Abstract
Objectives
To evaluate the relationship between back pain severe enough to restrict activity (restricting back pain) and subsequent disability in essential (e) and instrumental (i) activities of daily living (ADL) among community-living older adults.
Methods
In this prospective cohort study, we evaluated 754 adults, aged ≥70 years who were initially nondisabled in eADLs. Restricting back pain and disability were assessed during monthly interviews for up to 159 months. Associations between restricting back pain and subsequent eADL and iADL disability were evaluated using recurrent events Cox models, adjusted for fixed-in-time and time-varying covariates.
Results
Strong associations were found between restricting back pain and eADL and iADL disability, with HR (95%CI) of 3.47 (3.01,3.90) and 2.33 (2.08,2.61) respectively.
Conclusions
Restricting back pain was independently associated with subsequent disability in eADLs and iADLs. Interventions focused on decreasing restricting back pain in older adults have the potential to reduce the subsequent burden of disability.
Keywords: Aged, Back Pain, Disability, Activities Daily Living, Cohort Studies
Introduction
Back pain is the most frequent type of pain and among the most common complaints leading to a clinic visit.(1) We previously reported that back pain severe enough to restrict activities, hereafter referred to as restricting back pain, is common in older adults, with over 77% reporting an episode over 10+ years; episodes were often short-lived, lasting an average of one month,(2) and typically recurrent.(3) Based on 2005 dollars, the US spends over $100 billion for direct and indirect costs related to back pain,(4) and these costs are expected to rise as the prevalence of back pain increases.(5) Over the last decade, both diagnostic and therapeutic costs for back pain have escalated, but outcomes have not improved.(6, 7)
While back pain is highly prevalent and costly, longitudinal data evaluating its functional consequences in older adults are limited. Understanding the various ways that back pain impacts older adults is important as it can help guide appropriate outcome assessments as well as management approaches.(6, 8, 9) In 2014, experts and leaders in the field of chronic back pain published the NIH Task Force on Research Standards for Low Back Pain.(9) This report emphasized the importance of evaluating physical function as it relates to back pain.(9)
Activities of daily living (ADL), both essential and instrumental, are fundamental to maintaining independence in older adults. Disability is commonly assessed in the literature by inability to perform ADLs. It has been reported that 9% of the US population over 65 years of age has one or more disabilities in ADLs.(10) Those who lose the ability to perform ADLs are more likely to become institutionalized, have higher rates of morbidity, mortality, and experience poorer quality of life.(11–13) Several cross-sectional studies have demonstrated a strong relationship between pain, functional limitations and disability in ADLs.(14–16) Given the dynamic nature of pain and disability, longitudinal data are needed that will appropriately capture changes in these clinical phenomena.(17)
Few longitudinal studies have evaluated back pain and subsequent ADL disability in both older men and women. We have shown a significant association between restricting back pain and subsequent mobility disability in community-living older adults using longitudinal data.(18) To gain a more comprehensive understanding of the deleterious effects of restricting back pain in older adults, we sought to evaluate the associations between restricting back pain and both essential (e) and instrumental (i) ADL disability. We used data from a unique longitudinal study that includes monthly assessments of both restricting back pain and disability for more than 13 years in a large cohort of older community-living men and women. A better understanding of the impact of restricting back pain on eADL and iADL disability would provide additional evidence to support the need for interventions to improve clinical outcomes in this population.
Methods
Study Population
Participants were drawn from the Precipitating Events Project (PEP), a longitudinal study of 754 community-living adults, aged 70 and older, who were initially nondisabled in their eADLs: bathing, dressing, walking inside the house, and transferring from a chair. (19) Exclusion criteria were inability to speak English, significant cognitive impairment with no available proxy, (17) life expectancy less than 12 months, and plans to move out of the area. Based on initial sample size calculations, physically frail adults were oversampled in PEP. Of 2753 potential participants, only 4.6% of persons refused screening, and 75.2% of those eligible agreed to participate and were enrolled from March 1998 to October 1999. Those who refused to participate did not differ significantly from those who were enrolled in terms of age or sex.(19) The study protocol was approved by the Yale Human Investigation Committee.
