Abstract
Smoke-free policies effectively reduce secondhand smoke (SHS) exposure among non-smokers, and reduce consumption, encourage quit attempts, and minimize relapse to smoking among smokers. Such policies are uncommon in permanent supportive housing (PSH) for formerly homeless individuals. In this study, we collaborated with a PSH provider in San Diego, California to assess a smoke-free policy that restricted indoor smoking. Between August and November 2015, residents completed a pre-policy questionnaire on attitudes toward smoke-free policies and exposure to secondhand smoke, and then 7–9 months after policy implementation residents were re-surveyed. At follow-up, there was a 59.7% reduction in indoor smoking. The proportion of residents who identified as current smokers reduced by 13% (95% CI: −38, 10.2). The proportion of residents who reported never smelling SHS indoors (apartment 24.2%, 95% CI: 4.2, 44.1; shared areas 17.2%, 95% CI: 1.7, 32.7); in outdoor areas next to the living unit (porches or patio 56.7%, 95% CI: 40.7, 72.8); and in other outdoor areas (parking lot 28.6%, 95% CI: 8.3, 48.9) was lower post-policy compared with pre-policy. Overall, resident support increased by 18.7%; however, the greatest increase in support occurred among current smokers (from 14.8 to 37.5%). Fewer current smokers reported that the policy would enable cessation at post-policy compared to pre-policy. Our findings demonstrate the feasibility of implementing smoke-free policies in PSH for formerly homeless adults. However, policy alone appears insufficient to trigger change in smoking behavior, highlighting the need for additional cessation resources to facilitate quitting.
Background
Permanent supportive housing (PSH) is a highly successful federal program that offers subsidized permanent housing with on-site or closely linked supportive services (e.g. case management, substance use treatment) to formerly homeless adults [1–5]. PSH residents have a history of chronic homelessness and often have comorbid mental illness and substance use disorders [6], both of which are risk factors for smoking.
The prevalence of smoking among homeless adults is substantially higher (approximately 70%) than that of the general U.S. population (15.1%) [7–11]. Smoking-related cancers and other non-malignant chronic diseases are the leading causes of morbidity and mortality for homeless adults aged 45 years and older [10, 12–15]. For homeless adults who are younger than 45 years, the incidence of smoking-related chronic diseases is three times higher than the age-matched general population [14]. The increased tobacco-related burden among this population underscores the urgent need for effective policies and cessation interventions.
According to the existing research, PSH is the preferred and most effective way to end chronic homelessness [16–18]. PSH generally operates under the Housing First model which utilizes a harm-reduction philosophy, where receipt of housing is not contingent upon demonstration of substance use abstinence or engagement in mental health treatment. Studies have shown that receipt of Housing First is one of the major predictors of staying housed and engaging in mental health and substance use treatment [19]. PSH could offer a promising venue for smoking cessation because it offers a secure and stable environment for behavior change while being housed. Integrating smoking cessation treatment and smoke-free policies in supportive housing could be important because homeless adults face many barriers to cessation including lack of access to cessation resources and lack of access to smoke-free living environments [14].
Smoke-free policies are effective in reducing secondhand smoke (SHS) exposure among non-smokers [20] and reducing consumption, encouraging quit attempts, and minimizing relapse to smoking among smokers [21]. In subsidized multi-unit housing, smoke-free policies have changed norms around smoking and encouraged change in smoking behaviors among low-income adults [22]; however, such policies are uncommon in PSH for formerly homeless individuals.
Previous research on attitudes toward smoke-free policies in shelters has found that homeless adults are supportive of these policies to protect non-smokers and children from SHS-related harms [23–25]. These studies have also found that smoke-free policies could motivate reductions in smoking behaviors and interest in quitting among some homeless adults [24]. To date, no studies have explored the implementation of smoke-free policies in PSH for formerly homeless adults.
In this study, we partnered with a PSH provider in San Diego, California to evaluate a smoke-free policy that restricted indoor smoking in its properties. We hypothesized that the smoke-free policy would reduce consumption and increase interest in cessation smoking among residents who were smokers, and decrease self-reported exposure to SHS among smokers and non-smokers.
Methods
Study Design, Procedures and Recruitment
We conducted a pre/post policy evaluation in collaboration with a PSH provider that planned to implement an indoor smoke-free policy, effective January 1, 2016, in all four of its properties. The policy prohibited smoking indoors in living units, in shared areas, and within 25 feet of exits and windows. Prior to the policy change, between August 2015 and November 2015, trained on-site study staff announced the study during group meetings and administered a questionnaire to all residents living in the four affiliated PSH properties who were 18 years or older and able and willing to provide informed consent. Participants provided verbal consent prior to completing the questionnaire. Prior to implementation of the policy, residents were provided with information on local smoking cessation resources.
