Abstract
Objective
To deeply verify the clinical significance of CXCR3 in prediction of cancer patients’ prognosis.
Data sources
We performed a meta-analysis including 12 studies searched from PubMed, Web of Science, Embase, and Cochrane databases. A total of 1,751 patients were used to analyze the association between CXCR3 and patients’ prognosis, based on either overall survival or time to tumor progression.
Study selection
Studies evaluating CXCR3 expression for predicting prognosis in human solid tumors were included.
Results
It showed that patients with higher expression of CXCR3 had significantly shorter OS (pooled hazard ratio =2.315, 95% CI: 1.162–4.611, P=0.017). In addition, higher CXCR3 expression was associated with distant metastasis (yes vs no: pooled relative ratio [RR] =1.828, 95% CI: 1.140–2.931, P=0.012) in solid tumors and indicated advanced tumor stage (III/IV vs I/II, RR =2.656, 95% CI: 1.809–3.900, P<0.001) and lymph node metastasis (yes vs no: RR =2.28, 95% CI: 1.61–3.25, P<0.001) in colorectal cancer.
Conclusion
Our study highlights the role of CXCR3 as a potential prognostic marker and a promising therapeutic target in solid tumors.
Keywords: CXCR3, meta-analysis, solid tumor, prognostic marker, overall survival
Introduction
Chemokines comprise a family of chemotactic cytokines with low molecular weight which participate in multiple biologic processes such as angiogenesis, migration of leukocytes, tumor growth, and metastasis.1–3 There are currently four major families of chemokines based on the position of conserved cysteines of these small inducible proteins: CXC, CC, CX3C, and C.4 The CXC subgroup can be further classified into two groups, ELR+ and ELR− chemokines, according to the presence or absence of the “glu-leu-arg (ELR)” motif.5 Most, if not all, chemokines function through binding to and activating a family of G-protein–coupled receptors, namely, CXCR or CCR.6 Recent studies have highlighted the clinical importance of chemokines and their receptors in tumor initiation, progression, and metastasis.7 Among them, we noticed CXCR3 and analyzed several roles of it that seem to be of particular importance to us, especially its effects on tumor prognosis.
As the main receptor of the ELR− chemokines, CXCR3 is activated by specific binding of the ligands, CXCL4/PF4, CXCL9/MIG, CXCL10/IP10, CXCL11/IP9, and thus results in diverse cellular responses such as chemotactic migration, cell proliferation, or inhibition of migration according to different cell types and distinct microenvironment.8,9 It is reported that CXCR3 was upregulated in many human tumors; furthermore, the increased levels were correlated with poor prognosis in breast cancer, melanoma, renal cancer, prostate cancer, and colorectal cancer patients.9–13 In colon cancer specimens, high expression of CXCR3 was correlated with the metastatic frequencies to lymph nodes and distant organs; meanwhile, CXCR3-positive colon cancer patients exhibited shorter survival than CXCR3-negative patients.7 Importantly, the systematic administration of a CXCR3 inhibitor, AMG487, was recently reported to inhibit lung metastasis of colon cancer and breast cancer in a mouse model.14,15 Another group demonstrated that CXCR3 could be a molecular target in breast cancer metastasis.16 However, a study involving 96 gastric cancer patients reported opposite results.17 Overexpression of CXCR3 was found to be inversely associated with invasion depth and metastasis in gastric cancer, and further analysis showed that high CXCR3 expression was an independent prognostic factor and associated with favorable prognosis.
As for the multiple roles of CXCR3 in various biophysical processes, especially its divergent performance in different types of cancers, we herein carried out this meta-analysis to address the overall roles of CXCR3 in cancer patients’ prognosis. This study aimed at defining the clinical value of CXCR3 molecule, thereby supporting the use of specific genetic diagnosis for cancer patients and development of targeted strategies against CXCR3.
Materials and methods
Literature search
For this study, we searched papers published before 1 April 2017 from PubMed, Embase, Web of Science, and Cochrane databases, using the following search strategy: (“CXCR3” or “CMKBR3” or “CD183” or “Chemokine C-C Motif Receptor 3” or “CXC Chemokine Receptor 3”) and (“cancer” or “tumor” or “carcinoma” or “neoplasm”) and (“prognosis” or “survival” or “mortality” “death”). Furthermore, we manually searched the reference lists of relevant literature. When multiple studies of the same patient population were identified, we included the published study with the largest sample size.
Selection criteria
Articles were selected if they met the following criteria: 1) evaluation of CXCR3 expression for predicting prognosis in human cancer; 2) studies reporting survival data; 3) studies that detected CXCR3 protein expression by immunohistochemistry; and 4) studies with adequate data of pooled HRs and 95% CIs to be extracted or calculated. The exclusion criteria were as follows: 1) duplicate publication; 2) non-English papers; 3) author’s view, commentary, conference abstract, or review articles; 4) sample number fewer than 40 patients; 5) study only focused on animal models or cancer cell lines; and 6) study lacking sufficient data for individual HRs and 95% CIs to be extracted or calculated.18 All evaluations were independently performed by three individual researchers to ensure the accurate inclusion of studies.
