Abstract
Background
A split-dose (SD) regimen is crucial for colonoscopy quality. Compliance with SD for early morning colonoscopy is generally poor. The present study evaluated whether pre-colonoscopy counselling, in addition to a dedicated leaflet, might increase SD uptake.
Methods
Consecutive 50–69-year-old patients undergoing screening colonoscopy before 10 a.m. were randomized to either receive written information only on bowel preparation (Written Group, WG) or written and oral instructions (Written and Oral Group, WaOG). The leaflet strongly encouraged SD adoption. The primary endpoint was the number of patients adopting SD in each group. The secondary endpoints were predictors of SD uptake, compliance with preparation schemes and cleansing adequacy.
Results
A total of 286 patients (143 WG, 143 WaOG) were enrolled (mean age 59.6 ± 6.1 years, men 49.3%). SD was adopted by 114 and 125 patients in the WG and WaOG, respectively (79.7% versus 87.4%, p = 0.079). No significant differences were observed for the proportion of patients with full compliance with preparation scheme (97.9% versus 97.2%, p = 0.99) and of procedures with adequate bowel cleansing (95.6% versus 95.1%, p = 0.77). At multivariate analysis, a > 1 h travel time to the endoscopy service was inversely correlated with SD uptake (odds ratio (OR) 0.30, 95% confidence interval (CI) 0.09–0.98).
Conclusions
Our leaflet guaranteed satisfactory uptake of SD and excellent adherence to the preparation scheme for early morning colonoscopy. Its use might marginalize the need for additional oral instructions, particularly in open-access settings.
Keywords: Colonoscopy, split dose, colorectal cancer screening, bowel preparation, colonoscopy quality
Introduction
Colorectal cancer (CRC) is a major cause of morbidity and the second cause of cancer-related mortality in both Europe and the United States.1,2 Colonoscopy represents the most accurate test for the detection of colorectal neoplasia, but its accuracy is suboptimal. Missed lesions represent the dominant cause of post-colonoscopy CRCs,3 and a suboptimal adenoma detection rate (ADR) has been associated with a reduced efficacy of colonoscopy in preventing CRC incidence and mortality.4
Optimizing bowel preparation is critical to increase the effectiveness of colonoscopy. The adoption of a split-dose (SD) bowel cleansing regimen (the administration of the first half of the preparation the evening before colonoscopy and the second half in the morning of the procedure) has shown superior efficacy in bowel cleansing over traditional regimen of administering the whole preparation the day before (DB) the procedure,5 and it has been associated with a 30% higher detection rate of neoplasia in the setting of screening programmes.6 Its adoption is strongly recommended by practice guidelines for elective colonoscopies.7–9 Patient education is crucial for optimizing preparation results, and guidelines recommend that health care professionals should provide both oral and written instructions to patients for colonoscopy preparation.7–9
In large open-access systems, endoscopic procedures are prescribed by referring physicians without any previous clinic consultation and are scheduled by secretary staff.10 Therefore, the routine adoption of oral instructions in addition to written ones is unfeasible. It has been shown that the uptake of SD for early morning (before 10.00 a.m.) colonoscopies is unacceptably low (33%).11 The fear of incontinence on the way to the endoscopy service and the refusal to wake up in the very early morning to complete the bowel preparation represent the main barriers against SD.11 The risk of travel interruptions and/or faecal incontinence is very low, and only marginally increased with SD.11 Surveys have demonstrated that most patients tend to be receptive to SD regardless of appointment time, once they are given explanations of the importance of sticking to the instructions.12 Thus, patient education seems to be crucial to overcome barriers against SD and to improve patient compliance.
The present investigator-blinded prospective randomized controlled study was aimed at assessing whether pre-colonoscopy counselling – in addition to a dedicated and self-explanatory ad hoc designed leaflet – might increase SD uptake by patients scheduled for colonoscopy before 10 a.m.
Materials and methods
This investigator-blinded, randomized controlled study was conducted in one open-access endoscopy centre in Italy. The protocol was approved by the Ethical Review Board on 22 April 2015 and it was registered in the ClinicalTrials.gov registry [ClinicalTrials.gov identifier: NCT02638558]. Written and informed consent was obtained from all patients enrolled. The study protocol conforms to the ethical guidelines of the Declaration of Helsinki.
