Abstract
A 27-year-old male presented with a gradually increasing left scrotal mass. There was no significant past medical history. Ultrasonography of the left scrotum showed a hypoechoic, intratesticular mass with solid and cystic components. Laboratory investigations revealed normal serum levels of alpha-fetoprotein, beta human chorionic gonadotropin and lactate dehydrogenase. He underwent left high inguinal orchidectomy due to suspicion of testicular malignancy. After histopathologic examination and immunostaining, a diagnosis of high-grade primary testicular leimyosarcoma was ascertained. Only a few cases of primary intratesticular leiomyosarcoma have been reported in literature with the mean age of presentation of 50 years. In younger individuals, these tumors have been reported in a setting of predisposing factors like anabolic steroid use, testicular germ cell tumors, chronic inflammation of testis and testicular field radiation for treatment of leukemia. We present a case of high grade leiomyosarcoma of testis in a young male without any known predisposing factors.
Keywords: Immunohistochemistry, leiomyosarcoma, sarcoma, testis
Introduction
Primary intratesticular sarcomas are very rare neoplasms usually arising either from a testicular teratoma or spermatocytic seminoma. These sarcomas behave indolently and have a rare potential for distant metastasis, thus having a favorable prognosis.[1,2] Due to their rarity only a limited number of cases have been reported in literature. We are presenting an extremely rare occurrence of an unusual case of a high grade primary testicular leiomyosarcoma in a young male with absence of any predisposing features for this rare malignancy.
Case presentation
A 27-year-old male presented with a painless, gradually enlarging left sided scrotal swelling for six months. General physical examination was unremarkable with no urologic or constitutional symptoms, exposure to radiation or steroid intake. Local examination revealed a hard globular mass measuring 12×8 cm in the left scrotum. Scrotal ultrasonography showed a hypoechoic, intratesticular mass measuring 10×8 cm in size, with solid and cystic components. The contralateral testis and the spermatic cords were unremarkable. Laboratory investigations revealed normal serum levels of alpha-fetoprotein (AFP), beta human chorionic gonadotropin (β-HCG) and lactate dehydrogenase (LDH). Computed tomography (CT) scans did not reveal any other primary disease or metastatic deposits anywhere in the body. With a clinical diagnosis of testicular malignancy, patient underwent left high inguinal orchidectomy.
Grossly, the orchidectomy specimen measured 10×7×5 cm and weighed 480 gm. Outer surface was bosselated with areas of congestion. Cut surface was grey white, solid with foci of hemorrhage, necrosis and myxoid degeneration. The tumor replaced almost the entire testis with a thin rim of recognizable testicular tissue on the periphery (Figure 1).
Figure 1.

Macroscopic appearance of left testicular mass. Cut surface showing replacement of testicular tissue by a grey white, solid tumor with focal congestion and myxoid degeneration
On microscopic examination, tumor was composed of oval to spindle-shaped cells in interlacing bundles and fascicles (Figure 2a). The tumor cells contained moderate amount of eosinophilic cytoplasm and blunt ended cigar-shaped nuclei with moderate nuclear atypia and frequent mitoses (20/10hpf). In the periphery a few remnant seminiferous tubules (ST) were seen entrapped within the tumor (Figure 2b). Vascular tumor emboli (inset, Figure 2b), foci of hemorrhage, necrosis and myxoid degeneration were also observed. There was no invasion of the spermatic cord or tunica vaginalis. All surgical margins were free from tumor. Histomorphological features favoured a sarcoma. Immunohistochemically, tumor cells stained positively for vimentin, smooth muscle actin (SMA), focally for desmin (Figure 3 a–c) and negatively for S-100. Extensive sampling of the tumor did not reveal any foci of germ cells or teratomatous elements or paratesticular involvement. After ruling out any other primary site of origin, a final diagnosis of primary testicular leiomyosarcoma with pathological staging of pT2NXM0S0 (TNM stage IB) was made.
