Abstract
Importance
The overprescription of pain medications has been implicated as a driver of the burgeoning opioid epidemic; however, few guidelines exist regarding the appropriateness of opioid pain medication prescriptions after surgery.
Objectives
To describe patterns of opioid pain medication prescriptions after common surgical procedures and determine the appropriateness of the prescription as indicated by the rate of refills.
Design, Setting, and Participants
The Department of Defense Military Health System Data Repository was used to identify opioid-naive individuals 18 to 64 years of age who had undergone 1 of 8 common surgical procedures between January 1, 2005, and September 30, 2014. The adjusted risk of refilling an opioid prescription based on the number of days of initial prescription was modeled using a generalized additive model with spline smoothing.
Exposures
Length of initial prescription for opioid pain medication.
Main Outcomes and Measures
Need for an additional subsequent prescription for opioid pain medication, or a refill.
Results
Of the 215 140 individuals (107 588 women and 107 552 men; mean [SD] age, 40.1 [12.8] years) who underwent a procedure within the study time frame and received and filled at least 1 prescription for opioid pain medication within 14 days of their index procedure, 41 107 (19.1%) received at least 1 refill prescription. The median prescription lengths were 4 days (interquartile range [IQR], 3-5 days) for appendectomy and cholecystectomy, 5 days (IQR, 3-6 days) for inguinal hernia repair, 4 days (IQR, 3-5 days) for hysterectomy, 5 days (IQR, 3-6 days) for mastectomy, 5 days (IQR, 4-8 days) for anterior cruciate ligament repair and rotator cuff repair, and 7 days (IQR, 5-10 days) for discectomy. The early nadir in the probability of refill was at an initial prescription of 9 days for general surgery procedures (probability of refill, 10.7%), 13 days for women’s health procedures (probability of refill, 16.8%), and 15 days for musculoskeletal procedures (probability of refill, 32.5%).
Conclusions and Relevance
Ideally, opioid prescriptions after surgery should balance adequate pain management against the duration of treatment. In practice, the optimal length of opioid prescriptions lies between the observed median prescription length and the early nadir, or 4 to 9 days for general surgery procedures, 4 to 13 days for women’s health procedures, and 6 to 15 days for musculoskeletal procedures.
This cohort study uses data from the Department of Defense Military Health System Data Repository to describe patterns of opioid pain medication prescriptions after common surgical procedures and determine the appropriateness of the prescription as indicated by the rate of refills.
Key Points
Question
What are the optimal ranges of initial durations of opioid prescriptions in a cohort of opioid-naive patients who have undergone common surgical procedures?
Findings
In this cohort study of 215 140 individuals, the median observed prescription lengths were 4 days for general surgery procedures, 4 days for women’s health procedures, and 6 days for musculoskeletal procedures. The prescription lengths associated with lowest requirement for refill were 9 days for general surgery, 13 days for women’s health, and 15 days for musculoskeletal procedures.
Meaning
The ideal initial prescription duration likely falls between the observed median and the modeled nadir in refill rate.
Introduction
As rates of opioid prescribing have increased dramatically in recent years, the overprescription of pain medications has been implicated as a driver of the burgeoning opioid epidemic and the associated increases in overdose deaths in the United States. It is estimated that as many as 259 million opioid prescriptions were issued in 2012, four times the number prescribed in 1999. This increase in opioid prescriptions has come at a cost, however, including increased rates of overdose deaths, as well as expenditures associated with the treatment of prescription opioid abuse and dependence.
To address these issues, governmental efforts limiting the length of initial prescriptions of opioid pain medication, typically to fewer than 7 days, have recently been passed in several states, including New York and Massachusetts. Prescription drug monitoring programs have also become increasingly common despite a lack of evidence regarding appropriate duration of prescriptions of opioid pain medication or the efficacy of such legislation.
As a result, uncertainty remains regarding optimal prescribing practices for opioid pain medications, particularly in the setting of postoperative, outpatient pain management, where few guidelines exist. In this context, we investigated prescription patterns of opioid pain medications after common surgical procedures. We also endeavored to determine the appropriateness of the prescription as indicated by the rate of refills and to develop recommendations regarding optimal prescription length after common surgical procedures.