This was a no-profit study and the investigators had no relationship with the manufacturers of the bowel cleansing agent used; no funding for the study was solicited or accepted. All the authors provided critical revision and final approval of the article.
Study population
The target population included 50–69-year-old patients undergoing outpatient colonoscopy from January to June 2016 following a positive faecal immunochemical test (FIT) in the context of a CRC screening programme. We excluded from the study: (i) patients not eligible for invitation in the screening programme (colonoscopy already performed in the previous 5 years, personal history of CRC, colonic adenomas, inflammatory bowel disease, severe comorbidity); (ii) inpatients; (iii) patients with previous colonic resection; (iv) patients on antithrombotic therapy, precluding polyp resection; (v) patients who were not able or refused to give informed written consent.
All enrolled patients were scheduled for colonoscopy before 10.00 a.m.
Pre-colonoscopy bowel preparation instructions
We designed a dedicated educational leaflet on bowel preparation (see supplementary material), in which instructions were detailed in a simplified script with pictures and subtitles. The leaflet emphasized the importance of an adequate bowel preparation and of adhering to SD regimen to optimize colon cleansing, reporting that SD: (i) improves patient tolerability, (ii) minimizes the risk of missing neoplastic lesions and of repeating the procedure at shorter intervals, and (iii) favours a good prevention of cancer. It was also reported that the risk of bowel movements or incontinence during travel was minimal (<5%) despite the intake of the second part of cleansing solution on the same day of the procedure, and that this risk was not significantly higher compared with DB preparations.11 The leaflet also detailed the timing of bowel cleansing solution intake and dietary restrictions. Bowel preparations administered were: low volume (2 l) hypertonic polyethylene glycol (PEG) plus ascorbate solution (PEG-A, MOVIPREP®, Norgine, Harefield, UK) or 2 l PEG with citrate and simethicone plus bisacodyl (PEG-CS, LOVOL-Dyl LOVOL-Esse, Alfa Wassermann S.p.A., Alanno PE, Italy). The adoption of the SD regimen (1 l of PEG solution in the evening before colonoscopy at about 08:00 p.m. and the second one on the day of the procedure about 4 h before the scheduled procedure time) was strongly advised. The DB regimen (intake of the entire solution the evening before colonoscopy, the first litre between 06:00 and 07:00 p.m. and the second one between 09:00 and 10:00 p.m.) was also reported, albeit discouraged due to the higher risk of inadequate colon cleansing.
Participants were instructed to adhere to a low-residue diet for 3 days before the colonoscopy. They were allowed to have a standard breakfast and a light lunch on the day before the procedure, but no solid food was permitted after that. Clear liquids were permitted until 2 hours before the procedure.
Intervention
At the time of colonoscopy scheduling, patients who provided consent and met all eligibility criteria were randomized 1:1 by a computer-generated sequence either to receive only written instructions on bowel preparation, in accordance with our standard routine (Written Group, WG), or both written and oral instructions (Written and Oral Group, WaOG). WG subjects simply received the pre-colonoscopy educational leaflet, delivered by the secretary staff with the appointment instructions. WaOG patients received the educational leaflet and had a brief counselling session with a medical staff member to discuss the importance and rationale of bowel preparation – reinforcing the benefits of SD – and to fix the optimal times for the laxative intake. Allocation was performed via sealed and numbered envelopes by the secretary staff.
Data collection and colonoscopy procedure
Before colonoscopy, all patients received a multiple-choice questionnaire. The form included questions evaluating the characteristics of patients (seven items: age, sex, education, working and civil status, previous colonoscopy, travel time to get to the endoscopy centre), and the bowel preparation process (eight items: type of cleansing agent, timing of bowel preparation intake, main reason for the choice of SD versus DB regimen, compliance with preparation instructions, adverse events, sleep disturbances, need to stop and/or faecal incontinence while travelling to the endoscopy centre). Patient compliance was rated as optimal (intake of the whole preparation), fair (intake ≥75% of the preparation), and poor (intake <75% of the preparation). Colonoscopies were performed between 8:00 and 10:00 a.m. by five board-certified endoscopists with credentials for participating in the CRC screening programme who were blinded to which group patients were assigned.