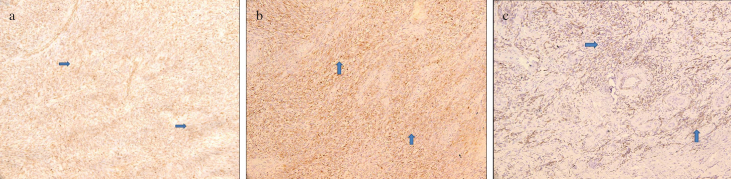
Figure 2. a, b.
Microscopic examination of tumor. (a) Oval to spindle- shaped tumor cells arranged in interlacing bundles and fascicles (arrows) (H&E, 100X). (b) Tumor cells showing moderate nuclear atypia and frequent mitoses (arrowhead) with entrapped seminiferous tubules (arrows) (H&E, 400X). Inset shows vascular tumor embolus (E)
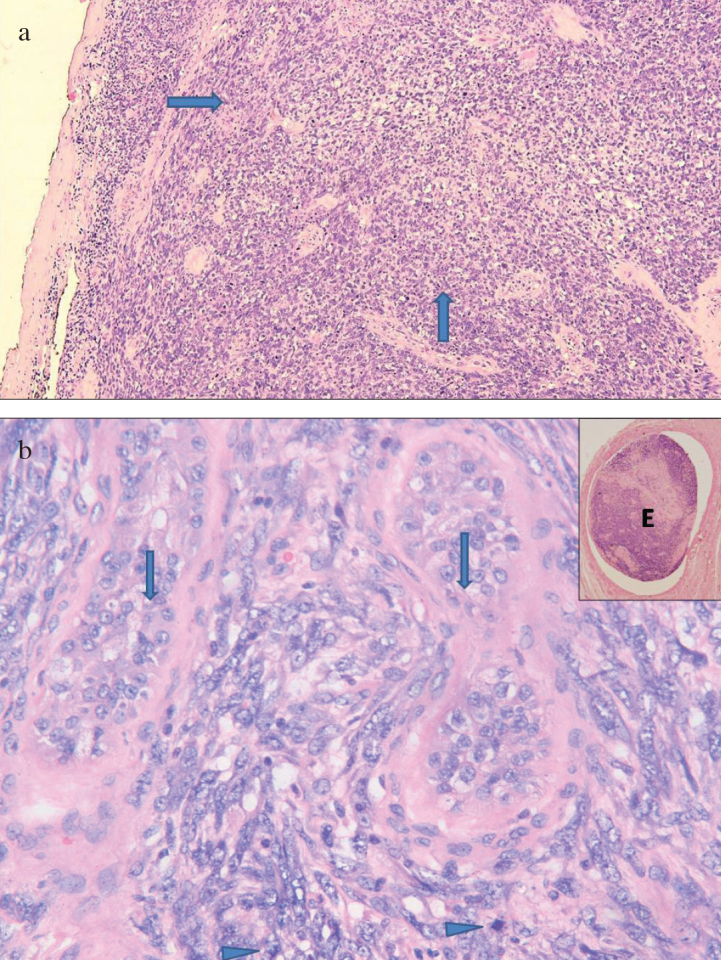
Figure 3. a–c.
Immunonohistochemistry shows positive staining with (a) Vimentin (diffuse staining, arrows) (b) SMA (diffuse staining, arrows) (c) Desmin (focal staining, arrows) (IHC, 200X)
Postoperative period was uneventful and the patient was not given any adjuvant therapy. During the postoperative two years, follow-up visits were performed at every six months with abdominal ultrasound, chest x-rays and CT scans, and the patient was found to be disease-free with no recurrence or metastases.
