This cohort study determines trends in use of ambulatory surgery centers and hospital outpatient departments for cataract surgery from 2001 to 2014 and factors affecting the site of surgery.
Key Points
Question
What proportion of cataract surgeries in the United States are performed at ambulatory surgery centers (ASCs), how has this changed over time, and what factors affect the location where cataract surgery takes place?
Findings
In this cohort study including 369 320 individuals in a large managed care network who underwent 531 325 surgeries, the proportion of cataract surgeries performed at ASCs increased from 43.6% in 2001 to 73.0% in 2014, with dramatic geographic variation in ASC use, from 1.6% in La Crosse, Wisconsin, to 98.8% in Pueblo, Colorado.
Meaning
The large shift of cataract surgery from hospital outpatient departments to ASCs has important implications for patient access to surgery, outcomes, safety, and societal costs.
Abstract
Importance
Cataract surgery is commonly performed at ambulatory surgery centers (ASCs) and hospital outpatient departments (HOPDs). These venues differ in many ways, including surgical efficiency, patient throughput, patient safety, and costs per surgery.
Objective
To determine trends in use of ASCs and HOPDs for cataract surgery from 2001 to 2014 and factors affecting the site of surgery.
Design, Setting, and Participants
This retrospective longitudinal cohort analysis involved individuals 40 years and older who underwent cataract surgery between January 2001 and December 2014 from a nationwide US managed care network. Data were analyzed from February 2016 to February 2017.
Main Outcomes and Measures
We identified all enrollees who underwent cataract surgery and determined whether the surgery was performed at an ASC or HOPD. We calculated the proportion of surgeries performed at each site each year from 2001 to 2014. Multivariable logistic regression identified characteristics of enrollees who had cataract surgery at an ASC vs a HOPD. We also assessed geographic variation in the proportion of cataract surgeries performed at ASCs in 306 communities throughout the United States.
Results
Of the 369 320 enrollees included in this study, 208 319 (56.4%) were female, and the mean (SD) age was 66.3 (10.4) years. All enrollees underwent cataract surgery (531 325 surgeries) from 2001 to 2014. Of these, 237 046 (64.2%) underwent cataract surgery at an ASC. The proportion of cataract surgeries performed at ASCs increased from 43.6% in 2001 to 73.0% in 2014. Compared with enrollees with incomes less than $40 000, those with incomes greater than $100 000 were 20% more likely to undergo cataract surgery at an ASC (odds ratio, 1.20; 95% CI, 1.12-1.29). Enrollees with better overall health were no more likely to undergo cataract surgery at an ASC (odds ratio, 1.00; 95% CI, 0.99-1.00) than at an HOPD. Enrollees who lived in communities without certificate of need laws were more than twice as likely to have surgery at an ASC (odds ratio, 2.49; 95% CI, 2.35-2.63). The proportion of cataract surgeries performed at ASCs from 2012 to 2014 varied considerably, from 1.6% in La Crosse, Wisconsin, to 98.8% in Pueblo, Colorado.
Conclusions and Relevance
We observed a large shift in the site of cataract surgery from HOPDs to ASCs from 2001 to 2014. Future research is needed to assess the effect of this transition in site of surgical care on patient access to surgery, surgical outcomes, patient safety, and societal costs.
Introduction
Approximately 53 million outpatient surgeries are performed in the United States annually. Years ago, nearly all of these surgeries required inpatient hospitalization. Over time, most of these surgeries moved to hospital outpatient departments (HOPDs), and now many are performed at ambulatory surgery centers (ASCs). By 2006, across all areas of medicine, nearly half of all outpatient surgeries were performed at ASCs.
Reasons for the increasing popularity of ASCs relative to HOPDs include enhanced surgeon productivity, improved convenience for patients and surgeons, decreased out-of-pocket patient costs, and decreased per-case costs for insurers. An advantage of performing surgeries at HOPDs rather than ASCs is that when HOPDs are attached to hospitals, they are often better equipped to deal with medical emergencies. To curtail rising surgical care costs, some insurers have considered incentivizing patients to undergo surgery at ASCs rather than HOPDs. These policies could profoundly affect ophthalmologic surgical care delivery, as more than 95% of ocular surgeries are performed in outpatient settings.
The proportion of ocular surgeries performed at ASCs increased considerably from 1998 to 2011 in Florida, but to the best of our knowledge, nationwide trends are unknown. In this study, we evaluate trends in the performance of cataract surgeries at ASCs and HOPDs from 2001 to 2014 among enrollees in a nationwide managed care network and the extent of geographic variation in ASC use over time. We also identify sociodemographic and other patient characteristics associated with the likelihood of receiving cataract surgery at an ASC vs an HOPD. Finally, we compare trends in ASC use for cataract surgery with several ophthalmic subspecialty surgeries. Understanding these shifts in facility choice has important implications for societal health care costs, access to care, and surgical efficiency, safety, and outcomes.
