Abstract
Importance
Robust laboratory use data are lacking to support the general assumption that teaching hospitals with trainees routinely order more laboratory tests for inpatients than do nonteaching hospitals.
Objective
To quantify differences in the use of laboratory tests between teaching and nonteaching hospitals.
Design, Setting, and Participants
A cross-sectional study was performed using a statewide database to identify hospitalizations with a primary diagnosis of bacterial pneumonia or cellulitis from January 1, 2014, to June 30, 2015, at teaching and nonteaching hospitals with 100 or more hospitalizations of each condition. Patients included were adult inpatients with a primary diagnosis of bacterial pneumonia (n = 24 118) or cellulitis (n = 19 211); patients excluded were those with an intensive care unit stay, transfer from another hospital, or a length of stay that was 2 SDs or more of the condition’s mean length of stay.
Main Outcomes and Measures
Mean laboratory tests per day stratified by illness severity, as well as factors associated with laboratory use rates.
Results
A total of 43 329 hospitalized patients (20493 women and 22836 men) had a principal diagnosis of bacterial pneumonia or cellulitis across 11 major teaching hospitals, 12 minor teaching hospitals, and 73 nonteaching hospitals in Texas. Mean number of laboratory tests per day varied significantly by hospital type and was highest for major teaching hospitals for both conditions (bacterial pneumonia: major teaching hospitals, 13.21; 95% CI, 12.91-13.51; nonteaching hospitals, 8.92; 95% CI, 8.84-9.00; P < .001; cellulitis: major teaching hospitals, 10.43; 95% CI, 10.16-10.70; nonteaching hospitals, 7.29; 95% CI, 7.22-7.36; P < .001). This association held for all levels of illness severity for both conditions, except for patients with cellulitis with the highest illness severity level. In generalized mixed linear regression models, controlling for additional patient and encounter covariates, there was a significant difference in the marginal effect of hospital teaching status on mean number of laboratory tests per day between major teaching and nonteaching hospitals (difference in marginal mean laboratory tests per day for bacterial pneumonia, 3.58; 95% CI, 2.61-4.55; P < .001; for cellulitis, 2.61; 95% CI, 1.76-3.47; P < .001).
Conclusions and Relevance
Compared with nonteaching hospitals, patients in Texas admitted to major teaching hospitals with bacterial pneumonia or cellulitis received significantly more laboratory tests after controlling for illness severity, length of stay, and patient demographics. These results support the need to examine how the culture of training environments may contribute to increased use of laboratory tests.
This cross-sectional study uses a statewide database to quantify differences in the use of laboratory tests between teaching and nonteaching hospitals.
Key Points
Question
Is there a difference in ordering patterns of laboratory tests between US teaching hospitals and nonteaching hospitals?
Findings
In a cross-sectional study of 43 329 adults hospitalized for bacterial pneumonia and cellulitis in Texas, mean laboratory test orders per inpatient day were significantly higher at 11 major teaching hospitals compared with 73 nonteaching hospitals after adjusting for illness severity and other patient and encounter covariates.
Meaning
Major teaching hospital status was associated with increased laboratory testing for 2 common medical conditions.
Introduction
It is often assumed that trainees at academic medical centers routinely order more laboratory tests for inpatients compared with more experienced physicians. Resident physicians may order more laboratory testing for many different reasons, including lack of nuanced knowledge about when a laboratory test may or may not be indicated, supervisors who are more likely to criticize missing morning laboratory test results rather than extra tests, and a lack of oversight and cost transparency. A significant proportion of inpatient laboratory tests are unnecessary, potentially harmful, and contribute to rising health care costs across the United States.
Prior studies at single academic medical centers have shown that teaching services ordered more laboratory testing and had higher mean laboratory costs compared with nonteaching services. A national retrospective database study found increased use of resources by supervised residents vs attending physicians alone in the emergency department setting. However, there is little direct evidence to support that this pattern of increased laboratory testing by trainees is truly a widespread phenomenon, particularly when accounting for the additional testing that may be warranted owing to inpatients with increased severity of illness at academic medical centers.
We sought to use a large statewide all-payer database to quantify differences between teaching and nonteaching hospitals in mean laboratory tests per day stratified by severity of illness. We chose to analyze patients hospitalized with bacterial pneumonia or cellulitis, since patients with these conditions are frequently admitted at both teaching and nonteaching hospitals, and specialized laboratory testing is generally not required for these conditions.
Methods
Data Source
We used the Texas Inpatient Public Use Data File (TIPUDF) to analyze all adult inpatient hospital discharges with a principal diagnosis of bacterial pneumonia or cellulitis from January 1, 2014, to June 30, 2015. The TIPUDF has a defined principal diagnosis field, which is the documented principal diagnosis at the time of discharge for that hospitalization. The TIPUDF is a billing-level administrative statewide data set maintained by the Texas Department of State Health Services. The TIPUDF captures 93% to 97% of all hospital discharges in the state and includes detailed deidentified inpatient discharge data on the demographic, clinical, resource use, and outcome domains from state-licensed hospitals. The TIPUDF allows up to 25 different diagnoses to be recorded for each hospitalization. This data set has been used in multiple prior studies. This study was approved by The University of Texas at Austin Office of Research Support. Informed consent was not obtained because the data were from deidentified and previously collected administrative data.
Inclusion Criteria and Study Population
We identified hospitalizations with a principal diagnosis of bacterial pneumonia (n = 24 118; International Classification of Diseases, Ninth Revision [ICD-9] codes 0382, 481, 485-6, 4820-4822, 4829, 48230-32, 48239, 48282-84, 48289, 48240-42, and 48249) or cellulitis (n = 19 211; ICD-9 codes 6822-26, 6828, and 6829) between January 1, 2014, and June 30, 2015. We excluded patients who were younger than 18 years of age, had an intensive care unit stay during the hospitalization, were transferred from another hospital, or had a length of stay (LOS) 2 SDs or higher than the condition’s mean LOS. Because hospitalizations with a documented cancer diagnosis were disproportionately distributed among hospital types, we excluded hospitalizations with a diagnosis of cancer with a reportable tumor type, as defined by the National Institutes of Health. We also excluded patients with a diagnosis of HIV and/or drug use, as these patients have restricted demographic data in the TIPUDF.
