This randomized clinical trial aims to identify measures with sufficient effect size and cross-site reliability to serve as glutamatergic target engagement biomarkers within early-phase clinical studies.
Key Points
Question
Can imaging-based biomarkers be used for glutamatergic drug development in psychiatry?
Findings
In this randomized clinical trial including 53 volunteers, a direct comparison of 3 proposed neuroimaging-based target engagement biomarkers for glutamatergic treatment development in the context of a multicenter ketamine challenge study was performed. Significant ketamine effects were observed for the ketamine-evoked changes in the functional magnetic imaging blood oxygen level–dependent (BOLD) response, with lesser degrees of change for magnetic resonance spectroscopy and task-based BOLD responses.
Meaning
This trial validates the ketamine-evoked increases in functional magnetic imaging BOLD response as a cross-site biomarker for glutamatergic drug development in schizophrenia.
Abstract
Importance
Despite strong theoretical rationale and preclinical evidence, several glutamate-targeted treatments for schizophrenia have failed in recent pivotal trials, prompting questions as to target validity, compound inadequacy, or lack of target engagement. A key limitation for glutamate-based treatment development is the lack of functional target-engagement biomarkers for translation between preclinical and early-stage clinical studies. We evaluated the utility of 3 potential biomarkers—ketamine-evoked changes in the functional magnetic imaging (fMRI) blood oxygen level–dependent response (pharmacoBOLD), glutamate proton magnetic resonance spectroscopy (1H MRS), and task-based fMRI—for detecting ketamine-related alterations in brain glutamate.
Objective
To identify measures with sufficient effect size and cross-site reliability to serve as glutamatergic target engagement biomarkers within early-phase clinical studies.
Design, Setting, and Participants
This randomized clinical trial was conducted at an academic research institution between May 2014 and October 2015 as part of the National Institute of Mental Health–funded Fast-Fail Trial for Psychotic Spectrum Disorders project. All raters were blinded to study group. Healthy volunteers aged 18 to 55 years of either sex and free of significant medical or psychiatric history were recruited from 3 sites. Data were analyzed between November 2015 and December 2016.
Interventions
Volunteers received either sequential ketamine (0.23 mg/kg infusion over 1 minute followed by 0.58 mg/kg/h infusion over 30 minutes and then 0.29 mg/kg/h infusion over 29 minutes) or placebo infusions.
Main Outcomes and Measures
Ketamine-induced changes in pharmacoBOLD, 1H MRS, and task-based fMRI measures, along with symptom ratings. Measures were prespecified prior to data collection.
Results
Of the 65 volunteers, 41 (63%) were male, and the mean (SD) age was 31.1 (9.6) years; 59 (91%) had at least 1 valid scan. A total of 53 volunteers (82%) completed both ketamine infusions. In pharmacoBOLD, a highly robust increase (Cohen d = 5.4; P < .001) in fMRI response was observed, with a consistent response across sites. A smaller but significant signal (Cohen d = 0.64; P = .04) was also observed in 1H MRS–determined levels of glutamate+glutamine immediately following ketamine infusion. By contrast, no significant differences in task-activated fMRI responses were found between groups.
Conclusions and Relevance
These findings demonstrate robust effects of ketamine on pharmacoBOLD across sites, supporting its utility for definitive assessment of functional target engagement. Other measures, while sensitive to ketamine effects, were not sufficiently robust for use as cross-site target engagement measures.
Trial Registration
clinicaltrials.gov Identifier: NCT02134951
Introduction
All currently approved treatments for schizophrenia, including both typical and atypical antipsychotics, function primarily by blocking dopamine D2 receptors. Nevertheless, these compounds are fully effective for only a minority of individuals with schizophrenia, indicating the need for alternative treatment approaches. Recent theories implicate dysfunction of brain glutamatergic systems in general and of neurotransmission mediated by N-methyl-D-aspartate-type glutamate receptors (NMDAR) in particular. This latter theory is based on the ability of phencyclidine, ketamine, MK-801 (dizocilpine), or other NMDAR antagonists to induce clinical symptoms and neurocognitive dysfunction closely resembling those of schizophrenia. In rodent studies, effects of NMDAR antagonists such as ketamine are mediated, at least in part, by stimulation of presynaptic glutamate release in frontal brain regions and are reversed by compounds acting either to enhance postsynaptic NMDAR function or to diminish presynaptic glutamate release, which either reverse the primary deficit in NMDAR dysfunction or block the NMDAR antagonist–induced increase in presynaptic glutamate release.
Nevertheless, a major limitation to glutamate-targeted treatment development is the lack of appropriate biomarkers to evaluate this effect in early-stage clinical trials to confirm target engagement. The present study evaluates 3 potential biomarkers of functional target engagement by ketamine, reversal or blockade of which would serve as functional evidence of a brain effect of novel glutamatergic agents in schizophrenia. The biomarkers include ketamine-evoked changes in (1) the functional magnetic imaging (fMRI) blood oxygen level–dependent (BOLD) response (pharmacoBOLD), (2) glutamate proton magnetic resonance (1H MRS) spectroscopy, and (3) task-based fMRI. Our primary goal was to identify biomarkers with a magnitude of effect at least equivalent to that observed in rodent studies (eg, z > 2.3), which successfully detected effects of metabotropic glutamate receptors (mGluR) 2 and 3 agonists in animal models.