Methods
Patient Data and Cohort Selection
This project used data from the Military Health System Data Repository and the TRICARE insurance program, the specifics of which have been described previously. The TRICARE insurance program covers more than 9 million beneficiaries, including members of the Department of Defense, dependents, retirees, and those with medical disabilities. Only 20% of covered individuals are active members of the US military. The TRICARE insurance program is not involved in the delivery of health care in combat zones, and beneficiaries are not obligated to receive care in the Veterans Affairs system. This study was approved as an exempt protocol and written informed consent was waived by the Partners Healthcare Institutional Review Board.
The Military Health System Data Repository was queried by International Classification of Diseases, Ninth Revision (ICD-9) and Current Procedural Terminology procedure codes to identify all patients 18 to 64 years of age who underwent 1 of 8 common surgical procedures (cholecystectomy, appendectomy, inguinal hernia repair, anterior cruciate ligament reconstruction, rotator cuff tear repair, discectomy, mastectomy, and hysterectomy; see eAppendix in the Supplement for ICD-9 and Current Procedural Terminology codes) between January 1, 2005, and September 30, 2014. Enrollees who underwent more than 1 procedure within 6 months of their index operation were excluded, given the potential for reoperation to confound requirements for opioid pain medications, as were those who could not be evaluated for at least 1 year before and after their operation. Individuals with an opioid prescription within the 6 months preceding the index procedure were similarly excluded. Individuals with initial prescription durations longer than 90 days were also excluded.
Demographic information including age, biological sex, race/ethnicity, marital status, sponsor rank (categorized as Junior enlisted [lowest 4 ranks in any branch], Senior enlisted [noncommissioned officers], Officers, and Other [cadets and warrant officers]), and beneficiary category were abstracted for all individuals in the study. The modified Charlson Comorbidity Index was used to account for medical comorbidities. Postoperative complications were also recorded using a previously published algorithm using ICD-9 coding.
Information on prescription claims billed to TRICARE is available through the Military Health System Data Repository. This information was queried for the medications defined by the Drug Enforcement Administration as opioid combinations, opioid partial agonists, or opioid agonists in categories II (high abuse potential) or III (moderate risk of dependence). For the purposes of this investigation, refill was defined as repeat prescription within 14 days of the end date of the initial prescription.
Adjusted Model
The adjusted risk of opioid prescription refill based on the number of days in the initial prescription was modeled using a generalized additive model with spline smoothing. In contrast with generalized linear models that assume a linear association between the dependent and independent variables, generalized additive models replace the linear assumptions with smooth functions, creating a nonparametric function that can estimate a greater variety of associations. Covariates in the model included age, biological sex, race/ethnicity, sponsor rank as a proxy for socioeconomic status, preoperative history of substance abuse, depression, fibromyalgia, and postoperative complications. The modified Charlson Comorbidity Index was used to adjust for comorbidities. By plotting risk of refill as a function of duration of the initial prescription, we were able to identify the adjusted risk of prescription refill associated with the length of initial opioid prescription as well as the initial prescription duration associated with the lowest modeled risk of refill, or the nadir of the adjusted curve. P < .05 and 95% CIs exclusive of 0.0 were used as the criteria for statistical significance. A stratified analysis was also performed comparing active duty TRICARE enrollees with nonactive-duty individuals. Data manipulation and statistical analysis were performed using SAS, version 9.4 (SAS Institute Inc).
