Key Points
Question
What are the drivers of payment variation in 90-day coronary artery bypass grafting episodes of care?
Findings
In this cohort study of 5910 patients, the highest coronary artery bypass grafting payment quartile hospitals, when compared with the lowest payment quartile hospitals, had significantly higher index hospitalization payments (15%), professional payments (34%), postacute care payments (30%), and readmission payments (35%). These differences were driven by increased use of evaluation and management services, higher utilization of inpatient rehabilitation, and patients with multiple readmissions.
Meaning
Hospitals and clinicians entering bundled payment programs for coronary artery bypass grafting should work to understand local sources of variation, with a focus on inpatient evaluation and management services, postdischarge rehabilitation care, and patients at risk for multiple readmissions.
Abstract
Importance
Coronary artery bypass grafting (CABG) is scheduled to become a mandatory Medicare bundled payment program in January 2018. A contemporary understanding of 90-day CABG episode payments and their drivers is necessary to inform health policy, hospital strategy, and clinical quality improvement activities. Furthermore, insight into current CABG payments and their variation is important for understanding the potential effects of bundled payment models in cardiac care.
Objective
To examine CABG payment variation and its drivers.
Design, Setting, and Participants
This retrospective cohort study used Medicare and private payer claims to identify patients who underwent nonemergent CABG surgery from January 1, 2012, through October 31, 2015. Ninety-day price-standardized, risk-adjusted, total episode payments were calculated for each patient, and hospitals were divided into quartiles based on the mean total episode payments of their patients. Payments were then subdivided into 4 components (index hospitalization, professional, postacute care, and readmission payments) and compared across hospital quartiles. Seventy-six hospitals in Michigan representing a diverse set of geographies and practice environments were included.
Main Outcomes and Measures
Ninety-day CABG episode payments.
Results
A total of 5910 patients undergoing nonemergent CABG surgery were identified at 33 of the 76 hospitals; of these, 4344 (73.5%) were men and mean (SD) age was 68.0 (9.3) years. At the patient level, risk-adjusted, 90-day total episode payments for CABG varied from $11 723 to $356 850. At the hospital level, the highest payment quartile of hospitals had a mean total episode payment of $54 399 compared with $45 487 for the lowest payment quartile (16.4% difference, P < .001). The highest payment quartile hospitals compared with the lowest payment quartile hospitals had 14.6% higher index hospitalization payments ($34 992 vs $30 531, P < .001), 33.9% higher professional payments ($8060 vs $6021, P < .001), 29.6% higher postacute care payments ($7663 vs $5912, P < .001), and 35.1% higher readmission payments ($3576 vs $2646, P = .06). The drivers of this variation are diagnosis related group distribution, increased inpatient evaluation and management services, higher utilization of inpatient rehabilitation, and patients with multiple readmissions.
Conclusions and Relevance
Wide variation exists in 90-day CABG episode payments for Medicare and private payer patients in Michigan. Hospitals and clinicians entering bundled payment programs for CABG should work to understand local sources of variation, with a focus on patients with multiple readmissions, inpatient evaluation and management services, and postdischarge outpatient rehabilitation care.
This cohort study evaluates payment variation in Medicare and private payer claims for coronary artery bypass grafting in anticipation of the Medicare bundled payment program.
Introduction
Multiple public and private payers are showing increased interest in bundled payment programs. Bundled payment programs aim to motivate hospitals and clinicians to increase coordination, improve quality of care, and reduce unwarranted variation. To do so, these programs hold hospitals and clinicians financially accountable for the entire care episode, including inpatient, outpatient, physician, and postacute care services, for specific conditions.
The United States spends an estimated $6.5 billion per year on coronary artery bypass grafting (CABG) procedures, making the procedure a substantial driver of hospital costs and a logical target of payment reform. In the Participating Heart Bypass Center Demonstration, the Health Care Financing Administration piloted a CABG bundled payment program in 4 hospitals. More recently, the Centers for Medicare & Medicaid Services (CMS) announced plans for a widespread, mandatory, 90-day, episode-based CABG bundled payment initiative. The program, scheduled to begin in January 2018, aims to improve the value of CABG care by specifically incentivizing improvements in postdischarge planning, postacute care quality, treatment adherence, and chronic disease management. Following suit, commercial insurers, Arkansas’ Medicaid program, and private employers have also begun to implement their own CABG bundled payment initiatives.