Methods
Data Source
We used the Clinformatics DataMart database (OptumInsight), which contains claims data for all beneficiaries in a nationwide US managed care network from 2001 to 2014. The data set includes information for all individuals in the network with 1 or more International Classification of Diseases, Ninth Revision, Clinical Modification codes for eye-related diagnoses (360-379.9), 1 or more Current Procedural Terminology codes for any eye-related visits and diagnostic or therapeutic procedures (65091-68899 and 92002-92499), or any other claim submitted by an ophthalmologist or optometrist from January 1, 2001, through December 31, 2014. We had access to all enrollees’ claims for ocular and nonocular conditions and all procedures performed. Information about enrollees’ age, sex, race/ethnicity, education level, and annual income were available. The database includes individuals with commercial health insurance along with those in Medicare Advantage plans and various plan types (eg, HMO and PPO). The database contains information on enrollees in states throughout the United States, although certain regions, such as the upper Midwest, are more heavily represented relative to others. We have used this resource previously to study ocular diseases. The University of Michigan Institutional Review Board approved this study. Informed consent was waived because data were deidentified.
Sample Selection
We identified individuals 40 years and older undergoing cataract surgery from 2001 to 2014. eTable 1 in the Supplement lists the billing codes used to identify cataract surgeries. The database captures the location of every surgery. Our analyses focus on enrollees who underwent cataract surgery at an HOPD or an ASC. We excluded those with surgery performed elsewhere, such as during an inpatient hospitalization, and those for whom the surgery site was unclear. Some enrollees had surgery on one eye at an ASC and the contralateral eye at an HOPD. Because of this, the sum of enrollees receiving surgery at each venue is greater than the total number of enrollees undergoing cataract surgery.
Analyses
We performed statistical analyses using SAS version 9.4 (SAS Institute). Enrollee characteristics were summarized using means and standard deviations for continuous variables and frequencies and percentages for categorical variables. Univariate differences were assessed with χ2 tests. For all analyses, we report 2-tailed P values, and P < .05 was considered statistically significant. To assess trends in cataract surgery over time, the proportions of cataract surgeries performed at ASCs and HOPDs were calculated annually. We used t tests as part of a linear regression to compare trends in other ocular surgeries and that of cataract surgery. The study was designed and completed from February 2016 to February 2017.
Geographic Variation in ASC vs HOPD Use for Cataract Surgery
To assess the extent of geographic variation in the use of ASCs and HOPDs for cataract surgery, we divided the United States into 306 hospital referral regions (HRRs). Hospital referral regions are geographic units based on referral patterns for tertiary medical care services. Enrollees were assigned to an HRR based on their residential zip code at plan enrollment. We assessed the proportion of patients undergoing cataract surgery at an ASC for each HRR during 2 periods: an earlier period (2004-2006) and a later period (2012-2014). Use of these years permitted a 3-year look-back period (2001-2003 and 2009-2011) for both groups. The change in proportion of cataract surgeries performed at ASCs during the 2004-2006 period to the 2012-2014 period was also calculated for each HRR. Some states have certificate of need (CON) laws, which regulate the number of ASCs that are permitted to operate in the state. Each HRR was characterized as possessing CON laws or no such laws; HRRs that covered states with and without CON laws were categorized as “mixed CON.”
Multivariable Regression Model
A multivariable logistic regression model identified characteristics of enrollees undergoing cataract surgery at an ASC vs an HOPD. For this particular analysis, enrollees were included in the model only if they had not had prior cataract surgery in a 3-year look-back period, as we were interested in assessing factors associated with the location of their initial cataract surgery. Enrollees were also required to have no record of aphakia or pseudophakia, indicative of prior cataract surgery during the look-back period. Model predictors included age at surgery, sex, race/ethnicity, education level, annual income, calendar year of surgery, whether the patient had exclusively commercial health insurance or Medicare Advantage, insurance plan type, and Charlson comorbidity index score (indicating patients’ overall health). Whether the enrollee lived in an HRR with CON, no CON, or mixed CON as well as the presence or absence of comorbid dementia, diabetes, hypertension, chronic kidney disease, congestive heart failure, chronic obstructive pulmonary disease, or myocardial infarction were also included in the model. Model results are presented as odds ratios (ORs) with 95% CIs.
Trends in Use of Cataract Surgery at ASCs and HOPDs Compared With Other Ophthalmic Surgeries
To compare with the trends in use of ASCs for cataract surgery, we evaluated the trends of use of other common ophthalmologic surgeries at ASCs vs HOPDs. Using Current Procedural Terminology codes, ophthalmologic surgeries were grouped into strabismus, cornea, glaucoma, or retina surgeries (eTable 1 in the Supplement). Because some of these other surgeries are frequently performed on children and adults, we did not restrict the sample to individuals 40 years and older for this subanalysis. The proportion of surgeries of each type performed at an ASC and HOPD was calculated annually from 2001 to 2014. Linear regression was used to calculate and compare the slope of change for each other surgery type with that of cataract surgery.
Results
Characteristics of Cataract Surgery Recipients at ASCs and HOPDs
There were 369 320 enrollees who underwent 1 or more cataract surgeries from 2001 to 2014, for a total of 531 325 cataract surgeries. The mean (SD) age at initial cataract surgery was 66.3 (10.4) years. During the 14-year period, 237 046 individuals (64.2%) underwent cataract surgery at an ASC, 136 261 (36.9%) at an HOPD, and 3987 (1.1%) at both settings. Among individuals who had surgery at an ASC, 133 329 (56.3%) were female, 176 501 (81.5%) were white, 21 667 (10.0%) were black, 13 536 (6.2%) were Latino, and 4959 (2.3%) were Asian American. Among those who had surgery at an HOPD, 77 284 (56.7%) were female, 97 268 (81.5%) were white, 13 900 (11.6%) were black, 5550 (4.6%) were Latino, and 2692 (2.3%) were Asian American (Table 1).