We included hospitalizations from hospitals with at least 100 cases of each principal diagnosis during the study period and categorized each hospital into 1 of 3 types: major teaching hospital (defined as a member of the Association of American Medical Colleges’ Council of Teaching Hospitals and Health Systems [n = 11]), minor teaching hospital (a hospital that is a teaching facility but is not a member of the Association of American Medical Colleges’ Council of Teaching Hospitals and Health Systems [n = 12]), and nonteaching hospital (n = 73).
Outcome Measure and Covariates
Our primary outcome measure was mean laboratory orders per hospital day stratified by illness severity, defined as the sum of the individual units billed for laboratory revenue codes divided by LOS. We used a severity of illness subclass score from the All Patient Refined (APR) Diagnosis Related Group (DRG) from the 3M APR-DRG Grouper to stratify mean laboratory tests per day by severity of illness. The score indicates the extent of physiological decompensation and incorporates all diagnoses, procedures, and some patient factors (age, sex, and discharge disposition) to calculate a number from 1 to 4 on a discrete scale (where 1 = minor, 2 = moderate, 3 = major, and 4 = extreme). This grouper has been used in previous studies to create subsets by severity of illness in inpatients.
In regression and sensitivity analyses, we used an outcome of mean laboratory tests per day. We used a log link and γ distribution to account for wide variance and nonnormal distribution in mean laboratory tests per day. Fixed covariates included hospital type (major teaching, minor teaching, and nonteaching), severity of illness (APR-DRG severity of illness score), LOS, patient age, patient sex, patient race, patient ethnicity, payer, admission type, and discharge disposition. Hospital was included as a random effect to account for clustering of laboratory test ordering patterns within hospitals.
Statistical Analysis
Patient Population and Hospital-Level Comparisons
All analyses were conducted using R, version 3.3.2 (Foundation for Statistical Computing) except for the generalized linear mixed effect models, which were fit using STATA, version 14.2 (StataCorp). Kruskal-Wallis rank sum and χ2 tests were used to compare characteristics of hospitalizations across hospital type for each condition. We used 1-way analysis of variance tests to determine if mean laboratory tests per day, mean LOS, and mean illness severity varied by hospital type. We calculated Spearman ρ correlation coefficient (rs) to examine the association between log mean laboratory tests per day for pneumonia and cellulitis.
Generalized Linear Mixed Effect Regression Analysis
We used the meglm function in STATA to create separate generalized linear mixed-effect regression models for each condition to determine if hospital type was associated with mean laboratory tests per day. We used the margins command to calculate the marginal effect of hospital teaching status on mean laboratory tests per day. We excluded hospitalizations with zero laboratory charges from the regression analysis (cellulitis, 16; and pneumonia, 80).
Sensitivity Analyses
We conducted sensitivity analyses by repeating the regression analyses under the following 3 alternative conditions: (1) only including patients with the lowest severity of illness score to address the concern that sicker patients more often go to teaching hospitals; (2) after excluding hospitalizations with a documented diagnosis of hyponatremia (ICD-9 code 2761), acute anemia (ICD-9 codes 2850-1, 2853, 2858-9, 28521-22, and 28529), or acute kidney injury (ICD-9 codes 5845-6 and 5848-9), since these conditions can lead to appropriate serial laboratory test monitoring; and (3) excluding hospitalizations from 1 major teaching hospital that was a major outlier in mean laboratory tests per day. We calculated mean laboratory tests per day in subsets by illness severity after excluding patients diagnosed with hyponatremia, acute anemia, or acute kidney injury, and after excluding 1 major teaching hospital outlier.
Results
Patient Population
We analyzed 24 118 patients hospitalized with the principal diagnosis of pneumonia and 19 211 patients hospitalized for cellulitis, across 11 major teaching hospitals, 12 minor teaching hospitals, and 73 nonteaching hospitals in Texas. The population of patients hospitalized varied by hospital type for each condition (Table 1). Major teaching hospitals were more likely than nonteaching hospitals to treat patients with pneumonia who had a higher illness severity, who were younger, black, non-Hispanic, uninsured, urgently admitted, and discharged home. Likewise, patients with cellulitis treated at major teaching hospitals were more likely to have a higher illness severity and be younger, black, uninsured, urgently admitted, and discharged to home when compared with patients with cellulitis treated at nonteaching hospitals.
Table 1. Comparison of Patient Characteristics by Hospital Type.