Previous CABG bundled payment research used Medicare claims and demonstrated variation in 30-day CABG episode payments. However, little is known about the drivers of CABG payment variation outside of the index hospital stay or about variation in private payer patients. Furthermore, these previous analyses used 30-day episode payments, which may not fully capture postdischarge payment variation in contemporary 90-day programs, such as the one proposed by the CMS. Additional insight into events occurring more than 30 days after discharge, such as postacute care and readmissions, will be needed for hospital leaders, clinicians, and policymakers to appreciate how new bundled payment initiatives could affect CABG care. Accordingly, we set out to characterize contemporary 90-day payment variation and drivers of that variation for CABG care.
In this study, we used a statewide Michigan claims registry that includes detailed CABG episode payment information for both Medicare and Blue Cross Blue Shield of Michigan patients. We examined differences in 90-day episode payments for CABG at the hospital level and identified specific drivers of CABG payment variation to provide a more nuanced understanding of CABG payment variation. We hypothesized that, despite years of payment reforms, significant payment variation still exists for CABG in both Medicare and private insurance patients. Furthermore, we hypothesized that readmissions—specifically the frequency of readmission—is a key driver of payment variation.
Methods
Michigan Value Collaborative and Data Sources
We analyzed 90-day CABG episode payments from the Michigan Value Collaborative. Data collection methods and statistical analysis for the Michigan Value Collaborative have been described previously. In brief, the Michigan Value Collaborative is a group of 76 Michigan acute care hospitals that aims to improve the quality of inpatient care while reducing episode payments. To help hospital leaders understand variation in health care payments and improve care for patients, the Michigan Value Collaborative coordinating center uses complete Medicare fee-for-service claims data and Blue Cross Blue Shield of Michigan preferred provider organization claims to create a registry detailing comprehensive 90-day episodes of care for admissions at Michigan hospitals. The University of Michigan Institutional Review Board deemed this work exempt from review.
Creation of Study Cohort
We used Medicare and Blue Cross Blue Shield of Michigan claims data from January 1, 2012, to October 31, 2015, to identify patients who underwent nonemergent CABG surgery in Michigan. We used International Classification of Diseases, Ninth Revision, Clinical Modification procedure codes (36.1-36.2, 36.11-36.17, and 36.19) and Current Procedural Terminology codes (33510-33516, 33517-33521, and 33533-33536) to identify CABG index hospitalizations. We excluded patients presenting with acute myocardial infarction, concomitant valve surgery, or heart transplantation (eAppendix in the Supplement). We identified all clinically relevant claims 90 days after discharge and created episodes of care from the claims.
Calculation of Standardized 90-Day Episode and Component Payments
We price standardized and risk adjusted claims for all patients to create expected payments. Prices were standardized using average Medicare payments for Michigan (C. Ellimoottil, MD, written communication, 2017). Payments were risk adjusted using a 2-step model that utilizes age, sex, admission acuity, and prior 6-month spending, together with significant variables among CMS condition categories and the CABG-specific risk adjustment variables listed in the eAppendix in the Supplement. In a manner similar to previously published methodologies, we then disaggregated the episodes of care into 4 primary payment components: index hospitalization, professional care, postacute care, and readmissions. For postacute care stays longer than 90 days, payments were truncated at 90 days. Ninety-day readmission payments were priced as a hospital payment and received a standardized price based on the diagnosis related group (DRG) of the readmission.
Computation of Hospital-Level Payments and Hospital Quartiles
We aggregated patient-level episodes of care at each index hospital to create mean 90-day total episode payments for each hospital. To be included in the cohort, hospitals had to perform more than 20 CABGs over the selected time frame. Hospitals were ranked from lowest to highest by mean risk-adjusted total episode payment and grouped into quartiles. We adjusted for hospital-to-hospital transfers by attributing all episode payments to the originating hospital.
Analysis of Payment Variation Between Quartiles
Mean episode payments and payment components were analyzed across quartiles. We used the Wilcoxon rank sum test to compare the total episode payment and payment components between quartiles. We performed 3 sensitivity analyses. First, we created a Medicare-only patient subgroup to ensure the results did not vary by payer. Second, we split patients by DRG type—specifically, those with major complication and comorbidity— to determine whether DRG intensity affected the results. Third, we compared payment variation using our definition of a CABG episode with variation using the CMS definition of a CABG episode (DRGs 231-236).