Table 1. Sociodemographic Characteristics of Eligible Enrollees Undergoing Cataract Surgery.
| Characteristic | No. (%) | ||
|---|---|---|---|
| Enrollees Undergoing Cataract Surgery at an ASC | Enrollees Undergoing Cataract Surgery at an HOPD | All Enrollees Undergoing Cataract Surgery | |
| No. of enrollees | 237 046 | 136 261 | 369 320 |
| No. of surgeriesa | 339 142 | 192 183 | 531 325 |
| Age, mean (SD), y | 66.0 (10.3) | 66.7 (10.6) | 66.3 (10.4) |
| Sex | |||
| Male | 103 717 (43.8) | 58 977 (43.3) | 161 001 (43.6) |
| Female | 133 329 (56.3) | 77 284 (56.7) | 208 319 (56.4) |
| Race/ethnicityb | |||
| White | 176 501 (81.5) | 97 268 (81.5) | 270 824 (81.5) |
| Black | 21 667 (10.0) | 13 900 (11.6) | 35 116 (10.6) |
| Latino | 13 536 (6.2) | 5550 (4.6) | 18 917 (5.7) |
| Asian American | 4959 (2.3) | 2692 (2.3) | 7565 (2.3) |
| Education levelc | |||
| <High school | 1380 (0.6) | 657 (0.5) | 2020 (0.6) |
| High school diploma | 68 464 (30.5) | 42 118 (34.0) | 109 390 (31.7) |
| Some college | 122 770 (54.7) | 63 177 (51.0) | 183 894 (53.4) |
| College diploma or more | 31 900 (14.2) | 17 940 (14.5) | 49 319 (14.3) |
| Annual income, $d | |||
| <40 000 | 56 989 (31.6) | 32 142 (35.4) | 88 047 (32.8) |
| 40 000-59 999 | 33 119 (18.4) | 17 240 (19.0) | 49 774 (18.6) |
| 60 000-99 999 | 44 280 (24.5) | 21 453 (23.6) | 65 034 (24.2) |
| ≥100 000 | 46 010 (25.5) | 20 042 (22.1) | 65 405 (24.4) |
| Insurance plan | |||
| Medicare advantage | 85 027 (35.9) | 45 938 (33.7) | 129 263 (35.0) |
| Commercial | 152 019 (64.1) | 90 323 (66.3) | 240 057 (65.0) |
| Plan type | |||
| HMO | 82 577 (34.8) | 52 448 (38.5) | 133 354 (36.1) |
| PPO | 24 910 (10.5) | 15 659 (11.5) | 40 164 (10.9) |
| EPO | 16 170 (6.8) | 7782 (5.7) | 23 731 (6.4) |
| POS | 78 493 (33.1) | 39 182 (28.8) | 116 613 (31.6) |
| IND | 23 167 (9.8) | 14 151 (10.4) | 36 881 (10.0) |
| Other | 11 729 (5.0) | 7039 (5.2) | 18 577 (5.0) |
| Year of first cataract surgery | |||
| 2001-2003 | 24 767 (10.5) | 28 994 (21.3) | 53 429 (14.5) |
| 2004-2006 | 42 846 (18.1) | 30 253 (22.2) | 72 390 (19.6) |
| 2007-2009 | 63 087 (26.6) | 33 057 (24.3) | 95 018 (25.7) |
| 2010-2012 | 67 030 (28.3) | 29 308 (21.5) | 95 211 (25.8) |
| 2013-2014 | 39 316 (16.6) | 14 649 (10.8) | 53 272 (14.4) |
Abbreviations: ASC, ambulatory surgery center; EPO, exclusive provider organization; HMO, health maintenance organization; HOPD, hospital outpatient department; IND, indemnity; POS, point of service; PPO, preferred provider organization.
Some enrollees had surgery on one eye at one of these surgical sites and the contralateral eye at a different site (n = 3987). Because of this, the sum of enrollees who had surgery at each venue is greater than the total number of enrollees undergoing cataract surgery.
Race/ethnicity information missing for 36 898 enrollees.
Education level information missing for 24 697 enrollees.
Annual income information missing for 101 060 enrollees.
Trends in Use of ASCs, 2001-2014
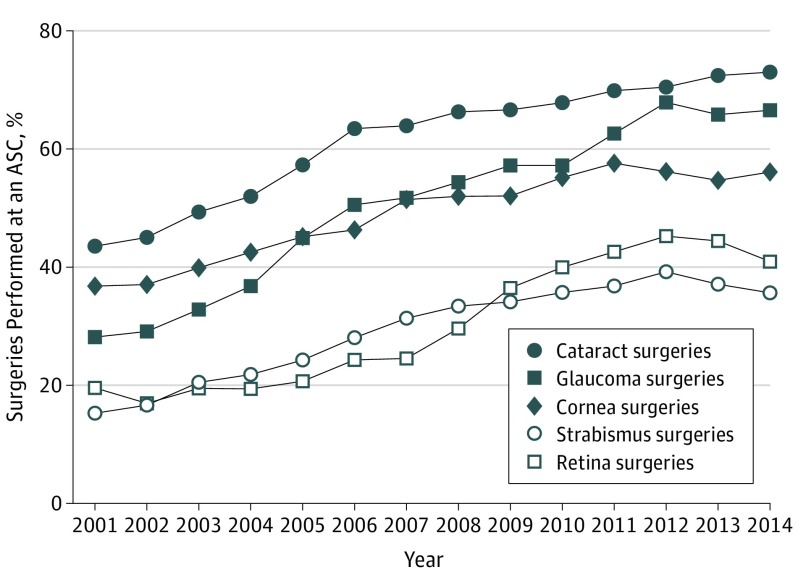
In 2001, 9693 of 22 258 cataract surgeries (43.6%) were performed at ASCs. The proportion of cataract surgeries performed at ASCs increased steadily over time, reaching 73.0% (25 040 of 34 288) in 2014, representing a 67.4% increase compared with 2001 (Figure 1).
