Key Points
Question
What is the association of overlapping surgery with increased risks for complications following surgical treatment of hip fractures and end-stage arthritis?
Findings
In this population-based cohort study of patients with hip fracture and hip arthritis, there were 960 and 1560 overlapping procedures, respectively. For patients undergoing overlapping procedures, there was an approximately 90% increase in the risk for surgical complications at 1 year, although the association was weaker in elective hip replacements than in hip fractures.
Meaning
Overlapping surgery is associated with an increased risk for complications in hip surgery, particularly for nonelective procedures.
Abstract
Importance
Overlapping surgery, also known as double-booking, refers to a controversial practice in which a single attending surgeon supervises 2 or more operations, in different operating rooms, at the same time.
Objective
To determine if overlapping surgery is associated with greater risk for complications following surgical treatment for hip fracture and arthritis.
Design, Setting, and Participants
This was a retrospective population-based cohort study in Ontario, Canada (population, 13.6 million), for the years 2009 to 2014. There was 1 year of follow-up. This study encompassed 2 large cohorts. The “hip fracture” cohort captured all persons older than 60 years who underwent surgery for a hip fracture during the study period. The “total hip arthroplasty” (THA) cohort captured all primary elective THA recipients for arthritis during the study period. We matched overlapping and nonoverlapping hip fractures by patient age, patient sex, surgical procedure (for the hip fracture cohort), primary surgeon, and hospital.
Exposures
Procedures were identified as overlapping if they overlapped with another surgical procedure performed by the same primary attending surgeon by more than 30 minutes.
Main Outcomes and Measures
Complication (infection, revision, dislocation) within 1 year.
Results
There were 38 008 hip fractures, and of those, 960 (2.5%) were overlapping (mean age of patients, 66 years [interquartile range, 57-74 years]; 503 [52.4%] were female). There were 52 869 THAs and of those, 1560 (3.0%) overlapping (mean age, 84 years [interquartile range, 77-89 years]; 1293 [82.9%] were female). After matching, overlapping hip fracture procedures had a greater risk for a complication (hazard ratio [HR], 1.85; 95% CI, 1.27-2.71; P = .001), as did overlapping THA procedures (HR, 1.79; 95% CI, 1.02-3.14; P = .04). Among overlapping hip fracture operations, increasing duration of operative overlap was associated with increasing risk for complications (adjusted odds ratio, 1.07 per 10-minute increase in overlap; P = .009).
Conclusions and Relevance
Overlapping surgery was relatively rare but was associated with an increased risk for surgical complications. Furthermore, increasing duration of operative overlap was associated with an increasing risk for complications. These findings support the notion that overlapping provision of surgery should be part of the informed consent process.
This cohort study determines if overlapping surgery is associated with greater risk for complications following surgical treatment for hip fracture and arthritis.
Introduction
Overlapping surgery refers to a situation in which a single attending surgeon supervises 2 or more operations, in different operating rooms, at the same time. Where overlapping surgery is performed, the attending surgeon is required to be present for critical parts of the procedure and readily available at other times, as needed. This longstanding practice is used to improve hospital resource utilization, provide opportunities to educate surgical trainees, and promote timely access to care, particularly for emergent cases.
Recently, media reports have suggested a link with postoperative complications, resulting in considerable concern and discussion among the public, surgical leaders, and policymakers. Foremost is the concern that the attending surgeon cannot appropriately supervise the procedure if not physically present, resulting in a potential quality-of-care deficit. Transparency in the informed consent process is also a concern. The American College of Surgeons (ACS) released guidelines around concurrent and overlapping surgery. While 2 recently published peer-reviewed studies have suggested that overlapping surgery is a safe practice, they both have significant limitations that limit their generalizability.
The current study sought to address this gap by examining the impact of overlapping surgery for hip fractures and for primary elective total hip arthroplasty (THA) at more than 75 hospitals in Ontario, Canada. The specific objectives of this study were to (1) determine the extent of overlapping surgery in patients receiving hip surgery; (2) assess whether overlapping procedures are at increased risk for relevant surgical complications; and (3) to explore whether there is an association with the duration of overlap and risk for complications.
Methods
Study Design and Setting
We conducted a population-based, matched-cohort study using data from several health administrative databases from Ontario, Canada (population of 13.5 million). Ontarians are insured under a single-payer system, which covers medically necessary procedures, including hip fracture surgery and elective hip arthroplasty. The study protocol was approved by the research ethics board at Sunnybrook Health Sciences Centre, Toronto, Ontario.
Data Sources
Data on every interaction a person has with our health care system are captured within administrative databases. These databases capture relevant demographic information on each patient (eg, age, sex, comorbidity) and physician (eg, years in practice, volume). The main data sources were hospital discharge abstracts from the Canadian Institute for Health Information Discharge Abstract Database (CIHI-DAD) and physician service claims from the Ontario Health Insurance Plan (OHIP) Claims History Database.
Participants
We defined 2 cohorts: the first comprised patients older than 60 years who had undergone an acute surgical procedure (fixation or replacement) for a hip fracture between April 1, 2009, and March 31, 2014. The second comprised patients older than 40 years who received a primary elective THA for arthritis between April 1, 2009, and March 31, 2015. During this study period, entry and exit times from the operating room for every surgical procedure in the province were recorded. We excluded procedures that were longer than 3 hours because this length of time is atypical and likely represented challenging cases that are not representative. See Table 1 for a full list of exclusions.