The first approach, pharmacoBOLD, leverages effects of glutamate on brain energy metabolism. During normal brain homeostasis, recycling of glutamate released from presynaptic glutamatergic terminals accounts for approximately 50% of energy expenditure. In animals, NMDAR antagonist–induced increases in glutamate release are accompanied by increased local metabolism and cerebral blood volume that reflect increased energy expenditure. These effects are prevented along with NMDAR antagonist–induced behaviors by compounds that block presynaptic glutamate release, such as lamotrigine or mGluR2/3 agonists. Compared with ketamine, dopaminergic agents, such as methylphenidate, have limited effect on cerebral blood volume in adults. In fMRI, increases in regional metabolism are associated with increased local blood flow and BOLD signal. Here, we evaluated these effects compared with placebo in a multicenter trial setting.
Second, we evaluated effects of ketamine on the local concentration of glutamate and metabolites determined using 1H MRS. In 1H MRS, the concentration of glutamate, glutamine, or glutamate+glutamine (Glx) can be measured directly. Prior studies have shown dysregulated glutamate release in the medial prefrontal or anterior cingulate cortex in patients diagnosed as having acutely psychotic, unmedicated schizophrenia, as well as those at high clinical risk. Elevated cingulate glutamate levels may also persist throughout later stages of illness in individuals who are antipsychotic resistant but not in those who are antipsychotic responsive and correlate with common allelic variants in glutamate-related risk genes. Several small studies have also shown ketamine-induced alterations in brain glutamate metabolism in the medial prefrontal or anterior cingulate cortex in healthy volunteers, but to our knowledge, the consistency of these findings in cross-site studies has not been evaluated.
Finally, we examined the effect of ketamine on functional activations observed during the Relational and Item-Specific Encoding (RISE) task, which is known to the engage dorsolateral prefrontal cortex (DLPFC) and hippocampal regions involved in long-term memory. Patients diagnosed as having schizophrenia show reduced DLPFC BOLD and hippocampus activation during relational encoding, suggesting task-based fMRI readouts involving DLPFC or hippocampus involvement during the RISE task might serve as biomarkers as well.
The primary goal of the study was to compare both the magnitude of response and feasibility of implementation of imaging-based biomarkers for glutamate-targeted drug development in psychotic disorders across measures within the context of a multicenter clinical trial as a method for validating a biomarker for future early-stage glutamatergic drug development in schizophrenia. In general, we hypothesized that ketamine effects would be in the direction observed in both animal studies with NMDAR antagonists and in schizophrenia—ie, toward increased BOLD response, increased 1H-MRS Glx levels, and reduced activation during the RISE task.
Methods
Participants
The study was approved by the Yale University Institutional Review Board, the University of California, Davis Institutional Review Board, and the New York State Psychiatric Institute Institutional Review Board. Written informed consent was obtained from all participants prior to participation. The trial protocol can be found in Supplement 1. Volunteers were medically healthy men and women aged 18 to 55 years without current or past Axis I or II psychiatric or substance history, as detailed in the eMethods in Supplement 2.
Design
Participants were randomized to ketamine or placebo in a 2:1 ratio. Volunteers participated in 2 magnetic resonance imaging sessions at least 2 weeks apart, with the first magnetic resonance imaging session always being 1H MRS only and the second session incorporating both pharmacoBOLD and task-based fMRI. In the 1H MRS session, an initial structural scan was conducted for voxel placement. Anterior cingulate cortex Glx levels were then obtained in 15-minute blocks starting 30 minutes prior to infusion (2 blocks) and continuing until the end of the 1-hour infusion (4 blocks). Participants maintained their blinded group assignment across scanning sessions.
Ketamine/Placebo Infusion
Racemic ketamine hydrochloride (0.23 mg/kg infusion over 1 minute followed by 0.58 mg/kg/h infusion over 30 minutes and then 0.29 mg/kg/h infusion over 29 minutes) or placebo (normal saline) was administered.
Clinical and Safety Measures
Participants were rated with the Brief Psychiatric Rating Scale (BPRS), Profile of Mood States (POMS), and Clinician Administered Dissociative States Scale (CADSS) tests as well as the Psychotomimetic States Inventory after the scanning period ended.
Imaging Methods
Detailed imaging methods are provided in the eMethods in Supplement 2. Briefly, for pharmacoBOLD, T2-weighted echo-planar imaging scans were collected for 10 minutes prior to and during each ketamine infusion, with a repetition time of 2 seconds and with 32 slices at a resolution of 3.4 × 3.4 × 4.0 mm. A prespecified region of interest analysis was performed using the midcingulate cortex. In addition, an exploratory whole-brain analysis was performed using multiple linear regression. Voxel-wise thresholds were set at P < .05 and were corrected for multiple comparisons using gaussian random field theory (P < .05).
For 1H MRS, the region of interest was placed in the medial prefrontal cortex anterior to the genu of the corpus callosum, oriented along the anterior commissure–posterior commissure line, and centered on the interhemispheric fissure, with dimensions 2.5 × 3.0 × 2.5 cm (volume, 18.8 cm3). The MRS acquisition used a standard point-resolved spectroscopy pulse sequence (repetition time/echo time = 2000/80 milliseconds) with 336 excitations. Four acquisitions (15 minutes each) were conducted over the 1-hour infusion period and compared with the preinfusion baseline. For data analysis, 8-channel phased-array coil data were combined into a single regular time-domain free-induction decay signal, using the unsuppressed voxel tissue water signal to derive the relative phased-array coil sensitivities. The primary outcome measure consisted of the pre/post ketamine change score for the Glx to creatinine ratio.
