Abstract
Objective
Compare the accuracy of the Eustachian Tube Dysfunction Questionnaire-7 (ETDQ-7) in identifying people with Eustachian tube (ET) dysfunction based on symptoms and based on an objective ET function test.
Study Design
Cross-sectional study.
Setting
Tertiary referral center.
Subjects and Methods
55 subjects with and without symptoms suggestive of ET dysfunction completed the ETDQ-7 questionnaire and had their ET function evaluated by the percentage of middle ear pressure equilibrated after 5 swallows (PEq5) either during a Pressure Chamber test (intact tympanic membranes) or by the Inflation-Deflation test (non-intact tympanic membranes). The ETDQ-7 score ≥ 14.5 and PEq5<60% were used to define ET dysfunction and sensitivity, specificity and Receiver Operating Characteristic curves were used to assess the level of association between ETDQ-7 scores and PEq5.
Results
25 asymptomatic (Group 1= 15 females, 15 whites, mean age 32±12.8 years) and 30 subjects with ET dysfunction symptoms (Group 2= 17 females, 25 whites, mean age 27±16.3 years) were included in the analysis. ETDQ-7 sensitivity and specificity regarding correct group assignment were 70% and 100% and with respect to predicting PEq5<60%, 54% and 78% respectively. An area under the curve (AUC) of 0.68 (95% CI 0.53–0.83) at the participant level and of 0.64 (95% CI 0.50–0.77) at ear level indicated a moderate level of association which was lower, although not statistically significant, for non-intact tympanic membranes (AUC=0.63 at participant and AUC=0.49 at ear level).
Conclusion
The ETDQ-7 score had higher correlation with ET dysfunction symptoms than with an objective measure of ET function.
Keywords: ETDQ-7, Eustachian tube, otitis media, Pressure Chamber test, Inflation-Deflation test, Percentage pressure equilibrated
INTRODUCTION
The preservation of middle ear (ME) health and normal hearing requires that ME pressure be maintained at near-ambient levels, which is achieved by transient, muscle-assisted dilations of the Eustachian tube (ET) lumen. Although ET dysfunction (ETD) is mainly regarded as the inefficiency to properly open to equalize pressure between the ME and the nasopharynx, it also comprises ears with a continuously open, patulous, ET.1 Various methods are described to assess ET function including sonotubometry2–4, Forced Response test5, 9-Step1, tubomanometry6,7, nasopharyngeal maneuvers5,8, video-endoscopy9,10, Pressure chamber (PC) test11–14 and the Inflation-Deflation test (IDT).5 Two of these tests can create consistent and reproducible ME-nasopharyngeal under- and over-pressure gradients: the PC test, used for intact tympanic membranes, and the IDT, used for non-intact tympanic membranes.5,8,15 At the standard under or over pressure condition, a maneuver that results in ET opening such as swallowing is performed to attempt equilibrating the pressure differential. The percentage of pressure equilibrated (PEq) after each swallow can then be used to quantify ET function.5,13–15 The advantages of PEq are that it can be used for intact and non-intact tympanic membranes, can be expressed as a continuous-interval measure and assesses the most important functional aspect of the ET – its efficiency for ME pressure regulation.
Yet, the use of ET function tests is limited by the need for high cost equipment and trained personnel which are mostly available in specialized centers. Therefore, a simple tool such as a questionnaire that could reliably identify people with ETD would be a valuable instrument for in office use. About 5 years ago, the Eustachian Tube Dysfunction Questionnaire-7 (ETDQ-7) was introduced as a new score system for quantitative assessment of ETD-related symptoms, with a possible score ranging from a minimum of 7 to a maximum of 49 points (Table 1). Receiver Operating Characteristic (ROC) curve analysis of the ETDQ-7 identified a cut point total score of ≥14.5 (mean score of ≥2.1) with perfect, 100% sensitivity and 100% specificity for categorizing a patient as having ETD. To avoid recall bias, the ETDQ-7 only includes the symptoms that were present in the past month.16
Table 1.