Figure 1. Proportion of Different Types of Ocular Surgeries Performed at an Ambulatory Surgery Center (ASC) Each Year from 2001 to 2014.
Geographic Variation in Use of ASCs vs HOPDs for Cataract Surgery
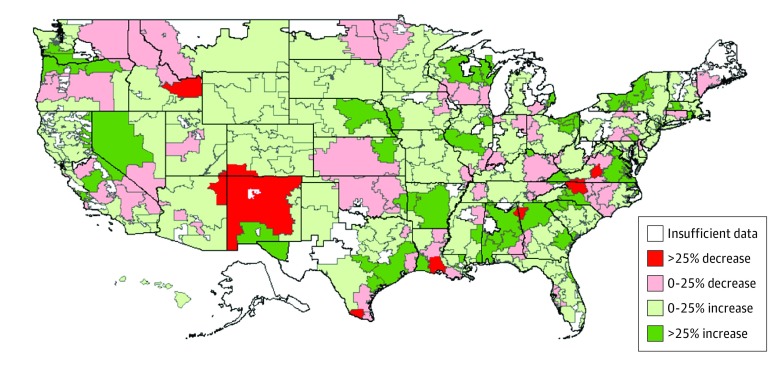
In the early period (2004-2006), the mean (SD) number of surgeries performed in each HRR was 325 (769), and the median was 101 surgeries. During the later period (2012-2014), the mean (SD) number of cataract surgeries in each HRR was 419 (819), and the median was 139 surgeries. There was considerable geographic variation in the proportion of cataract surgeries performed at ASCs rather than HOPDs. In the early period, the mountain states, desert southwest, and southwest Florida had large proportions of cataract surgeries performed at ASCs, while such proportions were much lower in the upper Midwest and Northeast (eFigure 1 in the Supplement). These same regions continued to have higher proportions of cataract surgeries performed at ASCs compared with other regions in the later period (eFigure 2 in the Supplement), although there was a widespread increase in the proportion of cataract surgeries performed in ASCs rather than HOPDs across much of the nation from 2004-2006 to 2012-2014 (Figure 2). Table 2 lists communities with the highest and lowest proportions of surgeries performed at ASCs rather than HOPDs in the early and late periods; eTable 2 in the Supplement lists communities with the largest change in proportions during these times.
Figure 2. Geographic Variation in the Change in Site of Surgery from 2004-2006 to 2012-2014.
Map showing the increase or decrease in proportion of cataract surgeries performed at ambulatory surgery centers from 2004-2006 to 2012-2014 by hospital referral region. Hospital referral regions with fewer than 20 patients undergoing cataract surgery in either 2004-2006 or 2012-2014 are reported as “insufficient data” (n = 42).
Table 2. Variation in Site of Cataract Surgery in Communities With at Least 100 Cataract Surgeries Performed.
| HRR | No. at ASCs | Total No. at ASCs + HOPDs | Cataract Surgeries Performed at ASCs, % |
|---|---|---|---|
| HRRs With the Lowest Proportion of Cataract Surgeries Performed at ASCs | |||
| 2004-2006 | |||
| Rochester, MN | 5 | 182 | 2.7 |
| Green Bay, WI | 7 | 198 | 3.5 |
| St. Paul, MN | 157 | 1097 | 14.3 |
| Hickory, NC | 15 | 100 | 15.0 |
| Appleton, WI | 31 | 198 | 15.7 |
| 2012-2014 | |||
| La Crosse, WI | 2 | 126 | 1.6 |
| Rochester, MN | 15 | 266 | 5.6 |
| Binghamton, NY | 7 | 116 | 6.0 |
| Waterloo, IA | 12 | 144 | 8.3 |
| Dubuque, IA | 42 | 416 | 10.1 |
| HRRs With the Highest Proportion of Cataract Surgeries Performed at ASCs | |||
| 2004-2006 | |||
| Hudson, FL | 672 | 680 | 98.8 |
| Bradenton, FL | 331 | 340 | 97.4 |
| Sun City, AZ | 366 | 377 | 97.1 |
| St. Petersburg, FL | 774 | 798 | 97.0 |
| Salem, OR | 186 | 193 | 96.4 |
| 2012-2014 | |||
| Pueblo, CO | 255 | 258 | 98.8 |
| St. Petersburg, FL | 662 | 671 | 98.7 |
| Bradenton, FL | 227 | 232 | 97.8 |
| Hattiesburg, MS | 130 | 134 | 97.0 |
| Sun City, AZ | 212 | 219 | 96.8 |
Abbreviations: ASC, ambulatory surgery center; HOPD, hospital outpatient department; HRR, hospital referral region.