Seven to nine-months after implementation of the smoke-free policy, eligible residents completed the same questionnaire. Residents were encouraged but not required to complete both (pre- and post-policy) questionnaires. New residents that had moved in during the interim were invited to complete the post-policy questionnaire. We attempted to match residents who completed both questionnaires using unique personal characteristics that were provided by resident participants (e.g. name of childhood elementary school, pet or friend, type of first car).
During the timeframe in which the post-policy questionnaires were administered, staff members were invited to complete a separate questionnaire focused on their knowledge and attitudes toward the smoke-free policy; level and frequency of complaints; experiences with enforcement of the policy; and perceived barriers. The University of California, San Francisco Committee on Human Research approved all study protocols.
Measures
Smoking Behavior
We used standard questions from prior national surveys to probe smoking behaviors in the pre- and post-policy questionnaires [26]. We asked participants to report whether they had ever smoked 100 cigarettes in their lifetime, and classified those who had as ever smokers. Ever smokers were subsequently asked whether they smoked “every day” or “some days” (current smokers) or “not at all” (former smokers). We asked current smokers to report the time it took to smoke their first cigarette after waking (after 60, 31–60, 6–30 min, or within 5 min), the number of cigarettes smoked on smoking days in the past week (average daily cigarette consumption), and whether they had an intention to quit smoking using the following response options: never expect to quit; may quit in the near 6 months; will quit in the next 6 months; will quit in the next month. Current smokers were also asked whether they had made a quit attempt in past 12 months and, if they did, to report the duration of the quit attempt.
Attitudes Toward Smoke-Free Policies
Attitudes toward the proposed no-smoking policy were assessed by asking all residents to indicate their level of agreement with the following statements: I support the proposed policy; I am happy to stay on this property because of the proposed policy; I would choose to live in a facility that had a policy that restricted smoking indoors. Residents responded using the following options: strongly disagree, disagree, neither agree nor disagree, agree, or strongly agree. We also asked current smokers to indicate their level of agreement with the following statements about a smoke-free policy that restricted smoking in indoor areas: I think I would be much more irritable because of the proposed policy; I would try to cut down on my smoking; I would try to quit smoking for a short time because of the proposed policy; I would try to stop smoking completely because of the proposed policy. We assessed residents’ knowledge of the no-smoking policy and adherence to the policy by asking where they currently smoke when at home (smoke in my apartment, outside on the porch or balcony, outside in other outdoor areas of the property). At follow-up, we used the same items to assess attitudes, knowledge and adherence to the “current” policy as opposed to the “proposed” policy.
Secondhand Smoke Exposure
We asked residents at both time points to report their exposure to SHS. Specifically, residents were asked to indicate how often during the past month they had smelled SHS inside their apartment, in the indoor shared areas, or outdoors, using the following response options: every day, a few times a week, a few times a month, hardly ever or never.
Resident Demographics
Residents self-reported their age, sex (male, female, and transgender), race (Black/African American, White, Latino, and Asian/Mixed/other), highest level of education (Less than high school, High school or GED, Some college, College or other profession training), whether they were currently employed, and estimated yearly income. We also asked how long they had lived at the current facility. Residents self-reported whether they had any of the following health problems: arthritis; lung or breathing problem; hearing problem; eye/vision problem; heart problem; stroke problem; diabetes; hypertension/high blood pressure; cancer; depression; anxiety; other psychological/emotional problem.
Enforcement, Complaints and Barriers to Enforcing Policies
After the policy implementation, we asked staff participants to complete a questionnaire on barriers to and facilitators of enforcement of the smoke-free policy. We asked staff to report the frequency (very frequently, frequently, occasionally, rarely, very rarely) with which they had to issue a verbal warning, written warning, or written violation in the past 6 months, and whether they had issued any evictions related to the policy (yes/no) in the same time period. We asked staff to indicate their level of agreement (5 point Likert scale) with the following perceived barriers to enforcement; residents smoking indoors/not following policy, lack of time to enforce the policy, lack of resources to support smoking cessation for residents and staff, concern for residents’ rights to smoke, and concern for occupancy rate.
Analysis
We calculated descriptive statistics for residents’ demographics, smoking behaviors, SHS exposure, and attitudes toward the proposed and current smoke-free policies. We calculated measures of central tendency (median and inter-quartile range; mean and standard deviations) for continuous variables and proportions for categorical variables. In order to compare participants’ responses before and after the policy was implemented, we calculated percent changes and 95% confidence intervals. We calculated percent changes using generalized linear models with robust standard errors, which accounted for correlation of responses among the individuals who completed both survey rounds. We reported percent differences in smoking behaviors, SHS exposure, and attitudes toward the policy between the pre- and post-policy samples. For attitudes toward the policy, we examined difference by smoking status (non-smokers vs. current smokers) using the Chi square test among the samples present at both time points. All analyses were conducted with Stata v. 14.0 [27].