The RISE task was implemented in accordance with Ragland et al. Briefly, participants viewed a series of visual depictions of objects during either an item-specific or relational encoding phase (eMethods in Supplement 2). The predesignated primary outcome measure was DLPFC BOLD activation during the task.
Group-level contrasts were made for encoding (relational minus item-specific), item recognition (hits minus misses for item-specific and hits minus misses for relational encoding), and associative recognition (hits minus misses). Structural masks from the WFU_PickAtlas were used to restrict analyses to subgroups of activated voxels within left and right DLPFC (Brodmann areas 9, 46, and 9/46). Secondary analysis assessed hippocampal effects.
Statistical Analysis
The ketamine effect on pharmacoBOLD and the RISE task were tested using a 2-sample t test (ketamine vs placebo). Ketamine effects on the 1H MRS response measures were tested with repeated-measures analysis of variance of the Glx responses across time during the infusion with 4 time intervals (0-15, 15-30, 30-45, and 45-60 minutes), treatment group, and time × treatment group with post hoc contrasts. Across-site differences in each biomarker outcome were tested using an analysis of variance, with treatment, site, and treatment × site as fixed effects.
Ketamine effects on clinical measurements (ie, BPRS, POMS, and CADSS measures) were assessed using change score measures (postinfusion minus preinfusion scores), except for the Psychotomimetic States Inventory measure, which was only collected after ketamine infusion. Associations among biomarker responses, clinical measures, and blood levels of ketamine and metabolites were assessed using Spearman correlations. Ratings on clinical measures were averaged across the 2 days for associations with biomarkers, and blood levels were taken from the specific day. Finally, logistic regression was used to model the odds of assignment to the ketamine group on the main response measures. The optimal cut points for sensitivity and specificity were selected using Youden J statistic (sensitivity + specificity − 1).
Between-group analyses were conducted using t tests. Effect sizes were assessed using the Cohen d statistic. Correlations between variables were assessed using nonparametric (Spearman) correlations. Values in the text are means and standard deviations unless indicated otherwise. All P values were 2-tailed, and significance was set at P < .05.
Results
Sample
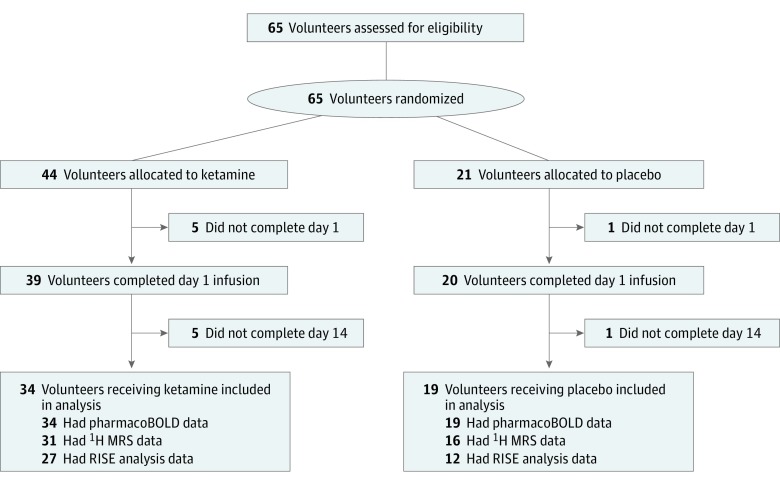
Sixty-five participants were randomized (Figure 1). The mean (SD) age was 31.1 (9.6) years and was similar across groups. No serious or unexpected adverse events were reported in the study.
Figure 1. CONSORT Diagram.
1H MRS indicates glutamate proton magnetic resonance spectroscopy; pharmacoBOLD, functional magnetic imaging blood oxygen level–dependent response.
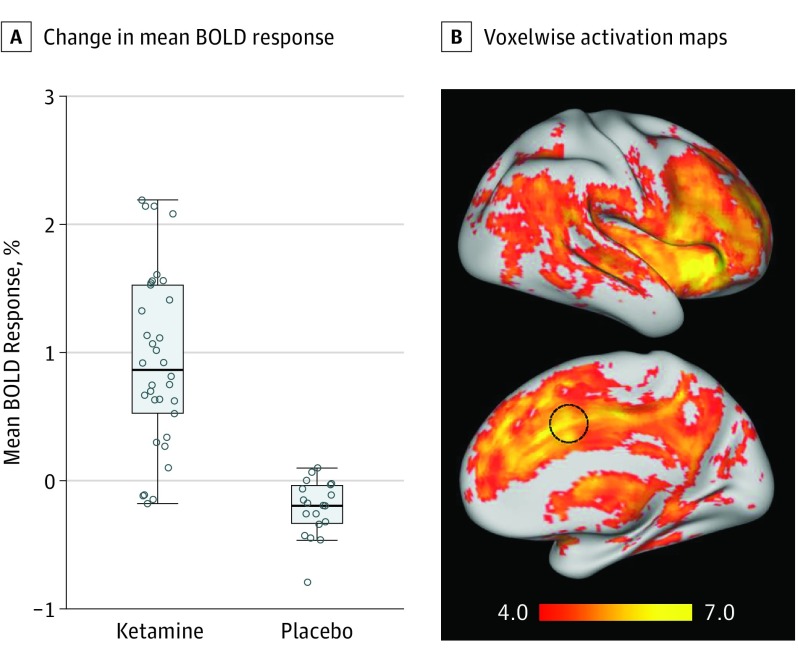
PharmacoBOLD
The mean ketamine-evoked response in the dorsal midcingulate cortex showed a very large effect size (t49 = 7.18; Cohen d = 5.4; P < .001) (Table 1) (Figure 2A), with no significant difference across treatment sites (F2,50 = 0.31; within-site effect size range, 4.6-5.6; P = .73). A voxelwise analysis (P < .05) demonstrated that most of the cortex was activated by ketamine administration (Figure 2B); only the orbitofrontal cortex did not show a positive BOLD response. The largest activations (z > 6) were found primarily in the dorsal anterior cingulate cortex (Montreal Neurological Institute brain atlas region 4, 22, and 32) and anterior insula (Montreal Neurological Institute brain atlas region 38, 28, 0; −32, −28, −2).
