Abstract
The recurrent gain-of-function JAK2V617F mutation confers growth factor-independent proliferation for hematopoietic cells and is a major contributor to the pathogenesis of myeloproliferative neoplasms (MPN). The lack of complete response in most patients treated with the JAK1/2 inhibitor ruxolitinib indicates the need for identifying novel therapeutic strategies. Metformin is a biguanide that exerts selective antineoplastic activity in hematological malignancies. In the present study, we investigate and compare effects of metformin and ruxolitinib alone and in combination on cell signaling and cellular functions in JAK2V617F-positive cells. In JAK2V617F-expressing cell lines, metformin treatment significantly reduced cell viability, cell proliferation, clonogenicity, and cellular oxygen consumption and delayed cell cycle progression. Metformin reduced cyclin D1 expression and RB, STAT3, STAT5, ERK1/2 and p70S6K phosphorylation. Metformin plus ruxolitinib demonstrated more intense reduction of cell viability and induction of apoptosis compared to monotherapy. Notably, metformin reduced Ba/F3 JAK2V617F tumor burden and splenomegaly in Jak2V617F knock-in-induced MPN mice and spontaneous erythroid colony formation in primary cells from polycythemia vera patients. In conclusion, metformin exerts multitarget antileukemia activity in MPN: downregulation of JAK2/STAT signaling and mitochondrial activity. Our exploratory study establishes novel molecular mechanisms of metformin and ruxolitinib action and provides insights for development of alternative/complementary therapeutic strategies for MPN.
Introduction
Philadelphia chromosome-negative myeloproliferative neoplasms (MPN), including essential thrombocythemia (ET), polycythemia vera (PV) and primary myelofibrosis (PMF), are characterized by excessive myeloid proliferation and have heightened risk for acute myeloid leukemia (AML) transformation1. Constitutive activation of the JAK2/STAT signaling pathway is a hallmark of these diseases and plays an important role for MPN pathogenesis. Ruxolitinib is a selective JAK1/2 inhibitor approved by the FDA for the treatment of intermediate and high-risk PMF, and PV patients with inadequate response or intolerant to hydroxyurea. In PMF patients, ruxolitinib is well tolerated, reduces inflammatory cytokines and splenomegaly, and ameliorates constitutional symptoms2–4. In PV patients, ruxolitinib controls the hematocrit, reduces the spleen volume, and improves symptoms5. However, ruxolitinib treatment does not reverse bone marrow fibrosis and does not lead to elimination of the malignant clone, suggesting the need for new therapeutic approaches to further improve patient responses.
Metformin (1,1-dimethylbiguanide) is a biguanide widely prescribed for the treatment of type II diabetes and metabolic syndromes. In recent years, studies using cancer cell lines and murine models have provided evidence for potential anticancer activity of metformin6,7. Some molecular mechanisms for this activity have been proposed, including inhibition of energetic metabolism, cell proliferation and survival signaling pathways, which may occur in an AMPK-dependent or AMPK-independent manner8–10. In addition, preclinical studies testing the combination of chemotherapeutic agents with metformin have appeared promising in the treatment of some solid tumors11.
Considering that metformin has been proposed to be selective for hematological malignant cells12–16 and that metformin has been used for a long time for the treatment of metabolic diseases, preclinical studies to assess the effect metformin may be interesting in MPN, since these findings have potential for incorporation in clinical practice. In the present study, we investigate the cellular and molecular effects of treatment with metformin alone and in combination with ruxolitinib in JAK2V617F MPN models.
Results
Metformin reduces cell viability, proliferation, clonogenicity and cell cycle progression in HEL and SET2 cells
To characterize the potential efficacy of metformin in human JAK2V617F-positive cells, we first investigated the effects of metformin treatment on cell viability in HEL and SET2 cells. In both JAK2V617F cell lines analyzed, metformin reduced cell viability in a dose-dependent and time-dependent manner (Fig. 1a). The IC50 values for metformin in HEL and SET2 cells were 18 and 10 mM at 72 h, respectively. Based on previous studies using leukemia cell lines17 and our IC50 results, we decided to use metformin at 5 and/or 10 mM for in vitro studies. Next, we evaluated the effects of metformin alone and in combination with ruxolitinib on JAK2V617F cell lines by methylthiazoletetrazolium (MTT) assay. In HEL and SET2 cells, treatment with either ruxolitinib or metformin alone significantly reduced the cell viability (p < 0.05), and the combination of ruxolitinib (300 nM) plus metformin (10 mM) significantly decreased cell viability when compared with monotherapy (p < 0.05) (Fig. 1b). Synergy analysis indicates that the combination of ruxolitinib ≥300 nM with metformin presented synergistic effects in HEL cells (all combination index (CI) values <0.60). In SET2 cells, combinations of ruxolitinib ≤300 nM or metformin ≤15 mM varied from slight synergism (CI: 0.85–0.90), moderate synergism (CI: 0.70–0.85), to synergism (CI < 0.60); the combinations of ruxolitinib >300 mM or metformin >15 mM showed no synergistic effects (Supplementary Figure 1).
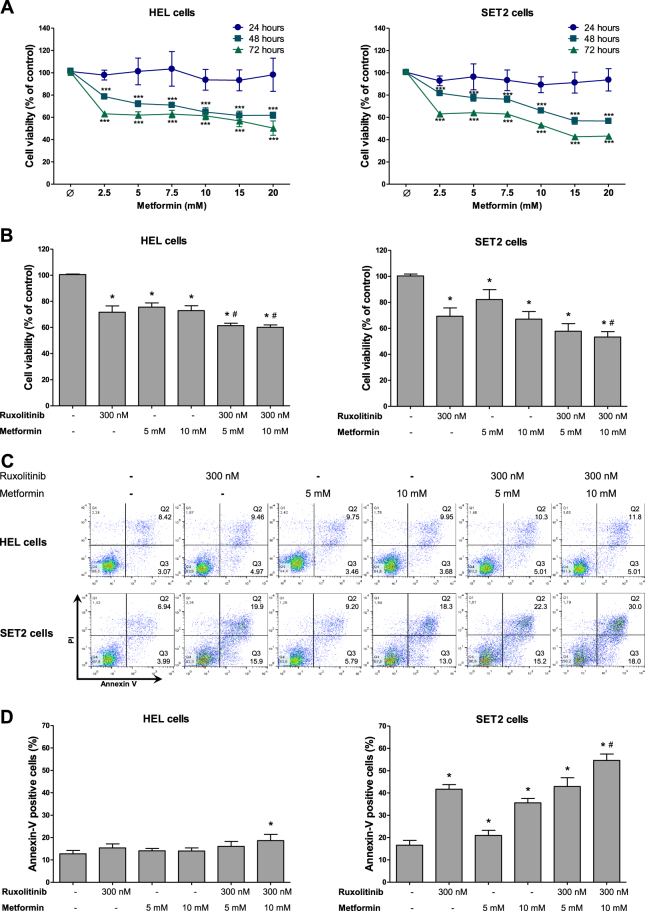
Fig. 1. Metformin potentiates ruxolitinib-induced cell viability reduction in JAK2V617F cells.
a Dose-response and time-response cytotoxicity curves analyzed by methylthiazoletetrazolium (MTT) assay for HEL and SET2 cells treated with metformin for 24, 48 and 72 h. Values are expressed as the percentage of viable cells for each condition relative to untreated controls. Results are shown as the mean ± SD of four independent experiments. ***p < 0.0001 for metformin-treated cells vs. untreated cells; ANOVA test and Bonferroni post-test, all pairs were analyzed and statistically significant differences are indicated. b Cell viability was determined by MTT assay in HEL or SET2 cells treated, or not, with the indicated concentrations of ruxolitinib and/or metformin for 48 h and normalized to corresponding untreated cells. Bar graphs represent the mean ± SD of at least four independent experiments. c Apoptosis was detected by flow cytometry in HEL or SET2 cells treated with ruxolitinib and/or metformin for 48 h using an annexin V/PI staining method. Representative dot plots are shown for each condition; the upper and lower right quadrants (Q2 plus Q3) cumulatively contain the apoptotic population (annexin V+ cells). d Bar graphs represent the mean ± SD of at least four independent experiments quantifying apoptotic cell death. The p values and cell lines are indicated in the graphs. *p < 0.05 for metformin-treated and/or ruxolitinib-treated cells vs. untreated cells, #p < 0.05 for metformin-treated or ruxolitinib-treated cells vs. combination treatment at the corresponding doses; ANOVA test and Bonferroni post-test, all pairs were analyzed and statistically significant differences are indicated
Given these findings, the effects of metformin combined with ruxolitinib were further assayed with respect to cell death and proliferation. Similar to findings for cell viability, SET2 cells subjected to metformin (5 and 10 mM) or ruxolitinib (300 mM) treatment significantly induced apoptosis, and combined treatment (10 mM metformin plus 300 nM ruxolitinib) presented higher levels of apoptosis compared with monotherapy (p < 0.05). By contrast, in HEL cells only the combination of metformin (10 mM) plus ruxolitinib (300 nM) significantly induced apoptosis (Fig. 1c,d). Ki-67 analysis revealed that treatment with metformin or ruxolitinib alone or in combination significantly reduced cell proliferation, but no additive effect of the combination was observed in HEL and SET2 cells (Fig. 2a).
