This study determines whether survival was affected by more stringent definitions of pathologic nodal staging quality in a cohort of patients with non–small cell lung cancer who underwent resection with curative intent.
Key Points
Question
Does the thoroughness of pathologic nodal examination affect the prognostic value of pN classification in resectable non–small cell lung cancer?
Findings
In this study of 2047 patients with non–small cell lung cancer, sequential improvement in survival of pN0 and pN1 cohorts with increasing stringency was found. The pN1 cohorts with examination of 3 or more mediastinal nodal stations had the greatest survival improvements.
Meaning
The prognostic value of pN stratification depends on the thoroughness of examination, potentially accounting for a large proportion of the intercontinental differences in lung cancer survival; more thorough nodal examination practice must be disseminated to improve the prognostic value of the TNM staging system.
Abstract
Importance
Pathologic nodal stage is the most significant prognostic factor in resectable non–small cell lung cancer (NSCLC). The International Association for the Study of Lung Cancer NSCLC staging project revealed intercontinental differences in N category–stratified survival. These differences may indicate differences not only in cancer biology but also in the thoroughness of the nodal examination.
Objective
To determine whether survival was affected by sequentially more stringent definitions of pN staging quality in a cohort of patients with NSCLC after resection with curative intent.
Design
This observational study used the Mid-South Quality of Surgical Resection cohort, a population-based database of lung cancer resections with curative intent. A total of 2047 consecutive patients who underwent surgical resection at 11 hospitals with at least 5 annual lung cancer resections in 4 contiguous US Dartmouth hospital referral regions in northern Mississippi, eastern Arkansas, and western Tennessee (>90% of the eligible population) were included. Resections were performed from January 1, 2009, through January 25, 2016. Survival was evaluated with the Kaplan-Meier method and Cox proportional hazards models.
Exposures
Eight sequentially more stringent pN staging quality strata included the following: all patients (group 1); those with complete resections only (group 2); those with examination of at least 1 mediastinal lymph node (group 3); those with examination of at least 10 lymph nodes (group 4); those with examination of at least 3 hilar or intrapulmonary and at least 3 mediastinal lymph nodes (group 5); those with examination of at least 10 lymph nodes, including at least 1 mediastinal lymph node (group 6); those with examination of at least 1 hilar or intrapulmonary and at least 3 mediastinal nodal stations (group 7); and those with examination of at least 1 hilar or intrapulmonary lymph node, at least 10 total lymph nodes, and at least 3 mediastinal nodal stations (group 8).
Main Outcomes and Measures
N category–stratified overall survival.
Results
Of the total 2047 patients (1046 men [51.1%] and 1001 women [48.9%]; mean [SD] age, 67.0 [9.6] years) included in the analysis, the eligible analysis population ranged from 541 to 2047, depending on stringency. Sequential improvement in the N category–stratified 5-year survival of pN0 and pN1 tumors was found from the least stringent group (0.63 [95% CI, 0.59-0.66] for pN0 vs 0.46 [95% CI, 0.38-0.54] for pN1) to the most stringent group (0.71 [95% CI, 0.60-0.79] for pN0 vs 0.60 [95% CI, 0.43-0.73] for pN1). The pN1 cohorts with 3 or more mediastinal nodal stations examined had the most striking survival improvements. More stringently defined mediastinal nodal examination was associated with better separation in survival curves between patients with pN1 and pN2 tumors.
Conclusions and Relevance
The prognostic value of pN stratification depends on the thoroughness of examination. Differences in thoroughness of nodal staging may explain a large proportion of intercontinental survival differences. More thorough nodal examination practice must be disseminated to improve the prognostic value of the TNM staging system. Future updates of the TNM staging system should incorporate more quality restraints.
Introduction
The TNM staging system remains the most prognostically discriminative method in lung cancer. The system communicates the extent of disease, suggests treatment options, provides a means of homogenizing groups of patients enrolled into clinical trials, and enables objective outcome comparisons. Improving the prognostic value of the TNM staging system is of interest by identifying independent but complementary prognostic factors, including genetic profiles of early-stage cancer that can identify patients with higher mortality risk within specific stage subsets. Such progressive work is impaired by variation in the quality of application of the TNM staging criteria.
