Abstract
Objective
To evaluate the efficacy of a telephone-delivered, home-based cognitive behavioral intervention for chronic low back pain in comparison to a matched supportive care treatment.
Methods
Participants (N=66) were patients with chronic back pain that were randomized to either an 8-week Cognitive-Behavioral Therapy (CBT) or a Supportive Care condition (SC) matched for contact frequency, format, and time. Participants completed validated measures of improvement in back pain disability, pain severity, and overall improvement.
Results
Intent-to-treat analyses at post-treatment showed that the treatment groups showed non-significantly different improvements in back pain disability (mean changes=−2.4 & −2.6 for CBT & SC, respectively; Cohen’s d’s=.49 & .55, respectively) and reductions in pain severity (mean changes=−.9 & −1.4 for CBT & SC respectively; Cohen’s d’s=.50, & .90, respectively). Participants rated their overall improvement levels at 31% (CBT) versus 18.5% (SC).
Discussion
Results from this clinical trial suggest that home-based, telephone-delivered CBT and SC treatments did not significantly differ in their benefits for back pain severity and disability, and may warrant further research for applications to hospital settings. Major limitations included recruitment difficulties that underpowered primary analyses, the lack of objectives improvement measures, and the absence of a usual care/untreated control group for comparisons.
Keywords: Chronic back pain, randomized clinical trial, cognitive behavioral therapy
Introduction
The need for effective behavioral treatments for the management of chronic back pain has arguably never been greater. The prevalence of chronic back pain has increased in the U.S. population over the past decade (1–2), suggesting a need for more treatment resources directed to pain (3–4). Further, there are increasing concerns regarding the use of common current pharmacological approaches to chronic back pain – concerns such as the adverse consequences associated with long-term use of opioids – that may limit treatment options (5, 3–4).
An emerging alternative approach for treating chronic pain is the use of telehealth interventions (e.g., 6). Telehealth treatments apply empirically supported chronic pain treatment modalities (6–7) in a format that allows for a regularity of contact and accessibility of treatment unsustainable in a usual model of in-clinic care. Telehealth technologies include modalities such as telephone, internet-based, and smartphone applications (7). One recent review (8) focused on telehealth interventions for chronic pain specifically in older adults. These and other recent reviews (7–9) reported evidence of mild to moderate efficacy of telehealth modalities for improving pain management outcomes, but also noted considerable study heterogeneity in design and results, a frequent absence of data regarding treatment time and participation levels, limited evidence regarding the relative efficacy of the different telehealth approaches, and a lack of data regarding how telehealth treatments compare to traditional in person treatments. Since these reviews, a 2017 trial (10) compared acceptance and commitment therapy (ACT) delivered in the standard, in person format, to a telephone-based version of ACT. The latter trial reported non-inferior results for the novel, telephone ACT treatment, supporting comparable benefits between the treatment modalities (although that the telephone version of the ACT treatment had higher dropout rates than the in person ACT treatment).
The current paper describes the results of a clinical trial evaluating a telehealth adaptation of cognitive behavioral therapy (CBT) for chronic back pain in comparison to a time and session frequency matched supportive care (SC) psychotherapy. The effectiveness of CBT for chronic pain has been established in prior research, but its efficacy relative to therapies that control for non-specific factors in a telehealth format are unknown. Clarifying the relative benefits of CBT may have implications for the dissemination of telehealth therapies. The study hypotheses were that, relative to the SC condition, CBT treated patients would demonstrate significantly greater improvements in back pain disability (Roland Morris Disability Questionnaire), pain severity (Visual Rating Scale), and greater levels of improvement as defined by ≥25% patient-rated improvement on the Patient Clinical Global Impressions Scale (11).