Table 1. Selection of Patients for Inclusion.
| Characteristic | No. |
|---|---|
| Hip fracture fixation procedures in Ontario, April 1, 2009, to March 31, 2014 | 49 051 |
| Exclusion criteria | |
| Prior hip fracture | 1859 |
| Age <60 y | 3356 |
| Associated fractures | 2084 |
| Cancer diagnosis | 198 |
| Osteomyelitis or infection prior to admission | 20 |
| Prior total hip replacement (within 5 y) | 894 |
| Not an Ontario resident | 30 |
| Died before or during surgery | 8 |
| Treated by nonorthopedic surgeon | 329 |
| Missing surgery start- or end-time data | 415 |
| Duration <30 min or >180 min | 1850 |
| Final cohort | 38 008 |
| Total hip arthroplasty procedures in Ontario, April 1, 2009, to March 31, 2015 | 77 403 |
| Exclusion criteria | |
| Not an Ontario resident or missing demographic data | 594 |
| Age <40 y | 1370 |
| Urgent admission | 10 098 |
| External injury | 7557 |
| Cancer diagnosis | 135 |
| Revision | 427 |
| Aborted | ≤5 |
| Osteomyelitis and other infections | 8 |
| Died at discharge | 57 |
| Treated by nonorthopedic surgeon | 217 |
| Missing surgery start- or end-time data | ≤5 |
| Duration <30 min or >180 min | 3137 |
| Multiple (different dates) hip replacement interventions within index admission | 41 |
| Admission date not between April 1, 2009, and March 31, 2015 | 90 |
| Primary surgeon not identified | 711 |
| Multiple indexes per person | 78 |
| Final cohort | 54 089 |
Main Exposure Variable—Overlapping Surgery
The start and end times captured in the database for each procedure reflect the entry and exit times into the operating room. As such, for each procedure, we chose the duration of overlap to define a procedure as overlapping that would indicate that the 2 procedures overlapped for a significant portion of time, after accounting for the time required to transfer the patient to the operating table, administer anesthesia, and properly position and drape the patient. We set the threshold of overlap to define a procedure as overlapping at 30 minutes, which is approximately 30% of the median duration (door-to-door) of both THAs and hip fracture surgery.
Primary Outcome—Surgical Complications
The primary outcomes were the occurrence of an infection, revision, or dislocation within a year. These were selected because they are the most likely to result from technical errors, which in turn may occur during unsupervised portions of the procedure. Other outcomes of interest were duration of surgery and death within 90 days.
Covariates of Interest
We measured and adjusted for several patient and physician covariates that have been previously shown to affect the risk of occurrence of complications following hip surgery. Patient age and sex were obtained from the OHIP Registered Persons Databases (RPDB). Comorbidities were assessed via an adaptation of the Charlson Comorbidity Index with a look-back of 5 years. The Adjusted Clinical Groups (ACGs) indicators were used to identify “frail” patients. Diabetes mellitus, prior myocardial infarction (MI), congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), cerebrovascular disease, chronic renal failure, and dementia were identified using validated algorithms. Median neighborhood household income quintile was used as a surrogate for socioeconomic status.
Hospital volume was defined as the number of hip fracture or THA procedures performed at the hospital in the 365 days prior to the index procedure. Surgeon volume was similarly defined for each hip fracture and THA patient. Presence of a billing surgical assistant was determined, as were his or her specialty (orthopedic surgeon, nonorthopedic surgeon, or family physician).
Matching
For each patient undergoing hip fracture repair or THA that overlapped with another procedure, we matched a patient who underwent the same surgical procedure by the same primary surgeon without an overlapping procedure; we used “greedy” matching. Patients were further matched according to age, sex, and hospital where the surgery was performed. We estimated standardized differences for all covariates after matching with more than 10 differences considered to be indicative of imbalance.
Statistical Analyses
Baseline cohort characteristics were described using proportions and medians as appropriate and were compared between groups using Wilcoxon rank sum tests for continuous variables and χ2 tests for categorical variables. Cox proportional hazard tests for the occurrence of a surgical complication were performed before and after matching, for the latter pair-matching into account by stratifying on matched pairs. All analyses were performed using SAS statistical software (version 9.3 and EG 6.1; SAS Institute). The type I error probability was set to α = .05 for all analyses.
Secondary Analysis
We also performed a secondary analysis in the overlapping procedures. First, restricted cubic splines were used to visualize the relationship between duration of overlap (measured in minutes) and the probability as well as relative risk for a complication. Second, generalized estimating equations were used to estimate the odds of complications following hip fracture surgery based on the duration of overlap, after controlling for relevant confounders. Other variables in the model included income quintile, rurality, Charlson Comorbidity Index, frailty, type of hip fracture, type of fixation, teaching hospital status, and physician volume, as well as controlling for clustering by the primary surgeon.
Results
Baseline Patient and Physician Characteristics
Between April 1, 2009, and March 31, 2014, there were 38 008 eligible patients with hip fracture (mean age, 66 years [interquartile range, 57-74 years]; 52.4% were female) (Table 1 and Table 2) and 52 869 eligible THA recipients(mean age, 84 years [interquartile range, 77-89 years]; 82.9% were female) (Table 1 and Table 3). A total of 960 (approximately 2.5%) hip fracture procedures and 1560 (approximately 3%) THAs were performed overlapping with another procedure. More than 70% of overlapping procedures were performed in teaching hospitals. Prior to matching, overlapping patients with hip fracture were not significantly different from patients who did not overlap, in terms of age, sex, comorbidity, or fracture type (Table 2). Among THAs, patients in overlapping procedures were slightly younger and had a lower prevalence of comorbid conditions (prior MI, dementia, diabetes, COPD). (Also see Appendices 1 and 2 and eTables 1-3 in the Supplement.)