Data Collection
Comprehensive home-based assessments were completed at baseline and every 18-months for up to 144 months, while telephone interviews were completed monthly through June 2011, with a completion rate of 99%. For participants with significant cognitive impairment or who were not available, a proxy was interviewed using a standardized protocol. (17) Deaths were ascertained from the local obituaries and/or an informant during a subsequent interview. Four hundred ninety-three (65%) participants died after a median follow-up of 82 months, and 38 (5.0%) dropped out of the study after a median follow-up of 26 months. Data were otherwise available for 98.4% of the 4175 comprehensive assessments and 98.5% of the 75,340 monthly interviews.
Restricting Back Pain
Back pain leading to restricted activity (restricting back pain), the independent variable, was assessed during monthly interviews with the following series of questions. Each month, participants were asked"Since we last talked [one month ago], have you stayed in bed at least half the day due to an illness, injury, or other problem?” and"Have you cut down on your usual activities due to an illness, injury, or other problem?” Participants who answered yes to either question were considered to have restricted activity and were subsequently asked whether their restricted activity was due to back pain. Test-retest reliability for restricting back pain was high, with kappa = 0.84.(20) The referent group included participants who did not have restricted activity, regardless of whether they had back pain, as this was not assessed in the absence of restricted activity.
Disability in Activities of Daily Living
Disability, the dependent variable, was defined for eADL as: dependence in bathing, dressing, walking inside the house, and transferring from a chair; and for iADL as: dependence in doing housework, preparing meals, and shopping. Each month, participants were asked"At the present time, do you need help from another person to [complete the task]?” for each of the eADLs and iADLs. Participants who reported"Yes” or “Unable to complete the task” were considered to have disability. For both eADLs and iADLs, an episode of disability was defined as disability in any of the relevant tasks that had to be preceded by a month with no disability. Among a subgroup of participants interviewed twice within a 2-day period by different interviewers (n=91), the test-retest reliability was substantial for eADL with a kappa of 0.75 and moderate for iADL disability with a kappa of 0.46.(17, 21)
Covariates
Data were collected on several covariates during the comprehensive assessments and dichotomized to assist in clinical interpretation.(22) Covariates were selected based on known associations with adverse functional outcomes.(18, 19, 22, 23) Demographic characteristics included age, sex, race/ethnicity, living situation, and education. Cognitive status was assessed by the Folstein Mini-Mental State Examination (MMSE).(24) Depressive symptoms were assessed by the Center for Epidemiologic Studies Depression (CES-D) scale.(25) Nine self-reported, physician-diagnosed chronic conditions were assessed: arthritis, hypertension, diabetes mellitus, myocardial infarction, chronic lung disease, cancer, stroke, congestive heart failure, and hip fracture. Body mass index (BMI) was calculated using participants’ self-reported height and weight, according to the World Health Organization definition. Physical frailty was defined by slow gait speed, as previously described.(17) Lower extremity (hip) weakness, an independent risk factor for restricting back pain, was assessed with a hand-held Chatillon MSE 100 dynamometer (AMATEK Measurement and Calibration, Largo, Florida).(26) The cut points demarcated the worst sex-specific quartile for the nondominant limb, on the basis of the first 356 enrolled participants randomly selected from the source population.(22) Table 1 provides additional operational details of the covariates.
Table 1.
Baseline Characteristics of Study Participants in Two Analytic Samples
| Characteristic | Operational Details |
eADL (n =754) n (%) |
iADL (n = 703) n (%) |
|---|---|---|---|
| Age in years, mean (±SD) | 78.4 (5.3) | 78.1 (5.2) | |
| Female | 487 (64.6) | 449 (63.9) | |
| Non-Hispanic white | 682 (90.5) | 640 (91.0) | |
| Living alone | 298 (39.5) | 276 (39.3) | |
| Did not complete high school | 249 (33.0) | 224 (31.9) | |
| Cognitive impairment | Score on Folstein MMSEa < 24 | 86 (11.4) | 73 (10.4) |
| High depressive symptoms | Score on CES-Db ≥ 16 | 156 (20.7) | 134 (19.1) |
| No. of chronic conditions ≥ 2c | 9 self-reported physician diagnoses | 405 (53.7) | 370 (52.6) |
| Overweight | BMI (kg/m2) ≥ 25 | 450 (59.7) | 425 (60.5) |
| Physical frailty | >10 seconds on rapid gait test(17) | 322 (42.7) | 275 (39.1) |
| Hip (lower extremity) weakness | < 7.9kg (women) or < 12.6kg (men) | 238 (35.8) | 238 (33.8) |
MMSE = Mini-Mental State Examination
CES-D = Center for Epidemiologic Studies Depression Scale
Cut-point was defined on the basis of the frequency distributions in the analytic sample.
