Key Points
Question
What are the associations of screening and adjuvant treatment with reductions in US breast cancer mortality rates by molecular subtype?
Findings
In this study of 6 simulation models that projected US breast cancer mortality trends for women aged 30 to 79 years, advances in treatment, such as use of newer adjuvant therapies, compared with screening advances were associated with greater estimated reductions in overall breast cancer mortality from 2000 to 2012, although the associations varied by breast cancer molecular subtype.
Meaning
Simulation modeling estimated that advances in treatment were associated with greater decreases in breast cancer mortality rates than advances in screening, although these associations varied by molecular subtype.
Abstract
Importance
Given recent advances in screening mammography and adjuvant therapy (treatment), quantifying their separate and combined effects on US breast cancer mortality reductions by molecular subtype could guide future decisions to reduce disease burden.
Objective
To evaluate the contributions associated with screening and treatment to breast cancer mortality reductions by molecular subtype based on estrogen-receptor (ER) and human epidermal growth factor receptor 2 (ERBB2, formerly HER2 or HER2/neu).
Design, Setting, and Participants
Six Cancer Intervention and Surveillance Network (CISNET) models simulated US breast cancer mortality from 2000 to 2012 using national data on plain-film and digital mammography patterns and performance, dissemination and efficacy of ER/ERBB2-specific treatment, and competing mortality. Multiple US birth cohorts were simulated.
Exposures
Screening mammography and treatment.
Main Outcomes and Measures
The models compared age-adjusted, overall, and ER/ERBB2-specific breast cancer mortality rates from 2000 to 2012 for women aged 30 to 79 years relative to the estimated mortality rate in the absence of screening and treatment (baseline rate); mortality reductions were apportioned to screening and treatment.
Results
In 2000, the estimated reduction in overall breast cancer mortality rate was 37% (model range, 27%-42%) relative to the estimated baseline rate in 2000 of 64 deaths (model range, 56-73) per 100 000 women: 44% (model range, 35%-60%) of this reduction was associated with screening and 56% (model range, 40%-65%) with treatment. In 2012, the estimated reduction in overall breast cancer mortality rate was 49% (model range, 39%-58%) relative to the estimated baseline rate in 2012 of 63 deaths (model range, 54-73) per 100 000 women: 37% (model range, 26%-51%) of this reduction was associated with screening and 63% (model range, 49%-74%) with treatment. Of the 63% associated with treatment, 31% (model range, 22%-37%) was associated with chemotherapy, 27% (model range, 18%-36%) with hormone therapy, and 4% (model range, 1%-6%) with trastuzumab. The estimated relative contributions associated with screening vs treatment varied by molecular subtype: for ER+/ERBB2−, 36% (model range, 24%-50%) vs 64% (model range, 50%-76%); for ER+/ERBB2+, 31% (model range, 23%-41%) vs 69% (model range, 59%-77%); for ER−/ERBB2+, 40% (model range, 34%-47%) vs 60% (model range, 53%-66%); and for ER−/ERBB2−, 48% (model range, 38%-57%) vs 52% (model range, 44%-62%).
Conclusions and Relevance
In this simulation modeling study that projected trends in breast cancer mortality rates among US women, decreases in overall breast cancer mortality from 2000 to 2012 were associated with advances in screening and in adjuvant therapy, although the associations varied by breast cancer molecular subtype.
This simulation study estimates reductions in breast cancer mortality associated with screening and treatment by estrogen-receptor and human epidermal growth factor receptor 2 (ERBB2) status.
Introduction
Breast cancer mortality rates have been steadily declining over time in the United States.1 Simulation models developed within the Cancer Intervention and Surveillance Network (CISNET) estimated that screening mammography and adjuvant therapy (treatment) contributed approximately equally to the reduction in breast cancer mortality from 1975 to 2000.2 Since then, mammography has transitioned from plain-film to digital technology optimized for tumor detection.3,4 At the same time, there have been advances in molecularly targeted treatments based on expression of estrogen-receptor (ER) and human epidermal growth factor receptor 2 (ERBB2, formerly HER2 or HER2/neu), including aromatase inhibitors for ER+, and trastuzumab for ERBB2+ cancers. In addition, there have been advances in chemotherapy, particularly increasing use of taxanes.5,6
It is not known how screening and treatment advances have contributed to recent population-level, molecular subtype–specific breast cancer mortality rates. No single national registry contains sufficient information to assess this progress. Moreover, most clinical trials do not consider both screening and treatment effects and do not readily translate to population effect. Given these circumstances, simulation modeling can be useful to integrate high-quality data from randomized controlled trials, large observational studies, and population registries to estimate the relative contributions of advances on population-level mortality.2
In this report, 6 CISNET models compared the separate and combined contribution associated with screening and treatment on US breast cancer mortality rates by molecular subtype from 2000 to 2012.
Methods
The institutional review board at Georgetown University, the site of the CISNET Breast Cancer Coordinating Center, approved the study as exempt based on the use of deidentified data. The 6 CISNET models were Dana-Farber Cancer Institute (model D),7 Erasmus Medical Center (model E),8 Georgetown University-Albert Einstein College of Medicine (model G-E),9 MD Anderson Cancer Center (model M),10 Stanford University (model S),11,12 and University of Wisconsin-Harvard (model W-H).13 Compared with earlier analyses2,14,15 the models portray ER/ERBB2-specific subtypes,11 include digital screening3,4 and recent treatment advances,16 and have updated incidence17 and competing non–breast cancer mortality.18 The modeling approach is summarized below; additional details are available in the Supplement and online.19
The models incorporated updated estimates of breast cancer incidence17 and ER/ERBB2-specific survival trends in the absence of screening or treatment and then incorporated information on screening use and molecular subtype-specific treatment patterns to reproduce observed US incidence and mortality trends.1,20,21 Screen-detection during the preclinical, screen-detectable period could result in diagnosis of earlier-stage or smaller tumors than diagnosed via symptomatic detection. This could translate into lower breast cancer mortality. Molecular subtype-specific, age-specific, and stage-specific treatment could reduce the hazards of breast cancer death (models D, G-E, M, and S) or result in cure for some cases (models E and W-H).