Data collection
Three investigators independently extracted the data from eligible studies using a predefined form. The collected data included the name of first author, the publication year, patients’ country of origin, tumor type, number of patients, sex, cancer stage or grade, percentage showing high CXCR3 expression and the corresponding cutoff value, and outcome. Multivariate HRs and 95% CIs were chosen if both univariate and multivariate results were reported in an individual study. For studies that presented only Kaplan–Meier curves, Engauge Digitizer version 4.1 was used to extract the survival data.19 The estimated HRs and 95% CIs were calculated by Tierney’s method.18 By checking among the three investigators, the final data collection was performed.
Statistical analysis
Using the data collected from each eligible study, we performed the meta-analysis to evaluate the relationship between solid tumor’s CXCR3 expression and patients’ prognosis. Stata version 14.0 (Stata Corporation, College Station, TX, USA) was used to carry out the statistical analysis. As the outcome endpoints disease-free survival, progression-free survival, and recurrence-free survival are similar in meaning, they were combined and a unified prognostic parameter, TTP, was used for the meta-analysis. The meta-analysis was, therefore, based on two outcome endpoints: OS and TTP. Pooled HRs and 95% CIs for the two outcome endpoints (OS, TTP) were used to evaluate the association of CXCR3 expression with solid tumor prognosis. Pooled RRs and 95% CIs were used to assess the correlations between CXCR3 expression and the clinicopathologic features of solid tumor, including TNM stage, T stage, lymph node metastasis, distant metastasis, and tumor differentiation. Heterogeneity assumption was checked using I2 statistic. I2 values <25% may be considered “low”, values around 50% may be considered “moderate”, and values >75% may be considered “high”.20 When the I2 values were >50%, a random-effect model was used to calculate the pooled HRs or RRs; otherwise, a fixed-effect model was used.21 An observed HR >1 and P<0.05 implied worse prognosis for patients with high CXCR3 expression. An observed RR >1 and P<0.05 implied more advanced clinicopathologic characteristics for the group of high CXCR3 expression.
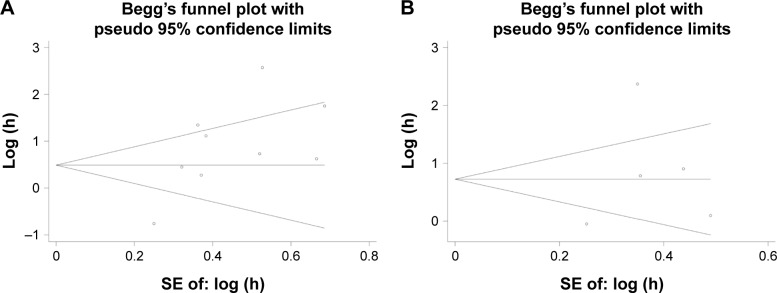
Publication bias and sensitivity analysis
Publication bias was tested using Begg’s funnel plot and Egger’s test.22 If the funnel plot is asymmetric and the Egger’s test reports a P-value of <0.05, publication bias is deemed to be probably existent. Meanwhile, we performed the sensitivity analysis by omitting each study or specific studies to assess the influence of individual studies to the entire meta-analysis.
Data availability
All data generated or analyzed during this study are included in this published article.
Results
Search results
A total of 1,511 articles were retrieved by a comprehensive search from PubMed, Embase, Web of Science, and Cochrane databases. A total of 409 duplicate reports were excluded. After screening the titles and abstracts, 450 articles were excluded for reasons such as commentary, review, author’s view, conference abstracts, and non-English paper. The remaining articles were viewed in full text for further selection. Six hundred and forty articles were excluded for reasons such as animal study, basic research, not about solid tumor or CXCR3, without CXCR3 survival data, sample number ≤40, and duplicated patient population. Finally, 12 studies that reported at least one outcome endpoint were included in this meta-analysis.10–12,23–31 A flowchart of the study selection process is shown in Figure 1.
Figure 1.
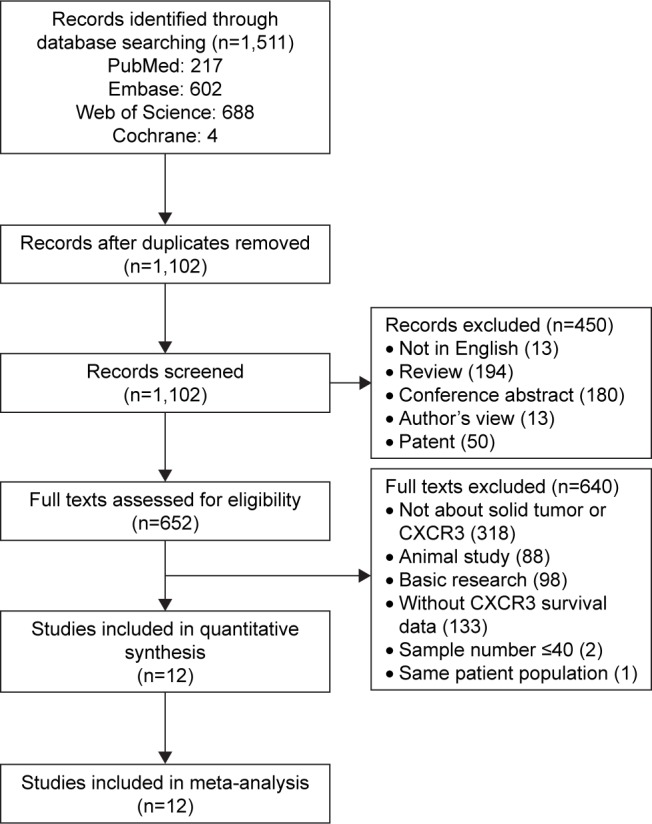
Flow diagram of study selection.