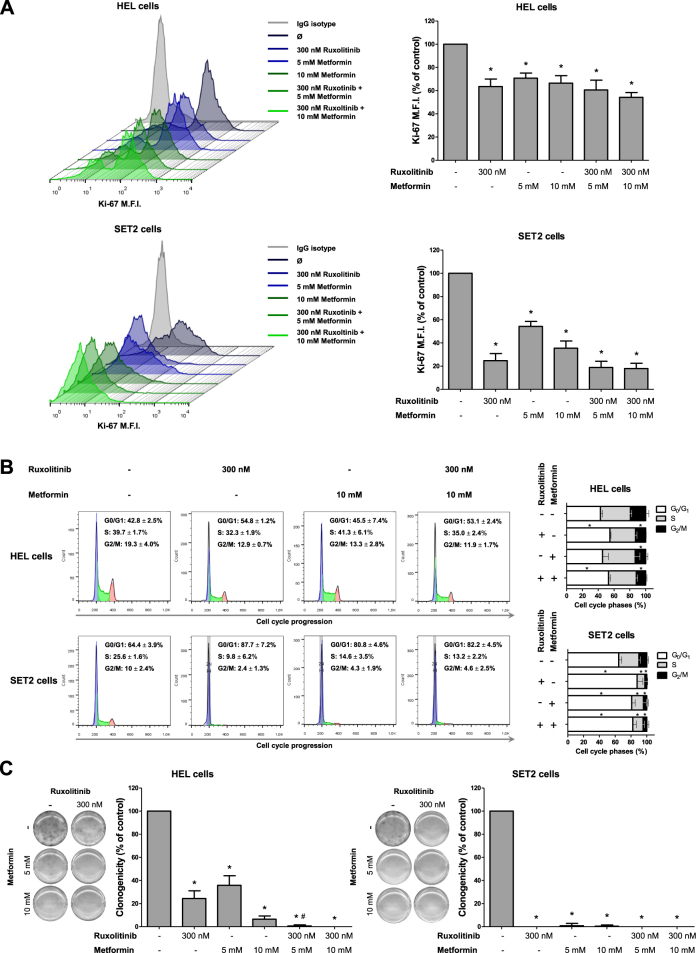
Fig. 2. Metformin and ruxolitinib reduce cell proliferation and delay cell cycle progression in HEL and SET2 cells.
a Ki-67 mean fluorescence intensity (MFI) was determined by flow cytometry after incubation of HEL or SET2 cells treated with ruxolitinib and/or metformin for 48 h; histogram traces are illustrated. The bar graphs represent the Ki-67 M.F.I normalized to the respective untreated control cells, and results are shown as mean ± SD of four independent experiments; *p < 0.05, ANOVA test and Bonferroni post-test, all pairs were analyzed and statistically significant differences are indicated. b Cell cycle progression was determined by BD Cycletest™ Plus DNA Reagent Kit in HEL or SET2 cells treated with the indicated concentrations of ruxolitinib and/or metformin for 48 h. A representative histogram for each condition is illustrated. Bar graphs represent the mean ± SD of the percent of cells in G0/G1, S and G2/M phase upon ruxolitinib (300 nM) and/or metformin (10 mM) for 48 h and represent at least four independent experiments. The p values and cell lines are indicated in the graphs. *p < 0.05 for metformin-treated and/or ruxolitinib-treated cells vs. untreated cells; ANOVA test and Bonferroni post-test, all pairs were analyzed and statistically significant differences are indicated. c Colonies containing viable cells were detected by MTT after 10 days of culture of HEL and SET2 cells treated with ruxolitinib and/or metformin and normalized to the corresponding untreated controls. Colony images are shown for one experiment and the bar graphs show the mean ± SD of at least four independent experiments. The p values and cell lines are indicated in the graphs: *p < 0.05 for metformin-treated and/or ruxolitinib-treated cells vs. untreated cells, #p < 0.05 for metformin-treated or ruxolitinib-treated cells vs. combination treatment at the corresponding doses; ANOVA test and Bonferroni post-test, all pairs were analyzed and statistically significant differences are indicated
In both JAK2V617F cell lines, metformin and/or ruxolitinib resulted in a delay of cell cycle progression, with significant reduction in the percentage of cells in G2/M phase (Fig. 2b); long-term exposure to metformin or ruxolitinib also strongly decreased clonogenicity. Interestingly, combined treatment (10 mM metformin plus 300 nM ruxolitinib) completely inhibited colony formation (Fig. 2c).
Metformin modulates the JAK2/STAT signaling pathway in HEL and SET2 cells
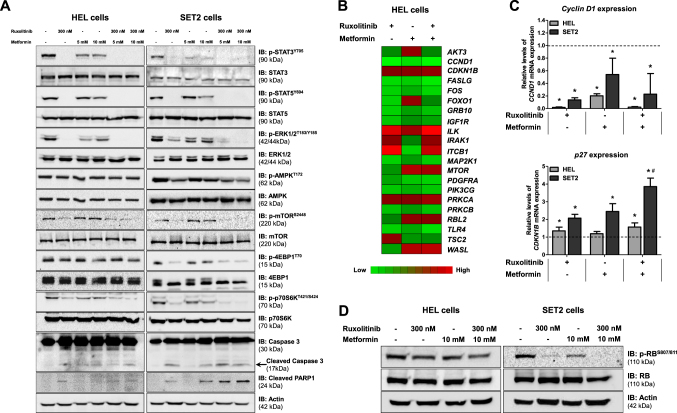
We next sought to compare the effects of metformin and ruxolitinib on activation of the JAK2/STAT and mTOR/p70S6K/4EBP1 signaling pathways. As expected, western blot analysis revealed that ruxolitinib (300 nM) was able to reduce STAT3, STAT5, ERK1/2, mTOR, 4EBP1 and p70S6K phosphorylation in HEL and SET2 cells. Surprisingly, treatment with metformin (5 and 10 mM) neither increased AMPK activation nor decreased mTOR phosphorylation in HEL and SET2 cells. Metformin reduced activation of STAT3, STAT5, ERK1/2, 4EBP1 and p70S6K, albeit to a lesser extent than ruxolitinib (Fig. 3a and Supplementary Figure 2). High levels of cleaved caspase 3 and cleaved PARP1 were observed following treatments with metformin and ruxolitinib alone and in combination in SET2 cells (Fig. 3a and Supplementary Figure 2).
Fig. 3. Metformin and ruxolitinib modulate JAK2/STAT signaling and PI3K/AKT-related genes in HEL and SET2 cells.
a Western blot analysis for p-STAT3Y705, p-STAT5Y694, p-ERK1/2T183/Y185, p-AMPKT172, p-mTORS2448, p-4EBP1T70, p-p70S6KT421/S424, caspase 3 (total and cleaved) and cleaved PARP1 levels in total cell extracts from HEL and SET2 cells treated with the indicated concentrations of ruxolitinib and/or metformin; membranes were reprobed with the antibody for the detection of the respective total protein or actin, and developed with the SuperSignal™ West Dura Extended Duration Substrate system using a Gel Doc XR+ imaging system. b Gene expression heatmap from qPCR array analysis of HEL cells treated with ruxolitinib (300 nM) and/or metformin (10 mM). mRNA levels are normalized to those of untreated HEL cells and calculated as fold change in expression; genes demonstrating ≥1.5-fold in either direction compared to untreated cells in any treatment are included in the heat map. Two independent experiments of each condition were used for the analysis; green indicates repressed mRNA levels and red elevated mRNA levels. c qPCR analysis of CCND1 and CDKN1B mRNA expression in HEL and SET2 cells treated with ruxolitinib (300 nM) and/or metformin (10 mM) for 48 h. The dashed line represents the mean gene expression in untreated cells and bars represent the fold change in gene expression in HEL and SET2 cells treated with ruxolitinib, metformin, or both compared to their respective untreated cells. The p values and cell lines are indicated in the graphs. *p < 0.05 for metformin-treated and/or ruxolitinib-treated cells vs. untreated cells, #p < 0.05 for metformin-treated or ruxolitinib-treated cells vs. combination treatment at the corresponding doses; ANOVA test and Bonferroni post-test, all pairs were analyzed and statistically significant differences are indicated. d Western blot analysis for p-RBS807/811levels in total cell extracts from HEL and SET2 cells treated with ruxolitinib and/or metformin; membranes were reprobed with the antibody for the detection of the total RB protein and actin
Metformin and ruxolitinib modulate PI3K/AKT-related genes in HEL and SET2 cells
Next, using PCR array, we investigated the effects of metformin alone and in combination with ruxolitinib on expression of PI3K/AKT-related genes in HEL cells. A total of 21 different genes demonstrated a change in expression of ≥1.5-fold in either direction compared to untreated cells: five downregulated genes (CCND1, FASLG, ITGB1, PDGFRA and TLR4) and six upregulated genes (AKT3, FOXO1, ILK, MTOR, RBL2 and WASL) by metformin treatment alone; 11 downregulated genes (CCND1, FASLG, FOS, FOXO1, GRB10, IGF1R, MAP2K1, PDGFRA, PIK3CG, PRKCB and TLR4) and three upregulated genes (ILK, ITGB1 and TSC2) by ruxolitinib treatment alone; and ten downregulated genes (CCND1, FASLG, FOS, GRB10, IGF1R, MAP2K1, PDGFRA, PIK3CG, PRKCB and TLR4) and seven upregulated genes (CDKN1B, ILK, IRAK1, ITGB1, MTOR, PRKCA and WASL) by the combination (Fig. 3b; Supplementary Table 1). Based on our findings indicating a cytostatic effect of metformin, we choose two genes (CCND1 and CDKN1B) involved in cell proliferation to validate in a larger number of experiments using HEL and SET2 cells, by qPCR. Metformin and ruxolitinib treatment alone or in combination significantly reduced CCND1 expression (p < 0.05) in both JAK2V617F cell lines. Ruxolitinib alone or in combination with metformin increased CDKN1B expression in HEL cells. In contrast, treatment with either metformin or ruxolitinib alone increased CDKN1B expression in SET2 cells, and this effect was enhanced by combined treatment (p < 0.05; Fig. 3c). In conjunction with these findings, we observed that phosphorylation of RB, a cyclin D1 target and a key cell cycle progression-related protein18, was reduced following metformin, ruxolitinib, or combination treatment in both JAK2V617F cell lines, though more prominently in SET2 cells (Fig. 3d).