Nodal staging is the most variable and potentially inaccurate of the TNM criteria. Variation in the thoroughness and accuracy of clinical and pathologic nodal staging is well reported. Pathologic nodal staging is more accurate than clinical staging. However, current pathologic staging quality ranges from nonexamination of lymph nodes (the pNX phenomenon) and poor examination of hilar or intrapulmonary (N1) and mediastinal lymph nodes to guideline-concordant staging. However, even guideline-concordant nodal staging varies in the specific requirements, depending on the guideline. The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee recently reported major intercontinental variation in pN category–stratified survival, with significantly higher survival among Asian patients with pN0 and pN1 findings than among patients from America, Australia, and Europe. Whether these differences reflect biological differences in the intercontinental populations with lung cancer or whether they reflect differences in surgical and pathologic practices in nodal staging remains unclear. We examined long-term postoperative survival in a US regional population with detailed information on the thoroughness of nodal staging to examine the stage-stratified survival effect of sequentially more thorough nodal examination based on existing examination criteria with and without modifications.
Methods
The Mid-South Quality of Surgical Resection (MS-QSR) cohort is a population-based database of lung cancer resections with curative intent that currently includes more than 90% of cases at all hospitals with at least 5 annual cases in 4 contiguous US Dartmouth hospital referral regions in northern Mississippi, eastern Arkansas, and western Tennessee from 2009 onward. These states have the second, third, and fourth highest rates of lung cancer incidence and mortality, respectively, in the United States. The current analysis of resections from January 1, 2009, through January 25, 2016, excludes patients who received neoadjuvant therapy (to avoid confounding from treatment effects on nodal counts), who died within 30 days of surgery (because of our interest in examining quality association of pathologic nodal staging with long-term outcomes), or who had small cell lung cancer and carcinoid tumors (because of their different long-term survival patterns). Survival status in the MS-QSR cohort is actively obtained from institutional clinical records or provided by each institution’s tumor registry and systematically updated for all patients every 12 months. The institutional review boards at each participating institution approved this research with a waiver of the requirement for informed consent.
Quality-Based Cohort Selection Strategy
We evaluated the N category–stratified survival in analytic cohorts selected with sequentially greater quality stringency. The sequence of selection of patients with non–small cell lung cancer (NSCLC) for the analysis cohorts included the following: all patients (group 1); those with complete (R0) resection (similar to the IASLC analysis cohort) (group 2); those with R0 resection and examination of at least 1 mediastinal lymph node (group 3); those with R0 resection and examination of a minimum of 10 lymph nodes, irrespective of source (similar to the American College of Surgeons Commission on Cancer [CoC] NSCLC quality surveillance criteria) (group 4); those with R0 resection, with examination of a minimum of 3 N1 and 3 mediastinal lymph nodes (as recommended by the Union for International Cancer Control [UICC]) (group 5); those with R0 resection and examination of at least 1 mediastinal lymph node and a minimum of 10 lymph nodes, irrespective of source (a stringent variation of the CoC criteria) (group 6); those with R0 and examination of at least 1 N1 lymph node and 3 or more mediastinal nodal stations (similar to the National Comprehensive Cancer Network [NCCN] recommendations) (group 7); and those with R0 and examination of at least 1 N1 lymph node, a minimum of 10 nodes, and a minimum of 3 mediastinal nodal stations (a combination of the NCCN and CoC criteria) (group 8) (Figure 1 and Table 1).
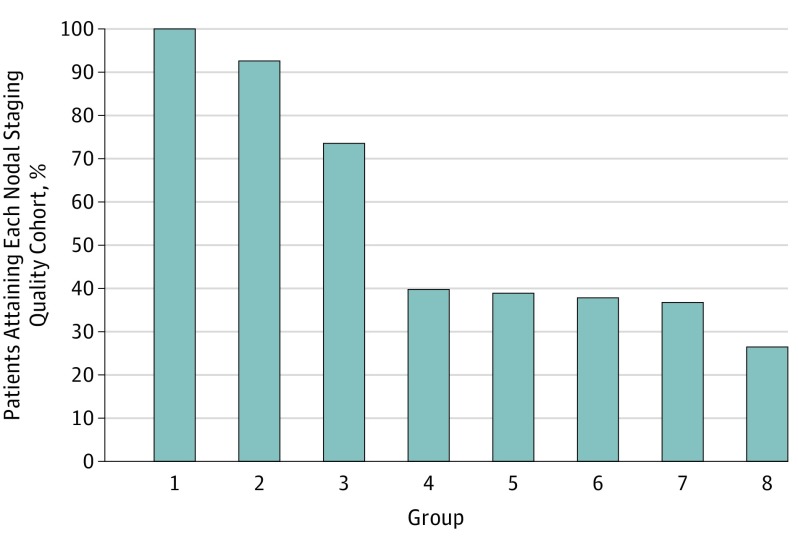
Figure 1. Proportion of Mid-South Quality of Surgical Resection Cohort Eligible for Analysis With Sequentially More Stringent Pathologic Nodal Staging Criteria.