Materials & Methods
Participants
Participants consisted of adult men and women receiving medical care in the San Diego community during the period of study recruitment. Recruitment commenced July 1, 2008 and concluded December 31, 2011. Participants were recruited by flyers posted in primary care clinic waiting areas, clinician referrals, and paid advertisements in public media. Inclusion criteria included: 1) age 18–75; 2) presence of low back pain (thoracic vertebra #6 or below) associated with degenerative disk disease; 3) Experience of pain “on a daily basis” ≥ 6 months at a minimum intensity ≥4/10 on a 10-point scale. Exclusion factors included patients with major medical conditions such as cancer and heart failure that could confound pain and function-related study endpoints, those with untreated mood (e.g., met criteria for major depressive disorder or bipolar disorder but were not receiving treatment), psychotic, or substance abuse disorders based on a structured psychiatric interview at baseline testing using Diagnostic and Statistical Manual-IV criteria, and those judged by a study physician to require a more intensive pain management approach as determined by chart review or study physician evaluation (e.g., high dose opioid use or markedly impaired function). Participants provided written informed consent prior to randomization and the study was approved by the UCSD Institutional Review Board and VASDHS Research and Development committee.
Study design
The study design consisted of a single blind, randomized controlled trial comparing a Cognitive-Behavioral Therapy (CBT) treatment adapted to a telephone format to a Supportive Care psychotherapy control condition (SC) matched for therapist contact time and session frequency. The CBT and SC treatments were delivered by the same two master’s degree level mental health therapists, working under the supervision of a licensed mental health professional specializing in pain management. The aim of this design was to minimize differences in nonspecific factors of therapy between the CBT and SC treatments (such as therapist competence, patient-therapist alliance, & treatment adherence that are important contributors to the effects of psychotherapy) by standardizing the therapists, treatment training and supervision, and format of treatment. Participants completed in person visits at baseline and at week 8 (post-treatment date). The flowchart in Figure 1 illustrates the pattern of participant screening and enrollment.
Figure 1.
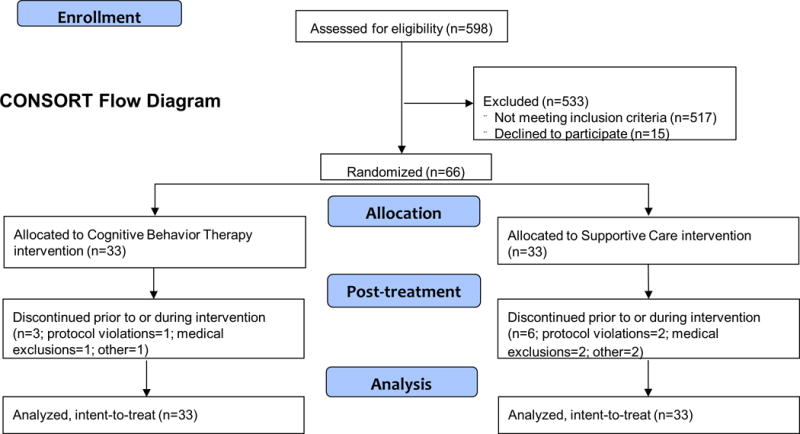
Flowchart of patient enrollment patterns across screening, randomization, and treatment completion stages.
The treatment phase contained 12 total sessions over eight weeks. Treatment session 1 was in clinic, face-to-face, of two hours duration, and introduced the rationale for the interventions. Treatment sessions 2 through 12 were completed by telephone, in 30 minute sessions. Total contact time for both treatments was eight hours.
Cognitive-Behavioral Therapy (CBT)
Each CBT session followed a manualized protocol, with the contents outlined in Table 1. The core content topics included pain management, stress management, cognitive changes, assertive communication, and goal setting. Each content topic in Table 1 was broken up over 2–3 sessions. Participants received a set of structured written materials designed for patients that accompanied each phone session to provide educational information, self-monitoring exercises, and homework assignments (e.g., readings, pain/activity diaries, etc.,). Session relevant homework exercises were assigned at the end of each visit.
Table 1.
Outline of the cognitive behavioral therapy (CBT) telehealth protocol.
A. Managing Pain
|
B. Managing Stress
|
C. Thinking Differently
|
D. Assertive Communication
|
E. Setting Goals for the Future
|
Supportive Care condition (SC)
The SC treatment was a non-directive treatment contrasting with the active and directive approach of the CBT treatment. The core ingredients of the supportive care treatment were: 1) Education by distribution of a standard text, The Back Pain Help Book (12); 2) Active Listening by the therapist to participant’s concerns; 3) Supportive involvement following person centered therapy principles such as expressing empathy for the patients concerns, believing in the patient’s capacity to create their own solutions, and unconditional positive regard for the patient (13); and 4) Recommendations to follow the advice of their caretakers providing usual medical care (e.g., maintaining their current medications and treatment practices).