| Characteristic | Hospital Typea | P Valueb | ||
|---|---|---|---|---|
| Major Teaching | Minor Teaching | Nonteaching | ||
| Hospitalizations, No. | ||||
| Bacterial pneumonia | 3439 | 3281 | 17 398 | NA |
| Cellulitis | 2912 | 2258 | 14 041 | NA |
| Length of stay, mean (SD), d | ||||
| Bacterial pneumonia | 3.95 (2.03) | 3.92 (2.02) | 3.91 (2.02) | .65 |
| Cellulitis | 3.77 (1.84) | 3.71 (1.83) | 3.75 (1.86) | .51 |
| Illness severityc | ||||
| Bacterial pneumonia, No. (%) | ||||
| 1 | 309 (9.0) | 416 (12.7) | 2151 (12.4) | <.001 |
| 2 | 1529 (44.5) | 1553 (47.3) | 8198 (47.1) | |
| 3 | 1452 (42.2) | 1183 (36.1) | 6467 (37.2) | |
| 4 | 149 (4.3) | 129 (3.9) | 582 (3.3) | |
| Cellulitis, No. (%) | ||||
| 1 | 772 (26.5) | 718 (31.8) | 4091 (29.1) | <.001 |
| 2 | 1454 (49.9) | 1137 (50.4) | 7320 (52.1) | |
| 3 | 645 (22.1) | 388 (17.2) | 2555 (18.2) | |
| 4 | 41 (1.4) | 15 (0.7) | 75 (0.5) | |
| Age group, y | ||||
| Bacterial pneumonia, No. (%) | ||||
| 18-34 | 316 (9.2) | 188 (5.7) | 1017 (5.8) | <.001 |
| 35-54 | 732 (21.3) | 585 (17.8) | 2969 (17.1) | |
| 55-74 | 1303 (37.9) | 1225 (37.3) | 6388 (36.7) | |
| ≥75 | 1088 (31.6) | 1283 (39.1) | 7024 (40.4) | |
| Cellulitis, No. (%) | ||||
| 18-34 | 423 (14.5) | 346 (15.3) | 2012 (14.3) | <.001 |
| 35-54 | 1079 (37.1) | 774 (34.3) | 4690 (33.4) | |
| 55-74 | 996 (34.2) | 741 (32.8) | 4745 (33.8) | |
| ≥75 | 414 (14.2) | 397 (17.6) | 2594 (18.5) | |
| Sex | ||||
| Bacterial pneumonia, No. (%) | ||||
| Female | 1910 (55.5) | 1858 (56.6) | 10 034 (57.7) | .05 |
| Male | 1529 (44.5) | 1423 (43.4) | 7364 (42.3) | |
| Cellulitis, No. (%) | ||||
| Female | 1317 (45.2) | 1044 (46.2) | 6673 (47.5) | .06 |
| Male | 1595 (54.8) | 1214 (53.8) | 7368 (52.5) | |
| Race | ||||
| Bacterial pneumonia, No. (%) | ||||
| Asian or Pacific Islander | 45 (1.3) | 87 (2.7) | 206 (1.2) | <.001 |
| Black | 830 (24.1) | 341 (10.4) | 1903 (10.9) | |
| White | 2107 (61.3) | 2222 (67.7) | 12761 (73.3) | |
| Other | 457 (13.3) | 631 (19.2) | 2528 (14.5) | |
| Cellulitis, No. (%) | ||||
| Asian or Pacific Islander | 24 (0.8) | 28 (1.2) | 92 (0.7) | <.001 |
| Black | 559 (19.2) | 178 (7.9) | 1299 (9.3) | |
| White | 1818 (62.4) | 1615 (71.5) | 10 211 (72.7) | |
| Other | 511 (17.5) | 437 (19.4) | 2439 (17.4) | |
| Ethnicity | ||||
| Bacterial pneumonia, No. (%) | ||||
| Hispanic | 752 (21.9) | 779 (23.7) | 4153 (23.9) | .04 |
| Non-Hispanic | 2687 (78.1) | 2502 (76.3) | 13 245 (76.1) | |
| Cellulitis, No. (%) | ||||
| Hispanic | 802 (27.5) | 616 (27.3) | 3984 (28.4) | .42 |
| Non-Hispanic | 2110 (72.5) | 1642 (72.7) | 10 057 (71.6) | |
| Payer | ||||
| Bacterial pneumonia, No. (%) | ||||
| Medicaid | 277 (8.1) | 193 (5.9) | 1021 (5.9) | <.001 |
| Medicare | 1757 (51.1) | 1806 (55.0) | 9339 (53.7) | |
| Military | 15 (0.4) | 23 (0.7) | 193 (1.1) | |
| Private | 732 (21.3) | 922 (28.1) | 5620 (32.3) | |
| Uninsured | 658 (19.1) | 337 (10.3) | 1225 (7.0) | |
| Cellulitis, No. (%) | ||||
| Medicaid | 189 (6.5) | 214 (9.5) | 1069 (7.6) | <.001 |
| Medicare | 929 (31.9) | 750 (33.2) | 4698 (33.5) | |
| Military | 18 (0.6) | 14 (0.6) | 126 (0.9) | |
| Private | 791 (27.2) | 792 (35.1) | 5783 (41.2) | |
| Uninsured | 985 (33.8) | 488 (21.6) | 2365 (16.8) | |
| Type of admission | ||||
| Bacterial pneumonia, No. (%) | ||||
| Emergency | 2700 (78.5) | 2859 (87.1) | 14 906 (85.7) | <.001 |
| Urgent | 671 (19.5) | 312 (9.5) | 1423 (8.2) | |
| Direct | 68 (2.0) | 110 (3.4) | 1069 (6.1) | |
| Cellulitis, No. (%) | ||||
| Emergency | 2222 (76.3) | 1806 (80.0) | 11 158 (79.5) | <.001 |
| Urgent | 610 (20.9) | 296 (13.1) | 1400 (10.0) | |
| Direct | 80 (2.7) | 156 (6.9) | 1483 (10.6) | |
| Discharge disposition | ||||
| Bacterial pneumonia, No. (%) | ||||
| Deceased | 24 (0.7) | 42 (1.3) | 206 (1.2) | <.001 |
| Home | 2637 (76.7) | 2318 (70.6) | 11 997 (69.0) | |
| Home with home health | 336 (9.8) | 291 (8.9) | 1819 (10.5) | |
| Hospice | 27 (0.8) | 55 (1.7) | 305 (1.8) | |
| Other | 145 (4.2) | 272 (8.3) | 1304 (7.5) | |
| Skilled nursing facility | 270 (7.9) | 303 (9.2) | 1767 (10.2) | |
| Cellulitis, No. (%) | ||||
| Deceased | 5 (0.2) | 2 (0.1) | 17 (0.1) | <.001 |
| Home | 2319 (79.6) | 1713 (75.9) | 10 228 (72.8) | |
| Home with home health | 294 (10.1) | 233 (10.3) | 1977 (14.1) | |
| Hospice | 6 (0.2) | 5 (0.2) | 26 (0.2) | |
| Other | 166 (5.7) | 190 (8.4) | 938 (6.7) | |
| Skilled nursing facility | 122 (4.2) | 115 (5.1) | 855 (6.1) | |
Abbreviation: NA, not applicable.