Factors Associated With Undergoing Cataract Surgery at an ASC
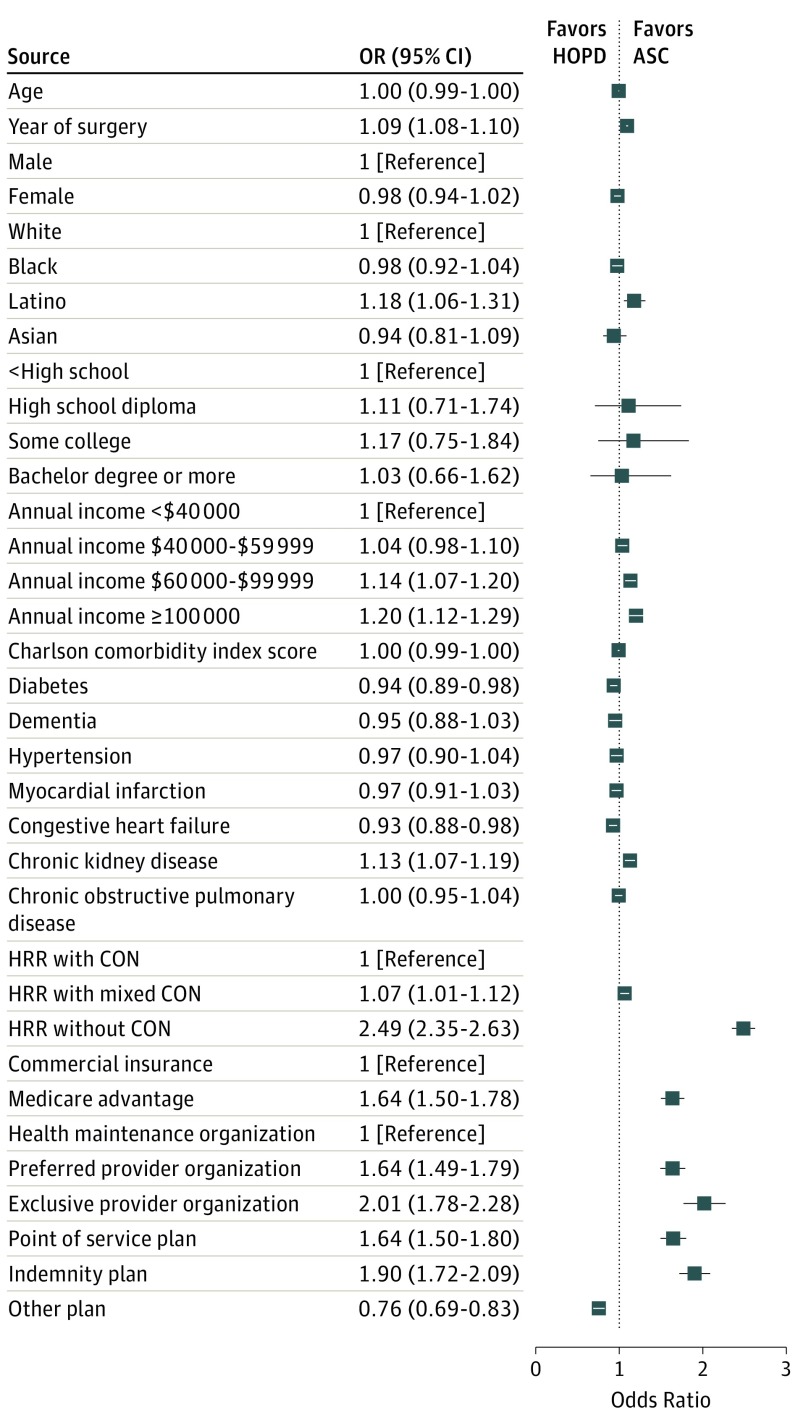
Older age (adjusted OR, 0.99; 95% CI, 0.99-1.00) was associated with a decreased likelihood of receiving surgery at an ASC. Compared with white individuals, Latino individuals had an 18% increased odds of undergoing cataract surgery at an ASC (OR, 1.18; 95% CI, 1.06-1.31). Compared with those with a household income less than $40 000, persons with incomes of $60 000-$99 000 had a 14% increased odds of undergoing cataract surgery at an ASC rather than an HOPD (OR, 1.14; 95% CI, 1.07-1.20); those with incomes of $100 000 or greater had a 20% increased odds of undergoing the surgery at an ASC (OR, 1.20; 95% CI, 1.12-1.29). Better overall health (lower Charlson comorbidity index score) was not associated with increased likelihood of undergoing cataract surgery at an ASC rather than an HOPD (OR, 1.00; 95% CI, 0.99-1.00). The presence of most concomitant medical conditions studied did not affect the odds of receiving surgery at an ASC either. Persons living in HRRs without CON laws were considerably more likely to have surgery at ASCs than at HOPDs (OR, 2.49; 95% CI, 2.35-2.63). The odds of undergoing cataract surgery at an ASC increased by 9.4% for each later calendar year the surgery took place (OR, 1.09; 95% CI, 1.08-1.10; P < .001) (Figure 3).
Figure 3. Factors Associated With Undergoing Cataract Surgery at an Ambulatory Surgery Center.