ETDQ-7 questions related to Eustachian tube dysfunction symptoms present in the past month and the scoring system from 1 to 7. Minimum score=7. Maximum score=49.
| Over the past 1 month, how much has each of the following been a problem for you? | No problem | Moderate Problem | Severe Problem | ||||
|---|---|---|---|---|---|---|---|
| 1. Pressure in the ears? | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 2. Pain in the ears? | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 3. A feeling that your ears are clogged or “under water”? | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 4. Ear symptoms when you have a cold or sinusitis? | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 5. Crackling or popping sounds in the ears? | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 6. Ringing in the ears? | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 7. A feeling that your hearing is muffled? | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
From McCoul ED, Anand VK, Christos PJ. Validating the clinical assessment of eustachian tube dysfunction: The Eustachian Tube Dysfunction Questionnaire (ETDQ-7). Laryngoscope 2012 122(5):1137–41.
Reproduced with permission of John Wiley & Sons Inc.
The ETDQ-7 has been translated into German17 and Dutch18, used for clinical evaluation of ETD18–20 and as an objective measure of surgical procedure outcomes such as the balloon dilation of the ET.20–22 Due to the increasing interest in a reliable score system that could help identify people with ETD, we designed a study to evaluate the accuracy of the ETDQ-7 for categorizing people with and without ETD based on symptoms and based on an objective measure of the ET function, the PEq.
METHODS
This cross-sectional study was approved by the Institutional Review Board at the University of Pittsburgh and written informed consent was obtained from all participants.
Study Population
Seventy-six generally healthy subjects participating in studies at the Middle Ear Physiology Laboratory and patients evaluated at the Eustachian Tube Dysfunction clinic had a detailed medical, ears, nose and throat history followed by otolaryngology examination, pneumatic otoscopy and tympanometry measurements (Titan, Interacoustics USA, Eden Prairie, MN, USA; sound frequency = 226 Hz).
Subjects were classified as Controls (Group 1) if they had no history of ear disease or symptoms related to ETD, had normal otoscopy and pneumatic otoscopy and type A tympanograms. Controls could have a unilateral tympanostomy tube inserted by us if they were participating in studies at the Middle Ear Physiology Laboratory that required a non-intact tympanic membrane to perform ET function tests. The symptomatic Group (Group 2) consisted of people (1) with a history of chronic or recurrent otitis media or ME effusion, with or without the need for tympanostomy tubes and with or without a residual tympanic membrane perforation; or (2) with symptoms suggestive of ETD such as persistent ear pressure, popping and crackling sounds, or fullness/otalgia due to rapid barometric changes that are not alleviated by swallowing, yawning or Valsalva maneuver. Each group was further stratified in subgroup A, if the tympanic membrane was non-intact either due to the presence of a tympanostomy tube or perforation and subgroup B, if the tympanic membrane was intact.
If signs of acute upper respiratory infection or nasal allergy, acute otitis media, ME fluid, otorrhea, type B tympanogram were present on the testing day, the subjects were dismissed and the testing session postponed until after the acute problem resolved. Subjects were excluded if they had a history of cleft palate, suspicion of submucous cleft, cranio-facial malformation, history of ossicular chain reconstruction or inability to perform the tests.
ETDQ-7 questionnaire
All participants were instructed to answer the ETDQ-7 questionnaire based on their symptoms present in the previous month (Table 1).16 Whenever necessary, children had the help of their caregivers to explain and answer the questionnaire. A total score < 14.5 or a mean score of < 2.1 was considered normal.
Eustachian tube function tests
The test chosen to drive over- and under- ME pressures relative to ambient and evaluate ET function depended on the tympanic membrane status: a pressure chamber was used for intact tympanic membranes and the IDT for tympanic membranes with a perforation or tympanostomy tube.