Model Input Parameters
Each group used a common set of inputs22 based on their specific model structure, prior research,15 and assumptions to best reproduce US breast cancer incidence and mortality trends (eTable 1 in the Supplement).5,6,10,11,12,13,14,15,16,17,22,23,24,25,26,27 Five models used age-period-cohort (APC) analyses to estimate 1975-2012 breast cancer incidence rates in the absence of screening (baseline incidence rate)17,25; model M applied a Bayesian approach to extend 1975-1979 Surveillance Epidemiology and End Results (SEER) rates forward in time with a 4% (SD, 0.2%) annual increase. Plain-film and digital mammography sensitivity data from the Breast Cancer Surveillance Consortium (BCSC) for 1994-2012 were used to estimate sensitivity for detection of invasive and ductal carcinoma in situ cancers by age group, first vs subsequent screening, and time since last mammogram.
Screening dissemination was derived from national survey data for age at first screen and subsequent screening frequency by birth cohort.23,24 Plain-film mammography was assumed before 2000. Digital mammography was phased-in starting in 2001 based on data from the BCSC (unpublished data) and the US Food and Drug Administration Mammography Quality Standards Act and Program.28
Molecular subtype–specific treatment dissemination was based on SEER patterns-of-care special studies for 1975-199626,27 and the National Comprehensive Cancer Network data for 1997 onwards.14,19 Tamoxifen was used in the 1980s; aromatase inhibitor use began in 1997; taxanes in 1998; and trastuzumab in 2006. Treatment effectiveness was conditioned on stage and ER/ERBB2 status (and age, if applicable) based on clinical trials; all estimates assumed local therapy.16
Analyses
Each model simulated mortality rates under 4 intervention scenarios: (1) no screening or treatment (the baseline mortality rate), (2) screening alone, (3) treatment alone, and (4) combined screening and treatment. Rates were age-adjusted using the 2000 US Standard Population,29 and outcomes were reported for women aged 30 to 79 years.
The absolute mortality reductions associated with screening alone, treatment alone, or the combination in a given calendar year were calculated as the difference between the age-adjusted mortality rates predicted with intervention (scenarios 2, 3, or 4) and the baseline mortality rate in that year (scenario 1). The percentage of mortality reduction (hereafter referred to as mortality reduction) in a given calendar year was calculated as this difference divided by the baseline mortality rate in that calendar year (scenario 1; eTable 2 in the Supplement).
ER/ERBB2-specific mortality rates were computed by dividing the number of women who died of breast cancer with that subtype by the total breast cancer population at risk. In this manner, rates of all subtypes sum to the overall age-adjusted breast cancer mortality rate.
To estimate the separate contributions associated with screening and treatment to mortality reductions, we considered the modeled effects of screening alone and of treatment alone as a fraction of the combined modeled effect in each calendar year.
The relative contribution associated with screening vs treatment to the combination associated with both was computed as the ratio of the screening alone modeled effect to the sum of the screening alone modeled effect and the treatment alone modeled effect; the relative contribution associated with treatment was calculated similarly. Alternative approaches for computing these relative contributions were considered, and the main conclusions were unchanged (eMethods and eTable 3 in the Supplement).
When considering the mortality reductions associated with each treatment intervention (eg, chemotherapy, hormonal therapy, and trastuzumab) to their combination, the relative contribution associated with the various treatments was decomposed by first considering the chemotherapy contribution; then the hormonal therapy contribution for ER+ cases, given chemotherapy contributions; and lastly, the contribution associated with trastuzumab for ERBB2+ cases, given the other therapies.
To estimate relative contributions associated with the most recent advancements, we compared the mortality reduction from 2000 to 2012. We focused on this difference to remove the modeled effect of changes in the baseline rate during this period.
Uncertainty Analysis
All results were reported by model and summarized as the mean and range across models. The range provided a measure of uncertainty because each model has different assumptions and structures to represent unobservable factors such as baseline incidence rate and breast cancer natural history. Results consistent across models were considered robust.
Results
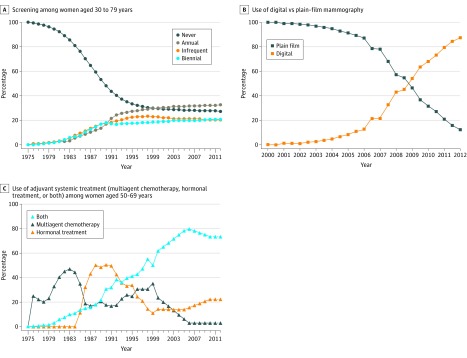
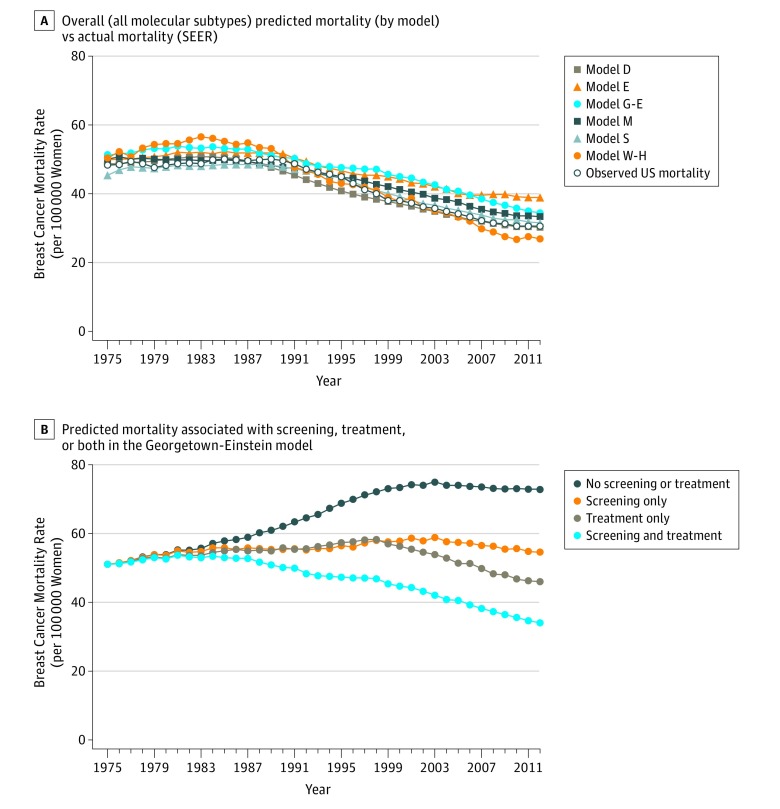
Rates of mammography increased over time (Figure 1A), and plain-film was rapidly replaced by digital mammography starting in 2001 (Figure 1B). Treatment use varied by molecular subtype, age, and stage, with high rates of dissemination of recent advances (Figure 1C). Incorporating these observed screening and treatment patterns, the models reproduced observed age-adjusted incidence (eFigure 1 in the Supplement) and breast cancer mortality trends from 1975 to 2012 (Figure 2A). Predicted mortality trends for a representative model (model G-E) illustrate that the mortality reduction associated with treatment alone increased faster than that associated with screening alone over time (Figure 2B).