At the end of the procedure, the endoscopist filled in a procedure assessment form reporting procedural data and the quality of bowel preparation, according to the Boston Bowel Preparation Scale (BBPS). BBPS is a 4-point scoring system applied to each of three segments of the colon: right side, transverse, and left side colon. Points (segment score) were assigned as follows: unprepared colon segment, 0; major residual stool or opaque liquid, 1; minor residual staining, 2; and entire mucosa easily visible, 3. The maximum BBPS score for a perfectly clean colon is 9, and the minimum BBPS score for an unprepared colon is 0. The scores of each segment were assigned by the colonoscopist after removing excess colonic content by suction and washing the mucosa.13 Adequate colon cleansing was defined as a BBPS ≥ 2 in each colon segment.
Outcome measures
The primary aim of the study was to assess the proportion of patients choosing SD for bowel preparation in each group. Secondary endpoints were to evaluate (i) the predictors of SD uptake, (ii) patient compliance to bowel preparation schemes, (iii) the quality of bowel preparation, and (iv) adverse events associated with the SD and DB regimens.
Statistical analysis
The expected uptake of SD in patients undergoing early morning colonoscopy was 33%, based on previous data.11 We considered an absolute 50% relative increase in SD uptake, resulting in an expected overall uptake of 50% as clinically relevant. With a two-sided significance level of 0.05 and a power of 0.80, 286 patients (143 per group) had to be included. Considering an expected 5% drop-out rate, we planned to enrol 300 patients; study enrolment was stopped after achieving the target sample in each arm. Patients who were randomized but did not attend their colonoscopy appointment were not included in the primary analysis.
Categorical variables were summarized using frequencies and percentages, while quantitative variables were summarized using means and standard deviations. A Chi-square test and Chi-square test for trends were used to compare categorical variables, as appropriate, whereas a Student’s t-test was used for continuous variables. All statistical tests were two-sided and were considered statistically significant at p < 0.05. A logistic stepwise regression model was used to assess the independent predictors of SD acceptance; all parameters with a p-value <0.2 on univariate analysis were included and those with a p-value >0.4 were removed, according to an automated stepwise procedure. For all comparisons, the odds ratio (OR) and 95% confidence interval (CI) were given for significant variables.
Analyses were carried out with the SAS statistical software package V.9.1 (SAS Institute, Cary, NC, USA). The results were reported according to CONsolidated Standards Of Reporting Trials (CONSORT) guidelines.14
Results
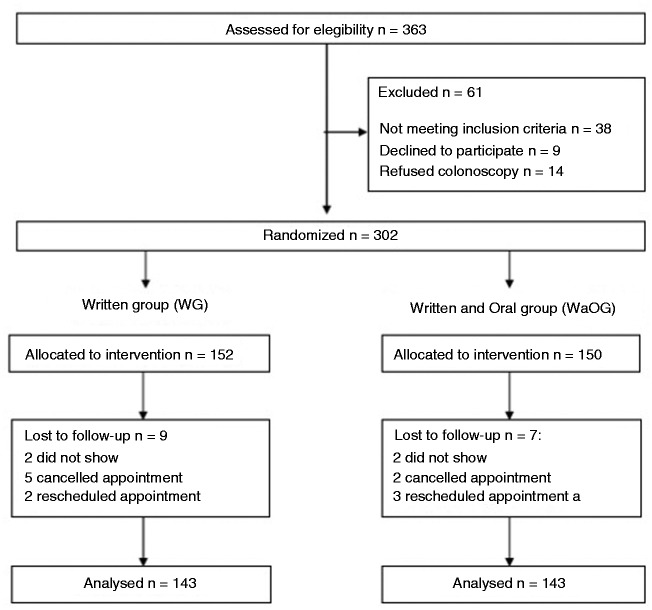
In the study period, a total of 363 FIT-positive patients were evaluated; 302 were considered eligible and were allocated 1:1 to WG or WaOG; 16 patients dropped out after randomization (4 did not show up at colonoscopy appointment, 7 cancelled and 5 rescheduled the appointment). A total of 286 patients (mean age 59. 6 ± 6.1 years, men 49.3%), were finally included in the analysis (Figure 1).
Figure 1.
Flow diagram of patients.
WG: Written Group; WaOG: Written and Oral Group.
The two groups, each including 143 patients, were well balanced in terms of demographics, education, employment and marriage status. The number of patients who underwent colonoscopy for the first time, the timing of colonoscopy appointment and the travel distance to the hospital were also comparable between the two groups (Table 1).