Table 2. Characteristics of Hip Fracture Cohort Before and After Matching.
| Characteristic | Prior to Matching | After Matching | |||||
|---|---|---|---|---|---|---|---|
| All Patients | Overlapping | Nonoverlapping | P Value | Overlapping | Nonoverlapping | Standardized Difference | |
| Patients, No. | 38 008 | 960 | 37 048 | 855 | 855 | ||
| Demographics | |||||||
| Age, median (IQR), y | 84 (77-89) | 84 (77-89) | 84 (77-89) | >.99 | 84 (77-89) | 84 (78-89) | 0 |
| Female, No. (%) | 27 101 (71.3) | 700 (72.9) | 26 401 (71.3) | .26 | 631 (73.8) | 631 (73.8) | 0 |
| Income quintile, No. (%) | <.001 | ||||||
| Lowest | 8486 (22.3) | 222 (23.1) | 8264 (22.3) | 187 (21.9) | 185 (21.6) | 0.01 | |
| 2 | 7703 (20.3) | 185 (19.3) | 7518 (20.3) | 163 (19.1) | 169 (19.8) | 0.02 | |
| 3 | 7335 (19.3) | 161 (16.8) | 7174 (19.4) | 150 (17.5) | 152 (17.8) | 0.01 | |
| 4 | 7315 (19.2) | 164 (17.1) | 7151 (19.3) | 147 (17.2) | 157 (18.4) | 0.03 | |
| Highest | 6978 (18.4) | 217 (22.6) | 6761 (18.2) | 198 (23.2) | 181 (21.2) | 0.05 | |
| Nursing home, No. (%) | 3923 (10.3) | 89 (9.3) | 3834 (10.3) | .28 | 80 (9.4) | 81 (9.5) | 0 |
| Comorbidities, No. (%) | |||||||
| Previous myocardial infarction | 2995 (7.9) | 52 (5.4) | 2943 (7.9) | .004 | 48 (5.6) | 76 (8.9) | 0.13 |
| Congestive heart failure | 9082 (23.9) | 224 (23.3) | 8858 (23.9) | .68 | 201 (23.5) | 211 (24.7) | 0.03 |
| Cerebrovascular disease | 2837 (7.5) | 68 (7.1) | 2769 (7.5) | .65 | 62 (7.3) | 69 (8.1) | 0.03 |
| COPD | 7575 (19.9) | 180 (18.8) | 7395 (20.0) | .35 | 159 (18.6) | 151 (17.7) | 0.02 |
| Dementia | 11 635 (30.6) | 286 (29.8) | 11 349 (30.6) | .58 | 260 (30.4) | 269 (31.5) | 0.02 |
| Diabetes | 11 389 (30.0) | 286 (29.8) | 11 103 (30.0) | .91 | 252 (29.5) | 236 (27.6) | 0.04 |
| Chronic renal failure | 4901 (12.9) | 119 (12.4) | 4782 (12.9) | .64 | 104 (12.2) | 97 (11.3) | 0.03 |
| Frailty | 6911 (18.2) | 167 (17.4) | 6744 (18.2) | .52 | 151 (17.7) | 160 (18.7) | 0.03 |
| Charlson score, No. (%) | .54 | ||||||
| No prior admission | 16 920 (44.5) | 421 (43.9) | 16 499 (44.5) | 365 (42.7) | 359 (42.0) | 0.01 | |
| 0 | 6160 (16.2) | 162 (16.9) | 5998 (16.2) | 153 (17.9) | 170 (19.9) | 0.05 | |
| 1 | 5564 (14.6) | 135 (14.1) | 5429 (14.7) | 121 (14.2) | 109 (12.7) | 0.04 | |
| 2 | 3582 (9.4) | 104 (10.8) | 3478 (9.4) | 92 (10.8) | 84 (9.8) | 0.03 | |
| ≥3 or more | 5782 (15.2) | 138 (14.4) | 5644 (15.2) | 124 (14.5) | 133 (15.6) | 0.03 | |
| Fracture characteristics, No. (%) | |||||||
| Fracture type | .10 | ||||||
| Femoral neck | 19 300 (50.8) | 516 (53.8) | 18 784 (50.7) | 475 (55.6) | 454 (53.1) | 0.05 | |
| Intertrochanteric | 16 950 (44.6) | 409 (42.6) | 16 541 (44.6) | 357 (41.8) | 373 (43.6) | 0.04 | |
| Subtrochanteric | 1758 (4.6) | 35 (3.6) | 1723 (4.7) | 23 (2.7) | 28 (3.3) | 0.03 | |
| Fixation | .01 | ||||||
| Hemiarthroplasty | 15 245 (40.1) | 424 (44.2) | 14 821 (40.0) | 388 (45.4) | 388 (45.4) | 0 | |
| Screw | 17 373 (45.7) | 395 (41.1) | 16 978 (45.8) | 360 (42.1) | 360 (42.1) | 0 | |
| Intramedullary nail | 5390 (14.2) | 141 (14.7) | 5249 (14.2) | 107 (12.5) | 107 (12.5) | 0 | |
| Admission characteristic | |||||||
| Hours from ED to OR median (IQR) | 31 (21-50) | 36 (22-51) | 31 (21-50) | .01 | 35 (22-51) | 35 (23-51) | 0.04 |
| Teaching hospital, No. (%) | 10 442 (27.5) | 690 (71.9) | 9752 (26.3) | <.001 | 601 (70.3) | 601 (70.3) | 0 |
| Surgical assistant, No. (%) | 22 278 (58.6) | 526 (54.8) | 21 752 (58.7) | .02 | 458 (53.6) | 441 (51.6) | 0.04 |
| Family physician, No. (%) | 15 698 (41.3) | 171 (17.8) | 15 527 (41.9) | <.001 | 161 (18.8) | 178 (20.8) | 0.05 |
| Nonorthopedic surgeon, No. (%) | 2820 (7.4) | 21 (2.2) | 2799 (7.6) | <.001 | 18 (2.1) | 24 (2.8) | 0.05 |
