Abstract
Purpose
Pediatric trauma is one of the major health problems around the world which threats the life of children. The survival of injured children depends upon appropriate care, accurate triage and effective emergent surgery. The objective of this study was to determine the predictive values of injury severity score (ISS), new injury severity score (NISS) and revised trauma score (RTS) on children's mortality, hospitalization and need for surgery.
Methods
In this study, records of trauma patients under 15 years old transported from a trauma scene to emergency department of Poursina hospital from 2010 to 2011 were included. Statistical analysis was applied to determine the ISS, NISS and RTS ability in predicting the outcomes of interest.
Results
There were 588 records in hospital registry system. The mean age of the patients was (7.3 ± 3.8) years, and 62.1% (n = 365) of patients were male. RTS was the more ability score to predict mortality with an area under curve (AUC) of 0.99 (95% CI, 0.99–1). In the hospital length of stay (LOS), ISS was best predictor for both the hospital LOS with AUC of 0.72 (95% CI, 0.67–0.76) and need for surgical surgery with AUC of 0.94 (95% CI, 0.90–0.98).
Conclusion
RTS as a physiological scoring system has a higher predicting AUC value in predicting mortality. The anatomic scoring systems of ISS and NISS have good performance in predicting of hospital LOS and need for surgery outcomes.
Keywords: Length of stay, Mortality, Pediatrics, Injury severity score
Introduction
Trauma is one of the major health problems in the world that results in death and disability and affects all age groups.1 It is estimated that by 2020, trauma will reach the third cause of death worldwide.2 Over half of the deaths related to unintentional injuries occur among children less than 19 years of age.3 Pediatric trauma is one of the major health threats in the life of children. The survival of injured children depends upon appropriate care, accurate triage and effective emergent surgery.4, 5 There are several injury scoring systems, anatomic, physiologic and combined scores, which have been used for prediction of patients' outcome such as mortality.6 injury severity score (ISS) and new injury severity score (NISS) as anatomic scoring systems and revised trauma score (RTS) as a physiologic scoring system are used for predicting trauma severity.7 Easy-to-use trauma scoring systems can be used for making good clinical decision before the patient reaches the hospital and at emergency department. These scoring systems can also be used for timely delivering medical support and preparing the patient for surgery in early stage.8 The scores of ISS and NISS have demonstrated association with interested outcomes of mortality, length of hospital stay among adult and pediatric trauma patients.9, 10 However, there is limited information about comparison of the anatomic and physiologic scoring system in predicting the outcome of need for surgical interventions in trauma patients. On the other hand there is no enough evidence to answer the question whether ISS or NISS or RTS is superior in predicting the patients who need surgery. Whereas it was shown that approximately half of injured patients die in the first 48 h.11 The time for emergency surgery in clinical practice should take place as soon as possible after injury.12, 13 In patients with traumatic shock, the time span for hemostatic surgery is one of the most important issues.14 Some studies have shown that early surgery for patients requiring surgery results in the decrease of 1-year mortality and hospital length of stay (LOS).15, 16
In Iran, trauma is the second leading cause of death in all ages and there is need to pay more attention to traumatic patients in order to provide right and timely services for needed patients.
This study aimed at evaluation of RTS as a physiologic trauma score in comparison with ISS and NISS in pediatric trauma patients outcomes including death, LOS and need for surgery interventions.
Materials and methods
Study design and setting
This is crossing sectional study which is based on the pediatric trauma patients who admitted in emergency department of Poursina hospital, Rasht, Iran from 2010 to 2011. The used data were: demographic characteristics (age, sex), injury (type of injury, mechanism of injury, organs affected by trauma, mode of transport), patient's hospital LOS, surgery intervention and mortality rate. Data were collected anonymously to respect the ethical consideration.
Participants
All participants were traumatic patients older than 14 years, who were referred to emergency department of Poursina hospital in city of Rasht in the years of 2010–2011.