Table 1.
Baseline demographic and clinical variables.
| Written Group (n = 143) | Written and Oral Group (n = 143) | p-value | |||
|---|---|---|---|---|---|
| Age, years, mean (SD) | 59.1 | (6.1) | 56.1 | (6.2) | 0.15° |
| Male, n (%) | 77 | (53.8) | 64 | (44.8) | 0.15* |
| Education, n (%) | |||||
| high school/ degree | 62 | (43.4) | 72 | (50.3) | 0.29* |
| less than high school | 81 | (56.6) | 71 | (49.7) | |
| Marital status, n (%) | |||||
| married | 116 | (81.1) | 119 | (83.2) | 0.75^ |
| divorced | 9 | (6.3) | 6 | (4.2) | |
| widowed | 3 | (2.1) | 5 | (3.5) | |
| single | 15 | (10.5) | 13 | (9.1) | |
| Work activity, n (%) | |||||
| full time | 61 | (42.7) | 57 | (39.8) | 0.77^ |
| part time | 3 | (2.1) | 6 | (4.1) | |
| unemployed/retired | 58 | (40.6) | 60 | (42.1) | |
| housekeeper | 21 | (14.6) | 20 | (14.0) | |
| First colonoscopy, n (%) | 121 | (84.6) | 110 | (76.9) | 0.13* |
| Colonoscopy scheduling time, n (%) | |||||
| from 8.00 to 9.00 a.m. | 77 | (53.8) | 84 | (58.7) | 0.47* |
| from 9.00 to 10.00 a.m. | 66 | (46.2) | 59 | (41.3) | |
| Travel time to hospital, n (%) | |||||
| <30 min | 72 | (50.3) | 76 | (53.1) | 0.47^ |
| from 30 to 60 min | 63 | (44.1) | 62 | (43.4) | |
| >60 min | 8 | (5.6) | 5 | (3.5) | |
Chi-square test
°Student’s t-test
^Chi-square test for trends
SD: standard deviation
In the study cohort, 114 patients in WG and 125 WaOG chose SD over DB regimen (79.7% versus 87.4%, p = 0.079). When comparing patients who chose SD versus DB regimen, no variable was significantly associated with SD uptake at univariate analysis (Table 2). Logistic regression analysis showed that travel time >1 h was the only variable (inversely) correlated with SD uptake (OR 0.30, 95% CI 0.09–0.98).
Table 2.
Demographic and clinical variables of patients choosing split-dose regimen and evening- before regimen.
| Split-Dosing Group (n = 239) | Evening-Before Group (n = 47) | p-value | |||
|---|---|---|---|---|---|
| Age, years, mean (SD) | 59.7 | (6.2) | 59.2 | (5.9) | 0.64° |
| Male, n (%) | 114 | (47.7) | 27 | (57.4) | 0.29* |
| Education, n (%) | |||||
| high school/ degree | 114 | (47.7) | 20 | (42.6) | 0.63* |
| less than high school | 125 | (52.3) | 27 | (57.4) | |
| Marital status, n (%) | |||||
| married | 198 | (82.8) | 37 | (78.7) | 0.85^ |
| divorced | 11 | (4.6) | 4 | (8.5) | |
| widowed | 6 | (2.5) | 2 | (4.3) | |
| single | 24 | (10.1) | 4 | (8.5) | |
| Work activity, n (%) | |||||
| full time | 99 | (41.4) | 19 | (40.4) | 0.62^ |
| part time | 9 | (3.8) | 0 | (0) | |
| unemployed/retired | 98 | (41.0) | 20 | (42.6) | |
| housekeeper | 33 | (13.8) | 8 | (17.0) | |
| First colonoscopy, n (%) | 45 | (18.8) | 10 | (21.3) | 0.85* |
| Colonoscopy scheduling time, n (%) | |||||
| from 8.00 to 9.00 a.m. | 131 | (54.8) | 30 | (63.8) | 0.33* |
| from 9.00 to 10.00 a.m. | 108 | (45.2) | 17 | (36.2) | |
| Travel time to hospital, n (%) | ( | ||||
| <30 min | 127 | (53.1) | 21 | 44.7) | 0.09^ |
| from 30 to 60 min | 104 | (43.5) | 21 | (44.7) | |
| >60 min | 8 | (3.4) | 5 | (10.6) | |
Chi-square test
°Student’s t-test
^Chi-square test for trends
SD: standard deviation
Full compliance (100% intake of the solution) was reported by 140 (97.9%) and 139 (97.2%) patients in WG and WaOG, respectively (p = 0.99).