Treatment fidelity and competence
The two treatment therapists received regular supervision from a licensed mental health provider across the duration of the study to monitor and maintain protocol adherence. Both study therapists (author initials: TCR & SP) had prior experience with psychotherapy for pain management and with delivering manualized treatments in research studies. Clinician fidelity was assessed in the cognitive behavioral and supportive care treatments using audio tapes (with informed consent) reviewed by an independent clinician using standard psychotherapy rating forms (14–15). Fidelity data indicated that the treatment were highly distinct, with sessions ratings >95% consistent with therapy modality.
Treatment Satisfaction
Treatment satisfaction among participants was measured using the Client Satisfaction Questionnaire-Revised (16), an 8-item questionnaire measuring satisfaction with health care treatment on a four-point Likert scale (1 = quite dissatisfied; 4 = very satisfied).
Study outcome measures
A study assistant blind to treatment assignment collected the baseline and treatment outcome data, with participants instructed not to reveal details about their treatment to the study assistant prior to assessment. Participants completed several outcome measures recommended by the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT; 17). This included the Roland-Morris Disability Questionnaire (RMDQ, Cronbach’s α=0.84–0.96; 18), a 24-item measure assessing pain interference with everyday function with demonstrated validity and responsiveness to change and the Numerical Rating Scale (NRS, Cronbach’s α=0.84–0.98; 17), a consensus measure of pain intensity measured on an 11-point scale (i.e., 0=No Pain, 10= Pain as bad as you can imagine in reference to their average pain during the previous week). The assistant also used a modification of the Patient Clinical Global Impressions Scale [CGI; 11] as a study outcome. The CGI is a self-rated outcome, based on the patient’s overall assessment of change in terms of pain intensity and its impact on everyday function. The modified version asked participants to rate themselves as “better,” “worse,” or “about the same” at each assessment. Thereafter, the individual was directed to rate the percentage of change from “0 to 100%.” In cases where a participant rated themselves as “about the same”, percentage change was coded as 0%. The study protocol also included supplementary measures of depression, anxiety, and quality of life that are not reported here because they were not part of the study’s a priori hypotheses.
Statistical analyses
This trial was powered at the ≥.80 level to detect statistically significant differences between the CBT and SC conditions based on a projected N=130 (using the same projected effect sizes, alpha level, and sample of N=66 that we actually obtained, our a priori power level for detecting between group differences would have been ~.63). Power calculations were made based on the RMDQ, the pre-specified primary outcome for the grant supporting the study (NCT00608530). The pain severity and CGI measure measures were also specified in the project grant as secondary outcomes. Participants were randomly allocated to experimental or control study groups on a sequential basis using standard computer generated random number tables and allocation algorithms. Because we expected a skewed distribution of gender, randomization was performed within gender to obtain equal representation across conditions (stratified random). Upon eligibility, the statistician provided the treatment assignment to the study coordinator for implementation.
Percentages, means, and standard deviations were used to describe demographic and pain characteristics of the sample. Primary analyses consisted of intent-to-treat analyses among randomized participants using between-within analysis of variance tests and chi-square tests comparing the CBT and SC conditions. Using SPSS software (version 23; SPSS.com) we used multiple imputation to address missing data in study outcomes. This procedure resulted in an initial set of five imputations that were then pooled for the final analyses. As measures of clinical significance, we report pre to post-treatment changes (i.e., within group changes) in effect sizes (Cohen’s d) for the RMDQ and NRS outcomes. Statistical testing was performed using two-tailed tests and alpha level of .05 for declaring statistical significance.
Results
Participant flow
Recruitment staff responded to study inquiries by conducting telephone screening of 598 potential participants, evaluating 118 individuals in person, and randomizing 66 to treatment. This number was substantially smaller than our projected sample size of 130. Figure 1 depicts the progress of volunteers through the trial.