| Orthopedic surgeon, No. (%) | 3960 (10.4) | 337 (35.1) | 3623 (9.8) | <.001 | 282 (33.0) | 244 (28.5) | 0.10 |
| Years in practice median (IQR) | 5 (0-27) | 0 (0-5) | 6 (0-27) | <.001 | 0 (0-4) | 0 (0-4) | 0.03 |
| Surgeon volume median (IQR) | 36 (25-49) | 39 (24-55) | 36 (25-49) | <.001 | 40 (27-56) | 39 (28-55) | 0.01 |
| Hospital volume median (IQR) | 206 (157-262) | 264 (187-320) | 204 (157-261) | <.001 | 268 (195-339) | 263 (195-342) | 0.02 |
| Characteristic | Total | Overlapping | Nonoverlapping | P Value | Overlapping | Nonoverlapping | P Value |
| Surgical complication, No. (%) | 2360 (6.2) | 80 (8.3) | 2280 (6.2) | .006 | 87 (10.2) | 53 (6.2) | .001 |
| Dislocation, No. (%) | 188 (0.5) | NA | 184 (0.5) | .73 | NA | NA | .74 |
| Infection, No. (%) | 1643 (4.3) | 60 (6.3) | 1583 (4.3) | .003 | 57 (6.7) | 36 (4.2) | .001 |
| Revision, No. (%) | 1802 (4.7) | 65 (6.8) | 1737 (4.7) | .003 | 61 (7.1) | 40 (4.7) | .02 |
| Duration of surgery, median (IQR), min | 95 (76-120) | 117 (93-140) | 95 (76-119) | <.001 | 116 (92-139) | 110 (90-131) | .003 |
| Death within 90 d, No. (%) | 5336 (14.0) | 138 (14.4) | 5198 (14.0) | .76 | 127 (15.0) | 107 (12.6) | .15 |
Abbreviations: ED, emergency department; IQR, interquartile range; NA, not applicable (<5 events); OR operating room.
Table 3. Characteristics of the Total Hip Arthroplasty Cohort Before and After Matching.
| Characteristic | Prior to Matching | After Matching | |||||
|---|---|---|---|---|---|---|---|
| All Patients | Overlapping | Nonoverlapping | P Value | Overlapping | Nonoverlapping | Standardized Difference | |
| Patients, No. | 52 869 | 1560 | 51 309 | 1456 | 1456 | ||
| Demographics | |||||||
| Age, median (IQR), y | 68 (60-76) | 66 (57-74) | 68 (60-76) | <.001 | 66 (58-74) | 66 (58-74) | 0 |
| Female, No. (%) | 28 836 (54.5) | 817 (52.4) | 28 019 (54.6) | .08 | 767 (52.7) | 767 (52.7) | 0 |
| Income quintile, No. (%) | .003 | 0.03 | |||||
| Lowest | 8093 (15.3) | 234 (15.0) | 7859 (15.3) | 219 (15.0) | 201 (13.8) | 0.04 | |
| 2 | 9782 (18.5) | 256 (16.4) | 9526 (18.6) | 243 (16.7) | 238 (16.3) | 0.01 | |
| 3 | 10 147 (19.2) | 261 (16.7) | 9886 (19.3) | 244 (16.8) | 270 (18.5) | 0.05 | |
| 4 | 11 377 (21.5) | 357 (22.9) | 11 020 (21.5) | 332 (22.8) | 314 (21.6) | 0.03 | |
| Highest | 13 293 (25.1) | 447 (28.7) | 12 846 (25.0) | 413 (28.4) | 430 (29.5) | 0.03 | |
| Comorbidities, No. (%) | |||||||
| Previous MI | 1802 (3.4) | 38 (2.4) | 1764 (3.4) | .03 | 35 (2.4) | 45 (3.1) | 0.04 |
| CHF | 2713 (5.1) | 83 (5.3) | 2630 (5.1) | .73 | 78 (5.4) | 67 (4.6) | 0.03 |
| Cerebrovascular disease | 559 (1.1) | 12 (0.8) | 547 (1.1) | .26 | 12 (0.8) | 19 (1.3) | 0.05 |
| COPD | 4027 (7.6) | 95 (6.1) | 3932 (7.7) | .02 | 93 (6.4) | 99 (6.8) | 0.02 |
| Dementia | 900 (1.7) | 14 (0.9) | 886 (1.7) | .01 | 12 (0.8) | 23 (1.6) | 0.07 |
| Diabetes | 10 921 (20.7) | 283 (18.1) | 10 638 (20.7) | .01 | 271 (18.6) | 251 (17.2) | 0.04 |
| Chronic renal failure | 1621 (3.1) | 45 (2.9) | 1576 (3.1) | .67 | 43 (3.0) | 45 (3.1) | 0.01 |
| Frailty | 2410 (4.6) | 76 (4.9) | 2334 (4.5) | .55 | 71 (4.9) | 63 (4.3) | 0.03 |
| Charlson score | .06 | ||||||
| No prior admission | 36 390 (68.8) | 1093 (70.1) | 35 297 (68.8) | 1021 (70.1) | 993 (68.2) | 0.04 | |
| 0 | 9807 (18.5) | 286 (18.3) | 9521 (18.6) | 261 (17.9) | 279 (19.2) | 0.03 | |
| 1 | 3069 (5.8) | 71 (4.6) | 2998 (5.8) | 70 (4.8) | 77 (5.3) | 0.02 | |
| 2 | 2123 (4.0) | 75 (4.8) | 2048 (4.0) | 70 (4.8) | 65 (4.5) | 0.02 | |
| ≥3 or more | 1480 (2.8) | 35 (2.2) | 1445 (2.8) | 34 (2.3) | 42 (2.9) | 0.03 | |
| Admission characteristics | |||||||
| Teaching hospital, No. (%) | 19 134 (36.2) | 1104 (70.8) | 18 030 (35.1) | <.001 | 1033 (70.9) | 1033 (70.9) | 0 |
| Surgical assistant, No. (%) | 40 287 (76.2) | 1104 (70.8) | 39 183 (76.4) | <.001 | 446 (30.6) | 473 (32.5) | 0.04 |