Results
A total of 55 residents (response rate 58%) completed the pre-policy questionnaire. Fifteen of these residents also completed the post-policy questionnaire, as did 27 other residents who had not completed the pre-policy questionnaire (n = 42; 44% response rate). The median age of the pre-policy sample was 53 years (IQR 46–63), approximately half of the sample was male (52%), White (54%), and the majority had completed at least some college (67%) (Table 1). The median number of health problems reported was 2 (IQR 1–5), and the most commonly reported health problems were depression (58%) and anxiety (54.6%). There were no significant demographic differences between the pre- and post-policy samples.
Table 1.
Demographic characteristics of samples before and after implementation of smoke-free policy
| Characteristic—no. (%) | Pre-policy (N = 55) | Post-policy (N = 42) |
|---|---|---|
| Sex | ||
| Male | 29 (52.7) | 23 (54.8) |
| Female | 23 (41.8) | 15 (35.7) |
| Smoking status | ||
| Current smoker | 27 (49.1) | 16 (13.1) |
| Former smoker | 7 (12.7) | 8 (19.1) |
| Never smoker | 21 (38.2) | 18 (42.9) |
| Race/ethnicity | ||
| Hispanic | 5 (9.1) | 1 (2.4) |
| Non-Hispanic black | 9 (16.4) | 8 (19.1) |
| Non-Hispanic white | 30 (54.6) | 21 (50.0) |
| Asian/other/mixed race | 5 (9.1) | 7 (16.7) |
| Education | ||
| Less than high school | 5 (9.01) | 2 (4.8) |
| High school or equivalent (GED) | 10 (18.2) | 13 (31.0) |
| Some college | 20 (36.4) | 14 (33.3) |
| College or other profession training | 17 (30.9) | 11 (26.2) |
| Employed | 8 (14.55) | 5 (11.90) |
| Yearly income | ||
| Less than $15,000 | 36 (65.5) | 30 (71.4) |
| More than $15,000 | 7 (12.7) | 7 (19.0) |
| Health problems | ||
| Depression | 32 (58.2) | 19 (45.2) |
| Anxiety | 30 (54.6) | 20 (47.6) |
| Other psychological/emotional | 16 (29.1) | 16 (38.1) |
| Arthritis | 16 (29.1) | 9 (21.4) |
| Eye/vision problem | 15 (27.3) | 12 (28.6) |
| Hypertension | 14 (25.5) | 11 (26.2) |
| Lung or breathing problems | 11 (20.0) | 8 (19.1) |
| Hearing problem | 7 (12.7) | 6 (14.3) |
| Heart problem | 3 (5.5) | 2 (4.8) |
| Stroke problem | 2 (3.6) | 1 (2.4) |
| Diabetes | 5 (9.1) | 4 (9.5) |
| Cancer | 2 (3.6) | 2 (4.8) |
| Years in Facility—mean (std) | 4.39 (5.2) | 4.90 (3.4) |
Cell counts do not sum up to column total because of missing responses
Tobacco Use
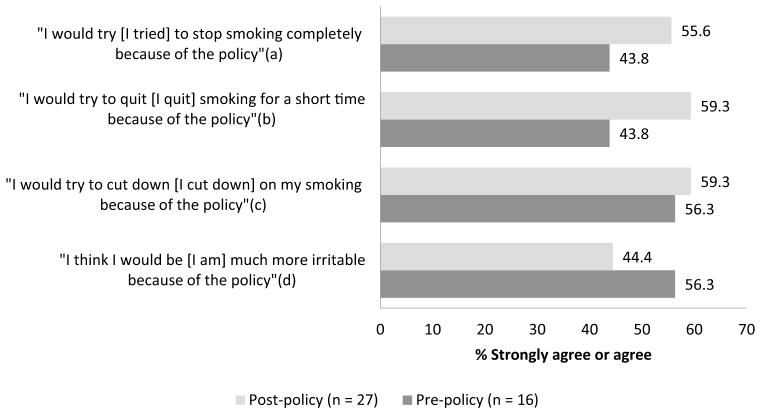
Post-policy, there was a 13.8% decrease in current daily smokers compared to the pre-policy sample (95% CI: −38, 10.2) (Table 2). Additionally, post-policy, there was a 31.3% (95% CI: 3.9, 58.6) increase in people who smoked after 60 min and a 57.6% (95% CI: −85.9, −29.3) decrease in people who needed to smoke within 5 min of waking, as compared to those in the pre-policy sample. Pre-policy, 55.6% (n = 15) of current smokers anticipated that they would cut down on their smoking because of the proposed policy and post-policy nearly the same proportion reported having actually cut back “as a result of the policy” (−1.5% change; 95% CI: −25.0, 28.1) (Fig. 1).