Abbreviation: CXCR3, C–X–C motif chemokine receptor 3.
Characteristics of studies
Detailed information of these eligible studies is summarized in Table 1. In total, the 12 studies provided a sample of 1,751 patients to assess the relationship between CXCR3 expression and solid tumor prognosis. The median sample size was 146, with a range from 45 to 364. Among all the cohorts, China (n=6) became the major source region of literature, followed by USA (n=2), Ireland (n=1), Sweden (n=1), Iran (n=1), and Japan (n=1). As for the cancer type, four studies evaluated colorectal cancer, three studies evaluated breast cancer, two studies evaluated gastric cancer, two studies evaluated renal cancer, and one study evaluated glioblastoma. Nine studies out of 12 focused on overall survival (OS), 3 focused on disease-free survival, 1 focused on progression-free survival, and 1 focused on recurrence-free survival. Various clinicopathologic data were reported in five studies (TNM stage in three studies, pathologic T stage in five studies, lymph node metastasis in three studies, distant metastasis in three studies, and tumor differentiation in five studies). All studies applied immunohistochemical staining to investigate CXCR3 expression. The cutoff values of positive CXCR3 expression varied among different studies, so we classified all the cases according to their original studies (negative or positive staining).
Table 1.
Characteristics of studies included in the meta-analysis
| Reference | Year | Country | Cancer type | Case | Male/female | Stage/grade | Percentage of high CXCR3 expression, cutoff value | Outcome |
|---|---|---|---|---|---|---|---|---|
| Wu et al30 | 2012 | China | Colorectal carcinoma | 112 | 59/53 | NA | 60/112 (53.6%), >25% of cells | OS |
| Kawada et al11 | 2007 | Japan | Colon cancer | 92 | 32/60 | TNM: I–IV | 31/92 (33.7%), >10% of cells | OS |
| Bai et al23 | 2016 | China | Colorectal cancer | 143 | NA | TNM: II | 14/143 (9.8%), NA | OS, DFS |
| Du et al12 | 2014 | China | Colorectal cancer | 145 | 84/61 | TNM: I/II | 26/145 (17.9%), >50% of cells | DFS |
| Zhou et al31 | 2016 | China | Gastric cancer | 103 | 72/31 | Grade: 1–3 | 75/103 (72.8%), NA | OS |
| Li et al26 | 2015 | China | Gastric cancer | 192 | 138/54 | TNM: I–IV | 112/192 (58.33%), >25% of cells | OS |
| Ma et al10 | 2009 | USA | Breast cancer | 75 | 0/75 | NA | 18/75 (24.0%), >75% of cell | OS |
| Mulligan et al27 | 2013 | Ireland | Breast cancer | 261 | NA | Grade: 1–3 | 52/263 (19.8%), >33% of cells | OS |
| Hilborn et al24 | 2014 | Sweden | Breast cancer | 364 | NA | NA | 290/364 (79.7%), NA | CSS, RFS |
| Rezakhaniha et al29 | 2016 | Iran | Renal cell carcinoma | 45 | 28/17 | TNM: I–IV | 34/45 (75.55%), ≥30% of cells | OS |
| Klatte et al25 | 2008 | USA | Clear cell renal cell carcinoma | 154 | 100/54 | Grade: 1–4 | 134/154 (87.0%), ≥30% of cells | DFS |
| Pu et al28 | 2015 | China | Glioblastoma | 65 | 24/41 | NA | 27/65 (41.54%), staining score >4 | OS, PFS |
Abbreviations: CXCR3, C–X–C motif chemokine receptor 3; DFS, disease-free survival; NA, not available; OS, overall survival; PFS, progression-free survival; RFS, recurrence-free survival; CSS, cancer specific survival.