Data gathering
The required data was derived from the hospital information system to compare the ISS, NISS and RTS scoring systems for predicting the pediatric trauma patient's outcomes of mortality, LOS and need for surgery. The scores of ISS and NISS are derived from the Abbreviated Injury Scale (AIS). ISS is calculated by adding the squares of the three highest AIS values in three different body regions and it ranges from 1 to 75. NISS is calculated by the sum of the square of AIS value of each patient's three most severe injuries despite the origin of injury.17 RTS is based on Glasgow coma scale (GCS), systolic blood pressure and respiratory rate and it ranges from 0 to 7.8408 (Table 1).18 The formula of RTS is RTSx = 0.7326SBPx + 0.2908RRc + 0.9368GCSx.
Table 1.
Calculation of RTS.
| Clinical parameter | Category | Score | Coefficient |
|---|---|---|---|
| Respiratory rate (breaths per minute) | 10–29 | 4 | 0.2908 |
| >29 | 3 | ||
| 6–9 | 2 | ||
| 1–5 | 1 | ||
| 0 | 0 | ||
| Systolic blood pressure (mmHg) | >89 | 4 | 0.7326 |
| 76–89 | 3 | ||
| 50–75 | 2 | ||
| 1–49 | 1 | ||
| 0 | 0 | ||
| Glasgow coma scale | 13–15 | 4 | 0.9368 |
| 9–12 | 3 | ||
| 6–8 | 2 | ||
| 4–5 | 1 | ||
| 3 | 0 |
Statistical analysis
The ability of each score in predicting the mortality, hospitalization and need for surgery was evaluated by ROC curve. The scores of ISS, NISS and RTS were compared by sensitivity, specificity, cut-off points according to the AUC with a confidence interval of 95%. All statistical analysis was performed by SPSS (ver. 18). The significant level was considered at 0.05.
Results
Among the 588 children aged 0–14 years referred to emergency department of Poursina hospital between the years of 2010 and 2011, 365 were boys (62.1%) and 223 girls (37.9%). The mean age of patients was (7.3 ± 3.8) years (ranging from 3 months to 14 years). The most common causes of injuries were traffic accidents (n = 248, 42.2%) and falling (n = 234, 39.8%); the most common injured area was extremities (n = 546, 92.9%), followed by head and neck (n = 161, 27.4%). Of the 588 cases, 574 (97.6%) were discharged from hospital and 14 died (2.4%). Of the total traumatic patients who transferred to the hospital, only 132 (22.4%) were transported by ambulance, while 436 (77.6%) by personal vehicles. Different surgical procedures were performed in 273 patients (46.4%). The mean length of hospital stay was (3.2 ± 6.3) days. Eleven patients needed ICU care. The mean length of ICU stay was (11.7 ± 12.3) days. Characteristics of traumatic children are presented in Table 2.
Table 2.
Characteristics of pediatric traumatic patients.
| Characteristics | Frequency (%)/Mean (±SD) |
|---|---|
| Age (years) | 7.3 (±3.8) |
| Sex | |
| Male | 365 (62.1) |
| Female | 223 (37.9) |
| Type of injury | |
| Blunt | 542 (92.2) |
| Penetrating | 46 (7.8) |
| Mechanism | |
| Traffic accidents | 248 (42.2) |
| Falling | 234 (39.8) |
| Sharp object | 43 (7.3) |
| Sport | 39 (6.6) |
| Assault | 10 (1.7) |
| Others | 14 (2.4) |
| Injured area | |
| Head and neck | 161 (27.4) |
| Face | 137 (23.3) |
| Abdomen | 50 (8.5) |
| Thorax | 33 (5.6) |
| Spine | 11 (1.9) |
| Extremity | 546 (92.9) |
| Trauma scores | |
| ISS | 6.54 (±6.11) |
| NISS | 8.58 (±7.73) |
| RTS | 7.49 (±0.81) |
Prognostic values of trauma scoring systems
The scoring systems had significant differences in both groups. The mean scores of ISS and NISS were higher in dead patients compared to alive ones. The observed difference was statistically significant (p < 0.0001, Table 3).
Table 3.