Feasibility analyses
Participants completed >90% of planned telephone treatment sessions in both conditions. SC participants completed an average of 10.8 (.76) out of a maximum of 11 telephone sessions, whereas CBT participants completed an average of 10.0 (2.2)/11 sessions. The median and modal average attendance values were 11/11 for both conditions. Participants in the supportive care (SC) condition (mean=3.2[.60]) reported treatment satisfaction levels similar to those in the CBT treatment (mean=3.5[.60]), p>.05. Among the total of nine randomized participants that withdrew during treatment, 6/9 were due to protocol violations (e.g., initiating new pain therapies) or new medical concerns; the other three participants dropped for unspecified reasons.
Fifty of the 66 randomized participants completed the eight week treatment (75.7% overall completion rate; 66.7% completion among CBT participants versus 84.8% completion among SC participants, p>.10 for difference). There were no differences between the completers and non-completers of treatment on demographic characteristics or RMDQ/NRS scores (all p’s>.05). No adverse events were reported by participants during the trial. Table 2 describes baseline demographic characteristics for the sample. There were no significant differences at baseline between the two treatment groups.
Table 2.
Characteristics of randomized participants (N=66).
| Variable | Supportive care (n=33) | Cognitive behavior therapy (n=33) |
|---|---|---|
| Gender (% female) | 39.4 | 37.5 |
| Marital status (% married) | 66.7 | 53.1 |
| Race (% Non-white) | 27.3 | 40.6 |
| Age (mean[standard deviation]) | 52.6(12.5) | 54.0(14.8) |
| Education (% college grad or higher) | 90.6 | 72.7 |
| VA Healthcare (% yes) | 21.2 | 18.8 |
Intent-to-treat analyses
Table 3 describes results of the RMDQ, NRS, and CGI. Although participants in both treatment groups showed within group statistically significant pre- to post-treatment improvements, there were no significant between group differences on these measures. Effect sizes (Cohen’s d values) for both groups were in the moderate range. Differences in self-rated improvement on the CGI were also nonsignificant (p>.10).
Table 3.
Baseline and post-treatment (8-week) scores (means [standard deviations]) on measures of back pain disability and pain severity among participants (N=66).
| Back Pain Disabilitya | ||||
|---|---|---|---|---|
| Group | Baseline | 8 weeks | Cohen’sd | |
| Total sample | 10.2(4.5) | 7.7(4.9)* | .53 | |
| CBT1 (n=33) | 10.0(4.7) | 7.6(5.0)* | .49 | |
| SC2 (n=33) | 10.4(4.4) | 7.8(5.0)* | .55 | |
| Pain Severityb | ||||
| Group | Baseline | 8 weeks | Cohen’sd | |
| Total sample | 5.3(1.7) | 4.1(1.6)* | .73 | |
| CBT1 (n=33) | 5.0(1.8) | 4.1(1.8)* | .50 | |
| SC2 (n=33) | 5.5(1.6) | 4.1(1.5)* | .90 | |
| % Self-rated Improvementc | ||||
| Group | Baseline | 8 weeks | ||
| Total sample | NA | 24.5% (27.2) | ||
| CBT1 (n=33) | NA | 31.0% (30.4) | ||
| SC2 (n=33) | NA | 18.5% (22.7) | ||
=Cognitive-Behavioral Therapy
=Supportive Care
=Roland-Morris Disability Questionnaire
=Numerical Rating Scale
=Global Clinical Impressions;
Significant changes from baseline to post-treatment scores, p<.05.
Discussion
In this clinical trial of patients with chronic low back pain receiving one of two telephone-adapted forms of psychotherapy treatment, intent-to-treat analyses showed that those receiving a the CBT treatment showed patterns of treatment participation, treatment satisfaction, and patient self-reported improvements that were generally comparable to patients receiving a parallel SC treatment. Significant pre to post-treatment reductions in back pain disability and pain severity were observed in both conditions, with effect sizes in the moderate range based on conventional standards (i.e., Cohen’s d values in the .5–.9 range). Combined with the data suggesting a high level of tolerability with the treatments, these results support the feasibility and potential efficacy of phone-adapted psychotherapy treatments among patients with chronic back pain, and encourage further research, while also highlighting possible challenges in successfully recruiting eligible patients (as demonstrated by our recruitment struggles and consequent poor statistical power for detecting hypothesized group differences) for these non-medical therapies.