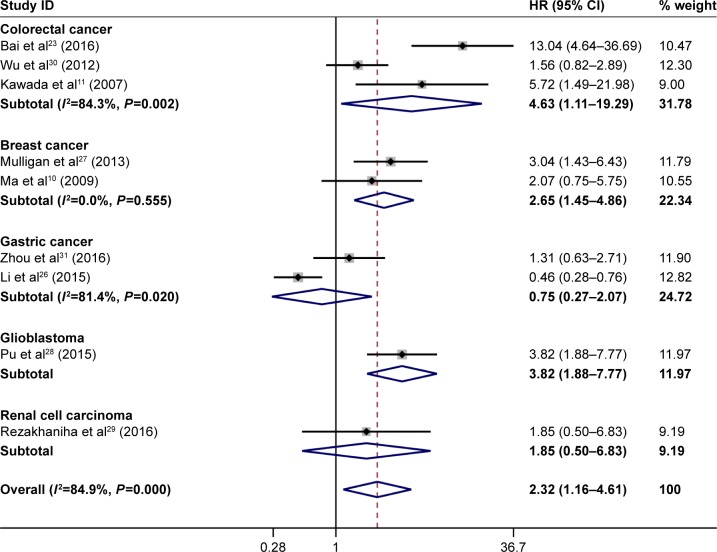
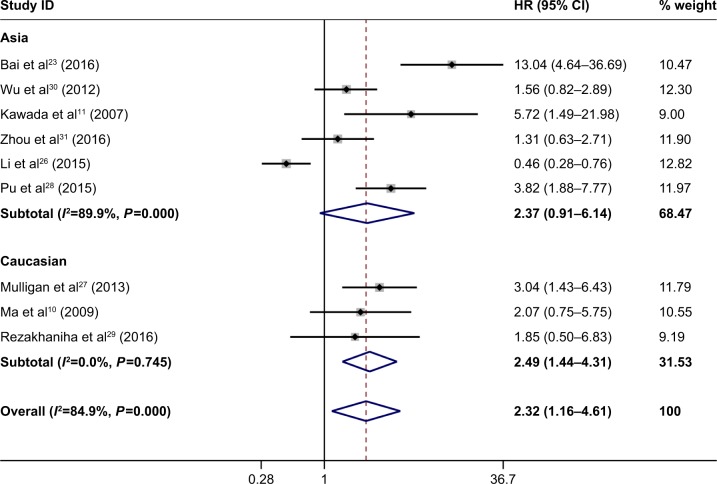
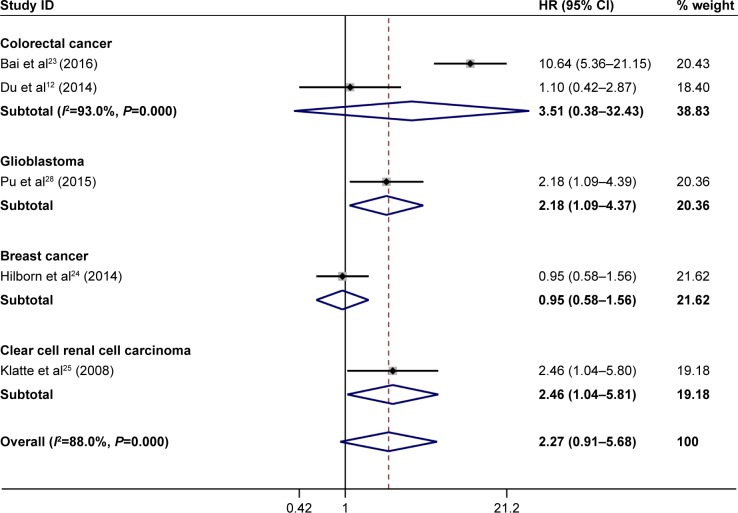
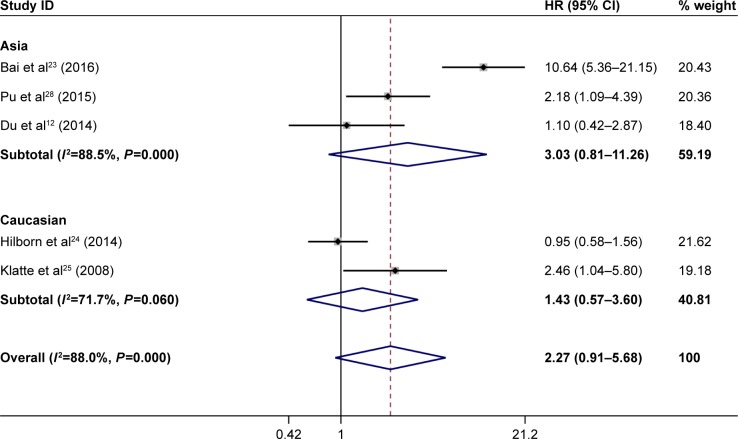
Meta-analysis
The meta-analysis of CXCR3 expression was based on two outcome endpoints: OS and time to tumor progression (TTP). Nine studies were included in the meta-analysis of OS. A random-effect model was applied to calculate the pooled hazard ratio (HR) and 95% CI because the heterogeneity test reported a P<0.001 and an I2 value of 84.9%. The results showed that CXCR3 overexpression was associated with poorer OS of solid tumors (pooled HR =2.315, 95% CI: 1.162–4.611, P=0.017; Figures 2 and 3). Five studies included in the meta-analysis reported TTP. A random-effect model was again used to calculate the pooled HR and 95% CI because the heterogeneity test reported a P<0.001 and an I2 value of 88.0%. The results demonstrated that there was no significant association between CXCR3 overexpression and TTP (pooled HR =2.273, 95% CI: 0.910–5.676, P=0.079; Figure 4). Furthermore, subgroup analysis was stratified by cancer type and races. With regard to race, high CXCR3 expression was associated with poorer OS (a fixed-effect model, HR =2.490, 95% CI: 1.439–4.311, P=0.001) in Caucasian patients while no difference on TTP (Figures 3 and 5; Table 2). For the cancer type, high CXCR3 expression was associated with poorer OS in colorectal cancer (a random-effect model, HR =4.635, 95% CI: 1.114–19.293, P=0.035; I2=84.3%; P=0.002), breast cancer (a fixed-effect model, HR =2.654, 95% CI: 1.449–4.858, P=0.002; I2=0.00%; P=0.555), and glioblastoma (HR =3.823, 95% CI: 1.880–7.773, P<0.001). Meanwhile, high CXCR3 expression was associated with poorer TTP in glioblastoma (HR =2.180, 95% CI: 1.090–4.390, P=0.028) and clear cell renal cell carcinoma (HR =2.460, 95% CI: 1.040–5.800, P=0.040; Figure 4; Table 2).
Figure 2.
Forest plots of studies evaluating CXCR3 expression level and patients’ overall survival with regard to cancer type.
Note: Weights are from random-effects analysis.