Comparison of ISS, NISS and RTS in alive and dead patients.
| Score | Alive patients (n = 574) Mean (SD) |
Dead patients (n = 14) Mean (SD) |
p value |
|---|---|---|---|
| ISS | 6.26 (5.90) | 17.71 (4.33) | 0.001 |
| NISS | 8.24 (7.44) | 22.78 (6.16) | 0.001 |
| RTS | 7.58 (0.52) | 3.87 (1.70) | 0.001 |
Considering the need for surgical procedures, the trauma scores were analyzed and compared in two groups. The mean scores of ISS and NISS in children who required surgery were significantly higher than the children who did not need operation. The mean score of RTS was higher in children who did not need surgery compared to the other group (Table 4).
Table 4.
Comparison of ISS, NISS and RTS based on need for surgery.
| Score | Need for surgery (n = 32) Mean (SD) |
No need for surgery (n = 556) Mean (SD) |
p value |
|---|---|---|---|
| ISS | 21.34 (9.74) | 5.68 (4.57) | 0.001 |
| NISS | 26.06 (11.97) | 7.57 (6.05) | 0.001 |
| RTS | 6.66 (1.11) | 7.54 (0.76) | 0.001 |
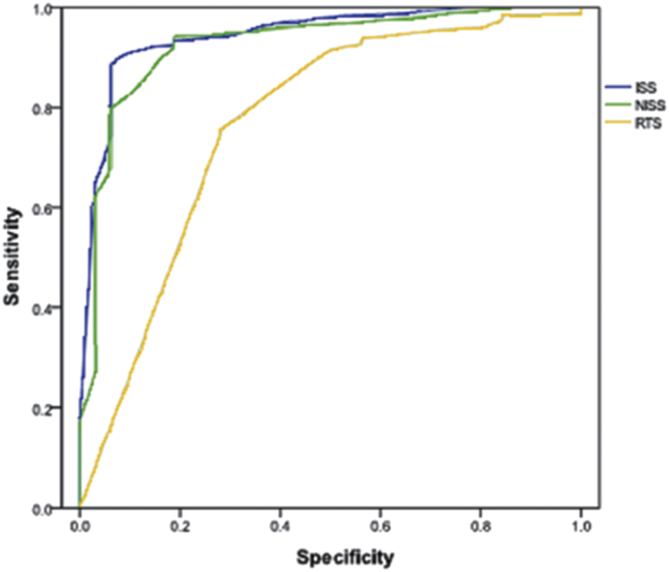
RTS was found to be the best score in predicting mortality among two other scores with an AUC of 0.99 (CI: 0.99–1). In predicting the length of hospital stay and need for surgical procedure, ISS had the strongest ability with an AUC of 0.72 (CI: 0.67–0.76) and 0.94 (CI: 0.90–0.98) respectively. There were no considerable differences between ISS and NISS power of prediction (Table 5).
Table 5.
Comparison of sensitivity, specificity and AUC of ISS, NISS and RTS in optimal cut-off points based on ROC curve.
| Score | Cut-off | AUC | 95% CI | Sensitivity (%) | Specificity (%) | |
|---|---|---|---|---|---|---|
| Mortality | ISS | ≤15 | 0.82 | 0.69–0.95 | 92 | 65 |
| NISS | ≤17.5 | 0.79 | 0.64–0.94 | 91 | 65 | |
| RTS | ≥4.8 | 0.99 | 0.99–1 | 99 | 64 | |
| Length of hospital stay | ISS | ≤12.5 | 0.72 | 0.67–0.76 | 97 | 80 |
| NISS | ≤15.5 | 0.70 | 0.66–0.74 | 98 | 78 | |
| RTS | ≥5.06 | 0.55 | 0.50–0.59 | 97 | 98 | |
| Need for surgery | ISS | ≤16.5 | 0.94 | 0.90–0.98 | 95 | 69 |
| NISS | ≤17.5 | 0.93 | 0.87–0.97 | 94 | 81 | |
| RTS | ≥7 | 0.77 | 0.67–0.86 | 91 | 50 |
ROC curve illustrates the sensitivity, specificity of trauma scores and determine the prediction value of mortality, hospital LOS and need for surgery (Fig. 1, Fig. 2, Fig. 3).
Fig. 1.
ROC curve of ISS, NISS and RTS for predicting mortality in traumatic children.
Fig. 2.
ROC curve of ISS, NISS and RTS for predicting LOS in traumatic children.
Fig. 3.