Table 2.
Tobacco use patterns among current smokers before and after implementation of smoke-free policy
| Characteristic | Pre-policy (n = 27) | Post-policy (n = 16) | Percent change (95% CI) | |
|---|---|---|---|---|
| Do you smoke every day or some days?—no. (%) | Every day | 24 (88.9) | 12 (75.0) | −13.8 (−38.0, 10.2) |
| Some days | 3 (11.1) | 4 (25.0) | ||
| If there were no smoking restrictions on you, how soon after you wake up would you have your first cigarette?—no. (%)a | After 60 min | 4 (14.8) | 7 (43.8) | 31.3 (3.9, 58.6) |
| 31–60 min | 4 (14.8) | 1 (6.3) | −8.7 (−27.9, 10.4) | |
| 6–30 min | 5 (18.5) | 1 (6.3) | −12.6 (−32.3, 7.2) | |
| Within 5 min | 13 (48.2) | 6 (37.5) | −57.6 (−85.9, −29.3) | |
| In the last month, have you smoked a cigarette where you were not supposed to?—no. (%) | Often | 1 (3.7) | 1 (6.3) | 3.0 (−11.9, 17.8) |
| Sometimes | 4 (14.8) | 3 (18.8) | 2.2 (−19.2, 23.6) | |
| Rarely | 3 (11.1) | 2 (12.5) | 5.2 (−20.1, 30.5) | |
| Never | 19 (70.4) | 9 (56.3) | −10.3 (−43.1, 22.4) | |
| What best describes your intention to quit smoking?—no. (%) | Never expect to quit | 7 (25.9) | 5 (31.3) | 9.8 (−19.9, 39.4) |
| May quit in next 6 months | 8 (29.6) | 3 (18.8) | −8.2 (−36.8, 20.4) | |
| Will quit in next 6 months | 5 (18.5) | 3 (18.8) | 2.9 (−23.6, 29.4) | |
| Will quit in next month | 7 (25.9) | 3 (18.8) | −4.5 (−32.0, 23.0) | |
| Stopped smoking for one day or longer because you were trying to quit smoking within the last 12 months—no. (% yes) | 20 (74.1) | 9 (56.3) | −9.8 (−3.7, 17.5) | |
| Average number of cigarettes consumed per day—mean (STD) | 12.9 (8.1) | 13.8 (8.1) | 0.94 (−3.8, 5.69) | |
Cell counts do not sum up to column total because of missing responses
Fig. 1.
Current smokers’ anticipated and reported responses to “proposed” and “current” smoke-free policy. Percent change (95% CI): (a) −11.0% (−40.3, 18.3); (b) −14.9% (−47.1, 17.3); (c) −1.5% (−28.1, 25.0); (d) 13.8% (−13.8, 41.5)
Secondhand Smoke Exposure
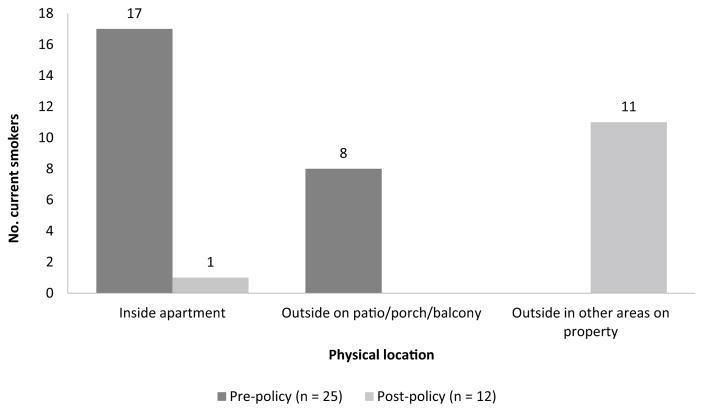
Between the pre- and post-policy survey time points there was a 59.7% (95% CI: −89.8, −31.5) decrease in the proportion of current smokers who reported smoking indoors in their apartments (Fig. 2). Consequently, post-policy, the proportion of residents who reported never smelling SHS during the last month increased in all locations queried (Table 3). Based on the reports, the most marked changes occurred in the outdoor areas, with a 56.7% (95% CI: 40.7, 72.8) and 28.2% (95% CI: 8.3, 48.9) increase in residents who reported never smelling SHS on patios and porches, and in other outdoor areas, respectively.
Fig. 2.
Reported locations where current smokers smoke when at home before and after implementation of smoke-free policy. [Missing responses: Pre = 2; Post = 4]
Table 3.