Figure 1. Dissemination of Screening Mammography, Type of Mammography, and Adjuvant Therapy Among US Women, 1975-2012.
A, Based on data from multiple rounds of the National Health Interview Survey over time and Breast Cancer Surveillance Consortium (BCSC) data from 1994 to 2012. B, Based on Mammography Quality Standards Act of 1992 data on digital mammography facilities from the US Food and Drug Administration and the BCSC. C, An exemplar stage and set of molecular markers (node-positive AJCC 6 stage 2b, ER+/ERBB2−) at diagnosis based on data from Surveillance, Epidemiology, and End Results (SEER) special patterns of care studies and the National Comprehensive Cancer Network. These data were used for all other combinations of ages, stages, and molecular subtypes. In general, starting in the mid-1990s anthracycline-based, multiagent chemotherapy regimens were in use, and, in 1997, taxanes could be added to those regimens. Hormonal therapy began with tamoxifen in the 1980s and, starting in 1997, also included aromatase inhibitors. For women diagnosed with ERBB2+ tumors (not shown in this example), trastuzumab was disseminated independently of other treatments and, based on its immediate rapid uptake, all ERBB2+ patients were modeled as receiving trastuzumab beginning in year 2006. Models used 2010 treatment dissemination data for subsequent years (indicated by the dashed lines).
Figure 2. Age-Adjusted Predicted Breast Cancer Mortality Rate Among US Women Aged 30 to 79 Years From 1975-2012.
SEER indicates Surveillance, Epidemiology, and End Results. For model abbreviations, see Methods.
Overall Breast Cancer Mortality in 2012
With the observed changes in screening technology and treatment regimens, we estimated a 49% (model range, 39%-58%) decrease in overall breast cancer mortality in 2012 relative to the estimated baseline rate in 2012 of 63 deaths (model range, 54-73) per 100 000 women (Table 1, column 4; eTable 2 in the Supplement). The estimated screening contribution associated with this mortality reduction was 37% (model range, 26%-51%), whereas the contribution associated with treatment was 63% (model range, 49%-74%). The larger contribution associated with treatment vs screening in 2012 was predicted in 5 of 6 models (Table 1, columns 7-8). Note, in 2000, screening was associated with 44% (model range, 35%-60%) of the mortality reduction and treatment was associated with 56% (model range, 40%-65%) (eTable 5 in the Supplement).
Table 1. Overall and Subtype-Specific Breast Cancer Mortality Reductions in 2012 Associated With Screening, Treatment, or Both by Modela.
| Model | Mortality Reduction, %b | Fraction of Combined Mortality Reduction, % | Relative Contribution to Combined Mortality Reduction, %c | ||||
|---|---|---|---|---|---|---|---|
| Associated With Screening Alone | Associated With Treatment Alone | Associated With Screening and Treatmentd | Associated With Screening Alonee | Associated With Treatment Alonef | Associated With Screeningg | Associated With Treatmenth | |
| Overall | |||||||
| Dana-Farber | 29 | 28 | 49 | 59 | 57 | 51 | 49 |
| Erasmus | 18 | 30 | 43 | 41 | 70 | 37 | 63 |
| Georgetown-Einstein | 25 | 37 | 53 | 47 | 69 | 40 | 60 |
| MD Anderson | 17 | 29 | 39 | 44 | 73 | 38 | 62 |
| Stanford | 18 | 37 | 50 | 36 | 74 | 33 | 67 |
| Wisconsin-Harvard | 17 | 49 | 58 | 30 | 84 | 26 | 74 |
| Mean | 21 | 35 | 49 | 43 | 71 | 37 | 63 |
| By Molecular Subtype | |||||||
| ER+/ERBB2− | |||||||
| Dana-Farber | 30 | 30 | 52 | 59 | 58 | 50 | 50 |
| Erasmus | 18 | 34 | 46 | 39 | 73 | 35 | 65 |
| Georgetown-Einstein | 26 | 39 | 54 | 48 | 71 | 40 | 60 |
| MD Anderson | 17 | 31 | 42 | 42 | 75 | 36 | 64 |
| Stanford | 19 | 41 | 53 | 35 | 77 | 31 | 69 |
| Wisconsin-Harvard | 16 | 51 | 59 | 27 | 86 | 24 | 76 |
| Mean | 21 | 38 | 51 | 42 | 73 | 36 | 64 |
| ER+/ERBB2+ | |||||||
| Dana-Farber | 27 | 38 | 57 | 46 | 67 | 41 | 59 |
| Erasmus | 20 | 42 | 52 | 39 | 82 | 32 | 68 |
| Georgetown-Einstein | 24 | 43 | 58 | 41 | 74 | 36 | 64 |
| MD Anderson | 18 | 38 | 46 | 38 | 82 | 32 | 68 |
| Stanford | 17 | 58 | 66 | 26 | 88 | 23 | 77 |
| Wisconsin-Harvard | 19 | 62 | 71 | 26 | 87 | 23 | 77 |
| Mean | 21 | 47 | 58 | 36 | 80 | 31 | 69 |
| ER−/ERBB2+ | |||||||
| Dana-Farber | 25 | 28 | 49 | 52 | 58 | 47 | 53 |
| Erasmus | 17 | 28 | 41 | 40 | 68 | 37 | 63 |
| Georgetown-Einstein | 25 | 32 | 52 | 48 | 62 | 43 | 57 |
| MD Anderson | 15 | 23 | 33 | 45 | 70 | 39 | 61 |
| Stanford | 17 | 25 | 40 | 42 | 63 | 40 | 60 |
| Wisconsin-Harvard | 23 | 43 | 55 | 41 | 79 | 34 | 66 |
| Mean | 20 | 30 | 45 | 45 | 67 | 40 | 60 |
| ER−/ERBB2− | |||||||
| Dana-Farber | 26 | 20 | 40 | 66 | 50 | 57 | 43 |
| Erasmus | 17 | 22 | 35 | 47 | 64 | 43 | 57 |
| Georgetown-Einstein | 24 | 29 | 46 | 53 | 63 | 45 | 55 |
| MD Anderson | 18 | 14 | 27 | 65 | 52 | 56 | 44 |
| Stanford | 18 | 17 | 33 | 53 | 50 | 52 | 48 |
| Wisconsin-Harvard | 18 | 30 | 42 | 43 | 70 | 38 | 62 |
| Mean | 20 | 22 | 37 | 55 | 58 | 48 | 52 |
Abbreviations: ER, estrogen-receptor; ERBB2; human epidermal growth factor receptor 2.