1. Pressure chamber test
The pressure chamber used was a HyperTec hyperbaric chamber (HyperTec 5100; Olney, TX, USA) modified during construction for hypo/hyperbaric applications. The subject entered the pressure chamber with a technician, who performed tympanometry measurements at specific time points. Another staff member located outside controlled the chamber pressures and recorded the tympanometry readings. During the test, subjects performed commanded swallows with 1ml aliquots of water from a 5ml plastic syringe. The protocol for all experiments consisted of: (1) baseline tympanometry at ambient pressure and repeated tympanometry after 1 and after 5 swallows; (2) then chamber pressure was increased at a rate of approximately 10 daPa/s to achieve a target ME pressure between −90 to −250 daPa (pressure chamber around +250 daPa and adjusted as necessary); (3) tympanometry before and after 1 and 5 swallows; (4) chamber pressure was returned to ambient; (5) tympanometry before and after 1 and 5 swallows - end of the test.
2. Inflation-Deflation test
The IDT instrument was developed by us and consists of an ear-canal probe coupled serially via tubing to an SDX01D4 differential pressure transducer (Honeywell), via a 3-way valve to a flow sensor (Respiratory Flowhead 1L MLT1l; AD Instruments), and via a second 3-way valve to a syringe. The transducer signals were routed via a PowerLab 4/35 data acquisition system (PL3504) to a personal computer running LabChart software, version 7.3.6 (AD Instruments), for real-time display of ear pressures and data storage.5 The ear probe was sealed into the test ear and ME pressure zeroed to ambient. ME pressure was then increased to 150 daPa above ambient and the valve was closed to reduce the system volume. The subject was asked to swallow 5 times at about 4-second intervals while the residual ME pressure values were concurrently recorded. Then, ME pressure was zeroed to ambient and the procedure was repeated at a ME pressure of −150 daPa. After 5 swallows, the ME pressure was zeroed and ear probes removed.
For this study, only the subject’s ability to equalize relative negative ME pressure was used in the analysis because it mimics the normal pathophysiology of ETD and ME disease.15 That condition corresponds to the deflation part of the IDT and the +250 daPa segment in the PC test. Only tests in which both left and right ME pressures reached a minimum of −90 daPa were considered evaluable and included in the analysis. The parameter for analysis was the percentage of ME under-pressure equilibrated after 5 swallows (PEq5) i.e., after 5 attempts to open the ET.13–15 PEq5 was calculated as the difference in ME gauged pressures pre and post 5 swallows divided by the pre-swallow ME pressure times 100.11,14 The PEq5 could not be calculated and tests were excluded from the analysis if the paired tympanograms for a test sequence had either a flat tracing (type B) or an otherwise non-measurable compliance peak. On average, the percentage of negative ME-nasopharyngeal pressure equilibrated after 5 swallows in the control population was 75%. To be more conservative, in this analysis we chose less than 60% as the cut off value to classify ears as having decreased ET function.
During both test protocols, input from submental surface electrodes (Noraxon Dual Electrodes, Noraxon USA Inc) placed over the anterior belly of the digastric muscle were continuously monitored for confirmation and timing of the commanded swallows.
Data Analysis
Sensitivity and specificity for Groups 1 and 2 assignment were computed using the ETDQ-7 score of ≥ 14.516 and PEq5<60% as an indication of ETD. The ETDQ-7 does not discriminate if symptoms come from left, right or both ears, so to avoid assumptions that could create a selection bias, the primary PEq5 statistical analysis was done at participant level using the lowest PEq5 for two ears, and at ear level using the same ETDQ-7 for both ears.
For participant level analysis, ETDQ-7 and PEq5 scores were compared between symptomatic and control groups using two-sample Wilcoxon test (proc npar1way, SAS v.9.4, Cary, NC). Exact 95% Clopper-Pearson confidence intervals (CI) were obtained for sensitivity and specificity (proc freq, SAS, v. 9.4) and Fisher exact test was used for comparing sensitivity or specificity between different subgroups of patients.
Kendall’s correlation coefficient was used to test association between the PEq5 and ETDQ-7 scores (proc corr, SAS, v.9.4). Association of ETDQ-7 scores with the inadequate PEq5<60% as well as with group assignment were assessed using empirical Area under the ROC curves (AUC).23,24
At ear-level data, statistical analysis (including evaluating Kendall’s coefficient and AUC) was performed using non-parametric bootstrap CI for clustered data with participant as a resampling unit, based on 10,000 bootstrap samples.25
RESULTS
From the initial 76 subjects evaluated, 17 were excluded because only data from one ear was available and 4 were excluded because the ME pressure gradient didn’t reach a minimum of −90 daPa for the PEq5 calculations.