For an explanation of hospital types, see the Inclusion Criteria and Study Population subsection of the Methods section.
χ2 Tests used for comparison of categorical data and one-way analysis of variance used for comparing means.
Illness severity refers to illness severity from the Texas Inpatient Public Use Data File, which is an assignment of a severity of illness score from the All Patient Refined (APR) Diagnosis Related Group (DRG) from the 3M APR-DRG Grouper. The score indicates the extent of physiological decompensation and ranges in a discrete scale from 1 to 4 (1 = minor, 2 = moderate, 3 = major, and 4 = extreme).
Hospital-Level Comparisons
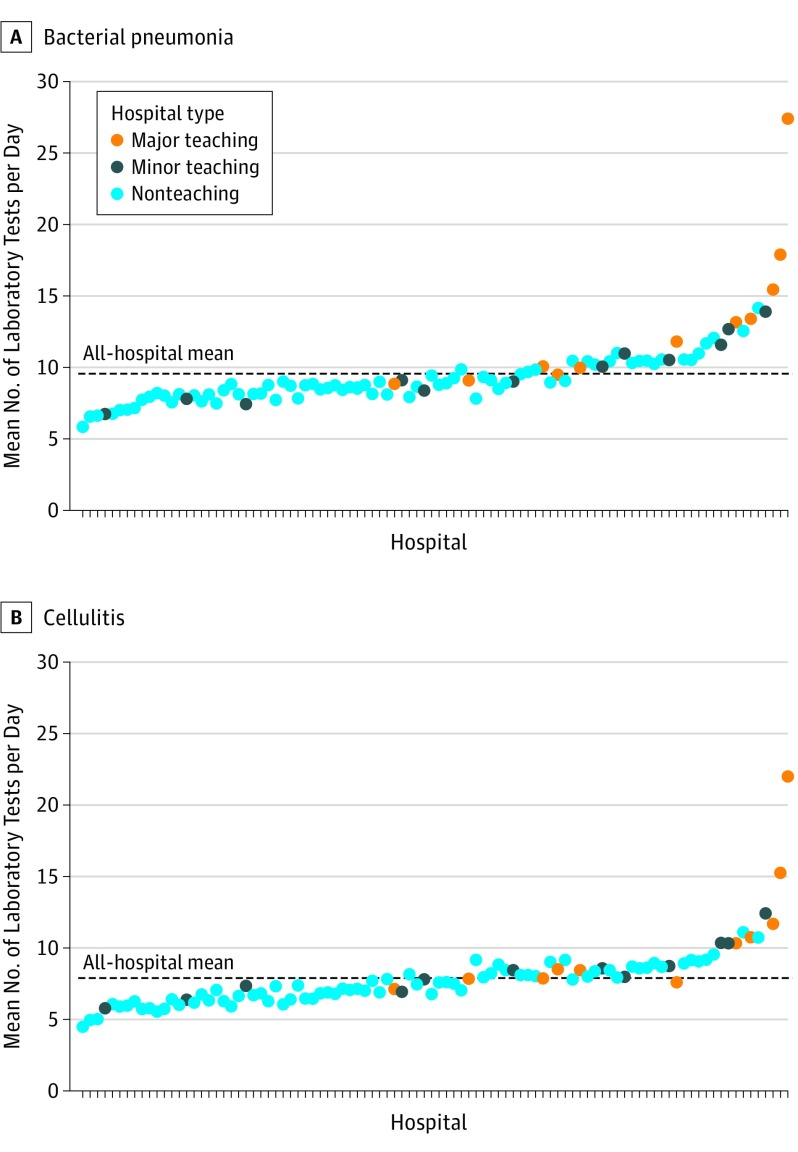
Mean number of laboratory tests per day varied significantly by hospital type and was highest for major teaching hospitals for both pneumonia and cellulitis (pneumonia: major teaching hospitals, 13.21; 95% CI, 12.91-13.51; nonteaching hospitals, 8.92; 95% CI, 8.84-9.00; P < .001; cellulitis: major teaching hospitals, 10.43; 95% CI, 10.16-10.70; nonteaching hospitals, 7.29; 95% CI, 7.22-7.36; P < .001; Table 2 and Figure 1). This association held for all levels of illness severity for both conditions, except for patients with cellulitis with an illness severity level of 4. When comparing major teaching and nonteaching hospitals, a patient with pneumonia at a major teaching hospital was estimated to receive an additional 4.29 laboratory tests per day (3.43 additional tests per day for illness severity level 1, 4.14 additional tests per day for level 2, 4.64 additional tests per day for level 3, and 3.86 additional tests per day for level 4), and a patient with cellulitis was estimated to receive an additional 3.14 laboratory tests per day (2.50 additional tests per day for illness severity level 1, 3.15 additional tests per day for level 2, and 3.63 additional tests per day for level 3). Of the 11 major teaching hospitals, 8 were above the mean number of laboratory tests performed across all hospitals for pneumonia and 7 were above the mean number of laboratory tests performed across all hospitals for cellulitis (Figure 1). Mean LOS did not vary by hospital type for either condition (Table 2). Mortality during the hospital encounter was lower at major teaching hospitals for patients with pneumonia (major teaching hospitals, 0.7%; minor teaching hospitals, 1.3%; and nonteaching hospitals, 1.2%; P = .03), but no difference in mortality was observed for patients with cellulitis (major teaching hospitals, 0.2%; minor teaching hospitals, 0.1%; and nonteaching hospitals, 0.1%; P = .68). No difference in mortality was observed for either condition when restricting to hospitalized patients with the lowest severity of illness.