No statistically significant difference was found between WG and WaOG as procedural data were concerned, including mean BBPS scores (7.8 ± 1.4 versus 8.1 ± 1.2, p = 0.06), procedures with adequate bowel cleansing (95.6% and 95.1%, p = 0.77), caecal intubation rate (99.3% versus 97.9%, p = 0.61), polyp detection rate (55.2% versus 53.8%, p = 0.91), and ADR (39.8% versus 36.1%, p = 0.54).
Procedural data and adverse events in split versus day-before regimen
When considering the quality of cleansing in patients who chose SD (n = 239) and in those who chose DB dose (n = 47), mean scores were significantly higher in the SD group (8.1 ± 1.2 versus 7.4 ± 1.3, p < 0.001), although the percentage of procedures with adequate bowel cleansing was similar (95.8% versus 95.7%, p = 0.70). At least one stop during travel occurred in 18 patients who chose SD and in 4 patients who chose the DB regimen (7.5% versus 8.7%, p = 0.94); 6 patients in the SD group and none in DB group experienced faecal incontinence (2.5% versus 0%, p = 0.59).
Discussion
This randomized controlled trial showed that, in a screening setting, the adoption of a simple self-explanatory leaflet – clearly emphasizing the benefits of SD – guaranteed high patient compliance with the SD regimen, even for early morning colonoscopies, marginalizing the need for additional oral educational instructions.
The results of our study are relevant for several reasons. First, they showed that the simple adoption of a dedicated educational leaflet instead of standard forms on bowel preparation might lead to an acceptable uptake rate of SD (about 80%). When considering the low compliance with SD for early morning colonoscopies11 and the association between SD and ADR,4,6 this intervention seems to be critical to optimize the effectiveness of colonoscopy on CRC prevention.
Second, the delivery of verbal instructions in addition to written ones did not offer significant advantages over written instructions only, in terms of SD uptake, patient adherence to the bowel preparation scheme, and quality of bowel cleansing. The leaflet used in this study was so effective in making patients aware of the benefits of SD and in empowering them to manage their own preparation, that a brief counselling session was of marginal importance. Several interventions to improve participation and compliance with bowel preparation have been previously evaluated, such as cartoon visual educational instruction,15,16 booklets,17 videos18 and telephone calls.19,20 However, these studies provided inconsistent results.
Practice guidelines strongly recommend that oral and written information about bowel preparation should be delivered together by healthcare professionals to increase patients’ compliance and improve preparation results.7–9 However, these guidelines are based on low-to-moderate quality evidence, mainly from a single observational study, which demonstrated that the use of both verbal and written instructions, compared with written instructions only, is an independent predictor of adequate bowel preparation quality.21 Data from interventional studies on the additional role of oral instructions are scant. One recent non-randomized study, including 105 outpatients undergoing screening colonoscopy, demonstrated that physician-delivered education consisting of a 10-minute counselling session, in addition to written instructions, significantly improved the quality of bowel preparation.22 To the best of our knowledge, the present study is the first randomized trial specifically evaluating the impact of oral instructions on bowel preparation outcomes, showing that physician-delivered oral instructions failed to improve the quality of bowel cleansing when a dedicated leaflet encouraging the adoption of SD was used. We acknowledge that this apparent failure is mainly related to the unexpected very high adherence to SD in the control arm, rather than the lack of efficacy of the proposed intervention. This high adherence to SD partly reflects the effectiveness of the new educational leaflet adopted in the study, but it might also be overestimated due to the study setting. FIT-positive screening patients are a selected colonoscopy population, in which the adherence to any recommendation aimed at improving the quality of colonoscopy is likely higher, due to the fear of cancer.
Third, at multivariate analysis we found that only patients who had to travel >1 hour to get to the endoscopy service remained reluctant to comply with the SD regimen, probably due to the fear of travel interruption and faecal incontinence and the need to wake up during the night to complete bowel preparation. For this subset of patients, the shifting of colonoscopy appointment in the second part of the morning (or in the afternoon) appears a viable alternative, and is easier to implement than any other intervention aimed at convincing them to comply with SD.