Identification of Drivers of Variation
To identify drivers of episode payment variation, we compared patients in the highest payment quartile with those in the lowest payment quartile. Specifically, for index hospitalization payments, we examined the distribution of DRG types across quartiles. For professional claims data, we analyzed Current Procedural Terminology codes, including procedural and evaluation and management (E&M) codes on each claim. For postacute care payments, we evaluated the rate and intensity of postdischarge services delivered.
Readmissions were analyzed by examining the cause and payment amount for each readmission. Readmissions with DRG codes 177 to 179, 193 to 195, 853 to 858, 862 to 863, and 870 to 872 were classified as postoperative infection. Readmissions with DRG codes 291 to 293 were classified as being due to heart failure. We also examined the number of times each patient was readmitted within 90 days and analyzed the use of postacute care following readmissions.
Statistical Analysis
The Wilcoxon rank sum test is a 2-tailed paired statistic tool. We used a P < .05 level of significance. All statistical analyses were performed using Stata, version 14 (StataCorp).
Results
Overall Variation in Total Payments
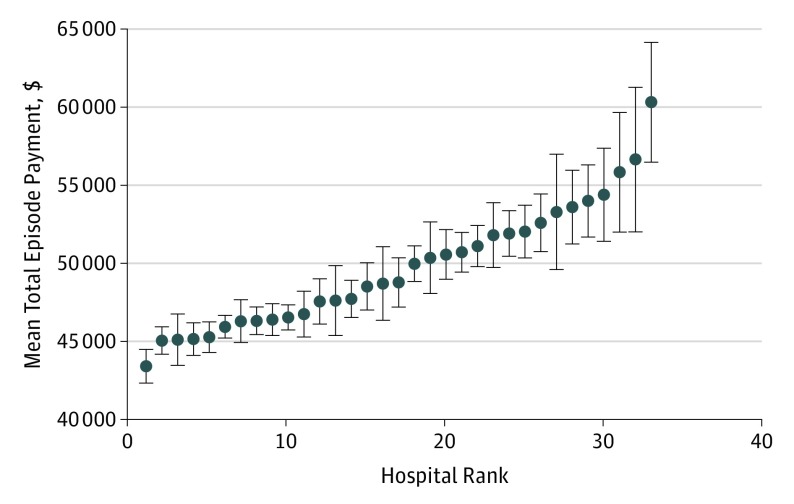
We identified 5910 patients (4344 [73.5%] men; mean [SD] age, 68.0 [9.3] years) who underwent elective CABG surgery at 33 nonfederal Michigan hospitals from January 1, 2012, to October 31, 2015. Forty-three of the original 76 hospitals were excluded due to low surgical volumes. At the patient level, the mean (SD) 90-day episode payment for CABG was $48 571 ($20 739) (range, $11 723-$356 850). At the hospital level, mean (SD) 90-day CABG payments ranged from $43 409 to $60 309 ($3951) (Figure 1). When examining hospital quartiles, the mean total episode payment for hospitals in the highest quartile of spending was $54 399 vs $45 487 for hospitals in the lowest quartile, a difference of $8912 (16.4% difference, P < .001) (Figure 2). Payer mix and mean age were similar across quartiles. The highest payment hospitals had lower case volumes and more women compared with the lowest payment hospitals (Table 1).
Figure 1. Hospital Ranking by Mean 90-Day Coronary Artery Bypass Grafting Total Episode Payment.
Hospitals ranked from lowest to highest by mean risk-adjusted total episode payment. Mean total episode payment was $48 571. Error bars indicate SEs.