Table 2. Mean Length of Stay and Mean Number of Laboratory Tests per Day.
| Characteristic | Hospital Typea | P Valueb | ||
|---|---|---|---|---|
| Major Teaching (n = 11) |
Minor Teaching (n = 12) |
Nonteaching (n = 73) |
||
| Bacterial pneumonia | ||||
| LOS, mean (SD), d (95% CI) | 3.95 (3.88-4.02) | 3.92 (3.85-3.99) | 3.91 (3.88-3.94) | .65 |
| Laboratory tests per day, mean, No. (95% CI) | 13.21 (12.91-13.51) | 9.48 (9.28-9.68) | 8.92 (8.84-9.00) | <.001 |
| Illness severity, mean, No. (95% CI)c | ||||
| 1 | 12.03 (11.17-12.89) | 9.30 (8.68-9.92) | 8.60 (8.37-8.83) | <.001 |
| 2 | 13.04 (12.58-13.50) | 9.39 (9.11-9.67) | 8.90 (8.78-9.02) | <.001 |
| 3 | 13.64 (13.18-14.10) | 9.58 (9.25-9.91) | 9.00 (8.87-9.13) | <.001 |
| 4 | 13.25 (11.88-14.62) | 10.17 (9.05-11.29) | 9.39 (8.92-9.86) | <.001 |
| Cellulitis | ||||
| LOS, mean (SD), d (95% CI) | 3.77 (3.70-3.84) | 3.71 (3.63-3.79) | 3.75 (3.72-3.78) | .51 |
| Laboratory tests per day, mean, No. (95% CI) | 10.43 (10.16-10.70) | 8.3 (8.09-8.51) | 7.29 (7.22-7.36) | <.001 |
| Illness severity, mean (95% CI)c | ||||
| 1 | 9.06 (8.60-9.52) | 7.46 (7.14-7.78) | 6.56 (6.44-6.68) | <.001 |
| 2 | 10.52 (10.15-10.89) | 8.55 (8.25-8.85) | 7.37 (7.26-7.48) | <.001 |
| 3 | 11.82 (11.16-12.48) | 9.08 (8.53-9.63) | 8.19 (8.01-8.37) | <.001 |
| 4 | 11.41 (9.62-13.20) | 9.66 (6.90-12.42) | 9.42 (8.03-10.81) | .21 |
Abbreviation: LOS, length of stay.
For an explanation of hospital types, see the Inclusion Criteria and Study Population subsection of the Methods section.
One-way analysis of variance tests were used for comparing means across hospital teaching status.
Illness severity refers to illness severity from the Texas Inpatient Public Use Data File, which is an assignment of a severity of illness score from the All Patient Refined (APR) Diagnosis Related Group (DRG) from the 3M APR-DRG Grouper. The score indicates the extent of physiological decompensation and ranges in a discrete scale from 1 to 4 (1 = minor, 2 = moderate, 3 = major, and 4 = extreme).
Figure 1. Comparison of Mean Laboratory Tests per Day by Hospital and Hospital Type.
The black dashed horizontal line represents the mean number of laboratory tests performed for bacterial pneumonia (A) and cellulitis (B) per day across all hospitals. For an explanation of hospital types, see the Inclusion Criteria and Study Population subsection of the Methods section.
When patients with hyponatremia, acute anemia, and/or acute kidney injury were removed from the analyses, mean number of laboratory tests per day remained highest at major teaching hospitals for both conditions (pneumonia: major teaching hospitals, 12.69; minor teaching hospitals, 9.35; and nonteaching hospitals, 8.71; P < .001; cellulitis: major teaching hospitals, 9.97; minor teaching hospitals, 8.15; and nonteaching hospitals, 7.02; P < .001) and across all illness severity categories (eTable 1 in the Supplement). With the removal of hospitalizations from the outlier major teaching hospital, the magnitude of the difference between hospital types decreased but still remained highest for major teaching hospitals (pneumonia: major teaching hospitals, 11.25; minor teaching hospitals, 9.48; and nonteaching hospitals, 8.92; P < .001; cellulitis: major teaching hospitals, 9.18; minor teaching hospitals, 8.30; and nonteaching hospitals, 7.29; P < .001). This pattern held across all illness severity categories and conditions, except for patients with cellulitis with an illness severity of 4 (eTable 1 in the Supplement).
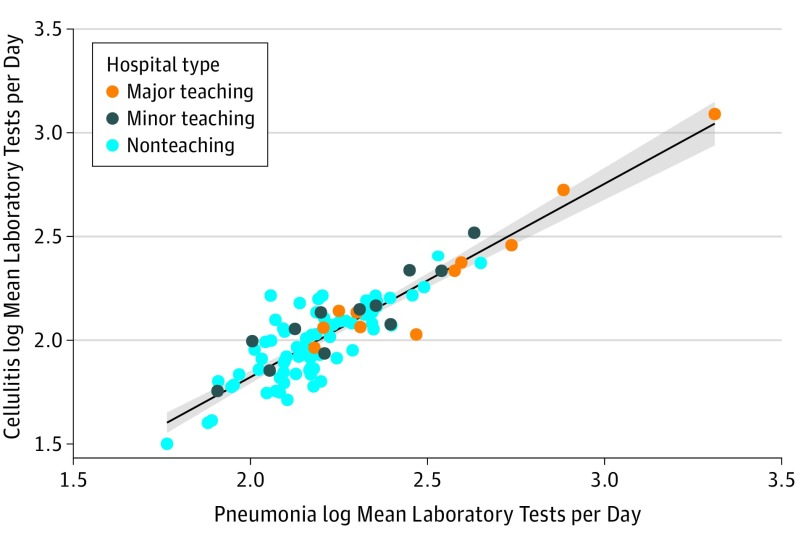
Correlation of Laboratory Test Ordering Patterns Across Conditions
There was an association between mean number of laboratory tests per day for pneumonia and cellulitis at the hospital level (r = 0.79; P < .001) (Figure 2), such that hospitals that had more laboratory tests ordered for patients with pneumonia also had more laboratory tests ordered for patients with cellulitis. There was no correlation between mean number of laboratory tests per day and mortality for either condition at the hospital level.