The current study represented a telephone format extension of a previous treatment trial carried out by this research team in which an acute low back pain population participating in an orthopedic clinic received an in person CBT treatment (19). In this previous trial, patients in the active treatment showed significantly greater rates of recovery (i.e., less progression to chronic pain) versus an attentional control condition. The telephone methods employed in the current study was designed to evaluate the CBT treatment in a modality reflecting current treatment trends towards technology-based interventions and providing a stronger comparison group in the form of the SC treatment. As summarized in recent reviews of telehealth interventions for pain (e.g., 7–8), telephone therapies such as those employed here are just one of a growing number of evolving smartphone, video-based, and internet and social media modalities. Relative to existing studies in this area and documented limitations in existing research this study: 1) standardized the delivery of the telehealth intervention (both treatments were treated exclusively via telephone and matched for time and session numbers); and 2) adapted the telehealth treatment in a structured, replicable format using a manualized intervention. In contrast, our study, unlike some other recent telehealth trials (e.g., 10) did not contain an in person CBT or SC arm against which to compare the interventions, or incorporate technologies such as smartphones, health sensors, or internet-based applications popular in current mobile health research (20). An ongoing challenge for research in this field is developing methods for rapidly evaluating fast changing telehealth modalities while maintaining scientific standards.
The focus of this study on chronic back pain was based on prior research showing that chronic back pain is one of the most prevalent conditions in settings such as primary care [21–22). Because chronic back pain is by definition treatment-resistant, it can create a strain for time-limited primary care providers to address, fostering a potential overreliance on opioids and other pharmacological treatment options that dispose additional long-term problems [23, 3–4]. For this reason, cost-effective behavioral treatments suitable for patients with chronic back pain have high potential value in modern hospital settings.
There are a handful of clinical trials using psychotherapies to date targeting populations with chronic back using a telephone treatment format against which to compare our population and findings. For example, relative to a 2014 telecare intervention for chronic pain in primary care trial (7), the baseline pain severity and reductions in pain severity we observed in response to treatment were similar (mean 5.3/10 to 4.5/10 after 3 months [7] vs. a mean of 5.3/10 to 4.1/10 in the current study). Similarly, the baseline severity of pain disability measured by the RMDQ was comparable to normative data for chronic low back pain populations (mean of 12.1 and standard deviations of 4–7–6.2, vs. a baseline mean and sd of 10.2[4.5] in the current study) published by the instrument authors (24). Finally, in a 2012 trial of telephone-adapted CBT (25) that targeted patients with widespread chronic pain (fibromyalgia), the authors reported significantly better treatment outcomes relative to a treatment as usual control group at end of treatment and at three months post-treatment. The latter study also included a third group, exercise treatment condition, involving an in person orientation with a personal trainer and monthly in person follow-up visits with the trainer to reinforce progress, observing similar improvements in the telephone CBT treatment and exercise program. Combining this latter trial and the present study results, there is accumulating data to suggest that telephone forms of CBT and SC therapy are effective and well tolerated by patients for a range of chronic pain diagnoses.
The comparison of telehealth adapted versions of CBT and an active control condition in the form of SC was one of the novel aspects of this study. The lack of differences we observed on study outcomes between the treatment conditions can be interpreted in at least several ways. For example, it is possible that a larger sample and adequate statistical power would have revealed group differences; however, the mostly comparable effect sizes we found do not support this theory. It is also possible that the conversion to a telehealth format either sacrificed some important elements of CBT (e.g., reduced accountability or self-monitoring structure) or added some important elements to SC (e.g., the regular appointments and visit times may have unintentionally created a sense of structure that promoted improvements). Future studies of telehealth CBT and related therapies will be necessary to address this question.