Table 1. Biomarker Results.
| Measure | Mean (SE) | Cohen da | P Value | |
|---|---|---|---|---|
| Ketamine | Placebo | |||
| Resting BOLD response | ||||
| No. of volunteers | 34 | 19 | NA | NA |
| Mean amplitude | 0.91 (0.10) | −0.27 (0.14) | 5.4 | <.001 |
| Glxb | ||||
| No. of volunteers | 31 | 16 | NA | NA |
| 0-15 min | 0.015 (0.002) | 0.007 (0.003) | 0.64 | .04 |
| 15-30 min | 0.009 (0.002) | 0.012 (0.003) | −0.22 | .47 |
| 30-45 min | 0.011 (0.002) | 0.010 (0.003) | 0.04 | .89 |
| 45-60 min | 0.014 (0.002) | 0.017 (0.003) | −0.17 | .57 |
| RISE task | ||||
| No. of volunteers | 27 | 12 | NA | NA |
| Discriminability index (d′) | −0.15 (0.10) | −0.10 (0.16) | −0.11 | .77 |
| Left DLPFC activation, overall | −1.12 (1.37) | 2.24 (2.06) | −0.42 | .18 |
| Left DLPFC activation, relational item | −1.69 (1.94) | 5.01 (2.91) | −0.79 | .06 |
| Right hippocampus hit miss | −0.53 (0.58) | −0.71 (0.90) | 0.08 | .87 |
Abbreviations: BOLD, blood oxygen level–dependent; DLPFC, dorsolateral prefrontal cortex; Glx, glutamate+glutamine; NA, not applicable; RISE, Relational and Item-Specific Encoding.
Cohen d calculated as difference in means divided by standard deviation of the placebo group.
Change in Glx level to creatine ratio relative to baseline acquisition.
Figure 2. Ketamine-Evoked Changes in the Functional Magnetic Imaging Blood Oxygen Level–Dependent (BOLD) Response.
A, Change in mean BOLD response following ketamine administration in the predefined region of interest (dorsal midcingulate cortex) (Cohen d = 5.4; P < .001). Each point represents an individual participant. The box indicates the 25th and 75th percentiles; the line, the median value; error bars, the data range excluding outliers. B, Voxelwise activation maps. Peak activations were located in the dorsal anterior cingulate cortex, insula, and thalamus. z Statistic maps were thresholded at z > 4.0. The circle indicates the region of interest used for primary analysis.
1H MRS
A moderate effect size in between-group difference in acute Glx level increase was noted within the first 15-minute interval following ketamine administration (t126 = 2.09; Cohen d = 0.64; P = .04) (Figure 3) (Table 1). However, no significant between-group differences were seen after the first acquisition, leading to statistically similar increases in Glx levels across the remaining 45 minutes of the infusion period and a nonsignificant group difference across the entire infusion period (F3,126 = 1.54; P = .21). There was not a significant difference in ketamine effects by site (F3,114 = 2.51; P = .06).
Figure 3. Magnetic Resonance Spectroscopy Response.
Change in glutamate+glutamine (Glx) to creatine ratio within the anterior cingulate cortex following ketamine vs the preinfusion baseline by glutamate proton magnetic resonance spectroscopy. The difference was significant (Cohen d = 0.64; P = .04) for the first 15-minute interval but was not significant for other intervals.
RISE Task
No significant behavioral difference was seen between groups in the a priori analysis of change in the discriminability index (d′) of item recognition following relational encoding (t37 = 0.30; Cohen d = −0.11; P = .77). Also, no significant effect in activation was detected in the DLPFC during the task (t37 = 1.36; Cohen d = −0.42; P = .18). However, a strong group × site interaction was observed (P = .005), reflecting both significant and nonsignificant (P range, .03-.12) but opposite direction tendencies across the sites. Similarly, there was no significant activation effect in the hippocampus (t35 = 0.16; Cohen d = 0.08; P = .87).
Clinical Ratings
As expected, large effect size and between-group differences were seen for all behavioral scales (Table 2). On BPRS, only the positive subscale showed significant changes. Similar changes in clinical ratings were seen in the ketamine group on days 1 and 14 for all clinical measures except the CADSS, which was significantly higher on day 1.