Figure 2. Correlation of Mean Laboratory Tests per Day for Cellulitis and Bacterial Pneumonia.
Spearman ρ correlation r = 0.79 (P < .001). The shading indicates standard error. For an explanation of hospital types, see the Inclusion Criteria and Study Population subsection of the Methods section.
Association Between Laboratory Test Ordering and Hospital Type
Generalized mixed linear regression analysis indicated an association between mean number of laboratory tests per day and major teaching hospital status for each condition when compared with nonteaching hospitals and after adjustment for patient and encounter covariates (pneumonia: relative rate, 1.40; 95% CI, 1.25-1.57; and cellulitis: RR, 1.35; 95% CI, 1.19-1.54; eTables 2 and 3 in the Supplement). There was a significant difference in the marginal effect of hospital teaching status on mean number of laboratory tests per day between major teaching and nonteaching hospitals for both conditions (difference in marginal mean number of laboratory tests per day for pneumonia, 3.58; 95% CI, 2.61-4.55; P < .001; difference in marginal mean number of laboratory tests per day for cellulitis, 2.61; 95% CI, 1.76-3.47; P < .001) (Table 3).Other factors significantly associated with increased laboratory testing varied by condition. For the cellulitis model these factors included severity of illness, LOS, age 35 to 54 years and 55 to 74 years, black race, Non-Hispanic ethnicity, uninsured patients, urgent and direct admissions, and patients discharged to home with home health care, skilled nursing facilities, and other locations when compared with the relevant reference group (eTable 2 in the Supplement). For the pneumonia model these factors included severity of illness, age, male sex, LOS, Non-Hispanic ethnicity, black and Asian or Pacific Islander race, urgent and direct admissions, and patients with a discharge disposition of deceased (eTable 3 in the Supplement).
Table 3. Comparison of Laboratory Testing Among Hospital Typesa.
| Characteristic | Marginal Effect of Hospital Teaching Status on Mean Laboratory Tests per Day, Mean (95% CI) | Difference Between Major Teaching and Nonteaching Hospital | P Value | ||
|---|---|---|---|---|---|
| Major Teaching | Minor Teaching | Nonteaching | |||
| Bacterial pneumonia | |||||
| Unadjusted | 12.78 (11.33-14.23) | 9.84 (8.77-10.91) | 9.01 (8.64-9.44) | 3.77 (2.69-4.79) | <.001 |
| Adjusted | 12.54 (11.19-13.89) | 9.70 (8.70-10.70) | 8.96 (8.58-9.34) | 3.58 (2.61-4.55) | <.001 |
| Illness severity 1 onlyb | 11.91 (10.52-13.29) | 9.23 (8.23-10.23) | 8.76 (8.36-9.16) | 3.15 (2.16-4.13) | <.001 |
| Excluding conditions requiring many laboratory tests | 12.16 (10.84-13.48) | 9.61 (8.61-10.60) | 8.72 (8.35-9.10) | 3.44 (2.49-4.38) | <.001 |
| Excluding major teaching hospital outlier | 11.56 (10.39-12.72) | 9.67 (8.77-10.54) | 8.93 (8.59-9.26) | 2.63 (1.80-3.46) | <.001 |
| Cellulitis | |||||
| Unadjusted | 10.25 (9.01-11.49) | 8.43 (7.45-9.41) | 7.43 (7.07-7.78) | 2.82 (1.94-3.71) | <.001 |
| Adjusted | 10.03 (8.83-11.24) | 8.49 (7.51-9.47) | 7.42 (7.07-7.77) | 2.61 (1.76-3.47) | <.001 |
| Illness severity 1 onlya | 8.70 (7.74-9.66) | 7.64 (6.83-8.45) | 6.64 (6.35-6.93) | 2.06 (1.39-2.73) | <.001 |
| Excluding conditions requiring many laboratory tests | 9.64 (8.48-10.80) | 8.30 (7.34-9.26) | 7.14 (6.80-7.48) | 2.50 (1.68-3.32) | <.001 |
| Excluding major teaching hospital outlier | 9.26 (8.19-10.33) | 8.46 (7.56-9.36) | 7.39 (7.07-7.71) | 1.87 (1.12-2.62) | <.001 |
For an explanation of hospital types, see the Inclusion Criteria and Study Population subsection of the Methods section.
Illness severity 1 refers to the lowest score assigned from the Texas Inpatient Public Use Data File, which is an assignment of a severity of illness score from the All Patient Refined (APR) Diagnosis Related Group (DRG) from the 3M APR-DRG Grouper. Covariates included in the generalized linear mixed-effect models included: illness severity score, length of stay, sex, age, race, ethnicity, admission type, discharge disposition, and payer. Hospital was included as a random effect. Illness severity was not included in models restricted to illness severity 1.
The results from the sensitivity analyses restricted to hospitalizations with the lowest severity of illness also indicated a significant difference in the marginal effect of teaching status on mean number of laboratory tests per day between major teaching and nonteaching hospitals for pneumonia and cellulitis (Table 3). When excluding patients with hyponatremia, acute anemia, or acute kidney injury, we obtained a similar magnitude of difference in the marginal effect of teaching status as the base model for both conditions (Table 3). Additional sensitivity analyses excluding 1 major teaching hospital outlier resulted in decreased magnitude of the marginal effect of teaching status when compared with the base model, but the marginal effect of major teaching hospital status on mean number of laboratory tests per day remained significantly higher for each condition (Table 3).