Reports of secondhand smoke exposure before and after implementation of the smoke-free policy
| Locations | Pre-policy (n = 55) | Post-policy (n = 42) | Percent change (95% CI) | |
|---|---|---|---|---|
| How often do you breathe or smell secondhand smoke | ||||
| Inside your apartment? | Never | 20 (36.4) | 26 (61.9) | 24.2 (4.2, 44.1) |
| Ever | 31 (56.4) | 15 (35.7) | ||
| In indoor shared areas? | Never | 36 (65.5) | 36 (85.7) | 17.2 (1.7, 32.7) |
| Ever | 15 (27.3) | 5 (11.9) | ||
| On porches or patios? | Never | 14 (25.5) | 35 (83.3) | 56.7 (40.7, 72.8) |
| Ever | 35 (63.6) | 6 (14.3) | ||
| In outdoor areas (parking lots)? | Never | 19 (34.6) | 27 (64.3) | 28.6 (8.3, 48.9) |
| Ever | 32 (58.2) | 14 (33.3) | ||
Cell counts do not sum up to column total because of missing responses
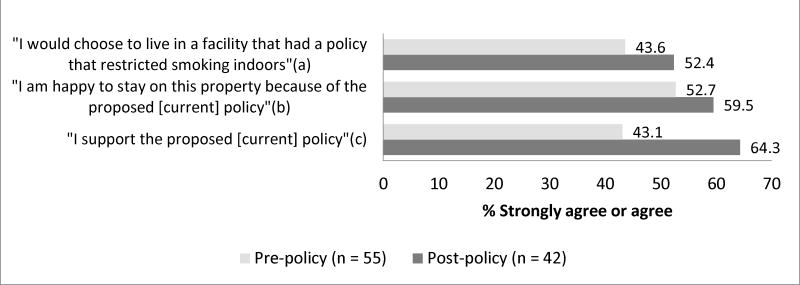
Attitudes Toward No-Smoking Policy
Overall, resident support for the smoke-free policy increased by 18.7% between the two time points (95% CI: 0.1, 36.7) (Fig. 3). In both pre- and post-policy surveys, non-smokers (never and former) were significantly more likely than current smokers to support the policy (pre-policy 65.6% vs. 14.8%; post-policy 75.0% vs. 37.5%). However, while current smokers reported lower overall levels of support pre- and post-policy, the greatest proportional increase in support for the policy occurred among current smokers (from 14.8 to 37.5%).
Fig. 3.
Attitudes towards “proposed” and “current” smoke-free policy in pre- and post-implementation samples. Percent change (95% CI): (a) 7.5% (−12.0, 27.0); (b) 10.3 (−9.3, 29.8); (c) 18.7% (0.1, 36.7)
Enforcement and Resident Complaints
At follow-up, five staff members completed the staff questionnaire (100% response rate). Their roles included director, property manager, and supervising resident manager, and all reported having college or professional training. Three of the staff members were male, two reported being a current smoker and two reported being a former smoker. Four staff members reported having heard complaints about the policy, however, as a whole, they did not perceive there to be a difference in frequency of complaints between smokers and nonsmokers. Four indicated that they had “challenges enforcing the policy”, and when asked how often they had issued verbal warning the responses ranged from “occasionally” (n = 3) to “very rarely” (n = 1). Similarly, when asked how often they had issued “written warnings” the responses ranged from “occasionally” (n = 3) to “very rarely” (n= 1). There was one “near eviction” that was in part related to repeated violations of the smoke-free policy, which was avoided by making arrangements for the resident to move to another facility. “Lack of time to enforce the policy” and “residents smok[ing] too close to non-smoking areas” were identified as barriers to enforcing the policy. However, “lack of resources for smoking cessation”, “concern for residents’ right to smoke”, and “concern for occupancy rates” were not perceived as barriers to enforcing the policy. All five staff members reported that they supported the current policy (“strongly agreed”).
Discussion
In this study, we examined the impact of a smoke-free policy on attitudes, cessation behaviors, and secondhand smoke exposure among residents living in PSH—a population associated with high rates of smoking. After implementation of a comprehensive smoke-free policy across the four participating PSH facilities, we found a 13.8% reduction in the number of residents who reported currently smoking, and, among current smokers, there was a 59.7% decrease in smoking indoors. Residents reported a 24.2% decrease in self-reported SHS exposure indoors after the policy implementation, and up to 56.7% decrease in outdoor area. Overall support for the policy remained high among staff and residents, and support for the policy increased after implementation among cigarette smoking residents.
Previous work has examined the feasibility of implementing smoke-free policies in homeless shelters. These studies found that sheltered homeless clients were supportive of the policies, and expressed interest in smoking cessation in relation to the policy [23, 24]. Our findings build on this work and demonstrate the feasibility of implementing smoke-free policies in PSH.