Table 2. Clinical Symptoms.
| Variable (Range) | Difference (Preinfusion vs Postinfusion), Mean (SD) | Difference, Mean (SE) | Cohen da | P Value | |
|---|---|---|---|---|---|
| Ketamine | Placebo | ||||
| Day 1 | |||||
| No. of volunteers | 44 | 21 | NA | NA | NA |
| POMS total (0-260) | 13.89 (17.76) | −0.93 (7.29) | 14.81 (5.60) | 2.03 | .01 |
| BPRS | |||||
| Total (19-133) | 4.59 (5.07) | 0.96 (1.24) | 3.63 (1.09) | 2.93 | .001 |
| Positive (4-28) | 2.16 (2.07) | 0.21 (0.46) | 1.95 (0.44) | 4.24 | <.001 |
| Negative (3-21) | 0.46 (1.02) | 0.14 (0.31) | 0.32 (0.21) | 1.03 | .14 |
| Activation (3-21) | 0.49 (1.21) | 0.11 (0.38) | 0.38 (0.27) | 1.01 | .16 |
| Hostility (4-28) | 0.33 (0.75) | 0.07 (0.36) | 0.26 (0.16) | 0.72 | .12 |
| CADSS total (0-92) | 14.21 (13.14) | 2.25 (2.43) | 11.95 (2.84) | 4.92 | <.001 |
| PSIb (0-144) | 20.18 (12.10) | 8.17 (4.28) | 12.00 (4.59) | 2.80 | .01 |
| Day 14 | |||||
| No. of volunteers | 34 | 19 | NA | NA | NA |
| POMS total (0-260) | 12.40 (14.22) | 4.45 (5.88) | 7.95 (3.44) | 1.35 | .02 |
| BPRS | |||||
| Total (19-133) | 3.12 (5.50) | 0.28 (1.11) | 2.84 (1.25) | 2.56 | .03 |
| Positive (4-28) | 1.41 (2.07) | 0.13 (0.40) | 1.29 (0.48) | 3.23 | .01 |
| Negative (3-21) | 0.47 (1.14) | 0.13 (0.32) | 0.34 (0.27) | 1.06 | .20 |
| Activation (3-21) | 0.43 (1.31) | 0.02 (0.47) | 0.41 (0.31) | 0.87 | .20 |
| Hostility (4-28) | 0.06 (0.75) | 0.06 (0.47) | 0.004 (0.18) | 0.01 | .98 |
| CADSS total (0-92) | 7.75 (8.12) | 1.72 (2.07) | 6.03 (1.90) | 2.91 | .003 |
| PSIb (0-144) | 15.58 (8.80) | 7.67 (4.69) | 7.91 (3.48) | 1.69 | .03 |
Abbreviations: BPRS, Brief Psychiatric Rating Scale; CADSS, Clinician Administered Dissociative States Scale; NA, not applicable; POMS, Profile of Mood States; PSI, Psychotomimetic States Inventory.
Cohen d calculated as difference in means divided by standard deviation of the placebo group.
PSI has only postinfusion measure; hence, means are the mean of postinfusion, not change scores.
Ketamine Level
Levels of ketamine, norketamine, and dehydronorketamine were obtained after the volunteers were removed from the scanner. Similar changes were seen on days 1 and 14 for ketamine (mean [SD] ng/mL, 108.5 [33.0] vs 111.9 [31.0]; t30 = 1.59; P = .12) and dehydronorketamine (mean [SD] ng/mL, 53.7 [16.2] vs 67.0 [19.1]; t30 = 1.57; P = .13). For norketamine, significantly lower levels were observed on day 1 vs day 14 (mean [SD] ng/mL, 28.2 [15.8] vs 33.4 [22.5]; t30 = 3.35; P = .002).
There were no significant associations with same-day ketamine levels for any of the primary outcome variables. There were also no significant associations between any of the primary outcome variables and levels of either norketamine or dehydronorketamine.
Relationship With Symptom Measures
Correlational analyses were conducted both across groups and within the ketamine group individually. Across groups, significant associations were seen between pharmacoBOLD increases and changes in the Psychotomimetic States Inventory score (rs = 0.37; P = .007), BPRS (rs = 0.43; P = .001), CADSS (rs = 0.56; P < .001), and POMS (rs = 0.30; P = .03) (eTable in Supplement 2). However, associations were not significant within the ketamine treatment group. If across-group correlations were corrected for multiple comparisons, the association with POMS would no longer be significant.
In contrast to pharmacoBOLD, no significant changes were observed for 1H MRS Glx levels relative to symptoms. By contrast, left DLPFC activation to relational encoding items was significantly associated with both BPRS negative symptoms (rs = 0.43; P = .03) and in ketamine-treated individuals alone (rs = 0.46; P = .02). No significant changes were observed for hippocampal activation relative to symptoms.
Group Assignment
A final analysis evaluated the degree to which the proposed biomarkers could be used to predict group membership (ketamine vs placebo group). As expected, pharmacoBOLD response (χ2 = 12.9; P < .001) significantly differentiated the groups, with sensitivity of 85.3% and specificity of 89.5%. Left DLPFC activation on the RISE task, despite absence of significant between-group difference, significantly predicted group membership (χ2 = 6.18; P = .01), with relatively high specificity (83.3%) relative to sensitivity (48.1%). Despite the significant between-group differences, Glx levels did not significantly predict group membership. A combined measure of pharmacoBOLD+RISE activation was highly predictive, with 90% sensitivity and 88.9% specificity, leading to correct classification of 90% of participants. For pharmacoBOLD, a cutoff value of 0.5% increase in BOLD signal eliminated all placebo responders while retaining 80% of ketamine responders.
