Abstract
Background
Despite high abstinence rates, American Indians experience elevated rates of many alcohol and other drug problems. American Indians also predominantly reside in poor and rural areas, which may explain some observed health disparities. We investigated whether geographic areas including reservations or large American Indian populations exhibited greater incidence of alcohol- and drug-related hospitalizations.
Methods
We obtained inpatient hospitalization records for two Northern Plain states (Nebraska and South Dakota) for the years 2007 to 2012. We constructed zip-code counts for 10 categories of hospitalization with diagnoses or injury causation commonly associated with alcohol or drug use. We related these to community sociodemographic characteristics using Bayesian Poisson space-time regression models and examined associations with and without controls for whether each zip code was located within an American Indian reservation.
Results
Controlling for other demographic and economic characteristics, zip codes with greater percent of American Indians exhibited greater incidence for all 10 substance-abuse related health outcomes (9 of 10 well supported); zip code areas within American Indian reservations had greater incidence of self-inflicted injury and drug dependence and abuse, and reduced incidence of alcohol cirrhosis and prescription opioid poisoning. However, the analyses generally demonstrated no well-supported differences in incidence associated with local residence percentages of American Indian vs. African American.
Conclusions
In our analyses, ethnicity or heredity alone did not account for alcohol- and drug-related hospitalizations among Native populations. Aspects of social, economic, and political dimensions of Native lives must be considered in the etiology of alcohol- and drug-related problems for rural-dwelling indigenous peoples.
INTRODUCTION
As a group, American Indians who drink alcohol are often characterized as having greater risks for alcohol abuse, problems and alcohol use disorders (Grant et al., 2015; Landen, Roeber, Naimi, Nielsen, & Sewell, 2014). American Indian populations have also been linked to elevated rates of drug abuse, with the highest rates of cannabis use disorder (Hasin et al., 2016), prescription opioid overdose fatalities (Calcaterra, Glanz, & Binswanger, 2013), stimulant dependence (including methamphetamine) (Gilder, Gizer, Lau, & Ehlers, 2014) and cigarette smoking and related mortality (Mowery et al., 2015) among major U.S. population groups. Prior research suggests that higher levels of substance use are related to rates of other health problems such as mental illness (Caspi et al., 2005), suicide or self-inflicted injury (Wilcox, Conner, & Caine, 2004), assault (Hingson, Heeren, & Edwards, 2008; Parker & Auerhahn, 1998), motor-vehicle crashes (Hingson et al., 2008), or other accidental injuries (Hingson, Edwards, Heeren, & Rosenbloom, 2009). These statements about American Indian substance use address a very heterogeneous collection of many different tribal groups with divergent histories, cultural heritages, and contemporary living conditions, this characterization may or may not be accurate. Epidemiologic evidence in this regard is not entirely clear.
The current epidemiological literature may both over- and under-estimate risks related to alcohol and drugs use among American Indians: Over-estimates certainly appear quite frequently in the popular press, but may also arise from studies of small groups living in rural areas; these analyses may not adequately control for the health-reducing impacts of poverty (Cerda, Diez-Roux, Tchetgen, Gordon-Larsen, & Kiefe, 2010) and limited access to health care in rural areas. In such cases accurate statistical estimates of incidence and prevalence of substance abuse and associated health problems and disorders are difficult to obtain (largely due to small area effects; Riva, Gauvin, & Barnett, 2007). Underestimates may arise when large-scale surveys assume that all self-identifying American Indians are from one common racial, ethnic or cultural group, ignoring altogether cultural diversity and the diverse social contexts within which these people may live. It is not very surprising, therefore, when national survey studies using sampling techniques proportional to population size find that American Indian respondents differ little from other respondents in responses to questions on alcohol or drug use and related problems; these respondents are likely to be from urban areas of the US, unlikely to be Native people living on tribal lands, and likely to exhibit the same sampling biases as other American respondents (for example, there is a clear telephone landline bias in studies like Behavioral Risk Factor Surveillance System [BRFSS] that include American Indians, selecting for higher socioeconomic class; Cunningham, Solomon, & Muramoto, 2015). Thus, the critical questions are whether alcohol and drug use, abuse, problems, or disorders among members of any particular tribal group differ from problems experienced among other non-tribal members living in similar circumstances? The current study begins to address these questions by using a common source of hospitalization data to compare substance-related problem incidence across state areas that include large and small American Indian populations both on and off tribal lands. In these analyses, we use spatial analysis methods to address small area analysis biases that often arise in these population studies and to provide best cross-area estimates of incidence rates of alcohol and drug related problems.
As Borders and Booth (2007) note, controlling for personal demographics (e.g., sex and age), rural people are more likely to be abstainers (especially in the U.S. South), but also more likely to experience heavy drinking days as well as current alcohol use disorder. The current analyses employ a rich set of demographic and socioeconomic indicators to help determine whether high reported rates of alcohol problems among rural Native people are actually due to cultural dimensions of American Indian “ethnicity” as opposed to other correlated characteristics such as poverty rate or location within a rural area (i.e., with low population density). Analyses are performed both with and without indicators of tribal land to investigate whether populations living in reservation areas have greater or lesser risk than would be predicted based on economic and demographic characteristics alone.
METHODS
Data sources and variables
We collected annual data, including inpatient hospital discharges as well as demographic and economic characteristics across zip codes within two Northern Plains states (Nebraska and South Dakota) over the years 2007 through 2012 (ESRI, 2012). Zip codes are periodically redefined for postal administrative purposes, with annual counts ranging from 917 to 920 during these years, producing a sample of 5,513 space-time units. Zip code populations varied between 0 and 45,665 persons (mean = 2,845.1, median = 768.3), with land area ranging from 0.02 to 2,358 square miles (mean = 167.9, median = 105.2). We used this data set to conduct population-level Bayesian space-time analysis of associations between substance-related hospitalizations and various local characteristics. The research was approved by the Institutional Review Board of Pacific Institute for Research and Evaluation. The research protocols and the submitted versions of this manuscript have been reviewed and acknowledged by the research ethics review board maintained by the Tribal nation primarily served by the Indian Health Service Unit whose data are included in this study (Tribal identity is protected per agreement with this review board).
Substance-related hospitalizations
We obtained inpatient hospital discharge data from the annual State Inpatient Databases of the Agency for Healthcare Research and Quality, Health Care Utilization Project (HCUP) (2007–2012). These databases encompass 97% of all U.S. community hospital discharges, but exclude Federal institutions such as those operated by the Indian Health Service (Skinner, Coffey, Jones, Heslin, & Moy, 2016). Each discharge record included up to 55 ICD-9 diagnosis codes and 6 external cause-of-injury codes. We should note that the HCUP Central Distributor only offers inpatient datasets for South Dakota, so we could not include emergency room data in these analyses. Across the two states, 99.7% of discharge records include a valid 5-digit zip code of patient residence, with 99.1% of in-state records matching to a valid zip code. We computed annual counts of discharges for each zip code within ten problem categories. Four of these are substance-related by definition: alcohol abuse and dependence, drug dependence and abuse, alcoholic cirrhosis, and prescription opioid poisoning. The remaining six categories that have previously been shown to be highly related to substance use: mental health problems, suicide and self-inflicted injury, assault, motor vehicle accidents, and total accidents both in the overall population and among those under age 18. We disregarded the precedence of diagnostic codes (primary, secondary, tertiary, etc.) and counted cases within a category if they included any of the associated codes. Table 1 lists the ICD-9 diagnostic and external cause codes used to identify each alcohol-related health category. The overall hospitalization rate, calculated as the total number of discharges per capita, was included as a covariate to control for differences in access to inpatient care. We have abided by all Health Care Utilization Project (HCUP) requirements for protecting confidentiality of these archival hospitalization-level records.
Table 1.