Discussion
In this cross-sectional study, patients hospitalized with 2 common conditions, pneumonia or cellulitis, at teaching hospitals had significantly more laboratory tests ordered compared with patients admitted with the same conditions to nonteaching hospitals. This association remained significant after multiple adjustments for illness severity, LOS, and patient demographics. Several sensitivity analyses also supported these findings, including removing the biggest hospital outlier from our data set and excluding patients who might have reasons for multiple laboratory tests, such as anemia, acute kidney injury, or hyponatremia. In addition, mean number of laboratory tests per day for pneumonia and cellulitis at the hospital level was highly correlated; thus, these laboratory test ordering practices are unlikely to be condition specific but rather associated with generalized practices within the training environment. These results provide evidence to support the common perception that residency training environments are associated with a culture of increased laboratory testing.
The size of the effect we discovered for each condition was approximately 3.6 additional laboratory tests per day for pneumonia and 2.6 additional laboratory tests per day for cellulitis. To illustrate this effect in a single hospital stay, consider a 42-year-old African American man with Medicaid insurance coverage who presented to the emergency department with community-acquired pneumonia, required a 4-night hospital stay, was discharged to home, and whose hospitalization was assigned an illness severity of 2. Our model estimates that if this patient were admitted to a nonteaching hospital, he would receive 10 laboratory tests per day during his hospitalization, for a total of 40 laboratory tests, whereas if he were admitted to a major teaching hospital he would receive 13 laboratory tests per day, for a total of 52 laboratory tests, which is a 30.0% increase in use of laboratory testing.
Our study used an all-payer database to examine practices across hospitals in the large state of Texas. Our results differ from those found in a study comparing test ordering by supervised residents vs attending physicians in an emergency department where resident involvement did not affect the odds of ordering blood tests. Unlike this emergency department study, our study focused on the inpatient setting and investigated laboratory testing during the course of an inpatient stay, rather than as a binary outcome showing simply whether laboratory tests were ordered or not in a given case. Another study comparing resource use for pediatric inpatients diagnosed with sepsis across hospital types found higher LOS, number of procedures, and cost for patients treated at teaching hospitals when compared with nonteaching hospitals, even after stratifying by severity of illness.
Owing to the presumption that many inpatient laboratory tests are unnecessary, there have been several previously described interventions focused on reducing laboratory testing within academic medical centers, including some specifically aimed at the ordering practices of resident physicians. Our study supports the need for further investigation of these types of efforts in training environments.
Although our study does not focus on the outcomes of patients with pneumonia and those with cellulitis across hospital types, we do have evidence that mortality for patients with pneumonia is lower at major teaching hospitals when compared with minor teaching and nonteaching hospitals. This result is supported by a recent analysis that found decreased 30-day mortality among Medicare patients at major teaching hospitals compared with nonteaching hospitals for many conditions, including patients with pneumonia. It is unlikely, although possible, that this difference in mortality could be associated with increased laboratory test ordering. Our data show no correlation between hospital-level mean number of laboratory tests per day and hospital-level encounter mortality.
Our data also show that patients with pneumonia at major teaching hospitals are sicker, perhaps leading to learned behaviors by trainees of ordering more laboratory tests. Perhaps higher rates of testing are justified for a substantial fraction of patients in teaching hospitals, but this behavior may then spill over to less acutely ill patients, such as patients with the lowest illness severity or those with less severe conditions such as cellulitis, for whom we observed no difference in mortality yet still saw a pattern of increased laboratory tests at major teaching hospitals. If this phenomenon exists it could complicate generalized efforts to reduce testing at academic medical centers and could even lead to harm if there is an overall nontargeted reduction in testing.
Limitations
Our study has some limitations. First, we relied on administrative billing data, which may not accurately capture diagnoses. Second, we measured illness severity as a score from an APR-DRG Grouper, which incorporates the severity of all diagnoses and procedures assigned to an encounter. It is possible that there are additional confounders associated with the severity of illness that are not captured. Third, we analyzed laboratory test ordering practices at the level of the hospital, so we could not truly differentiate between laboratory tests ordered by trainees vs those ordered by attending physicians or other health care professionals such as nurse practitioners or physician assistants within major teaching hospitals. Given the recent growth of services covered by non–resident physicians in many academic medical centers, this limitation may be relevant; however, the main finding that academic medical centers order significantly more tests compared with nontraining sites is still valid. In addition, our results apply only to hospitals with larger volumes of patients diagnosed primarily with pneumonia and cellulitis. The results do not apply to patients who were excluded from our analyses, including those with an abnormally long LOS, pediatric patients, and those who were admitted to an intensive care unit at any time during their hospitalization. Furthermore, the effect of teaching hospital status on laboratory test ordering behavior is variable and depends on many factors. With our current analyses, we are unable to determine the factors underlying this behavior between different hospitals. Finally, there does not seem to be good evidence measuring national rates of daily laboratory test ordering in US hospitals; thus, we are unable to confirm that our rates are representative outside of Texas.