The column labels are defined as follows:
Relative to the estimated baseline mortality in 2012.
These columns sum to 100%.
Combined mortality reduction.
Column 2 divided by column 4.
Column 3 divided by column 4.
Column 2 divided by the sum of columns 2 and 3.
Column 3 divided by the sum of columns 2 and 3.
The estimated 63% (model range, 49%-74%) relative contribution associated with treatment in 2012 consisted of 31% (model range, 22%-37%) from chemotherapy, 27% (model range, 18%-36%) from hormone therapy, and 4% (model range, 1%-6%) from trastuzumab (Table 2).
Table 2. Relative Contributions of Treatments to Mortality Reduction in 2012.
| Model | Relative Contribution, %a | ||
|---|---|---|---|
| Associated With Chemotherapy | Associated With Hormone Therapy | Associated With Trastuzumab | |
| Overall | |||
| Dana-Farber | 23 | 24 | 2 |
| Erasmus | 37 | 25 | 1 |
| Georgetown-Einstein | 37 | 18 | 4 |
| MD Anderson | 22 | 34 | 6 |
| Stanford | 34 | 28 | 5 |
| Wisconsin-Harvard | 33 | 36 | 5 |
| Mean | 31 | 27 | 4 |
| By Molecular Subtype | |||
| ER+/ERBB2− | |||
| Dana-Farber | 25 | 25 | 0 |
| Erasmus | 30 | 35 | 0 |
| Georgetown-Einstein | 34 | 24 | 0 |
| MD Anderson | 21 | 42 | 0 |
| Stanford | 33 | 36 | 0 |
| Wisconsin-Harvard | 29 | 47 | 0 |
| Mean | 29 | 35 | 0 |
| ER+/ERBB2+ | |||
| Dana-Farber | 24 | 23 | 12 |
| Erasmus | 28 | 30 | 10 |
| Georgetown-Einstein | 32 | 23 | 9 |
| MD Anderson | 15 | 36 | 18 |
| Stanford | 30 | 30 | 17 |
| Wisconsin-Harvard | 25 | 34 | 18 |
| Mean | 26 | 29 | 14 |
| ER−/ERBB2+ | |||
| Dana-Farber | 36 | 0 | 16 |
| Erasmus | 45 | 0 | 18 |
| Georgetown-Einstein | 43 | 0 | 11 |
| MD Anderson | 24 | 0 | 29 |
| Stanford | 35 | 0 | 25 |
| Wisconsin-Harvard | 42 | 0 | 23 |
| Mean | 37 | 0 | 21 |
| ER−/ERBB2− | |||
| Dana-Farber | 43 | 0 | 0 |
| Erasmus | 57 | 0 | 0 |
| Georgetown-Einstein | 55 | 0 | 0 |
| MD Anderson | 44 | 0 | 0 |
| Stanford | 48 | 0 | 0 |
| Wisconsin-Harvard | 62 | 0 | 0 |
| Mean | 52 | 0 | 0 |
Abbreviations: ER, estrogen-receptor; ERBB2; human epidermal growth factor receptor 2.
The row sum of columns 2 through 4 equals the value in the corresponding row in column 8 of Table 1, within rounding error.
Molecular Subtype–Specific Breast Cancer Mortality in 2012
The ER+/ERBB2− subtype was estimated to be associated with 64% (model range, 61%-70%) of the overall mortality reduction in 2012 because it was the most common subtype (eTable 7 in the Supplement).
Within-subtype analyses demonstrated significant variations in breast cancer mortality reduction in 2012 (vs estimated subtype-specific baseline rates; Table 1, column 4). The estimated mortality reduction was largest for the ER+/ERBB2+ subtype at 58% (model range, 46%-71%), followed by ER+/ERBB2− at 51% (model range, 42%-59%), and ER−/ERBB2+ at 45% (model range, 33%-55%). The lowest mortality reduction was estimated for the ER−/ERBB2− subtype at 37% (model range, 27%-46%).
The estimated relative contributions associated with screening vs treatment also varied by molecular subtype, ranging from 31% (model range, 23%-41%) with screening vs 69% (model range, 59%-77%) with treatment for the ER+/ERBB2+ subtype to 48% (model range, 38%-57%) with screening vs 52% (model range, 43%-62%) with treatment for ER−/ERBB2− (Table 1, columns 7-8). The estimated relative contributions associated with specific treatments varied by subtype (Table 2). For example, for the ER+/ERBB2+ subtype, of the 69% (model range, 59%-77%) relative contribution associated with treatment, 26% (model range, 15%-32%) was associated with chemotherapy, 29% (model range, 23%-36%) with hormone therapy, and 14% (model range, 9%-18%) with trastuzumab (Table 2). For the ER−/ERBB2− subtype, the 52% (model range, 43%-62%) relative contribution associated with treatment was associated with chemotherapy alone.
Contribution Associated With Screening and Treatment Advances From 2000 To 2012
The estimated overall breast cancer mortality reduction in 2000 was 37% (model range, 27%-42%) relative to the estimated baseline rate in 2000 of 64 deaths (model range, 56-73) per 100 000 women (Table 3, column 2; eTable 2 in the Supplement). The estimated overall breast cancer mortality reduction in 2012 was 49% (model range, 39%-58%) relative to the estimated baseline rate in 2012 of 63 deaths (model range, 54-73) per 100 000 women (Table 3, column 3; eTable 2 in the Supplement). Hence, the estimated difference in the overall breast cancer mortality reduction in 2012 vs 2000 was 12% (model range, 10%-16%) (Table 3, column 4; eTable 5 in the Supplement). The estimated relative contribution associated with screening advances to this difference was 17% (model range, 2%-31%) (Table 3, column 5); treatment advances were 83% (model range, 69%-98%) (Table 3, sum of columns 6-8, with rounding; eTable 5 in the Supplement). Of the 83% (model range, 69%-98%) treatment-related advances, 38% (model range, 21%-54%) was associated with advances in chemotherapy (largely taxanes); 29% (model range, 9%-44%) was associated with advances in hormone therapy (largely the addition of aromatase inhibitors), and 15% (model range, 4%-25%) with the introduction of trastuzumab (Table 3, columns 6-8).