ICD-9 Diagnostic or External-Cause-of-Injury Codes for each Outcome Measure
| Outcome Measure | ICD-9 Diagnostic Codes or E-Codes |
|---|---|
| Alcohol Dependence & Abuse | 303.0, 305.0 |
| Drug Dependence or Abuse | 304, 305.2–305.9 |
| Alcohol Cirrhosis | 571.1–571.3 |
| Prescription Opioid Poisoning | E850.1, E850.2, E935.1, E935.2 |
| Mental Health Problems | 300.0, 300.3, 300.4, 306, 308, 309, 311 |
| Assault | E960–E969 |
| Suicide / Self-Inflicted Injury | E950–E959 |
| Motor Vehicle Accidents | E810–E819 |
| Accidents (Total, or Ages 0–17) | E800–E807, E850–E858, E860–E869, E880–E888, E890-E899, E900–E909, E910–E915, E916–E928, E929, E980–E989 |
Indian Health Service data
In addition to hospitalizations, tribal members may also receive ambulatory care from the Indian Health Service (IHS). The IHS provided de-identified data on selected ambulatory encounters from a single service unit located within a large reservation over the years 2007 to 2012. Comparable IHS data were not available across all service units in the region. We obtained data for patients with specified ICD-9 diagnostic or external-cause-of-injury codes commonly associated with alcohol abuse, including alcohol dependence or abuse, alcohol cirrhosis, assault, suicide or self-inflicted injury, single vehicle crashes, child abuse or domestic violence, excessive cold, and partner violence. These were aggregated to annual counts per patient residential zip code. We used these data to obtain a descriptive comparison of differences in incidence rates between IHS outpatient visits and HCUP hospital admission data. We expected there to be some differences between these sources as they represent cases with very different degrees of severity (see below) and reflect either chronic or acute conditions. For example, chronic issues such as mental health might be seen more at IHS clinics, as demonstrated by the high numbers of repeat visits within a year seen in our IHS dataset overall (unique patients seen within a year were provided only in total, not by zip code).
Demographic and economic covariates
Estimated annual zip code-level economic and demographic data included median real household income ($10,000s of 2012 dollars), percentage of families in poverty, racial/ethnic distribution (percentages Hispanic, Black, and American Indian or Alaska Native, as defined by Census racial / ethnic categories); age distribution (percentages aged 0–19, 20–24, 25–44, and 45–64, with percentage aged 65 and above excluded as the reference category); population density (100s per square mile); and percentage male. We calculated these zip code covariates using between-census projections at the census block group level (Geolytics, 2013). Because Census block groups are not cleanly nested within zip codes, we reallocated annual block group estimates to overlapping zip code areas weighted by populations or households within shared 2010 Census blocks. Proportional demographic indicators were undefined in 0.2% of zip codes reporting zero population; these were replaced with average values.
Reservation status
Some models also included an indicator for whether each zip code’s centroid was located within the borders of any of the 13 American Indian reservations which co-occur with the states of South Dakota and Nebraskai. These “reservation” zip codes provided a good spatial match to the boundariesii of 10 larger reservations which co-occur with these states. Judging by captured Census blocks, 95.2% of these reservations’ total population was located within the zip codes used to approximate reservations, and 97.9% of the population in these zip codes was located within the reservations. Three smaller reservations did not contain any zip codes’ centroids, and therefore their three encompassing zip codes were not identified as “reservation.” This exclusion appears justified as the three reservations’ populations represented very small proportions (between 1.9% and 11.7%) of the populations of their respective zip codes.
Statistical approach
We used a hierarchical Bayesian Poisson space-time misalignment model to perform analyses at the zip code level over a period of 7 years. This class of Bayesian spatial models uses Conditional Autoregressive (CAR) random effects to control for spatial autocorrelation of residuals (Bernardinelli et al., 1995; Besag, York, & Mollié, 1991; Carlin & Louis, 2000). The approach reduces the influence of outliers by allowing each spatial area to “borrow strength” from its neighbors (Waller & Gotway, 2004). This advantage is especially important when analyzing incidence data from low-population zip codes where a single hospitalization can result in a very high incidence rate per resident. The CAR spatial random effects are assumed to be mean zero with a common standard deviation across years, and the model incorporates a non-spatial random effect which effectively controls for over-dispersion (Lord, Washington, & Ivan, 2005). Because zip code boundaries are occasionally redefined for postal service administrative purposes, potential bias related to area misalignment is controlled by identifying the sizes of populations shifting from one unit to another over time and by introducing year-specific CAR random effects in accordance with each year’s zip-code adjacency map (Zhu, Waller, & Ma, 2013).
Since the outcome measures were counts of hospital discharges in a given zip code in each year, we used a Poisson regression model:
where Yi,t represents the count of some class of hospitalizations in zip code i during year t, while Ei,t denotes the expected number of discharges under the assumption that study-wide cases are distributed among zip codes in direct proportion to population. Therefore, exp(μi,t) is interpreted as the relative rate of residing in spatial unit i at time t. Regions with exp(μi,t) > 1 will have greater counts than expected, and regions with exp(μi,t) < 1 will have fewer than expected. Following standard generalized linear models, the log relative rate, μi,t, is modeled linearly as:
This is a linear combination of fixed covariate effects and random effects designed to account for spatial autocorrelation. X′i,t is a matrix containing space-and time-varying covariates and β is a vector of fixed-effects estimates of the association of those covariates with the rate of hospital discharges. θi,t and φi,t denote the pair of random effects capturing spatially unstructured heterogeneity and CAR spatial dependence, respectively.
We estimated models using WinBUGS 1.4.3 software (Lunn, Thomas, Best, & Spiegelhalter, 2000). Non-informative priors were specified for all fixed and random effects. Models were allowed to burn-in for at least 100,000 Markov Chain Monte Carlo (MCMC) iterations, a sufficient number of iterations for all parameter estimates to stabilize and converge between two chains with different initial values. Posterior estimates were sampled for an additional 50,000 MCMC iterations to provide model results.
RESULTS
Table 2 compares the incidence of eight health conditions observed in the IHS and HCUP data obtained for this project. Because the IHS data were all from a service unit located within a specific reservation, we compared incidence counts only among those patients whose residential zip codes had centroids within that reservation (summed over the years 2007 to 2012). The incidence counts were uniformly higher for IHS visits than for HCUP inpatient admissions. The table also presents the percentage of each system’s total incidence within each problem category. IHS and HCUP have similar shares for alcohol dependence or abuse (roughly 45%) and self-inflicted injuries (7%), but differing shares with respect to acute incidents like injuries related to assaults (10.3% in HCUP vs. 33.1% in IHS) and severe chronic conditions like alcoholic cirrhosis (32.2% in HCUP vs. 8.0% in IHS). Many assault injuries will not result in an overnight hospital stay, while alcoholic cirrhosis often requires continued contact with hospital facilities to manage this condition (Greenfeld & Smith, 1999; Harrison, 2015).
Table 2.
Comparing incidence of selected health problems between HCUP inpatient stays and IHS outpatient visits 2007–2012 visits from 11 residential zip codes centered within the reservation containing the sampled IHS service unit
| Inpatient Hospitalizations (HCUP) |
Outpatient Visits (IHS) | |||
|---|---|---|---|---|
| Outcome (ICD-9 codes) | 6-year incidence (# of visits) |
Percent of total | 6-year incidence (# of visits) |
Percent of total |
| Alcohol Dependence or Abuse (303.0, 305.0) | 849 | 44.9% | 7,265 | 46.5% |
| Alcohol Cirrhosis (571.1–571.3) | 608 | 32.2% | 1,254 | 8.0% |
| Assault (E960–E969) | 194 | 10.3% | 5,179 | 33.1% |
| Suicide or self-inflicted injury (E950–E959) | 133 | 7.0% | 1,139 | 7.3% |
| Single Vehicle Crash (E815, E816) | 92 | 4.9% | 221 | 1.4% |
| Child Abuse and Domestic Violence (V61.21, 995.5, E967) | 8 | 0.4% | 353 | 2.3% |
| Excess Cold (E901.0, E901.9) | 5 | 0.3% | 89 | 0.6% |
| Partner Violence (E967.3) | 0 | 0.0% | 130 | 0.8% |
| Total of listed categories | 1,889 | 100% | 15,630 | 100% |
Table 3 presents descriptive statistics for the HCUP inpatient data as well as demographic covariates. These are provided for the sampled states as a whole, and then separately for the zip codes whose centroids were and were not part of an Indian reservation. Hospitalization rates per 1000 residents ranged from 0.2 for prescription opioid poisoning to 13.2 for mental health diagnoses. Per capita hospitalization rates in reservation zip codes were higher than in non-reservation areas for 8 of 10 categories, with the exceptions being prescription opioid poisoning and all-age injuries due to accidents. Hospitalization rates among individuals living in reservation zip code areas were more than double those in other areas for alcoholic cirrhosis, assault injuries, alcohol abuse and dependence, and drug abuse and dependence.