Results
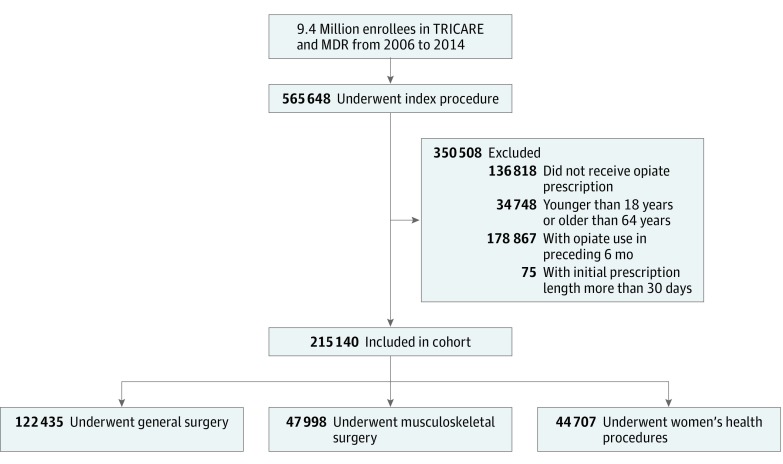
In the period under study, 565 648 individuals underwent 1 of the 8 procedures of interest and 428 830 (75.8%) filled at least 1 opioid pain medication prescription in the 14 days after the procedure (Figure 1). Among these individuals, 34 748 (8.1%) were excluded owing to age restrictions and an additional 178 867 were excluded because they had filled an opioid pain medication prescription in the 6 months prior to their index procedure. An additional 75 individuals had an initial prescription length of longer than 30 days and were also excluded. This left a final 215 140 individuals within the study cohort. The mean (SD) age of the final study population was 40.1 (12.8) years. A total of 107 552 individuals (50.0%) were male, and 129 357 participants (60.1%) were white (Table 1). Most of the study population had a modified Charlson Comorbidity Index score of 0 (201 995 [93.9%]). General surgery procedures were performed in 122 435 individuals, while 47 998 underwent musculoskeletal procedures and 44 707 received a mastectomy or hysterectomy.
Figure 1. Study Cohort.
MDR indicates Military Health System Data Repository.
Table 1. Demographics.
| Characteristic | No. (%) (N = 215 140) |
|---|---|
| Age, y | |
| 18-24 | 32 786 (15.2) |
| 25-34 | 44 602 (20.7) |
| 35-44 | 53 134 (24.7) |
| 45-64 | 84 618 (39.3) |
| Male | 107 552 (50) |
| Married | 169 414 (78.8) |
| White race/ethnicity | 129 357 (60.1) |
| Sponsor rank | |
| Officer | 37 796 (17.6) |
| Enlisted junior | 33 938 (15.8) |
| Enlisted senior | 135 943 (63.2) |
| Others | 6629 (3.1) |
| Beneficiary category | |
| Active duty | 78 455 (36.5) |
| Retired | 36 453 (16.9) |
| Dependent | 95 477 (44.4) |
| Others | 4755 (2.2) |
| Hospital region | |
| South | 125 150 (58.2) |
| West | 55 033 (25.6) |
| Midwest | 23 033 (10.7) |
| Northeast | 9817 (4.6) |
| Charlson comorbidity index score | |
| 0 | 201 995 (93.9) |
| 1 | 7452 (3.5) |
| ≥2 | 5693 (2.6) |
Initial Duration of Opioid Prescription
Among patients undergoing general surgery procedures, the median duration of initial opioid pain medication prescription was 4 days (interquartile range [IQR], 3-5 days) for appendectomy and cholecystectomy and 5 days (IQR, 3-6 days) for inguinal hernia repair (Table 2). Among musculoskeletal procedures, the median duration of initial prescription was 5 days (IQR, 4-8 days) for anterior cruciate ligament repair and rotator cuff repair and 7 days (IQR, 5-10 days) for discectomy. The median duration of initial opioid pain medication prescription was 5 days (IQR, 3-6 days) for mastectomy and 4 days (IQR, 3-5 days) for hysterectomy.
Table 2. Opioid Pain Medication Prescription Duration Information by Procedure Type After Common Surgical Procedures.
| Characteristic | Appendectomy (n = 34 516) |
Choleystectomy (n = 48 622) |
Inguinal Hernia Repair (n = 39 297) |
ACL Repair (n = 16 511) |
Rotator Cuff Repair (n = 14 840) |
Discectomy (n = 16 647) |
Mastectomy (n = 5233) |
Hysterectomy (n = 39 474) |
|---|---|---|---|---|---|---|---|---|
| Initial opioid prescription duration, d | ||||||||
| Mean (SD) | 5.79 (6.14) | 5.72 (5.79) | 6.26 (6.46) | 7.37 (5.67) | 6.90 (5.21) | 9.32 (6.43) | 6.23 (5.89) | 5.73 (5.74) |
| Median (IQR) [range] | 4 (3-5) [1-30] | 4 (3-5) [1-30] | 5 (3-6) [1-30] | 5 (4-8) [1-30] | 5 (4-8) [1-30] | 7 (5-10) [1-30] | 5 (3-6) [1-30] | 4 (3-5) [1-30] |
Abbreviations: ACL, anterior cruciate ligament; IQR, interquartile range.