Metformin reduces cell viability and potentiates ruxolitinib effects in JAK2V617F-driven cellular and allograft models
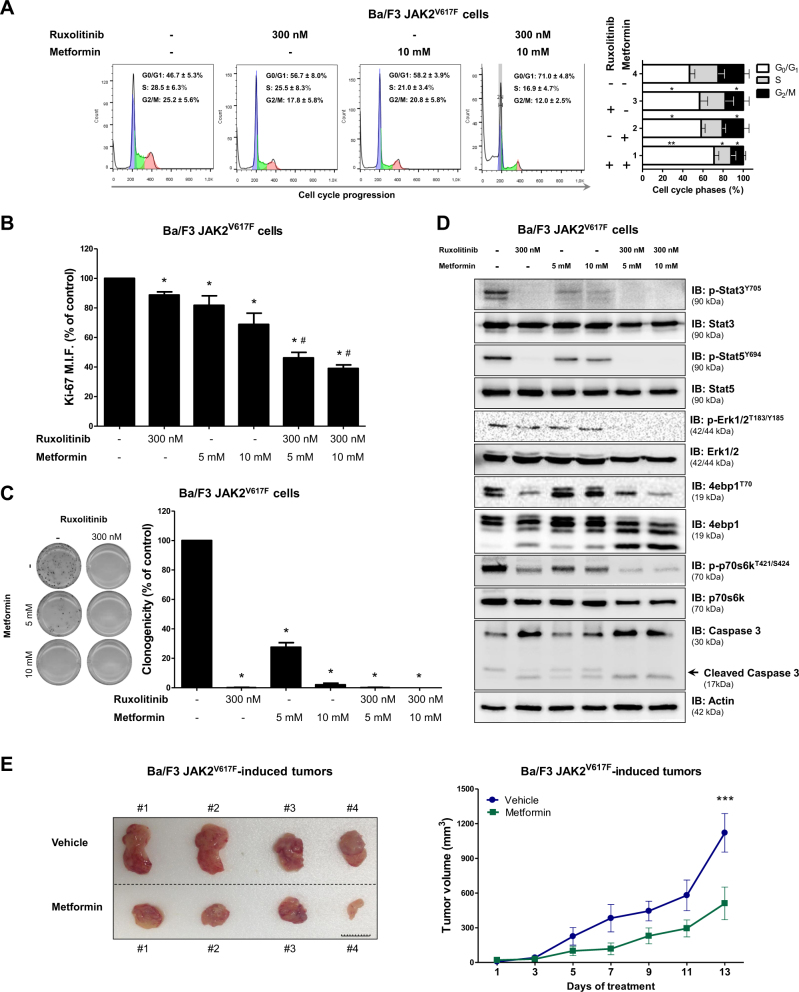
Ba/F3 cells are an IL3-dependent line which, when expressing the JAK2V617F mutant gene, acquire IL3-independent growth19. Using Ba/F3 JAK2WT and Ba/F3 JAK2V617F models, we evaluated the effect of metformin and/or ruxolitinib on cell viability and apoptosis in the presence or absence of IL-3-rich Wehi-3B-conditioned medium. With or without supplemented Wehi-3B conditioned medium, both metformin and ruxolitinib were able to reduce cell viability and induce apoptosis to similar levels in both Ba/F3 JAK2WT and Ba/F3 JAK2V617F cells, and combined treatment presented more prominent efficacy (p < 0.05; Supplementary Figure 3). Based on these results, we performed subsequent experiments using only IL3-deprived Ba/F3 JAK2V617F cells, which are a model where cell viability is supported by the JAK2V617F mutant’s oncogenic potential. Treatment with metformin, ruxolitinib, or the combination induced cell cycle arrest, reduced cell proliferation and clonogenicity, and downregulated STAT3, STAT5 and p70S6K phosphorylation (Fig. 4a–d). Metformin treatment (125 mg/kg/day) was able to reduce the tumor burden of Ba/F3 JAK2V617F cells implanted into NSG mice (p < 0.05; Fig. 4e and Supplementary Figure 4).
Fig. 4. Metformin delays cell cycle progression, reduces colony formation, downregulates JAK2/STAT activation and decreases tumor burden in Ba/F3 JAK2V617F cells.
a Cell cycle phase profiling was determined by BD Cycletest™ Plus DNA Reagent Kit in Ba/F3 JAK2V617F cells treated with ruxolitinib and/or metformin for 24 h. A representative histogram for each condition is illustrated. Bar graphs represent the mean ± SD of the fraction of cells in G0/G1, S and G2/M phase for each treatment condition across at least four independent experiments. b Ki-67 MFI was determined by flow cytometry after incubation of Ba/F3 JAK2V617F cells treated with the indicated concentrations of ruxolitinib and/or metformin for 24 h. The Ki-67 M.F.I was normalized to the respective untreated control cells and results are shown as the mean ± SD of four independent experiments. c Colonies containing viable cells were detected by MTT after 10 days of culture of Ba/F3 JAK2V617F cells treated with ruxolitinib and/or metformin and normalized to the corresponding untreated controls. Colony images are shown for one experiment and the bar graphs show the mean ± SD of at least four independent experiments. d Western blot analysis for p-Stat3Y705, p-Stat5Y694, p-Erk1/2T183/Y185, p-4ebp1T70, p-p70s6kT421/S424 and caspase 3 (total and cleaved) levels in total cell extracts from Ba/F3 JAK2V617F cells treated with ruxolitinib and/or metformin for 24 h; membranes were reprobed with the antibody for the detection of the respective total protein or actin, and developed with the SuperSignal™ West Dura Extended Duration Substrate system and a Gel Doc XR+ system. e Images and volumes (mean ± SEM) of tumors induced by subcutaneous injection of Ba/F3 JAK2V617F cells in NSG mice, treated with vehicle (PBS) (n = 4) or metformin (125 mg/kg/day) (n = 4). Tumor volume (V) was calculated using the formula (V = W2 × L × 0.52), where W and L represent the smallest and largest diameters, respectively. Images of individual animal tumors are shown; Scale Bar: 10 mm. The p values and cell lines are indicated in the graphs. *p < 0.05, **p < 0.01, ***p < 0.001 for metformin-treated and/or ruxolitinib-treated cells vs. untreated-cells, #p < 0.05 for metformin-treated or ruxolitinib-treated cells vs. combination treatment at the corresponding doses; ANOVA test and Bonferroni post-test, all pairs were analyzed and statistically significant differences are indicated
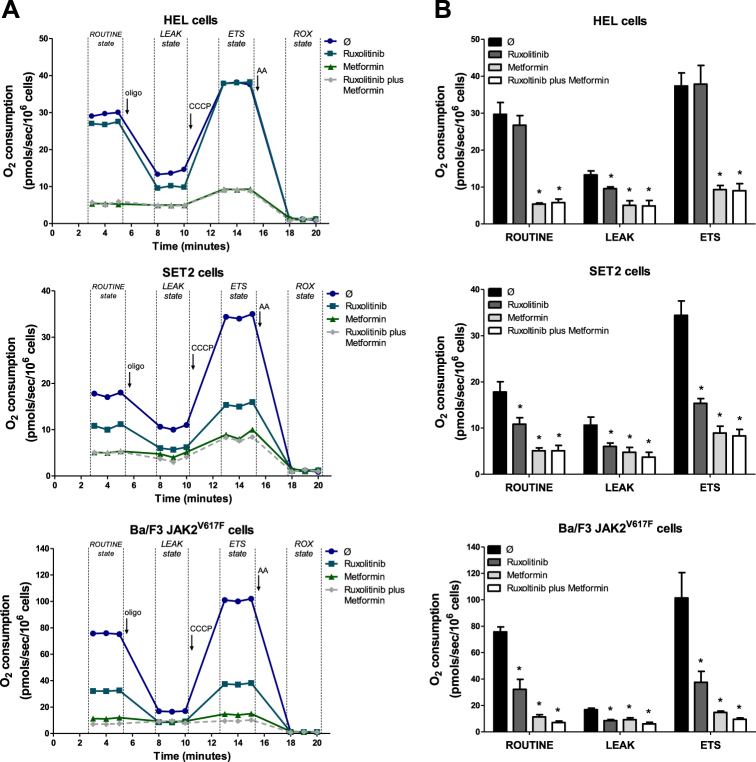
Metformin reduces the oxygen consumption in JAK2V617F cells
Metformin has been described as a mitochondrial complex I inhibitor in cancer cells13,20. Thus, we investigated the impact of metformin alone or in combination with ruxolitinib treatment on oxygen consumption in JAK2V617F-positive cell lines using a high-resolution respiratory assay. We observed a strong reduction in cellular oxygen consumption at the state supported by exogenous substrates in culture media (ROUTINE state), at the non-phosphorylating state (LEAK State) and at the maximum respiratory capacity (ETS state) in metformin-treated and metformin plus ruxolitinib-treated HEL, SET2 and Ba/F3 JAK2V617F cells (p < 0.05). Unexpectedly, ruxolitinib also significantly reduced oxygen consumption as a single agent at ROUTINE, LEAK and ETS states in SET2 and Ba/F3 JAK2V617F cells, and at LEAK state in HEL cells (Fig. 5).