Table 3.
Weighted descriptive statistics, overall and by whether a zip code is located within a recognized American Indian reservation
| Total Sample (N = 5,513) | Zip centroid is within a Reservation (N = 308) | Zip centroid is not in a Reservation (N = 5,205) | |||||||||||||
| HCUP hospitalization rates relative to zip code population: | Mean | SD | Min | Median | Max | Mean | SD | Min | Median | Max | Mean | SD | Min | Median | Max |
| Alcohol Abuse & Dependence Discharges per 1000 people | 2.03 | 1.87 | 0.00 | 0.79 | 74.54 | 5.95 | 4.74 | 0.00 | 2.11 | 74.54 | 1.92 | 1.59 | 0.00 | 0.76 | 51.42 |
| Drug Dependence & Abuse Discharges per 1000 people | 2.52 | 2.59 | 0.00 | 0.23 | 141.63 | 5.03 | 4.68 | 0.00 | 2.33 | 141.63 | 2.45 | 2.47 | 0.00 | 0.00 | 29.07 |
| Alcohol Cirrhosis Discharges per 1000 people | 0.65 | 1.03 | 0.00 | 0.00 | 176.31 | 3.07 | 3.25 | 0.00 | 0.00 | 67.09 | 0.58 | 0.79 | 0.00 | 0.00 | 176.31 |
| Prescription Opioid Discharges per 1000 people | 0.33 | 0.36 | 0.00 | 0.00 | 32.15 | 0.21 | 0.47 | 0.00 | 0.00 | 12.14 | 0.33 | 0.35 | 0.00 | 0.00 | 32.15 |
| Mental Health Discharges per 1000 people | 13.20 | 7.43 | 0.00 | 9.69 | 141.00 | 14.13 | 8.92 | 0.00 | 8.72 | 134.17 | 13.18 | 7.38 | 0.00 | 9.72 | 141.00 |
| Assault Discharges per 1000 people | 0.21 | 0.42 | 0.00 | 0.00 | 14.67 | 0.93 | 1.18 | 0.00 | 0.00 | 14.67 | 0.19 | 0.36 | 0.00 | 0.00 | 7.13 |
| Suicide & Self-Inflicted Injury Discharges per 1000 people | 0.73 | 0.64 | 0.00 | 0.00 | 14.61 | 1.09 | 0.98 | 0.00 | 0.00 | 6.72 | 0.72 | 0.63 | 0.00 | 0.00 | 14.61 |
| Motor Vehicle Accident Discharges per 1000 people | 0.59 | 0.61 | 0.00 | 0.00 | 24.57 | 1.11 | 1.27 | 0.00 | 0.00 | 15.29 | 0.58 | 0.57 | 0.00 | 0.00 | 24.57 |
| All Accident Discharges per 1000 people | 5.68 | 2.89 | 0.00 | 4.76 | 119.26 | 4.29 | 3.58 | 0.00 | 2.73 | 119.26 | 5.72 | 2.86 | 0.00 | 4.86 | 80.28 |
| Accident Under Age 18 Discharges per 1000 Under 18 | 1.26 | 1.66 | 0.00 | 0.00 | 132.86 | 1.39 | 2.17 | 0.00 | 0.00 | 40.29 | 1.25 | 1.63 | 0.00 | 0.00 | 132.86 |
| Zip Code Characteristics (Estimates from GeoLytics) | Mean | SD | Min | Median | Max | Mean | SD | Min | Median | Max | Mean | SD | Min | Median | Max |
| Population | 2,845.1 | 6,080.5 | 3.0 | 768.3 | 45,665 | 1,373.6 | 1,548.8 | 38.2 | 906.5 | 8,520.7 | 2,932.2 | 6,235.7 | 3.0 | 759.9 | 45,665 |
| Households | 1,111.6 | 2,422.5 | 0.00 | 300.26 | 18,837 | 415.2 | 440.8 | 17.2 | 283.1 | 2,114 | 1,152.8 | 2,484.8 | 0.0 | 301.0 | 18,837 |
| Population Under 18 | 660.04 | 1,468.0 | 3.00 | 167.0 | 11,699 | 455.1 | 560.3 | 10.3 | 281.2 | 3,298 | 672.1 | 1,503.8 | 3.0 | 162.7 | 11,699 |
| Square Miles | 167.9 | 215.9 | 0.02 | 105.2 | 2,357.9 | 301.2 | 350.2 | 23.4 | 171.1 | 1,599.7 | 160.0 | 202.5 | 0.02 | 101.9 | 2,357.9 |
| Hospital Discharges Per Capita | 0.11 | 0.03 | 0.00 | 0.10 | 1.00 | 0.11 | 0.06 | 0.00 | 0.08 | 1.00 | 0.11 | 0.03 | 0.00 | 0.10 | 0.66 |
| Real Median HH Income ($10,000s of 2012 dollars) | 4.70 | 1.45 | 0.26 | 3.86 | 12.78 | 2.91 | 0.77 | 0.92 | 2.96 | 7.73 | 4.74 | 1.44 | 0.26 | 3.90 | 12.78 |
| % Families in Poverty | 8.70 | 7.05 | 0.00 | 9.30 | 100.00 | 31.99 | 14.82 | 3.16 | 24.02 | 72.64 | 8.14 | 5.67 | 0.00 | 9.00 | 100.00 |
| Population Density (100s of people per square mile) | 0.17 | 1.46 | 0.00 | 0.08 | 169.77 | 0.05 | 0.04 | 0.00 | 0.04 | 0.44 | 0.18 | 1.54 | 0.00 | 0.08 | 169.77 |
| % Age 0–19 | 27.59 | 4.53 | 3.43 | 25.54 | 70.05 | 39.12 | 6.48 | 23.22 | 36.23 | 50.90 | 27.27 | 4.02 | 3.43 | 25.36 | 70.05 |
| % Age 20–24 | 7.37 | 1.05 | 3.61 | 7.40 | 25.07 | 8.54 | 0.91 | 5.48 | 8.35 | 10.97 | 7.34 | 1.04 | 3.61 | 7.37 | 25.07 |
| % Age 25–44 | 25.55 | 4.85 | 8.43 | 21.57 | 75.05 | 23.41 | 2.06 | 14.86 | 22.70 | 28.84 | 25.61 | 4.89 | 8.43 | 21.53 | 75.05 |
| % Age 45–64 | 24.70 | 3.33 | 2.08 | 26.19 | 35.57 | 18.40 | 3.50 | 10.36 | 20.25 | 30.90 | 24.87 | 3.15 | 2.08 | 26.35 | 35.57 |
| % Male | 49.65 | 1.85 | 38.60 | 50.25 | 83.99 | 49.97 | 1.33 | 43.70 | 50.39 | 57.04 | 49.64 | 1.86 | 38.60 | 50.25 | 83.99 |
| % Black | 3.39 | 8.84 | 0.00 | 0.03 | 70.65 | 0.34 | 0.56 | 0.00 | 0.07 | 7.42 | 3.47 | 8.95 | 0.00 | 0.03 | 70.65 |
| % Hispanic | 6.34 | 9.48 | 0.00 | 1.29 | 59.83 | 2.58 | 2.16 | 0.00 | 1.45 | 21.90 | 6.44 | 9.58 | 0.00 | 1.28 | 59.83 |
| % American Indian | 3.26 | 12.06 | 0.00 | 0.31 | 99.35 | 67.74 | 26.78 | 0.52 | 49.38 | 99.35 | 1.47 | 3.35 | 0.00 | 0.26 | 89.69 |
| South Dakota Zip Code Indicator | 0.31 | 0.46 | 0.00 | 0.00 | 1.00 | 0.90 | 0.30 | 0.00 | 1.00 | 1.00 | 0.29 | 0.46 | 0.00 | 0.00 | 1.00 |
| % Zip Code Population Instability from Boundary Changes | 0.16 | 1.30 | 0.00 | 0.00 | 47.64 | 0.55 | 3.47 | 0.00 | 0.00 | 44.25 | 0.15 | 1.19 | 0.00 | 0.00 | 47.64 |
The lower panel of Table 3 indicates that residents in reservation zip codes tended to be younger, lower-income, more likely to live in poverty, and from less-densely populated areas than those in other zip codes. American Indians represented 67.7% of population in the reservation zip codes, but only 1.5% of residents in other zip codes within these states. South Dakota contained 90% of residents of the two state’s reservation zip codes versus 29% for non-reservation zip codes. The overall rates of hospitalization per capita were virtually identical between these two types of communities.