Statistical Analysis
Of the 754 participants, all were included in the eADL analysis as all participants were free of eADL disability at baseline. For the iADL analysis, 51 (6.7%) participants reported iADL disability at baseline and throughout the follow-up period and were never at risk for developing a new episode of iADL disability. Therefore, the primary analytic sample for the iADL analysis included the remaining 703 participants, who were at risk for developing iADL disability over the follow-up period.
The baseline characteristics were summarized using means and standard deviations for continuous variables, and frequencies and proportions for categorical variables. The amount of missing data for the covariates ranged from 0 for physical frailty to 3.5% for depressive symptoms, with the exception of hip weakness, for which 10% of the observations were missing. This small amount of missing data were accounted for using multiple imputation with 50 random draws per missing observation. The incidence of disability in eADLs and iADLs was estimated using a Generalized Estimation Equation binomial model. The 95% confidence intervals (CI) were based on empirical standard errors that accounted for the correlation of recurrent events in the same participants.
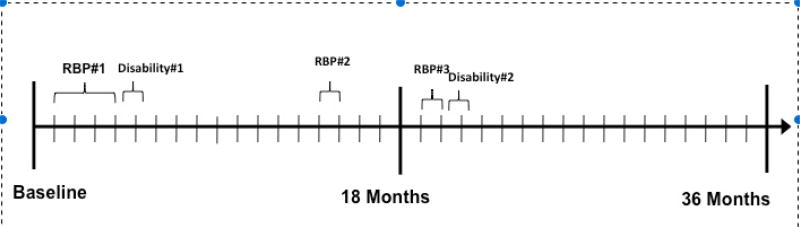
A multivariate Cox model for recurrent events was used to evaluate the association between restricting back pain and incidence of subsequent eADL and iADL disability. Temporal precedence, as depicted in Figure 1, was established, using monthly interviews, by assessing ADL disability “at the present time”, while assessing restricting back pain over the preceding month"Since we last talked [one month ago]…” In this model, participants were at risk for developing recurrent episodes of eADL and iADL disability over the 13+ years of follow-up. All covariates, other than sex and race, were updated every 18-months, and entered into the models as time-dependent variables. The crude and adjusted hazard ratios (HR) (and 95% CIs) for developing eADL and iADL disability were estimated for restricting back pain, with robust sandwich variance estimators to account for the correlation within individuals.(27, 28)
Figure 1. Assessing Association between Restricting Back Pain and Disability Over Time.
Example participant with restricting back pain (RBP) #1 and #3 reported within one month disability in activities of daily living (ADL). RBP#2 is not associated with subsequent disability.
Since prior research shows that women report back pain more frequently than men,(2) we tested for potential statistical interaction between restricting back pain and sex. We also conducted two sets of secondary analyses. First, based on prior work demonstrating that episodes of disability are often short-lasting (i.e. one month or less), we evaluated the association between restricting back pain and eADL and iADL disability that persisted for at least two months (persistent disability).(17) Second, to further strengthen a temporal and potentially causal association, we repeated the primary iADL analysis after excluding participants who had iADL disability at baseline (n=532); all participants were nondisabled in eADLs at baseline, as described above.
All statistical tests were two-tailed, and p<0.05 was considered to indicate statistical significance. All analyses were performed using SAS version 9.1 (SAS Institute, Inc., Cary, NC).
Results
As shown in Table 1, the baseline characteristics of participants in the two analytic samples were comparable. On average, participants were nearly 80 years old; the majority were female, white, and had completed high school. A minority of participants were cognitively impaired or reported depressive symptoms. The majority of participants were overweight. Greater than half of the participants reported two or more chronic conditions, with the most common being hypertension, arthritis, coronary artery disease, or diabetes.