Table 3. Relative Contributions Associated with Advances in Screening and Treatment to the Difference in the Mortality Reduction Between 2000 and 2012a.
| Model | Mortality Reduction, % | Relative Contributions to the Difference in the Mortality Reduction Between 2000 and 2012, % | |||||
|---|---|---|---|---|---|---|---|
| In 2000b | In 2012c | Difference Between 2000 and 2012d | Associated With Screening Advances | Associated With Chemotherapy Advances | Associated With Hormone Therapy Advances | Associated With Trastuzumab | |
| Overall | |||||||
| Dana-Farber | 39 | 49 | 10 | 13 | 34 | 44 | 10 |
| Erasmus | 32 | 43 | 10 | 31 | 32 | 33 | 4 |
| Georgetown-Einstein | 39 | 53 | 14 | 21 | 54 | 9 | 15 |
| MD Anderson | 27 | 39 | 13 | 23 | 21 | 37 | 18 |
| Stanford | 40 | 50 | 10 | 14 | 41 | 20 | 25 |
| Wisconsin-Harvard | 42 | 58 | 16 | 2 | 48 | 31 | 18 |
| Mean | 37 | 49 | 12 | 17 | 38 | 29 | 15 |
| By Molecular Subtype | |||||||
| ER+/ERBB2− | |||||||
| Dana-Farber | 43 | 52 | 9 | 14 | 39 | 47 | 0 |
| Erasmus | 34 | 46 | 13 | 21 | 14 | 64 | 0 |
| Georgetown-Einstein | 41 | 54 | 13 | 29 | 62 | 9 | 0 |
| MD Anderson | 29 | 42 | 13 | 24 | 25 | 50 | 0 |
| Stanford | 45 | 53 | 8 | 19 | 46 | 35 | 0 |
| Wisconsin-Harvard | 45 | 59 | 14 | 3 | 49 | 48 | 0 |
| Mean | 39 | 51 | 12 | 19 | 39 | 42 | 0 |
| ER+/ERBB2+ | |||||||
| Dana-Farber | 41 | 57 | 17 | 10 | 19 | 29 | 42 |
| Erasmus | 33 | 52 | 19 | 24 | 8 | 41 | 27 |
| Georgetown-Einstein | 41 | 58 | 17 | 14 | 46 | 16 | 24 |
| MD Anderson | 28 | 46 | 18 | 17 | 6 | 32 | 45 |
| Stanford | 47 | 66 | 19 | 4 | 23 | 14 | 58 |
| Wisconsin-Harvard | 46 | 71 | 25 | 0 | 29 | 20 | 51 |
| Mean | 39 | 58 | 19 | 12 | 22 | 25 | 41 |
| ER−/ERBB2+ | |||||||
| Dana-Farber | 33 | 49 | 16 | 11 | 37 | 0 | 52 |
| Erasmus | 26 | 41 | 15 | 13 | 37 | 0 | 50 |
| Georgetown-Einstein | 33 | 52 | 19 | 21 | 44 | 0 | 35 |
| MD Anderson | 20 | 33 | 13 | 20 | 3 | 0 | 78 |
| Stanford | 26 | 40 | 14 | 0 | 30 | 0 | 70 |
| Wisconsin-Harvard | 33 | 55 | 22 | 0 | 42 | 0 | 58 |
| Mean | 29 | 45 | 15 | 11 | 32 | 0 | 57 |
| ER−/ERBB2− | |||||||
| Dana-Farber | 34 | 40 | 6 | 13 | 87 | 0 | 0 |
| Erasmus | 26 | 35 | 10 | 34 | 66 | 0 | 0 |
| Georgetown-Einstein | 35 | 46 | 11 | 14 | 86 | 0 | 0 |
| MD Anderson | 22 | 27 | 5 | 41 | 59 | 0 | 0 |
| Stanford | 27 | 33 | 7 | 23 | 77 | 0 | 0 |
| Wisconsin-Harvard | 32 | 42 | 10 | 9 | 91 | 0 | 0 |
| Mean | 29 | 37 | 8 | 22 | 78 | 0 | 0 |
Abbreviations: ER, estrogen-receptor; ERBB2; human epidermal growth factor receptor 2.
Details on the computations are included in eMethods and eTable 5 in the Supplement. Briefly, in terms of means only, the overall mortality reduction between 2000 and 2012 associated with combined screening and treatment advances is estimated to be 12% (column 4). In 2012, the estimated relative contribution of screening to the mortality reduction associated with combined screening and treatment is 37% (Table 1, column 7). Hence, in 2012, the mortality reduction associated with screening is 37% of 49% = 18%. Similarly, in 2000, the mortality reduction associated with screening is 16% (eTable 5, row F). The difference in the mortality reduction associated with screening advances between 2012 and 2000 is 2% (= 18% in 2012 minus 16% in 2000). The relative contribution of screening advances to the mortality reduction associated with combined screening and treatment advances is 2% divided by 12% (column 4), giving 17% (column 5). The remainder (83% = 100% − 17%) is associated with treatment advances between 2000 and 2012; 83% is distributed by treatment type in columns 6 through 8. Columns 5 to 8 total 100%, within rounding error.
Relative to the estimated baseline mortality rate in 2000.
Relative to the estimated baseline mortality rate in 2012.
Difference of columns 3 and 2.
Within each molecular subtype, the estimated difference in the breast cancer mortality reductions from 2000 to 2012 was largest for the ER+/ERBB2+ subtype at 19% (model range, 17%-25%) and the smallest for ER−/ERBB2− at 8% (model range, 5%-11%) (Table 3, column 4). The estimated relative contribution associated with screening and treatment to these differences also varied by subtype: the relative contribution associated with trastuzumab was 41% (model range, 27%-58%) in the ER+/ERBB2+ subtype and 57% (model range, 35%-78%) in ER−/ERBB2+ (Table 3, column 8).