Abbreviations: CXCR3, C–X–C motif chemokine receptor 3; HR, hazard ratio.
Figure 3.
Forest plots of studies evaluating CXCR3 expression level and patients’ overall survival with regard to ethnicity.
Note: Weights are from random-effects analysis.
Abbreviations: CXCR3, C–X–C motif chemokine receptor 3; HR, hazard ratio.
Figure 4.
Forest plots of studies evaluating CXCR3 expression level and patients’ TTP.
Notes: Patients’ TTP with regard to cancer type. Weights are from random-effects analysis.
Abbreviations: CXCR3, C–X–C motif chemokine receptor 3; HR, hazard ratio; TTP, time to tumor progression.
Figure 5.
Forest plots of studies evaluating CXCR3 expression level and patients’ TTP.
Notes: Patients’ TTP with regard to race. Weights are from random-effects analysis.
Abbreviations: CXCR3, C–X–C motif chemokine receptor 3; HR, hazard ratio; TTP, time to tumor progression.
Table 2.
Subgroup analysis of pooled HR for solid tumor patients with CXCR3 overexpression
| Outcome | Subgroup | Studies | Pooled HR | 95% CI | P-value | Model | Heterogeneity I2 (%) | P-value |
|---|---|---|---|---|---|---|---|---|
| OS | Cancer type | |||||||
| Colorectal cancer | 3 | 4.635 | 1.114–19.293 | 0.035 | Random | 84.3 | 0.002 | |
| Breast cancer | 2 | 2.654 | 1.449–4.858 | 0.002 | Fixed | 0.0 | 0.555 | |
| Gastric cancer | 2 | 0.752 | 0.273–2.072 | 0.581 | Random | 81.4 | 0.020 | |
| Glioblastoma | 1 | 3.823 | 1.880–7.773 | <0.001 | ||||
| Renal cell carcinoma | 1 | 1.854 | 0.503–6.830 | 0.354 | ||||
| Race | ||||||||
| Asian | 6 | 2.365 | 0.912–6.136 | 0.077 | Random | 89.9 | <0.001 | |
| Caucasian | 3 | 2.490 | 1.439–4.311 | 0.001 | Fixed | 0.0 | 0.745 | |
| TTP | Cancer type | |||||||
| Colorectal cancer | 2 | 3.511 | 0.380–32.434 | 0.268 | Random | 93.0 | <0.001 | |
| Glioblastoma | 1 | 2.180 | 1.090–4.390 | 0.028 | ||||
| Breast cancer | 1 | 0.950 | 0.580–1.560 | 0.839 | ||||
| Clear cell renal cell carcinoma | 1 | 2.460 | 1.040–5.800 | 0.040 | ||||
| Race | ||||||||
| Asian | 3 | 3.028 | 0.814–11.263 | 0.098 | Random | 88.5 | <0.001 | |
| Caucasian | 2 | 1.429 | 0.568–3.596 | 0.449 | Random | 71.7 | 0.060 |
Abbreviations: CXCR3, C–X–C motif chemokine receptor 3; HR, hazard ratio; OS, overall survival; TTP, time to tumor progression; Random, random-effect model; Fixed, fixed-effect model.
In the comprehensive analysis of the role of CXCR3 expression in solid tumors as a biomarker, we investigated the association of high CXCR3 expression and clinicopathologic characteristics in each cancer type. As shown in Table 3, high CXCR3 expression was significantly associated with distant metastasis (yes vs no: relative ratio [RR] =1.828, 95% CI: 1.140–2.931, P=0.012), lymph node metastasis in colorectal cancer (yes vs no: RR =2.28, 95% CI: 1.61–3.25, P<0.001), TNM stage in colorectal cancer (III/IV vs I/II: RR =2.656, 95% CI: 1.809–3.900, P<0.001), and lymph node metastasis in gastric cancer (yes vs no: RR =0.714, 95% CI: 0.610–0.837, P<0.001). However, no significant relationship was observed between CXCR3 overexpression and other clinical characteristics such as T stage and tumor differentiation in solid tumors, which may be due to insufficient data available.
Table 3.
Meta-analysis of the association between high CXCR3 expression and clinicopathologic features of each cancer type
| Variables | Cancer type | Studies | Pooled RR | 95% CI | P-value | Model | Heterogeneity I2 (%) | P-value |
|---|---|---|---|---|---|---|---|---|
| TNM stage | Overall | 3 | 1.654 | 0.641–4.270 | 0.298 | Random | 93.4 | <0.001 |
| Renal cell carcinoma | 1 | 2.206 | 0.604–8.062 | 0.232 | Fixed | – | – | |
| Gastric cancer | 1 | 0.893 | 0.761–1.048 | 0.166 | Fixed | – | – | |
| Colorectal cancer | 1 | 2.656 | 1.809–3.900 | <0.001 | Fixed | – | – | |
| T stage | Overall | 5 | 1.242 | 0.870–1.772 | 0.232 | Random | 88.5 | <0.001 |
| Colorectal cancer | 3 | 1.245 | 0.879–1.764 | 0.217 | Random | 82.1 | 0.004 | |
| Gastric cancer | 2 | 1.448 | 0.294–7.130 | 0.649 | Random | 94.4 | <0.001 | |
| Lymph node metastasis | Overall | 3 | 1.329 | 0.678–2.605 | 0.407 | Random | 94.3 | <0.001 |
| Colorectal cancer | 2 | 2.605 | 1.604–4.230 | <0.001 | Random | 52.2 | 0.148 | |
| Gastric cancer | 1 | 0.714 | 0.610–0.837 | <0.001 | Fixed | – | – | |
| Distant metastasis | Overall | 3 | 1.828 | 1.140–2.931 | 0.012 | Random | 51.2 | 0.129 |
| Colorectal cancer | 2 | 1.770 | 0.955–3.283 | 0.07 | Random | 73.1 | 0.054 | |
| Renal cell carcinoma | 1 | 2.265 | 0.833–6.160 | 0.109 | Fixed | – | – | |
| Tumor differentiation | Overall | 5 | 1.111 | 0.856–1.442 | 0.43 | Random | 76.8 | <0.001 |
| Colorectal cancer | 3 | 1.199 | 0.799–1.799 | 0.381 | Random | 87.0 | <0.001 | |
| Gastric cancer | 1 | 1.160 | 0.897–1.500 | 0.258 | Fixed | – | – | |
| Renal cell carcinoma | 1 | 0.768 | 0.481–1.228 | 0.271 | Fixed | – | – |
Note: “–” indicates no data.