Group criteria are described in detail in Table 1.
Table 1. Group Description and Source of Quality Restriction for 2047 Patients.
| Group No. | Description | Source of Quality Restriction |
|---|---|---|
| 1 (n = 2047) | All patients | NA |
| 2 (n = 1894) | R0 resection | Eliminates margin-positive resections, similar to the IASLC analysis cohort |
| 3 (n = 1505) | R0 resection and examination of ≥1 mediastinal LN | Also eliminates patients without mediastinal LN examination |
| 4 (n = 814) | R0 resection and examination of ≥10 LNs irrespective of source | Similar to the CoC NSCLC quality surveillance criteria |
| 5 (n = 797) | R0 resection and examination of ≥3 N1 LNs and 3 mediastinal LNs | Recommended by the UICC |
| 6 (n = 774) | R0 and examination of ≥1 mediastinal LN and ≥10 LNs irrespective of source | Hypothetically more stringent variation of the CoC criteria, imposing a mandate for mediastinal LN examination |
| 7 (n = 753) | R0 and examination of ≥1 N1 LN and ≥3 mediastinal LNs | Similar to the NCCN recommendations |
| 8 (n = 541) | R0 and examination of ≥1 N1 LN, ≥10 LNs, and ≥3 mediastinal LNs | Hypothetical model of thoroughness combining the CoC mandate for comprehensive overall nodal evaluation with the NCCN mandate for comprehensive mediastinal LN examination |
Abbreviations: CoC, American College of Surgeons Commission on Cancer; IASLC, International Association for the Study of Lung Cancer; LN, lymph node; NA, not applicable; NCCN, National Comprehensive Cancer Network; NSCLC, non–small cell lung cancer; UICC, Union for International Cancer Control.
Statistical Analysis
Univariate frequency (percentages) or means (SDs) are reported for each variable of interest. Overall and pN category–stratified survival estimates were calculated using the Kaplan-Meier method and evaluated graphically. Survival time was defined as years from the date of surgery to the date of death or last follow-up (censored patients). One-, 3-, and 5-year survival estimates were reported, and survival curves were compared between groups with the log-rank test. We used Cox proportional hazards models to estimate crude and adjusted hazard ratios (HRs) with 95% CIs comparing pN categories. Statistical comparisons are made between pN categories within each quality cohort, including all patients meeting the quality criteria (Figure 1). All statistical comparisons of overall survival between quality cohorts compare independent groups of patients, such that each patient is only counted once, as part of the highest-quality cohort attained. P < .05 was considered to be statistically significant, and all analyses were conducted using SAS software (version 9.4; SAS Institute).
Results
Cohort Characteristics
The demographic and clinical characteristics of the total cohort of 2047 eligible patients (1046 men [51.1%] and 1001 women [48.9%]; mean [SD] age, 67.0 [9.6] years) were consistent across the quality cohorts (eTable 1 in the Supplement). Most patients had histologic findings of adenocarcinoma (1108 [54.1%]) or squamous cell carcinoma (690 [33.7%]). The distribution of histologic type, grade, or tumor size did not change substantially when more stringent quality restrictions were applied (eTables 1 and 2 in the Supplement). Pathologic T and N categories also appeared to be consistent across quality categories except for the exclusion of pNX in groups 3 through 8, which required the examination of at least 1 lymph node (eTables 1 and 2 in the Supplement). Overall, 153 patients (7.5%) had positive margins; 145 patients (7.1%), pNX findings. Adjuvant chemotherapy was used in 337 patients (16.5%); radiation therapy, in 95 (4.6%).
Oncologic Resection Quality Subcohorts
The proportion of patients in each analytic subcohort was inversely proportional to the degree of stringency of the quality criteria. Numbers of patients ranged from 1894 (92.5%) for group 2 (R0 resection) to 541 (26.4%) for group 8 using the combination of the NCCN and CoC criteria (Figure 1).