Discussion
Most psychiatric drugs in clinical use derive from serendipitous discoveries that were then reverse engineered to develop comparable or incrementally improved medications. Although there have been dramatic increases in the pathophysiological understanding of disorders, such as schizophrenia, these have not yet translated into innovations in pharmacotherapeutics or enhanced therapeutic outcome. One of the major obstacles to developing novel neurotherapeutic agents at present is the limited availability of validated biomarkers to establish a dose that reaches the desired target in the brain and produces some functional effect that may lead to a therapeutic response. There is a critical absence of validated biomarkers in the case of glutamate-targeted treatments, which are presumed to work at least in part by modulation of presynaptic glutamate release. Ideal biomarkers not only have large associated magnitudes of effect but also have high translatability across sites, permitting use in multicenter clinical trials.
The present study evaluated 3 potential biomarkers of glutamate-based functional target engagement—pharmacoBOLD, 1H MRS Glx, and task-based fMRI (RISE task)—based on their sensitivity to ketamine administration in healthy volunteers. Critical issues include magnitude of effect and feasibility for cross-site implementation. Although each measure has been studied in isolation, to our knowledge, this is the first study to investigate them in parallel in the same sample in a rigorously designed, randomized, placebo-controlled, blinded, multisite investigation.
The primary finding is that the pharmacoBOLD results were very robust, with both a large magnitude of effect (Cohen d = 5.4) and strong cross-site consistency, suggesting its potential as a biomarker durable enough to be applied in multicenter studies, provided that adequate quality control, methodology, and minimum-capability 3-T magnetic resonance imaging systems from one of the major vendors (ie, Siemens, GE, or Philips) are used. Other measures provided complementary findings and may possess additional biomarker utility, depending on the therapeutic target and experimental compound.
An important feature of the pharmacoBOLD measure is that it recapitulates the effects of NMDAR antagonists in rodents, where acute administration of NMDAR antagonists increases blood flow, as measured by cerebral blood volume. Effects are reversed by glutamatergic agents, such as mGluR2/3 receptor agonists, and NMDAR glycine-site modulators, such as D-serine or glycine transport inhibitors, as well as atypical antipsychotics, such as clozapine. Therefore, the pharmacoBOLD biomarker may be particularly relevant to developing mGluR2/3 and NMDAR modulator–type compounds, establishing appropriate doses, and implementing experimental medicine type drug development principles.
In the present study, effect sizes for the pharmacoBOLD response were larger than those noted in prior studies using this approach, which have generally been in the range of 2.0 to 3.0 SD units. The larger effect size is likely because of the greater infusion of ketamine given (0.23 mg/kg) vs prior studies (0.1 mg/kg). As in prior studies, the BOLD response peaked within the first 5 minutes and was likely driven by the initial infusion, suggesting that sustained ketamine infusion is likely not required. In the present study, a cutoff value of 0.5% mean signal change fully separated individuals receiving ketamine from placebo and could be used in target engagement-type studies to maximize power to detect a significant medication effect.
The pharmacoBOLD response was also significantly associated with symptoms across but not within groups. This finding may reflect nonlinear relationships between pharmacoBOLD measures and psychosis within the ketamine group, such as saturation of the pharmacoBOLD response at high levels, as well as threshold levels needed to induce symptoms. Additionally, symptom ratings were not obtained until the end of the scan session, potentially weakening the associations. The pharmacoBOLD response was highly significant despite being obtained in the second scan, raising the possibility that even greater results and potentially stronger correlations with behavior might have been obtained if no prior scan was performed. In prior studies, high test-retest reliability of the pharmacoBOLD response has been observed across administrations.
In contrast to the pharmacoBOLD response, Glx levels measured by 1H MRS showed much smaller, albeit significant, effect-size differences between treatments (Cohen d = 0.64; P = .04). The lower sensitivity of 1H MRS to ketamine effects may reflect difficulties in distinguishing synaptic from extrasynaptic glutamate.
Finally, effects of task-based fMRI in this study were less robust than those of pharmacoBOLD. Nevertheless, a moderate to large effect size difference in left DLPFC activation in response to relational items was observed (Cohen d = −0.42; P = .06). These changes also correlated with severity of ketamine-induced negative symptoms, both across treatment groups (r = 0.36; P = .03) and in the ketamine group itself (r = 0.43; P = .03).
Changes in left DLPFC activation also contributed to the differentiation of ketamine and placebo treatment groups over and above contributions of pharmacoBOLD. In particular, changes were highly specific to the ketamine group, albeit with relatively low sensitivity. Ketamine is also known to affect other NMDAR-dependent functions, such as working memory, smooth pursuit eye movement, and auditory information processing. Therefore, the combination of task-based measures with pharmacoBOLD may help refine the biomarker algorithm.
Limitations
Our study has limitations. We selected a single sequence—point-resolved spectroscopy echo time 80 acquisition with linear combination model difference method analysis—that could be reliably implemented at each of the sites. It is possible that alternative 1H MRS approaches might have yielded stronger results. A nonsignificant (P = .06) site-to-site variability was observed even with the consensus sequence and might be exacerbated by site-specific measurement protocols.
Conclusions
One of the major hurdles to neuroscience-based treatment development in psychiatry is the lack of appropriate functional target engagement measures. The present cross-site, randomized trial demonstrates that ketamine-induced pharmacoBOLD provides a robust and reliable measure of excess cortical glutamate release and may therefore serve as an informative measure for the development of novel glutamate-targeted therapeutic agents. The study also supports the potential utility of MRS and task-based fMRI, pending appropriate method refinements, and enables future target-engagement based research for development of glutamatergic medications in schizophrenia.
Trial protocol.
eMethods.
eTable. Correlations between biomarkers and ketamine-induced symptoms.