Discussion
Sarcomas constitute only 1% of all malignant lesions of the testis. Leiomyosarcomas are the third most common malignant tumors of soft-tissue (sarcoma) after malignant testicular fibrous histiocytoma and liposarcoma. Leiomyosarcomas arise from undifferentiated smooth muscle cells of mesenchymal origin. However, almost all testicular leiomyosarcomas are in fact paratesticular, originating from the spermatic cord, epididymis or scrotum.[3–5] Primary intratesticular leiomyosarcomas usually occur between fourth to seventh decades with the mean age of presentation being 50 years. Our patient was a young male aged 27 years which is very unusual for this tumor. In young patients, they are usually associated with testicular germ cell tumors (GCT), chronic inflammation[6,7] or testicular radiotherapy received for leukemia.[3] Without these predisposing factors its occurrence is rare as in our case where no such history was elicited.
Majority of these patients present with painless testicular enlargement and inguinoscrotal discomfort. Scrotal ultrasound shows a well-circumscribed, hypoechoic mass with or without calcification. Clinically other differentials include seminoma, sertoli cell and Leydig cell tumors of testis. Tumor markers (AFP, HCG-β and LDH) are usually within normal range in leiomyosarcomas thereby excluding the possibility of GCT. The greatest mean diameter of 8.0 cm has been reported for leiomyosarcomas in literature[8] and in our case it was 10 cm. Though tumors with ≤ 3.5cm diameter can be considered of low malignant potential, their biological behavior is unpredictable as four patients have been reported to develop metastatic disease.[8]
The origin of testicular leiomyosarcomas is controversial with the histogenesis being attributed to descent of smooth muscle elements from the spermatic cord or epididymis.[2,8] Intratesticular leiomyosarcomas must be differentiated from paratesticular leiomyosarcomas and sarcomas arising within a teratoma. Since sarcomatous areas have been documented in yolk sac tumors, spermatocytic seminomas and some sex-cord stromal tumors,[9] thorough sampling of the tumor is mandatory before assigning the diagnosis of primary intratesticular leiomyosarcoma to a tumor with spindle-shaped cells. The importance of excluding GCT and paratesticular neoplasms originating from scrotum and epididymis has been emphasized by several authors because of radiosensitive nature of GCT.[2,4]
As per our literature search, this patient is the 20th case reported so far in medical literature.[8] Owing to only a few reports specific histopathological criteria used for grading of intratesticular leiomyosarcomas are lacking in literature. The diagnostic criteria used for uterine spindle- cell leiomyosarcomas like presence of significant nuclear atypia, mitotic count ≥10/10 high-power field (hpf) and coagulative necrosis with nuclear debris[10] may be used for the diagnosis,[4] with subsequent immunohistochemical profiling to support the diagnosis.[2] Accordingly, this case was a high-grade lesion owing to the presence of high mitoses (20/10 hpf), necrosis and nuclear atypia. Unlike our case, eight of the ten reported primary intratesticular leiomyosarcomas were either low grade or unspecified and of these only three patients were below 40 years of age.[4]
Compared to leiomyosarcomas at other sites, prognosis of testicular leiomyosarcoma appears to be better with a low metastatic potential.[4,5] Irrespective of the tumor grade, high inguinal orchidectomy is considered an adequate treatment of choice. Close follow-up is however required because late metastasis can occur in low- grade tumors and death due to pulmonary metastasis has been reported even 14 months after orchidectomy.[2,4] Due to the rarity of these tumors 5- year- survival rates are not known exactly, but two patients who were free of recurrence and metastasis 6 years after post orchiectomy has been cited in the literature.[4] Even though the role of radiotherapy and chemotherapy is not well known additional chemotherapy is usually required in cases with advanced disease.[10]
In conclusion, due to rarity of this tumor there is lack of data on the natural history, histological diagnostic criteria, prognostic factors, survival rates and treatment recommendations. Literature indicates that indolent tumors have a potential for cure if treated early and also they should be differentiated from the more common sarcomas of the spermatic cord as well as from those associated with GCT. Our patient was only 27 years old with no predisposing factors, had a large, high grade tumor and underwent high orchidectomy without any adjuvant therapy. He has been on follow-up for 2 years and despite the high grade nature of the tumor he has been free from recurrence or metastasis thereby indicating that irrespective of the tumor grade, a high inguinal orchidectomy is an adequate treatment for these tumors. It also proves that testicular leiomyosarcoma has a better prognosis than leiomyosarcomas involving any other site.