| Family physician | 25 042 (47.4) | 441 (28.3) | 24 601 (47.9) | 420 (28.8) | 374 (25.7) | 0.07 | |
| Nonorthopedic surgeon | 6624 (12.5) | 165 (10.6) | 6459 (12.6) | 144 (9.9) | 149 (10.2) | 0.01 | |
| Orthopedic surgeon | 8621 (16.3) | 498 (31.9) | 8123 (15.8) | 446 (30.6) | 460 (31.6) | 0.02 | |
| Surgeon volume, median (IQR) | 59 (40-88) | 82 (49-126) | 59 (40-87) | <.001 | 87 (53-130) | 86 (52-132) | 0.01 |
| Hospital volume, median (IQR) | 265 (181-496) | 415 (273-550) | 263 (180-487) | <.001 | 456 (275-553) | 435 (276-550) | 0.05 |
| Characteristic | Total | Overlapping | Nonoverlapping | P Value | Overlapping | Nonoverlapping | P Value |
| Surgical complication, No. (%) | 1145 (2.2) | 36 (2.3) | 1109 (2.2) | .70 | 34 (2.3) | 20 (1.4) | .052 |
| Dislocation | 267 (0.5) | 6 (0.4) | 261 (0.5) | .50 | NA | 6 (0.4) | .76 |
| Infection | 251 (0.5) | 8 (0.5) | 243 (0.5) | .82 | 7 (0.5) | 6 (0.4) | .78 |
| Revision | 845 (1.6) | 25 (1.6) | 820 (1.6) | >.99 | 24 (1.6) | 17 (1.2) | .26 |
| Duration of surgery, median (IQR), min | 108 (92-127) | 120 (99-142) | 107 (92-127) | <.001 | 119 (99-140) | 109 (91-132) | <.001 |
| Death within 90 d, No. (%) | 108 (0.2) | 6 (0.4) | 102 (0.2) | .11 | 6 (0.4) | NA | .53 |
Abbreviations: CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; IQR, interquartile range; MI, myocardial infarction; NA, not applicable (<5 events).
Matching
A total of 855 overlapping hip fracture procedures (89%) were successfully matched (by age, sex, procedure, attending surgeon, and hospital) to nonoverlapping procedures (Table 2). After matching, absolute standardized differences were 10.0 or less for all measured confounders (Table 2), except for prior MI, which was higher in the nonoverlapping group, and was controlled for in subsequent analyses.
A total of 1456 overlapping THAs (93%) were successfully matched (by age, sex, attending surgeon, and hospital) to nonoverlapping procedures (Table 3). After matching, absolute standardized differences were 10 or less for all measured confounders.
Outcomes After Matching
After matching, overlapping hip fractures were at a higher risk for surgical complications (hazard ratio [HR], 1.85; 95% CI, 1.27-2.71) (Table 4), particularly infection and early revision. Similarly, overlapping THA procedures were at a higher risk for complications (HR, 1.79; 95% CI, 1.02-3.14), but we could not determine the relative risk for individual complications as we were underpowered.
Table 4. Outcomes (Hazards Ratio) for Postoperative Complications.
| Cohort | Prior to Matching | After Matching | ||
|---|---|---|---|---|
| Adjusted Hazard Ratio (95% CI) | P Value | Hazard Ratio (95% CI) | P Value | |
| Hip fracture | ||||
| Composite complication | 1.40 (1.12-1.76) | .004 | 1.85 (1.27-2.71) | .001 |
| Dislocation | 1.01 (0.33-3.15) | .98 | 0.41 (0.08-2.06) | .27 |
| Superficial infection | 1.44 (1.06-1.95) | .02 | 1.89 (1.19-3.01) | .008 |
| Revision | 1.41 (1.05-1.90) | .02 | 1.77 (1.13-2.77) | .01 |
| Total hip arthroplasty | ||||
| Composite complication | 1.10 (0.75-1.62) | .63 | 1.79 (1.02-3.14) | .04 |
Secondary Analysis—Impact of Duration of Overlap in Overlapping Procedures
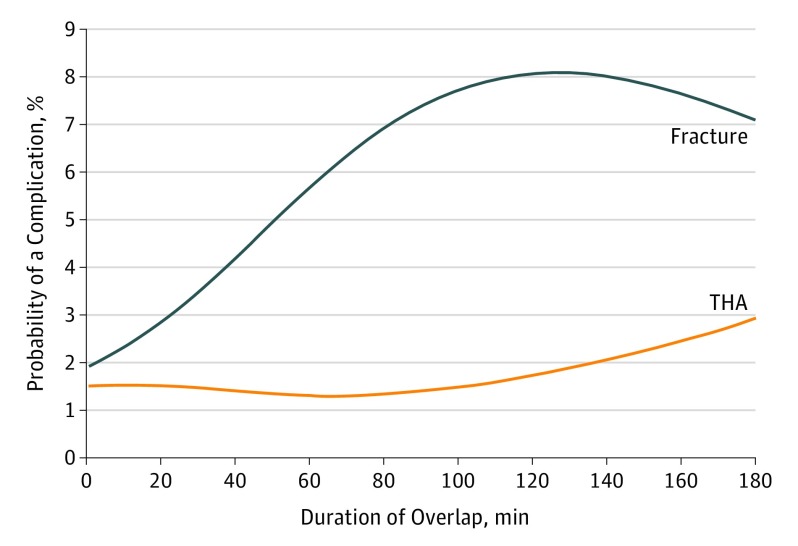
The restricted cubic splines relating duration of overlap to the risk for a surgical complication (Figure) suggest that these risks increase with increasing duration of overlap, but differently in hip fracture procedures than in THAs. Our regression analysis also indicated that increased duration of overlap is associated with an increased risk for complications in hip fracture procedures (adjusted odds ratio, 1.07 for every additional 10 minutes of overlap, P = .009).