Table 4 presents the results of two different Bayesian analyses of the 10 health outcomes in the study: (A) core analyses without a covariate for reservations status, with full covariate effects reported, and (B) selected results from a specification test adding an indicator for “reservation status,” i.e., whether each zip code appeared within a reservation boundary. (Covariate effects in the second analysis were virtually identical to those in the first and are not reported.) Results of the core analyses display all the technical information necessary for interpretation of the demographic associations in the study: (1) The first block of the table shows that the control for overall hospital discharges was essential; greater numbers of discharges were related to greater numbers of each observed outcome (independent of population size, the expectation for the Poisson model). (2) The second block shows that there were substantive differences in discharge rates between South Dakota and Nebraska (greater in SD with the exception of accidents among persons under age 18). (3) Following reports of coefficients related to demographic relationships, the fourth block of the table shows that the CAR spatial random effect accounted for over half of unexplained zip code variance in 9 of the 10 analyses, but the covariate for direct effects of zip code misalignment was never well supported. The counts of all outcomes were over-dispersed and substantively spatial autocorrelated, lacking statistical independence. The extent of spatial autocorrelation was further characterized using Moran’s I coefficient, a measure approximately bounded [−1.0, 1.0] and in all cases exceeding a value of 0.75. Thus, absent of these corrections, statistical tests of effects would exhibit very high Type I error rates and posteriors calculated from the statistical model would exhibit strong small area effects.
Table 4.
Association of community characteristics with zip code rates of substance-related hospitalization (expressed as relative rates)
| Variable: | Alcohol Dependence & Abuse: |
Drug Dependence and Abuse: |
Alcohol Cirrhosis: |
Prescription Opioid Poisoning: |
Mental Health Problems: |
Assault: | Suicide & Self- Inflicted Injury: |
Motor Vehicle Accidents: |
All Accidents: | Accidents Under Age 18: |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| (A) Core analyses without reservation status: | ||||||||||
|
| ||||||||||
| Hospital Discharges per Capita | 4.015* | 4.251* | 4.374* | 3.333* | 6.598* | 3.487* | 3.518* | 3.319* | 4.959* | 2.774* |
| (3.367, 4.768) | (3.422, 5.211) | (3.303, 5.612) | (2.701, 3.973) | (5.717, 7.582) | (2.390, 4.598) | (2.834, 4.306) | (2.692, 4.031) | (4.305, 5.724) | (2.212, 3.372) | |
|
| ||||||||||
| Zip Code within South Dakota | 1.516* | 1.492* | 2.146* | 1.140 | 2.652* | 1.013 | 1.219 | 1.155 | 0.940 | 0.758* |
| (1.285, 1.770) | (1.179, 1.858) | (1.633, 2.684) | (0.981, 1.345) | (2.369, 3.000) | (0.787, 1.268) | (0.993, 1.487) | (0.954, 1.398) | (0.825, 1.073) | (0.647, 0.913) | |
|
| ||||||||||
| Real Median HH Income ($10,000s of 2012 dollars) | 0.897* | 0.901* | 0.863* | 0.975 | 0.944* | 0.825* | 0.983 | 0.859* | 0.941* | 1.014 |
| (0.867, 0.928) | (0.868, 0.935) | (0.817, 0.919) | (0.937, 1.017) | (0.923, 0.972) | (0.764, 0.888) | (0.938, 1.029) | (0.824, 0.901) | (0.917, 0.962) | (0.965, 1.065) | |
| % of Families in Poverty | 0.994* | 0.993* | 0.996 | 0.993 | 0.987* | 0.993 | 0.995 | 1.003 | 0.991* | 1.006 |
| (0.989, 0.999) | (0.987, 0.999) | (0.986, 1.003) | (0.983, 1.001) | (0.983, 0.990) | (0.983, 1.001) | (0.988, 1.002) | (0.997, 1.009) | (0.987, 0.995) | (0.997, 1.014) | |
| Population Density (100s of people per square mile) | 1.002 | 1.002 | 1.007* | 1.001 | 0.996* | 1.007* | 1.001 | 0.998 | 0.997* | 0.996* |
| (0.999, 1.005) | (0.998, 1.006) | (1.001, 1.012) | (0.998, 1.004) | (0.994, 0.999) | (1.002, 1.012) | (0.998, 1.005) | (0.994, 1.001) | (0.995, 1.000) | (0.992, 0.999) | |
| % Age 0-19 | 1.008 | 1.021* | 1.020* | 0.979* | 0.985* | 1.032* | 1.020* | 1.031* | 0.971* | 0.975* |
| (0.997, 1.016) | (1.012, 1.032) | (1.003, 1.040) | (0.966, 0.991) | (0.980, 0.991) | (1.014, 1.053) | (1.006, 1.032) | (1.017, 1.045) | (0.965, 0.977) | (0.962, 0.991) | |
| % Age 20_24 | 0.892* | 0.859* | 0.855* | 0.899* | 0.929* | 0.786* | 0.866* | 0.986 | 0.924* | 0.919* |
| (0.862, 0.926) | (0.828, 0.902) | (0.806, 0.911) | (0.855, 0.942) | (0.913, 0.953) | (0.722, 0.841) | (0.828, 0.900) | (0.951, 1.024) | (0.904, 0.945) | (0.882, 0.961) | |
| % Age 25_44 | 1.030* | 1.050* | 1.027* | 0.993 | 0.996 | 1.060* | 1.058* | 0.988* | 0.975* | 0.998 |
| (1.021, 1.036) | (1.040, 1.059) | (1.014, 1.043) | (0.981, 1.004) | (0.992, 1.001) | (1.046, 1.084) | (1.046, 1.069) | (0.978, 0.998) | (0.972, 0.981) | (0.987, 1.011) | |
| % Age 45_64 | 1.028* | 1.031* | 1.051* | 1.003 | 0.977* | 1.052* | 1.026* | 1.044* | 0.973* | 1.000 |
| (1.013, 1.039) | (1.015, 1.043) | (1.034, 1.068) | (0.986, 1.021) | (0.970, 0.988) | (1.023, 1.100) | (1.004, 1.048) | (1.027, 1.061) | (0.966, 0.980) | (0.981, 1.018) | |
| % Male | 0.974* | 0.967* | 0.968* | 0.967* | 0.968* | 0.998 | 0.968* | 1.010 | 0.976* | 1.033* |
| (0.960, 0.982) | (0.957, 0.976) | (0.945, 0.982) | (0.950, 0.981) | (0.964, 0.971) | (0.968, 1.019) | (0.946, 0.980) | (0.990, 1.025) | (0.968, 0.982) | (1.018, 1.056) | |
| % Black | 1.016* | 1.026* | 1.019* | 1.008* | 1.012* | 1.042* | 1.016* | 1.000 | 1.005* | 1.012* |
| (1.010, 1.022) | (1.019, 1.034) | (1.009, 1.028) | (1.002, 1.015) | (1.007, 1.016) | (1.033, 1.050) | (1.010, 1.023) | (0.995, 1.006) | (1.001, 1.010) | (1.005, 1.018) | |
| % Hispanic | 1.006* | 1.006* | 1.009* | 1.000 | 1.003* | 1.018* | 1.002 | 0.994* | 1.001 | 1.001 |
| (1.001, 1.010) | (1.002, 1.011) | (1.001, 1.016) | (0.995, 1.005) | (1.001, 1.006) | (1.011, 1.026) | (0.997, 1.007) | (0.990, 0.999) | (0.998, 1.004) | (0.995, 1.006) | |
| % American Indian | 1.022* | 1.022* | 1.025* | 1.005* | 1.007* | 1.036* | 1.014* | 1.005* | 1.009* | 1.009* |
| (1.020, 1.026) | (1.018, 1.026) | (1.02, 1.030) | (1.000, 1.011) | (1.005, 1.009) | (1.029, 1.043) | (1.011, 1.019) | (1.001, 1.009) | (1.006, 1.011) | (1.004, 1.014) | |
|
| ||||||||||
| Zip Code Misalignment (%) | 1.000 | 0.988 | 0.991 | 1.004 | 0.999 | 1.010 | 0.992 | 1.002 | 0.994 | 0.972 |
| (0.988, 1.011) | (0.974, 1.002) | (0.971, 1.010) | (0.979, 1.026) | (0.992, 1.005) | (0.985, 1.032) | (0.971, 1.010) | (0.984, 1.018) | (0.986, 1.003) | (0.940, 1.000) | |
| SD of CAR spatial random effect | 0.488 | 0.661 | 0.519 | 0.308 | 0.565 | 0.562 | 0.469 | 0.588 | 0.594 | 0.419 |
| (0.442, 0.531) | (0.603, 0.726) | (0.410, 0.628) | (0.261, 0.374) | (0.536, 0.598) | (0.462, 0.632) | (0.399, 0.546) | (0.520, 0.651) | (0.558, 0.635) | (0.342, 0.495) | |