Association With Aggregate Overall Survival
Aggregate overall survival and survival stratified by pN category were evaluated within each sequentially more stringent quality cohort. Aggregate 3-year survival estimates increased from 69% (95% CI, 67%-72%) for group 1 to 75% (95% CI, 70%-79%) for group 8; aggregate 5-year survival estimates showed an absolute increase of 8% from group 1 (57%; 95% CI, 54%-60%) to group 8 (65%; 95% CI, 58%-72%) (eTable 3 and eFigure, A, in the Supplement). After adjusting for age at surgery, sex, race, insurance status, histologic type, extent of surgical resection, number of comorbidities, pN category, and pT category, patients with resections meeting the most stringent quality definition (group 8 [n = 541]) had a 24% reduction in the hazard of death (adjusted HR, 0.76; 95% CI, 0.62-0.95; P = .01) compared with patients with R0 and less stringently defined nodal staging quality (groups 2-7 [n = 1353]) and a 40% reduction in death compared with resections meeting the least-stringent quality definition (non-R0 group 1 [n = 153]) (adjusted HR, 0.60; 95% CI, 0.43-0.83; P = .002). We found a sequential 2% improvement in aggregate survival with each level of stringency from groups 1 to 4 (5-year survival, 0.57, 0.59, 0.61, and 0.63, respectively) and from groups 5 to 6 (5-year survival, 0.63 and 0.65, respectively); aggregate survival was similar between groups 4 and 5 and between groups 6 and 8 (5-year survival, 0.65 for both) (eFigure, A, in the Supplement).
Association With Comparative N Category–Stratified Survival
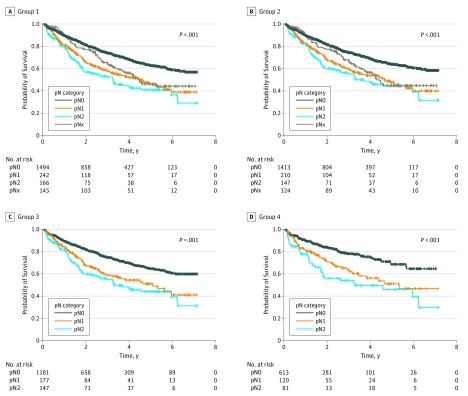
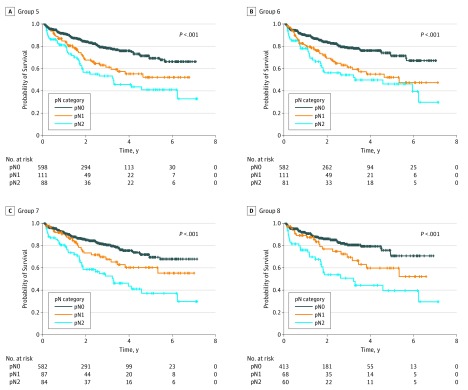
The delineation in 5-year survival curves between patients with pN1 (0.46; 95% CI, 0.38-0.54) and pN2 (0.41; 95% CI, 0.32-0.50) tumors was almost nonexistent in the entire cohort but was apparent in the more stringently defined quality groups (eg, 0.60 [95% CI, 0.43-0.73] for pN1 vs 0.39 [95% CI, 0.24-0.55] for pN2 in group 8) (eFigure, B-C, and eTable 3 in the Supplement). In the full cohort, the crude HR for death compared with patients with pN0 tumors was 1.77 (95% CI, 1.42-2.20) for pN1 and 2.17 (95% CI, 1.72-2.75) for pN2, compared with 1.71 (95% CI, 1.03-2.84) for pN1 and 3.29 (95% CI, 2.11-5.10) for pN2 in group 8 (Table 2) (P < .05 unless noted). Results were consistent after adjusting for age at surgery, sex, race, insurance status, histologic type, extent of surgical resection, number of comorbidities, and pT category in multiple variable models (Table 2). These adjusted HRs (eFigure, D, in the Supplement) reveal the increasing discrimination of pN1 vs pN2 as stringency increases from group 1 (pN1 vs pN0, 1.53 [95% CI, 1.21-1.92]; pN2 vs pN0, 2.08 [95% CI, 1.63-2.67]) to group 8 (pN1 vs pN0, 1.41 [95% CI, 0.79-2.51]; pN2 vs pN0, 3.23 [95% CI, 2.00-5.24]) (Figure 2 and Figure 3).