The strength of the study is the choice of an objective primary endpoint (SD uptake) – instead of the quality of bowel cleansing – to marginalize any subjectivity in outcome assessment.
The high patient compliance with SD and bowel preparation instructions in both study groups accounted for the very high percentage of procedures with adequate bowel cleansing observed in this study, which is consistent with the highest levels of bowel cleansing reported in the FIT-based CRC screening setting.23,24
When comparing SD and DB regimens, higher colon cleansing scores were observed in patients adopting SD; however, no difference between the two regimens was found as to the proportion of procedures with adequate colon cleansing. As only 16% of study population adopted the DB regimen, the study was largely underpowered for the purpose to detect any difference in preparation quality between the two groups. Although a lower benefit of SD over the DB regimen might be assumed for early morning procedures, due to the relatively shorter runway time, this should not discourage the adoption of SD for early morning procedures, as it is well known that the highest levels of preparation quality are associated with the highest adenoma detections.25
We did not observe significant difference between the SD and DB regimens in terms of adverse events, including the need to stop on the way to the hospital because of bowel movements and/or faecal incontinence. These findings confirmed that SD is overall well tolerated by patients even for early morning procedures.
We acknowledge some limitations to the present study. First, we demonstrated that a dedicated leaflet may overcome the need for oral instructions for bowel preparation in subjects participating to the CRC screening programme. The reproducibility of these results out of the screening setting, where patients could be less alerted on the importance of high quality colonoscopy, need to be tested in further studies. In settings where the adherence to SD is expected to be lower, an intensive intervention including oral information, as recommended by practice guidelines, may still be effective.
Second, the study was carried out in a single institution; a multicentre study is needed to verify if these results can be generalized. Third, the overall efficacy of a dedicated leaflet for bowel preparation should be also tested for late morning and afternoon colonoscopy patients; the uptake of SD is more critical for early morning procedures, but the benefits of the leaflet might be extended to all colonoscopy patients.
Conclusion
In conclusion, the present trial showed that in a screening setting the systematic adoption of a self-explanatory leaflet favouring SD bowel preparation guaranteed a high patient uptake and an excellent level of bowel cleansing, thus marginalizing the need for additional oral education for early morning colonoscopies. This could represent a cost effective and simple intervention to improve the quality of colonoscopy.
Supplementary Material
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of conflicting interests
The authors declare no conflicts of interest in preparing this article.
Informed consent
Written and informed consent was obtained from all patients enrolled.
Ethics approval
The protocol was approved by the Ethical Review Board on 22 April 2015.
References
- 1.Edwards BK, Ward E, Kohler BA, et al. Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 2010; 116: 544–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferlay J, Parkin DM, Steliarova-Focher E. Estimates of the cancer incidence and mortality in Europe in 2008. Eur J Cancer 2010; 46: 765–781. [DOI] [PubMed] [Google Scholar]
- 3.Pohl H, Robertson DJ. Colorectal cancers detected after colonoscopy frequently result from missed lesions. Clin Gastroenterol Hepatol 2010; 8: 858–864. [DOI] [PubMed] [Google Scholar]
- 4.Corley DA, Jensen CD, Marks AR, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 2014; 370: 1298–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martel M, Barkun AN, Menard C, et al. Split-dose preparations are superior to day-before bowel cleansing regimens: A meta-analysis. Gastroenterology 2015; 149: 79–88. [DOI] [PubMed] [Google Scholar]
- 6.Radaelli F, Paggi S, Hassan C, et al. Split-dose preparation for colonoscopy increases adenoma detection rate: A randomised controlled trial in an organised screening programme. Gut 2017; 66: 270–277. [DOI] [PubMed] [Google Scholar]