Multivariable logistic regression model identifying factors associated with undergoing cataract surgery at an ambulatory surgery center (ASC) rather than a hospital outpatient department (HOPD). The error bars indicate 95% CIs. CON indicates certificate of need law; HRR, hospital referral region; OR, odds ratio.
Trends in ASC Use for Other Ocular Surgeries
Like cataract surgery, other types of ocular surgeries were increasingly performed at ASCs rather than HOPDs from 2001 to 2014 (Figure 1). For glaucoma surgery, the proportion of surgeries performed at ASCs increased from 28.3% (478 of 1687) in 2001 to 66.6% (1247 of 1873) in 2014. Use of ASCs for cornea surgery rose from 36.8% (439 of 1192) in 2001 to 56.1% (594 of 1059) in 2014. For strabismus surgery, the proportion of surgeries performed at ASCs rose from 15.3% (220 of 1436) in 2001 to 35.6% (548 of 1538) in 2014. The proportion of retina surgeries performed at ASCs increased from 19.6% (790 of 4026) in 2001 to 40.9% (2677 of 6546) in 2014. The rate of increase in ASC use for cataract surgery of 2.34% per year was similar to the rate of increase for strabismus surgery of 1.84% per year (P = .08) and for retina surgery of 2.44% per year (P = .70). The rate of increase for glaucoma surgery (3.26% per year) was faster than cataract surgery (P = .002). The rate of increase for cornea surgery (1.68% per year) was slower than cataract surgery (P = .02).
Discussion
Over the past 14 years, use of ASCs for cataract surgery rose dramatically. The largest increase in ASC use for cataract surgery occurred from 2001 to 2006, although further increases were noted from 2007 to 2014. This increase in use occurred in many US communities from the early to the later period, such that in some locales, nearly every cataract surgery in the database took place at an ASC. Patients were more likely to undergo cataract surgery at an ASC rather than an HOPD if they were younger age, had higher income, lived in states without CON laws, and had surgery during later calendar years. Similar trends in ASC use to those observed for cataract surgery were noted for all of the subspecialty ocular surgeries studied.
Surgery performed at ASCs is less expensive for insurers than surgery performed at HOPDs. In 2014, the national average Medicare facility payment rate for cataract removal was $976 at an ASC and $1766 at an HOPD. One analysis estimated that cataract surgeries performed at ASCs rather than HOPDs saved Medicare $829 million in 2011. Ambulatory surgery centers also save money for beneficiaries through lower copayments; the average cataract surgery copayment in 2014 was approximately $190 at an ASC and $350 at an HOPD. Although the facility fee and the patient copayment are less for surgeries performed at ASCs, the physician payment is the same at both facility types. However, because some surgeons have partial ownership of the ASC where they perform surgery, they receive a portion of the facility payment plus the physician fee. This, coupled with improved surgeon efficiency, may explain some of the observed shift in surgical care from HOPDs to ASCs.
Although surgeries performed at ASCs are reimbursed at a lower rate than those performed at HOPDs, ASCs maintain their financial solvency through greater efficiency and patient throughput and lower turnover times, resulting in increased surgical volume. This is particularly beneficial for relatively quick surgeries like cataract extraction; many surgeries can be performed on a given day at a single ASC. Ambulatory surgery centers are more convenient than HOPDs for many patients because they are often closer to patients’ homes. Additionally, across all types of surgeries, the average surgical experience is reduced by at least 30 minutes when performed in an ASC compared with an HOPD.
When comparing and contrasting surgical care at ASCs and HOPDs, an important issue is patient safety. One advantage of HOPDs is that these facilities are often better equipped to deal with serious medical complications that may occur because they are typically attached to a hospital. A few high-profile cases of severe medical complications and deaths that occurred during surgeries performed at ASCs highlight the importance of this issue. Nevertheless, studies have demonstrated similar patient safety between the 2 facility types. However, the studies’ authors have recommended performing surgeries at ASCs only in selected patient populations with few medical comorbidities.
Whether ASCs are as safe as HOPDs for patients with multiple medical conditions is less clear. In one study, only 1 in 1000 patients without major preexisting medical comorbidities required hospitalization in the first postoperative week after cataract surgery, compared with 8 in 1000 among patients with 4 or more medical comorbidities. In our analyses, the overall health of the patients (according to their Charlson comorbidity index score) appeared not to be driving use of surgical care at one facility type vs another. Given the increasing trend toward topical and monitored anesthesia care with intravenous sedation for most anterior segment surgeries, including cataract extraction, coexisting medical comorbidities may be of lesser importance in the decision to perform surgery at an ASC vs an HOPD than in years past. Nevertheless, in our study, older enrollees were more likely to have surgery in an HOPD, suggesting that in selected patient groups, surgeons may feel more comfortable performing cataract surgery at an HOPD. Additional research is required to assess for differences in safety between the 2 facility types.
Of interest, wealthier enrollees were more likely to undergo cataract surgery at an ASC than at an HOPD. More affluent individuals may be more likely to live in communities with more ASCs or be more apt to seek care from surgeons who prefer to operate in these facilities. Because patient copayments tend to be higher for surgeries performed at HOPDs and a disproportionately greater number of lesser affluent patients undergo cataract surgery at these facilities, this may influence the ability for some lesser affluent patients to undergo cataract surgery, despite their possessing health insurance.