Footnotes
Informed Consent: Could not be taken for this manuscript as the patient was unavailable on the contact number provided in his file. Patient’s identity has not been disclosed anywhere in the manuscript.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – F.S.; Design – F.S., S.S.; Supervision – F.S., S.S.; Resources – F.S., C.R.; Materials – P.V.; Data Collection and/or Processing – F.S., C.R.; Analysis and/or Interpretation – F.S., S.S., P.V.; Literature Search – F.S., C.R.; Writing Manuscript – F.S., C.R.; Critical Review – F.S., S.S., C.R., P.V.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Hachi H, Bougtab A, Amhajji R, Otmany F, al Bouzidi A, Laalou L, et al. A case report of testicular leiomyosarcoma. Med Trop(Mars) 2002;62:531–3. [PubMed] [Google Scholar]
- 2.Singh R, Chandra A, O’Brien TS. Primary intratesticular leiomyosarcoma in a mixed race man: a case report. Clin Pathol. 2004;57:1319–20. doi: 10.1136/jcp.2004.018770. https://doi.org/10.1136/jcp.2004.018770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Canales BK, Lukasewycz SJ, Manivel JC, Pryor JL. Postradiotherapy intratesticular leiomyosarcoma. Urology. 2005;66:657. doi: 10.1016/j.urology.2005.03.027. https://doi.org/10.1016/j.urology.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 4.Kumar M, Patne SC, Kumar S, Shukla VK. Primary high-grade testicular leiomyosarcoma. Indian J Pathol Microbiol. 2009;52:91–3. doi: 10.4103/0377-4929.44977. https://doi.org/10.4103/0377-4929.44977. [DOI] [PubMed] [Google Scholar]
- 5.Narula V, Siraj F, Bansal A. Renal leiomyosarcoma with soft tissue metastasis: An unusual presentation. Can Urol Assoc J. 2015;9:139–41. doi: 10.5489/cuaj.2396. https://doi.org/10.5489/cuaj.2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Froeher M, Fischer R, Leike S, Hakenberg OW, Noack B, Wirth MP. Intratesticular leiomyosarcoma in a young man after high doping with oral Turinabol: a case report. Cancer. 1999;86:1571–5. doi: 10.1002/(sici)1097-0142(19991015)86:8<1571::aid-cncr26>3.0.co;2-c. https://doi.org/10.1002/(SICI)1097-0142(19991015)86:8<1571::AID-CNCR26>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 7.Ali Y, Kehinde EO, Makar R, Al-Awadi KA, Anim JT. Leiomyosarcoma complicating chronic inflammation of the testis. Med Princ Pract. 2002;11:157–60. doi: 10.1159/000063239. https://doi.org/10.1159/000063239. [DOI] [PubMed] [Google Scholar]
- 8.Abdullazade S, Kara O, Akdoğan B, Baydar DE. Primary low grade intratesticular leiomyosarcoma: case report and review of the literature. Turk Patoloji Derg. 2013;29:227–30. doi: 10.5146/tjpath.2013.01179. https://doi.org/10.5146/tjpath.2013.01179. [DOI] [PubMed] [Google Scholar]
- 9.Malagon HD, Valdez AM, Moran CA, Suster S. Germ cell tumors with sarcomatous components: a clinicopathologic and immunohistochemical study of 46 cases. Am J Surg Pathol. 2007;31:1356–62. doi: 10.1097/PAS.0b013e318033c7c4. https://doi.org/10.1097/PAS.0b013e318033c7c4. [DOI] [PubMed] [Google Scholar]
- 10.Damle RP, Suryawanshi KH, Dravid NV, Newadkar DV. Primary intratesticular pleomorphic leiomyosarcoma: A rare case report. Indian J Pathol Microbiol. 2013;56:425–7. doi: 10.4103/0377-4929.125360. https://doi.org/10.4103/0377-4929.125360. [DOI] [PubMed] [Google Scholar]