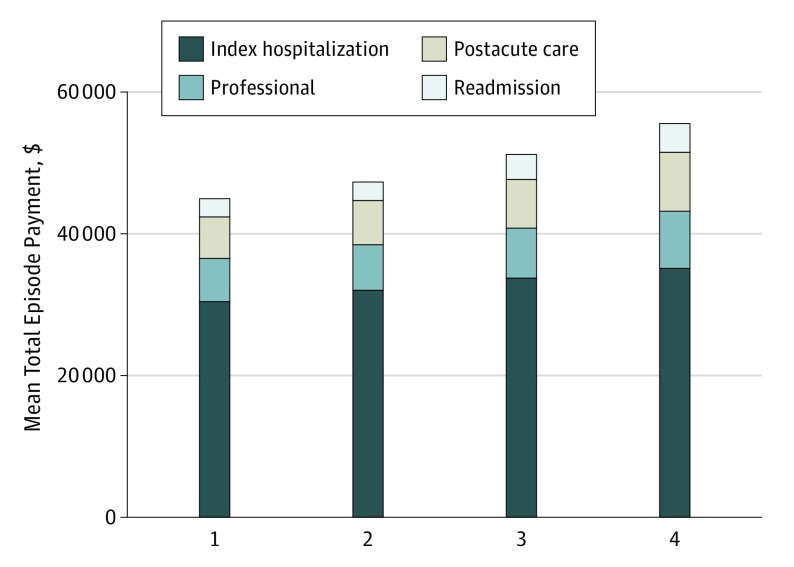
Figure 2. Breakdown of Total Episode Payment Components by Hospital Quartile.
Payment variation between the highest and lowest quartiles for all payment components.
Table 1. Hospital Characteristics and Patient Demographics by Hospital Quartile.
| Quartile | Facility Count | Episodes, No. | Payers, No. (%) | Age, Mean (SD), y | Men, No. (%) | |
|---|---|---|---|---|---|---|
| Medicare | BCBSM | |||||
| 1 | 9 | 2228 | 1708 (76.7) | 520 (23.3) | 67.9 (9.4) | 1673 (75.1) |
| 2 | 8 | 1326 | 1010 (76.2) | 316 (23,8) | 68.1 (9.6) | 1004 (75.7) |
| 3 | 8 | 1697 | 1305 (76.9) | 392 (23.1) | 68.2 (9.1) | 1212 (71.4) |
| 4 | 8 | 659 | 497 (75.4) | 162 (24.6) | 67.5 (9.2) | 455 (69.0) |
Abbreviation: BCBSM, Blue Cross Blue Shield of Michigan.
Payment Variation Across Quartiles
There was considerable payment variation between the highest and lowest quartiles for all payment components (Figure 2). The highest payment quartile hospitals compared with the lowest payment quartile hospitals had 14.6% higher index hospitalization payments ($34 992 vs $30 531, P < .001), 33.9% higher professional payments ($8060 vs $6021, P < .001), 29.6% higher postacute care payments ($7663 vs $5912, P < .001), and 35.1% higher readmission payments ($3576 vs $2646, P = .06).
A sensitivity analysis using a Medicare-only subgroup revealed similar results, although the readmission payment difference was even more pronounced (53.3% difference; range, $2559 [quartile 1] to $3923 [quartile 4]; P = .005). A sensitivity analysis including only patients with major complication and comorbidity DRGs also provided similar results, indicating that our findings are not caused only by DRG distribution. Last, we compared our definition of a CABG episode with the CMS definition and found a 91.8% patient match. Further analysis of patients falling under the CMS CABG definition showed results similar to those stated above.
Drivers of Payment Variation
Index hospital payment variation was primarily associated with differences in index DRG intensity. For example, 42.8% of index DRGs at high-cost hospitals were more expensive major complication and comorbidity DRGs, while 19.7% of index DRGs at low-cost hospitals were major complication and comorbidity DRGs (P < .001).
Variation in professional payments was mainly driven by differences in inpatient E&M claims (Table 2). The E&M payments are driven by the total length of hospitalizations, including index and readmission days, and the number of hospital E&M services per day. The average patient in the highest payment quartile spent 2.6 days longer in the hospital than patients in the lowest payment quartile (13.9 vs 11.3 days, P < .001). In addition, patients in the highest payment hospitals had more E&M claims per day compared with those in the lowest payment hospitals (1.5 vs 0.7 E&M claims per day, P < .001).
Table 2. Episode Cost Component and Subcomponent Payments at Highest and Lowest Payment Quartile Hospitalsa.
| Payment Component | Subcomponent | Lowest Payment Hospitals, $ | Highest Payment Hospitals, $ | Difference, $ | P Value |
|---|---|---|---|---|---|
| Facility | Facility payment | 29 876 | 34 243 | 4367 | <.001 |
| Professional | Outpatient E&M | 211 | 318 | 107 | <.001 |
| Inpatient E&M | 976 | 2368 | 1392 | <.001 | |
| Surgical procedures | 3115 | 3365 | 250 | <.001 | |
| Anesthesia | 901 | 1175 | 274 | <.001 | |
| Imaging | 241 | 369 | 128 | <.001 | |
| Postacute care | Inpatient rehabilitation | 583 | 1687 | 1104 | <.001 |
| Outpatient rehabilitation | 534 | 453 | 81 | <.001 | |
| Emergency department | 374 | 222 | 152 | <.001 | |
| Home health | 2437 | 2751 | 314 | .006 | |
| Skilled nursing facility | 1054 | 1406 | 352 | .24 | |
| Readmissions | Mean payment | 2646 | 3576 | 930 | .06 |
Abbreviation: E&M, evaluation and management.
