Abstract
The rectus abdominis muscle is innervated by intercostal nerves T7–T12, and most thoracotomies are performed through the fourth to sixth intercostal spaces, so direct nerve damage to the rectus abdominis seems unlikely. However, at least one trocar is inserted below the seventh intercostal space in most multi-port video-assisted thoracoscopic surgeries (VATSs), and injury of the seventh or lower intercostal nerve with related paralysis of the rectus abdominis is possible, albeit rare. Only two cases of rectus abdominis paralysis caused by after VATSs have been reported, and these cases were not permanent injuries. This is the first report of permanent paralysis of the rectus abdominis after VATSs.
Keywords: paralysis, rectus abdominis, after video-assisted thoracoscopic surgery
Introduction
Upper abdominal palsy after thoracic surgery is very rare.1,2) In particular, paralysis of the rectus abdominis after video-assisted thoracoscopic surgery (VATS) has been reported in only two cases worldwide.3,4) Paralysis of the rectus abdominis can theoretically occur in the thoracic surgery area, including VATS. We experienced permanent paralysis of the rectus abdominis after VATS segmentectomy and pleurectomy and reviewed the world literature to understand this complication.
Case Report
A 42-year-old man presented to the hospital with dyspnea and pleuritic pain lasting for 2 months. A chest computed tomography (CT) scan revealed a solitary pulmonary nodule on the right upper lobe with pleural effusion and symmetrical thickness on both sides of the rectus abdominis (Fig. 1a). We confirmed the adenocarcinoma through percutaneous needle biopsy at anterior chest wall the third intercostal space. Based on his preoperative brain magnetic resonance imaging (MRI) and positron emission tomography-CT, we suspected no metastatic region except the pleura, and the clinical stage was estimated at T1aN0Mla.
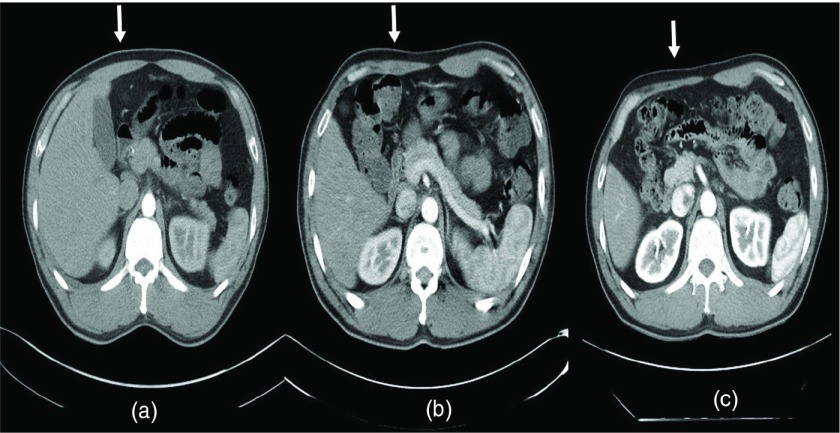
Fig. 1. (a) Preoperative abdominal CT scan revealed symmetry in the thickness of both sides of the rectus abdominis. (b) Abdominal CT on postoperative day 15 showed asymmetry in the thickness of both sides of the rectus abdominis. (c) Abdominal CT 2 years after the surgery showed progressive worsening of muscle atrophy. CT: computed tomography.
He underwent VATS for a right upper lobe anterior segmentectomy, total pleurectomy, and intrapleural hyperthermic chemotherapy. A 5-cm size working window was performed on the fifth intercostal space, and two 12-mm ports were inserted at the seventh and eighth intercostal spaces. The surgery was successful. The patient was extubated in the operating room, recovered uneventfully, and was transferred for chemotherapy 15 days after surgery. The right upper paratracheal lymph node and a pleural specimen were positive for metastatic adenocarcinoma. His pathologic stage was confirmed to be stage IV T3N2M1a.
The patient was numb from the right chest area to around the navel and complained of repeated clamping pain after surgery. A physical examination showed asymmetry of the upper abdomen and a T3–T9 level sensory abnormality. An abdominal CT scan performed 15 days after surgery to assess the right upper abdominal bulging and weakness showed asymmetrical thickness on both sides of the rectus abdominis (Fig. 1b).
The patient complained of persistent abdominal discomfort, nausea, dyspepsia, and abdominal pain. Endoscopic and thoracic spine MRI were performed to detect and treat the cause of that symptom. The T-spine MRI and endoscopic findings revealed no lesions. A routine abdominal CT to evaluate the status of the rectus abdominis over 2 years showed progressive worsening of the muscle atrophy (Fig. 1c). The diagnosis was permanent paralysis of the rectus abdominis muscle due to the thoracic operation. The patient continues to suffer from abdominal discomfort after the laparoscopic omentectomy due to carcinomatosis peritonei despite several cycles of chemotherapy.
Discussion
The rectus abdominis muscle is innervated by intercostal nerves T7–T12. Most thoracotomies are performed through the fourth to sixth intercostal spaces, so direct damage to these nerves seems unlikely. However, at least one trocar is inserted below the seventh intercostal space in most multi-port VATS, and injury to the seventh or lower intercostal nerve with related paralysis of the rectus abdominis is possible, albeit rare. Only two cases of rectus abdominis paralysis caused by VATS have been reported in the world.