Abbreviations: CXCR3, C–X–C motif chemokine receptor 3; RR, relative ratio; Random, random-effect model; Fixed, fixed-effect model.
Publication bias
Begg’s funnel plot and Egger’s test were used to estimate the publication bias of the included literature. The shapes of the funnel plots for TTP showed no evidence of obvious asymmetry (Figure 6), and Egger’s tests revealed nonsignificant values (P=0.619). However, publication bias may exist for OS (P=0.035) in the analysis of high vs low CXCR3 expression.
Figure 6.
Begg’s funnel plot estimating the publication bias of the included literature.
Note: (A) For CXCR3 and OS and (B) for CXCR3 and TTP.
Abbreviations: CXCR3, C–X–C motif chemokine receptor 3; OS, overall survival; SE, standard error; TTP, time to tumor progression.
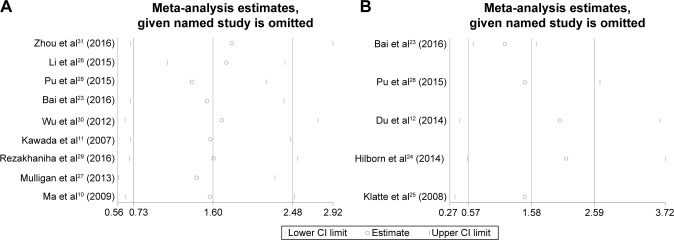
Sensitivity analysis
Moreover, sensitivity analysis was carried out to assess the influence of individual studies on the overall results of OS and TTP. No individual study dominated this meta-analysis, and the removal of any single study had no significant effect on the overall conclusion (Figure 7).
Figure 7.
Sensitivity analysis of this meta-analysis.
Note: (A) For CXCR3 and OS and (B) for CXCR3 and TTP.
Abbreviations: CXCR3, C–X–C motif chemokine receptor 3; OS, overall survival; TTP, time to tumor progression.
Discussion
Our current meta-analysis is so far the only one that has made a comprehensive assessment of the published studies regarding CXCR3 expression and patients’ survival. We systematically analyzed survival data for 1,751 patients with various solid tumors. Among tumors in which CXCR3 overexpression is commonly observed (colorectal cancer, breast cancer, glioblastoma), there was a strong association between CXCR3 overexpression and unfavorable outcome compared with normal CXCR3 expression. Besides, we also evaluated the association between CXCR3 expression and clinicopathologic features, which showed a significant correlation between CXCR3 overexpression and tumor distant metastasis. Especially in colorectal cancer, high CXCR3 expression was related to unfavorable performances such as advanced tumor stage and lymph node metastasis. All these results indicated that CXCR3 probably participates in tumor progression and finally affects tumor prognosis. However, there seemed to be a negative association between high CXCR3 expression and lymph node metastasis in gastric cancer, and one of the two studies regarding gastric cancer, indeed, showed a protective role for CXCR3 in patients’ OS, while the other one showed no significant correlation. We noticed that CXCR3 appeared to act differently in gastric cancer than the other cancer types. Actually, in Li et al’s study, CXCR3 was highly expressed in advanced gastric cancer tissues compared with corresponding paracancerous tissues, which is the same as in other cancer types. However, in advanced gastric cancer tissues, higher CXCR3 correlated with better prognosis.26 To explain this, they suggested a possible pathway that the CXCR3 played a role in recruiting tumor-infiltrating lymphocytes to promote antitumor function resulting in a better prognosis. Due to the limited studies evaluating gastric cancer and the scale of the study, it is hard to make a conclusion here, but we think it is worthy to investigate the underlying mechanism for the divergent performance.
Just like other chemokine receptors, CXCR3 is a seven transmembrane G-protein–coupled receptor which is reported to trigger several downstream pathways such as MAPK, SRC, and PI3K signaling that affect several cellular responses (calcium influx, proliferation, actin rearrangement, migration).32 In tumor organs, CXCR3 is expressed on the tumor cells, stroma cells, and recruited leukocytes, with various ligands also expressed on most of these cells. Consequently, CXCR3 mediated tumor progression directly or indirectly by regulating tumor growth, migration, invasion, angiogenesis, and immunity.32 It has been generally verified that the expression profiles of CXCR3 exhibited a significant increase in metastatic organs compared to corresponding primary cancer tissues in colorectal cancer, breast cancer, and melanoma,10,33,34 further confirming the important role of CXCR3 in tumor progression.