Only differences of more than $75 are displayed.
Variation in postacute care payments was chiefly associated with the use of inpatient rehabilitation services. Patients in high- and low-payment hospitals had similar utilization rates for all rehabilitation services (58.0% vs 53.6%, P = .04). However, the highest payment hospitals used more inpatient rehabilitation services (13.2% vs 3.0%, P < .001) and fewer outpatient rehabilitation services than the lowest payment hospitals. This led to a $1104 mean difference in inpatient rehabilitation payments between quartiles (P < .001) (Table 2).
There was considerable variation in readmission payments between hospitals in the highest and lowest payment quartiles (Table 2). Patients in the highest quartile hospitals had 35% higher readmission payments than those in the lowest quartile ($3576 vs $2646, P = .06). Patients who experienced multiple readmissions were major drivers of this variation. Hospitals in the highest and lowest payment quartiles had nearly equal rates of patients with single readmissions (14.8% vs 13.7%, P = .49). However, the highest payment hospitals had a 77% higher rate of patients with multiple readmissions (6.8% vs 3.9%, P < .001). Patients with multiple readmissions had a total mean episode payment of $85 983 and spent 35 of 90 days hospitalized. In contrast, patients with single readmissions had a mean total episode payment of $61 712 and spent 18 of 90 days hospitalized.
We then examined, at the patient level, the clinical cause of these multiple readmissions. When patients were readmitted for a postoperative infection, 41.7% (10 of 24) of patients at high-quartile hospitals were readmitted multiple times compared with 30.8% (20 of 65) of patients at low-quartile hospitals. Similarly, of all patients who were admitted for heart failure, 27.3% (3 out of 11) of patients at high-quartile hospitals were readmitted multiple times compared with 10.8% (4 of 37) of patients from the low-quartile hospitals.
Finally, we analyzed the use of postacute care following readmissions. Among patients with a first readmission for postoperative infection or heart failure, only 5.1% (5 of 98) of those with subsequent readmissions received postacute care between their first and second readmissions. In contrast, 49.0% (100 of 204) of patients without subsequent readmissions received postacute care within 30 days after their readmissions.
Discussion
We found significant variation in 90-day, risk-adjusted CABG episode payments in Michigan. In addition, our results indicate that readmission, professional, and postacute care payments had relatively similar influences on statewide payment variation. Patients with multiple readmissions drove a substantial portion of readmission payment variation. These results underscore that there are meaningful opportunities to improve quality and reduce costs in CABG bundled payment programs, and success will require clinicians and hospital leaders to pay particular attention to care beyond the initial hospitalization.
Our findings align with those of previously published studies that characterize the structural and patient-level factors influencing CABG payments. Specifically, lower hospital CABG volume has been shown to correlate with higher episode payments, and female sex is known to be associated with higher inpatient CABG costs. Other work in this area has found that payment variation between high- and low-payment hospitals for 30-day CABG Medicare payments was greatest for postacute care, followed by readmissions, professional payments, and index hospitalization payments. In contrast, we have shown that readmissions, postacute care, and professional payments are relatively similar sources of 90-day CABG payment variation.
Our data suggest that patients with multiple readmissions drive the majority of variation seen in CABG readmission payments. These patients represent a particularly high-cost, at-risk population. Previous research has documented the prevalence and cost burden of patients with multiple readmissions within the general Medicare population but not among patients who undergo CABG. Studies of heart failure in elderly individuals found the rate of multiple readmissions to be as high as 16.4%. These same studies determined that multidisciplinary heart failure management programs focused on improving patient education, discharge coordination, transitions of care, and home follow-up can reduce the rates of multiple readmissions by more than 50%. Our findings suggest that there could be opportunities to improve the use of postacute care for patients who undergo CABG, especially among those readmitted with postoperative infection or heart failure.