Over a median follow-up of 111 months, the rate (95% CI) of eADL and iADL disability was 3.6 (3.4,3.9) and 8.5 (8.1,9.0) per 100-person months, respectively. Of the 2,269 episodes of eADL disability and 6,103 episodes of iADL disability, the median duration was two months for each (interquartile range, (IQR) 1–4 and 1–5, respectively). The frequency of disability in each of the eADL and iADL tasks is provided in Table 2.
Table 2.
Frequency of Disability in Essential and Instrumental Activities of Daily Living
| eADLa | 16,189 total months of eADL disability |
Frequency in months n (%) per disability task |
|---|---|---|
| Dependence in bathing | 14,554 (89.9%) | |
| Dependence in dressing | 10,717 (66.2%) | |
| Dependence in walking inside the house | 5,682 (35.1%) | |
| iADLb | 44,154 total months of iADL disability | Frequency in months n (%) per disability task |
| Dependence in doing housework | 39,341 (89.1%) | |
| Dependence in preparing meals | 23,622 (53.5%) | |
| Dependence in shopping | 29,848 (67.6%) |
eADL = essential activities of daily living, as defined in the text.
iADL = instrumental activities of daily living, as defined in the text.
Table 3 provides hazard ratios for the association between restricting back pain and eADL and iADL disability in the primary and secondary analyses. In the primary analysis, there was a strong independent association between restricting back pain and eADL and iADL disability, with adjusted HR (95% CI)=3.47 (3.01,3.90) and 2.33 (2.08,2.61) respectively. There was no significant interaction between restricting back pain and sex for either outcome (p=0.57 for eADL and 0.24 for iADL). In the secondary analysis, the results were comparable for persistent disability. When participants with baseline iADL disability were excluded (analytic sample, n=532), there was also a strong independent association between restricting back pain and iADL disability, with adjusted HR (95% CI 2.56 (2.26,2.91).
Table 3.
Associations of Restricting Back Pain and Subsequent Disability
| Hazard Ratio (95% Confidence Interval) |
||
|---|---|---|
| Primary Analysis, Disability | eADL Disabilitya (n = 754) |
iADL Disability (n = 703) |
| Unadjusted | 3.83 (3.83–4.37) | 2.32 (2.05–2.62) |
| Adjustedb | 3.47 (3.01–3.90) | 2.33 (2.08–2.61) |
| Secondary Analysis, Persistent Disabilityc | ||
| Unadjusted | 3.83 (3.20–4.58) | 2.47 (2.12–2.87) |
| Adjusted | 3.62 (2.99–4.37) | 2.54 (2.20–2.93) |
Included all episodes regardless of duration.
Adjusted for age (in years), female sex, non white race, living alone status, less than high school education, depressive symptoms, overweight, physical frailty, cognitive impairment, ≥ 2 chronic conditions, hip weakness. Additional details are provided in the text and Table 1.
Analytic samples are described in the text. Persistent disability refers to e/iADL disability lasting two or more months duration.
Discussion
We found that restricting back pain, commonly reported in older adults,(2) is independently associated with subsequent (within one month) disability in both eADLs and iADLs. These relationships did not differ between men and women. It has become increasingly important to understand back pain in the context of physical function and our study contributes to this literature.
While disability in eADLs and iADLs is associated with increased morbidity,(15, 17) the relationship with restricting back pain is uncertain. In a prior study that used data from the Women’s Health and Aging Study, older women with severe back pain had a higher likelihood of having difficulty with eADLs.(15) However, because this study was cross-sectional and focused on women who were disabled, the directionality of the pain-disability relationship could not be established. Recent longitudinal data found that older individuals with chronic non cancer pain, including spine pain, were not at higher risk of subsequent ADL disability; however, this study was limited by the biannual frequency of assessments and limited characterization of pain.(11) Prior studies that did not show a significant association between [back] pain and subsequent disability were not designed to satisfactorily establish a temporal relationship.(11, 15) Our study, evaluating both men and women, showed a strong association between restricting back pain and subsequent disability in eADLs and iADLs. These results complement our previous work that showed a strong relationship between restricting back pain and mobility disability as well as our qualitative findings highlighting not only the physical, but also the psychological and social impacts of restricting back pain.(8, 18) We now have a more thorough understanding of the various ways restricting back pain impacts older adults, and therefore can attempt to target these areas of importance for older adults.