- 7.Hassan C, Bretthauer M, Kaminski MF, et al. Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2013; 45: 142–150. [DOI] [PubMed] [Google Scholar]
- 8.Johnson DA, Barkun AN, Cohen LB, et al. Optimizing adequacy of bowel cleansing for colonoscopy: Recommendations from the US multi-society task force on colorectal cancer. Gastrointest Endosc 2014; 80: 543–562. [DOI] [PubMed] [Google Scholar]
- 9.Saltzman JR, Cash BD, Pasha SF, et al. Bowel preparation before colonoscopy. ASGE Standards of Practice Committee. Gastrointest Endosc 2015; 81: 781–794. [DOI] [PubMed] [Google Scholar]
- 10.Chandrasekhara V, Eloubeidi MA, Bruining DH, et al. ASGE Standards of Practice Committee. Open access endoscopy. Gastrointest Endosc 2015; 81: 1326–1329. [DOI] [PubMed] [Google Scholar]
- 11.Radaelli F, Paggi S, Repici A, et al. Barriers against split-dose bowel preparation for colonoscopy. Gut. Epub ahead of print 19 April 2016; DOI: 10.1136/gutjnl-2015-311049. [DOI] [PubMed]
- 12.Unger RZ, Amstutz SP, Seo DH, et al. Willingness to undergo split-dose bowel preparation for colonoscopy and compliance with split-dose instructions. Dig Dis Sci 2010; 55: 2030–2034. [DOI] [PubMed] [Google Scholar]
- 13.Calderwood AH, Jacobson BC. Comprehensive validation of the Boston Bowel Preparation Scale. Gastrointest Endosc 2010; 72: 686–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boutron I, Moher D, Altman DG, et al. Extending the consort statement to randomized trials of nonpharmacologic treatment: Explanation and elaboration. Ann Int Med 2008; 148: 295–309. [DOI] [PubMed] [Google Scholar]
- 15.Calderwood AH, Lai EJ, Fix OK, et al. An endoscopist-blinded, randomized, controlled trial of a simple visual aid to improve bowel preparation for screening colonoscopy. Gastrointest Endosc 2011; 73: 307–314. [DOI] [PubMed] [Google Scholar]
- 16.Tae JW, Lee JC, Hong SJ, et al. Impact of patient education with cartoon visual aids on the quality of bowel preparation for colonoscopy. Gastrointest Endosc 2012; 76: 804–811. [DOI] [PubMed] [Google Scholar]
- 17.Spiegel BM, Talley J, Shekelle P, et al. Development and validation of a novel patient educational booklet to enhance colonoscopy preparation. Am J Gastroenterol 2011; 106: 875–883. [DOI] [PubMed] [Google Scholar]
- 18.Park JS, Kim MS, Kim H, et al. A randomized controlled trial of an educational video to improve quality of bowel preparation for colonoscopy. BMC Gastroenterol 2016; 16: 64–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu X, Luo H, Zhang L, et al. Telephone-based re-education on the day before colonoscopy improves the quality of bowel preparation and the polyp detection rate: a prospective, colonoscopist-blinded, randomised, controlled study. Gut 2014; 63: 125–130. [DOI] [PubMed] [Google Scholar]
- 20.Park J, Kim TO, Lee NY, et al. The effectiveness of short message service to assure the preparation-to-colonoscopy interval before bowel preparation for colonoscopy. Gastroenterol Res Pract 2015; 2015: 628049–628049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hassan C, Fuccio L, Bruno M, et al. A predictive model identifies patients most likely to have inadequate bowel preparation for colonoscopy. Clin Gastroenterol Hepatol 2012; 10: 501–506. [DOI] [PubMed] [Google Scholar]
- 22.Shieh TY, Chen MJ, Chang CW, et al. Effect of physician-delivered patient education on the quality of bowel preparation for screening colonoscopy. Gastroenterol Res Pract 2013; 2013: 570180–570180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zorzi M, Valiante F, Germanà B, et al. Comparison between different colon cleansing products for screening colonoscopy. A non-inferiority trial in population-based screening programs in Italy. Endoscopy 2016; 48: 223–231. [DOI] [PubMed] [Google Scholar]
- 24.Zorzi M, Senore C, Da Re F, et al. Quality of colonoscopy in an organised colorectal cancer screening programme with immunochemical faecal occult blood test: the EQuIPE study (Evaluating Quality Indicators of the Performance of Endoscopy). Gut 2015; 64: 1389–1396. [DOI] [PubMed] [Google Scholar]
- 25.Clark BT, Protiva P, Nagar A, et al. Quantification of adequate bowel preparation for screening or surveillance colonoscopy in men. Gastroenterology 2016; 150: 396–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.