We also identified considerable geographic variation in the rate of cataract surgery performed at ASCs, ranging from less than 10% in some communities to nearly 100% in others. Unsurprisingly, during the later period (2012-2014), several communities with the lowest proportions of cataract surgeries performed at ASCs had large academic medical centers, such as in Rochester, Minnesota (5.6%), Iowa City, Iowa (15.9%), and Durham, North Carolina (16.4%). Most communities (74.6%) experienced an increase in ASC use for cataract surgery from 2004-2006 to 2012-2014, although approximately one-fourth of the communities studied experienced a decline. Certificate of need laws may be influencing some of the observed geographic variation, as they likely affect the number of ASCs present in a given community. Additionally, some health care systems have acquired ASCs and converted them to HOPDs to increase revenue; this may help explain the decline of ASC use for cataract surgery in some communities. Moreover, some insurers may have contracts with hospitals requiring patients to receive surgery at specific HOPDs. Furthermore, if many ophthalmologists who are practicing in a given community are members of one large group practice and there is a change in the sites where they operate (eg, the sale of an ASC to a hospital system, which then converts it to an HOPD), then this could greatly affect some of the observed trends. This may help explain the large decline in ASC use in selected communities.
Strengths and Limitations
A strength of these analyses is the use of a database with millions of enrollees, more than 350 000 of whom underwent cataract surgery. This large sample size enabled sophisticated modeling to evaluate patient-level factors associated with use of ASCs vs HOPDs for cataract surgery and to study geographic variation. To our knowledge, this is the first study reporting rates of ASC use for various ophthalmologic subspecialty surgeries and changes in rates over time.
Our study has limitations. These results may be nongeneralizable to patients outside this particular managed care network who have other forms of health insurance. Future work repeating these analyses using other data sources, such as Medicare claims, will assess the generalizability of these findings. Our database lacks information on the types of facilities at which the patients’ surgeons have privileges. Whether surgeons have privileges to perform surgeries at only ASCs or HOPDs or at both facility types would certainly affect the site of surgical care.
Conclusions
A major shift in ophthalmic surgical care in the United States from HOPDs to ASCs occurred over the past decade. Additional research is needed to assess whether this observed increase in the use of ASCs for cataract and other ocular surgeries affects overall access to surgery, surgical outcomes, patient safety, and societal costs.
eTable 1. Listing of the Current Procedural Terminology (CPT) and International Classification of Diseases (ICD-9-CM) billing codes capturing the various ocular surgeries of interest.
eTable 2. Hospital referral regions (HRRs) with the largest change in proportion of cataract surgeries done at ambulatory surgery centers (ASCs) from 2004-2006 to 2012-2014.
eFigure 1. Geographic variation in the proportion of cataract surgeries performed at an ambulatory surgery center during 2004-2006.
eFigure 2. Geographic variation in the proportion of cataract surgeries performed at an ambulatory surgery center during 2012-2014.
References
- 1.Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Report. 2009;(11):1-25. [PubMed] [Google Scholar]
- 2.Koenig L, Doherty J, Dreyfus J, Xanthaopoulos J An analysis of recent growth of ambulatory surgical centers: final report. http://www.cascacolorado.com/wp-content/uploads/2009/06/KNG-Health-ASC-Growth-Factors-Final-Report-6-012-09.pdf. Accessed May 8, 2017.
- 3.Kadhim M, Gans I, Baldwin K, Flynn J, Ganley T. Do surgical times and efficiency differ between inpatient and ambulatory surgery centers that are both hospital owned? J Pediatr Orthop. 2016;36(4):423-428. [DOI] [PubMed] [Google Scholar]
- 4.Shactman D. Specialty hospitals, ambulatory surgery centers, and general hospitals: charting a wise public policy course. Health Aff (Millwood). 2005;24(3):868-873. [DOI] [PubMed] [Google Scholar]
- 5.Higgins A, Veselovskiy G, Schinkel J. National estimates of price variation by site of care. Am J Manag Care. 2016;22(3):e116-e121. [PubMed] [Google Scholar]
- 6.Wynn BO, Hilborne LH, Hussey P, Sloss EM, Murphy E Medicare payment differentials across ambulatory settings. http://www.rand.org/content/dam/rand/pubs/working_papers/2008/RAND_WR602.pdf. Accessed May 8, 2017.