References
- 1.Leucht S, Cipriani A, Spineli L, et al. . Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382(9896):951-962. [DOI] [PubMed] [Google Scholar]
- 2.Kapur S, Remington G. Dopamine D(2) receptors and their role in atypical antipsychotic action: still necessary and may even be sufficient. Biol Psychiatry. 2001;50(11):873-883. [DOI] [PubMed] [Google Scholar]
- 3.Kahn RS, Fleischhacker WW, Boter H, et al. ; EUFEST study group . Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial. Lancet. 2008;371(9618):1085-1097. [DOI] [PubMed] [Google Scholar]
- 4.Lieberman JA, Stroup TS, McEvoy JP, et al. ; Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators . Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209-1223. [DOI] [PubMed] [Google Scholar]
- 5.Javitt DC, Zukin SR. Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry. 1991;148(10):1301-1308. [DOI] [PubMed] [Google Scholar]
- 6.Krystal JH, Karper LP, Seibyl JP, et al. . Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans: psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry. 1994;51(3):199-214. [DOI] [PubMed] [Google Scholar]
- 7.Coyle JT. NMDA receptor and schizophrenia: a brief history. Schizophr Bull. 2012;38(5):920-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moghaddam B, Adams B, Verma A, Daly D. Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. J Neurosci. 1997;17(8):2921-2927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moghaddam B, Adams BW. Reversal of phencyclidine effects by a group II metabotropic glutamate receptor agonist in rats. Science. 1998;281(5381):1349-1352. [DOI] [PubMed] [Google Scholar]
- 10.Moghaddam B, Krystal JH. Capturing the angel in “angel dust”: twenty years of translational neuroscience studies of NMDA receptor antagonists in animals and humans. Schizophr Bull. 2012;38(5):942-949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gozzi A, Large CH, Schwarz A, Bertani S, Crestan V, Bifone A. Differential effects of antipsychotic and glutamatergic agents on the phMRI response to phencyclidine. Neuropsychopharmacology. 2008;33(7):1690-1703. [DOI] [PubMed] [Google Scholar]
- 12.Paul SM, Mytelka DS, Dunwiddie CT, et al. . How to improve R&D productivity: the pharmaceutical industry’s grand challenge. Nat Rev Drug Discov. 2010;9(3):203-214. [DOI] [PubMed] [Google Scholar]
- 13.Javitt DC, Schoepp D, Kalivas PW, et al. . Translating glutamate: from pathophysiology to treatment. Sci Transl Med. 2011;3(102):102mr2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rothman DL, De Feyter HM, de Graaf RA, Mason GF, Behar KL. 13C MRS studies of neuroenergetics and neurotransmitter cycling in humans. NMR Biomed. 2011;24(8):943-957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schobel SA, Chaudhury NH, Khan UA, et al. . Imaging patients with psychosis and a mouse model establishes a spreading pattern of hippocampal dysfunction and implicates glutamate as a driver. Neuron. 2013;78(1):81-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lorrain DS, Baccei CS, Bristow LJ, Anderson JJ, Varney MA. Effects of ketamine and N-methyl-D-aspartate on glutamate and dopamine release in the rat prefrontal cortex: modulation by a group II selective metabotropic glutamate receptor agonist LY379268. Neuroscience. 2003;117(3):697-706. [DOI] [PubMed] [Google Scholar]
- 17.Schrantee A, Tamminga HG, Bouziane C, et al. . Age-dependent effects of methylphenidate on the human dopaminergic system in young vs adult patients with attention-deficit/hyperactivity disorder: a randomized clinical trial. JAMA Psychiatry. 2016;73(9):955-962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Simoni S, Schwarz AJ, O’Daly OG, et al. . Test-retest reliability of the BOLD pharmacological MRI response to ketamine in healthy volunteers. Neuroimage. 2013;64:75-90. [DOI] [PubMed] [Google Scholar]
- 19.Poels EM, Kegeles LS, Kantrowitz JT, et al. . Imaging glutamate in schizophrenia: review of findings and implications for drug discovery. Mol Psychiatry. 2014;19(1):20-29. [DOI] [PubMed] [Google Scholar]
- 20.Poels EM, Kegeles LS, Kantrowitz JT, et al. . Glutamatergic abnormalities in schizophrenia: a review of proton MRS findings. Schizophr Res. 2014;152(2-3):325-332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zarate CA Jr, Mathews DC, Furey ML. Human biomarkers of rapid antidepressant effects. Biol Psychiatry. 2013;73(12):1142-1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bartha R, Williamson PC, Drost DJ, et al. . Measurement of glutamate and glutamine in the medial prefrontal cortex of never-treated schizophrenic patients and healthy controls by proton magnetic resonance spectroscopy. Arch Gen Psychiatry. 1997;54(10):959-965. [DOI] [PubMed] [Google Scholar]
- 23.Théberge J, Bartha R, Drost DJ, et al. . Glutamate and glutamine measured with 4.0 T proton MRS in never-treated patients with schizophrenia and healthy volunteers. Am J Psychiatry. 2002;159(11):1944-1946. [DOI] [PubMed] [Google Scholar]
- 24.Théberge J, Williamson KE, Aoyama N, et al. . Longitudinal grey-matter and glutamatergic losses in first-episode schizophrenia. Br J Psychiatry. 2007;191:325-334. [DOI] [PubMed] [Google Scholar]
- 25.Aoyama N, Théberge J, Drost DJ, et al. . Grey matter and social functioning correlates of glutamatergic metabolite loss in schizophrenia. Br J Psychiatry. 2011;198(6):448-456. [DOI] [PubMed] [Google Scholar]