Opioid Prescription Refill Rates
Observed prescription refill rates ranged from 11.3% (5513 of 48 622) for cholecystectomy to 39.3% (6485 of 16 511) after anterior cruciate ligament repair (Table 3). The median time to refill was 6 days (appendectomy, cholecystectomy, and inguinal hernia repair) to 10 days (discectomy) from the date of the initial prescription. The median duration of a refill prescription ranged from 4 days (appendectomy, cholecystectomy, hernia repair, and hysterectomy) to 8 days (discectomy).
Table 3. Opioid Pain Medication Refill Rate and Duration by Procedure Type for Opioid-Naive Patients After Common Surgical Procedures.
| Characteristic | Appendectomy (n = 34 516) |
Cholecystectomy (n = 48 622) |
Inguinal Hernia Repair (n = 39 297) |
ACL Repair (n = 16 511) |
Rotator Cuff Repair (n = 14 840) |
Discectomy (n = 16 647) |
Mastectomy (n = 5233) |
Hysterectomy (n = 39 474) |
|---|---|---|---|---|---|---|---|---|
| Enrollees receiving ≥1 refill, No. (%) | 4676 (13.6) | 5513 (11.3) | 5611 (14.3) | 6485 (39.3) | 5337 (36.0) | 5017 (30.1) | 1650 (31.5) | 6818 (17.3) |
| Time to refill, d | ||||||||
| Mean (SD) | 7.10 (5.65) | 7.30 (5.73) | 7.20 (5.52) | 7.79 (4.73) | 8.50 (5.48) | 11.29 (6.71) | 8.48 (5.53) | 8.03 (5.31) |
| Median (IQR) [range] | 6 (3-10) [1-45] |
6 (3-10) [1-45] |
6 (3-10) [1-45] |
7 (5-11) [1-44] |
8 (4-12) [1-45] |
10 (7-15) [1-45] |
7 (5-12) [1-44] |
7 (4-11) [1-45] |
| Duration of first refill, d | ||||||||
| Mean (SD) | 6.22 (7.19) | 6.44 (7.47) | 6.49 (7.43) | 7.67 (8.09) | 7.40 (7.50) | 10.51 (7.85) | 6.42 (6.43) | 6.02 (6.44) |
| Median (IQR) [range] | 4 (3-5) [1-60] |
4 (3-6) [1-90] |
4 (3-5) [1-42] |
5 (4-8) [1-300] |
5 (4-8) [1-300] |
8 (5-13) [1-84] |
5 (3-7) [1-60] |
4 (3-5) [1-41] |
Abbreviations: ACL, anterior cruciate ligament; IQR, interquartile range.
Adjusted Results
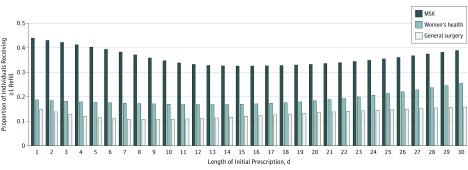
In the adjusted model, the modeled proportion of individuals requiring a refill prescription varied based on procedure type and the duration of initial prescription, ranging from 10.7% for those undergoing general surgery procedures who received an initial prescription of 9 days’ duration to 43.9% for those undergoing musculoskeletal procedures who received an initial prescription of 1 day’s duration (Figure 2). The early nadir in the proportion of patients requiring refill after musculoskeletal procedures was 32.5% at an initial prescription duration of 15 days (Figure 2). Among general surgery procedures, the early nadir in the proportion of patients requiring a refill was 10.7% at 9 days. For mastectomy and hysterectomy, the early nadir was 16.8% at 13 days. When stratified by beneficiary category, the overall early nadir in refill rate was similar between active duty individuals and all others, with the early nadir at 16.5% associated with an initial prescription duration of 16 days for those on activity duty and 12.8% at 15 days for all others. By procedure category, when active duty individuals were excluded from the analysis, for all other individuals, the nadir in the proportion of individuals requiring a refill was 10.0% for general surgery procedures and was associated with an initial prescription length of 8 days, 16.2% for women’s health procedures at 13 days, and 30.2% for musculoskeletal procedures at 15 days.