- 7.Robinson JC, Brown T, Whaley C. Reference-based benefit design changes consumers’ choices and employers’ payments for ambulatory surgery. Health Aff (Millwood). 2015;34(3):415-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hollingsworth JM, Birkmeyer JD, Ye Z, Miller DC. Specialty-specific trends in the prevalence and distribution of outpatient surgery: implications for payment and delivery system reforms. Surg Innov. 2014;21(6):560-565. [DOI] [PubMed] [Google Scholar]
- 9.Vaziri K, Moshfeghi DM, Hernandez-Boussard T, Callaway NF, Moshfeghi AA. Ambulatory surgery center utilization by vitreoretinal surgeons: 1999-2011. Ophthalmic Surg Lasers Imaging Retina. 2015;46(3):355-361. [DOI] [PubMed] [Google Scholar]
- 10.American Medical Association International Classification of Diseases, Ninth Revision, Clinical Modification. Chicago, IL: American Medical Association Press; 2006. [Google Scholar]
- 11.American Medical Association Current Procedural Terminology: Professional Edition. Chicago, IL: American Medical Association Press; 2006. [Google Scholar]
- 12.Stein JD, Lum F, Lee PP, Rich WL III, Coleman AL. Use of health care claims data to study patients with ophthalmologic conditions. Ophthalmology. 2014;121(5):1134-1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kauh CY, Blachley TS, Lichter PR, Lee PP, Stein JD. Geographic variation in the rate and timing of cataract surgery among US communities. JAMA Ophthalmol. 2016;134(3):267-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wubben TJ, Talwar N, Blachley TS, et al. Rates of vitrectomy among enrollees in a United States managed care network, 2001-2012. Ophthalmology. 2016;123(3):590-598. [DOI] [PubMed] [Google Scholar]
- 15.Wang SY, Hall J, Pollack CE, et al. Associations between end-of-life cancer care patterns and Medicare expenditures. J Natl Compr Canc Netw. 2016;14(8):1001-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Donohue JM, Normand SL, Horvitz-Lennon M, Men A, Berndt ER, Huskamp HA. Regional variation in physician adoption of antipsychotics: impact on US Medicare expenditures. J Ment Health Policy Econ. 2016;19(2):69-78. [PMC free article] [PubMed] [Google Scholar]
- 17.National Conference of State Legislatures CON-Certificate of Need state laws. http://www.ncsl.org/research/health/con-certificate-of-need-state-laws.aspx#Regulated. Accessed May 1, 2017.
- 18.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245-1251. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen C, Milstein A, Hernandez-Boussard T, Curtin CM. The effect of moving carpal tunnel releases out of hospitals on reducing United States health care charges. J Hand Surg Am. 2015;40(8):1657-1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fabricant PD, Seeley MA, Rozell JC, et al. Cost savings from utilization of an ambulatory surgery center for orthopaedic day surgery. J Am Acad Orthop Surg. 2016;24(12):865-871. [DOI] [PubMed] [Google Scholar]
- 21.Medicare Payment Advisory Commission Report to the Congress: Medicare payment policy. http://www.medpac.gov/docs/default-source/reports/march-2016-report-to-the-congress-medicare-payment-policy.pdf?sfvrsn=0. Accessed May 8, 2017.
- 22.Fulton B, Kim S Medicare cost savings tied to ambulatory surgery centers. https://tascs.memberclicks.net/assets/docs/medicare%20cost%20savings%20tied%20to%20ascs.pdf. Accessed May 8, 2017.
- 23.Nantz J. HOPD or ASC: 5 questions for hospitals to consider. http://www.beckershospitalreview.com/hospital-management-administration/hopd-or-asc-5-questions-for-hospitals-to-consider.html. Accessed May 8, 2017. [Google Scholar]
- 24.Ifft D. Moving cataract surgery into the practice setting: CMS inquiry into the concept raises many questions. http://www.ophthalmologymanagement.com/supplements/2015/october-2015/october-2015-the-ophthalmic-asc/moving-cataract-surgery-into-the-practice-setting. Accessed May 8, 2017. [Google Scholar]
- 25.Munnich EL, Parente ST. Procedures take less time at ambulatory surgery centers, keeping costs down and ability to meet demand up. Health Aff (Millwood). 2014;33(5):764-769. [DOI] [PubMed] [Google Scholar]
- 26.Rice S. Joan Rivers' death highlights risks for seniors in outpatient surgery. http://www.modernhealthcare.com/article/20140913/MAGAZINE/309139963. Accessed March 1, 2017. [PubMed] [Google Scholar]
- 27.Brolin TJ, Mulligan RP, Azar FM, Throckmorton TW. Neer Award 2016: outpatient total shoulder arthroplasty in an ambulatory surgery center is a safe alternative to inpatient total shoulder arthroplasty in a hospital: a matched cohort study. J Shoulder Elbow Surg. 2017;26(2):204-208. [DOI] [PubMed] [Google Scholar]
- 28.Goyal KS, Jain S, Buterbaugh GA, Imbriglia JE. The safety of hand and upper-extremity surgical procedures at a freestanding ambulatory surgery center: a review of 28,737 cases. J Bone Joint Surg Am. 2016;98(8):700-704. [DOI] [PubMed] [Google Scholar]
- 29.Nezhat C, Main J, Paka C, Soliemannjad R, Parsa MA. Advanced gynecologic laparoscopy in a fast-track ambulatory surgery center. JSLS. 2014;18(3):e2014.00291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Billing PS, Crouthamel MR, Oling S, Landerholm RW. Outpatient laparoscopic sleeve gastrectomy in a free-standing ambulatory surgery center: first 250 cases. Surg Obes Relat Dis. 2014;10(1):101-105. [DOI] [PubMed] [Google Scholar]
- 31.Wang SY, Blachley TS, Andrews CA, Ayanian JZ, Lee PP, Stein JD. Hospitalization after cataract surgery in a nationwide managed-care population. PLoS One. 2016;11(2):e0149819. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Listing of the Current Procedural Terminology (CPT) and International Classification of Diseases (ICD-9-CM) billing codes capturing the various ocular surgeries of interest.
eTable 2. Hospital referral regions (HRRs) with the largest change in proportion of cataract surgeries done at ambulatory surgery centers (ASCs) from 2004-2006 to 2012-2014.
eFigure 1. Geographic variation in the proportion of cataract surgeries performed at an ambulatory surgery center during 2004-2006.
eFigure 2. Geographic variation in the proportion of cataract surgeries performed at an ambulatory surgery center during 2012-2014.