Fig. 5. Metformin reduces the oxygen consumption of JAK2V617F cells.
a Oxygen consumption was determined in HEL, SET2 or Ba/F3 JAK2V617F cells following treatment with ruxolitinib (300 nM) and/or metformin (10 mM) for 24 h using a high-resolution respirometry. A representative line graph containing oxygen consumption at ROUTINE, LEAK, ETS and ROX states is illustrated. The black arrows indicate the sequential addition of oligomycin (oligo, 1 mg/mL), protonophore carbonyl cyanide m-chlorophenyl hydrazone (CCCP, 2 μM) and antimycin A (AA, 3 μM); oxygen consumption rates were measured over time. b Bar graphs represent the mean ± SD rate of oxygen consumption mean at ROUTINE, LEAK and ETS states of at least six independent experiments. Values of respiratory rates at ROX state were subtracted from the other states. The p values and cell lines are indicated in the graphs. *p < 0.05 for metformin-treated and/or ruxolitinib-treated cells vs. untreated cells; ANOVA test and Bonferroni post-test, all pairs were analyzed and statistically significant differences are indicated
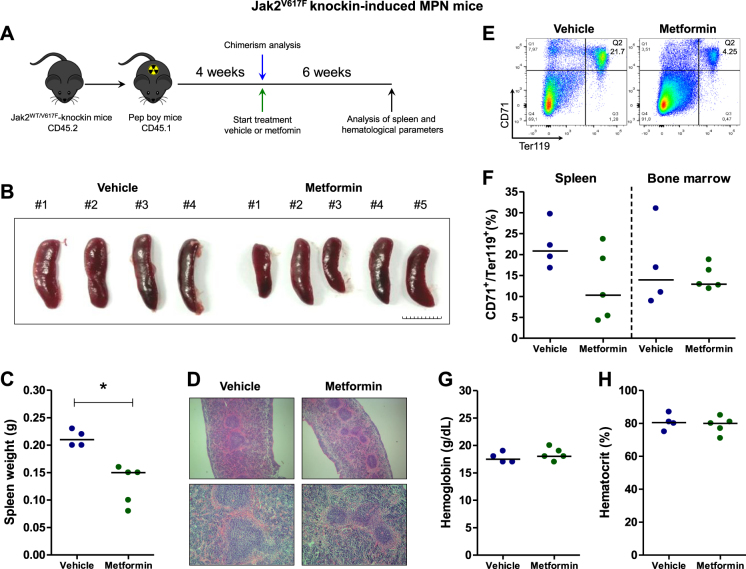
Metformin reduces splenomegaly in a Jak2V617F knockin-induced MPN mouse model
In order to formally assess the effect of metformin treatment using an in vivo model of MPN-like disease, we induced MPN phenotype by transplantation of cells from Jak2WT/V617F knockin mice into Pep boy recipient mice (Fig. 6a). In Jak2V617F knockin-induced MPN animals, metformin treatment (125 mg/kg/day) was well-tolerated, reduced splenomegaly (p = 0.02, Fig. 6b,c) and improved splenic architecture (Fig. 6d). Erythroid progenitors in the spleen and bone marrow did not differ between control and metformin-treated groups, but the smaller spleens (from metformin-treated mice #1 and #3) presented a low percentage of erythroid progenitors (4.2 and 5.4%, respectively) (Fig. 6e,f). Hemoglobin and hematocrit were not modulated by metformin treatment (Fig. 6g,h). In Pep boy recipient mice transplanted with Jak2WT/WT, metformin treatment (125 mg/kg/day) was well-tolerated and altered neither hematological parameters nor spleen size or architecture (Supplementary Figure 5).
Fig. 6. Metformin reduces splenomegaly in Jak2V617F knockin-induced MPN mice.
a Experimental design for induction of MPN phenotype in mice. Bone marrow cells from Jak2V617F mice were transplanted into lethally irradiated Pep boy mice. After chimerism evaluation at 4 weeks, mice were randomized and daily treated with vehicle (n = 4) or metformin (125 mg/kg) (n = 5) for 6 weeks. b Spleen images and c weight of vehicle and metformin-treated MPN mice. Scale Bar: 10 mm.*p < 0.05, Mann–Whitney test. d Representative histopathology H&E sections of spleen from vehicle and metformin-treated mice. Magnification of 40× (upper panel) and 100× (lower panel). e Illustrative dot plots of erythroid progenitor analysis in the spleen. f Dispersion graphs showing the percentage of early erythroid progenitors (CD71+/Ter119+ cells) in spleen and bone marrow. g Dispersion graphs showing the hemoglobin and h hematocrit levels
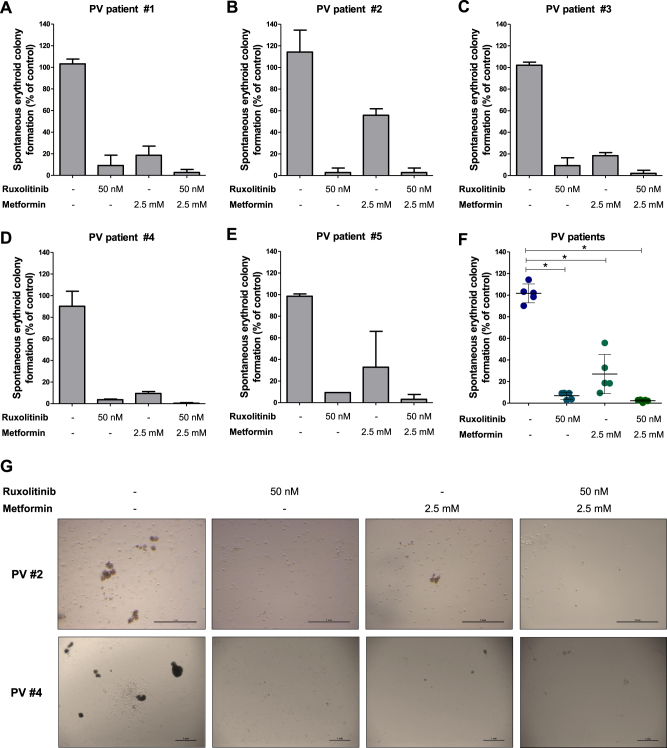
Metformin inhibits erythropoietin-independent colony formation of primary PV cells
Spontaneous erythroid colony formation in the absence of erythropoietin is a common finding in cells from PV patients cultured in methylcellulose21,22. We performed erythropoietin-independent colony assays to verify the effects of metformin (2.5 mM) with and without ruxolitinib (50 nM) in primary cells from PV patients. We observed that metformin was able to reduce spontaneous erythroid colony formation in cells from all PV patients tested. Ruxolitinib presented a strong reduction in erythropoietin-independent colony formation and no additional effects were observed with the combined treatment (Fig. 7).