Figure 2. Modeled Proportion of Individuals Requiring Opioid Pain Medication Refill by Length of Initial Prescription by Procedure Group.
Adjusted proportion of individuals requiring repeated opioid prescription after procedure by duration of initial prescription. Risk was adjusted for age, sex, race/ethnicity, socioeconomic status, and postoperative complications. The modified Charlson Comorbidity Index was used to adjust for comorbidities. MSK indicates musculoskeletal.
Discussion
In this study including more than 215 000 opioid-naive patients undergoing a variety of general surgical, orthopedic, and women’s health procedures, the median initial opioid prescription duration ranged from 4 to 7 days, and 11.3% to 39.3% of patients required at least 1 refill, depending on procedure undergone. The modeled early nadir in rate of prescription refill was 9 days after general surgery procedures, 13 days after breast and gynecologic procedures, and 15 days after orthopedic and neurosurgical procedures.
These results expand on previously published work examining prescribing patterns of pain medications after surgical interventions in opioid-naive patients, which has thus far been limited largely to single-institution trials. A strength of this study is its inclusion of a large population considered to be nationally representative in many respects. We were also able to include a variety of procedures across general, orthopedic, neurosurgical, and gynecologic care. In terms of generalizability, only procedures for which patients are commonly discharged to home were included, given the fact that discharge to a rehabilitation or skilled nursing facility would likely confound prescription practices. Patients with preoperative pain medication use were also excluded from the study given its effect on postprocedure pain requirements as well as recovery times. More than 40% of the cohort who filled an opioid pain medication prescription after their index procedure had received at least 1 opioid prescription in the 6 months preceding surgery, which is notable given results that suggest that individuals taking preoperative narcotics have poorer outcomes.
Orthopedic procedures appeared to be associated with the highest refill rates and the highest median length of initial prescriptions, which is in line with previous work that showed that chronic use of postoperative opioid medications was higher after orthopedic and neurosurgical procedures. For noncancer pain, orthopedic surgeons prescribe opioids more frequently than any other provider type and, among Medicare beneficiaries, have the highest frequency of opioid pain medication claims of any surgical specialty.
In terms of guidelines for pain management, there are relatively few efforts that help inform evidence-based prescribing guidelines in the postoperative, outpatient setting. The American College of Occupational and Environmental Medicine guidelines on opioid treatment include postoperative pain, but the recommendations are limited to screening patients who continue opioid pain medications beyond the second postoperative week, prescribing a maximum daily dose of 50 mg morphine equivalent in opioid-naive patients, and discontinuing opioids for patients who have reached meaningful functional recovery. The American Pain Society recommends instructing patients on opioid use at the transition to outpatient care but otherwise has no recommendations on type or duration of analgesia. The Institute for Clinical Systems Improvement recommends limiting initial prescriptions to 3 days or 20 tablets with appropriate adjuncts, education, and follow-up, without specification regarding the type of procedure performed.
The optimal length of opioid prescription after common surgical procedures likely lies between the observed median prescription length and the early nadir in the modeled probability of refill: 4 to 9 days for general surgery procedures, 4 to 13 days for women’s health procedures, and 6 to 15 days for musculoskeletal procedures. Although a 7-day limit on initial opioid prescription appears to be adequate for many common general surgery and gynecologic procedures, for patients undergoing orthopedic and neurosurgical interventions, a 7-day limit may be inappropriately restrictive and place an undue burden on patients and clinicians.
Limitations
This study is not without limitations. It addresses only prescription opioid use within this population and cannot address opioid medications obtained through other means. It also does not capture rates of unused prescriptions, which have been shown to be as high as 70% in some groups. Similarly, information on use of nonopioid adjuncts, including acetaminophen and nonsteroidal anti-inflammatory drugs, is also not available within the current data set; however, these medications likely affect postoperative opioid use. Specific procedural approaches and techniques as well as intraoperative anesthesia adjuncts may also affect postoperative pain control. However, we were unable to make determinations regarding these details in light of the claims-based nature of the information presently available through the Military Health System Data Repository. Although the concern could be raised that this study represents only the experience of a military population, active duty members of the military represent a minority of this cohort and, in a sensitivity analysis, risk of prescription refill was similar between groups. Furthermore, prior work has found this population to be sociodemographically similar to individuals younger than 65 years of age among the US population as a whole. Finally, data were available only for prescription days rather than the number of pills or tablets issued. However, given that opioid legislation thus far has focused primarily on limiting the number of prescription days rather than quantity, these data are directly comparable with currently available guidelines.