Conclusions
Our study demonstrated that, in nearly 100 hospitals, patients with 2 common inpatient conditions who were treated in major teaching hospitals had significantly more laboratory tests per day when compared with patients seen at nonteaching hospitals, after adjusting for differences in illness severity and other patient characteristics. Future work should examine potential cultural differences between training vs nontraining environments and how these differences may contribute to increased laboratory use for conditions that do not routinely require laboratory testing.
eTable 1. Mean Length of Stay by Hospital Teaching Status and Mean Laboratory Tests Per Day By Illness Severity Category and Hospital Teaching Status for Sensitivity Analyses
eTable 2. Cellulitis Generalized Mixed Linear Regression Results for Main Adjusted Model
eTable 3. Bacterial Pneumonia Generalized Mixed Linear Regression Results for Main Adjusted Model
References
- 1.Sedrak MS, Patel MS, Ziemba JB, et al. Residents’ self-report on why they order perceived unnecessary inpatient laboratory tests. J Hosp Med. 2016;11(12):869-872. [DOI] [PubMed] [Google Scholar]
- 2.Detsky AS, Verma AA. A new model for medical education: celebrating restraint. JAMA. 2012;308(13):1329-1330. [DOI] [PubMed] [Google Scholar]
- 3.Moriates C, Shah N, Arora VM. Medical training and expensive care. Health Aff (Millwood). 2013;32(1):196. [DOI] [PubMed] [Google Scholar]
- 4.Korenstein D, Smith CD. Celebrating minimalism in residency training. JAMA Intern Med. 2014;174(10):1649-1650. [DOI] [PubMed] [Google Scholar]
- 5.Zhi M, Ding EL, Theisen-Toupal J, Whelan J, Arnaout R. The landscape of inappropriate laboratory testing: a 15-year meta-analysis. PLoS One. 2013;8(11):e78962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salisbury AC, Reid KJ, Alexander KP, et al. Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171(18):1646-1653. [DOI] [PubMed] [Google Scholar]
- 7.Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513-1516. [DOI] [PubMed] [Google Scholar]
- 8.Ellenbogen MI, Ma M, Christensen NP, Lee J, O’Leary KJ. Differences in routine laboratory ordering between a teaching service and a hospitalist service at a single academic medical center. South Med J. 2017;110(1):25-30. [DOI] [PubMed] [Google Scholar]
- 9.Khaliq AA, Huang CY, Ganti AK, Invie K, Smego RA Jr. Comparison of resource utilization and clinical outcomes between teaching and nonteaching medical services. J Hosp Med. 2007;2(3):150-157. [DOI] [PubMed] [Google Scholar]
- 10.Pitts SR, Morgan SR, Schrager JD, Berger TJ. Emergency department resource use by supervised residents vs attending physicians alone. JAMA. 2014;312(22):2394-2400. [DOI] [PubMed] [Google Scholar]
- 11.Texas Health and Human Services, Texas Department of State Health Services. Texas inpatient public use data file (PUDF). https://www.dshs.texas.gov/thcic/hospitals/Inpatientpudf.shtm. Accessed September 26, 2017.
- 12.Oud L, Watkins P. Contemporary trends of the epidemiology, clinical characteristics, and resource utilization of necrotizing fasciitis in Texas: a population-based cohort study. Crit Care Res Pract. 2015;2015:618067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Medford-Davis LN, Shah R, Kennedy D, Becker E. Factors associated with potentially preventable pediatric admissions vary by diagnosis: findings from a large state. Hosp Pediatr. 2016;6(10):595-606. [DOI] [PubMed] [Google Scholar]
- 14.Surveillance, Epidemiology, and End Results Program, National Cancer Institute, National Institutes of Health 2014 ICD-9-CM casefinding list. https://seer.cancer.gov/tools/casefinding/case2014.html. Accessed January 25, 2017.
- 15.3M Health Information Systems. Averill RF, Goldfield N, Hughes JS, et al. 3M APR DRG classification system version 26.1 (effective 10/01/2008) methodology overview. https://www.hcup-us.ahrq.gov/db/nation/nis/v261_aprdrg_meth_ovrview.pdf. Accessed July 27 2017.
- 16.Adrados M, Lajam C, Hutzler L, Slover J, Bosco J. The effect of severity of illness on total joint arthroplasty costs across New York state hospitals: an analysis of 172,738 cases. J Arthroplasty. 2015;30(1):12-14. [DOI] [PubMed] [Google Scholar]
- 17.Wang H, Johnson C, Robinson RD, et al. Roles of disease severity and post-discharge outpatient visits as predictors of hospital readmissions. BMC Health Serv Res. 2016;16(1):564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsu BS, Meyer BD, Lakhani SA. Financial, resource utilization, and mortality impacts of teaching hospital status on pediatric patients admitted for sepsis. Pediatr Infect Dis J. 2017;36(8):712-719. [DOI] [PubMed] [Google Scholar]
- 19.Wertheim BM, Aguirre AJ, Bhattacharyya RP, et al. An educational and administrative intervention to promote rational laboratory test ordering on an academic general medicine service. Am J Med. 2017;130(1):47-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vidyarthi AR, Hamill T, Green AL, Rosenbluth G, Baron RB. Changing resident test ordering behavior: a multilevel intervention to decrease laboratory utilization at an academic medical center. Am J Med Qual. 2015;30(1):81-87. [DOI] [PubMed] [Google Scholar]
- 21.Melendez-Rosado J, Thompson KM, Cowdell JC, et al. Reducing unnecessary testing: an intervention to improve resident ordering practices. Postgrad Med J. 2017;93(1102):476-479. [DOI] [PubMed] [Google Scholar]
- 22.Wheeler D, Marcus P, Nguyen J, et al. Evaluation of a resident-led project to decrease phlebotomy rates in the hospital: think twice, stick once. JAMA Intern Med. 2016;176(5):708-710. [DOI] [PubMed] [Google Scholar]
- 23.Burke LG, Frakt AB, Khullar D, Orav EJ, Jha AK. Association between teaching status and mortality in US hospitals. JAMA. 2017;317(20):2105-2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Mean Length of Stay by Hospital Teaching Status and Mean Laboratory Tests Per Day By Illness Severity Category and Hospital Teaching Status for Sensitivity Analyses
eTable 2. Cellulitis Generalized Mixed Linear Regression Results for Main Adjusted Model
eTable 3. Bacterial Pneumonia Generalized Mixed Linear Regression Results for Main Adjusted Model