The smoke-free policy was motivated by a desire to promote the health and wellbeing of residents and staff. Supportive housing utilizes a harm-reduction framework that prioritizes housing stability without requiring abstinence from alcohol or drugs to obtain housing because receipt of housing is considered the foundation for recovery [28]. Therefore, implementing smoke-free policies in supportive housing may pose challenges because restricting a high-risk behavior may contradict supportive housing’s harm-reduction framework [28], potentially leading to unintended consequences of increasing unsheltered homeless should individuals leave their housing because of the policy. This study suggests that implementing smoke-free policies in PSH facilities is feasible and based on our findings; the newly adopted policy did not appear to negatively affect residents’ attitudes toward the living environment or their intention to stay. In contrast, support among never and former smokers was already high at baseline (>70%) and remained high, and among current smokers there was a significant increase in support post-policy. Furthermore, in spite of reports of challenges related to enforcement, staff members continued to report strong support for the policy, mirroring the overall positive response of the residents.
At baseline, the proportion of current smokers who reported that they anticipated stopping smoking completely, trying to quit for a short time and/or cutting down was actually higher before policy implementation than after, suggesting that residents anticipated or hoped that the policy would support them in their efforts to reduce tobacco use. As has been observed among homeless adults, these findings suggest that interest in quitting is high among the population in supportive housing [8, 29]. These findings in turn also speak to the need for greater access to smoking cessation services in combination with smoke-free policies to increase efficacy of quit attempts among residents in supportive housing.
The residents in this sample reported high rates of co-morbidities. It is well established that homeless individuals experience high burden of disease and health disparities, which are only compounded by smoking [30]. Residents of PSH rely primarily on Medicaid for access to medical services. Despite enhancements made to the coverage of tobacco dependence treatment in Medicaid, the reach remains limited [31]. In 2013, less than 10 percent of current smokers enrolled in Medicaid received cessation medications, and tobacco control experts have continued to identify gaps in smoking cessation services among vulnerable adult populations, including adults living in poverty and experiencing homelessness [31, 32]. PSH offers an integrated and holistic model of care for individuals who have experienced homelessness. However, more effort is needed to ensure that treatment for smoking cessation is included in these models of care to increase adherence to a smoke free policy and increase wellbeing among residents.
In order to maximize the effectiveness of smoke-free policies in reducing exposure to SHS and reducing tobacco use there is a need for greater understanding of the individual, social and environmental level barriers that influence support for smoke-free policies [33]. There are many factors that could influence support for smoke-free policy change and adoption. Using a social ecological framework, Hood et al. [33] identified a number of individual and social factors associated with support for smoke-free policies within subsidized multi-unit housing residents. Similar to the current study, support was higher among nonsmokers. In addition, they found higher levels of SHS-related knowledge, lower perceived acceptability of smoking in presence of children, and lack of perceived difficulty in addressing other’s smoking in the home to be associated with higher levels of support for smoke-free policies [33]. However, influencing factors may vary in the PSH population, particularly considering the high rate of co-morbidities in this population. The high rates of disability may influence whether or not residents can go outside to smoke. Additionally, for many this is the first housing they have had in years and they may be highly motivated to live in a clean, smoke-free home environment. Other factors that may be associated with support for smoke-free policies include, presence of children for those in families, and level of safety in the neighborhood to allow for smoking outdoors. Further studies are needed to understand the role these factors and others have on increasing support for smoke-free policies. Once identified, there is a need for tailored strategies, which address these individual- and social-level barriers to implementing smoke-free policies in supportive housing. Based on studies conducted in other multi-unit housing, the recommendation is that these be implemented in parallel with the adoption of smoke-free policies [22, 33].
Our study had limitations. While the sample was representative of the homeless population in San Diego, California based on 2015 point-in-time counts [34], the findings may not be generalizable to other PSH facilities in other parts of the United States with varied demographic distributions and social norms. The sample size was small and this may have limited the ability to detect differences between the pre- and post-policy samples. We were unable to gather information on non-respondents’ smoking status at time of follow-up, which may overestimate the policy’s effects on reducing current smoking. While the method used in this study for matching surveys in the two time points was selected to safeguard residents’ anonymity, we were unable to assess whether more than 15 residents had completed both surveys which raises the possibility that the confidence intervals reported throughout this manuscript overstate the precision of our point estimates. Finally, although used extensively in tobacco control research, the results of this study were based on self-reports, which are susceptible to social desirability, recall and misclassification bias [20]. Incorporating objective measures to evaluate smoking status and SHS exposure would enhance future studies.
Conclusions
The results of this study support the feasibility of implementing smoke-free policies within PSH. Post-policy, overall attitudes remained supportive of the smoke-free policy and resulted in significant reductions in self-reported exposure to SHS, particularly in outdoor areas. The large proportion of current smokers who reported having tried to quit, cut down, or tried to stop smoking completely because of the policy change highlights a role for smoke-free policy as a motivator of cessation behaviors. However, in order for these interventions to be more useful in promoting cessation it is critical that they are implemented in conjunction with access to smoking cessation support and resources.