Of the 55 remaining subjects, 25 were classified as Group 1 consisting of 15 females and 10 males, 15 white, 9 black and 1 other race, and mean age of 32±12.8 years. Thirty were included in Group 2 where 17 were females and 13 males, 25 whites, 4 blacks and 1 other race, with mean age of 27±16.3 years. Of the 110 tested ears, 30 had tympanostomy tubes (Group 1A= 6 (due to participation in studies at the Middle Ear Physiology Laboratory), Group 2A= 24), 4 had residual perforation due to recurrent ME infections and/or tympanostomy tube insertion (Group 2A= 4) and 76 had intact tympanic membranes (Group 1A= 6, Group 1B= 38, Group 2A= 6 and Group 2B= 26).
Table 2 shows the distribution of ETDQ-7 scores for each individual question and the total and mean scores and Standard Error (StdErr) for the ETDQ-7 and PEq5 in each of the 4 groups. Controls had ETDQ-7 total scores ranging from 7 to a maximum of 12, while in the symptomatic group the scores went from 7 to 41. Interestingly, 9 symptomatic subjects had scores < 14.5 (5 had bilateral long term tympanostomy tubes, 1 had unilateral perforation and 3 had bilateral intact tympanic membranes) and 24 ears had PEq5≥60% (8 non-intact and 16 intact tympanic membranes). Among controls, there were 9 ears with PEq5<60%, 3 with tympanostomy tubes and 6 with intact tympanic membranes.
Table 2.
Summaries for ETDQ-7 and PEq5 scores for participants in control and symptomatic groups (Groups 1–2A: non-intact tympanic membranes and Groups 1–2B: intact tympanic membranes).
| Controls | Symptomatics | ||||||
|---|---|---|---|---|---|---|---|
| Group 1A | Group 1 B | All | Group 2A | Group 2B | All | ||
| Number of participants | 6 | 19 | 25 | 17 | 13 | 30 | |
|
| |||||||
| Question 1 | Mean | 1.50 | 1.11 | 1.20 | 2.59 | 3.92 | 3.17 |
| StdErr | 0.22 | 0.07 | 0.08 | 0.43 | 0.57 | 0.36 | |
| Question 2 | Mean | 1.00 | 1.00 | 1.00 | 2.47 | 2.69 | 2.57 |
| StdErr | 0.00 | 0.00 | 0.00 | 0.44 | 0.49 | 0.32 | |
| Question 3 | Mean | 1.33 | 1.05 | 1.12 | 2.47 | 4.00 | 3.13 |
| StdErr | 0.21 | 0.05 | 0.07 | 0.47 | 0.65 | 0.41 | |
| Question 4 | Mean | 1.83 | 1.37 | 1.48 | 2.35 | 4.46 | 3.27 |
| StdErr | 0.40 | 0.11 | 0.13 | 0.41 | 0.61 | 0.40 | |
| Question 5 | Mean | 1.00 | 1.11 | 1.08 | 3.00 | 4.00 | 3.43 |
| StdErr | 0.00 | 0.07 | 0.06 | 0.43 | 0.67 | 0.38 | |
| Question 6 | Mean | 1.33 | 1.00 | 1.08 | 2.71 | 3.23 | 2.93 |
| StdErr | 0.21 | 0.00 | 0.06 | 0.43 | 0.61 | 0.36 | |
| Question 7 | Mean | 1.17 | 1.11 | 1.12 | 2.53 | 3.77 | 3.07 |
| StdErr | 0.17 | 0.07 | 0.07 | 0.46 | 0.60 | 0.38 | |
|
| |||||||
| ETDQ-7 total score | Mean | 9.17 | 7.74 | 8.08 | 18.12 | 26.08 | 21.57 |
| StdErr | 0.70 | 0.25 | 0.28 | 2.41 | 3.00 | 1.99 | |
| ETDQ-7 score ≥14.5 | Rate | 0.00 | 0.00 | 0.00 | 0.65 | 0.77 | 0.70 |
|
| |||||||
| PEq5 (worst ear) | Mean (%) | 53 | 74 | 69 | 29 | 51 | 39 |
| StdErr (%) | 17 | 7 | 7 | 6 | 11 | 6 | |
| PEq5<60% | Rate | 0.50 | 0.16 | 0.24 | 0.88 | 0.54 | 0.73 |
Association with the group assignment
The total ETDQ-7 score was significantly higher in the symptomatic than in the control group (21.6 vs. 8.1, p<0.0001). The difference stemmed primarily from participants with intact membranes (26.1 vs 7.7, p<0.0001), whereas participants with non-intact membranes had a relatively small difference (18.1 vs 9.2, p=0.95). Sensitivity and specificity of ETDQ-7 with respect to Groups 1 and 2 classification were correspondingly 70% (95% CI 0.51–0.85) and 100% (95% CI 0.86–1.00) with an AUC= 0.89 (95% CI 0.80–0.98), indicating a high correlation with group assignment. Sensitivity level appeared to be higher, albeit not statistically significant, for participants with intact than with non-intact membranes (77% vs. 65% respectively, p=0.6908).