To complement the above analysis, we decomposed the overall mortality reduction in 2012 in terms of the contributions associated with advances before 2000 and after 2000 (eTable 6 in the Supplement). Of the 37% mortality reduction (model range, 27%-42%) associated with screening in 2012, 33% (model range, 29%-48%) was associated with screening advances before 2000 and 4% (model range, 1%-8%) after 2000 (largely digital mammography). The introduction of trastuzumab was associated with 15% of overall mortality reduction between 2000 and 2012. Of the 31% mortality reduction (model range, 23%-37%) associated with chemotherapy, 22% (model range, 15%-30%) was associated with chemotherapy advances before 2000 and 9% (model range, 7%-14%) after 2000 (largely taxanes). Of the 27% mortality reduction (model range, 18%-36%) associated with hormone therapy, 20% (model range, 15%-27%) was associated with advances in hormone therapy before 2000 and 7% (model range, 2%-12%) after 2000 (largely from aromatase inhibitors). eTable 6 in the Supplement provides subtype-specific results.
Discussion
This model-based analysis provides clinically relevant insights about the separate and combined population contributions associated with screening and treatment advances on reducing breast cancer mortality by molecular subtype. Six independent models found that both screening and treatment were associated with overall and subtype-specific breast cancer mortality decreases over time. Between 2000 and 2012, advances in treatment were associated with a larger contribution than screening to overall US breast cancer mortality decreases and for all molecular subtypes except ER−/ERBB2−, the subtype that also had the lowest modeled mortality reduction.
These results build upon past CISNET analyses and other studies that have examined the period before 20002,30,31,32 or considered the role of ER− status.15,33 The current analysis considered the study period from 2000 to 2012. In this period, digital mammography increased screening sensitivity compared with plain-film mammography, especially for women younger than 50 years and women with dense breasts,34 and has increased somewhat the number of breast cancer deaths averted with screening.35 The current results support findings that advances in mammography continue to contribute to reducing breast cancer mortality. It will be important to update the analysis when there is sufficient evidence about the benefits of tomosynthesis or other emerging screening approaches.36,37
Even with the recent screening advances, findings from this model-based analysis demonstrate a shift in the relative contributions associated with screening and treatment to breast cancer mortality, with greater contributions associated with treatment in 2012. Recent observational analyses have also found stage-specific survival improvements related to current treatment.33 The results from this model analysis confirm the benefits at the population level from the discovery and rapid dissemination over this past decade of several new classes of molecularly targeted therapies, improvements in delivery of standard regimens, and refinements in therapy based on molecular subtype according to ER and ERBB2 status.
A unique contribution of this population-level analysis is how the relative contributions associated with screening and treatment varied by molecular subtype. In 2012, when gains from treatment alone were estimated, treatment alone could have been associated with roughly 70% of the predicted mortality reduction achieved with both screening and treatment for the all the subtypes expressing the ER, ERBB2 receptors, or both. However, screening is likely to remain important even if future treatments could cure all breast cancers because screening can detect disease at earlier stages, which has less surgical and treatment-related morbidity compared with more advanced stages.
Among the advances in recent adjuvant therapies, advances in chemotherapy with the addition of taxanes were associated with roughly 37% of the difference in overall breast cancer mortality reduction from 2000 to 2012. Advances in hormone therapy with the addition of aromatase inhibitors had comparable contribution associated with mortality reduction. The contribution associated with trastuzumab was smaller on overall mortality reduction (15%), because ERBB2+ cases account for approximately 20% of all newly diagnosed breast cancer cases, with variations based on age and race.38 However, trastuzumab was associated with more than 40% of the difference in mortality reduction from 2000 to 2012 among the ERBB2+ subtypes.
All of the models concluded that the ER−/ERBB2− subtype had the lowest overall modeled mortality reduction over time, although the relative contributions associated with screening and treatment varied somewhat by model, with 3 of the 6 models estimating a modestly higher contribution associated with treatment compared with screening in 2012. Prior analysis of SEER data have similar results, with greater mortality declines for those with ER+ vs ER− tumors.15,39 Given that treatment advancements are lagging for ER−/ERBB2− cancers, more intensive screening approaches, or screening with different modalities, might be considered for groups at highest risk for this subtype, including African American women. Continued investments to discover molecularly targeted treatments for the ER−/ERBB2− subgroup remain important to continue to lower breast cancer death rates.
Overall, the models projected that screening and treatment each were associated with continued reductions in breast cancer mortality, but, in 2012, treatment was associated with a larger relative proportion than screening of the mortality reductions overall and for all subtypes, except the ER−/ERBB2−. Because ER+ cancers are the most prevalent and this group is expected to increase with time,40 additional advances for this subtype could have the largest effect on reducing the overall population burden of breast cancer. Looking ahead, model-based approaches may continue to be important to evaluate continued population-level progress in reducing the burden of breast cancer through a combination of continued discovery and dissemination of effective molecularly targeted therapies, invention of novel screening technologies to optimize early detection of aggressive cancer subtypes, and greater ability to identify risk of developing specific molecular subtypes to permit tailored prevention and early detection.
This study has several strengths. First, by synthesizing national and clinical trial data, the results fill an important knowledge gap, especially because current surveillance data systems do not contain information on both screening and treatment. Second, the main findings were robust across 6 independent models, despite differences in model structures and assumptions. Third, the validity of this comparative modeling approach is supported by the consistency of conclusions across models, and the ability of each model to closely replicate the patterns of observed trends in incidence and mortality.
Limitations
This research has several limitations. First, the accuracy of model results depends on the availability of good-quality data for input parameters and reasonable assumptions about unobservable events. For instance, because there are limited long-term clinical trial or registry data on survival by ERBB2 status, the models extrapolated long-term survival. Second, modeled treatment effects were based on efficacy in trials included in the Oxford Overview,16 so there could be a slight overestimation of actual population treatment effects and the relative contribution of treatment to mortality reductions. Third, each model also made different assumptions about the baseline incidence and natural history of breast cancer, leading to variability in the magnitude of results. Fourth, the models considered only 5 years of hormonal therapy since recommendations to consider 10 years among women at high-risk of late recurrence were just recently introduced and have not yet been uniformly applied. Future modeling could incorporate the population-level dissemination and effectiveness of longer-term hormonal therapy. Fifth, progesterone-receptor status was not explicitly modeled because it is missing from many data sources. Sixth, subtype results for various racial/ethnic subgroups were not modeled. Understanding interactions between race, ethnicity, and subtype-specific outcomes represents an important future direction.41 Seventh, the effect of screening and subtype-specific treatment on morbidity and all-cause mortality was not evaluated. Eighth, modeling was based on estimates until 2012, and it is uncertain whether or how well these estimates reflect current breast cancer screening, treatment, or outcomes after 2012.