Acknowledgments
We would like to thank the staff and residents at the supportive housing program that participated in this study.
Funding This study was funded by the NIH National Cancer Institute [Grant number: T32CA113710; Petersen was a postdoctoral fellow at the UCSF Center for Tobacco Control Research and Education when this work was completed]. Dr. Vijayaraghavan was supported by the Tobacco Related Disease Research Program [Grant number: 25IP-0015]. The funders played no role in the conduct of this research or the preparation of this manuscript.
Footnotes
Compliance with Ethical Standards
Conflict of interest The authors declare that they have no conflicts of interest.
References
- 1.HUD Exchange. Supportive housing program eligibility requirments. 2011 Retrieved from https://www.hudexchange.info/programs/shp/shp-eligibility-requirements/
- 2.Clifasefi SL, Malone DK, Collins SE. Exposure to project-based housing first is associated with reduced jail time and bookings. International Journal of Drug Policy. 2013;24(4):291–296. doi: 10.1016/j.drugpo.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Larimer ME, Malone DK, Garner MD, Atkins DC, Burlingham B, Lonczak HS, … Marlatt GA. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301(13):1349–1357. doi: 10.1001/jama.2009.414. [DOI] [PubMed] [Google Scholar]
- 4.Henwood BF, Katz ML, Gilmer TP. Aging in place within permanent supportive housing. International Journal of Geriatric Psychiatry. 2015;30(1):80–87. doi: 10.1002/gps.4120. [DOI] [PubMed] [Google Scholar]
- 5.Collins SE, Malone DK, Clifasefi SL, Ginzler JA, Garner MD, Burlingham B, … Larimer ME. Project-based Housing First for chronically homeless individuals with alcohol problems: Within-subjects analyses of 2-year alcohol trajectories. American Journal of Public Health. 2012;102(3):511–519. doi: 10.2105/AJPH.2011.300403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Padgett DK, Gulcur L, Tsemberis S. Housing first services for people who are homeless with co-occurring serious mental illness and substance abuse. Research on Social Work Practice. 2006;16(1):74–83. doi: 10.1177/1049731505282593. [DOI] [Google Scholar]
- 7.Connor SE, Cook RL, Herbert MI, Neal SM, Williams JT. Smoking cessation in a homeless population. Journal of General Internal Medicine. 2002;17(5):369–372. doi: 10.1046/j.1525-1497.2002.10630.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baggett TP, Rigotti NA. Cigarette smoking and advice to quit in a national sample of homeless adults. American Journal of Preventive Medicine. 2010;39(2):164–172. doi: 10.1016/j.amepre.2010.03.024. [DOI] [PubMed] [Google Scholar]
- 9.Gelberg L, Linn LS, Usatine RP, Smith MH. Health, homelessness, and poverty: A study of clinic users. Archives of Internal Medicine. 1990;150(11):2325–2330. doi: 10.1001/archinte.1990.00390220069014. [DOI] [PubMed] [Google Scholar]
- 10.Lee TC, Hanlon JG, Ben-David J, Booth GL, Cantor WJ, Connelly PW, Hwang SW. Risk factors for cardiovascular disease in homeless adults. Circulation. 2005;111(20):2629–2635. doi: 10.1161/circulationaha.104.510826. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Current cigarette smoking among adults—United States, 2005–2015. Morbidity and Mortality Weekly Report. 2016;65:1205–1211. doi: 10.15585/mmwr.mm6544a2. [DOI] [PubMed] [Google Scholar]
- 12.Hwang SW. Homelessness and health. Canadian Medical Association Journal. 2001;164(2):229–233. [PMC free article] [PubMed] [Google Scholar]
- 13.Hwang SW, Orav EJ, O’Connell JJ, Lebow JM, Brennan TA. Causes of death in homeless adults in Boston. Annals of Internal Medicine. 1997;126(8):625–628. doi: 10.7326/0003-4819-126-8-199704150-00007. [DOI] [PubMed] [Google Scholar]
- 14.Baggett TP, Hwang SW, O’Connell JJ, Porneala BC, Stringfellow EJ, Orav EJ, … Rigotti NA. Mortality among homeless adults in Boston: Shifts in causes of death over a 15-year period. JAMA Internal Medicine. 2013;173(3):189–195. doi: 10.1001/jamainternmed.2013.1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hwang SW, Wilkins R, Tjepkema M, O’Campo PJ, Dunn JR. Mortality among residents of shelters, rooming houses, and hotels in Canada: 11 year follow-up study. BMJ (Clinical Research ed) 2009;339:b4036. doi: 10.1136/bmj.b4036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Culhane DP, Metraux S, Byrne T. A prevention-centered approach to homelessness assistance: A paradigm shift? Housing Policy Debate. 2011;21(2):295–315. doi: 10.1080/10511482.2010.536246. [DOI] [Google Scholar]