The PEq5 score was significantly lower in the symptomatic than in the control group (0.39 vs. 0.69, p=0.0027). The difference stemmed from both participants with intact (0.51 vs 0.74, p<0.1715) and non-intact tympanic membranes (0.29 vs 0.53, p=0.1201). Sensitivity and specificity of PEq5 with respect to Groups 1 and 2 classification were correspondingly 73% (95% CI 0.54–0.88) and 76% (95% CI 0.55–0.91).
Association between ETDQ-7 X PEq5
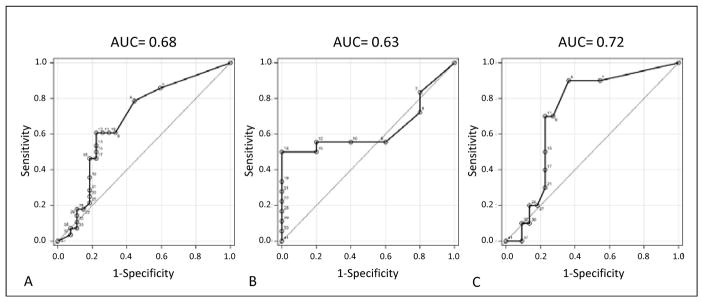
With respect to predicting PEq5<60%, ETDQ-7 had sensitivity and specificity of 54% and 78% respectively at participant level. Also, at participant level, the ETDQ-7 and the lowest PEq5 scores were not significantly correlated (Kendall’s correlation of −0.18, p=0.0689). With respect to predicting PEq5<60%, ETDQ-7 had AUC of 0.68 (95% CI 0.53–0.83) indicating a moderate level of association (Figure 1A). The level of association appeared to be lower, albeit not statistically significant for participants with non-intact tympanic membranes (AUC=0.63, 95% CI 0.40–0.87) (Figure 1B) than for participants with intact membranes (AUC=0.72, 95% CI 0.54–0.91) (Figure 1C).
Figure 1.
Participant level empirical ROC curves for ETDQ-7 with PEq5 as a reference. A. All participants; B. Participants with non-intact tympanic membranes (IDT); C. Participants with intact tympanic membranes (PC test).
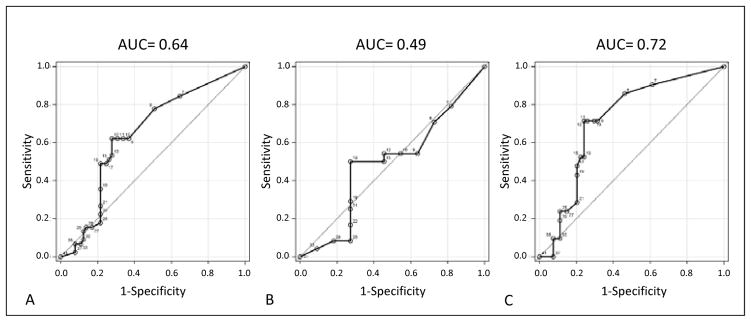
At ear level, the ETDQ-7 and ear-specific PEq5 scores remained at approximately the same low, and statistically non-significant, level (Kendall’s coefficient of −0.13, 95% CI −0.31–0.05). With respect to predicting PEq5<60%, ETDQ-7 had AUC of 0.64 (95% CI 0.50–0.77) indicating a moderate level of association (Figure 2A). The association appeared to be weaker, albeit not statistically significantly, for ears with non-intact tympanic membranes (AUC=0.49, 95% CI 0.29–0.71) (Figure 2B) than for ears with intact membranes (AUC=0.72, 95% CI 0.53–0.87) (Figure 2C).