| SD of noise random effects | 0.286 | 0.304 | 0.680 | 0.159 | 0.103 | 0.271 | 0.310 | 0.050 | 0.051 | 0.197 |
| (0.236, 0.335) | (0.244, 0.357) | (0.587, 0.760) | (0.074, 0.248) | (0.068, 0.151) | (0.123, 0.366) | (0.237, 0.362) | (0.024, 0.127) | (0.025, 0.107) | (0.057, 0.301) | |
| Proportion of residual error variance that is spatial | 0.744 | 0.826 | 0.367 | 0.793 | 0.968 | 0.810 | 0.696 | 0.993 | 0.993 | 0.810 |
| (0.647, 0.828) | (0.752, 0.891) | (0.237, 0.522) | (0.557, 0.957) | (0.929, 0.986) | (0.664, 0.956) | (0.571, 0.832) | (0.962, 0.998) | (0.967, 0.998) | (0.601, 0.987) | |
| Spatial Autocorrelation | 0.857 | 0.849 | 0.909 | 0.951 | 0.750 | 0.939 | 0.912 | 0.933 | 0.844 | 0.910 |
|
| ||||||||||
| (B) Selected results from a specification test adding reservation status: | ||||||||||
|
| ||||||||||
| % American Indian | 1.023* | 1.017* | 1.033* | 1.015* | 1.008* | 1.041* | 1.010* | 1.006* | 1.008* | 1.005 |
| (1.019, 1.027) | (1.012, 1.022) | (1.026, 1.040) | (1.008, 1.023) | (1.005, 1.011) | (1.033, 1.049) | (1.004, 1.016) | (1.001, 1.011) | (1.005, 1.011) | (0.998, 1.012) | |
| Zip Code within an American Indian Reservation | 0.956 | 1.603* | 0.541* | 0.473* | 0.915 | 0.692 | 1.436* | 0.950 | 1.036 | 1.397 |
| (0.772, 1.179) | (1.224, 2.046) | (0.377, 0.781) | (0.294, 0.753) | (0.796, 1.042) | (0.420, 1.147) | (1.038, 2.008) | (0.690, 1.314) | (0.880, 1.221) | (0.927, 2.077) | |
Coefficients are expressed as relative rates, with 95% credible interval in parentheses.
Well-supported finding (95% credible interval excludes 1.000).
With these technical controls in place, best estimates of demographic effects are presented in the third block of Table 4. Greater median household income was generally related to lower hospital admissions, with well-supported effects for alcohol and drug dependence and abuse, alcohol cirrhosis, assault injuries, mental health problems, motor vehicle crashes and all accidents. Greater percentages of families in poverty were related to lower rates of alcohol and drug dependence and abuse, mental health problems and all accidents. Greater population density was related to greater assault injuries, fewer mental health problems, greater hospital discharges related to alcoholic cirrhosis, and fewer accidents including those specifically among persons under age 18. Areas with greater proportion of population aged 20 to 24 tended to have lower rates of hospitalization across all categories, while zip codes with higher proportions aged 25 to 64 were associated with elevated rates of assault, self-inflicted injury, cirrhosis, and abuse and dependence related to alcohol or drugs. Areas with high proportions of males had lower hospitalization rates in most categories, but had higher risks for accidents under age 18. Hospitalization risks tended to be elevated in zip codes with high proportions of Black residents, while percent Hispanic was positively related to rates of five problem outcomes but negatively related to motor vehicle injury risks. Controlling for other covariates, zip codes with greater percentages of American Indian residents presented elevated risks for all ten types of alcohol-related hospitalizations (compared to the excluded race/ethnic category, which is primarily White). These effects are often large: a 1 percentage point increase in the American Indian population share is associated with a 3.6% higher risk of assault, 2.5% more cirrhosis discharges, 2.2% more alcohol abuse and dependence, 2.2% more drug abuse and dependence, and 1.4% higher risk of suicide or self-inflicted injury.
Model posterior estimates were analyzed to test whether percent American Indian had a larger direct relationship with problem risks than did the percentages of Black or Hispanic residents. These results suggest no well-supported difference in effects between percent American Indian and percent Black in eight of the ten problem outcomes, with the exceptions being that percent American Indian had a 0.6% larger positive association with alcohol abuse and dependence (calculated as the difference between the 1.022 American Indian relative rate in Table 4 and the 1.016 relative rate for percent Black) and percent Black had a 0.4% greater positive association with mental health problems (the rounded difference between the 1.012 relative rates for percent Black minus the 1.007 relative rate for percent American Indian). Conversely, the percentage American Indian had a larger positive association with nine of ten problem outcomes than did percentage Hispanic, with only prescription opioid poisoning not having a well-supported difference in effects.
Section B of Table 4 summarizes key results from a supplementary set of analyses that introduced an indicator variable for whether each zip code had its centroid within one of the 13 recognized reservations within these states. The results for all covariates other than percent American Indian were nearly identical to those shown in Section A. The associations of hospitalization risk with the percentage American Indian remained strongly positive when reservation status was controlled, being statistically well-supported in nine of the 10 analyses (all except accidents among those under age 18). However, predicted hospitalization risks related to whether a zip code was centered within the boundaries of a reservation varied dramatically from one outcome to another, with substantial effects related to self-inflicted injury (44% greater incidence), drug dependence and abuse (60% greater incidence), alcohol cirrhosis (46% less incidence) and prescription opioid poisoning (53% less incidence).
The relative predictive power of percentage American Indian and reservation status is demonstrated in Figures 1 and 2. Each figure shows model-predicted incidence rate ratios between a hypothetical “reservation” and “non-reservation” zip code. In Figure 1, the two hypothetical zip codes are assumed to have study-wide average values for all independent variables except for percentage American Indian, comparing predicted hospitalization risks between having the mean reservation share (67.7% American Indian) versus the average non-reservation share (1.5%). The hypothetical reservation community has far higher risks (incidence rate ratios above one) for all health outcomes, and the credible intervals exclude 1.0 in all analyses except accidents among those under age 18. Figure 2 isolates only the effect of the reservation-zip-code identifier while holding all other covariates at sample means, and these incidence rate ratios are evenly distributed above and below 1.0, suggesting that reservations status does not consistently predict higher or lower risks of the health problems studied.
Figure 1.