ROC curve of ISS, NISS and RTS for predicting the need for surgical procedures in traumatic children.
Discussion
Trauma in children is one of the major health problems that threat the life of children. Timely trauma care has an important role in surviving the patients. The scoring systems can be used for timely delivering medical support and preparing the patient for surgery in early stage.8 The most frequently used ones are general scoring systems used in both adult and pediatric patients. In our study, we evaluated the relation of ISS, NISS, RTS with mortality, hospital LOS and need for surgery in pediatric patients. This study is the first research which aimed to examine the performance of ISS and NISS as anatomic scoring systems in comparison with RTS as a physiological scoring system in predicting need to surgery beside the hospital LOS and mortality. In this study, RTS showed highest sensitivity and specificity at cut-off value of ≥4.8 for mortality. In hospital LOS and need for surgery outcomes, ISS had highest value at cut-off ≤12.5 and ≤ 16.5, respectively.
According to our findings, RTS showed highest sensitivity (99%) at cut-off value of ≥4.8 for predicting mortality. On the other hand, ISS has sensitivity of 92% and specificity of 65% at cut-off ≤15 in predicting mortality. Also, NISS has sensitivity of 91% and specificity of 65% at cut-off ≤17.5. In comparing these two scores in pediatric trauma patients, Grisoni et al.18 found similar predictive values for ISS and NISS for mortality. The findings of a study showed that NISS had sensitivity of 53.3% at cut-off value ≤39.5 and specificity of 54.3% for predicting mortality.8 The observed difference in cut-off value of anatomic scoring systems between our study and other study can be due to delay in delivering the medical care to injured patients.
Although the sensitivity and specificity values of ISS and NISS were similar, the findings of some previous studies showed that in pediatric trauma patients who were not severely injured, the NISS performed as well as the ISS in predicting mortality.19 From clinical point of view, NISS has several advantages over the ISS. In all injuries, NISS gives equal priority even if injuries occur in the same body region.20
Our findings showed that the AUC value of ISS and NISS were similar and greater than RTS value of AUC. This is discordant with Tamim et al. findings which have shown that ISS had a better performance than NISS in predicting the length of hospital stay.21 On the other hand, some studies have shown that NISS has better performance in predicting hospital LOS than ISS.9, 10
In our study, 5.75% of patients need for surgery. In a study, emergency operation was done in 17% of patients.22 Although the RTS as a physiological scoring system had higher predicting AUC value in predicting mortality, the anatomic scoring systems of ISS and NISS had good performance in predicting hospital LOS and need for surgery. In a study by Kaufmann et al.23 the ability of RTS in predicting the need for operation was considerable. According to findings of the meta-analysis study, earlier surgery was associated with a lower risk of death.
In addition, it seems that there is a need for more research to examine the scoring system ability in predicting the hospital LOS and need for surgery in traumatic patients.
RTS as a physiological scoring system has higher predicting AUC value in predicting mortality. The anatomic scoring systems of ISS and NISS have good performance in predicting hospital LOS and need for surgery.