Figure 2.
Ear level empirical ROC curves for ETDQ-7 with PEq5 as a reference. A. All participants; B. Participants with non-intact tympanic membranes (IDT); C. Participants with intact tympanic membranes (PC test).
DISCUSSION
Previous studies have reported sensitivity of 91–100%16,17, specificity of 95–100%16,17 and AUC= 0.95–1.0 (CI= 0.874–1.00)16,18 to the accuracy of the ETDQ-7 to discriminate people with ETD, but none of them based their results on an objective assessment of the ET function.
In the first part of the analysis we also used the participants’ perception and report of their symptoms to assign them to Groups 1 or 2. As expected, the ETDQ-7 showed 100 % specificity for this group assignment as none of the 25 controls reported complaints related to ETD or had scores above 12. The lower sensitivity found in our study (70%) derived from the 9 people in Group 2 that reported scores < 14.5: 5 had bilateral tympanostomy tubes (scores were 7,7,7,8 and 9), 1 had unilateral perforation (score=9) and 3 had bilateral intact tympanic membranes (scores were 9, 13 and 13). We believe that these lower scores were either because tubes and tympanic membrane perforations temporarily bypass ET problems or due to the intermittent nature of the symptoms that failed to be captured by the one month time frame comprised by the questionnaire.
On the second part of the analysis, instead of symptoms, we evaluated the ETDQ-7 accuracy for categorizing ETD based on an objective measure of the ET function. With respect to predicting PEq5<60%, ETDQ-7 had sensitivity and specificity of 54% and 78% respectively and AUC of 0.68 (95% CI 0.53–0.83) at participant level (Figure 1A) and of 0.64 (95% CI 0.50–0.77) at ear level (Figure 2A), indicating only a moderate level of association. As shown in Figures 1B and 2B, the association was weaker, although not statistically significant, in ears with non-intact tympanic membranes - AUC=0.63 and 0.49 at participant and ear levels respectively. Nine ears in the control group with no reported history of ME disease or ETD had PEq5<60% and 24 ears in the symptomatic group had PEq5≥60%, showing that symptoms alone are not sufficient to assess the level of ET function. Subjects with patulous ETs were tested but did not meet the study inclusion criteria because they cannot hold changes in ME pressure during the PC test or IDT. However, in the study conducted by Van Roeyen et al, the ETDQ-7 failed to differentiate between obstructive and patulous types of ETD.18 Together, all these factors have important implications if the ETDQ-7 is used as the only method to assess ETD for indications of surgical procedures. For example, patients with symptoms but normal ET function will not benefit or might even become patulous if subjected to the balloon dilation of the ET, while a patient with an already patulous ET has the risk of worsening of the problem.
Regarding the ETDQ-7 questions, symptoms such as ear pain, tinnitus and muffled hearing can also be present in a series of trigeminal nerve and inner ear pathologies, so these questions do not help differentiate cases not related to ETD. Muffled hearing and clogged ears are very similar symptoms, which introduces redundancy to the questionnaire and scoring system. In this study, 6 children were between 6 and 11 years old and, despite the help of their caregivers in explaining the questionnaire and the scoring system, we found it difficult for children younger than 12 years to consistently assess their symptoms, which restricts the use of the ETDQ-7 in this age group.
