502 doi: 10.1371/journal.pmed.1001502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chereau F, Herindrainy P, Garin B, Huynh BT, Randrianirina F, et al. (2015) Colonization of extended-spectrum-beta-lactamase- and NDM-1-producing Enterobacteriaceae among pregnant women in the community in a low-income country: a potential reservoir for transmission of multiresistant Enterobacteriaceae to neonates. Antimicrob Agents Chemother 59: 3652–3655. doi: 10.1128/AAC.00029-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huynh B-T, Kermorvant-Duchemin E, Herindrainy P, Rakotoarimanana FMJ, Herisoa F, et al. (2017. (In Press)) Antibiotic resistance, early detection, and treatment of neonatal infections in a community-based cohort, Madagascar. Emerg Infect Dis. [Google Scholar]
- 25.Beukes LS, King TLB, Schmidt S (2017) Assessment of pit latrines in a peri-urban community in KwaZulu-Natal (South Africa) as a source of antibiotic resistant E. coli strains. Int J Hyg Environ Health 220: 1279–1284. doi: 10.1016/j.ijheh.2017.08.002 [DOI] [PubMed] [Google Scholar]
- 26.Herindrainy P, Randrianirina F, Ratovoson R, Ratsima Hariniana E, Buisson Y, et al. (2011) Rectal carriage of extended-spectrum beta-lactamase-producing gram-negative bacilli in community settings in Madagascar. PLoS One 6: e22738 doi: 10.1371/journal.pone.0022738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ewers C, Grobbel M, Stamm I, Kopp PA, Diehl I, et al. (2010) Emergence of human pandemic O25:H4-ST131 CTX-M-15 extended-spectrum-beta-lactamase-producing Escherichia coli among companion animals. J Antimicrob Chemother 65: 651–660. doi: 10.1093/jac/dkq004 [DOI] [PubMed] [Google Scholar]
- 28.Platell JL, Cobbold RN, Johnson JR, Heisig A, Heisig P, et al. (2011) Commonality among fluoroquinolone-resistant sequence type ST131 extraintestinal Escherichia coli isolates from humans and companion animals in Australia. Antimicrob Agents Chemother 55: 3782–3787. doi: 10.1128/AAC.00306-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Comité d'Antibiogramme de la Société Française de Microbiologie (CA-SFM) European Committee on antimicrobial Susceptibility testing (EUCAST). Recommandations Janvier 2015;V1.
- 30.Penders J, Thijs C, Vink C, Stelma FF, Snijders B, et al. (2006) Factors influencing the composition of the intestinal microbiota in early infancy. Pediatrics 118: 511–521. doi: 10.1542/peds.2005-2824 [DOI] [PubMed] [Google Scholar]
- 31.Mammina C, Di Carlo P, Cipolla D, Giuffre M, Casuccio A, et al. (2007) Surveillance of multidrug-resistant gram-negative bacilli in a neonatal intensive care unit: prominent role of cross transmission. Am J Infect Control 35: 222–230. doi: 10.1016/j.ajic.2006.04.210 [DOI] [PubMed] [Google Scholar]
- 32.Hijazi SM, Fawzi MA, Ali FM, Abd El Galil KH (2016) Multidrug-resistant ESBL-producing Enterobacteriaceae and associated risk factors in community infants in Lebanon. J Infect Dev Ctries 10: 947–955. doi: 10.3855/jidc.7593 [DOI] [PubMed] [Google Scholar]
- 33.Kothari C, Gaind R, Singh LC, Sinha A, Kumari V, et al. (2013) Community acquisition of beta-lactamase producing Enterobacteriaceae in neonatal gut. BMC Microbiol 13: 136 doi: 10.1186/1471-2180-13-136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ruppe E, Woerther PL, Diop A, Sene AM, Da Costa A, et al. (2009) Carriage of CTX-M-15-producing Escherichia coli isolates among children living in a remote village in Senegal. Antimicrob Agents Chemother 53: 3135–3137. doi: 10.1128/AAC.00139-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tellevik MG, Blomberg B, Kommedal O, Maselle SY, Langeland N, et al. (2016) High Prevalence of Faecal Carriage of ESBL-Producing Enterobacteriaceae among Children in Dar es Salaam, Tanzania. PLoS One 11: e0168024 doi: 10.1371/journal.pone.0168024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karanika S, Karantanos T, Arvanitis M, Grigoras C, Mylonakis E (2016) Fecal Colonization with Extended-Spectrum Beta-Lactamase-Producing Enterobacteriaceae and Risk Factors among Healthy Individuals: A Systematic Review and Meta-Analysis. Clin Infect Dis. [DOI] [PubMed] [Google Scholar]