Acknowledgment
The authors would like to express their gratitude to Poursina Hospital, Guilan University of Medical Sciences.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Krug E.G., Sharma G.K., Lozano R. The global burden of injuries. Am J Public Health. 2000;90:523–526. doi: 10.2105/ajph.90.4.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gomes E., Araújo R., Carneiro A. Mortality distribution in a trauma system: from data to health policy recommendations. Eur J Trauma Emerg Surg. 2008;34:561–569. doi: 10.1007/s00068-007-6189-3. [DOI] [PubMed] [Google Scholar]
- 3.Cooper A., Barlow B., Davidson L. Epidemiology of pediatric trauma: importance of population-based statistics. J Pediatr Surg. 1992;27:149–154. doi: 10.1016/0022-3468(92)90303-o. [DOI] [PubMed] [Google Scholar]
- 4.Engum S.A., Mitchell M.K., Scherer L.R. Prehospital triage in the injured pediatric patient. J Pediatr Surg. 2000;35:82–87. doi: 10.1016/s0022-3468(00)80019-6. [DOI] [PubMed] [Google Scholar]
- 5.Athey J., Dean J.M., Ball J. Ability of hospitals to care for pediatric emergency patients. Pediatr Emerg Care. 2001;17:170–174. doi: 10.1097/00006565-200106000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Lefering R. Trauma scoring systems. Curr Opin Crit care. 2012;18:637–640. doi: 10.1097/MCC.0b013e3283585356. [DOI] [PubMed] [Google Scholar]
- 7.Tohira H., Jacobs I., Mountain D. Systematic review of predictive performance of injury severity scoring tools. Scand J Trauma Resusc Emerg Med. 2012;20:63. doi: 10.1186/1757-7241-20-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Gamasy M.A., Elezz A.A., Basuni A.S. Pediatric trauma BIG score: predicting mortality in polytraumatized pediatric patients. Indian J Crit Care Med. 2016;20:640–646. doi: 10.4103/0972-5229.194011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balogh Z.J., Varga E., Tomka J. The new injury severity score is a better predictor of extended hospitalization and intensive care unit admission than the injury severity score in patients with multiple orthopaedic injuries. J Orthop Trauma. 2003;17:508–512. doi: 10.1097/00005131-200308000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Lavoie A., Moore L., LeSage N. The injury severity score or the new injury severity score for predicting intensive care unit admission and hospital length of stay? Injury. 2005;36:477–483. doi: 10.1016/j.injury.2004.09.039. [DOI] [PubMed] [Google Scholar]
- 11.Sauaia A., Moore F.A., Moore E.E. Epidemiology of trauma deaths: a reassessment. J Trauma. 1995;38:185–193. doi: 10.1097/00005373-199502000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Campbell I.W., Nairn M. Management of diabetes. Br J Diabetes Vasc Dis. 2002;2:50–52. [Google Scholar]
- 13.Chalfin D.B., Trzeciak S., Likourezos A. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]
- 14.Ruchholtz S., Lefering R., Paffrath T. Reduction in mortality of severely injured patients in Germany. Dtsch Arztebl Int. 2008;105:225–231. doi: 10.3238/arztebl.2008.0225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bottle A., Aylin P. Mortality associated with delay in operation after hip fracture: observational study. BMJ. 2006;332:947–951. doi: 10.1136/bmj.38790.468519.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamlet W.P., Lieberman J.R., Freedman E.L. Influence of health status and the timing of surgery on mortality in hip fracture patients. Am J Orthop (Belle Mead NJ) 1997;26:621–627. [PubMed] [Google Scholar]
- 17.Kingston R., O'Flanagan S.J. Scoring systems in trauma. Ir J Med Sci. 2000;169:168–172. doi: 10.1007/BF03167688. [DOI] [PubMed] [Google Scholar]
- 18.Champion H.R., Sacco W.J., Copes W.S. A revision of the trauma score. J Trauma. 1989;29:623–629. doi: 10.1097/00005373-198905000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Sullivan T., Haider A., DiRusso S.M. Prediction of mortality in pediatric trauma patients: new injury severity score outperforms injury severity score in the severely injured. J Trauma. 2003;55:1083–1088. doi: 10.1097/01.TA.0000102175.58306.2A. [DOI] [PubMed] [Google Scholar]
- 20.Bulut M., Koksal O., Korkmaz A. Childhood falls: characteristics, outcome, and comparison of the injury severity score and new injury severity score. Emerg Med J. 2006;23:540–545. doi: 10.1136/emj.2005.029439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tamim H., Al Hazzouri A.Z., Mahfoud Z. The injury severity score or the new injury severity score for predicting mortality, intensive care unit admission and length of hospital stay: experience from a university hospital in a developing country. Injury. 2008;39:115–120. doi: 10.1016/j.injury.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 22.Narcı A., Solak O., Turhan-Haktanır N. The prognostic importance of trauma scoring systems in pediatric patients. Pediatr Surg Int. 2009;25:25–30. doi: 10.1007/s00383-008-2287-5. [DOI] [PubMed] [Google Scholar]
- 23.Simunovic N., Devereaux P., Sprague S. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ. 2010;182:1609–1616. doi: 10.1503/cmaj.092220. [DOI] [PMC free article] [PubMed] [Google Scholar]