Table 2. Crude and Adjusted Cox Proportional Hazard Models by Group.
| pN Category | Quality Group, HR (95% CI)a | |||||||
|---|---|---|---|---|---|---|---|---|
| Group 1 (n = 2047) |
Group 2 (n = 1894) |
Group 3 (n = 1505) |
Group 4 (n = 814) |
Group 5 (n = 797) |
Group 6 (n = 774) |
Group 7 (n = 753) |
Group 8 (n = 541) |
|
| Crude model | ||||||||
| pN0 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| pN1 | 1.77 (1.42-2.20) | 1.74 (1.38-2.20) | 1.71 (1.31-2.22) | 1.88 (1.32-2.68) | 1.88 (1.30-2.71) | 1.99 (1.37-2.88) | 1.59 (1.03-2.45) | 1.71 (1.03-2.84) |
| pN2 | 2.17 (1.72-2.75) | 2.03 (1.57-2.62) | 2.09 (1.61-2.72) | 2.56 (1.77-3.72) | 2.68 (1.88-3.83) | 2.65 (1.82-3.87) | 2.90 (2.02-4.17) | 3.29 (2.11-5.10) |
| pNx | 1.48 | 1.5 | NA | NA | NA | NA | NA | NA |
| Adjusted modelb | ||||||||
| pN0 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| pN1 | 1.53 (1.21-1.92) | 1.52 (1.18-1.94) | 1.55 (1.17-2.05) | 1.59 (1.08-2.33) | 1.56 (1.04-2.35) | 1.76 (1.18-2.63) | 1.26 (0.78-2.02)c | 1.41 (0.79-2.51)d |
| pN2 | 2.08 (1.63-2.67) | 1.88 (1.44-2.45) | 1.94 (1.48-2.56) | 2.34 (1.57-3.50) | 2.69 (1.82-3.97) | 2.47 (1.65-3.69) | 2.68 (1.81-3.95) | 3.23 (2.00-5.24) |
| pNx | 1.18 (0.86-1.63)d | 1.25 (0.88-1.77)d | NA | NA | NA | NA | NA | NA |
Abbreviations: HR, hazard ratio; NA, not applicable.
P < .05 comparing each pN category with the reference group pN0 unless otherwise specified.
Adjusted for age at surgery, sex, race, insurance status, histologic type, extent of resection, number of comorbidities, and pathologic T category.
P < .10.
P > .10.
Figure 2. Stage-Stratified Estimated Survival Among Patients in Sequentially More Stringent Pathologic Nodal Staging Quality Cohorts 1 Through 4.
Group criteria are described in detail in Table 1. In group 1, pNX, pN1, and pN2 survival curves converged. In group 2, the survival pattern is indistinct from that of group 1. In group 3, the pNX group was eliminated, but pN1 and pN2 survival curves converged. In group 4, residual overlap remained between pN1 and pN2 survival curves. + Indicates censored patients.
Figure 3. Stage-Stratified Estimated Survival Among Patients in Sequentially More Stringent Pathologic Nodal Staging Quality Cohorts 5 Through 8.
Group criteria are described in detail in Table 1. In group 5, separation occurred among pN0, pN1, and pN2 survival curves with the greater stringency of mediastinal lymph node examination requirement based on the number of mediastinal nodes. In group 6, lack of mediastinal nodal mapping stringency failed to separate pN1 and pN2 survival curves. In group 7, separation occurred among the pN0, pN1, and pN2 survival plots, but the pN1 survival was closer to the pN0 curve. In group 8, combination of the American College of Surgeons Commission on Cancer and National Comprehensive Cancer Network criteria shows the most balanced separation between the survival plots, by coupling thorough hilar and intrapulmonary lymph node examination with thorough mediastinal lymph node examination based on station mapping. + Indicates censored patients.
Although the aggregate survival among patients meeting the CoC criteria (group 4) was similar to that among patients meeting the UICC criteria (group 5), we found a complete separation of the pN1 and pN2 survival curves with the greater thoroughness of mediastinal nodal examination mandated by the UICC criteria (Figure 3A)compared with the CoC criteria (Figure 2D), which did not specify from where the mandated minimum of 10 examined lymph nodes should be derived and in which overlap occurred in the pN1 and pN2 survival curves. Similarly, groups 7 and 8, for whom a minimum of 3 examined mediastinal nodal stations were required, showed clear separation of the pN0, pN1, and pN2 survival curves (Figure 3C and D). The requirement for examination of at least 1 mediastinal lymph node among the minimum of 10 nodes mandated by the CoC (group 6) did not resolve the lack of precision between pN1 and pN2 prognostication (Figure 3B). Only 40 patients who had 10 or more examined lymph nodes failed to meet the requirement for at least 1 mediastinal lymph node (eTables 1 and 2 in the Supplement).