Fig. 7. Metformin reduces spontaneous erythroid colony formation in primary polycythemia vera patient cells.
a–e Peripheral blood or bone marrow mononuclear cells from 5 polycythemia vera (PV) patients were plated in methylcellulose, containing cytokines but lacking erythropoietin, in the presence or not of metformin and/or ruxolitinib. Spontaneous erythroid colonies were counted after 14 days of culture and are represented as the percent of untreated controls. Bars indicate the mean ± SD of the duplicate assays for each patient. f Dispersion graph comparing combined colony formation results from all five PV patients; the horizontal line represents the mean ± SD. The p values are indicated in the graphs; *p < 0.05 for metformin- and/or ruxolitinib-treated cells vs. untreated controls; ANOVA test and Bonferroni post-test, all pairs were analyzed and statistically significant differences are indicated. g Representative images of erythropoietin-independent colony formation at 14 days of culture from two PV patients are illustrated
Discussion
Herein, we have characterized in vitro and in vivo efficacy of metformin in the context of JAK2V617F-driven MPN models. Our results show that metformin reduces cell viability, proliferation, cell cycle progression and clonogenicity in JAK2V617F cells. Metformin is a biguanide used in the treatment of type II diabetes and metabolic syndromes, and epidemiological studies suggest that the drug exerts an antineoplastic activity in humans23. In addition, preclinical studies already include a range of evidence indicating a potential therapeutic use for metformin in cancer, and clinical trials are currently in progress (www.clinicaltrials.gov)6. In hematological neoplasms, antineoplastic effects of metformin have been described in chronic myeloid leukemia17,24, AML9,12,25,26, acute lymphoblastic leukemia (ALL)8,16,24,27,28, chronic lymphocytic leukemia29,30, lymphoma15 and multiple myeloma13. Importantly, metformin effects appear to act selectively in cancer cells, since cytotoxicity was observed only on leukemia cells and not for colonies from normal hematopoeitic cells12, culture of normal peripheral blood mononuclear cells13,14, normal cord blood CD34+ cells15 or normal T lymphocytes16.
In the present study, AMPK activation was not modulated by metformin treatment in JAK2V617F cells. Several mechanisms have been proposed to underlie metformin activity and are commonly grouped into (i) AMPK-dependent or (ii) AMPK-independent, both of which have already been described in hematological malignancies. Leclerc and colleagues8 observed that metformin induces apoptosis in ALL cell lines, which was abrogated by AMPK silencing, indicating that metformin-induced apoptosis in these cell lines was AMPK-dependent. Scotland and colleagues9, using AML cell lines, reported that metformin inhibits cell proliferation and increases apoptosis in an AMPK-independent manner.
Notably, a modest effect was observed with the combination of metformin and ruxolitinib, suggesting that both drugs may share some similarities in mechanisms of action in these cells. In our study, metformin was able to inhibit STAT3 and STAT5 phosphorylation even in the presence of the JAK2V617F mutation in HEL, SET2 and Ba/F3 JAK2V617F cell lines. The inhibitory effect of metformin on STAT3 phosphorylation was reported in breast cancer31, esophageal squamous cell carcinoma32, lung cancer33–35, bladder cancer36,37 and pancreatic cancer38. There are no reports of metformin effects on STAT5 phosphorylation in solid tumors. Recently, Kawashima and Kirito39 showed that metformin reduces cell viability and downregulates the JAK2/STAT5 axis in an AMPK-dependent and PP2A activation-dependent manner in HEL and SET2 cells. In contrast, our results suggest that STAT5 downregulation occurs independently of AMPK activation in JAK2V617F cells.
We also observed downregulation of cyclin D1 (CCND1) and upregulation of p27 (CDKN1B) by PCR array and qPCR in metformin-treated and/or ruxolitinib-treated HEL and SET2 cells, which may explain the delay in the cell cycle, the reduction of RB phosphorylation and the cytostatic effect, highlighting our findings regarding JAK2/STAT signaling inhibition by metformin. Supporting these results, it is well established that STAT5 activation leads to p27 inhibition, promoting cell cycle progression in HEL cells40, and that STAT3 and/or STAT5 activation induces cyclin D1 expression in several types of cells41,42. Reduced ERK1/2 activation may also contribute to metformin-induced and/or ruxolitinib-induced cell cycle delay, since the MAPK pathway directly acts on the cell cycle machinery by regulating the expression and/or localization of cyclin D1 and p2743,44. The CDK4/6-cyclin D complex phosphorylates RB protein, which represents a critical gatekeeper of cell cycle progression from G1 to S phase18. In our study, cyclin D1 reduction was consistent with the reduction of RB phosphorylation in JAK2V617F cells upon treatment with metformin, ruxolitinib, or the combination. Particularly, SET2 cells showed lower levels of RB phosphorylation and more intense cell cycle arrest in the G0/G1 phase. Further studies are needed to determine whether other cyclin D isoforms (e.g., CCND2, CCND3), or even small amounts of CCND1 are sufficient to induce cell cycle progression in HEL cells. Indeed, differences in the response to metformin and/or ruxolitinib between HEL and SET2 cells were observed. HEL cells are derived from a patient with erythroleukemia45, featuring faster growth in culture conditions and less sensitivity to ruxolitinib, even at doses that are able to inhibit the JAK2/STAT activation. SET2 cells are derived from a patient with leukemic transformation of ET and shows slower growth, better response to ruxolitinib, and requirement for high fetal bovine serum (FBS) concentration for growth46. These differences among HEL and SET2 cell lines may affect cell response to metformin.
Metformin has been described as a mitochondrial complex I inhibitor20,47, which has been implicated as an important mechanism involved in its antineoplastic effects on hematological malignancies13,26. Mitochondria play a key role in the activation of oncogenic signaling pathways as the effector organelle for cellular energy generation (adenosine triphosphate, ATP) by coupling the tricarboxylic acid cycle with oxidative phosphorylation48,49. Our findings indicate that metformin-mediated reduction of mitochondrial activity contributes to decreased cell viability in MPN cells, highlighting the importance of increased energy demand for the proliferation of cancer cells50.
Metformin treatment at a dose of 125 mg/kg/day effectively reduced tumor burden in Ba/F3 JAK2V617F allograft and splenomegaly in Jak2V617F knockin-induced MPN murine models. In humans, this dose is equivalent to 10.4 mg/kg/day according to the coefficient of conversion proposed by Freireich et al.51, which represents a pharmacological dose lower than that used for type II diabetes treatment. Metformin also reduced spontaneous erythroid colony formation in primary cells from patients with PV. Additionally, although metformin and/or ruxolitinib treatment had modest effects on the induction of apoptosis and/or cell cycle arrest in JAK2V617F cell lines, prolonged exposure to these drugs (in monotherapy or in combination), in the absence of growth factors, strongly reduced autonomous growth, which is a characteristic that is usually associated with aggressiveness in leukemia cells52,53. Using U937 cells, we also confirm that metformin reduces cell viability in JAK2WT cells (Supplementary Figure 6), corroborating the multitarget potential of metformin in hematological malignancies9. Based on our in vitro studies, we speculate that the current clinically indicated dose of metformin may provide better improved clinical results for such patients.
In summary, metformin exerts an antileukemic activity and downregulates JAK2/STAT signaling in JAK2V617F cells. PCR-array identified cyclin D1 and p27 as contributors to the mechanism of metformin and ruxolitinib efficacy, corroborating cell cycle and proliferation findings. Our exploratory study establishes novel molecular mechanisms of metformin action alone and in combinations with ruxolitinib on JAK2V617F aberrant signaling and provides insights for development of alternative/complementary therapeutic strategies for MPN.
Materials and methods
Cell culture and inhibitors
HEL and U937 cells were obtained from ATCC (Philadelphia, PA, USA) and SET2 cells were kindly provided by Prof. Dr. Fabíola Attié de Castro (School of Pharmaceutical Sciences of Ribeirão Preto, University of São Paulo, Ribeirão Preto, Brazil). HEL and SET2 cells harboring JAK2V617F mutation, and U937 cells (JAK2 wild-type) were tested and authenticated by Short Tandem Repeat (STR) matching analysis using the PowerPlex® 16 HS system (Promega, Madison, WI, USA) and the ABI 3500 Sequence Detector System (Life Technologies, Foster City, CA, USA). Ba/F3 cells expressing murine erythropoietin receptor and JAK2 wild-type or JAK2V617F (named as Ba/F3 JAK2WT and Ba/F3 JAK2V617F, respectively), and Wehi-3B cells were kindly provided by Prof. Dr. Susumu Kobayashi (Division of Hematology/Oncology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA). Cell culture conditions were performed in accordance with the recommendations of ATCC and DSMZ. All cell lines were mycoplasma free. Ruxolitinib was obtained from Novartis Pharmaceuticals (Basel, Switzerland). Metformin was obtained from Sigma-Aldrich (St. Louis, MO, USA).