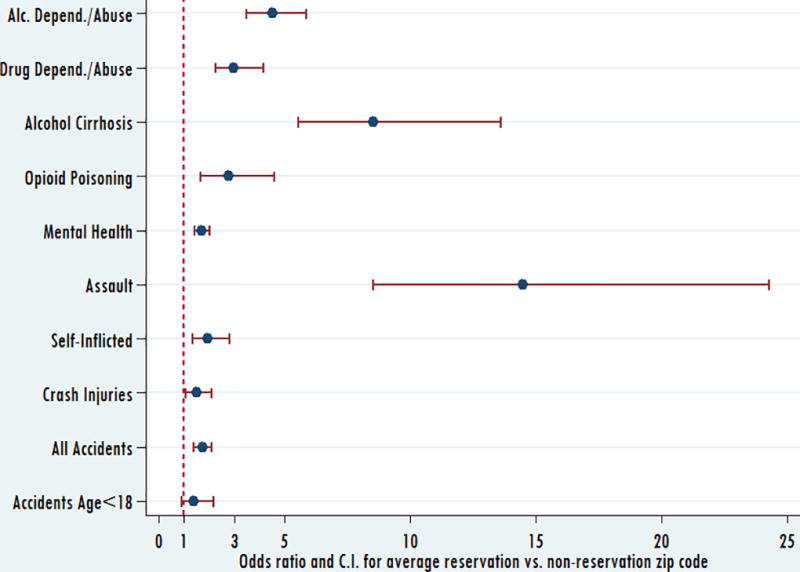
Odds ratios comparing estimated hospitalization risks associated with a zip code having the average American Indian concentration among reservation zip codes (67.7%) versus the average concentration among non-reservation zip codes (1.5%). These calculations assume that all other zip-code characteristics are at study means.
Figure 2.
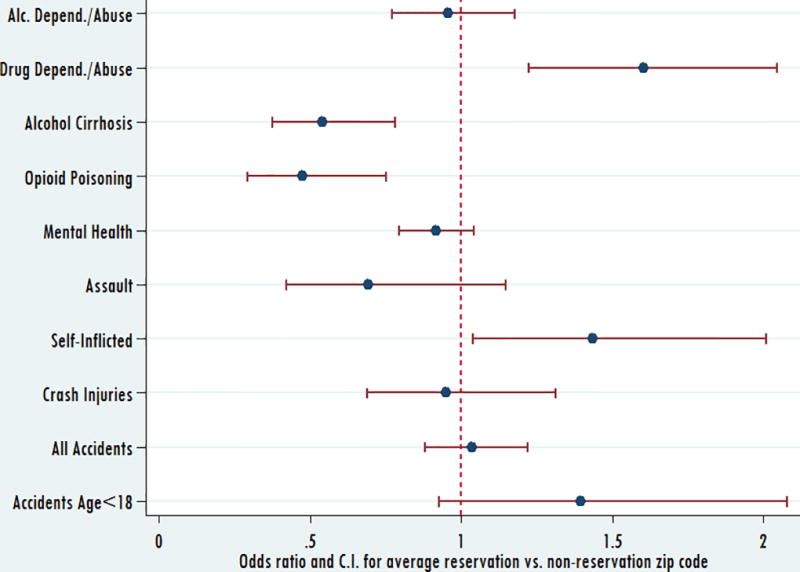
Odds ratios comparing estimated hospitalization risks associated with a zip code having its centroid within the boundaries of an American Indian reservation versus not being within a reservation. These calculations assume that all other zip-code characteristics are at study means.
DISCUSSION
The results of this study suggest that a variety of health issues that have been linked to the use of alcohol and other drugs are more likely to be experienced in areas with high concentrations of American Indian residents. This was observed to be the case both in terms of crude hospitalization rates and in terms of incidence rate ratios estimated from Bayesian Poisson models controlling for differences in population characteristics such as income, population density, age and gender, ethnic group composition, and location within an American Indian reservation. Importantly, however, although it would appear that American Indian populations may be at greater risk for these problems, these risks are shared across areas of South Dakota and Nebraska with greater proportions of Black residents, although not in areas with greater proportions of Hispanic residents. Indeed, greater proportions of Hispanic population were uniformly related to fewer problems than were proportions of American Indian residents, with the difference being well-supported in 9 of 10 analyses. These findings suggest that the effects observed may, therefore, be related to a history of multi-generational economic and social disadvantage related to these two groups rather than specifically to American Indian ethnicity or heritage per se.
Unlike many other ethnically-defined groups in the U.S., people of African and indigenous ancestries share legacies of historical trauma due to the massive violence and expropriations through which they have come involuntarily to be citizens of the U.S. (Brave Heart, 2003; Eyerman, 2001). On-going violence, both physical and structural, may contribute to the continuation of social disadvantage: for example, American Indians have the highest per capita rates of violent victimization of all race/ethnic groups (Perry, 2004); American Indians are as or more likely to be killed by police (Males, 2014); American Indians become incarcerated at 4.3 times the rates for whites (Hartney & Vuong, 2009). These disparities become more pronounced in some regions: American Indians have far higher risks for being jailed in the Northern Plains states of Minnesota, North Dakota, South Dakota, and Nebraska than in any other US states (Hartney & Vuong, 2009).
The data and analyses presented here speak powerfully to the role that social and economic disadvantage plays in this region. These profound effects may well be linked to the history that these reservations in South Dakota and Nebraska were redlined by banks for over 70 years, forbidden from any access to capital, helping to generate their third world-like conditions today (Chavers, 2009). This observation would help explain why problems are worse in reservation zip codes (as shown in Table 3), but doesn’t help to explain why percent American Indian of a population is so strongly linked to health conditions in any given zip code. These conditions are not unlike those which have deprived minority Black populations of access to economic and social resources for many decades and multiple generations (Dymski & Mason, 2005). Although lifetime experiences of trauma and post-traumatic stress have been associated with behavioral health risks in Hispanic populations (Ehlers et al., 2016; Melroy-Greif, Wilhelmsen, Yehuda, & Ehlers, 2017), these effects are magnified and maintained–affectively and perhaps genetically–in populations for whom large-scale major traumas continue to be experienced across generations, as historical trauma (Ehlers, Gizer, Gilder, Ellingson, & Yehuda, 2013; Nutton & Fast, 2015; Soto, Baezconde-Garbanati, Schwartz, & Unger, 2015; Sule et al., 2017; Truesdale-Moore, 2017). Recent research links “historical trauma” to changes in DNA methylation (so-called epigenetic changes) (Aguiar & Halseth, 2013; Brockie, Heinzelmann, & Gill, 2013), although among American Indians and Alaska Natives this research may be limited by indigenous people’s understandable reluctance to provide tissue for such analyses (Lock, 2015). AIANs living in “tribal” zip codes are at risk for poorer health, and therefore possibly more adverse changes in methylation, than those living in metropolitan statistical areas. For example, AIANs living on or immediately near their reservation have considerably higher rates of cancer than AI/ANs living in urban areas (Wiggins et al., 2008).
These analyses also speak powerfully to the economic and demographic conditions which, independent of ethnic group status, are also related to greater health risks across rural communities; incidences of mental health problems, accidents of all kinds, and those among persons under 18 years of age were greater in areas with lower population density. Coupled with the lower incomes that are characteristically observed in rural areas of the U.S. (Hawk, 2013), risks for all types of alcohol and drug related outcomes appear to be substantively greater in rural areas. Thus, the health burdens of minority or Native status may be exacerbated in rural communities.
Study Limitations
This study uses hospitalization data at the zip code level for the purpose of health surveillance. As Probst and colleagues have observed regarding health surveillance in rural settings “if results are aggregated at a state or national level, planners may never recognize that rural racial/ethnic minority populations are not receiving intended programs and services” (Probst, Moore, Glover, & Samuels, 2004, p.1700). The current study takes advantage of these data to examine health outcomes across areas of two largely rural states in an effort to identify where the incidence of alcohol and drug related health problems are greatest. In terms of public health surveillance, although zip code hospital utilization data are poorly resolved with regard to areas within communities, with most communities identified by single zip codes, they do give a sense of differences between communities across the large geographic expanses that compose rural areas of all states in the U.S. This benefit comes at some cost, however. In particular, although the observed statistical differences between areas are accurately assessed and can be interpreted without concern, risks for the ecological fallacy are substantive and should be carefully avoided. While it is possible to interpret aggregate effects as originating in ethnically-specific social structures, experiences, and behaviors, the validity of these assertions is in doubt without supplemental research. As such, surveillance analyses of the current type serve well to direct research resources toward rural areas in which specific rural health issues can be fruitfully explored.