Discussion
The TNM staging method serves to compare patients across time and space, provides a means of estimating risk for death, enables the identification of candidates for adjuvant therapy, and provides a means of homogenizing comparison groups in clinical trials. Nodal staging is the most difficult component of the TNM constructs to accurately determine because of variability in use and accuracy of clinical staging tests and in the thoroughness of application of pN staging procedures.
The IASLC Staging and Prognostic Factors Committee recently demonstrated significant differences in survival among patients with pN0, pN1, and pN2 NSCLC in the international database used to reconfigure the TNM staging descriptors. Five-year survival among Asian patients (mostly from Japan and South Korea) with pN0, pN1, and pN2 disease was 79%, 54%, and 39%, respectively, compared with 67%, 48%, and 42%, respectively, among American patients (mostly from 2 major US institutions); 58%, 41%, and 33%, respectively, among Australian patients; and 54%, 34%, and 22%, respectively, among European patients. Two plausible explanatory hypotheses for these differences are intercontinental differences in cancer biology and differences in the thoroughness of lymph node examination.
We tested the latter hypothesis by examining stage-stratified survival in cohorts of patients with sequentially more thorough lymph node examination. We observed that sequential quality curbs were strongly associated with improved outcomes. Moreover, the association between the specific quality criteria and the pattern of survival improvement suggests the source of the survival deficit in unselected populations. Survival among patients without any examined lymph nodes (pNX), although their clinical stage was N0, tracked more closely with that among patients with pN1 disease. This finding has been suggested as evidence of dual failure of surgical harvest and pathologic examination practices. We speculate that this higher mortality risk was caused by the combination of de facto incomplete resection for some patients with hilar and mediastinal lymph node metastasis left by the surgeon and failure to recognize the residual mortality risk connoted by intrapulmonary lymph node metastasis missed by pathologists. Adjuvant therapy may have been beneficial to some of these patients with missed N1 or N2 nodal metastasis.
Mandating examination of a minimum of 10 lymph nodes (as the CoC has done) was associated with the biggest increase in pN0 survival, suggesting the value of more thorough retrieval of N1 nodes. Imposition of a specific requirement for mediastinal nodal examination, especially the NCCN recommendation to examine a minimum of 3 mediastinal nodal stations, was associated with the biggest increase in N1 survival, suggesting more accurate detection of N2 nodal metastasis. Only the cohorts that mandated examination of multiple mediastinal lymph nodes (group 5 [Figure 3A]) or multiple mediastinal lymph node stations (groups 7 and 8 [Figure 3C and D]) achieved separation in survival between patients with pN1 and pN2 disease. Therefore, the highest-quality recommendations should mandate examining a minimum of 10 total lymph nodes, with sampling from at least 3 mediastinal stations.
The quality of pN staging matters. All the virtues of the TNM staging system inhere in its risk-stratification value, which relies heavily on proper application. Loss of this prognostic ability was demonstrated in the evolving stage-stratified survival plots, in which increased stringency of N1 and mediastinal nodal examination eliminated overlaps between stage-stratified survival plots and improved the separation between the pN strata (Figures 2 and 3). This finding suggests that the full prognostic value of the TNM system depends on the thoroughness of application and that imposition of survival-impactful quality criteria is required in analysis cohorts used to test the prognostic value of nodal staging descriptors. Of particular concern is the potential effect of heterogeneity in thoroughness of nodal examination on the design, accrual, results, and interpretation of clinical trials.
Limitations
We excluded patients who died within 30 days of surgery because we were interested in examining the long-term survival impact of oncologic quality of resection and needed to eliminate potential confounding caused by short-term postoperative mortality. The causes of postoperative mortality have been figured out and are more or less universally agreed on. In addition, this nonrandomized observational study was subject to the limitations, including biases and potential confounding inherent in such a study design. Furthermore, we did not examine the influences of institutional and clinician factors. The institutions in this study are involved in ongoing surgical quality improvement initiatives, which may affect the surgical sampling of lymph nodes and the quality of pathologic examination.