Our study has several strengths. PEP data include monthly assessments of restricting back pain and disability in both eADL and iADL with over 13+ years of follow-up. There was a very low rate of attrition for reasons other than death. In contrast to other observational studies that assessed exposure and outcome at limited/infrequent intervals, our study, with monthly assessments, increases the likelihood of a temporal relationship. To help show temporal precedence, during monthly interviews, restricting back pain was ascertained over the preceding month, whereas eADL and iADL disability were assessed “at the present time,” creating a time lag between exposure and outcomes. While monthly data are more granular than many observational studies, the data do not specify which days during the preceding month the restricting back pain resulted in eADL or iADL disability.
Our study also has several limitations. The severity, etiology, and the treatments used for restricting back pain were not evaluated. Self-reported restricted activities due to back pain may be secondary to other factors including a number of psycho-social factors, such as fear avoidance.(29) While the focus of the current study was on restricting back pain, participants could have provided reasons other than back pain for their restricted activity. (19) Although test-reliability was substantial for eADL, it was only moderate for iADL disability. Measurement error, however, should have reduced the associations between restricting back pain and these disability outcomes. The generalizability of our results may be limited because participants were members of a single health care plan in the greater New Haven region. The demographics of our cohort, however, mirror those of the US population except for race and ethnicity.(30) Lastly, this was an observational study and therefore the associations reported cannot be interpreted as causal.
Conclusion
In conclusion, restricting back pain is strongly associated with subsequent disability in both eADL and iADL. This study provides further evidence for the functional impact of restricting back pain. In the evaluation and treatment of back pain, the impact on function of these everyday activities should be strongly considered.
References
- 1.Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine. 2006;31(23):2724–7. doi: 10.1097/01.brs.0000244618.06877.cd. [DOI] [PubMed] [Google Scholar]
- 2.Makris UE, Fraenkel L, Han L, Leo-Summers L, Gill TM. Epidemiology of restricting back pain in community-living older persons. J Am Geriatr Soc. 2011;59(4):610–4. doi: 10.1111/j.1532-5415.2011.03329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thielke SM, Whitson H, Diehr P, O'Hare A, Kearney PM, Chaudhry SI, et al. Persistence and Remission of Musculoskeletal Pain in Community-Dwelling Older Adults: Results from the Cardiovascular Health Study. Journal of the American Geriatrics Society. 2012;60(8):1393–400. doi: 10.1111/j.1532-5415.2012.04082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88(Suppl 2):21–4. doi: 10.2106/JBJS.E.01273. [DOI] [PubMed] [Google Scholar]
- 5.Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169(3):251–8. doi: 10.1001/archinternmed.2008.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weiner DK. Introduction to Special Series: Deconstructing chronic low back pain in the older adult: shifting the paradigm from the spine to the person. Pain Med. 2015;16(5):881–5. doi: 10.1111/pme.12759. [DOI] [PubMed] [Google Scholar]
- 7.Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, et al. Expenditures and health status among adults with back and neck problems. JAMA. 2008;299(6):656–64. doi: 10.1001/jama.299.6.656. [DOI] [PubMed] [Google Scholar]
- 8.Makris UE, Higashi RT, Marks EG, Fraenkel L, Gill TM, Friedly JL, et al. Physical, Emotional, and Social Impacts of Restricting Back Pain in Older Adults: A Qualitative Study. Pain Med. 2016 doi: 10.1093/pm/pnw196. pii: pnw196. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deyo RA, Dworkin SF, Amtmann D, Andersson G, Borenstein D, Carragee E, et al. Report of the NIH Task Force on research standards for chronic low back pain. Pain Med. 2014;15(8):1249–67. doi: 10.1111/pme.12538. [DOI] [PubMed] [Google Scholar]