A further limitation is that the hospitalization data used in this study provide no way to assess whether geographic distribution of gene polymorphisms can help explain elevated risks for alcohol and drug problems among these American Indian populations. There has been considerable research into alcohol and acetaldehyde dehydrogenase genetics and American Indians, without conclusive results which may inform this study. Ehlers and colleagues have concluded that, while at least part of the liability for alcohol dependence, is genetically driven (Ehlers, Wall, Betancourt, & Gilder, 2004; Peng et al., 2014), nevertheless molecular genetic studies provide little support for the hypothesis that Native American groups have an unusual metabolism of alcohol which might explain observed elevated rates of alcohol dependence, and that such rates will be most likely be explained by environmental as well as genetic factors, which may vary across American Indian groups (Ehlers & Gizer, 2013; Ehlers, Liang, & Gizer, 2012; Enoch & Albaugh, 2017; Gizer, Edenberg, Gilder, Wilhelmsen, & Ehlers, 2011).
Other limitations of the current study include (1) these are incidence, not prevalence, data and so the current results must be interpreted with this in mind; (2) hospital discharge data identify zip code of residence, which may not correspond to where drinking or injuries happen (Amram et al., 2015) and this may be even more exaggerated for reservation residents, many of whom live there part-time; (3) areas of reservations do not match perfectly to zip codes, and no zip codes had centroids within 3 of the 13 reservations in the states studied; and (4) there is a critical distinction between the two health data sources analyzed here: the HCUP data cover inpatient admission discharges which require an overnight stay, often representing more serious health outcomes. The Indian Health Service, which like other Federal hospitals is excluded from HCUP, primarily serves outpatient cases, discharges from which are dominated by either chronic conditions which require frequent visits (i.e., alcohol abuse) or acute outcomes frequently addressed in outpatient settings (i.e., minor assaults, Table 2).
In conclusion: the analyses presented here suggest that zip-code incidence rates of alcohol- and drug-related health problems are positively related to population proportions of both American Indians and African Americans. This was true even after accounting for numerous other demographic and economic characteristics of zip code areas such as income, poverty and population density. These health risks were not consistently related to whether a zip code was located within an American Indian reservation. The results imply that health disparities among both American Indians and African Americans may be related to both current differences in their local living conditions (e.g., income and rural status) and to independent factors related to long-standing disadvantage among their respective populations.
Acknowledgments
Research for and preparation of this manuscript were supported by a supplement to National Institute on Alcohol Abuse and Alcoholism Research Center Grant Number P60-AA06282 as well as National Institute on Alcohol Abuse and Alcoholism Research Grant Number R01-AA023755.
Footnotes
While Indian reservations are sometimes spoken of as “being within” or “belonging to” states, reservations are the land bases of sovereign nations with nation-to-nation relationships with the U.S. Federal Government and therefore are spatially separate from states.
The boundaries of Indian reservations have been established through treaties with the United States government. In the Northern Plains region, the Fort Laramie Treaty of 1868 established the entire western half of the state of South Dakota as the Great Sioux Reservation, but subsequent acts of Congress broke up this reservation into numerous smaller reservations, which have been further reduced through various state and federal appropriations, so that the boundaries of many present-day reservations are contested. For our analyses we use reservation boundaries as presented in the U.S. Census Bureau’s “2014 TIGER/Line Shapefiles: American Indian Area Geography”, downloaded from https://www.census.gov/cgi-bin/geo/shapefiles/index.php?year=2014&layergroup=American+Indian+Area+Geography on 4/28/2016.
References
- Agency for Healthcare Research and Quality. HCUP State Inpatient Databases (SID). Healthcare Cost and Utilization Project (HCUP). 2007–2012. 2007–2012 Retrieved from: www.hcup-us.ahrq.gov/sidoverview.jsp.
- Aguiar W, Halseth R. Aboriginal peoples and historic trauma: the processes of intergenerational transmission. Canada: National Collaborating Centre for Aboriginal Health= Centre de collaboration nationale de la santé autochtone; 2013. [Google Scholar]
- Amram O, Schuurman N, Yanchar NL, Pike I, Friger M, Griesdale D. Use of geographic information systems to assess the error associated with the use of place of residence in injury research. Injury Epidemiology. 2015;2(1):1–8. doi: 10.1186/s40621-015-0059-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardinelli L, Clayton D, Pascutto C, Montomoli C, Ghislandi M, Songini M. Bayesian analysis of space—time variation in disease risk. Statistics in Medicine. 1995;14(21–22):2433–2443. doi: 10.1002/sim.4780142112. [DOI] [PubMed] [Google Scholar]
- Besag J, York J, Mollié A. Bayesian image restoration, with two applications in spatial statistics. Annals of the Institute of Statistical Mathematics. 1991;43(1):1–20. [Google Scholar]
- Borders TF, Booth BM. Rural, suburban, and urban variations in alcohol consumption in the United States: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Rural Health. 2007;23(4):314–321. doi: 10.1111/j.1748-0361.2007.00109.x. [DOI] [PubMed] [Google Scholar]
- Brave Heart MY. The historical trauma response among natives and its relationship with substance abuse: a Lakota illustration. J Psychoactive Drugs. 2003;35(1):7–13. doi: 10.1080/02791072.2003.10399988. [DOI] [PubMed] [Google Scholar]
- Brockie TN, Heinzelmann M, Gill J. A framework to examine the role of epigenetics in health disparities among Native Americans. Nursing Research And Practice. 2013;2013:410395–410395. doi: 10.1155/2013/410395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calcaterra S, Glanz J, Binswanger IA. National trends in pharmaceutical opioid related overdose deaths compared to other substance related overdose deaths: 1999–2009. Drug Alcohol Depend. 2013;131(3):263–270. doi: 10.1016/j.drugalcdep.2012.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlin BP, Louis TA. Bayes and empirical Bayes methods for data analysis (2nd ed.) New York: Chapman & Hall; 2000. [Google Scholar]
- Caspi A, Moffitt TE, Cannon M, McClay J, Murray R, Harrington H, Craig IW. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene × environment interaction. Biol Psychiatry. 2005;57(10):1117–1127. doi: 10.1016/j.biopsych.2005.01.026. [DOI] [PubMed] [Google Scholar]
- Cerda M, Diez-Roux AV, Tchetgen ET, Gordon-Larsen P, Kiefe C. The relationship between neighborhood poverty and alcohol use: estimation by marginal structural models. Epidemiology. 2010;21(4):482–489. doi: 10.1097/EDE.0b013e3181e13539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavers D. Racism in Indian Country. Peter Lang; New York, NY: 2009. [Google Scholar]
- Cunningham JK, Solomon TA, Muramoto ML. Alcohol use among Native Americans compared to whites: Examining the veracity of the "Native American elevated alcohol consumption" belief. Drug & Alcohol Dependence. 2015;160:65–75. doi: 10.1016/j.drugalcdep.2015.12.015. [DOI] [PubMed] [Google Scholar]
- Dymski GA, Mason PL. Racial Inequality and African Americans' Disadvantage in the Credit and Capital Markets. African Americans in the US Economy, edited by Cecilia Conrad. 2005:151–156. [Google Scholar]
- Ehlers CL, Gizer IR. Evidence for a genetic component for substance dependence in Native Americans. Am J Psychiatry. 2013;170(2):154–164. doi: 10.1176/appi.ajp.2012.12010113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers CL, Gizer IR, Gilder DA, Ellingson JM, Yehuda R. Measuring historical trauma in an American Indian community sample: contributions of substance dependence, affective disorder, conduct disorder and PTSD. Drug Alcohol Depend. 2013;133(1):180–187. doi: 10.1016/j.drugalcdep.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers CL, Kim C, Gilder DA, Stouffer GM, Caetano R, Yehuda R. Lifetime history of traumatic events in a young adult Mexican American sample: Relation to substance dependence, affective disorder, acculturation stress, and PTSD. J Psychiatr Res. 2016;83:79–85. doi: 10.1016/j.jpsychires.2016.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers CL, Liang T, Gizer IR. ADH and ALDH polymorphisms and alcohol dependence in Mexican and Native Americans. Am J Drug Alcohol Abuse. 2012;38(5):389–394. doi: 10.3109/00952990.2012.694526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers CL, Wall TL, Betancourt M, Gilder DA. The clinical course of alcoholism in 243 Mission Indians. Am J Psychiatry. 2004;161(7):1204–1210. doi: 10.1176/appi.ajp.161.7.1204. [DOI] [PubMed] [Google Scholar]
- Enoch MA, Albaugh BJ. Review: Genetic and environmental risk factors for alcohol use disorders in American Indians and Alaskan Natives. Am J Addict. 2017;26(5):461–468. doi: 10.1111/ajad.12420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ESRI. ESRI Data and Maps (DVD) 2012 [Google Scholar]
- Eyerman R. Cultural Trauma: Slavery and the Formation of African American Identity. Cambridge, UK: Cambridge University Press; 2001. [Google Scholar]
- Geolytics. Geolytics Estimates Premium. East Brunswick, NJ: Geolytics, Inc; 2013. [Google Scholar]
- Gilder DA, Gizer IR, Lau P, Ehlers CL. Stimulant dependence and stimulant-associated psychosis: clinical characteristics and age of onset in a native American community sample. J Addict Med. 2014;8(4):241–248. doi: 10.1097/adm.0000000000000039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gizer IR, Edenberg HJ, Gilder DA, Wilhelmsen KC, Ehlers CL. Association of alcohol dehydrogenase genes with alcohol-related phenotypes in a Native American community sample. Alcohol Clin Exp Res. 2011;35(11):2008–2018. doi: 10.1111/j.1530-0277.2011.01552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Huang B. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72(8):757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfeld LA, Smith SK. American Indians and Crime. (NCJ 173386) Washington, D.C.: 1999. Retrieved from https://www.bjs.gov/content/pub/pdf/aic.pdf. [Google Scholar]
- Harrison PM. Management of patients with decompensated cirrhosis. Clin Med (Lond) 2015;15(2):201–203. doi: 10.7861/clinmedicine.15-2-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartney C, Vuong L. Created Equal: Racial and Ethnic Disparities in the US Criminal Justice System. 2009 Retrieved from http://www.nccdglobal.org/publications/created-equal-racial-and-ethnic-disparities-in-the-us-criminal-justice-system.
- Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, Grant BF. Prevalence and Correlates of DSM-5 Cannabis Use Disorder, 2012–2013: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Am J Psychiatry. 2016;173(6):588–599. doi: 10.1176/appi.ajp.2015.15070907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawk W. Expenditures of urban and rural households in 2011 2013 [Google Scholar]
- Hingson RW, Edwards EM, Heeren T, Rosenbloom D. Age of drinking onset and injuries, motor vehicle crashes, and physical fights after drinking and when not drinking. Alcohol Clin Exp Res. 2009;33(5):783–790. doi: 10.1111/j.1530-0277.2009.00896.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Edwards EM. Age at drinking onset, alcohol dependence, and their relation to drug use and dependence, driving under the influence of drugs, and motor-vehicle crash involvement because of drugs. J Stud Alcohol Drugs. 2008;69(2):192–201. doi: 10.15288/jsad.2008.69.192. [DOI] [PubMed] [Google Scholar]
- Landen M, Roeber J, Naimi T, Nielsen L, Sewell M. Alcohol-attributable mortality among American Indians and Alaska Natives in the United States, 1999–2009. American Journal of Public Health. 2014;104(S3):S343–S349. doi: 10.2105/AJPH.2013.301648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lock M. Comprehending the body in the era of the epigenome. Current Anthropology. 2015;56(2):151–177. doi: 10.1086/680350. [DOI] [Google Scholar]
- Lord D, Washington SP, Ivan JN. Poisson, Poisson-gamma and zero-inflated regression models of motor vehicle crashes: balancing statistical fit and theory. Accid Anal Prev. 2005;37(1):35–46. doi: 10.1016/j.aap.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Lunn DJ, Thomas A, Best N, Spiegelhalter D. WinBUGS-a Bayesian modelling framework: concepts, structure, and extensibility. Statistics and Computing. 2000;10(4):325–337. [Google Scholar]
- Males M. [Accessed 21 Dec. 2017];Who are police killing? [online] Center on Juvenile and Criminal Justice. 2014 Available at: http://www.cjcj.org/news/8113.
- Melroy-Greif WE, Wilhelmsen KC, Yehuda R, Ehlers CL. Genome-Wide Association Study of Post-Traumatic Stress Disorder in Two High-Risk Populations. Twin Res Hum Genet. 2017;20(3):197–207. doi: 10.1017/thg.2017.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mowery PD, Dube SR, Thorne SL, Garrett BE, Homa DM, Nez Henderson P. Disparities in Smoking-Related Mortality Among American Indians/Alaska Natives. Am J Prev Med. 2015;49(5):738–744. doi: 10.1016/j.amepre.2015.05.002. [DOI] [PubMed] [Google Scholar]
- Nutton J, Fast E. Historical Trauma, Substance Use, and Indigenous Peoples: Seven Generations of Harm From a "Big Event". Subst Use Misuse. 2015;50(7):839–847. doi: 10.3109/10826084.2015.1018755. [DOI] [PubMed] [Google Scholar]
- Parker RN, Auerhahn K. Alcohol, Drugs, and Violence. Annual Review of Sociology. 1998;24(1):291–311. doi: 10.1146/annurev.soc.24.1.291. [DOI] [Google Scholar]
- Peng Q, Gizer IR, Libiger O, Bizon C, Wilhelmsen KC, Schork NJ, Ehlers CL. Association and ancestry analysis of sequence variants in ADH and ALDH using alcohol-related phenotypes in a Native American community sample. Am J Med Genet B Neuropsychiatr Genet. 2014;165B(8):673–683. doi: 10.1002/ajmg.b.32272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry SW. Bureau of Justice Statistics, American Indians and Crime: A BJS Statistical Profile, 1992-2002. (NCJ 203097, Dec. 2004). [Google Scholar]
- Probst JC, Moore CG, Glover SH, Samuels ME. Person and place: the compounding effects of race/ethnicity and rurality on health. American Journal of Public Health. 2004;94(10):1695–1703. doi: 10.2105/ajph.94.10.1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riva M, Gauvin L, Barnett TA. Toward the next generation of research into small area effects on health: a synthesis of multilevel investigations published since July 1998. Journal of Epidemiology and Community Health. 2007;61(10):853–861. doi: 10.1136/jech.2006.050740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HG, Coffey R, Jones J, Heslin KC, Moy E. The effects of multiple chronic conditions on hospitalization costs and utilization for ambulatory care sensitive conditions in the United States: a nationally representative cross-sectional study. BMC Health Services Research. 2016;16(1):1. doi: 10.1186/s12913-016-1304-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soto C, Baezconde-Garbanati L, Schwartz SJ, Unger JB. Stressful life events, ethnic identity, historical trauma, and participation in cultural activities: Associations with smoking behaviors among American Indian adolescents in California. Addict Behav. 2015;50:64–69. doi: 10.1016/j.addbeh.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sule E, Sutton RM, Jones D, Moore R, Igbo I, Jones LA. The Past Does Matter: a Nursing Perspective on Post Traumatic Slave Syndrome (PTSS) J Racial Ethn Health Disparities. 2017 doi: 10.1007/s40615-016-0328-7. [DOI] [PubMed] [Google Scholar]
- Truesdale-Moore S. Race, Ethnicity and Law. Emerald Publishing Limited; 2017. Understanding the Historical Influences on Contemporary Assessment and Counseling Issues of African American Offenders; pp. 39–61. [Google Scholar]
- Waller LA, Gotway CA. Applied Spatial Statistics for Public Health Data. New York: Wiley-Interscience; 2004. [Google Scholar]
- Wiggins CL, Espey DK, Wingo PA, Kaur JS, Wilson RT, Swan J, Lanier AP. Cancer among American Indians and Alaska Natives in the United States, 1999–2004. Cancer. 2008;113(S5):1142–1152. doi: 10.1002/cncr.23734. [DOI] [PubMed] [Google Scholar]
- Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend. 2004;76(Suppl):S11–19. doi: 10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Zhu L, Waller LA, Ma J. Spatial-temporal disease mapping of illicit drug abuse or dependence in the presence of misaligned ZIP codes. Geojournal. 2013;78(3):463–474. doi: 10.1007/s10708-011-9429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