Cell viability assay
Cell viability was measured by MTT assay. HEL or U937 (2 × 104 cells/well) and SET2 cells (4 × 104 cells/well) were cultured in a 96-well plate in RPMI medium containing 10 or 20% FBS, respectively, in the presence of ruxolitinib (300 nM) and/or metformin (5 and 10 mM) for 48 h. For time-response and dose-response curves, HEL and SET2 cells were cultured as described above in 96-well plates in the presence of graded concentrations of metformin (0, 2.5, 5, 7.5, 10, 15 and 20 mM) for 24, 48 and 72 h. IC50 values were calculated using a nonlinear regression analysis on GraphPad Prism 5 (GraphPad Software, Inc., San Diego, CA, USA). For experiments involving Ba/F3 JAK2WT or Ba/F3 JAK2V617F cell lines, 2 × 104 cells per well were cultured in RPMI medium supplemented with 10% FBS in a 96-well plate with or without Wehi-3B-conditioned medium, ruxolitinib (300 nM) and/or metformin (5 and 10 mM) for 48 h. At the end of each culture period, 10 μL of a 5 mg/mL solution of MTT was added to each well followed by incubation at 37 °C for 4 h. The reaction was stopped using 100 μL of 0.1 N HCl in anhydrous isopropanol. Cell viability was evaluated by measuring the absorbance at 570 nm, using an iMark™ Microplate Absorbance Reader (Bio-Rad, Richmond, CA, USA). For synergism analysis, HEL and SET2 cells were treated with graded doses of ruxolitinib (3, 10, 30,100, 300 and 1000 nM) and metformin (2.5, 5, 7.5, 10, 15 and 20 mM) alone or in combination with each other for 48 h. The CI was calculated using CompuSyn software (ComboSyn, Inc., Paramus, NJ, USA), and the data obtained were interpreted according to Chou54 and illustrated using multiple experiment viewer (MeV) 4.9.0 software (http://www.tm4.org/mev/).
Apoptosis assay
HEL, SET2, Ba/F3 JAK2WT, Ba/F3 JAK2V617F and U937 cells were seeded in 24-well plates and treated with ruxolitinib (300 nM) and/or metformin (5 or 10 mM) for 48 h. Cells were then washed twice with ice cold PBS and resuspended in binding buffer containing 1 μg/mL propidium iodide (PI) and 1 μg/mL APC-labeled annexin V. All specimens were acquired by flow cytometry (FACSCalibur; Becton Dickinson) after incubation for 15 minutes at room temperature in a light-protected area and analyzed using FlowJo software (Treestar, Inc., San Carlos, CA, USA).
Assessment of cell proliferation by Ki-67 staining
HEL and SET2 cells were treated with ruxolitinib (300 nM) and/or metformin (5 or 10 mM) for 48 h, fixed with 70% ethanol and stored at −20 °C. Ba/F3 JAK2V617F cells were treated with ruxolitinib (300 nM) and/or metformin (5 or 10 mM) for 24 h, fixed with 70% ethanol and stored at −20 °C. Ki-67 staining was performed following the manufacturer’s instructions (Ki-67 FITC clone B56; BD Bioscience, San Jose, CA, USA) and the mean of fluorescence intensity (MFI) was obtained by flow cytometry using a FACSCalibur instrument (Becton-Dickinson). IgG isotype was used as negative control for each condition.
Cell cycle analysis
Cell cycle phases were determined using BD Cycletest™ Plus DNA Reagent Kit (Becton-Dickinson, Mountain View, CA, USA) according to the manufacturer’s instructions. In brief, HEL and SET2 cells were cultured in the presence of ruxolitinib (300 nM) and/or metformin (10 mM) for 48 h. Ba/F3 JAK2V617F cells were cultured without Wehi-3B-conditioned medium, in the presence of ruxolitinib (300 nM) and/or metformin (10 mM) for 24 h. DNA content distribution was acquired in a FACSCalibur cytometer (Becton-Dickinson) and analyzed using FlowJo software (Treestar, Inc.).
Colony formation assay
Colony formation capacity was evaluated out in semisolid methylcellulose medium (1 × 103 cells/mL for HEL cells, 2.5 × 103 cells/mL for SET2 cells and 1 × 103 cells/mL for Ba/F3 JAK2V617F cells; MethoCult 4230; StemCell Technologies Inc., Vancouver, BC, Canada). Colonies were detected after 10 days of culture by adding 1 mg/mL of MTT reagent and scored by Image J quantification software (US National Institutes of Health, Bethesda, MD, USA).
Western blot analysis
Equal amounts of protein were used as total extracts, followed by SDS-PAGE, Western blot analysis with the indicated antibodies and imaging using the SuperSignal™ West Dura Extended Duration Substrate System (Thermo Fisher Scientific, San Jose, CA, USA) and Gel Doc XR+ system (Bio-Rad, Hercules, CA, USA) or ImageQuant LAS 4000 (GE Healthcare Life Sciences, Piscataway, NJ, USA). Antibodies against STAT3 (sc-7179), STAT5 (sc-835), p-p70S6KT421/S424 (sc-7984), p70S6K (sc-8418), PARP1 (sc-56197) and actin (sc-1616) were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Antibodies against p-RBS807/811 (#9308), RB (#9309), p-STAT3Y705 (#9131S), p-STAT5Y694 (#9359S), p-AMPKT172 (#2535S), AMPK (#2532S), p-mTORS2448 (#2971), mTOR (#2972), p-4EBP1T70 (#9455S), 4EBP1 (#9452S) and caspase 3 (#9665) were obtained from Cell Signaling Technology (Danvers, MA, USA). Antibodies against p-ERK1/2T183/Y185 (700012) and ERK1/2 (44654G) were from Life Technologies. Cropped gels retain important bands, but whole gel images are available in Supplementary Figure 7A-C. Band intensities were determined using UN-SCAN-IT gel 6.1 software (Silk Scientific; Orem, UT, USA).
PI3K/AKT signaling pathway profile by PCR array
Total RNA from HEL cells treated with metfomin (10 mM) and/or ruxolitinib (300 nM) was obtained using TRIzol reagent (Thermo Fisher Scientific). The cDNA was synthesized from 1 µg of RNA using High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher Scientific). PCR array was performed using the PI3K-AKT Signaling Pathway RT2 Profiler PCR Array kit (#PAHS-058A; SA Biosciences, Frederick, MD, USA) according to the manufacturer’s instructions. mRNA levels were normalized to those detected in untreated cells, and genes that presented a fold change ≥1.5-fold in any treatment were included in the heatmap using Heatmap builder software (The Ashley Lab, Stanford University, CA, USA). Amplification was performed in an ABI 7500 Sequence Detector System (Life technologies).
Quantitative PCR
Total RNA from HEL and SET2 cells treated with metfomin (10 mM) and/or ruxolitinib (300 nM) was obtained using TRIzol reagent (Thermo Fisher Scientific). The cDNA was synthesized from 1 µg of RNA using High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher Scientific). Quantitative PCR (qPCR) was performed with an ABI 7500 Sequence Detector System (Life Technologies) with specific primers for CCND1 (Cyclin D1, forward: CTCGGTGTCCTACTTCAAATG; reverse: AGCGGTCCAGGTAGTTCAT), CDKN1B (cyclin-dependent kinase inhibitor 1B, also known as p27, forward: ACTCTGAGGACACGCATTTGGT; reverse: TCTGTTCTGTTGGCTCTTTTGTT) and HPRT1 (hypoxanthine phosphoribosyltransferase 1; forward: GAACGTCTTGCTCGAGATGTGA; reverse: TCCAGCAGGTCAGCAAAGAAT). The relative quantification value was calculated using the equation 2−ΔΔCT. A negative “no template control” was included for each primer pair.
Ba/F3 JAK2V617F tumor formation in NSG mice
NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) mice were purchased from The Jackson Laboratory (Bar Harbor, Maine, USA). Experimental groups consisted of 8–10 week-old female mice that received a 100 µL (50 µL PBS plus 50 µL matrigel) dorsal subcutaneous injection of 2 × 106 Ba/F3 JAK2V617F cells and daily treatment by intraperitoneal injection of vehicle (PBS, n = 9) or metformin (125 mg/kg, n = 9) for 13 days. Tumor volume (V) was obtained using the formula (V = W2 × L × 0.52), where W and L are the smaller and larger diameters, respectively. The dose of metformin at 125 mg/kg/day used for mouse experiments was based on a previous study13, and represents a dose equivalent to 10.4 mg/kg/day for humans51. All experiments were approved by the Institutional Animal Care and Use Committee of Oregon Health & Science University and the Animal Ethics Committee of the University of São Paulo, and were performed according to IACUC guidelines.