It is notable that CXCR3 is a risk factor for cancer distant metastasis combining all the included cancer types, since metastatic cancers are responsible for about 90% of cancer-related mortality.35 Disseminated cancers are usually more refractory to prior cancer treatments; thus, an ideal strategy is to prevent metastasis by limiting initial dissemination and preventing secondary spread.36 Consequently, CXCR3 may be a promising therapeutic target as increasing evidence has shown its overexpression in many primary and metastatic tumors. Moreover, targeting CXCR3 using its inhibitor AMG487 significantly suppressed metastasis and improved host antitumor immunity in metastatic breast cancer; while CXCR3-knockout mice showed decreased metastasis.16 Though there are no clinical trials regarding CXCR3-targeted therapy currently, it is, indeed, a potential target and more studies are required to verify this. In most cases, chemokines are released locally and their effects are usually confined to local tissues, which are different from those of other cytokines that may cause systemic effects. Thus, CXCR3 could be better targets with less off-target side effects.
In conclusion, this meta-analysis demonstrates that high level of CXCR3 expression is associated shorter OS and tumor metastasis for patients, which suggests that CXCR3 is a valuable prognostic marker and a promising therapeutic target for solid tumors. We are looking forward to see more supportive data regarding CXCR3 in various tumors in the near future.
Footnotes
Author contributions
YZ and MP: concept and design, data collection, data analysis, and drafting the paper. LX: concept and critical revision of the paper. MP: study supervision. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Struyf S, Proost P, Van Damme J. Regulation of the immune response by the interaction of chemokines and proteases. Adv Immunol. 2003;81:1–44. doi: 10.1016/s0065-2776(03)81001-5. [DOI] [PubMed] [Google Scholar]
- 2.Billottet C, Quemener C, Bikfalvi A. CXCR3, a double-edged sword in tumor progression and angiogenesis. Biochim Biophys Acta. 2013;1836(2):287–295. doi: 10.1016/j.bbcan.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Vandercappellen J, Van Damme J, Struyf S. The role of CXC chemokines and their receptors in cancer. Cancer Lett. 2008;267(2):226–244. doi: 10.1016/j.canlet.2008.04.050. [DOI] [PubMed] [Google Scholar]
- 4.Zlotnik A, Yoshie O. Chemokines: a new classification system and their role in immunity. Immunity. 2000;12(2):121–127. doi: 10.1016/s1074-7613(00)80165-x. [DOI] [PubMed] [Google Scholar]
- 5.Hu M, Li K, Maskey N, et al. Corrigendum to “Overexpression of the chemokine receptor CXCR3 and its correlation with favorable prognosis in gastric cancer” (Hum Pathol. 2015;46:1872–1880) Hum Pathol. 2016;54:203–204. doi: 10.1016/j.humpath.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 6.Rot A, von Andrian UH. Chemokines in innate and adaptive host defense: basic chemokinese grammar for immune cells. Annu Rev Immunol. 2004;22:891–928. doi: 10.1146/annurev.immunol.22.012703.104543. [DOI] [PubMed] [Google Scholar]
- 7.Murakami T, Kawada K, Iwamoto M, et al. The role of CXCR3 and CXCR4 in colorectal cancer metastasis. Int J Cancer. 2013;132(2):276–287. doi: 10.1002/ijc.27670. [DOI] [PubMed] [Google Scholar]
- 8.Dagan-Berger M, Feniger-Barish R, Avniel S, et al. Role of CXCR3 carboxyl terminus and third intracellular loop in receptor-mediated migration, adhesion and internalization in response to CXCL11. Blood. 2006;107(10):3821–3831. doi: 10.1182/blood-2004-01-0214. [DOI] [PubMed] [Google Scholar]
- 9.Wu Q, Dhir R, Wells A. Altered CXCR3 isoform expression regulates prostate cancer cell migration and invasion. Mol Cancer. 2012;11:3. doi: 10.1186/1476-4598-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma X, Norsworthy K, Kundu N, et al. CXCR3 expression is associated with poor survival in breast cancer and promotes metastasis in a murine model. Mol Cancer Ther. 2009;8(3):490–498. doi: 10.1158/1535-7163.MCT-08-0485. [DOI] [PubMed] [Google Scholar]
- 11.Kawada K, Hosogi H, Sonoshita M, et al. Chemokine receptor CXCR3 promotes colon cancer metastasis to lymph nodes. Oncogene. 2007;26(32):4679–4688. doi: 10.1038/sj.onc.1210267. [DOI] [PubMed] [Google Scholar]
- 12.Du C, Yao Y, Xue W, Zhu WG, Peng Y, Gu J. The expression of chemokine receptors CXCR3 and CXCR4 in predicting postoperative tumour progression in stages I–II colon cancer: a retrospective study. BMJ Open. 2014;4(8):e005012. doi: 10.1136/bmjopen-2014-005012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Monteagudo C, Martin JM, Jorda E, Llombart-Bosch A. CXCR3 chemokine receptor immunoreactivity in primary cutaneous malignant melanoma: correlation with clinicopathological prognostic factors. J Clin Pathol. 2007;60(6):596–599. doi: 10.1136/jcp.2005.032144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cambien B, Karimdjee BF, Richard-Fiardo P, et al. Organ-specific inhibition of metastatic colon carcinoma by CXCR3 antagonism. Br J Cancer. 2009;100(11):1755–1764. doi: 10.1038/sj.bjc.6605078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walser TC, Rifat S, Ma X, et al. Antagonism of CXCR3 inhibits lung metastasis in a murine model of metastatic breast cancer. Cancer Res. 2006;66(15):7701–7707. doi: 10.1158/0008-5472.CAN-06-0709. [DOI] [PubMed] [Google Scholar]