Limitations
Interpretation of the present trial results warrants several important cautions. The study fell substantially short of its targeted sample size of N=130, limiting statistical power to detect hypothesized group differences. The recruitment difficulties we encountered may reflect upon the stringent entrance criteria (only about 1/5 study inquiries led to a successful in person screening visit. Most commonly, prospective study subjects did not meet enrollment criteria due to not reporting daily pain levels at the ≥4/10 level). This study targeted patients with chronic pain without severe psychiatric or psychosocial impairments for whom our low intensiveness treatment was not perceived as appropriate. This focus limits the generalizability of the findings to patients with similar demographic and psychosocial profiles. Although we used IMMPACT recommended self-report measures of pain and mood in the protocol, we did not include more objective measures of functional change such as the 5-minute walk test or measure possible changes in medication or hospital utilization. The study did not employ a usual care condition because our aim was to determine if CBT was superior to a supportive, non-directive approach in a telephone format. The absence of a no treatment reference group made it more difficult to establish the overall efficacy of the CBT and SC conditions as back pain can sometimes show improvement even without an active intervention.
Summary
In a sample of patients with chronic back pain, participants receiving a telephone-delivered form of CBT versus SC therapy demonstrated statistically significant and comparable patterns of improved outcomes on measures of back pain disability, pain severity, and self-rated improvement. Both treatments were well-tolerated, with strong participation and treatment satisfaction ratings. With chronic back pain among the most common presentations in hospital settings, and a condition for which physicians are increasingly encouraged to consider non-pharmacological approaches for management, further research on the development of telehealth treatments such as that demonstrated in this trial work is an important objective.
Supplementary Material
Acknowledgments
This research was supported by the Office of Research and Development, Rehabilitation Research and Development Service, Department of Veterans Affairs. The funding organization was not involved in the 1) design and conduct of the study; 2) collection, management, analysis, and interpretation of the data; 3) preparation, review, or approval of the manuscript; or 4) decision to submit the manuscript for publication.
This research was supported by the Office of Research and Development, Rehabilitation Research and Development Service, Department of Veterans Affairs. The funding source had no role in data analysis or development of this manuscript.
Footnotes
Trial Registry: ClinicalTrials.gov NCT00608530.
Conflict of interest statement: All authors declared no study-related conflicts of interest in the development of this manuscript.
Author declaration: All listed authors had full access to the data for this manuscript and contributed directly to the development of the manuscript through writing, editorial review, and statistical analyses. The corresponding author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Rutledge and Dr. Slater conducted all study analyses and assembled the tables and figures for the manuscript.
References
- 1.Institute of Medicine Report from the Committee on Advancing Pain Research, Care, and Education: Relieving Pain in America, A Blueprint for Transforming Prevention, Care, Education and Research. The National Academies Press; 2011. [PubMed] [Google Scholar]
- 2.Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. Journal of Pain. 2010;11:1230–1239. doi: 10.1016/j.jpain.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Internal Medicine. 2013;173:1573–1581. doi: 10.1001/jamainternmed.2013.8992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sullivan MD, Howe CQ. Opioid therapy for chronic pain in the United States: promises and perils. Pain. 2013;154:S94–100. doi: 10.1016/j.pain.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garland EL, Froeliger B, Zeidan F, Partin K, Howard MO. The downward spiral of chronic pain, prescription opioid misuse, and addiction: cognitive, affective, and neuropsychopharmacologic pathways. Neuroscience & Biobehavioral Review. 2013;37:2597–607. doi: 10.1016/j.neubiorev.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kroenke K, Krebs EE, Wu J, Yu Z, Chumbler NR, Bair MJ. Telecare collaborative management of chronic pain in primary care: a randomized clinical trial. JAMA. 2014;312:240–248. doi: 10.1001/jama.2014.7689. [DOI] [PubMed] [Google Scholar]