Assessment of oxygen consumption
Viable HEL, SET2 and Ba/F3 JAK2V617F cells (2 × 106) were cultured alone or in the presence of metformin (10 mM) and/or ruxolitinib (300 nM) for 24 h and submitted to oxygen consumption evaluation by high-resolution respirometry assay (Oxygraph-2k, Oroboros Instruments, Innsbruck, Austria). After determination of respiratory rates supported by exogenous substrates in culture media (ROUTINE state), modulators of mitochondrial function were sequentially added: oligomycin (1 mg/mL), an ATP synthase inhibitor that establishes the non-phosphorylating respiration (LEAK state); protonophore carbonyl cyanide m-chlorophenyl hydrazone (2 μM), which determines the state of maximum capacity of the electron transport system (ETS state); and antimycin A (3 μM), a mitochondrial complex III inhibitor that establishes the residual oxygen consumption due to oxidative side reactions (rox state). The DatLab software package (Oroboros) was used for data acquisition and analysis.
Generation of JAK2V617F knockin-induced MPN mice by bone marrow transplantation
For MPN phenotype induction, 5 × 106 bone marrow cells from Jak2V617F knockin (Jak2WT/V617F) mice55 were transplanted into lethally irradiated Pep boy mice (B6.SJL-Ptprca Pepcb/BoyJ, The Jackson Laboratory). A total of 5 × 106 bone marrow cells from Jak2WT/WT were transplanted into lethally irradiated Pep boy mice as a experimental control group. After 4 weeks, chimerism was evaluated by CD45.1 and CD45.2 markers (Becton-Dickinson) by flow cytrometry in peripheral blood. Mice with ≥70% CD45.2 cells were randomized and treated daily by intraperitoneal injection of vehicle (PBS) or metformin (125 mg/kg) for 6 weeks. At the conclusion of the experiment, animals were harvested and subjected to analysis of spleen, bone marrow and hematological parameters. Erythroid progenitors in the spleen and bone marrow were evaluated by CD71 and Ter119 markers (Becton-Dickinson) by flow cytometry. All experiments were approved by the Animal Ethics Committee of the University of São Paulo.
Erythropoietin-independent colony formation
Mononuclear cells were isolated from peripheral blood or bone marrow from PV patients (n = 5, median age 52 years [range 24–74]) by Ficoll-gradient centrifugation. A total of 2 × 105 cells were plated onto methocult H4535 (supplemented with cytokines and without erythropoietin, StemCell Technologies) in the presence or not of metformin (2.5 mM) and/or ruxolitinib (50 nM)21. Each condition was performed in duplicate. Erythroid colonies (burst-forming units plus colony-forming units-E) were counted after 14 days.
Statistical analysis
Statistical analyses were performed using GraphPad Prism 5 (GraphPad Software, Inc.). For comparisons, Mann–Whitney test or ANOVA test and Bonferroni post-test was used. A p value < 0.05 was considered as statistically significant. All pairs were analyzed and statistically significant differences are indicated.
Electronic supplementary material
Acknowledgements
Funding for this work was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq; 402587/2016-2), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP; 2014/23092-0; 2015/02200-2). The authors would like to thank Cleide Lúcia Araújo Silva and Silvia Elena Sanchez Mendoza for their valuable technical assistance in animal experiments and Vani Maria Alves Correa for her valuable technical assistance in histopathology H&E section preparation. B.J.D. is an investigator for the Howard Hughes Medical Institute.
Authors' contributions
J.A.M-N. designed the study and experiments, performed all the experiments, statistical analyses, manuscript preparation, completion and final approval. B.A.F., R.S-R., J.L.C-S., J.C.F., A.P.N.R.A. and L.L.F.P. contributed with inputs on overall design of study, participated in experiments using animal models and primary human cells, manuscript editing and final approval. P.S.S. participated in flow cytrometry experiments, in the analysis of the data and final approval. C.R.P.D. and L.C.A. participated in oxygen consumption experiments, in the analysis of the data and final approval. C.A.E., B.P.S., C.E.T., B.J.D. and E.M.R. participated in the interpretation of manuscript data, in manuscript editing and final approval. F.T. was the principal investigator and participated in overall design of study and experiments, statistical analyses, manuscript preparation, editing, completion and final approval.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Edited by M. Herold
Electronic supplementary material
Supplementary Information accompanies this paper at 10.1038/s41419-017-0256-4.
References
- 1.Thoennissen NH, et al. Prevalence and prognostic impact of allelic imbalances associated with leukemic transformation of Philadelphia chromosome-negative myeloproliferative neoplasms. Blood. 2010;115:2882–2890. doi: 10.1182/blood-2009-07-235119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pardanani A, et al. JAK inhibitor therapy for myelofibrosis: critical assessment of value and limitations. Leukemia. 2011;25:218–225. doi: 10.1038/leu.2010.269. [DOI] [PubMed] [Google Scholar]
- 3.Harrison C, et al. JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis. N. Engl. J. Med. 2012;366:787–798. doi: 10.1056/NEJMoa1110556. [DOI] [PubMed] [Google Scholar]
- 4.Verstovsek S, et al. A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N. Engl. J. Med. 2012;366:799–807. doi: 10.1056/NEJMoa1110557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vannucchi AM, et al. Ruxolitinib versus standard therapy for the treatment of polycythemia vera. N. Engl. J. Med. 2015;372:426–435. doi: 10.1056/NEJMoa1409002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chae YK, et al. Repurposing metformin for cancer treatment: current clinical studies. Oncotarget. 2016;7:40767–40780. doi: 10.18632/oncotarget.8194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pollak M. Potential applications for biguanides in oncology. J. Clin. Invest. 2013;123:3693–3700. doi: 10.1172/JCI67232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leclerc GM, Leclerc GJ, Kuznetsov JN, DeSalvo J, Barredo JC. Metformin induces apoptosis through AMPK-dependent inhibition of UPR signaling in ALL lymphoblasts. PLoS. One. 2013;8:e74420. doi: 10.1371/journal.pone.0074420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scotland S, et al. Mitochondrial energetic and AKT status mediate metabolic effects and apoptosis of metformin in human leukemic cells. Leukemia. 2013;27:2129–2138. doi: 10.1038/leu.2013.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosilio C, Ben-Sahra I, Bost F, Peyron JF. Metformin: a metabolic disruptor and anti-diabetic drug to target human leukemia. Cancer Lett. 2014;346:188–196. doi: 10.1016/j.canlet.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 11.Zhang HH, Guo XL. Combinational strategies of metformin and chemotherapy in cancers. Cancer Chemother. Pharmacol. 2016;78:13–26. doi: 10.1007/s00280-016-3037-3. [DOI] [PubMed] [Google Scholar]
- 12.Green AS, et al. The LKB1/AMPK signaling pathway has tumor suppressor activity in acute myeloid leukemia through the repression of mTOR-dependent oncogenic mRNA translation. Blood. 2010;116:4262–4273. doi: 10.1182/blood-2010-02-269837. [DOI] [PubMed] [Google Scholar]
- 13.Dalva-Aydemir S, et al. Targeting the metabolic plasticity of multiple myeloma with FDA-approved ritonavir and metformin. Clin. Cancer Res. 2015;21:1161–1171. doi: 10.1158/1078-0432.CCR-14-1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gwak H, Kim Y, An H, Dhanasekaran DN, Song YS. Metformin induces degradation of cyclin D1 via AMPK/GSK3beta axis in ovarian cancer. Mol. Carcinog. 2017;56:349–358. doi: 10.1002/mc.22498. [DOI] [PubMed] [Google Scholar]
- 15.Shi WY, et al. Therapeutic metformin/AMPK activation blocked lymphoma cell growth via inhibition of mTOR pathway and induction of autophagy. Cell Death Dis. 2012;3:e275. doi: 10.1038/cddis.2012.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grimaldi C, et al. AMP-dependent kinase/mammalian target of rapamycin complex 1 signaling in T-cell acute lymphoblastic leukemia: therapeutic implications. Leukemia. 2012;26:91–100. doi: 10.1038/leu.2011.269. [DOI] [PubMed] [Google Scholar]
- 17.Vakana E, Altman JK, Glaser H, Donato NJ, Platanias LC. Antileukemic effects of AMPK activators on BCR-ABL-expressing cells. Blood. 2011;118:6399–6402. doi: 10.1182/blood-2011-01-332783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Giacinti C, Giordano A. RB and cell cycle progression. Oncogene. 2006;25:5220–5227. doi: 10.1038/sj.onc.1209615. [DOI] [PubMed] [Google Scholar]
- 19.Warmuth M, Kim S, Gu XJ, Xia G, Adrian F. Ba/F3 cells and their use in kinase drug discovery. Curr. Opin. Oncol. 2007;19:55–60. doi: 10.1097/CCO.0b013e328011a25f. [DOI] [PubMed] [Google Scholar]