An intercostal nerve injury in the thoracic surgery area is a frequent complication, and Roger et al.5) reported that this injury occurs in >50% of patients. Most intercostal nerve injuries caused by thoracic surgery are sensory abnormalities with pain, and recover within months, but some may cause permanent nerve damage. In general, neuronal damage in the thoracic surgery area is called neuropraxia, and most of the neuropathy recovers within a short time due to the temporary intercostal nerve crushing injury caused by the spreader. Benedetti et al.6) reported that most patients who lose superficial abdominal reflexes after a thoracotomy recover within a short period of time, and only 10% of the patients report persistent reflex loss for >2 months. If nerve continuity is maintained, the rate of neurological recovery is reported to be 1–3 mm/day, and rapid recovery is possible with transient nerve damage. Permanent damage to the intercostal nerve due to thoracotomy is possible in some cases. Axonotmesis, which involves loss of the relative continuity of the axon and its myelin covering but preservation of the connective tissue framework of the nerve, and appears as a severe form of crushing injury due to the use of a spreader, and neuropraxia, which is a complete nerve injury caused by cutting or thermal injury of the intercostal nerve, are possible. The type of nerve injury caused by VATS is called neuropraxia rather than axonotmesis.
We analyzed the seven reported cases, including our case (Table 1). Most of the motor nerve damage was neurotmesis. In four of the seven cases, motor function was recovered after a certain period of time. Two cases did not recover after more than a 1-year follow-up, and were considered a permanent nerve injury.2–4) Long-term follow-up was lost in one case. Total pleurectomy was performed additionally in two patients who did not recover neurologically. It is difficult to conclude that pleurectomy is a factor in permanent injury of the intercostal nerve. However, as the extent of the surgical procedure under the seventh intercostal space increases, the possibility of injury to the rectus abdominis increases.
Table 1. Various studies on paralysis of the rectus abdominis muscle after thoracic surgery.
| First author (citation and year) | Diagnosis | Age | Sex | Operation name | Procedure | Incision site | Additional procedure | Permanent nerve injury |
|---|---|---|---|---|---|---|---|---|
| Our study, 2015 | Lung cancer | M | 42 | Segmentectomy | VATS | 5th and 7th intercostal space | Total pleurectomy | Yes |
| Timmermans, 20132) | Chilaiditi syndrome | M | 54 | Plication of diaphragm | Thoracotomy | 8th intercostal space | None | No |
| Lung cancer | M | 54 | Lobectomy | Thoracotomy | 5th and 6th intercostal space | None | No | |
| Benign pleural thickening | M | 64 | Decortication | Thoracotomy | Just above the diaphragm | Total pleurectomy | Yes | |
| Patila, 20094) | Pneumothorax | M | 17 | Bullectomy | VATS | 5th and 7th intercostal space | Parietal pleurectomy | No |
| Pleural effusion | M | 51 | Decortication | Thoracotomy | 6th intercostal space | Parietal pleurectomy | No | |
| Antonescu, 20113) | Pneumothorax | M | 16 | Bullectomy | VATS | 4th, 5th, and 7th intercostal space | None | Long-term follow-up loss |
VATS: video-assisted thoracoscopic surgery
In conclusion, although a clinically apparent injury to the intercostal nerve associated with paralysis of the upper rectus abdominis is a rare complication of VATS, any surgical intervention performed below the seventh intercostal space can cause such injuries. Careful attention is necessary to prevent paralysis of the rectus abdominis when a thoracotomy or a trocar is inserted below the seventh intercostal space.
Disclosure Statement
No conflicts of interest.
References
- 1).Ho J, Richardson JK. Rectus abdominis denervation after subcostal open laparotomy. Am J Phys Med Rehabil 2015; 94: e43-4. [DOI] [PubMed] [Google Scholar]
- 2).Timmermans L, Klitsie PJ, Maat AP, et al. Abdominal wall bulging after thoracic surgery, an underdiagnosed wound complication. Hernia 2013; 17: 89-94. [DOI] [PubMed] [Google Scholar]
- 3).Antonescu I, Baird R. Paralysis of the rectus abdominis muscle after video-assisted thoracoscopic surgery for recurrent spontaneous pneumothorax. J Pediatr Surg 2011; 46: 2397-400. [DOI] [PubMed] [Google Scholar]
- 4).Pätilä T, Sihvo EI, Räsänen JV, et al. Paralysis of the upper rectus abdominis muscle after video-assisted or open thoracic surgery: an underdiagnosed complication? Ann Thorac Surg 2009; 88: 1335-7. [DOI] [PubMed] [Google Scholar]
- 5).Rogers ML, Henderson L, Mahajan RP, et al. Preliminary findings in the neurophysiological assessment of intercostal nerve injury during thoracotomy. Eur J Cardiothorac Surg 2002; 21: 298-301. [DOI] [PubMed] [Google Scholar]
- 6).Benedetti F, Vighetti S, Ricco C, et al. Neurophysiologic assessment of nerve impairment in posterolateral and muscle-sparing thoracotomy. J Thorac Cardiovasc Surg 1998; 115: 841-7. [DOI] [PubMed] [Google Scholar]