Limitations
This study has several limitations. First, our data contain episode payments from a single state. However, Michigan has the 10th largest patient population and is known to have heterogeneous, representative demographics. Second, our sample size for comparing the causes of multiple readmission is small for some comparison groups, and future readmissions analyses will require a substantially larger study population. Last, we have not yet included and analyzed clinical quality-of-care measures, including mortality data or patient-level factors, such as use of cardiopulmonary bypass, that can be obtained only from clinical registries. Understanding the association between quality and cost of care will be important for informing the value of future CABG payment reform initiatives. Such patient- and procedure-specific quality measures will be available through registry programs, such as the Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative.
Conclusions
These limitations notwithstanding, our findings have important implications for policymakers, institutions, cardiovascular surgeons, and the care teams. Relevant to policymakers, we have illustrated significant 90-day variation in readmissions and postdischarge care, confirming the focus of key initiatives within the new Medicare CABG bundled payment program. In addition, since patients with multiple readmissions are key drivers of payment variation, we recommend that Medicare consider including such patients in their quality improvement programs, such as the Hospital Readmission Reduction Program.
For hospital leaders and clinicians, our findings suggest that succeeding in contemporary CABG bundled payment initiatives requires improving the value of postdischarge care and reducing readmissions. For example, increased attention to wound care and comprehensive heart failure management may help to lower episode payments and improve patient outcomes by limiting multiple readmissions. In addition, optimizing the balance between the use of outpatient and inpatient cardiac rehabilitation will be important since inpatient rehabilitation is costlier and has not been shown to improve outcomes compared with outpatient rehabilitation. However, there is unlikely to be a singular solution for lowering episode payments at all hospitals. Instead, clinicians and hospital leaders will need accurate, up-to-date local data to effectively target and tailor local interventions.
Collectively, these findings underscore that payment variation exists in contemporary public and private 90-day CABG episode payments and there are important opportunities for quality improvement. Expanding our knowledge about drivers of CABG payment variation is necessary to inform national discussions among policymakers, hospital leaders, clinicians, and patients about these potential health care reform models. Moving forward, research and reform in this area should focus on developing patient care initiatives that enhance the value of CABG care by improving quality and reducing episode costs.
eAppendix. CABG Episode Definition
References
- 1.CMS.gov. Centers for Medicare & Medicaid Services. Bundled Payments for Care Improvement (BPCI) initiative. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2016-Fact-sheets-items/2016-04-18.html. Published April 18, 2016. Accessed February 1, 2017.
- 2.Department of Health and Human Services; Centers for Medicare & Medicaid Services. Advancing Care Coordination Through Episode Payment Models (EPMs); Cardiac Rehabilitation Incentive Payment Model; and Changes to the Comprehensive Care for Joint Replacement Model (CJR). 42 CFR Parts 510 and 512. CMS-5519-P. https://innovation.cms.gov/Files/x/advancing-care-coordination-nprm.pdf. Published July 25, 2016. Accessed February 1, 2017.
- 3.Arkansas Department of Human Services. Episode of Care: coronary arterial bypass graft (CABG) episode design summary. http://www.paymentinitiative.org/Websites/paymentinitiative/images/Episode%20Design%20Summary%20-%20CABG%20-%202016-06-02%20-%20Final.pdf. Published June 2, 2016. . Accessed February 1, 2017.
- 4.Advisory Board. Commercial bundled payment tracker. https://www.advisory.com/Research/Health-Care-Advisory-Board/Resources/2013/Commercial-Bundled-Payment-Tracker. Published 2017. Accessed February 1, 2017.
- 5.Delbanco S. The payment reform landscape: bundled payment. Health Affairs blog. http://healthaffairs.org/blog/2014/07/02/the-payment-reform-landscape-bundled-payment/. Published July 2, 2014.. Accessed February 1, 2017.
- 6.National Center for Health Statistics; Centers for Disease Control and Prevention. Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities Hyattsville, MD: National Center for Health Statistics; 2016. [PubMed] [Google Scholar]
- 7.RAND Corporation Increase the use of “bundled” payment approaches. http://www.rand.org/pubs/technical_reports/TR562z20/analysis-of-bundled-payment.html#top. Published 2010. Accessed January 24, 2016.