- 20.Wheaton WW, et al. Metformin inhibits mitochondrial complex I of cancer cells to reduce tumorigenesis. Elife. 2014;3:e02242. doi: 10.7554/eLife.02242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mazzacurati L, et al. The PIM inhibitor AZD1208 synergizes with ruxolitinib to induce apoptosis of ruxolitinib sensitive and resistant JAK2-V617F-driven cells and inhibit colony formation of primary MPN cells. Oncotarget. 2015;6:40141–40157. doi: 10.18632/oncotarget.5653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quintas-Cardama A, et al. Preclinical characterization of the selective JAK1/2 inhibitor INCB018424: therapeutic implications for the treatment of myeloproliferative neoplasms. Blood. 2010;115:3109–3117. doi: 10.1182/blood-2009-04-214957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taubes G. Cancer research. Cancer prevention with a diabetes pill? Science. 2012;335:29. doi: 10.1126/science.335.6064.29. [DOI] [PubMed] [Google Scholar]
- 24.Shi R, et al. The antileukemia effect of metformin in the Philadelphia chromosome-positive leukemia cell line and patient primary leukemia cell. Anticancer Drugs. 2015;26:913–922. doi: 10.1097/CAD.0000000000000266. [DOI] [PubMed] [Google Scholar]
- 25.Wang F, et al. Metformin synergistically sensitizes FLT3-ITD-positive acute myeloid leukemia to sorafenib by promoting mTOR-mediated apoptosis and autophagy. Leuk. Res. 2015;39:1421–1427. doi: 10.1016/j.leukres.2015.09.016. [DOI] [PubMed] [Google Scholar]
- 26.Velez J, et al. Biguanides sensitize leukemia cells to ABT-737-induced apoptosis by inhibiting mitochondrial electron transport. Oncotarget. 2016;7:51435–51449. doi: 10.18632/oncotarget.9843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosilio C, et al. The metabolic perturbators metformin, phenformin and AICAR interfere with the growth and survival of murine PTEN-deficient T cell lymphomas and human T-ALL/T-LL cancer cells. Cancer Lett. 2013;336:114–126. doi: 10.1016/j.canlet.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 28.Rodriguez-Lirio A, et al. Metformin induces cell cycle arrest and apoptosis in drug-resistant leukemia cells. Leuk. Res. Treat. 2015;2015:516460. doi: 10.1155/2015/516460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bruno S, et al. Metformin inhibits cell cycle progression of B-cell chronic lymphocytic leukemia cells. Oncotarget. 2015;6:22624–22640. doi: 10.18632/oncotarget.4168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Voltan R, et al. Metformin combined with sodium dichloroacetate promotes B leukemic cell death by suppressing anti-apoptotic protein Mcl-1. Oncotarget. 2016;7:18965–18977. doi: 10.18632/oncotarget.7879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deng XS, et al. Metformin targets Stat3 to inhibit cell growth and induce apoptosis in triple-negative breast cancers. Cell Cycle. 2012;11:367–376. doi: 10.4161/cc.11.2.18813. [DOI] [PubMed] [Google Scholar]
- 32.Feng Y, et al. Metformin promotes autophagy and apoptosis in esophageal squamous cell carcinoma by downregulating Stat3 signaling. Cell Death Dis. 2014;5:e1088. doi: 10.1038/cddis.2014.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li L, et al. Metformin sensitizes EGFR-TKI-resistant human lung cancer cells in vitro and in vivo through inhibition of IL-6 signaling and EMT reversal. Clin. Cancer Res. 2014;20:2714–2726. doi: 10.1158/1078-0432.CCR-13-2613. [DOI] [PubMed] [Google Scholar]
- 34.Lin CC, et al. Metformin enhances cisplatin cytotoxicity by suppressing signal transducer and activator of transcription-3 activity independently of the liver kinase B1-AMP-activated protein kinase pathway. Am. J. Respir. Cell Mol. Biol. 2013;49:241–250. doi: 10.1165/rcmb.2012-0244OC. [DOI] [PubMed] [Google Scholar]
- 35.Zhao Z, et al. Metformin inhibits the IL-6-induced epithelial-mesenchymal transition and lung adenocarcinoma growth and metastasis. PLoS One. 2014;9:e95884. doi: 10.1371/journal.pone.0095884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pan Q, et al. Metformin can block precancerous progression to invasive tumors of bladder through inhibiting STAT3-mediated signaling pathways. J. Exp. Clin. Cancer Res. 2015;34:77. doi: 10.1186/s13046-015-0183-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu Q, et al. Metformin represses bladder cancer progression by inhibiting stem cell repopulation via COX2/PGE2/STAT3 axis. Oncotarget. 2016;7:28235–28246. doi: 10.18632/oncotarget.8595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yue W, et al. Metformin combined with aspirin significantly inhibit pancreatic cancer cell growth in vitro and in vivo by suppressing anti-apoptotic proteins Mcl-1 and Bcl-2. Oncotarget. 2015;6:21208–21224. doi: 10.18632/oncotarget.4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kawashima I, Kirito K. Metformin inhibits JAK2V617F activity in MPN cells by activating AMPK and PP2A complexes containing the B56alpha subunit. Exp. Hematol. 2016;44:1156–1165. doi: 10.1016/j.exphem.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 40.Walz C, et al. Activated Jak2 with the V617F point mutation promotes G1/S phase transition. J. Biol. Chem. 2006;281:18177–18183. doi: 10.1074/jbc.M600064200. [DOI] [PubMed] [Google Scholar]
- 41.Frank DA. STAT3 as a central mediator of neoplastic cellular transformation. Cancer Lett. 2007;251:199–210. doi: 10.1016/j.canlet.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 42.Matsumura I, et al. Transcriptional regulation of the cyclin D1 promoter by STAT5: its involvement in cytokine-dependent growth of hematopoietic cells. EMBO J. 1999;18:1367–1377. doi: 10.1093/emboj/18.5.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fabris L, et al. p27kip1 controls H-Ras/MAPK activation and cell cycle entry via modulation of MT stability. Proc. Natl. Acad. Sci. USA. 2015;112:13916–13921. doi: 10.1073/pnas.1508514112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baldassarre G, Belletti B. Meet me in the cytoplasm: A role forp27(Kip1) in the control of H-Ras. Small GTPases. 2016;7:71–75. doi: 10.1080/21541248.2016.1171279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Martin P, Papayannopoulou T. HEL cells: a new human erythroleukemia cell line with spontaneous and induced globin expression. Science. 1982;216:1233–1235. doi: 10.1126/science.6177045. [DOI] [PubMed] [Google Scholar]
- 46.Uozumi K, et al. Establishment and characterization of a new human megakaryoblastic cell line (SET-2) that spontaneously matures to megakaryocytes and produces platelet-like particles. Leukemia. 2000;14:142–152. doi: 10.1038/sj.leu.2401608. [DOI] [PubMed] [Google Scholar]
- 47.Owen MR, Doran E, Halestrap AP. Evidence that metformin exerts its anti-diabetic effects through inhibition of complex 1 of the mitochondrial respiratory chain. Biochem. J. 2000;348:607–614. doi: 10.1042/bj3480607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Solaini G, Sgarbi G, Baracca A. Oxidative phosphorylation in cancer cells. Biochim. Biophys. Acta. 2011;1807:534–542. doi: 10.1016/j.bbabio.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 49.Cheng Z, Tseng Y, White MF. Insulin signaling meets mitochondria in metabolism. Trends Endocrinol. Metab. 2010;21:589–598. doi: 10.1016/j.tem.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wallace DC. Mitochondria and cancer. Nat. Rev. Cancer. 2012;12:685–698. doi: 10.1038/nrc3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Freireich EJ, Gehan EA, Rall DP, Schmidt LH, Skipper HE. Quantitative comparison of toxicity of anticancer agents in mouse, rat, hamster, dog, monkey, and man. Cancer Chemother. Rep. 1966;50:219–244. [PubMed] [Google Scholar]
- 52.Lowenberg B, van Putten WL, Touw IP, Delwel R, Santini V. Autonomous proliferation of leukemic cells in vitro as a determinant of prognosis in adult acute myeloid leukemia. N. Engl. J. Med. 1993;328:614–619. doi: 10.1056/NEJM199303043280904. [DOI] [PubMed] [Google Scholar]
- 53.Yan Y, et al. Autonomous growth potential of leukemia blast cells is associated with poor prognosis in human acute leukemias. J. Hematol. Oncol. 2009;2:51. doi: 10.1186/1756-8722-2-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chou TC. Theoretical basis, experimental design, and computerized simulation of synergism and antagonism in drug combination studies. Pharmacol. Rev. 2006;58:621–681. doi: 10.1124/pr.58.3.10. [DOI] [PubMed] [Google Scholar]
- 55.Mullally A, et al. Physiological Jak2V617F expression causes a lethal myeloproliferative neoplasm with differential effects on hematopoietic stem and progenitor cells. Cancer Cell. 2010;17:584–596. doi: 10.1016/j.ccr.2010.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.