- 16.Zhu G, Yan HH, Pang Y, et al. CXCR3 as a molecular target in breast cancer metastasis: inhibition of tumor cell migration and promotion of host anti-tumor immunity. Oncotarget. 2015;6(41):43408–43419. doi: 10.18632/oncotarget.6125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu M, Li K, Maskey N, et al. Overexpression of the chemokine receptor CXCR3 and its correlation with favorable prognosis in gastric cancer. Hum Pathol. 2015;46(12):1872–1880. doi: 10.1016/j.humpath.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 18.Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. doi: 10.1186/1745-6215-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y, Cai P, Liang T, Wang L, Hu L. TIM-3 is a potential prognostic marker for patients with solid tumors: a systematic review and meta-analysis. Oncotarget. 2017;8(19):31705–31713. doi: 10.18632/oncotarget.15954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 21.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bai M, Chen X, Ba YI. CXCL10/CXCR3 overexpression as a biomarker of poor prognosis in patients with stage II colorectal cancer. Mol Clin Oncol. 2016;4(1):23–30. doi: 10.3892/mco.2015.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hilborn E, Sivik T, Fornander T, Stal O, Nordenskjold B, Jansson A. C-X-C ligand 10 and C-X-C receptor 3 status can predict tamoxifen treatment response in breast cancer patients. Breast Cancer Res Treat. 2014;145(1):73–82. doi: 10.1007/s10549-014-2933-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klatte T, Seligson DB, Leppert JT, et al. The chemokine receptor CXCR3 is an independent prognostic factor in patients with localized clear cell renal cell carcinoma. J Urol. 2008;179(1):61–66. doi: 10.1016/j.juro.2007.08.148. [DOI] [PubMed] [Google Scholar]
- 26.Li K, Zhu Z, Luo J, et al. Impact of chemokine receptor CXCR3 on tumor-infiltrating lymphocyte recruitment associated with favorable prognosis in advanced gastric cancer. Int J Clin Exp Pathol. 2015;8(11):14725–14732. [PMC free article] [PubMed] [Google Scholar]
- 27.Mulligan AM, Raitman I, Feeley L, et al. Tumoral lymphocytic infiltration and expression of the chemokine CXCL10 in breast cancers from the Ontario Familial Breast Cancer Registry. Clin Cancer Res. 2013;19(2):336–346. doi: 10.1158/1078-0432.CCR-11-3314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pu Y, Li S, Zhang C, Bao Z, Yang Z, Sun L. High expression of CXCR3 is an independent prognostic factor in glioblastoma patients that promotes an invasive phenotype. J Neurooncol. 2015;122(1):43–51. doi: 10.1007/s11060-014-1692-y. [DOI] [PubMed] [Google Scholar]
- 29.Rezakhaniha B, Dormanesh B, Pirasteh H, et al. Immunohistochemical distinction of metastases of renal cell carcinoma with molecular analysis of overexpression of the chemokines CXCR2 and CXCR3 as independent positive prognostic factors for the tumorigenesis. IUBMB Life. 2016;68(8):629–633. doi: 10.1002/iub.1520. [DOI] [PubMed] [Google Scholar]
- 30.Wu Z, Han X, Yan J, et al. The prognostic significance of chemokine receptor CXCR3 expression in colorectal carcinoma. Biomed Pharmacother. 2012;66(5):373–377. doi: 10.1016/j.biopha.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 31.Zhou H, Wu J, Wang T, Zhang X, Liu D. CXCL10/CXCR3 axis promotes the invasion of gastric cancer via PI3K/AKT pathway-dependent MMPs production. Biomed Pharmacother. 2016;82:479–488. doi: 10.1016/j.biopha.2016.04.069. [DOI] [PubMed] [Google Scholar]
- 32.Ma B, Khazali A, Wells A. CXCR3 in carcinoma progression. Histol Histopathol. 2015;30(7):781–792. doi: 10.14670/HH-11-594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rubie C, Kollmar O, Frick VO, et al. Differential CXC receptor expression in colorectal carcinomas. Scand J Immunol. 2008;68(6):635–644. doi: 10.1111/j.1365-3083.2008.02163.x. [DOI] [PubMed] [Google Scholar]
- 34.Kawada K, Taketo MM. Significance and mechanism of lymph node metastasis in cancer progression. Cancer Res. 2011;71(4):1214–1218. doi: 10.1158/0008-5472.CAN-10-3277. [DOI] [PubMed] [Google Scholar]
- 35.Mehlen P, Puisieux A. Metastasis: a question of life or death. Nat Rev Cancer. 2006;6(6):449–458. doi: 10.1038/nrc1886. [DOI] [PubMed] [Google Scholar]
- 36.Wells A, Grahovac J, Wheeler S, Ma B, Lauffenburger D. Targeting tumor cell motility as a strategy against invasion and metastasis. Trends Pharmacol Sci. 2013;34(5):283–289. doi: 10.1016/j.tips.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.