We also did not test the alternative, biological hypothesis of the intercontinental outcome differences in stage-stratified lung cancer survival nor did we prove the quality of staging hypothesis because we could not directly compare the IASLC and MS-QSR cohorts. Nevertheless, we used this unique population-based database, which has significantly more details about nodal staging than are available in other large databases, such as the Surveillance, Epidemiology and End Results database or the National Cancer Data Base, to examine a problem in lung cancer care, namely, the disparity in outcomes between individuals with ostensibly identical stage of disease. We could not determine from this analysis whether the survival differences resulted from stage migration with more thorough nodal examination or whether there is an inherent survival benefit from more thorough examination (as potentially suggested by differences in aggregate or non–stage-stratified survival differences). Finally, any quality metric that uses the number of examined lymph nodes is subject to potential confounding from the manner of counting lymph node fragments.
Conclusions
Future examinations of the nodal staging criteria should highlight the need to standardize staging quality with use of high-quality analytic cohorts at least in sensitivity analyses. The IASLC has started in this direction with examination of the effect of excluding incomplete resections from the final analysis cohort. We recommend further evaluation by incorporating sensitivity analyses of sequentially more stringent nodal quality subsets in analyses leading to future updates of the TNM staging system. Meanwhile, efforts to disseminate improved surgical and pathologic nodal staging practices must be actively promoted. Progress in understanding the elemental question of heterogeneous cancer biology and the development of stage-independent prognostic factors are potentially submerged within the quality gap of nodal staging.
eTable 1. Summary Statistics by Groups 1-4
eTable 2. Summary Statistics by Groups 5-8
eTable 3. Kaplan-Meier Survival Estimates for Groups 1-8
eFigure. Evolution of Survival Across 8 Sequentially More Stringent Pathologic Nodal Staging Quality Cohorts
References
- 1.Goldstraw P, Chansky K, Crowley J, et al. ; International Association for the Study of Lung Cancer Staging and Prognostic Factors Committee, Advisory Boards, and Participating Institutions; International Association for the Study of Lung Cancer Staging and Prognostic Factors Committee advisory boards and participating institutions . The IASLC Lung Cancer Staging Project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11(1):39-51. [DOI] [PubMed] [Google Scholar]
- 2.Osarogiagbon RU. Predicting survival of patients with resectable non–small cell lung cancer: beyond TNM. J Thorac Dis. 2012;4(2):214-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Osarogiagbon RU, Allen JW, Farooq A, Wu JT. Objective review of mediastinal lymph node examination in a lung cancer resection cohort. J Thorac Oncol. 2012;7(2):390-396. [DOI] [PubMed] [Google Scholar]
- 4.Detterbeck FC. The fable of Babel and building a foundation for quality. J Thorac Oncol. 2012;7(2):267-268. [DOI] [PubMed] [Google Scholar]
- 5.Farjah F, Flum DR, Ramsey SD, Heagerty PJ, Symons RG, Wood DE. Multi-modality mediastinal staging for lung cancer among Medicare beneficiaries. J Thorac Oncol. 2009;4(3):355-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Detterbeck F. What is quality and does it matter? J Thorac Oncol. 2009;4(3):279-280. [DOI] [PubMed] [Google Scholar]
- 7.Detterbeck F, Puchalski J, Rubinowitz A, Cheng D. Classification of the thoroughness of mediastinal staging of lung cancer. Chest. 2010;137(2):436-442. [DOI] [PubMed] [Google Scholar]
- 8.Osarogiagbon RU, Yu X. Mediastinal lymph node examination and survival in resected early-stage non–small-cell lung cancer in the Surveillance, Epidemiology, and End Results database. J Thorac Oncol. 2012;7(12):1798-1806. [DOI] [PubMed] [Google Scholar]
- 9.Osarogiagbon RU, Yu X. Nonexamination of lymph nodes and survival after resection of non–small cell lung cancer. Ann Thorac Surg. 2013;96(4):1178-1189. [DOI] [PubMed] [Google Scholar]
- 10.Osarogiagbon RU, Ogbata O, Yu X. Number of lymph nodes associated with maximal reduction of long-term mortality risk in pathologic node-negative non–small cell lung cancer. Ann Thorac Surg. 2014;97(2):385-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.D’Cunha J, Herndon JE II, Herzan DL, et al. ; Cancer and Leukemia Group B . Poor correspondence between clinical and pathologic staging in stage 1 non–small cell lung cancer: results from CALGB 9761, a prospective trial. Lung Cancer. 2005;48(2):241-246. [DOI] [PubMed] [Google Scholar]
- 12.Osarogiagbon RU, Decker PA, Ballman K, Wigle D, Allen MS, Darling GE. Survival implications of variation in the thoroughness of pathologic lymph node examination in American College of Surgeons Oncology Group Z0030 (Alliance). Ann Thorac Surg. 2016;102(2):363-369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Comprehensive Cancer Network clinical practice guidelines in oncology. Non–small cell lung cancer. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Version 8.2017, July 14, 2017. Accessed February 8, 2016.