- 7.Heapy AA, Higgins DM, Cervone D, Wandner L, Fenton B, Kerns RD. A Systematic Review of Technology-assisted Self-Management Interventions for Chronic Pain: Looking Across Treatment Modalities. Clin J Pain. 2015;31:470–492. doi: 10.1097/AJP.0000000000000185. [DOI] [PubMed] [Google Scholar]
- 8.Bhattarai P, Phillips JL. The role of digital health technologies in management of pain in older people: An integrative review. Archives of Gerontology and Geriatrics. 2017;68:14–24. doi: 10.1016/j.archger.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Dario AB, Moreti Cabral A, Almeida L, Ferreira ML, Refshauge K, Simic M, Pappas E, Ferreira PH. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: systematic review with meta-analysis. Spine J. 2017 Apr 13; doi: 10.1016/j.spinee.2017.04.008. pii: S1529-9430(17)30142-0. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 10.Herbert MS, Afari N, Liu L, Heppner P, Rutledge T, Williams K, Eraly S, VanBuskirk K, Nguyen C, Bondi M, Atkinson JH, Golshan S, Wetherell JL. Telehealth versus in-person acceptance and commitment therapy for chronic pain: A randomized noninferiority trial. Journal of Pain. 2017;18:200–211. doi: 10.1016/j.jpain.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 11.Busner J, Targum SD. The Clinical Global Impressions Scale: Applying a Research Tool in Clinical Practice. Psychiatry. 2007;4:28–37. [PMC free article] [PubMed] [Google Scholar]
- 12.Moore JE, Von Korff M, Lorig K, Gonzalez VM, Laurent DD. Back Pain Helpbook: A Proven Self-Care Program for Managing Chronic or Recurrent Back Pain. Cambridge, MA: Perseus Publishing; 1999. [Google Scholar]
- 13.Rogers CR, Stevens B. Person to person: the problem of being human; a new trend in psychology. Walnut Creek: Real People Press; 1967. [Google Scholar]
- 14.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. Journal of Behavior Therapy and Experimental Psychiatry. 2000;31:73–86. doi: 10.1016/s0005-7916(00)00012-4. 2000. [DOI] [PubMed] [Google Scholar]
- 15.McGrew JH, Bond GR, Dietzen L, Salyers M. Measuring the fidelity of implementation of a mental health program model. Journal of Consulting and Clinical Psychology. 1994;62:670–678. doi: 10.1037//0022-006x.62.4.670. [DOI] [PubMed] [Google Scholar]
- 16.Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Evaluation Program Planning. 1979;2:197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- 17.Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, Kerns RD, Stucki G, Allen RR, Bellamy N, Carr DB, Chandler J, Cowan P, Dionne R, Galer BS, Hertz S, Jadad AR, Kramer LD, Manning DC, Martin S, McCormick CG, McDermott MP, McGrath P, Quessy S, Rappaport BA, Robbins W, Robinson JP, Rothman M, Royal MA, Simon L, Stauffer JW, Stein W, Tollett J, Wernicke J, Witter J. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19. doi: 10.1016/j.pain.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 18.Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–144. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Slater MA, Weickgenant AL, Greenberg MA, Wahlgren DR, Williams RA, Carter C, Patterson TL, Grant I, Garfin SR, Webster JS, Atkinson JH. Preventing progression to chronicity in first onset, subacute low back pain: an exploratory study. Archive of Physical Medicine and Rehabilitation. 2009;90:545–552. doi: 10.1016/j.apmr.2008.10.032. [DOI] [PubMed] [Google Scholar]
- 20.Silva BMC, Rodrigues JPC, de la Torres Diez I, Lopez-Coronado M, Saleem K. Mobile-health: a review of current state in 2015. Journal of Biomedical Informatics. 2015;56:265–272. doi: 10.1016/j.jbi.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Frank JW, Bair MJ, Becker WC, Krebs EE, Liebschutz JM, Alford DP. Update in pain medicine for primary care providers: a narrative review, 2010-2012. Pain Med. 2014;15:425–31. doi: 10.1111/pme.12337. [DOI] [PubMed] [Google Scholar]
- 22.Lalonde L, Choinière M, Martin E, Berbiche D, Perreault S, Lussier D. Costs of moderate to severe chronic pain in primary care patients – a study of the ACCORD Program. J Pain Res. 2014;7:389–403. doi: 10.2147/JPR.S55388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Leon-Casasola OA. Opioids for chronic pain: new evidence, new strategies, safe prescribing. Am J Med. 2013;126:S3–11. doi: 10.1016/j.amjmed.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 24.Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000;25:3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 25.McBeth J, Prescott G, Scotland G, Lovell K, Keeley P, Hannaford P, McNamee P, Symmons DP, Woby S, Gkazinou C, Beasley M, Macfarlane GJ. Cognitive behavior therapy, exercise, or both for treating chronic widespread pain. Archives of Internal Medicine. 2012;172:48–57. doi: 10.1001/archinternmed.2011.555. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