Figure. Probability for a Complication in Overlapping Hip Fracture and Total Hip Arthroplasty (THA) Procedures vs Duration of Overlap.
Discussion
Key Results
We found that approximately 2.5% of patients with hip fracture and 3.0% of THA recipients were operated on by a surgeon who was also performing another operation. After matching, patients undergoing overlapping hip fracture repairs had a significantly increased risk for surgical complications (an increase from 6.4% to 10.4%). This risk worsened as the duration of overlap increased, with every additional 10 minutes of overlap raising the risk for a complication by approximately 7.0%. Overlapping THA procedures were also at increased risk; however, the relationship was not as pronounced (an increase from 1.4% to 2.3%).
Interpretation
The primary outcome of our study was the occurrence of surgical complications that directly related to the technical performance of the surgery itself. Overlapping procedures were at increased risk for the occurrence of a complication, particularly infection and early revision. The most likely mechanism for increased risk arises from having less experienced surgeons or surgical trainees perform portions of the case. We know from previous work that lack of experience and low surgical volumes are associated with an increased risk for surgical complications related to technical error. One of the tasks most frequently delegated to trainees and assistants is closure of the operative wound, as this is not typically considered “critical.” However, inadequate closure increases the risk for prolonged wound healing and infection, which in turn increases the likelihood of early revision. Interestingly the risk associated with overlapping surgery was much lower in elective hip arthroplasty than in nonelective hip fracture procedures. This suggests that the provision of overlapping surgery may be safer when the entire surgical team can prepare to deliver care to multiple patients, and perhaps when the primary surgeon can select assistants that he or she believes are suitable to have certain parts of the case delegated to them.
We selected hip fracture repair and elective THA as the study procedures for several reasons. The rates of these hip fractures are increasing in North America and there is a large body of evidence pointing toward improved outcomes with early surgical intervention. In addition, timely treatment of hip fractures is a quality indicator benchmark used by the provincial government, and in other jurisdictions, to assess hospital performance. As nonelective procedures, scheduling of hip fracture procedures must be balanced with the needs of patients who have been on waiting lists for elective procedures. All of these factors contribute to overlapping hip fracture surgery. However, THAs are one of the most common elective orthopedic procedures in North America, and many centers have developed standardized care pathways designed to safely maximize operating room throughput for these procedures. In addition, we wished to explore the safety of overlapping surgery in the setting of an elective procedure, and indeed found that it may be safer than for a nonelective procedure.
We defined overlapping in our cohort as an overlap that lasted for at least 30 minutes. This represents approximately 30% of the median time in the operating room for both hip fracture procedures and THAs and allows for time to position the patient and administer anesthesia. As such, procedures labeled as overlapping likely represent ones with a genuine surgical overlap, and that the overlap resulted in someone other than the attending surgeon operating unsupervised for at least a portion of the case. Our secondary analysis found that increased duration of overlap in hip fracture procedures was associated with an increased risk for complications, indicating that as the likelihood that the surgical procedures themselves overlapped (as opposed to positioning or induction of anesthesia), so did the risk for a complication.
Generalizability
Our findings may not generalize to hospitals where overlapping surgical procedures are more commonly performed. Indeed, overlapping hip fracture surgery seems to be an anomaly in our jurisdiction, rather than standard of practice, which may have had an impact on the quality of its performance. We also cannot assume our findings are generalizable to other surgical procedures, such as more acute surgical emergencies, where timely care may necessitate overlapping surgery. However, we were able to assess overlapping surgery in both elective and nonelective circumstances. While our findings in the arthroplasty cohort indicate that overlapping surgery might lead to slightly increased risk for complications, the absolute increase in the rates of complications is low. These findings further suggest that overlapping surgery may be safer when performed in the context of an elective procedure, when the surgeon and the rest of the health care team can adequately prepare to deliver care in an overlapping fashion.
Strengths and Limitations
While overlapping surgery has come under increasing scrutiny of late, this study is, to our knowledge, the first population-based study of this issue. We had the ability to capture complications that presented at centers other than where the original procedure was performed. We were also able to examine long-term outcomes (≤1 year), which allowed us to compare complications that may result from technical error (eg, infection, revision surgery). We controlled for various confounders, including patient (age, sex, comorbidity) and physician (surgeon volume, hospital volume, teaching hospital) factors. Recently, 2 studies have been published that indicated that overlapping surgery does not confer any increased risk for complications. Zhang et al performed a retrospective review of a single institution over a 3-year period, and compared the rates of complications at 30 days in multiple outpatient procedures. However, they did not perform any risk adjustment for procedure, or by patient and physician factors. Hyder et al looked at multiple surgical procedures at a single center, using an m:n matching strategy in which all overlapping procedures of a particular type of surgery were matched to all nonoverlapping procedures of the same type of surgery, with subsequent adjustment for the individual surgeon. Neither study was able to capture complications that presented at a different center.
This study used operating room entry and exit times on a population-wide scale (ie, across an entire geographic area as opposed to a single center or group of hospitals) to identify overlapping surgical procedures. The data on surgery times have high face validity; basic tests of their quality included that (1) start times always occurred after the hospital admission time and that (2) “sensible” surgical durations are predicted by surgery start and end times. We were able to measure and balance a wide variety of patient and physician factors between groups. Matching by procedure, surgeon, and hospital levels allowed us to control for unmeasured physician factors. Limitations to this study primarily relate to unmeasured factors that were not captured in our database(s), and the study design. We attempted to mitigate the impact of unmeasured confounders for physicians by matching by surgeon and hospital. However, there were other patient-level variables we were unable to assess or control for, such as body mass index and smoking history.