- 17.Rog DJ, Marshall T, Dougherty RH, George P, Daniels AS, Ghose SS, Delphin-Rittmon ME. Permanent supportive housing: Assessing the evidence. Psychiatric Services. 2014;65(3):287–294. doi: 10.1176/appi/ps.201300261. [DOI] [PubMed] [Google Scholar]
- 18.Tsemberis S. Housing First: Ending homelessness, promoting recovery and reducing costs. In: O’Flaherty B, Ellen IG, editors. How to house the homeless. New York, NY: Russell Sage Foundation; 2010. pp. 37–56. [Google Scholar]
- 19.Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: A randomized trial. JAMA. 2009;301(17):1771–1778. doi: 10.1001/jama.2009.561. [DOI] [PubMed] [Google Scholar]
- 20.International Agency for Research on Cancer & World Health Organization. Evaluating the effectiveness of smoke-free policies. Lyon, France: IARC Press, International Agency for Research on Cancer; 2009. [Google Scholar]
- 21.Mills AL, White MM, Pierce JP, Messer K. Home smoking bans among U.S. households with children and smokers opportunities for intervention. American Journal of Preventive Medicine. 2011;41(6):559–565. doi: 10.1016/j.amepre.2011.08.016. [DOI] [PubMed] [Google Scholar]
- 22.Pizacani BA, Maher JE, Rohde K, Drach L, Stark MJ. Implementation of a smoke-free policy in subsidized multiunit housing: Effects on smoking cessation and secondhand smoke exposure. Nicotine & Tobacco Research. 2012;14(9):1027–1034. doi: 10.1093/ntr/ntr334. [DOI] [PubMed] [Google Scholar]
- 23.Vijayaraghavan M, Hurst S, Pierce JP. A qualitative examination of smoke-free policies and electronic cigarettes among sheltered homeless adults. American Journal of Health Promotion. 2015;31(3):243–250. doi: 10.4278/ajhp.150318-QUAL-781. [DOI] [PubMed] [Google Scholar]
- 24.Vijayaraghavan M, Pierce JP. Interest in smoking cessation related to a smoke-free policy among homeless adults. Journal of Community Health. 2015;40(4):686–691. doi: 10.1007/s10900-014-9985-9. [DOI] [PubMed] [Google Scholar]
- 25.Businelle MS, Poonawalla IB, Kendzor DE, Rios DM, Cuate EL, Savoy EJ, … Reitzel LR. Smoking policy change at a homeless shelter: Attitudes and effects. Addictive Behaviors. 2014;40:51–56. doi: 10.1016/j.addbeh.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 26.Al-Delaimy WK. California Tobacco Survey (CTS) 2015 Retrieved from: http://library.ucsd.edu/dc/collection/bb9353145q.
- 27.StataCorp. Stata Statistical Software. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 28.Tsemberis S, Gulcur L, Nakae M. Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. American Journal of Public Health. 2004;94(4):651–656. doi: 10.2105/AJPH.94.4.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tsai J, Rosenheck RA. Smoking among chronically homeless adults: Prevalence and correlates. Psychiatric Services. 2012;63(6):569–576. doi: 10.1176/appi.ps.201100398. [DOI] [PubMed] [Google Scholar]
- 30.Henwood BF, Cabassa LJ, Craig CM, Padgett DK. Permanent supportive housing: Addressing homelessness and health disparities? American Journal of Public Health. 2013;103(S2):S188–S192. doi: 10.2105/AJPH.2013.301490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ku L, Bruen BK, Steinmetz E, Bysshe T. Medicaid tobacco cessation: Big gaps remain in efforts to get smokers to quit. Health Affairs. 2016;35(1):62–70. doi: 10.1377/hlthaff.2015.0756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vijayaraghavan M, Schroeder SA, Kushel M. The effectiveness of tobacco control policies on vulnerable populations in the USA: A review. Postgraduate Medical Journal. 2016:1–7. doi: 10.1136/postgradmedj-2014-133193. [DOI] [PubMed] [Google Scholar]
- 33.Hood NE, Ferketich AK, Klein EG, Wewers ME, Pirie P. Individual, social, and environmental factors associated with support for smoke-free housing policies among subsidized multiunit housing tenants. Nicotine & Tobacco Research. 2013;15(6):1075–1083. doi: 10.1093/ntr/nts246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.San Diego County Regional Taskforce on the Homeless. 2015 WEALLCOUNT Results. 2015 Retrieved from http://www.rtfhsd.org/wp-content/uploads/2017/07/2015-PITC-Results-Updated-7.2.15.pdf.