- 37.Woerther PL, Angebault C, Jacquier H, Hugede HC, Janssens AC, et al. (2011) Massive increase, spread, and exchange of extended spectrum beta-lactamase-encoding genes among intestinal Enterobacteriaceae in hospitalized children with severe acute malnutrition in Niger. Clin Infect Dis 53: 677–685. doi: 10.1093/cid/cir522 [DOI] [PubMed] [Google Scholar]
- 38.Andriatahina T, Randrianirina F, Hariniana ER, Talarmin A, Raobijaona H, et al. (2010) High prevalence of fecal carriage of extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in a pediatric unit in Madagascar. BMC Infect Dis 10: 204 doi: 10.1186/1471-2334-10-204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Das P, Singh AK, Pal T, Dasgupta S, Ramamurthy T, et al. (2011) Colonization of the gut with Gram-negative bacilli, its association with neonatal sepsis and its clinical relevance in a developing country. J Med Microbiol 60: 1651–1660. doi: 10.1099/jmm.0.033803-0 [DOI] [PubMed] [Google Scholar]
- 40.Peretz A, Skuratovsky A, Khabra E, Adler A, Pastukh N, et al. (2016) Peripartum maternal transmission of extended-spectrum beta-lactamase organism to newborn infants. Diagn Microbiol Infect Dis. [DOI] [PubMed] [Google Scholar]
- 41.T GE, Moges F, Eshetie S, Yeshitela B, Abate E (2017) Bacterial etiologic agents causing neonatal sepsis and associated risk factors in Gondar, Northwest Ethiopia. BMC Pediatr 17: 137 doi: 10.1186/s12887-017-0892-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mueller NT, Bakacs E, Combellick J, Grigoryan Z, Dominguez-Bello MG (2015) The infant microbiome development: mom matters. Trends Mol Med 21: 109–117. doi: 10.1016/j.molmed.2014.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dominguez-Bello MG, Costello EK, Contreras M, Magris M, Hidalgo G, et al. (2010) Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci U S A 107: 11971–11975. doi: 10.1073/pnas.1002601107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Blaser MJ, Falkow S (2009) What are the consequences of the disappearing human microbiota? Nat Rev Microbiol 7: 887–894. doi: 10.1038/nrmicro2245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lohr IH, Rettedal S, Natas OB, Naseer U, Oymar K, et al. (2013) Long-term faecal carriage in infants and intra-household transmission of CTX-M-15-producing Klebsiella pneumoniae following a nosocomial outbreak. J Antimicrob Chemother 68: 1043–1048. doi: 10.1093/jac/dks502 [DOI] [PubMed] [Google Scholar]
- 46.Althabe F, Sosa C, Belizan JM, Gibbons L, Jacquerioz F, et al. (2006) Cesarean section rates and maternal and neonatal mortality in low-, medium-, and high-income countries: an ecological study. Birth 33: 270–277. doi: 10.1111/j.1523-536X.2006.00118.x [DOI] [PubMed] [Google Scholar]
- 47.Betran AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, et al. (2007) Rates of caesarean section: analysis of global, regional and national estimates. Paediatr Perinat Epidemiol 21: 98–113. doi: 10.1111/j.1365-3016.2007.00786.x [DOI] [PubMed] [Google Scholar]
- 48.Stanton CK, Holtz SA (2006) Levels and trends in cesarean birth in the developing world. Stud Fam Plann 37: 41–48. [DOI] [PubMed] [Google Scholar]
- 49.Buekens P, Curtis S, Alayon S (2003) Demographic and Health Surveys: caesarean section rates in sub-Saharan Africa. BMJ 326: 136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nelson JP (2017) Indications and appropriateness of caesarean sections performed in a tertiary referral centre in Uganda: a retrospective descriptive study. Pan Afr Med J 26: 64 doi: 10.11604/pamj.2017.26.64.9555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rettedal S, Hoyland Lohr I, Natas O, Sundsfjord A, Oymar K (2013) Risk factors for acquisition of CTX-M-15 extended-spectrum beta-lactamase-producing Klebsiella pneumoniae during an outbreak in a neonatal intensive care unit in Norway. Scand J Infect Dis 45: 54–58. doi: 10.3109/00365548.2012.713116 [DOI] [PubMed] [Google Scholar]