Despite these limitations, this work highlights the wide variation in prescribing patterns for postoperative pain management among surgeons as well as the variability in opioid requirements between procedures and patients. Furthermore, it offers empirical guidance to clinicians regarding opioid prescribing practices after surgery. Although 7 days appears to be more than adequate for many patients undergoing common general surgery and gynecologic procedures, prescription lengths likely should be extended to 10 days, particularly after common neurosurgical and musculoskeletal procedures, recognizing that as many as 40% of patients may still require 1 refill at a 7-day limit.
Conclusions
An opioid prescription after surgery should balance adequate pain treatment with minimizing the duration of treatment and potential for medication complications including issues with dependence. Although 7-day limits on initial opioid pain medication prescriptions are likely adequate in many settings, and indeed also sufficient for many common general surgery and gynecologic procedures, in the postoperative setting, particularly after many orthopedic and neurosurgical procedures, a 7-day limit may be inappropriately restrictive. Critically, further work is needed to better identify the 10% to 30% of patients who will require more intensive pain management to better tailor postoperative pain regimens to these individuals.
eAppendix. ICD-9 and Current Procedural Terminology Codes
References
- 1.Dart RC, Surratt HL, Cicero TJ, et al. . Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372(3):241-248. [DOI] [PubMed] [Google Scholar]
- 2.Hill MV, McMahon ML, Stucke RS, Barth RJ Jr. Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg. 2017;265(4):709-714. [DOI] [PubMed] [Google Scholar]
- 3.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624-1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paulozzi LJ, Mack KA, Hockenberry JM; Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control, CDC . Vital signs: variation among states in prescribing of opioid pain relievers and benzodiazepines—United States, 2012. MMWR Morb Mortal Wkly Rep. 2014;63(26):563-568. [PMC free article] [PubMed] [Google Scholar]
- 5.Florence CS, Zhou C, Luo F, Xu L. The Economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54(10):901-906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller J. Governor Baker signs opioid bill. Boston Globe March 14, 2016. http://www.bostonglobe.com/metro/2016/03/14/baker-due-sign-opioid-bill-monday/EYWh7oJXvKCRguHErxrWhI/story.html. Accessed December 5, 2016.
- 7.Huetteman E. Senate approves bill to combat opioid addiction crisis. New York Times July 13, 2016. https://www.nytimes.com/2016/07/14/us/politics/senate-opioid-addiction-bill.html. Accessed December 5, 2016.
- 8.Irvine JM, Hallvik SE, Hildebran C, Marino M, Beran T, Deyo RA. Who uses a prescription drug monitoring program and how? insights from a statewide survey of Oregon clinicians. J Pain. 2014;15(7):747-755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin DH, Lucas E, Murimi IB, et al. . Physician attitudes and experiences with Maryland’s prescription drug monitoring program (PDMP). Addiction. 2017;112(2):311-319. [DOI] [PubMed] [Google Scholar]
- 10.Meara E, Horwitz JR, Powell W, et al. . State legal restrictions and prescription-opioid use among disabled adults. N Engl J Med. 2016;375(1):44-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chou R, Gordon DB, de Leon-Casasola OA, et al. . Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council [published correction appears in J Pain. 2016;17(4):508-510]. J Pain. 2016;17(2):131-157. [DOI] [PubMed] [Google Scholar]
- 12.Hegmann KT, Weiss MS, Bowden K, et al. ; American College of Occupational and Environmental Medicine . ACOEM practice guidelines: opioids for treatment of acute, subacute, chronic, and postoperative pain. J Occup Environ Med. 2014;56(12):e143-e159. [DOI] [PubMed] [Google Scholar]
- 13.Schoenfeld AJ, Jiang W, Harris MB, et al. . Association between race and postoperative outcomes in a universally insured population vs patients in the state of California. Ann Surg. 2017;266(2):267-273. [DOI] [PubMed] [Google Scholar]