Conclusions
In this simulation modeling study that projected trends in breast cancer mortality rates among US women, decreases in overall breast cancer mortality from 2000 to 2012 were associated with advances in screening and in adjuvant therapy, although the associations varied by breast cancer molecular subtype.
eMethods.
eTable 1. Model Parameters
eTable 2. Computation of the Mortality Reduction, Relative to the Baseline Rate
eTable 3. Comparison of 3 Alternative Methods to Compute the Relative Contributions Associated With Screening and Treatment on Overall Breast Cancer Mortality Reduction
eTable 4. Comparison of Breast Cancer Mortality Reduction, Overall and By ER/ERBB2-Subtype in 2000 vs 2012
eTable 5. Relative Contributions Associated With Screening and Treatment Advances on the Difference in the Breast Cancer Mortality Reduction Between 2000 and 2012
eTable 6. Relative Contributions Associated With Screening, Chemotherapy, Hormone Therapy and Trastuzumab to Breast Cancer Mortality Reduction in 2012, Broken Down by Advances Before and After 2000
eTable 7. Breakdown of Overall Breast Cancer Mortality Reduction in 2012 by Molecular Subtype
eFigure 1. Comparison of Model Projections to Observed US Breast Cancer Incidence, for Women Ages 30-79
eFigure 2. Comparison of Model Projections for ER-/ ERBB2-Specific Breast Cancer Mortality Trends Between 1975-2012, for Women Ages 30-79, by Molecular Subtype
eFigure 3. Individual Model Projections for Overall US Breast Cancer Incidence and Mortality (vs SEER) and ER/ERBB2-Subtype-Specific Mortality From 1975-2012, for Women Ages 30-79
eReferences
References
- 1.National Cancer Institute Surveillance, Epidemiology, and End Results Program. Breast Cancer Statistics. https://seer.cancer.gov/statfacts/html/breast.html. Accessed March 31, 2017.
- 2.Berry DA, Cronin KA, Plevritis SK, et al. ; Cancer Intervention and Surveillance Modeling Network (CISNET) Collaborators . Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005;353(17):1784-1792. [DOI] [PubMed] [Google Scholar]
- 3.Kerlikowske K, Hubbard RA, Miglioretti DL, et al. ; Breast Cancer Surveillance Consortium . Comparative effectiveness of digital versus film-screen mammography in community practice in the United States: a cohort study. Ann Intern Med. 2011;155(8):493-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kerlikowske K, Zhu W, Tosteson AN, et al. ; Breast Cancer Surveillance Consortium . Identifying women with dense breasts at high risk for interval cancer: a cohort study. Ann Intern Med. 2015;162(10):673-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giordano SH, Temin S, Kirshner JJ, et al. ; American Society of Clinical Oncology . Systemic therapy for patients with advanced human epidermal growth factor receptor 2-positive breast cancer: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2014;32(19):2078-2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Comprehensive Cancer Network Breast Cancer Guidelines NCCN guidelines and clinical resources. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed March 31, 2017.
- 7.Lee SJ, Li X, Huang H, Zelen M. The Dana-Farber CISNET model for breast cancer screening strategies: an update. Med Decis Making. 2018;38(1s). doi: 10.1177/0272989X17741634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van den Broek JJ, van Ravesteyn NT, Heijnsdijk EA, de Koning H. Simulating the impact of risk-based screening and treatment on breast cancer outcomes with MISCAN-Fadia. Med Decis Making. 2018;38(1s). doi: 10.1177/0272989X17711928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schechter CB, Near AM, Jayasekera J, Chang Y, Mandelblatt JS. Structure, function, and applications of the Georgetown-Einstein (GE) breast cancer simulation model. Med Decis Making. 2018;38(1s). doi: 10.1177/0272989X17698685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang X, Li Y, Song J, Berry D. A Bayesian simulation model for breast cancer screening, incidence, treatment, and mortality. Med Decis Making. 2018;38(1s). doi: 10.1177/0272989X17714473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Munoz D, Plevritis SK. Estimating breast cancer progression features and survival by molecular subtype in the absence of screening and treatment. Med Decis Making. 2018;38(1s). doi: 10.1177/0272989X17743236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Munoz D, Xu C, Plevritis S. A molecular subtype-specific stochastic simulation model of US breast cancer incidence and mortality trends from 1975 to 2010. Med Decis Making. 2018;38(1s). doi: 10.1177/0272989X17737508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alagoz O, Ergun MA, Cevik M, et al. The University of Wisconsin breast cancer epidemiology simulation model: an update. Med Decis Making. 2018;38(1s). doi: 10.1177/0272989X17711927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mandelblatt JS, Cronin KA, Bailey S, et al. ; Breast Cancer Working Group of the Cancer Intervention and Surveillance Modeling Network . Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med. 2009;151(10):738-747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Munoz D, Near AM, van Ravesteyn NT, et al. Effects of screening and systemic adjuvant therapy on ER-specific US breast cancer mortality. J Natl Cancer Inst. 2014;106(11):dju289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peto R, Davies C, Godwin J, et al. ; Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) . Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100 000 women in 123 randomised trials. Lancet. 2012;379(9814):432-444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gangnon RE, Sprague BL, Stout NK, et al. The contribution of mammography screening to breast cancer incidence trends in the United States: an updated age-period-cohort model. Cancer Epidemiol Biomarkers Prev. 2015;24(6):905-912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gangnon RE, Stout NK, Alagoz O, Hampton JM, Sprague BL, Trentham-Dietz A. Contribution of breast cancer to overall mortality for US women. Med Decis Making. 2018;38(1s). doi: 10.1177/0272989X17717981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mandelblatt JS, Cronin K, de Koning H, Miglioretti DL, Schechter CS, Stout N. Collaborative modeling of US breast cancer screening strategies: AHRQ publication No 14-05201-EF-4. https://www.uspreventiveservicestaskforce.org/Page/Document/modeling-report-collaborative-modeling-of-us-breast-cancer-1/breast-cancer-screening1. Accessed May 1, 2015.