We selected 30 minutes of overlap as our threshold to identify a procedure as overlapping because it was approximately one-third of the median door-to-door times for both cohorts; this would provide sufficient time for induction of anesthesia, positioning, and draping. However, it is possible that in some procedures these steps would have taken longer, particularly in patients with hip fracture because they generally have a higher burden of medical comorbidities. As such, we performed a second analysis wherein we determined the impact of the duration of overlap on the risk for complications following hip fracture repair. We also generated splines for both cohorts to visualize the relationship between overlap duration and complication risk. These splines suggested that increasing overlap was associated with an increased risk for complications; this was more pronounced in hip fracture procedures than in elective hip arthroplasty.
Most important, we could not identify the actual location of the attending surgeon, and could not determine where the attending surgeon was during “critical portions” of the case. According to the ACS, “concurrent” procedures occur when “the critical or key components of the procedures for which the primary attending surgeon is responsible are occurring all or in part at the same time,” whereas in overlapping procedures, the surgeon is present for all critical portions while a “qualified practitioner” performs the noncritical portions in the primary surgeon’s absence. Although the distinction is potentially important, this concept is severely limited by the fact that there are no widely accepted definitions of what constitutes a critical portion of a procedure; this is determined by the primary surgeon. Every surgeon might have a unique definition for what might be a critical aspect of a specific procedure, which might vary depending on the assistant(s) available to them. Our contention is that without having knowledge of which portions of a procedure the attending surgeon would identify as critical, then potentially every step of the procedure from incision to closure may meet this threshold. This might explain our findings that overlapping (as opposed to concurrent) hip surgery is also associated with an increased risk for complications.
Conclusions
To our knowledge, this is the first population-based study examining the consequences of overlapping surgery at the level of a health care system. Our results indicate that while overlapping surgery is uncommon in our jurisdiction for hip surgery, it is a risk factor for complications, particularly for hip fractures. Furthermore, an increasing duration of overlap with another procedure is associated with progressively increasing risk for complications. Most important, our findings reinforce the notion that overlapping provision of surgery must be part of the informed consent process.
eAppendix 1. Predictors of hip fracture revision
eTable 1. Predictors of revision of hip fractures within 1 y of surgery
eAppendix 2. Adding type of assistant to the matched variables
eTable 2. Characteristics of hip fracture cohort after matching
eTable 3. Outcomes (hazards ratio) for postoperative complications in matched hip fracture patients
References
- 1.Beasley GM, Pappas TN, Kirk AD. Procedure delegation by attending surgeons performing concurrent operations in academic medical centers: balancing safety and efficiency. Ann Surg. 2015;261(6):1044-1045. [DOI] [PubMed] [Google Scholar]
- 2.American College of Surgeons Statements on Principles. 2016. https://www.facs.org/about-acs/statements/stonprin. Accessed October 18, 2017. [Google Scholar]
- 3.Brown MJ, Subramanian A, Curry TB, Kor DJ, Moran SL, Rohleder TR. Improving operating room productivity via parallel anesthesia processing. Int J Health Care Qual Assur. 2014;27(8):697-706. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Medicare & Medicaid Services (CMS) CMS Manual System Pub 100-04: Medicare Claims. 2011. https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R2303CP.pdf]. Accessed October 18, 2017.
- 5.Boston Globe. Clash in the name of care: a Spotlight Team Report. 2015. http://apps.bostonglobe.com/spotlight/clash-in-the-name-of-care/?p1=Clash_Story_to-landing. Accessed November 12, 2015.
- 6.Boston Globe. Overlapping surgeries to face US Senate inquiry. 2016. https://www.bostonglobe.com/metro/2016/03/12/senator-launches-inquiry-into-simultaneous-surgeries-hospitals-including-mass-general/wxEsbg5r2poqtk88LkcHQI/story.html. Accessed March 13, 2016.
- 7.Mello MM, Livingston EH. Managing the risks of concurrent surgeries. JAMA. 2016;315(15):1563-1564. [DOI] [PubMed] [Google Scholar]
- 8.Hyder JA, Hanson KT, Storlie CB, et al. Safety of overlapping surgery at a high-volume referral center. Ann Surg. 2017;265(4):639-644. [DOI] [PubMed] [Google Scholar]
- 9.Zhang AL, Sing DC, Dang DY, et al. Overlapping surgery in the ambulatory orthopaedic setting. J Bone Joint Surg Am. 2016;98(22):1859-1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ravi B, Jenkinson R, Austin PC, et al. Relation between surgeon volume and risk of complications after total hip arthroplasty: propensity score matched cohort study. BMJ. 2014;348:g3284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ravi B, Croxford R, Hollands S, et al. Increased risk of complications following total joint arthroplasty in patients with rheumatoid arthritis. Arthritis Rheumatol. 2014;66(2):254-263. [DOI] [PubMed] [Google Scholar]
- 12.Do LN, Kruke TM, Foss OA, Basso T. Reoperations and mortality in 383 patients operated with parallel screws for Garden I-II femoral neck fractures with up to ten years follow-up. Injury. 2016;47(12):2739-2742. [DOI] [PubMed] [Google Scholar]
- 13.Dodd AC, Bulka C, Jahangir A, Mir HR, Obremskey WT, Sethi MK. Predictors of 30-day mortality following hip/pelvis fractures. Orthop Traumatol Surg Res. 2016;102(6):707-710. [DOI] [PubMed] [Google Scholar]
- 14.Berggren M, Stenvall M, Englund U, Olofsson B, Gustafson Y. Co-morbidities, complications and causes of death among people with femoral neck fracture: a three-year follow-up study. BMC Geriatr. 2016;16(120):120. doi: 10.1186/s12877-016-0291-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-619. [DOI] [PubMed] [Google Scholar]
- 16.Weiner JP, Abrams C The Johns Hopkins ACG® System: Technical Reference Guide. Version 10.0. Baltimore, MD: Johns Hopkins University;2011.