- 8.Health Care Financing Administration Medicare Participating Heart Bypass Center Demonstration. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/downloads/oregon2_1998_3.pdf. Published September 1998. Accessed January 11, 2016.
- 9.Birkmeyer JD, Gust C, Baser O, Dimick JB, Sutherland JM, Skinner JS. Medicare payments for common inpatient procedures: implications for episode-based payment bundling. Health Serv Res. 2010;45(6, pt 1):1783-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller DC, Gust C, Dimick JB, Birkmeyer N, Skinner J, Birkmeyer JD. Large variations in Medicare payments for surgery highlight savings potential from bundled payment programs. Health Aff (Millwood). 2011;30(11):2107-2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herrel LA, Syrjamaki JD, Linsell SM, Miller DC, Dupree JM. Identifying drivers of episode cost variation with radical prostatectomy. Urology. 2016;97:105-110. [DOI] [PubMed] [Google Scholar]
- 12.Grenda TR, Pradarelli JC, Thumma JR, Dimick JB. Variation in hospital episode costs with bariatric surgery. JAMA Surg. 2015;150(12):1109-1115. [DOI] [PubMed] [Google Scholar]
- 13.Weiss AJ, Elixhauser A. Trends in operating room procedures in US hospitals, 2001-2011 Statistical brief #171. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: Agency for Health Care Policy and Research; 2006. [Google Scholar]
- 14.Cooper Z, Craig S, Gaynor M, Van Reenen J The price ain’t right? hospital prices and health spending on the privately insured. http://www.healthcarepricingproject.org/sites/default/files/pricing_variation_manuscript_0.pdf. Published December 2015. Accessed January 24, 2016. [DOI] [PMC free article] [PubMed]
- 15.Gottlieb DJ, Zhou W, Song Y, Andrews KG, Skinner JS, Sutherland JM. Prices don’t drive regional Medicare spending variations. Health Aff (Millwood). 2010;29(3):537-543.https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20110290&dopt=Abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pope GC, Kautter J, Ellis RP, et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financ Rev. 2004;25(4):119-141. [PMC free article] [PubMed] [Google Scholar]
- 17.Ellis RP, Pope GC, Iezzoni L, et al. Diagnosis-based risk adjustment for Medicare capitation payments. Health Care Financ Rev. 1996;17(3):101-128. [PMC free article] [PubMed] [Google Scholar]
- 18.Saleh SS, Racz M, Hannan E. The effect of preoperative and hospital characteristics on costs for coronary artery bypass graft. Ann Surg. 2009;249(2):335-341. [DOI] [PubMed] [Google Scholar]
- 19.Kilic A, Shah AS, Conte JV, et al. Understanding variability in hospital-specific costs of coronary artery bypass grafting represents an opportunity for standardizing care and improving resource use. J Thorac Cardiovasc Surg. 2014;147(1):109-115.https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24100097&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 20.Diodato M, Chedrawy EG. Coronary artery bypass graft surgery: the past, present, and future of myocardial revascularisation. Surg Res Pract. 2014;2014:726158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Regenbogen SE, Gust C, Birkmeyer JD. Hospital surgical volume and cost of inpatient surgery in the elderly. J Am Coll Surg. 2012;215(6):758-765. [DOI] [PubMed] [Google Scholar]
- 22.Anderson GF, Steinberg EP. Hospital readmissions in the Medicare population. N Engl J Med. 1984;311(21):1349-1353.https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=6436703&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 23.McAlister FA, Lawson FM, Teo KK, Armstrong PW. A systematic review of randomized trials of disease management programs in heart failure. Am J Med. 2001;110(5):378-384.https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=11286953&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 24.Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333(18):1190-1195.https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=7565975&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 25.US Census Bureau; American FactFinder. National, state, and Puerto Rico Commonwealth characteristics datasets: population estimates by age (18+). https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t. Accessed July 10, 2017.
- 26.Austin J, Williams R, Ross L, Moseley L, Hutchison S. Randomised controlled trial of cardiac rehabilitation in elderly patients with heart failure. Eur J Heart Fail. 2005;7(3):411-417.https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15718182&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 27.Schweikert B, Hahmann H, Steinacker JM, et al. Intervention study shows outpatient cardiac rehabilitation to be economically at least as attractive as inpatient rehabilitation. Clin Res Cardiol. 2009;98(12):787-795. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. CABG Episode Definition