- 14.Zogg CK, Jiang W, Chaudhary MA, et al. . Racial disparities in emergency general surgery: Do differences in outcomes persist among universally insured military patients? J Trauma Acute Care Surg. 2016;80(5):764-775. [DOI] [PubMed] [Google Scholar]
- 15.Stewart KA, Higgins PC, McLaughlin CG, Williams TV, Granger E, Croghan TW. Differences in prevalence, treatment, and outcomes of asthma among a diverse population of children with equal access to care: findings from a study in the military health system. Arch Pediatr Adolesc Med. 2010;164(8):720-726. [DOI] [PubMed] [Google Scholar]
- 16.Bagchi AD, Stewart K, McLaughlin C, Higgins P, Croghan T. Treatment and outcomes for congestive heart failure by race/ethnicity in TRICARE. Med Care. 2011;49(5):489-495. [DOI] [PubMed] [Google Scholar]
- 17.Gimbel RW, Pangaro L, Barbour G. America’s “undiscovered” laboratory for health services research. Med Care. 2010;48(8):751-756. [DOI] [PubMed] [Google Scholar]
- 18.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-619. [DOI] [PubMed] [Google Scholar]
- 19.Hastie T, Tibshirani R. Generalized additive models. Stat Sci. 1986;1(3):297-310. doi: 10.1214/ss/1177013604 [DOI] [PubMed] [Google Scholar]
- 20.Jiang X, Orton M, Feng R, et al. . Chronic opioid usage in surgical patients in a large academic center. Ann Surg. 2017;265(4):722-727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li Y, Stocchi L, Cherla D, Liu X, Remzi FH. Association of preoperative narcotic use with postoperative complications and prolonged length of hospital stay in patients with Crohn disease. JAMA Surg. 2016;151(8):726-734. [DOI] [PubMed] [Google Scholar]
- 22.Morris BJ, Sciascia AD, Jacobs CA, Edwards TB. Preoperative opioid use associated with worse outcomes after anatomic shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25(4):619-623. [DOI] [PubMed] [Google Scholar]
- 23.Zywiel MG, Stroh DA, Lee SY, Bonutti PM, Mont MA. Chronic opioid use prior to total knee arthroplasty. J Bone Joint Surg Am. 2011;93(21):1988-1993. [DOI] [PubMed] [Google Scholar]
- 24.Lawrence JTR, London N, Bohlman HH, Chin KR. Preoperative narcotic use as a predictor of clinical outcome: results following anterior cervical arthrodesis. Spine (Phila Pa 1976). 2008;33(19):2074-2078. [DOI] [PubMed] [Google Scholar]
- 25.Sun EC, Darnall BD, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;176(9):1286-1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ringwalt C, Gugelmann H, Garrettson M, et al. . Differential prescribing of opioid analgesics according to physician specialty for Medicaid patients with chronic noncancer pain diagnoses. Pain Res Manag. 2014;19(4):179-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen JH, Humphreys K, Shah NH, Lembke A. Distribution of opioids by different types of Medicare prescribers. JAMA Intern Med. 2016;176(2):259-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Institute for Clinical Systems Improvement Pain: assessment, non-opioid treatment approaches and opioid management. https://www.icsi.org/guidelines__more/catalog_guidelines_and_more/catalog_guidelines/catalog_neurological_guidelines/pain/. Revised September 2016. Accessed August 14, 2017.
- 29.Clark JY, Thompson IM. Military rank as a measure of socioeconomic status and survival from prostate cancer. South Med J. 1994;87(11):1141-1144. [DOI] [PubMed] [Google Scholar]
- 30.Schoenfeld AJ, Goodman GP, Burks R, Black MA, Nelson JH, Belmont PJ Jr. The influence of musculoskeletal conditions, behavioral health diagnoses, and demographic factors on injury-related outcome in a high-demand population. J Bone Joint Surg Am. 2014;96(13):e106. doi: 10.2106/JBJS.M.01050 [DOI] [PubMed] [Google Scholar]
- 31.Tarman GJ, Kane CJ, Moul JW, et al. . Impact of socioeconomic status and race on clinical parameters of patients undergoing radical prostatectomy in an equal access health care system. Urology. 2000;56(6):1016-1020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. ICD-9 and Current Procedural Terminology Codes