In conclusion, our results showed that although the ETDQ-7 had high correlation with symptoms, it was only moderately associated with an objective measure of the ET function. The scoring system also appears less reliable when applied to people with non-intact tympanic membranes. Further studies on the validation of the ETDQ-7 are necessary and should include test-retest reliability, assessment of the placebo effect on the scoring system and evaluation of accuracy for categorizing ETD based on other modalities of ET function tests. Despite these refinements, it seems improbable that symptoms alone will supplant the information derived from objective ET function tests.26
Acknowledgments
Funding: NIH Grant DC007667
This study was supported in part by a grant from the National Institutes of Health, P50 DC007667. The authors thank Dr William J Doyle PhD for his help in the study concept, and initial data analysis and interpretation; Dr Andriy I Bandos PhD for the ultimate statistical analysis and Ms Jenna El-Wagaa for her help in data entry.
Footnotes
Financial Disclosure Information: The authors have no financial disclosures.
Conflict of Interest: The authors have no conflicts to disclose.
The content of this paper was presented at the 2016 Annual Meeting of the American Academy of Otolaryngology – San Diego, CA.
CONFLICT OF INTEREST STATEMENT
None of the listed authors have any real or apparent conflicts of interest with respect to the material presented in this manuscript.
References
- 1.Bluestone CD. Eustachian Tube Structure, Function, Role in Otitis Media. Ontario: BC Decker Inc; 2005. [Google Scholar]
- 2.Virtanen H. Sonotubometry. An acoustical method for objective measurement of auditory tubal opening. Acta Otolaryngol. 1978;86(1–2):93–103. doi: 10.3109/00016487809124724. [DOI] [PubMed] [Google Scholar]
- 3.Asenov DR, Nath V, Telle A, Antweiler C, Walther LE, Vary P, et al. Sonotubometry with perfect sequences: first results in pathological ears. Acta Otolaryngol. 2010;130(11):1242–8. doi: 10.3109/00016489.2010.492481. [DOI] [PubMed] [Google Scholar]
- 4.Teixeira MS, Banks J, Swarts JD, Alper CM, Doyle WJ. Eustachian tube opening measured by sonotubometry is poorer in adults with a history of past middle ear disease. Int J Pediatr Otorhinolaryngol. 2014;78(4):593–8. doi: 10.1016/j.ijporl.2014.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doyle WJ, Swarts JD, Banks J, Casselbrant ML, Mandel EM, Alper CM. Sensitivity and specificity of eustachian tube function tests in adults. JAMA Otolaryngol Head Neck Surg. 2013;139(7):719–27. doi: 10.1001/jamaoto.2013.3559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ars B, Dirckx JJJ. Tubomanometry. In: Ars B, editor. Fibrocartilaginous Eustachian tube - middle ear cleft. The Netherlands: Kugler Publications, The Hauge; 2003. pp. 151–8. [Google Scholar]
- 7.Alper CM, Teixeira MS, Kim JH, Douglas Swarts J. Diagnostic accuracy of tubomanometry R value in detecting the Eustachian tube pressure equalizing function. Eur Arch Otorhinolaryngol. 2017;274(4):1865–72. doi: 10.1007/s00405-016-4430-6. [DOI] [PubMed] [Google Scholar]
- 8.Smith ME, Tysome JR. Tests of Eustachian tube function: a review. Clin Otolaryngol. 2015;40(4):300–11. doi: 10.1111/coa.12428. [DOI] [PubMed] [Google Scholar]
- 9.Poe DS, Pyykko I. Measurements of Eustachian tube dilation by video endoscopy. Otol Neurotol. 2011;32(5):794–8. doi: 10.1097/MAO.0b013e31821c6355. [DOI] [PubMed] [Google Scholar]
- 10.Alper CM, Teixeira MS, Swarts JD, Doyle WJ. Quantitative description of eustachian tube movements during swallowing as visualized by transnasal videoendoscopy. JAMA Otolaryngol Head Neck Surg. 2015;141(2):160–8. doi: 10.1001/jamaoto.2014.3002. [DOI] [PubMed] [Google Scholar]