- 10.Cigolle CT, Langa KM, Kabeto MU, Tian Z, Blaum CS. Geriatric conditions and disability: the Health and Retirement Study. Ann Intern Med. 2007;147(3):156–64. doi: 10.7326/0003-4819-147-3-200708070-00004. [DOI] [PubMed] [Google Scholar]
- 11.Andrews JS, Cenzer IS, Yelin E, Covinsky KE. Pain as a risk factor for disability or death. J Am Geriatr Soc. 2013;61(4):583–9. doi: 10.1111/jgs.12172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fried LP, Guralnik JM. Disability in older adults: evidence regarding significance, etiology, and risk. J Am Geriatr Soc. 1997;45(1):92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- 13.Docking RE, Fleming J, Brayne C, Zhao J, Macfarlane GJ, Jones GT, et al. The relationship between back pain and mortality in older adults varies with disability and gender: results from the Cambridge City over-75s Cohort (CC75C) study. Eur J Pain. 2015;19(4):466–72. doi: 10.1002/ejp.568. [DOI] [PubMed] [Google Scholar]
- 14.Covinsky KE, Lindquist K, Dunlop DD, Yelin E. Pain, functional limitations, and aging. J Am Geriatr Soc. 2009;57(9):1556–61. doi: 10.1111/j.1532-5415.2009.02388.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leveille SG, Guralnik JM, Hochberg M, Hirsch R, Ferrucci L, Langlois J, et al. Low back pain and disability in older women: independent association with difficulty but not inability to perform daily activities. J Gerontol A Biol Sci Med Sci. 1999;54(10):487–93. doi: 10.1093/gerona/54.10.m487. [DOI] [PubMed] [Google Scholar]
- 16.Reid MC, Guo Z, Towle VR, Kerns RD, Concato J. Pain-related disability among older male veterans receiving primary care. J Gerontol A Biol Sci Med Sci. 2002;57(11):M727–32. doi: 10.1093/gerona/57.11.m727. [DOI] [PubMed] [Google Scholar]
- 17.Gill TM, Guo Z, Allore HG. Subtypes of disability in older persons over the course of nearly 8 years. J Am Geriatr Soc. 2008;56(3):436–43. doi: 10.1111/j.1532-5415.2007.01603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Makris UE, Fraenkel L, Han L, Leo-Summers L, Gill TM. Restricting back pain and subsequent mobility disability in community-living older persons. J Am Geriatr Soc. 2014;62(11):2142–7. doi: 10.1111/jgs.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001;135(5):313–21. doi: 10.7326/0003-4819-135-5-200109040-00007. [DOI] [PubMed] [Google Scholar]
- 20.Reid MC, Williams CS, Concato J, Tinetti ME, Gill TM. Depressive symptoms as a risk factor for disabling back pain in community-dwelling older persons. J Am Geriatr Soc. 2003;51(12):1710–7. doi: 10.1046/j.1532-5415.2003.51554.x. [DOI] [PubMed] [Google Scholar]
- 21.Kramer MS, Feinstein AR. Clinical biostatistics. LIV. The biostatistics of concordance. Clinical pharmacology and therapeutics. 1981;29(1):111–23. doi: 10.1038/clpt.1981.18. [DOI] [PubMed] [Google Scholar]
- 22.Gill TM, Murphy TE, Barry LC, Allore HG. Risk factors for disability subtypes in older persons. J Am Geriatr Soc. 2009;57(10):1850–5. doi: 10.1111/j.1532-5415.2009.02443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gill TM, Hardy SE, Williams CS. Underestimation of disability in community-living older persons. J Am Geriatr Soc. 2002;50(9):1492–7. doi: 10.1046/j.1532-5415.2002.50403.x. [DOI] [PubMed] [Google Scholar]
- 24.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 25.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5(2):179–93. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 26.Makris UE, Fraenkel L, Han L, Leo-Summers L, Gill T. Risk factors for restricting back pain in older persons. Journal of the American Medical Directors Association. 2014;15(1):62–7. doi: 10.1016/j.jamda.2013.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wei LJ, Lin DY, Weissfeld L. Regression analysis of multivariate incomplete failure time data by modeling marginal distributions. J Am Stat Soc. 1989;84:1065–73. [Google Scholar]
- 28.Therneau TMGP, editor. Modeling Survival Data: Extending the Cox Model. New York: Springer; 2000. [Google Scholar]
- 29.Camacho-Soto A, Sowa GA, Perera S, Weiner DK. Fear Avoidance Beliefs Predict Disability in Older Adults With Chronic Low Back Pain Pm&R. American Academy of Physical Medicine and Rehabilitation. 2012;4(7):493–7. doi: 10.1016/j.pmrj.2012.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. [Accessed January 22, 2013];American FactFinder: United States Census Bureau. 2013 Available from: http://factfinder2.census.gov.