- 52.Persaud RR, Azad MB, Chari RS, Sears MR, Becker AB, et al. (2015) Perinatal antibiotic exposure of neonates in Canada and associated risk factors: a population-based study. J Matern Fetal Neonatal Med 28: 1190–1195. doi: 10.3109/14767058.2014.947578 [DOI] [PubMed] [Google Scholar]
- 53.Mylonas I (2011) Antibiotic chemotherapy during pregnancy and lactation period: aspects for consideration. Arch Gynecol Obstet 283: 7–18. doi: 10.1007/s00404-010-1646-3 [DOI] [PubMed] [Google Scholar]
- 54.Okeke IN, Laxminarayan R, Bhutta ZA, Duse AG, Jenkins P, et al. (2005) Antimicrobial resistance in developing countries. Part I: recent trends and current status. Lancet Infect Dis 5: 481–493. doi: 10.1016/S1473-3099(05)70189-4 [DOI] [PubMed] [Google Scholar]
- 55.Organization WH. Antimicrobial resistance: global report on surveillance Geneva: WHO Press; 2014. [Google Scholar]
- 56.Bebell LM, Muiru AN (2014) Antibiotic use and emerging resistance: how can resource-limited countries turn the tide? Glob Heart 9: 347–358. doi: 10.1016/j.gheart.2014.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Goossens H (2009) Antibiotic consumption and link to resistance. Clin Microbiol Infect 15 Suppl 3: 12–15. [DOI] [PubMed] [Google Scholar]
- 58.Shallcross LJ, Davies DS (2014) Antibiotic overuse: a key driver of antimicrobial resistance. Br J Gen Pract 64: 604–605. doi: 10.3399/bjgp14X682561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Graham K, Sinyangwe C, Nicholas S, King R, Mukupa S, et al. (2016) Rational use of antibiotics by community health workers and caregivers for children with suspected pneumonia in Zambia: a cross-sectional mixed methods study. BMC Public Health 16: 897 doi: 10.1186/s12889-016-3541-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Abdel-Hady H, Hawas S, El-Daker M, El-Kady R (2008) Extended-spectrum beta-lactamase producing Klebsiella pneumoniae in neonatal intensive care unit. J Perinatol 28: 685–690. doi: 10.1038/jp.2008.73 [DOI] [PubMed] [Google Scholar]
- 61.Crivaro V, Bagattini M, Salza MF, Raimondi F, Rossano F, et al. (2007) Risk factors for extended-spectrum beta-lactamase-producing Serratia marcescens and Klebsiella pneumoniae acquisition in a neonatal intensive care unit. J Hosp Infect 67: 135–141. doi: 10.1016/j.jhin.2007.07.026 [DOI] [PubMed] [Google Scholar]
- 62.Li X, Xu X, Yang X, Luo M, Liu P, et al. (2017) Risk factors for the infection and/or colonization of extended-spectrum beta-lactamase-producing bacteria in a neonatal intensive care unit: a meta-analysis. Int J Antimicrob Agents. [DOI] [PubMed] [Google Scholar]
- 63.Shakil S, Ali SZ, Akram M, Ali SM, Khan AU (2010) Risk factors for extended-spectrum beta-lactamase producing Escherichia coli and Klebsiella pneumoniae acquisition in a neonatal intensive care unit. J Trop Pediatr 56: 90–96. doi: 10.1093/tropej/fmp060 [DOI] [PubMed] [Google Scholar]
- 64.Denkel LA, Schwab F, Kola A, Leistner R, Garten L, et al. (2014) The mother as most important risk factor for colonization of very low birth weight (VLBW) infants with extended-spectrum beta-lactamase-producing Enterobacteriaceae (ESBL-E). J Antimicrob Chemother 69: 2230–2237. doi: 10.1093/jac/dku097 [DOI] [PubMed] [Google Scholar]
- 65.Rettedal S, Lohr IH, Bernhoff E, Natas OB, Sundsfjord A, et al. (2015) Extended-spectrum beta-lactamase-producing Enterobacteriaceae among pregnant women in Norway: prevalence and maternal-neonatal transmission. J Perinatol 35: 907–912. doi: 10.1038/jp.2015.82 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
The data underlying this study are legally restricted by both French and Malagasy regulations. The procedures carried out with the French data privacy authority (CNIL, Commission nationale de l'informatique et des libertés) do not provide for public availability of the database. Requests for data may be sent to the following points of contact: Dr. Ravelomanantena Hantamalala Vololoniaina (Ethics Committee of the Malagasy Public Health Ministry) at hanta.agmed@blueline.mg, or Dr. Gwenaelle Carn (quality assurance manager at Institut Pasteur in Madagascar) at Gwenaelle@pasteur.mg.