- 11.Bylander A. Upper respiratory tract infection and eustachian tube function in children. Acta Otolaryngol. 1984;97(3–4):343–9. doi: 10.3109/00016488409130998. [DOI] [PubMed] [Google Scholar]
- 12.Bylander A, Tjernstrom O, Ivarsson A. Pressure opening and closing functions of the Eustachian tube by inflation and deflation in children and adults with normal ears. Acta Otolaryngol. 1983;96(3–4):255–68. doi: 10.3109/00016488309132898. [DOI] [PubMed] [Google Scholar]
- 13.Swarts JD, Casselbrant ML, Teixeira MS, Mandel EM, Richert BC, Banks JM, et al. Eustachian tube function in young children without a history of otitis media evaluated using a pressure chamber protocol. Acta Otolaryngol. 2014;134(6):579–87. doi: 10.3109/00016489.2014.882017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doyle WJ, Singla A, Banks J, El-Wagaa J, Swarts JD. Pressure chamber tests of eustachian tube function document lower efficiency in adults with colds when compared to without colds. Acta Otolaryngol. 2014;134(7):691–7. doi: 10.3109/00016489.2014.892213. [DOI] [PubMed] [Google Scholar]
- 15.Mandel EM, Casselbrant ML, Richert BC, Teixeira MS, Swarts JD, Doyle WJ. Eustachian Tube Function in 6-Year-Old Children with and without a History of Middle Ear Disease. Otolaryngol Head Neck Surg. 2016;154(3):502–7. doi: 10.1177/0194599815620149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCoul ED, Anand VK, Christos PJ. Validating the clinical assessment of eustachian tube dysfunction: The Eustachian Tube Dysfunction Questionnaire (ETDQ-7) Laryngoscope. 2012;122(5):1137–41. doi: 10.1002/lary.23223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schroder S, Lehmann M, Sudhoff H, Ebmeyer J. Assessment of chronic obstructive eustachian tube dysfunction: Evaluation of the German version of the Eustachian Tube Dysfunction Questionnaire. HNO. 2014;62(3):160–4. doi: 10.1007/s00106-013-2764-6. [DOI] [PubMed] [Google Scholar]
- 18.Van Roeyen S, Van de Heyning P, Van Rompaey V. Value and discriminative power of the seven-item Eustachian Tube Dysfunction Questionnaire. Laryngoscope. 2015;125(11):2553–6. doi: 10.1002/lary.25316. [DOI] [PubMed] [Google Scholar]
- 19.Liu P, Su K, Zhu B, Wu Y, Shi H, Yin S. Detection of eustachian tube openings by tubomanometry in adult otitis media with effusion. Eur Arch Otorhinolaryngol. 2016;273(10):3109–15. doi: 10.1007/s00405-016-3938-0. [DOI] [PubMed] [Google Scholar]
- 20.Van Roeyen S, Van de Heyning P, Van Rompaey V. Responsiveness of the 7-item Eustachian Tube Dysfunction Questionnaire. J Int Adv Otol. 2016;12(1):106–8. doi: 10.5152/iao.2016.2086. [DOI] [PubMed] [Google Scholar]
- 21.Randrup TS, Ovesen T. Balloon eustachian tuboplasty: a systematic review. Otolaryngol Head Neck Surg. 2015;152(3):383–92. doi: 10.1177/0194599814567105. [DOI] [PubMed] [Google Scholar]
- 22.McCoul ED, Anand VK. Eustachian tube balloon dilation surgery. Int Forum Allergy Rhinol. 2012;2(3):191–8. doi: 10.1002/alr.21007. [DOI] [PubMed] [Google Scholar]
- 23.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–45. [PubMed] [Google Scholar]
- 24.Zhou XH, Obuchowski NA, McClish DK. Statistical methods in diagnostic medicine. New York: Wiley & Sons Inc; 2011. [Google Scholar]
- 25.Field CA, Welsh AH. Bootstrapping clustered data. J R Statist Soc B. 2007;69(3):369–90. [Google Scholar]
- 26.Schroder S, Lehmann M, Sauzet O, Ebmeyer J, Sudhoff H. A novel diagnostic tool for chronic obstructive eustachian tube dysfunction-the eustachian tube score. Laryngoscope. 2015;125(3):703–8. doi: 10.1002/lary.24922. [DOI] [PubMed] [Google Scholar]