- 14.Gajra A, Newman N, Gamble GP, Kohman LJ, Graziano SL. Effect of number of lymph nodes sampled on outcome in patients with stage I non–small-cell lung cancer. J Clin Oncol. 2003;21(6):1029-1034. [DOI] [PubMed] [Google Scholar]
- 15.Darling GE, Allen MS, Decker PA, et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with N0 or N1 (less than hilar) non–small cell carcinoma: results of the American College of Surgery Oncology Group Z0030 Trial. J Thorac Cardiovasc Surg. 2011;141(3):662-670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American College of Surgeons. CoC Quality of Care Measures. CoC Measures for Quality of Cancer Care. https://www.facs.org/quality-programs/cancer/ncdb/qualitymeasures. Posted Fall 2014. Accessed August 20, 2017.
- 17.Asamura H, Chansky K, Crowley J, et al. The International Association for the Study of Lung Cancer Lung Cancer Staging Project: proposals for the revision of the N descriptors in the forthcoming 8th edition of the TNM classification for lung cancer. J Thorac Oncol 2015;10(12):1675-84. [DOI] [PubMed] [Google Scholar]
- 18.Osarogiagbon RU, Smeltzer MP, Faris N, Rami-Porta R, Goldstraw P, Asamura H Comment on the proposals for the revision of the N descriptors in the forthcoming 8th edition of the TNM classification for lung cancer. J Thorac Oncol 2016;11(10):1612-1614. [DOI] [PubMed] [Google Scholar]
- 19.Faris N, Smeltzer MP, Lu F, et al. Evolution in the surgical care of non–small cell lung cancer (NSCLC) patients in the Mid-South Quality of Surgical Resection (MS-QSR) cohort. Semin Thorac Cardiovasc Surg. 2017;29(1):91-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Cancer Society Cancer Facts & Figures 2016. Atlanta, GA: American Cancer Society; 2016. [Google Scholar]
- 21.Osarogiagbon RU, Ray MA, Faris NR, et al. Prognostic value of National Comprehensive Cancer Network lung cancer resection quality parameters. Ann Thorac Surg. 2017;103(5):1557-1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Osarogiagbon RU, Darling GE. Towards optimal pathologic staging of resectable non–small cell lung cancer. Transl Lung Cancer Res. 2013;2(5):364-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Osarogiagbon RU. Strategic approach to minimally invasive mediastinal nodal staging: a brave new world? Lancet Respir Med. 2016;4(12):926-927. [DOI] [PubMed] [Google Scholar]
- 24.Osarogiagbon RU, Allen JW, Farooq A, Berry A, Spencer D, O’Brien T. Outcome of surgical resection for pathologic N0 and Nx non–small cell lung cancer. J Thorac Oncol. 2010;5(2):191-196. [DOI] [PubMed] [Google Scholar]
- 25.Allen JW, Farooq A, O’Brien TF, Osarogiagbon RU. Quality of surgical resection for nonsmall cell lung cancer in a US metropolitan area. Cancer. 2011;117(1):134-142. [DOI] [PubMed] [Google Scholar]
- 26.Ramirez RA, Wang CG, Miller LE, et al. Incomplete intrapulmonary lymph node retrieval after routine pathologic examination of resected lung cancer. J Clin Oncol. 2012;30(23):2823-2828. [DOI] [PubMed] [Google Scholar]
- 27.Smeltzer MP, Faris N, Yu X, et al. Missed intrapulmonary lymph node metastasis and survival after resection of non–small cell lung cancer. Ann Thorac Surg. 2016;102(2):448-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Samson P, Crabtree T, Broderick S, et al. Quality measures in clinical stage I non–small cell lung cancer: improved performance is associated with improved survival. Ann Thorac Surg. 2017;103(1):303-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Farjah F, Backhus L, Cheng A, et al. Failure to rescue and pulmonary resection for lung cancer. J Thorac Cardiovasc Surg. 2015;149(5):1365-1371. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Summary Statistics by Groups 1-4
eTable 2. Summary Statistics by Groups 5-8
eTable 3. Kaplan-Meier Survival Estimates for Groups 1-8
eFigure. Evolution of Survival Across 8 Sequentially More Stringent Pathologic Nodal Staging Quality Cohorts