- 17.McIsaac DI, Bryson GL, van Walraven C. Association of frailty and 1-year postoperative mortality following major elective noncardiac surgery: a population-based cohort study. JAMA Surg. 2016;151(6):538-545. [DOI] [PubMed] [Google Scholar]
- 18.Stukel TA, Fisher ES, Alter DA, et al. Association of hospital spending intensity with mortality and readmission rates in Ontario hospitals. JAMA. 2012;307(10):1037-1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, To T. Identifying individuals with physician diagnosed COPD in health administrative databases. COPD. 2009;6(5):388-394. [DOI] [PubMed] [Google Scholar]
- 20.Shah BR, Lipscombe LL. Clinical diabetes research using data mining: a Canadian perspective. Can J Diabetes. 2015;39(3):235-238. [DOI] [PubMed] [Google Scholar]
- 21.Juurlink D, Preyra C, Croxford R, et al. Canadian Institute for Health Information Discharge Abstract Database: A Validation Study. Toronto, ON: Institute for Clinical Evaluative Sciences; 2006. [Google Scholar]
- 22.Tu JV, Naylor CD, Austin P. Temporal changes in the outcomes of acute myocardial infarction in Ontario, 1992-1996. CMAJ. 1999;161(10):1257-1261. [PMC free article] [PubMed] [Google Scholar]
- 23.Jong P, Gong Y, Liu PP, Austin PC, Lee DS, Tu JV. Care and outcomes of patients newly hospitalized for heart failure in the community treated by cardiologists compared with other specialists. Circulation. 2003;108(2):184-191. [DOI] [PubMed] [Google Scholar]
- 24.Tu K, Mitiku T, Lee DS, Guo H, Tu JV. Validation of physician billing and hospitalization data to identify patients with ischemic heart disease using data from the Electronic Medical Record Administrative data Linked Database (EMRALD). Can J Cardiol. 2010;26(7):e225-e228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agabiti N, Picciotto S, Cesaroni G, et al. ; Italian Study Group on Inequalities in Health Care . The influence of socioeconomic status on utilization and outcomes of elective total hip replacement: a multicity population-based longitudinal study. Int J Qual Health Care. 2007;19(1):37-44. [DOI] [PubMed] [Google Scholar]
- 26.Santaguida PL, Hawker GA, Hudak PL, et al. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51(6):428-436. [PMC free article] [PubMed] [Google Scholar]
- 27.Kralj B. Measuring “Rurality” for Purposes of Health Care Planning: An Empirical Measure for Ontario. Toronto: Ontario Medical Association; 2005. [Google Scholar]
- 28.Parsons LS. Reducing bias in a propensity score matched-pair sample using greedy matching techniques. http://www2.sas.com/proceedings/sugi26/p214-26.pdf. Accessed October 18, 2018.
- 29.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083-3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hospital MG. About concurrent/overlapping surgery. 2016. http://www.massgeneral.org/overlapping-surgery/about.aspx. Accessed October 18, 2018.
- 31.Leaper DJ. Traumatic and surgical wounds. BMJ. 2006;332(7540):532-535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Papadimitropoulos EA, Coyte PC, Josse RG, Greenwood CE. Current and projected rates of hip fracture in Canada. CMAJ. 1997;157(10):1357-1363. [PMC free article] [PubMed] [Google Scholar]
- 33.Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ. 2010;182(15):1609-1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bhandari M, Sprague S, Schemitsch EH; International Hip Fracture Research Collaborative . Resolving controversies in hip fracture care: the need for large collaborative trials in hip fractures. J Orthop Trauma. 2009;23(6):479-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lizaur-Utrilla A, Martinez-Mendez D, Collados-Maestre I, Miralles-Muñoz FA, Marco-Gomez L, Lopez-Prats FA. Early surgery within 2 days for hip fracture is not reliable as healthcare quality indicator. Injury. 2016;47(7):1530-1535. [DOI] [PubMed] [Google Scholar]
- 36.Health Quality Ontario Quality-Based Procedures: Clinical Handbook for Hip Fracture. http://www.hqontario.ca/evidence/publications-and-ohtac-recommendations/clinical-handbooks. 2013. Accessed October 18, 2017.
- 37.Maradit Kremers H, Larson DR, Crowson CS, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97(17):1386-1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Medicare and Medicaid Services Hospital Readmissions Reduction Program (HRRP). 2015. https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Accessed October 18, 2017.
- 39.Ravi B, Croxford R, Austin PC, et al. The relation between total joint arthroplasty and risk for serious cardiovascular events in patients with moderate-severe osteoarthritis: propensity score matched landmark analysis. BMJ. 2013;347:f6187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Frood J, Johnson T. Improving measures of hip fracture wait times: a focus on Ontario. Healthc Q. 2010;13(4):16-18. [DOI] [PubMed] [Google Scholar]
- 41.Redelmeier DA, Thiruchelvam D, Daneman N. Introducing a methodology for estimating duration of surgery in health services research. J Clin Epidemiol. 2008;61(9):882-889. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Predictors of hip fracture revision
eTable 1. Predictors of revision of hip fractures within 1 y of surgery
eAppendix 2. Adding type of assistant to the matched variables
eTable 2. Characteristics of hip fracture cohort after matching
eTable 3. Outcomes (hazards ratio) for postoperative complications in matched hip fracture patients