- 20.Surveillance, Epidemiology, and End Results (SEER) Program SEER*Stat database: mortality—all COD, aggregated with state, total US (1969-2014) <Katrina/Rita population adjustment>, National Cancer Institute, DCCPS, Surveillance Research Program. Released December 2016. https://www.seer.cancer.gov/. Accessed December 14, 2017.
- 21.National Center for Health Statistics Compressed mortality file. https://www.cdc.gov/nchs/data_access/cmf.htm. Accessed March 31, 2017.
- 22.Mandelblatt JS, Near AM, Miglioretti DL, et al. Common model inputs used in CISNET collaborative breast cancer modeling. Med Decis Making. 2018;38(1s). doi: 10.1177/0272989X17700624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cronin KA, Mariotto AB, Clarke LD, Feuer EJ. Additional common inputs for analyzing impact of adjuvant therapy and mammography on US mortality. J Natl Cancer Inst Monogr. 2006;(36):26-29. [DOI] [PubMed] [Google Scholar]
- 24.Cronin KA, Yu B, Krapcho M, et al. Modeling the dissemination of mammography in the United States. Cancer Causes Control. 2005;16(6):701-712. [DOI] [PubMed] [Google Scholar]
- 25.Holford TR, Cronin KA, Mariotto AB, Feuer EJ. Changing patterns in breast cancer incidence trends. J Natl Cancer Inst Monogr. 2006;(36):19-25. [DOI] [PubMed] [Google Scholar]
- 26.Mariotto A, Feuer EJ, Harlan LC, Wun LM, Johnson KA, Abrams J. Trends in use of adjuvant multi-agent chemotherapy and tamoxifen for breast cancer in the United States: 1975-1999. J Natl Cancer Inst. 2002;94(21):1626-1634. [DOI] [PubMed] [Google Scholar]
- 27.Mariotto AB, Feuer EJ, Harlan LC, Abrams J. Dissemination of adjuvant multiagent chemotherapy and tamoxifen for breast cancer in the United States using estrogen receptor information: 1975-1999. J Natl Cancer Inst Monogr. 2006;(36):7-15. [DOI] [PubMed] [Google Scholar]
- 28.US Food and Drug Administration Mammography Quality Standards Act and program. https://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActandProgram/default.htm. Accessed January 1, 2015.
- 29.US Bureau of the Census Population Projections of the United States by Age, Sex, Race and Hispanic Origin: 1995 to 2050: Current Population Reports, P25-1130. Washington, DC: US Government Printing Office; 1996. [Google Scholar]
- 30.Elkin EB, Hudis C, Begg CB, Schrag D. The effect of changes in tumor size on breast carcinoma survival in the US: 1975-1999. Cancer. 2005;104(6):1149-1157. [DOI] [PubMed] [Google Scholar]
- 31.Hermon C, Beral V. Breast cancer mortality rates are levelling off or beginning to decline in many western countries: analysis of time trends, age-cohort and age-period models of breast cancer mortality in 20 countries. Br J Cancer. 1996;73(7):955-960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peto R, Boreham J, Clarke M, Davies C, Beral V. UK and USA breast cancer deaths down 25% in year 2000 at ages 20-69 years. Lancet. 2000;355(9217):1822. [DOI] [PubMed] [Google Scholar]
- 33.Park JH, Anderson WF, Gail MH. Improvements in US breast cancer survival and proportion explained by tumor size and estrogen-receptor status. J Clin Oncol. 2015;33(26):2870-2876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pisano ED, Gatsonis C, Hendrick E, et al. ; Digital Mammographic Imaging Screening Trial (DMIST) Investigators Group . Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med. 2005;353(17):1773-1783. [DOI] [PubMed] [Google Scholar]
- 35.Stout NK, Lee SJ, Schechter CB, et al. Benefits, harms, and costs for breast cancer screening after US implementation of digital mammography. J Natl Cancer Inst. 2014;106(6):dju092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Friedewald SM, Rafferty EA, Rose SL, et al. Breast cancer screening using tomosynthesis in combination with digital mammography. JAMA. 2014;311(24):2499-2507. [DOI] [PubMed] [Google Scholar]
- 37.Lee CI, Lehman CD. Digital breast tomosynthesis and the challenges of implementing an emerging breast cancer screening technology into clinical practice. J Am Coll Radiol. 2013;10(12):913-917. [DOI] [PubMed] [Google Scholar]
- 38.Howlader N, Altekruse SF, Li CI, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106(5):dju055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jatoi I, Chen BE, Anderson WF, Rosenberg PS. Breast cancer mortality trends in the United States according to estrogen receptor status and age at diagnosis. J Clin Oncol. 2007;25(13):1683-1690. [DOI] [PubMed] [Google Scholar]
- 40.Rosenberg PS, Barker KA, Anderson WF. Estrogen receptor status and the future burden of invasive and in situ breast cancers in the United States. J Natl Cancer Inst. 2015;107(9):pii:djv159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iqbal J, Ginsburg O, Rochon PA, Sun P, Narod SA. Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the United States. JAMA. 2015;313(2):165-173. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eTable 1. Model Parameters
eTable 2. Computation of the Mortality Reduction, Relative to the Baseline Rate
eTable 3. Comparison of 3 Alternative Methods to Compute the Relative Contributions Associated With Screening and Treatment on Overall Breast Cancer Mortality Reduction
eTable 4. Comparison of Breast Cancer Mortality Reduction, Overall and By ER/ERBB2-Subtype in 2000 vs 2012
eTable 5. Relative Contributions Associated With Screening and Treatment Advances on the Difference in the Breast Cancer Mortality Reduction Between 2000 and 2012
eTable 6. Relative Contributions Associated With Screening, Chemotherapy, Hormone Therapy and Trastuzumab to Breast Cancer Mortality Reduction in 2012, Broken Down by Advances Before and After 2000
eTable 7. Breakdown of Overall Breast Cancer Mortality Reduction in 2012 by Molecular Subtype
eFigure 1. Comparison of Model Projections to Observed US Breast Cancer Incidence, for Women Ages 30-79
eFigure 2. Comparison of Model Projections for ER-/ ERBB2-Specific Breast Cancer Mortality Trends Between 1975-2012, for Women Ages 30-79, by Molecular Subtype
eFigure 3. Individual Model Projections for Overall US Breast Cancer Incidence and Mortality (vs SEER) and ER/ERBB2-Subtype-Specific Mortality From 1975-2012, for Women Ages 30-79
eReferences