- 26.Kegeles LS, Mao X, Stanford AD, et al. . Elevated prefrontal cortex γ-aminobutyric acid and glutamate-glutamine levels in schizophrenia measured in vivo with proton magnetic resonance spectroscopy. Arch Gen Psychiatry. 2012;69(5):449-459. [DOI] [PubMed] [Google Scholar]
- 27.Merritt K, Egerton A, Kempton MJ, Taylor MJ, McGuire PK. Nature of glutamate alterations in schizophrenia: a meta-analysis of proton magnetic resonance spectroscopy studies. JAMA Psychiatry. 2016;73(7):665-674. [DOI] [PubMed] [Google Scholar]
- 28.Mouchlianitis E, Bloomfield MA, Law V, et al. . Treatment-resistant schizophrenia patients show elevated anterior cingulate cortex glutamate compared to treatment-responsive. Schizophr Bull. 2016;42(3):744-752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Egerton A, Bhachu A, Merritt K, McQueen G, Szulc A, McGuire P. Effects of antipsychotic administration on brain glutamate in schizophrenia: a systematic review of longitudinal (1)H-MRS studies. Front Psychiatry. 2017;8:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bustillo JR, Patel V, Jones T, et al. . Risk-conferring glutamatergic genes and brain glutamate plus glutamine in schizophrenia. Front Psychiatry. 2017;8:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rowland LM, Bustillo JR, Mullins PG, et al. . Effects of ketamine on anterior cingulate glutamate metabolism in healthy humans: a 4-T proton MRS study. Am J Psychiatry. 2005;162(2):394-396. [DOI] [PubMed] [Google Scholar]
- 32.Stone JM, Dietrich C, Edden R, et al. . Ketamine effects on brain GABA and glutamate levels with 1H-MRS: relationship to ketamine-induced psychopathology. Mol Psychiatry. 2012;17(7):664-665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taylor MJ, Tiangga ER, Mhuircheartaigh RN, Cowen PJ. Lack of effect of ketamine on cortical glutamate and glutamine in healthy volunteers: a proton magnetic resonance spectroscopy study. J Psychopharmacol. 2012;26(5):733-737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ragland JD, Ranganath C, Barch DM, et al. . Relational and Item-Specific Encoding (RISE): task development and psychometric characteristics. Schizophr Bull. 2012;38(1):114-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ragland JD, Blumenfeld RS, Ramsay IS, et al. . Neural correlates of relational and item-specific encoding during working and long-term memory in schizophrenia. Neuroimage. 2012;59(2):1719-1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ragland JD, Ranganath C, Harms MP, et al. . Functional and neuroanatomic specificity of episodic memory dysfunction in schizophrenia: a functional magnetic resonance imaging study of the relational and item-specific encoding task. JAMA Psychiatry. 2015;72(9):909-916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.First MB, Spitzer RL, Gibbon M, Williams J. Structural Clinical Interview for DSM-IV Axis I Disorders (SCID-IV). New York, NY: New York State Psychiatric Institute; 1997. [Google Scholar]
- 38.D’Souza DC, Ahn K, Bhakta S, et al. . Nicotine fails to attenuate ketamine-induced cognitive deficits and negative and positive symptoms in humans: implications for schizophrenia. Biol Psychiatry. 2012;72(9):785-794. [DOI] [PubMed] [Google Scholar]
- 39.D’Souza DC, Singh N, Elander J, et al. . Glycine transporter inhibitor attenuates the psychotomimetic effects of ketamine in healthy males: preliminary evidence. Neuropsychopharmacology. 2012;37(4):1036-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mason OJ, Morgan CJ, Stefanovic A, Curran HV. The psychotomimetic states inventory (PSI): measuring psychotic-type experiences from ketamine and cannabis. Schizophr Res. 2008;103(1-3):138-142. [DOI] [PubMed] [Google Scholar]
- 41.Maldjian JA, Laurienti PJ, Kraft RA, Burdette JH. An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. Neuroimage. 2003;19(3):1233-1239. [DOI] [PubMed] [Google Scholar]
- 42.Insel TR. The NIMH experimental medicine initiative. World Psychiatry. 2015;14(2):151-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gozzi A, Herdon H, Schwarz A, et al. . Pharmacological stimulation of NMDA receptors via co-agonist site suppresses fMRI response to phencyclidine in the rat. Psychopharmacology (Berl). 2008;201(2):273-284. [DOI] [PubMed] [Google Scholar]
- 44.Doyle OM, De Simoni S, Schwarz AJ, et al. . Quantifying the attenuation of the ketamine pharmacological magnetic resonance imaging response in humans: a validation using antipsychotic and glutamatergic agents. J Pharmacol Exp Ther. 2013;345(1):151-160. [DOI] [PubMed] [Google Scholar]
- 45.Driesen NR, McCarthy G, Bhagwagar Z, et al. . The impact of NMDA receptor blockade on human working memory-related prefrontal function and connectivity. Neuropsychopharmacology. 2013;38(13):2613-2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Steffens M, Becker B, Neumann C, et al. . Effects of ketamine on brain function during smooth pursuit eye movements. Hum Brain Mapp. 2016;37(11):4047-4060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rosburg T, Kreitschmann-Andermahr I. The effects of ketamine on the mismatch negativity (MMN) in humans: a meta-analysis. Clin Neurophysiol. 2016;127(2):1387-1394. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial protocol.
eMethods.
eTable. Correlations between biomarkers and ketamine-induced symptoms.